e29e8d6b94cca7f1188bccb94e1c3599.ppt
- Количество слайдов: 46
Chapter 6 Skeletal System: Bones and Bone Tissue
Skeletal System Functions • Support - provides hard framework for soft tissue • Protection of underlying organs – Brain, Eyes, Inner ear structures, heart & lungs, kidneys • Movement - skeletal muscles use bones as levers • Storage. – Calcium and Phosphorous • Stored then released as needed. – Fat stored in marrow cavities • Blood cell production (Hematopoiesis). Bone marrow that gives rise to blood cells and platelets
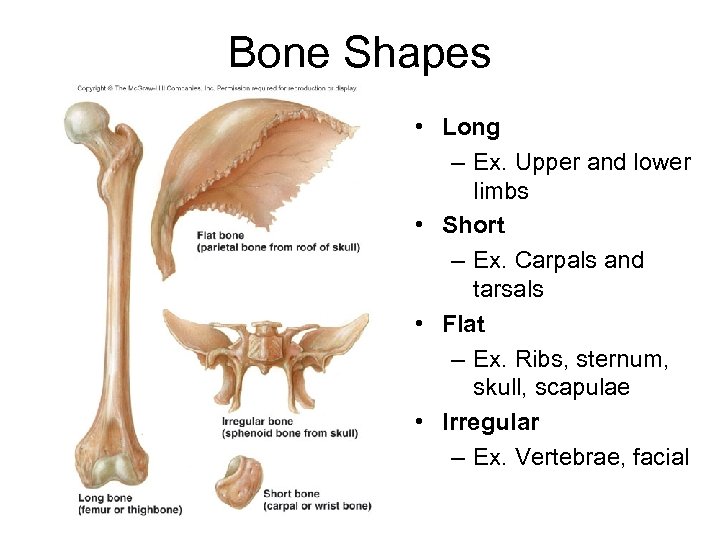
Bone Shapes • Long – Ex. Upper and lower limbs • Short – Ex. Carpals and tarsals • Flat – Ex. Ribs, sternum, skull, scapulae • Irregular – Ex. Vertebrae, facial
Long Bone Structure • Diaphysis – Shaft – Compact bone • Epiphysis – End of the bone – Aka Cancellous bone – Epiphyseal plate - responsible for growth in length of bone • Composed of hyaline cartilage • present until growth stops • Medullary cavity - centra, hollow cavity – filled with yellow marrow • Membranes – Periosteum - surrounds diaphysis – Sharpey’s fibers – Endosteum - lines medullary cavity
Long Bone Structure • Periosteum - membrane surrounding diaphysis – Composed of 2 layers • Outer fibrous layer of collage fibers • Inner osteogenic (bone forming) layer – A single layer of bone cells including osteoblasts, osteoclasts and osteochondral progenitor cells – Fibers of tendon that bind muscle to bone become continuous with fibers of periosteum. – Sharpey’s fibers - periosteal fibers that penetrate into the bone matrix. – Strengthen attachment of tendon to bone. • Endosteum. Similar to inner layer of periosteum. Lines all internal spaces including spaces in cancellous bone.
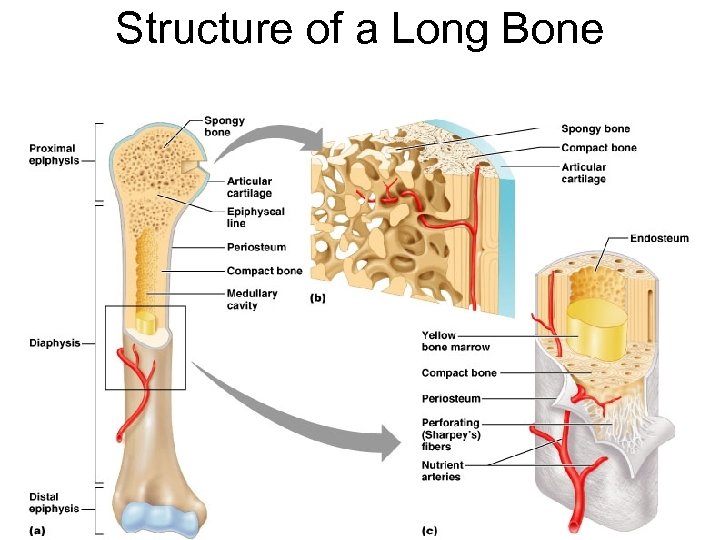
Structure of a Long Bone Figure 6. 3 a-c
Compact Bone • Osteon - basic function unit of compact bone – Central canal - run parallel to surface of bone • contains blood vessels – Concentric lamellae - cylinders of bone – Lacunae - house osteocytes – Canaliculi - minute passageways that lacunae • Processes of osteocytes extend into canaliculi – Perforating or Volkmann’s canal • run perpendicular to long axis. • contain blood vessels that then branch to enter central canal
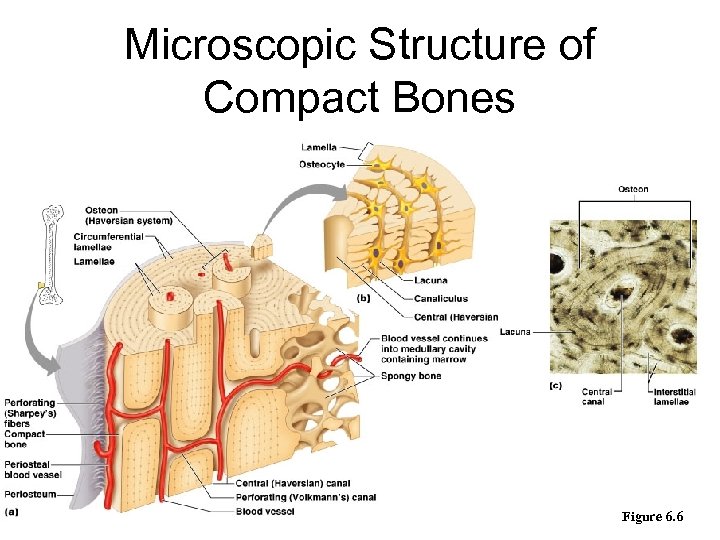
Microscopic Structure of Compact Bones Figure 6. 6
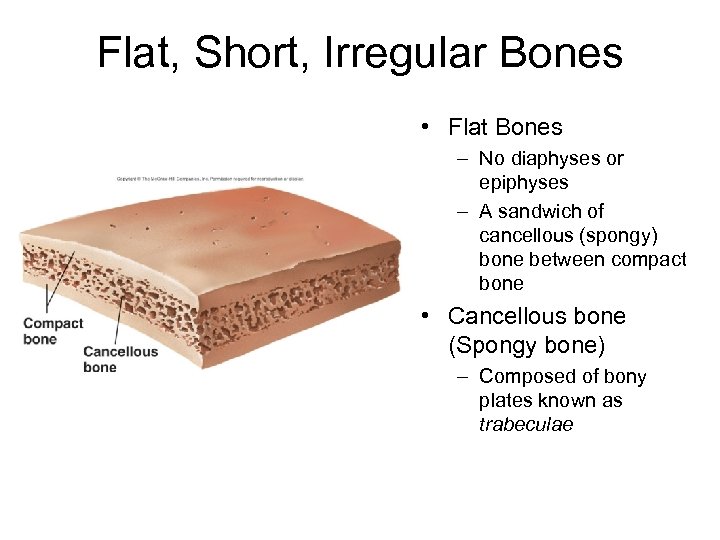
Flat, Short, Irregular Bones • Flat Bones – No diaphyses or epiphyses – A sandwich of cancellous (spongy) bone between compact bone • Cancellous bone (Spongy bone) – Composed of bony plates known as trabeculae
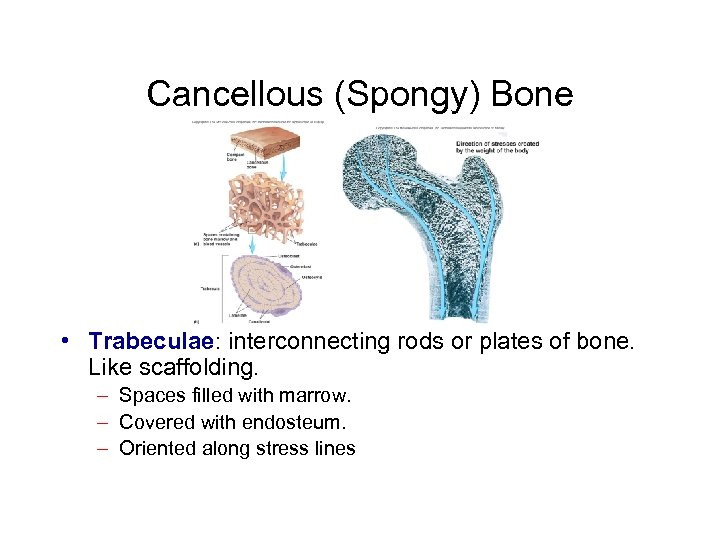
Cancellous (Spongy) Bone • Trabeculae: interconnecting rods or plates of bone. Like scaffolding. – Spaces filled with marrow. – Covered with endosteum. – Oriented along stress lines
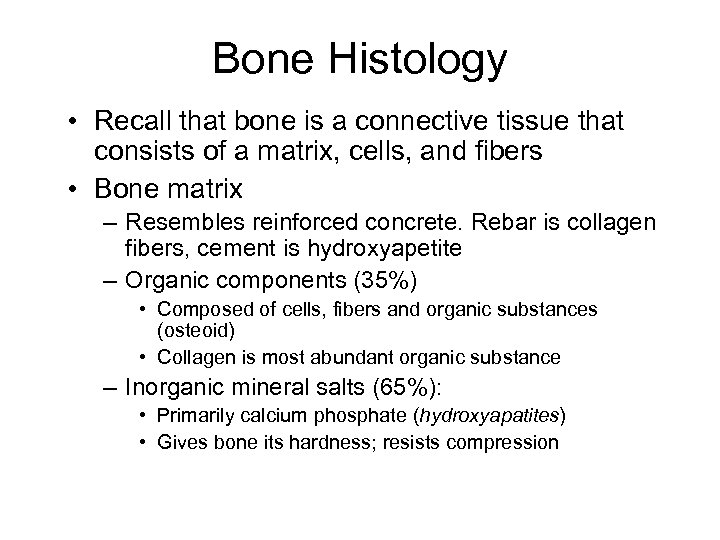
Bone Histology • Recall that bone is a connective tissue that consists of a matrix, cells, and fibers • Bone matrix – Resembles reinforced concrete. Rebar is collagen fibers, cement is hydroxyapetite – Organic components (35%) • Composed of cells, fibers and organic substances (osteoid) • Collagen is most abundant organic substance – Inorganic mineral salts (65%): • Primarily calcium phosphate (hydroxyapatites) • Gives bone its hardness; resists compression
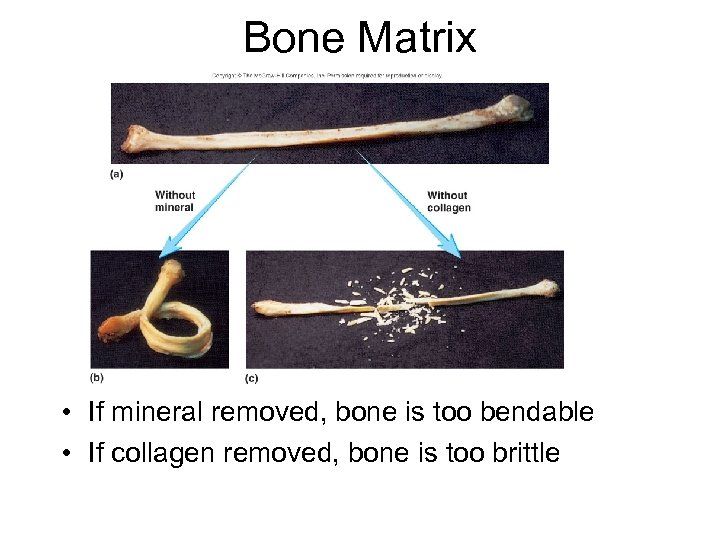
Bone Matrix • If mineral removed, bone is too bendable • If collagen removed, bone is too brittle
Bone Cells • Bone cells (see following slides for particulars) – – Osteoblasts Osteocytes Osteoclasts Stem cells or osteochondral progenitor cells
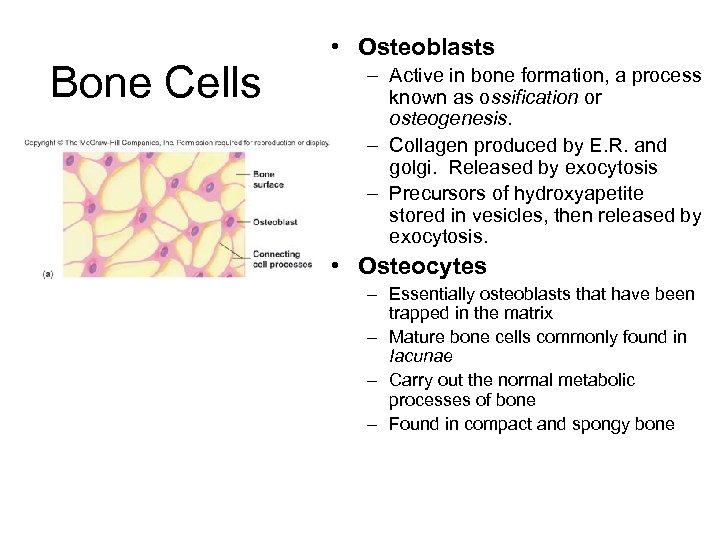
Bone Cells • Osteoblasts – Active in bone formation, a process known as ossification or osteogenesis. – Collagen produced by E. R. and golgi. Released by exocytosis – Precursors of hydroxyapetite stored in vesicles, then released by exocytosis. • Osteocytes – Essentially osteoblasts that have been trapped in the matrix – Mature bone cells commonly found in Iacunae – Carry out the normal metabolic processes of bone – Found in compact and spongy bone
Osteoclasts and Stem Cells • Osteoclasts. – Cells used to breakdown bone (bone resorption) – Ruffled border: where cell membrane borders bone and resorption is taking place. – H+ ions pumped across membrane, acid forms, breaks down mineral salts (demineralization) – Release enzymes that digest the organic proteins of matrix – Derived from monocytes (which are formed from stem cells in red bone marrow) – Multinucleated and probably arise from fusion of a number of cells • Stem Cells. Mesenchyme (Osteochondral Progenitor Cells) become chondroblasts or osteoblasts.
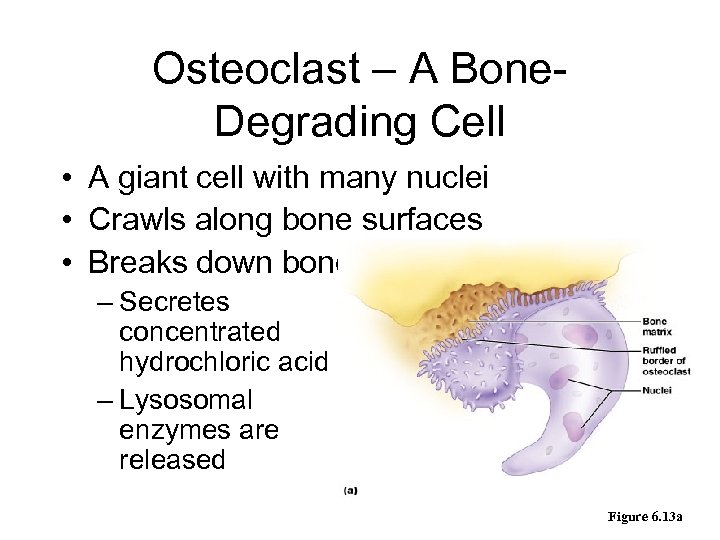
Osteoclast – A Bone. Degrading Cell • A giant cell with many nuclei • Crawls along bone surfaces • Breaks down bone tissue – Secretes concentrated hydrochloric acid – Lysosomal enzymes are released Figure 6. 13 a
Bone Development Osteogenesis • Bone formation occurs in 2 different ways – Intramembranous ossification • Occurs in connective tissue membrane – Endochondral ossification • Occurs in cartilage • Both methods of ossification – Produce woven bone that is then remodeled
Intramembranous Ossification • • • Takes place in connective tissue membrane formed from embryonic mesenchyme Forms many flat skull bones, part of mandible, diaphyses of clavicles When remodeled, indistinguishable from endochondral bone.
Endochondral Ossification • All bones except some bones of the skull and clavicles • Bones are modeled in hyaline cartilage • Begins forming late in 2 nd month of human development • Continues forming until early adulthood
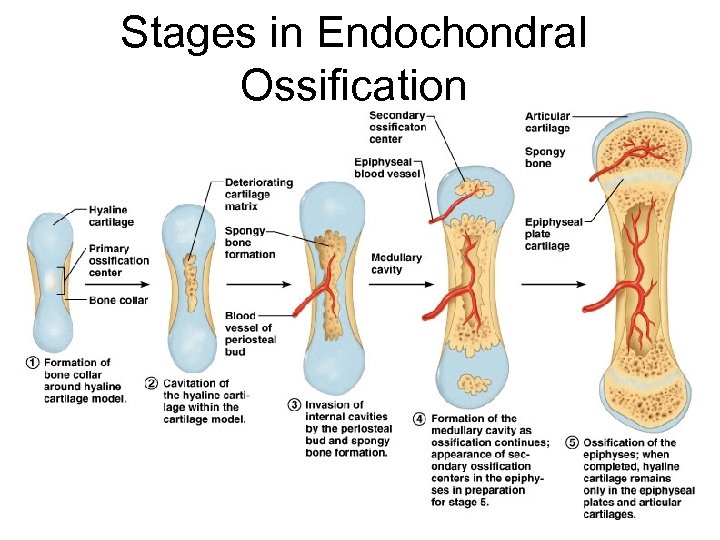
Stages in Endochondral Ossification Figure 6. 10
Anatomy of Epiphyseal Growth Areas • In epiphyseal plates of growing bones – Cartilage is organized for quick, efficient growth – Cartilage cells form tall stacks • Chondroblasts at the top of stacks divide quickly – Pushes the epiphysis away from the diaphysis – Lengthens entire long bone
Anatomy of Epiphyseal Growth Areas • Older chondrocytes signal surrounding matrix to calcify • Older chondrocytes then die and disintegrate – Leaves long trabeculae (spicules) of calcified cartilage on diaphysis side – Trabeculae are partly eroded by osteoclasts – Osteoblasts then cover trabeculae with bone tissue – Trabeculae finally eaten away from their tips by osteoclasts
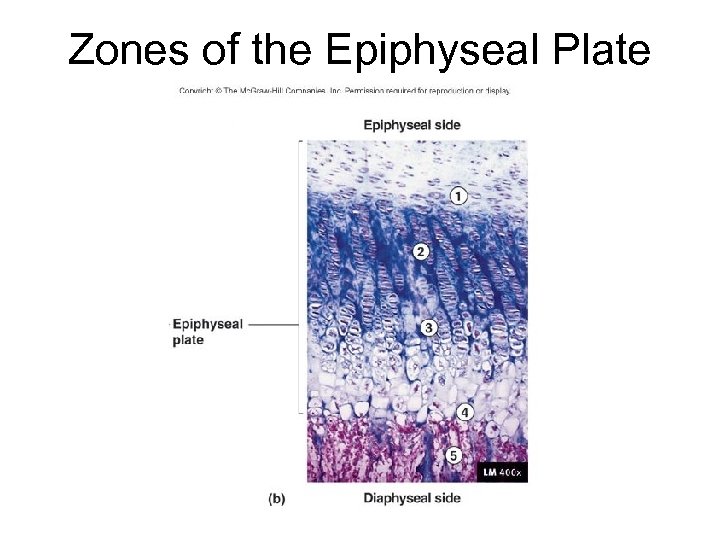
Zones of the Epiphyseal Plate
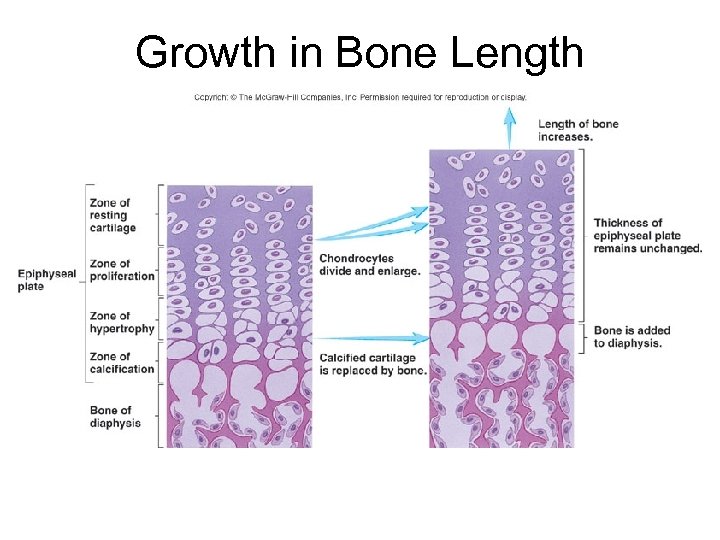
Growth in Bone Length
Postnatal Growth of Endochondral Bones • During childhood and adolescence – Bones lengthen entirely by growth of the epiphyseal plates – Cartilage is replaced with bone tissue as quickly as it grows – Epiphyseal plate maintains constant thickness – Whole bone lengthens
Postnatal Growth of Endochondral Bones • As adolescence draws to an end – Chondroblasts divide less often – Epiphyseal plates become thinner • Cartilage stops growing • Replaced by bone tissue – Long bones stop lengthening when diaphysis and epiphysis fuse
Postnatal Growth of Endochondral Bones • Growing bones widen as they lengthen – Osteoblasts – add bone tissue to the external surface of the diaphysis – Osteoclasts – remove bone from the internal surface of the diaphysis • Appositional growth – growth of a bone by addition of bone tissue to its surface
Bone Remodeling • Bone deposit and removal – Occurs at periosteal and endosteal surfaces • Bone remodeling – Bone deposition – accomplished by osteoblasts – Bone reabsorption – accomplished by osteoclasts
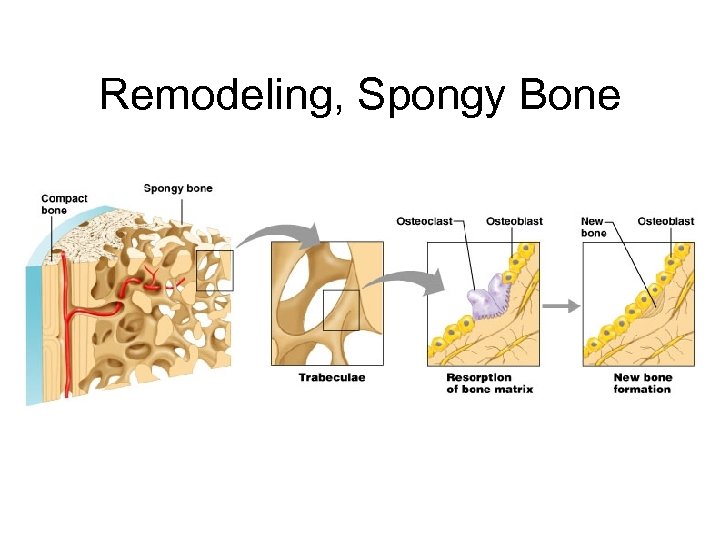
Remodeling, Spongy Bone
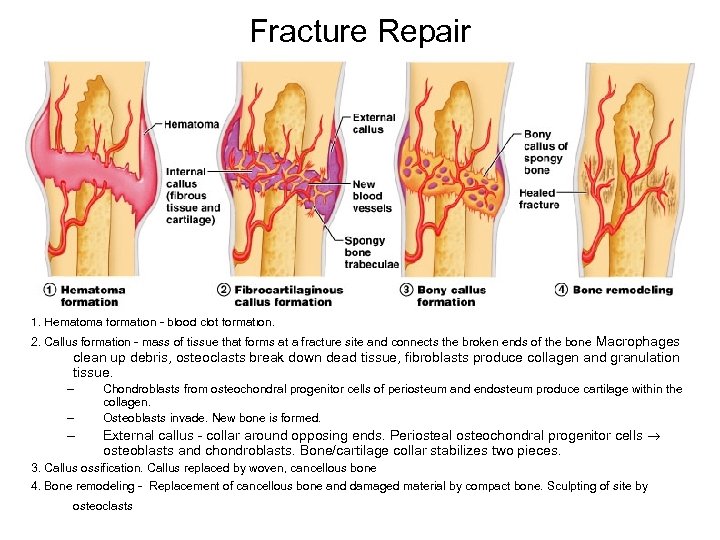
Fracture Repair 1. Hematoma formation - blood clot formation. 2. Callus formation - mass of tissue that forms at a fracture site and connects the broken ends of the bone Macrophages clean up debris, osteoclasts break down dead tissue, fibroblasts produce collagen and granulation tissue. – – – Chondroblasts from osteochondral progenitor cells of periosteum and endosteum produce cartilage within the collagen. Osteoblasts invade. New bone is formed. External callus - collar around opposing ends. Periosteal osteochondral progenitor cells osteoblasts and chondroblasts. Bone/cartilage collar stabilizes two pieces. 3. Callus ossification. Callus replaced by woven, cancellous bone 4. Bone remodeling - Replacement of cancellous bone and damaged material by compact bone. Sculpting of site by osteoclasts
Factors Affecting Bone Growth • Size and shape of a bone determined genetically but can be modified and influenced by nutrition and hormones • Nutrition – Lack of calcium, protein and other nutrients during growth and development can cause bones to be small – Vitamin D • Necessary for absorption of calcium from intestines • Can be eaten or manufactured in the body • Rickets: lack of vitamin D during childhood • Osteomalacia: lack of vitamin D during adulthood leading to softening of bones – Vitamin C • Necessary for collagen synthesis by osteoblasts • Scurvy: due to deficiency of vitamin C • Lack of vitamin C also causes wounds not to heal, teeth to fall out
Dwarfism • Achondroplastic – long bones stop growing in childhood • normal torso, short limbs – spontaneous mutation during DNA replication – failure of cartilage growth • Pituitary – lack of growth hormone – normal proportions with short stature
Factors Affecting Bone Growth, cont. • Hormones – Growth hormone from anterior pituitary. Stimulates interstitial cartilage growth and appositional bone growth – Thyroid hormone required for growth of all tissues – Sex hormones such as estrogen and testosterone • Cause growth at puberty, but also cause closure of the epiphyseal plates and the cessation of growth
Calcium Homeostasis • Bone is major storage site for calcium • The level of calcium in the blood depends upon movement of calcium into or out of bone. – Calcium enters bone when osteoblasts create new bone – Calcium leaves bone when osteoclasts break down bone – Two hormones control blood calcium levelsparathyroid hormone increases it and calcitonin lowers it.
Ion Imbalances • Changes in blood calcium levels can be serious – plasma concentration is ~ 10 mg/d. L – Hypocalcemia - low blood calcium • causes excitability of nervous system if too low – muscle spasms, tremors or tetany ~6 mg/d. L – laryngospasm and suffocation ~4 mg/d. L – Hypercalcemia -excess of blood calcium • muscle weakness and sluggish reflexes, cardiac arrest at ~12 mg/d. L
Control of Hypocalcemia by Parathormone • Secreted by parathyroid glands on posterior surface of thyroid • Released in response to low calcium blood levels (hypocalcemia) • Function = raises calcium blood level – causes osteoblasts to release osteoclast-stimulating factor (RANKL) increasing osteoclast population • Osteoclast in turn increase bone resorption and add Ca to blood – promotes calcium resorption by the kidneys – promotes calcitriol (Vit D) synthesis in the kidneys • Calcitriol then increases calcium absorption by intestines – inhibits collagen synthesis and bone deposition by osteoblasts • Sporatic injection of low levels of PTH causes bone deposition
Calcitriol (Activated Vitamin D) • Produced by the following process – UV radiation and epidermal keratinocytes convert steroid derivative to cholecalciferol - D 3 – liver converts it to calcidiol – kidney converts that to calcitriol (vitamin D) • Calcitriol behaves as a hormone that raises blood calcium concentration – increases intestinal absorption and absorption from the skeleton – increases stem cell differentiation into osteoclasts – promotes urinary reabsorption of calcium ions • Abnormal softness (rickets) in children and (osteomalacia) in adults without vitamin D
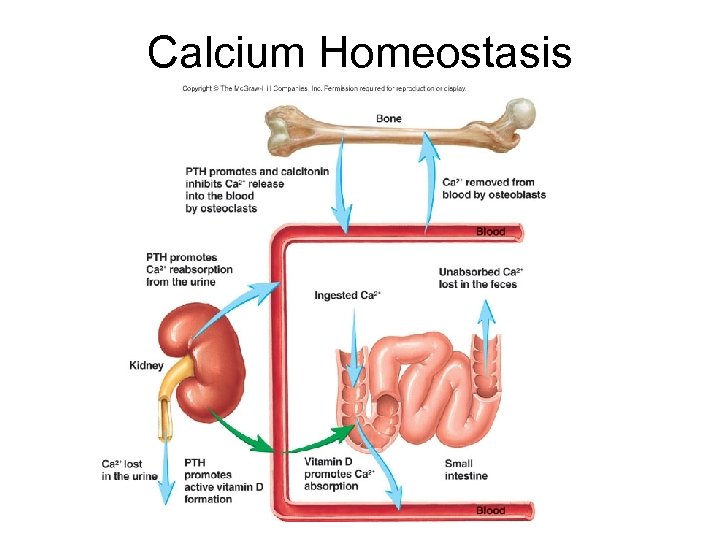
Calcium Homeostasis
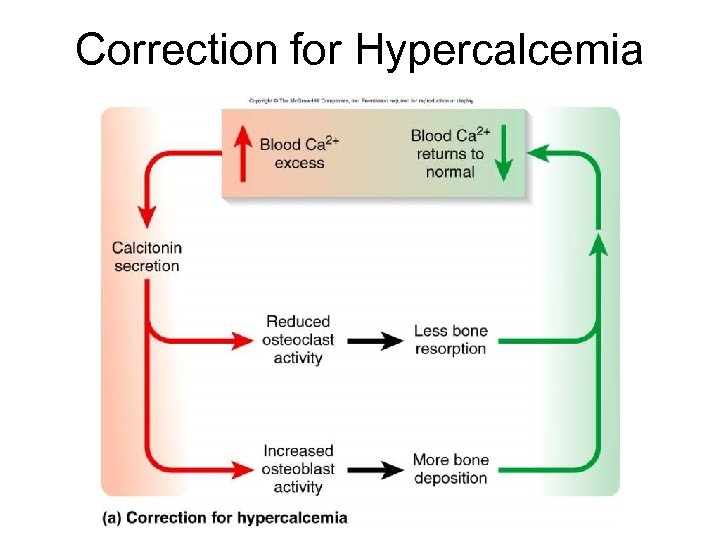
Correction for Hypercalcemia
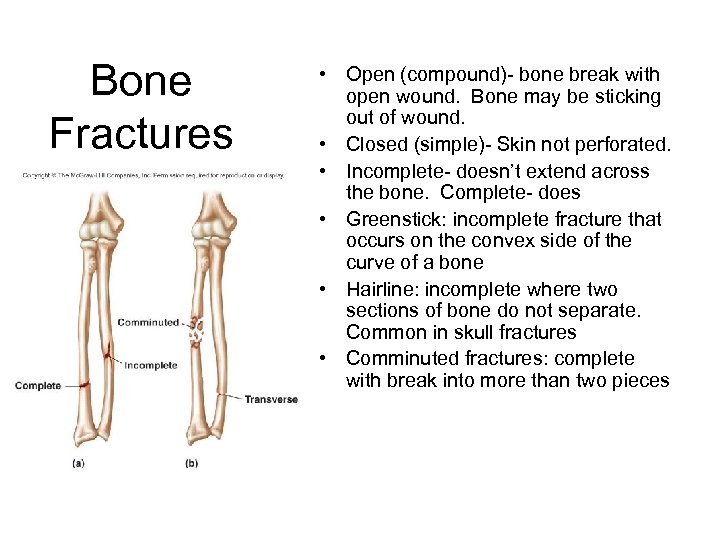
Bone Fractures • Open (compound)- bone break with open wound. Bone may be sticking out of wound. • Closed (simple)- Skin not perforated. • Incomplete- doesn’t extend across the bone. Complete- does • Greenstick: incomplete fracture that occurs on the convex side of the curve of a bone • Hairline: incomplete where two sections of bone do not separate. Common in skull fractures • Comminuted fractures: complete with break into more than two pieces
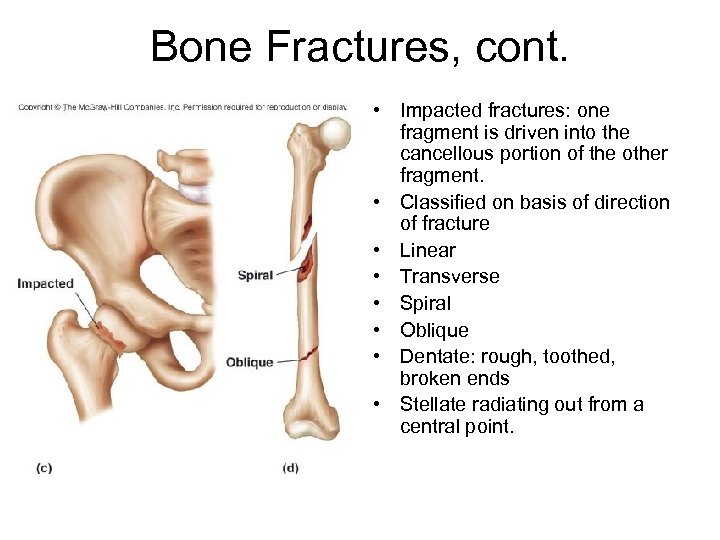
Bone Fractures, cont. • Impacted fractures: one fragment is driven into the cancellous portion of the other fragment. • Classified on basis of direction of fracture • Linear • Transverse • Spiral • Oblique • Dentate: rough, toothed, broken ends • Stellate radiating out from a central point.
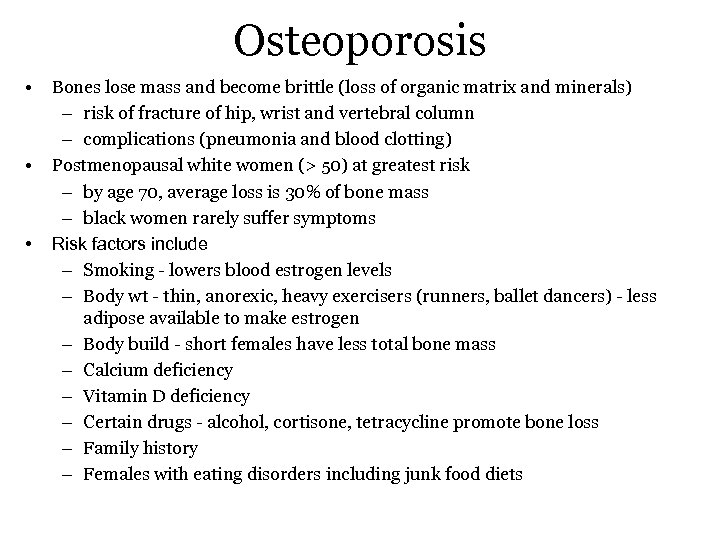
Osteoporosis • • • Bones lose mass and become brittle (loss of organic matrix and minerals) – risk of fracture of hip, wrist and vertebral column – complications (pneumonia and blood clotting) Postmenopausal white women (> 50) at greatest risk – by age 70, average loss is 30% of bone mass – black women rarely suffer symptoms Risk factors include – Smoking - lowers blood estrogen levels – Body wt - thin, anorexic, heavy exercisers (runners, ballet dancers) - less adipose available to make estrogen – Body build - short females have less total bone mass – Calcium deficiency – Vitamin D deficiency – Certain drugs - alcohol, cortisone, tetracycline promote bone loss – Family history – Females with eating disorders including junk food diets
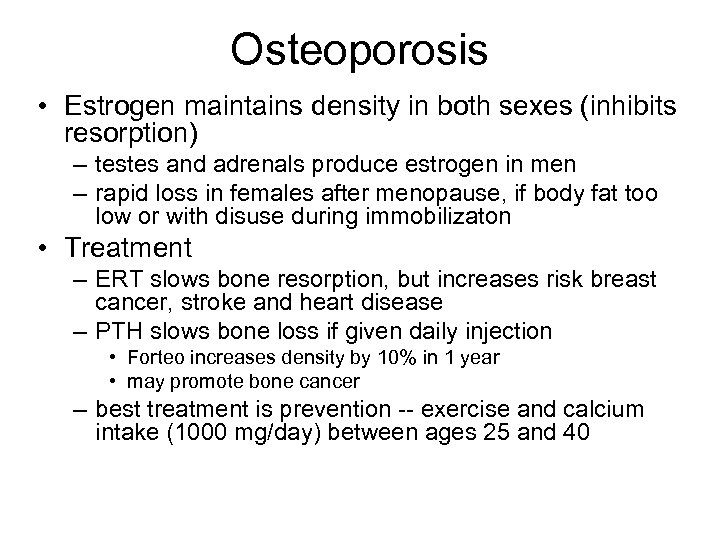
Osteoporosis • Estrogen maintains density in both sexes (inhibits resorption) – testes and adrenals produce estrogen in men – rapid loss in females after menopause, if body fat too low or with disuse during immobilizaton • Treatment – ERT slows bone resorption, but increases risk breast cancer, stroke and heart disease – PTH slows bone loss if given daily injection • Forteo increases density by 10% in 1 year • may promote bone cancer – best treatment is prevention -- exercise and calcium intake (1000 mg/day) between ages 25 and 40
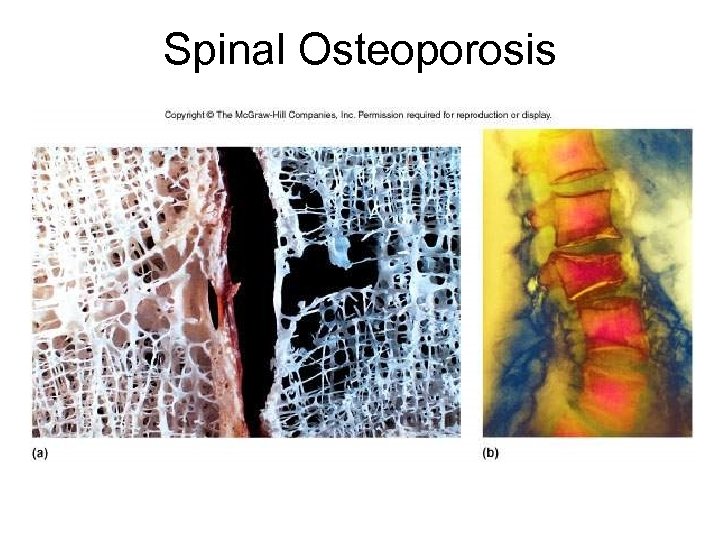
Spinal Osteoporosis
Other Pathologies of Bone • Osteomyelitis - all infectious diseases of bone – Organisms spread via the blood from wounds, boils, TB – Pott’s disease = tuberculosis of the spine (Hunchback) • Osteosarcoma - malignant tumors of bone – Capable of metastasizing to other tissues/organs • Paget’s disease – Characterized by excessive bone formation and breakdown – In males more than females – In skull (hat size changes), pelvis, extremities • Myeloma - cancer of bone marrow • Osteogenesis imperfecta – Familial in nature – Very fragile bones; may break while turning in bed – Due to an inborn error of metabolism - aminoaciduria
Effects of Aging on Skeletal System • Bone matrix decreases. – More brittle due to lack of collagen; but also less hydroxyapetite. • Bone mass decreases. – Highest around 30. – Male bone mass denser due to testosterone and greater weight. – African Americans and Hispanics have higher bone masses than Caucasians and Asians. – Rate of bone loss increases 10 fold after menopause. • Cancellous bone lost first, then compact. • Increased bone fractures • Bone loss causes deformity, loss of height, pain, stiffness – Stooped posture – Loss of teeth
e29e8d6b94cca7f1188bccb94e1c3599.ppt