db5917bc761151bf3f5fb9e02b91cb16.ppt
- Количество слайдов: 21
 Charcot-Marie-Tooth CURRENT TOPICS AND TREATMENT OPTIONS IN PODIATRIC MEDICINE AND SURGERY Tuesday, September 27, 2011 New York, NY HAL ORNSTEIN, DPM, FASPS Howell, New Jersey hornstein@aappm. org H
Charcot-Marie-Tooth CURRENT TOPICS AND TREATMENT OPTIONS IN PODIATRIC MEDICINE AND SURGERY Tuesday, September 27, 2011 New York, NY HAL ORNSTEIN, DPM, FASPS Howell, New Jersey hornstein@aappm. org H
 History / Epidemiology • Descriptions since the 1800 s • 1886 Jean Martin Charcot and his student Pierre Marie (France) and Howard Tooth (England) • Prevalence as high as 1/2500 • Autosomal dominant inheritance most common – 36 / 100, 000 • Males > Females • Rare in African Americans • FH of “thin legs / high arches” www. baillement. com
History / Epidemiology • Descriptions since the 1800 s • 1886 Jean Martin Charcot and his student Pierre Marie (France) and Howard Tooth (England) • Prevalence as high as 1/2500 • Autosomal dominant inheritance most common – 36 / 100, 000 • Males > Females • Rare in African Americans • FH of “thin legs / high arches” www. baillement. com
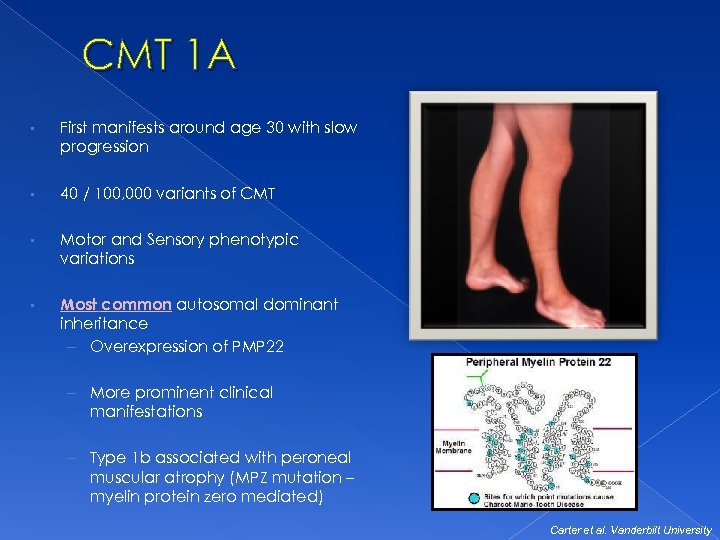 CMT 1 A • First manifests around age 30 with slow progression • 40 / 100, 000 variants of CMT • Motor and Sensory phenotypic variations • Most common autosomal dominant inheritance – Overexpression of PMP 22 – More prominent clinical manifestations – Type 1 b associated with peroneal muscular atrophy (MPZ mutation – myelin protein zero mediated) Carter et al. Vanderbilt University
CMT 1 A • First manifests around age 30 with slow progression • 40 / 100, 000 variants of CMT • Motor and Sensory phenotypic variations • Most common autosomal dominant inheritance – Overexpression of PMP 22 – More prominent clinical manifestations – Type 1 b associated with peroneal muscular atrophy (MPZ mutation – myelin protein zero mediated) Carter et al. Vanderbilt University
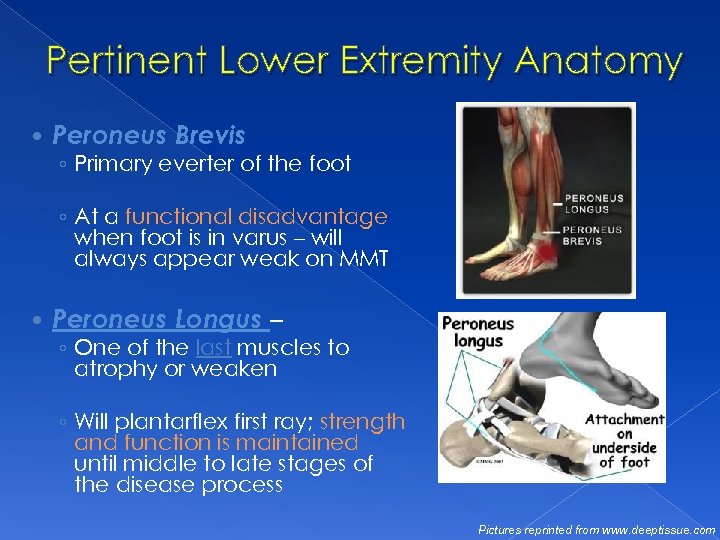 Pertinent Lower Extremity Anatomy Peroneus Brevis ◦ Primary everter of the foot ◦ At a functional disadvantage when foot is in varus – will always appear weak on MMT Peroneus Longus – ◦ One of the last muscles to atrophy or weaken ◦ Will plantarflex first ray; strength and function is maintained until middle to late stages of the disease process Pictures reprinted from www. deeptissue. com
Pertinent Lower Extremity Anatomy Peroneus Brevis ◦ Primary everter of the foot ◦ At a functional disadvantage when foot is in varus – will always appear weak on MMT Peroneus Longus – ◦ One of the last muscles to atrophy or weaken ◦ Will plantarflex first ray; strength and function is maintained until middle to late stages of the disease process Pictures reprinted from www. deeptissue. com
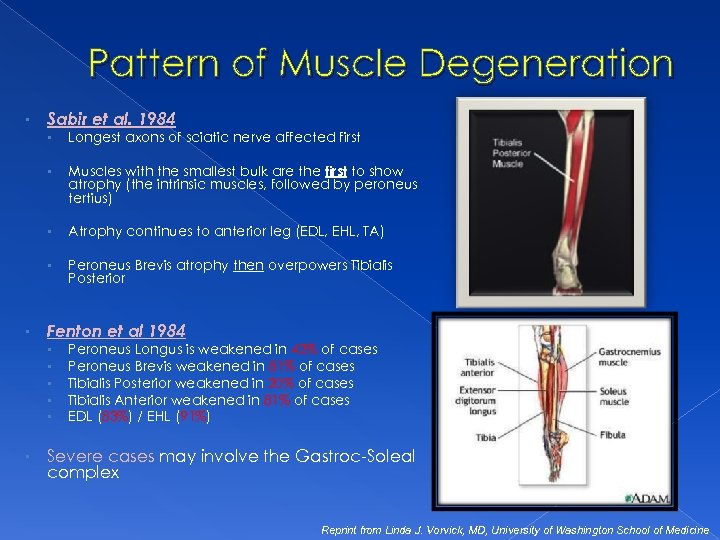 Pattern of Muscle Degeneration • Sabir et al. 1984 • • Muscles with the smallest bulk are the first to show atrophy (the intrinsic muscles, followed by peroneus tertius) • Atrophy continues to anterior leg (EDL, EHL, TA) • • Longest axons of sciatic nerve affected first Peroneus Brevis atrophy then overpowers Tibialis Posterior Fenton et al 1984 • • • Peroneus Longus is weakened in 42% of cases Peroneus Brevis weakened in 81% of cases Tibialis Posterior weakened in 20% of cases Tibialis Anterior weakened in 81% of cases EDL (83%) / EHL (91%) Severe cases may involve the Gastroc-Soleal complex Reprint from Linda J. Vorvick, MD, University of Washington School of Medicine
Pattern of Muscle Degeneration • Sabir et al. 1984 • • Muscles with the smallest bulk are the first to show atrophy (the intrinsic muscles, followed by peroneus tertius) • Atrophy continues to anterior leg (EDL, EHL, TA) • • Longest axons of sciatic nerve affected first Peroneus Brevis atrophy then overpowers Tibialis Posterior Fenton et al 1984 • • • Peroneus Longus is weakened in 42% of cases Peroneus Brevis weakened in 81% of cases Tibialis Posterior weakened in 20% of cases Tibialis Anterior weakened in 81% of cases EDL (83%) / EHL (91%) Severe cases may involve the Gastroc-Soleal complex Reprint from Linda J. Vorvick, MD, University of Washington School of Medicine
 The Role of the Podiatric Physician Palliative Care for callus/corn/keratoderma Professional shoe fitting/ education and modification AFO/bracing fabrication Physical therapy Surgical intervention for recalcitrant deformity Orthotics
The Role of the Podiatric Physician Palliative Care for callus/corn/keratoderma Professional shoe fitting/ education and modification AFO/bracing fabrication Physical therapy Surgical intervention for recalcitrant deformity Orthotics
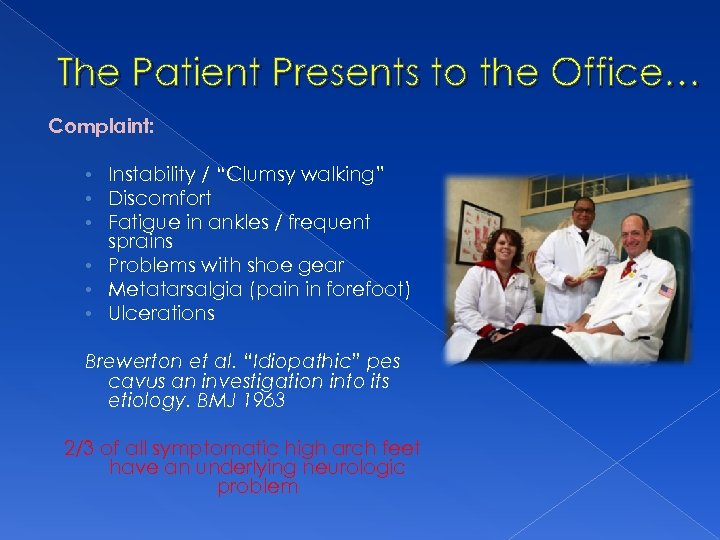 The Patient Presents to the Office… Complaint: • Instability / “Clumsy walking” • Discomfort • Fatigue in ankles / frequent sprains • Problems with shoe gear • Metatarsalgia (pain in forefoot) • Ulcerations Brewerton et al. “Idiopathic” pes cavus an investigation into its etiology. BMJ 1963 2/3 of all symptomatic high arch feet have an underlying neurologic problem
The Patient Presents to the Office… Complaint: • Instability / “Clumsy walking” • Discomfort • Fatigue in ankles / frequent sprains • Problems with shoe gear • Metatarsalgia (pain in forefoot) • Ulcerations Brewerton et al. “Idiopathic” pes cavus an investigation into its etiology. BMJ 1963 2/3 of all symptomatic high arch feet have an underlying neurologic problem
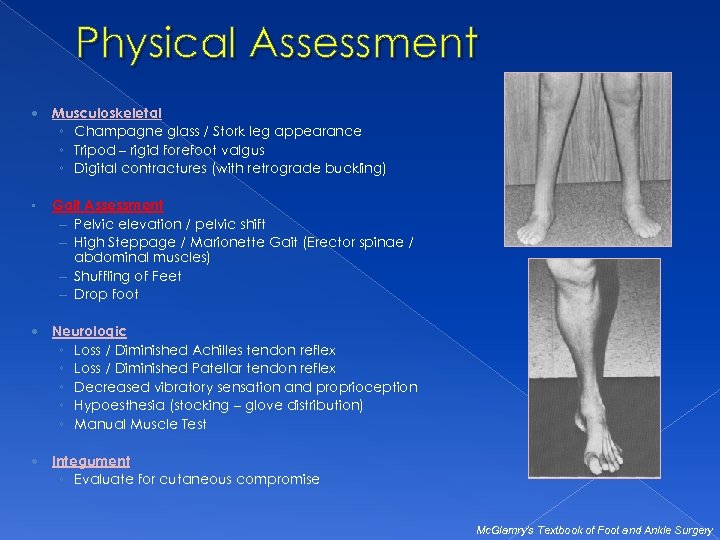 Physical Assessment Musculoskeletal ◦ Champagne glass / Stork leg appearance ◦ Tripod – rigid forefoot valgus ◦ Digital contractures (with retrograde buckling) • Gait Assessment – Pelvic elevation / pelvic shift – High Steppage / Marionette Gait (Erector spinae / abdominal muscles) – Shuffling of Feet – Drop foot Neurologic ◦ Loss / Diminished Achilles tendon reflex ◦ Loss / Diminished Patellar tendon reflex ◦ Decreased vibratory sensation and proprioception ◦ Hypoesthesia (stocking – glove distribution) ◦ Manual Muscle Test Integument ◦ Evaluate for cutaneous compromise Mc. Glamry’s Textbook of Foot and Ankle Surgery
Physical Assessment Musculoskeletal ◦ Champagne glass / Stork leg appearance ◦ Tripod – rigid forefoot valgus ◦ Digital contractures (with retrograde buckling) • Gait Assessment – Pelvic elevation / pelvic shift – High Steppage / Marionette Gait (Erector spinae / abdominal muscles) – Shuffling of Feet – Drop foot Neurologic ◦ Loss / Diminished Achilles tendon reflex ◦ Loss / Diminished Patellar tendon reflex ◦ Decreased vibratory sensation and proprioception ◦ Hypoesthesia (stocking – glove distribution) ◦ Manual Muscle Test Integument ◦ Evaluate for cutaneous compromise Mc. Glamry’s Textbook of Foot and Ankle Surgery
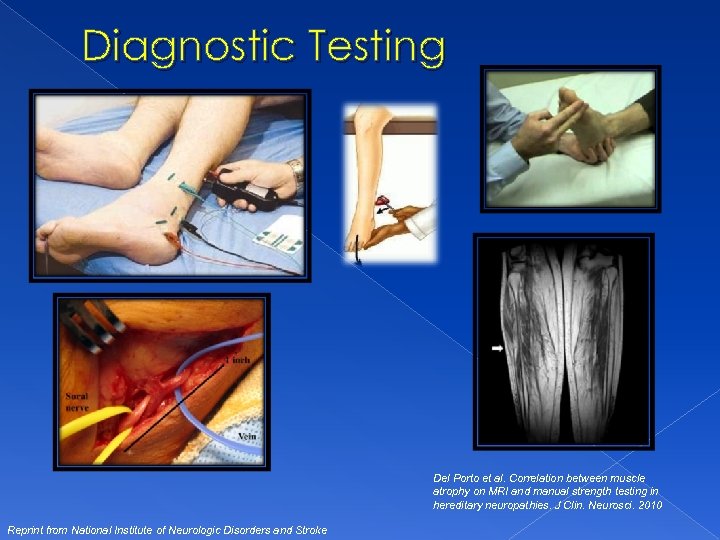 Diagnostic Testing Del Porto et al. Correlation between muscle atrophy on MRI and manual strength testing in hereditary neuropathies. J Clin. Neurosci. 2010 Reprint from National Institute of Neurologic Disorders and Stroke
Diagnostic Testing Del Porto et al. Correlation between muscle atrophy on MRI and manual strength testing in hereditary neuropathies. J Clin. Neurosci. 2010 Reprint from National Institute of Neurologic Disorders and Stroke
 Conservative Treatments • Indicated for: • • • Mechanically controllable deformity Slowly progressive deformity Prevent falling and ankle sprains • Extra depth shoes with accommodative insoles / orthotics +/- metatarsal padding • Decreased inversion 2/2 plantarflexed 1 st ray with custom orthotic • Molded Ankle Foot Orthoses for drop foot +/- double upright brace with spring • Strengthening / stretching programs designed to decrease contracture from secondary muscle imbalance. • • i. e. . Picking up marbles, towel rolling, extensor strengthening exercises Suboptimal results reported for non surgical intervention on severe cavus, cavovarus, or Calcaneovarus deformity
Conservative Treatments • Indicated for: • • • Mechanically controllable deformity Slowly progressive deformity Prevent falling and ankle sprains • Extra depth shoes with accommodative insoles / orthotics +/- metatarsal padding • Decreased inversion 2/2 plantarflexed 1 st ray with custom orthotic • Molded Ankle Foot Orthoses for drop foot +/- double upright brace with spring • Strengthening / stretching programs designed to decrease contracture from secondary muscle imbalance. • • i. e. . Picking up marbles, towel rolling, extensor strengthening exercises Suboptimal results reported for non surgical intervention on severe cavus, cavovarus, or Calcaneovarus deformity
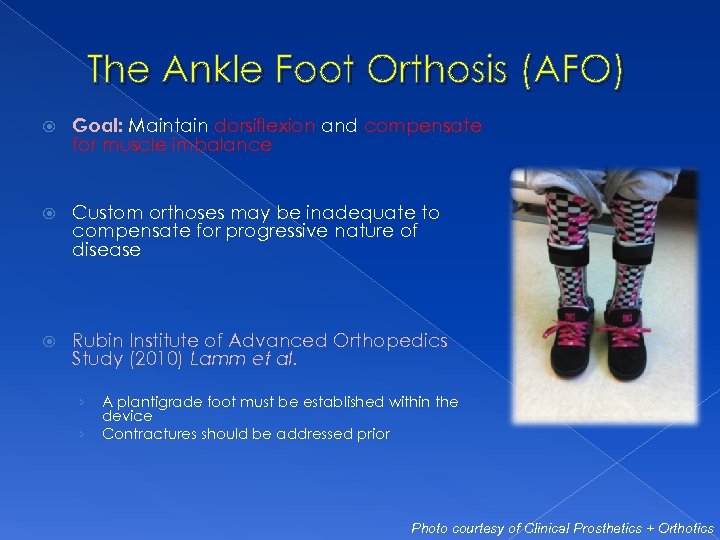 The Ankle Foot Orthosis (AFO) Goal: Maintain dorsiflexion and compensate for muscle imbalance Custom orthoses may be inadequate to compensate for progressive nature of disease Rubin Institute of Advanced Orthopedics Study (2010) Lamm et al. › › A plantigrade foot must be established within the device Contractures should be addressed prior Photo courtesy of Clinical Prosthetics + Orthotics
The Ankle Foot Orthosis (AFO) Goal: Maintain dorsiflexion and compensate for muscle imbalance Custom orthoses may be inadequate to compensate for progressive nature of disease Rubin Institute of Advanced Orthopedics Study (2010) Lamm et al. › › A plantigrade foot must be established within the device Contractures should be addressed prior Photo courtesy of Clinical Prosthetics + Orthotics
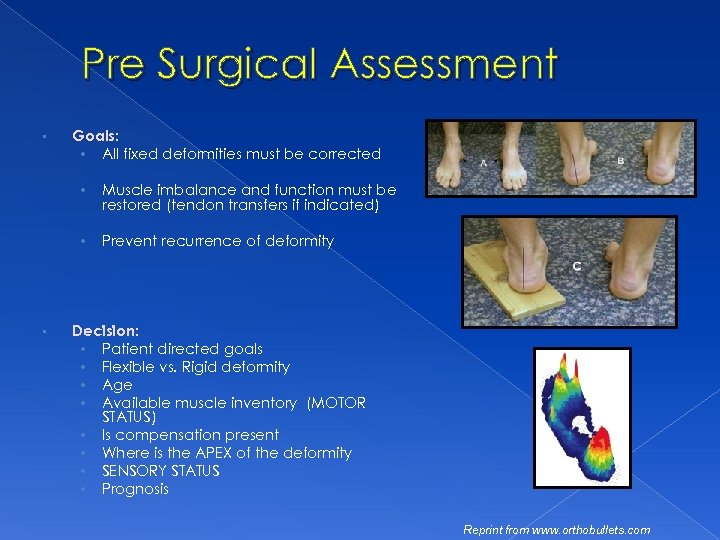 Pre Surgical Assessment • Goals: • All fixed deformities must be corrected • • • Muscle imbalance and function must be restored (tendon transfers if indicated) Prevent recurrence of deformity Decision: • Patient directed goals • Flexible vs. Rigid deformity • Age • Available muscle inventory (MOTOR STATUS) • Is compensation present • Where is the APEX of the deformity • SENSORY STATUS • Prognosis Reprint from www. orthobullets. com
Pre Surgical Assessment • Goals: • All fixed deformities must be corrected • • • Muscle imbalance and function must be restored (tendon transfers if indicated) Prevent recurrence of deformity Decision: • Patient directed goals • Flexible vs. Rigid deformity • Age • Available muscle inventory (MOTOR STATUS) • Is compensation present • Where is the APEX of the deformity • SENSORY STATUS • Prognosis Reprint from www. orthobullets. com
 • Procedures performed during lack of progression have been shown to provide better outcomes • Digital Deformity Correction • Metatarsal Deformity • • Rearfoot Deformity • • Midfoot Deformity Dropfoot Deformity Ankle Equinus Deformity
• Procedures performed during lack of progression have been shown to provide better outcomes • Digital Deformity Correction • Metatarsal Deformity • • Rearfoot Deformity • • Midfoot Deformity Dropfoot Deformity Ankle Equinus Deformity
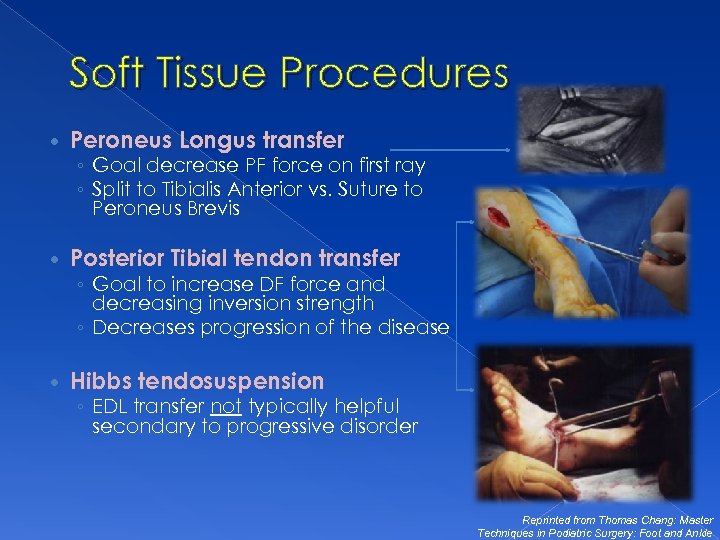 Soft Tissue Procedures Peroneus Longus transfer ◦ Goal decrease PF force on first ray ◦ Split to Tibialis Anterior vs. Suture to Peroneus Brevis Posterior Tibial tendon transfer ◦ Goal to increase DF force and decreasing inversion strength ◦ Decreases progression of the disease Hibbs tendosuspension ◦ EDL transfer not typically helpful secondary to progressive disorder Reprinted from Thomas Chang: Master Techniques in Podiatric Surgery: Foot and Ankle
Soft Tissue Procedures Peroneus Longus transfer ◦ Goal decrease PF force on first ray ◦ Split to Tibialis Anterior vs. Suture to Peroneus Brevis Posterior Tibial tendon transfer ◦ Goal to increase DF force and decreasing inversion strength ◦ Decreases progression of the disease Hibbs tendosuspension ◦ EDL transfer not typically helpful secondary to progressive disorder Reprinted from Thomas Chang: Master Techniques in Podiatric Surgery: Foot and Ankle
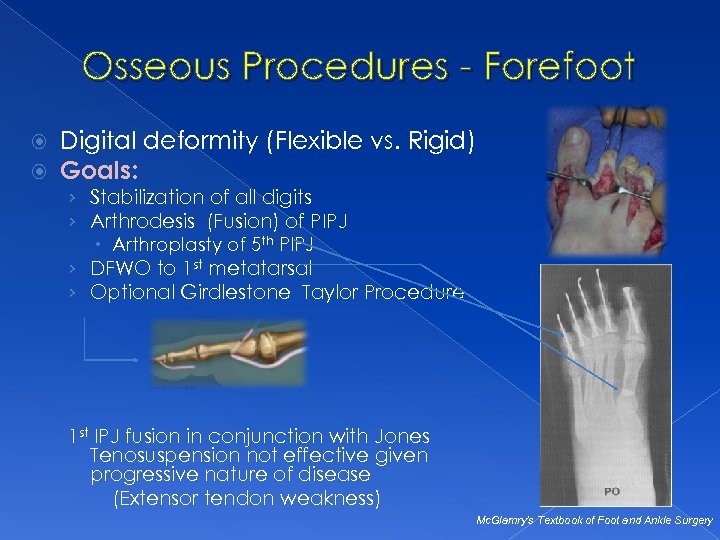 Osseous Procedures - Forefoot Digital deformity (Flexible vs. Rigid) Goals: › Stabilization of all digits › Arthrodesis (Fusion) of PIPJ Arthroplasty of 5 th PIPJ › DFWO to 1 st metatarsal › Optional Girdlestone Taylor Procedure 1 st IPJ fusion in conjunction with Jones Tenosuspension not effective given progressive nature of disease (Extensor tendon weakness) Mc. Glamry’s Textbook of Foot and Ankle Surgery
Osseous Procedures - Forefoot Digital deformity (Flexible vs. Rigid) Goals: › Stabilization of all digits › Arthrodesis (Fusion) of PIPJ Arthroplasty of 5 th PIPJ › DFWO to 1 st metatarsal › Optional Girdlestone Taylor Procedure 1 st IPJ fusion in conjunction with Jones Tenosuspension not effective given progressive nature of disease (Extensor tendon weakness) Mc. Glamry’s Textbook of Foot and Ankle Surgery
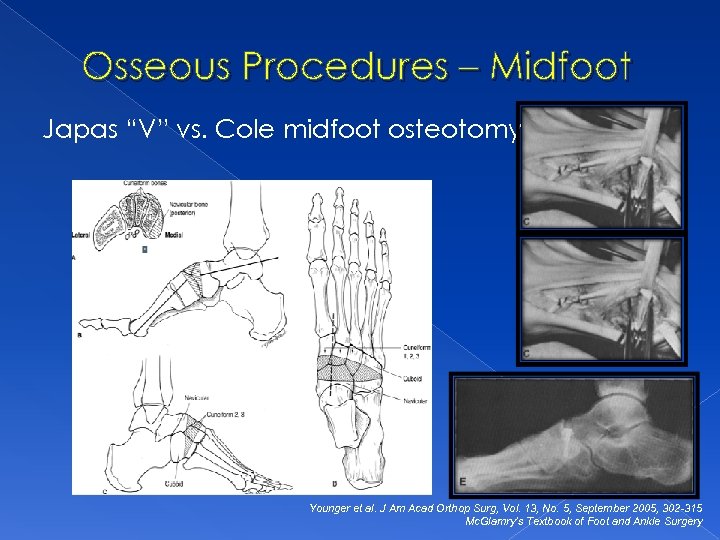 Osseous Procedures – Midfoot Japas “V” vs. Cole midfoot osteotomy Younger et al. J Am Acad Orthop Surg, Vol. 13, No. 5, September 2005, 302 -315 Mc. Glamry’s Textbook of Foot and Ankle Surgery
Osseous Procedures – Midfoot Japas “V” vs. Cole midfoot osteotomy Younger et al. J Am Acad Orthop Surg, Vol. 13, No. 5, September 2005, 302 -315 Mc. Glamry’s Textbook of Foot and Ankle Surgery
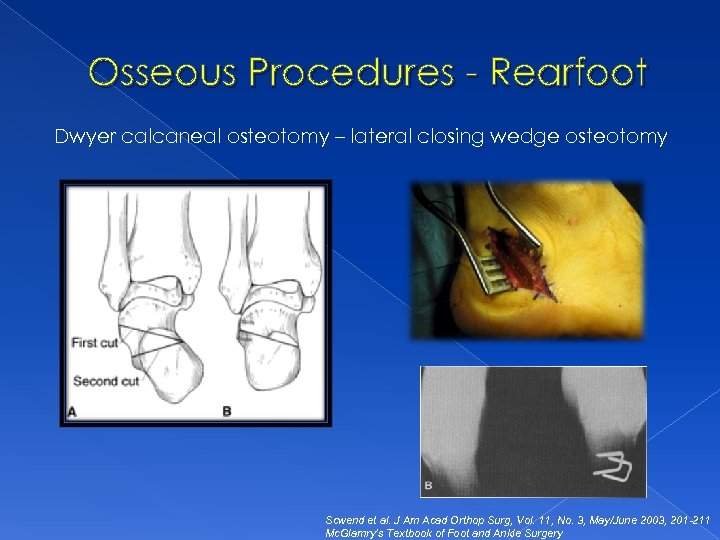 Osseous Procedures - Rearfoot Dwyer calcaneal osteotomy – lateral closing wedge osteotomy Scwend et al. J Am Acad Orthop Surg, Vol. 11, No. 3, May/June 2003, 201 -211 Mc. Glamry’s Textbook of Foot and Ankle Surgery
Osseous Procedures - Rearfoot Dwyer calcaneal osteotomy – lateral closing wedge osteotomy Scwend et al. J Am Acad Orthop Surg, Vol. 11, No. 3, May/June 2003, 201 -211 Mc. Glamry’s Textbook of Foot and Ankle Surgery
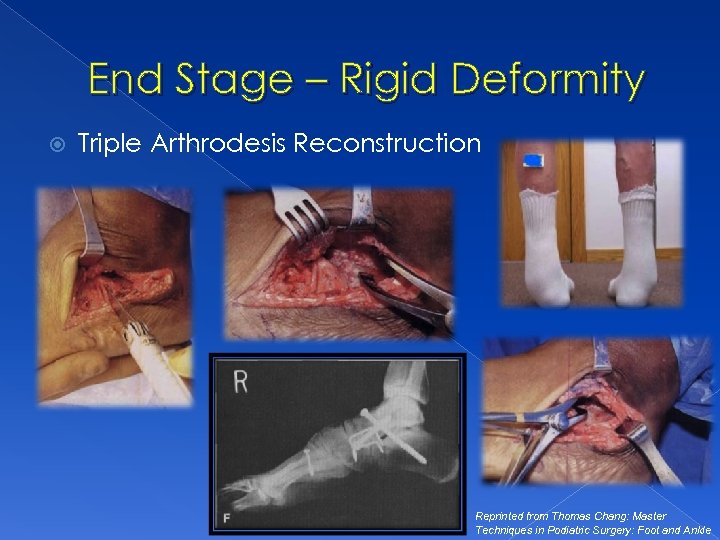 End Stage – Rigid Deformity Triple Arthrodesis Reconstruction Reprinted from Thomas Chang: Master Techniques in Podiatric Surgery: Foot and Ankle
End Stage – Rigid Deformity Triple Arthrodesis Reconstruction Reprinted from Thomas Chang: Master Techniques in Podiatric Surgery: Foot and Ankle
 Conclusions Progressive disease with phenotypic variation Important to weigh physical findings with patient goals for effective treatment strategy Structural deformity will guide prognosis for surgical vs. conservative therapy Podiatric physicians in collaboration with primary care physicians, neurologists, physical therapists / physical medicine & rehabilitation specialists, and genetic counselors are crucial to the interdisciplinary approach to improvement in patient outcomes.
Conclusions Progressive disease with phenotypic variation Important to weigh physical findings with patient goals for effective treatment strategy Structural deformity will guide prognosis for surgical vs. conservative therapy Podiatric physicians in collaboration with primary care physicians, neurologists, physical therapists / physical medicine & rehabilitation specialists, and genetic counselors are crucial to the interdisciplinary approach to improvement in patient outcomes.
 References 1. Berciano J, Gallardo E, Garcıa A, Pelayo-Negro AL, Infante G, Combarros O. New insights into the pathophysiology of pes cavus in Charcot–Marie–Tooth disease type 1 A duplication. J Neurol 2011 2. Brewerton DA, Sandifer PH, Sweetnam DR. Br Med J. 1963 Sep 14; 2(5358): 659 -61 3. Burns J, Ouvrier RA, Yiu EM, et al. Effect of ascorbic acid in patients with Charcot-Marie-Tooth disease type 1 A: a multicentre, randomized, double blind, placebo-controlled trial. Lancet Neurol 2009; 8: 1103. 4. Burns J, Ryan MM, Ouvrier RA. Evolution of Foot and Ankle Manifestations in Children with CMT 1 A. Muscle Nerve 39: 158 – 166, 2009 5. Burns J, Scheinberg A, Ryan MM, Ouvrier RA. Randomized Trial of Botulinum Toxin to Prevent Pes Cavus Progression in Pediatric Charcot-Marie-Tooth Type 1 A. Muscle and Nerve. 262 -7, 2010 6. Chetlin R, Gutmann L, Tarnopolsky M, Ullrich I, Yeater, R. Resistance Training Effectiveness in Patients with Charcot-Marie – Tooth Disease: Recommendations for Exercise Prescription; Arch Phys Med Rehabil 2004; 85: 1217 -1222 7. Croban et al. CMT Facts IV. Treatment of Familial Neuropathies. Vol 4. 1998. 8. Del Porto LA, Nicholson GA, Ketheswaren P. Correlation between muscle atrophy on MRI and manual strength testing in hereditary neuropathies. Journal of Clinical Neuroscience 17 874– 878, 2010 9. Duval A, Kalempokas K, Penicaud A, Guiochon A, Mantel E, Bachmeyer C. Neuropathic leg ulcer indicating late adultonset of Charcot-Marie-Tooth disease. J Am Acad Dermatol (64); 1215 -1216, 2011. 10. Lupski et al. Finding CMT gene ends a quest and begins a new era. Science Med. March 2010. 11. Guyton, G. Orthopaedic Aspects of Charcot-Marie-Tooth Disease. Foot and Ankle International. Vol 27. 2006; 1003 -10. 12. Hewitt SM, Tagoe M. Surgical Management of Pes Cavus Deformity with an Underlying Neurological Disorder: A Case Presentation. JFAS (50) 235– 240, 2011 13. Mc. Glamry’s Comprehensive Textbook of Foot and Ankle Surgery. Third Ed. Section 5: Chapter 34 Charcot- Marie- Tooth Disease. 2001; 1071 -1089 14. Menotti F, Felici F, Damiani A, Mangiola F, Vannicelli R, Macaluso A. Charcot-Marie Tooth 1 A patients with a higher energy cost of walking than healthy individuals; Neuromuscular Disorders 2011; 21: 52 -573 15. Micaleff J, Attarian S, Dubourg O, et al. Effect of ascorbic acid in patients with Charcot Marie Tooth disease type 1 A: a multicentre, randomized, double blind, placebo-controlled trial. Lancet Neurol 2009; 8: 1103 16. Mondelli M. Some considerations on atypical cases of Charcot-Marie-Tooth disease and use of genetic testing in idiopathic polyneuropathies. Clinical Neurology and Neurosurgery 112 (2010) 745– 746 17. Oatis Carol. Charcot-Marie Tooth Disorders: Pathophysiology, Molecular Genetics and Therapy. John Wiley & Sons, Inc. 1990 18. Ramcharitar SI: Lower Extremity Manifestations of Neuromuscular Diseases. Clinics of Podiatric Medicine & Surgery, 15: 722 -724, 1998. 19. Reilly M, Murphy S, Laura M. Charcot-Marie-Tooth Disease. Journal of the Peripheral Nervous System 2011; 16: 1 -14 20. Sreda MW, Meyer zu Horste G, Suter U, et al. Therapeutic administration of progesterone antagonist in a model of Charcot -Marie-Tooth disease (CMT-1 A). Nat Med 2003; 9: 1533 21. Van der Linden MH, Van der Linden SC, A, Hendricks HT, Van Engelen BGM, Geurts ACH. Postural instability in Charcot. Marie-Tooth type 1 A patients is strongly associated with reducedsomatosensation. Gait & Posture 31 (2010) 483– 488 22. Walsh B, Fontera W. Brace modification improves aerobic performance in Charcot-Marie Tooth disease: A single-subject design. AM J Phys Med Rehabil 2001; 80: 578 -582. 23. Ward et al. “Long-Term Results of Reconstruction for Treatment of a Flexible Cavovarus Foot in CMT disease. ” The Journal of Bone and Joint Surgery. 90: 2631 -42. 2008. 24. Westmore et al. “Long-Term Results of Triple Arthrodesis in CMT disease. ” The Journal of Bone and Joint Surgery. 71 -A No 3. 1989.
References 1. Berciano J, Gallardo E, Garcıa A, Pelayo-Negro AL, Infante G, Combarros O. New insights into the pathophysiology of pes cavus in Charcot–Marie–Tooth disease type 1 A duplication. J Neurol 2011 2. Brewerton DA, Sandifer PH, Sweetnam DR. Br Med J. 1963 Sep 14; 2(5358): 659 -61 3. Burns J, Ouvrier RA, Yiu EM, et al. Effect of ascorbic acid in patients with Charcot-Marie-Tooth disease type 1 A: a multicentre, randomized, double blind, placebo-controlled trial. Lancet Neurol 2009; 8: 1103. 4. Burns J, Ryan MM, Ouvrier RA. Evolution of Foot and Ankle Manifestations in Children with CMT 1 A. Muscle Nerve 39: 158 – 166, 2009 5. Burns J, Scheinberg A, Ryan MM, Ouvrier RA. Randomized Trial of Botulinum Toxin to Prevent Pes Cavus Progression in Pediatric Charcot-Marie-Tooth Type 1 A. Muscle and Nerve. 262 -7, 2010 6. Chetlin R, Gutmann L, Tarnopolsky M, Ullrich I, Yeater, R. Resistance Training Effectiveness in Patients with Charcot-Marie – Tooth Disease: Recommendations for Exercise Prescription; Arch Phys Med Rehabil 2004; 85: 1217 -1222 7. Croban et al. CMT Facts IV. Treatment of Familial Neuropathies. Vol 4. 1998. 8. Del Porto LA, Nicholson GA, Ketheswaren P. Correlation between muscle atrophy on MRI and manual strength testing in hereditary neuropathies. Journal of Clinical Neuroscience 17 874– 878, 2010 9. Duval A, Kalempokas K, Penicaud A, Guiochon A, Mantel E, Bachmeyer C. Neuropathic leg ulcer indicating late adultonset of Charcot-Marie-Tooth disease. J Am Acad Dermatol (64); 1215 -1216, 2011. 10. Lupski et al. Finding CMT gene ends a quest and begins a new era. Science Med. March 2010. 11. Guyton, G. Orthopaedic Aspects of Charcot-Marie-Tooth Disease. Foot and Ankle International. Vol 27. 2006; 1003 -10. 12. Hewitt SM, Tagoe M. Surgical Management of Pes Cavus Deformity with an Underlying Neurological Disorder: A Case Presentation. JFAS (50) 235– 240, 2011 13. Mc. Glamry’s Comprehensive Textbook of Foot and Ankle Surgery. Third Ed. Section 5: Chapter 34 Charcot- Marie- Tooth Disease. 2001; 1071 -1089 14. Menotti F, Felici F, Damiani A, Mangiola F, Vannicelli R, Macaluso A. Charcot-Marie Tooth 1 A patients with a higher energy cost of walking than healthy individuals; Neuromuscular Disorders 2011; 21: 52 -573 15. Micaleff J, Attarian S, Dubourg O, et al. Effect of ascorbic acid in patients with Charcot Marie Tooth disease type 1 A: a multicentre, randomized, double blind, placebo-controlled trial. Lancet Neurol 2009; 8: 1103 16. Mondelli M. Some considerations on atypical cases of Charcot-Marie-Tooth disease and use of genetic testing in idiopathic polyneuropathies. Clinical Neurology and Neurosurgery 112 (2010) 745– 746 17. Oatis Carol. Charcot-Marie Tooth Disorders: Pathophysiology, Molecular Genetics and Therapy. John Wiley & Sons, Inc. 1990 18. Ramcharitar SI: Lower Extremity Manifestations of Neuromuscular Diseases. Clinics of Podiatric Medicine & Surgery, 15: 722 -724, 1998. 19. Reilly M, Murphy S, Laura M. Charcot-Marie-Tooth Disease. Journal of the Peripheral Nervous System 2011; 16: 1 -14 20. Sreda MW, Meyer zu Horste G, Suter U, et al. Therapeutic administration of progesterone antagonist in a model of Charcot -Marie-Tooth disease (CMT-1 A). Nat Med 2003; 9: 1533 21. Van der Linden MH, Van der Linden SC, A, Hendricks HT, Van Engelen BGM, Geurts ACH. Postural instability in Charcot. Marie-Tooth type 1 A patients is strongly associated with reducedsomatosensation. Gait & Posture 31 (2010) 483– 488 22. Walsh B, Fontera W. Brace modification improves aerobic performance in Charcot-Marie Tooth disease: A single-subject design. AM J Phys Med Rehabil 2001; 80: 578 -582. 23. Ward et al. “Long-Term Results of Reconstruction for Treatment of a Flexible Cavovarus Foot in CMT disease. ” The Journal of Bone and Joint Surgery. 90: 2631 -42. 2008. 24. Westmore et al. “Long-Term Results of Triple Arthrodesis in CMT disease. ” The Journal of Bone and Joint Surgery. 71 -A No 3. 1989.
 Thank You!!! Life Just Gets Better Hal Ornstein, DPM, FACFAS Affiliated Foot and Ankle Center, LLP 4645 Highway 9 North Howell, New Jersey 07731 732 -905 -1110 hornstein@aappm. org www. footdoctorsnj. com
Thank You!!! Life Just Gets Better Hal Ornstein, DPM, FACFAS Affiliated Foot and Ankle Center, LLP 4645 Highway 9 North Howell, New Jersey 07731 732 -905 -1110 hornstein@aappm. org www. footdoctorsnj. com


