b38da85a7075b8eeaf56fe90b482ec3f.ppt
- Количество слайдов: 68
 Chapter 6 Nutrition During Lactation Nutrition Through the Life Cycle Judith E. Brown
Chapter 6 Nutrition During Lactation Nutrition Through the Life Cycle Judith E. Brown
 Key Nutrition Concept #1 • Human milk is the best food for newborn infants for the first year of life or longer.
Key Nutrition Concept #1 • Human milk is the best food for newborn infants for the first year of life or longer.
 Key Nutrition Concept #2 • Maternal diet does not significantly alter the protein, carbohydrate, fat and major mineral composition of breast milk, but it does affect the fatty acid profile and the amounts of some vitamins and trace minerals.
Key Nutrition Concept #2 • Maternal diet does not significantly alter the protein, carbohydrate, fat and major mineral composition of breast milk, but it does affect the fatty acid profile and the amounts of some vitamins and trace minerals.
 Key Nutrition Concept #3 • When maternal diet is inadequate, the quality of the milk is preserved over the quantity for the majority of nutrients.
Key Nutrition Concept #3 • When maternal diet is inadequate, the quality of the milk is preserved over the quantity for the majority of nutrients.
 Key Nutrition Concept #4 • Health care policies and procedures and the knowledge and attitudes of health care providers affect community breastfeeding rates.
Key Nutrition Concept #4 • Health care policies and procedures and the knowledge and attitudes of health care providers affect community breastfeeding rates.
 Introduction • Information beneficial to health care professionals to promote breastfeeding is included: – Benefits of breastfeeding – Lactation physiology – Human milk composition – How to breastfeed an infant – Maternal dietary needs – Breastfeeding promotion, facilitation, & support
Introduction • Information beneficial to health care professionals to promote breastfeeding is included: – Benefits of breastfeeding – Lactation physiology – Human milk composition – How to breastfeed an infant – Maternal dietary needs – Breastfeeding promotion, facilitation, & support
 Breastfeeding Goals for the United States “During the twentieth century, infant feeding practices have undergone dramatic changes that reflect shifts in values and attitudes in the U. S. society as a whole. They have tended to occur first among those women at the forefront of changes in dominant social values and among those with resources (whether it is time, energy or money) to permit adoption of new feeding practices. ” − Institute of Medicine, Subcommittee on Nutrition During Lactation, 1991
Breastfeeding Goals for the United States “During the twentieth century, infant feeding practices have undergone dramatic changes that reflect shifts in values and attitudes in the U. S. society as a whole. They have tended to occur first among those women at the forefront of changes in dominant social values and among those with resources (whether it is time, energy or money) to permit adoption of new feeding practices. ” − Institute of Medicine, Subcommittee on Nutrition During Lactation, 1991
 Breastfeeding Goals for the United States • Healthy People 2010 contains wide-ranging national health goals focusing on two major themes: – Increasing the quality and years of healthy life – Eliminating racial and ethnic disparities in health status • A specific objective related to breastfeeding is to “increase the proportion of women who breastfeed”
Breastfeeding Goals for the United States • Healthy People 2010 contains wide-ranging national health goals focusing on two major themes: – Increasing the quality and years of healthy life – Eliminating racial and ethnic disparities in health status • A specific objective related to breastfeeding is to “increase the proportion of women who breastfeed”
 Lactation Physiology Key Terms • Mammary gland – Source of milk for offspring, AKA breast • Alveoli – Rounded or oblong shaped cavity present in breast • Secretory cells – Cells in acinus (milk gland) that are responsible for secreting milk components into ducts
Lactation Physiology Key Terms • Mammary gland – Source of milk for offspring, AKA breast • Alveoli – Rounded or oblong shaped cavity present in breast • Secretory cells – Cells in acinus (milk gland) that are responsible for secreting milk components into ducts
 Lactation Physiology More Key Terms • Myoepithelial cells – Line the alveoli & can contract to cause milk to be secreted into ducts • Oxytocin – Hormone produced during letdown that causes milk to eject into ducts • Lactiferous sinuses – Larger ducts for storage of milk behind the nipple
Lactation Physiology More Key Terms • Myoepithelial cells – Line the alveoli & can contract to cause milk to be secreted into ducts • Oxytocin – Hormone produced during letdown that causes milk to eject into ducts • Lactiferous sinuses – Larger ducts for storage of milk behind the nipple
 Lactation Physiology And More Key Terms • Lobes – Rounded structures of mammary glands • Lactogenesis – Term for human milk production • Prolactin – A hormone necessary for milk production
Lactation Physiology And More Key Terms • Lobes – Rounded structures of mammary glands • Lactogenesis – Term for human milk production • Prolactin – A hormone necessary for milk production
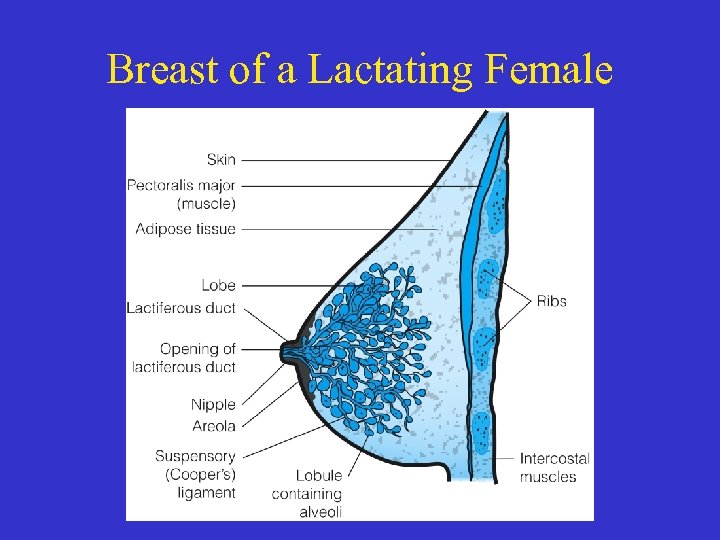 Breast of a Lactating Female
Breast of a Lactating Female
 Functional Units of the Mammary Glands – Avleoli in mammary glands are the functional units – Each is composed of secretory cells with a duct in the center – Myoepithelial cells, that line the alveoli, contract during letdown causing milk ejection – Milk is stored in lactiferous sinuses
Functional Units of the Mammary Glands – Avleoli in mammary glands are the functional units – Each is composed of secretory cells with a duct in the center – Myoepithelial cells, that line the alveoli, contract during letdown causing milk ejection – Milk is stored in lactiferous sinuses
 Mammary Gland Development • During puberty, the ovaries mature with increases in estrogen & progesterone • Hormones impacting lactation and their functions are in Table 6. 3 • Primary hormones contributing to breast development and lactation are: – Estrogen —Progesterone – Human growth hormone —Prolactin – Human placental lactogen —Oxytocin
Mammary Gland Development • During puberty, the ovaries mature with increases in estrogen & progesterone • Hormones impacting lactation and their functions are in Table 6. 3 • Primary hormones contributing to breast development and lactation are: – Estrogen —Progesterone – Human growth hormone —Prolactin – Human placental lactogen —Oxytocin
 Mammary Gland Development
Mammary Gland Development
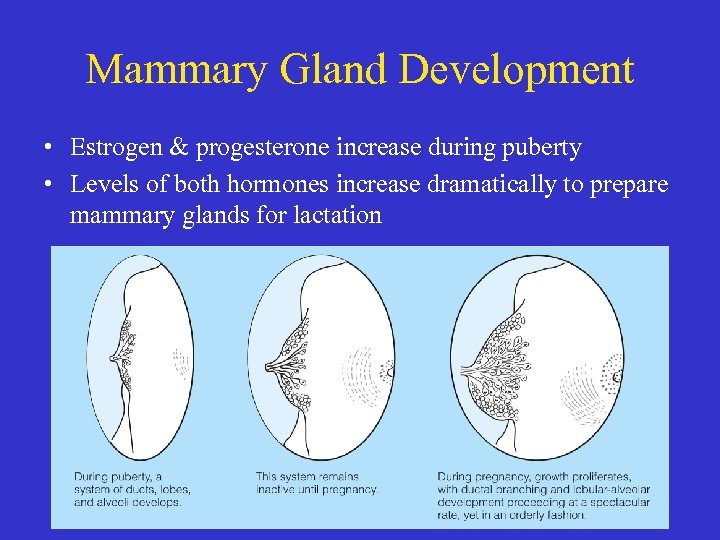 Mammary Gland Development • Estrogen & progesterone increase during puberty • Levels of both hormones increase dramatically to prepare mammary glands for lactation
Mammary Gland Development • Estrogen & progesterone increase during puberty • Levels of both hormones increase dramatically to prepare mammary glands for lactation
 Stages of Lactogenesis • Lactogenesis I (birth to 2 -5 days) milk formation begins • Lactogenesis II—(begins 2 -5 days after birth) increased blood flow to breast; milk “comes in” • Lactogenesis III—(begins at ~10 day after birth) milk composition is stable
Stages of Lactogenesis • Lactogenesis I (birth to 2 -5 days) milk formation begins • Lactogenesis II—(begins 2 -5 days after birth) increased blood flow to breast; milk “comes in” • Lactogenesis III—(begins at ~10 day after birth) milk composition is stable
 Hormonal Control of Lactation • Prolactin – Stimulates milk production – Released in response to suckling, stress, sleep, & sexual intercourse • Oxytocin – Stimulates letdown – Tingling of the breast may occur corresponding to contractions in milk duct – Causes uterus to contract, seal blood vessels, & shrink in size
Hormonal Control of Lactation • Prolactin – Stimulates milk production – Released in response to suckling, stress, sleep, & sexual intercourse • Oxytocin – Stimulates letdown – Tingling of the breast may occur corresponding to contractions in milk duct – Causes uterus to contract, seal blood vessels, & shrink in size
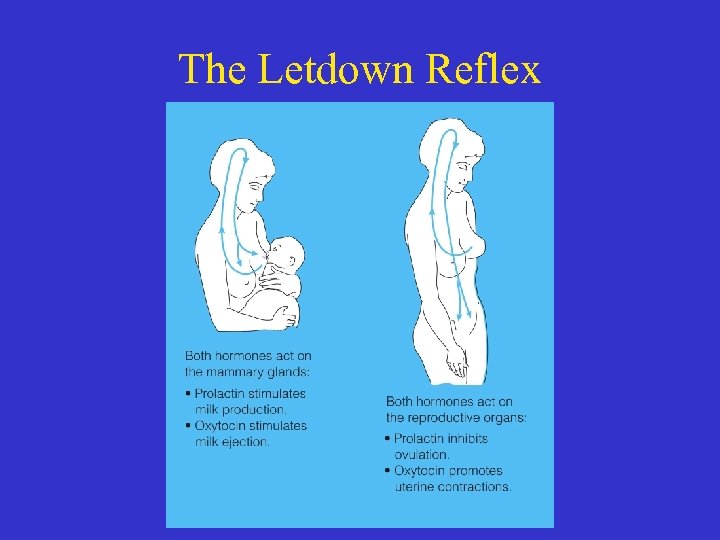 The Letdown Reflex
The Letdown Reflex
 Human Milk Composition • Human milk is the only food needed by the majority of healthy infants for ~ 6 months – It nurtures & protects infants from infectious diseases • The composition changes over a single feeding, over a day, based on age of the infant, presence of infection in the breast, with menses, & maternal nutrition status
Human Milk Composition • Human milk is the only food needed by the majority of healthy infants for ~ 6 months – It nurtures & protects infants from infectious diseases • The composition changes over a single feeding, over a day, based on age of the infant, presence of infection in the breast, with menses, & maternal nutrition status
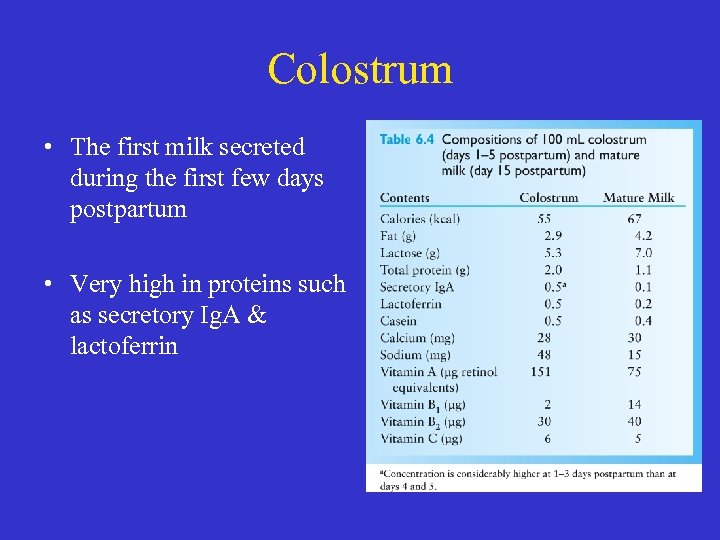 Colostrum • The first milk secreted during the first few days postpartum • Very high in proteins such as secretory Ig. A & lactoferrin
Colostrum • The first milk secreted during the first few days postpartum • Very high in proteins such as secretory Ig. A & lactoferrin
 Water and Energy in Human Milk • Water – Major component in human milk – Isotonic with maternal plasma • Energy – ~0. 65 kcal/m. L – Calories may vary with fat, protein and carbohydrate composition – Lower in calories than human milk substitute (HMS)
Water and Energy in Human Milk • Water – Major component in human milk – Isotonic with maternal plasma • Energy – ~0. 65 kcal/m. L – Calories may vary with fat, protein and carbohydrate composition – Lower in calories than human milk substitute (HMS)
 Lipids in Human Milk • Lipids—provide ½ the calories in human milk • Effect of maternal diet on fat composition – Fatty acid profile reflects dietary intake of mother – Very fat diet with adequate CHO & protein, milk is in medium-chain fatty acids
Lipids in Human Milk • Lipids—provide ½ the calories in human milk • Effect of maternal diet on fat composition – Fatty acid profile reflects dietary intake of mother – Very fat diet with adequate CHO & protein, milk is in medium-chain fatty acids
 DHA, Trans Fatty Acids, and Cholesterol in Human Milk • DHA (docosahexaenoic acid) – Essential for retinal development – Associated with higher IQ scores • Trans fatty acids – Present in human milk from maternal diet • Cholesterol – Higher in human milk than HMS – Early consumption of cholesterol through breast milk appears to be related to lower blood cholesterol levels later in life
DHA, Trans Fatty Acids, and Cholesterol in Human Milk • DHA (docosahexaenoic acid) – Essential for retinal development – Associated with higher IQ scores • Trans fatty acids – Present in human milk from maternal diet • Cholesterol – Higher in human milk than HMS – Early consumption of cholesterol through breast milk appears to be related to lower blood cholesterol levels later in life
 Proteins in Human Milk • Total proteins – Lower than in whole cow’s milk (0. 32 vs. 0. 98 g/oz) – Have antiviral & antimicrobial effects • Casein – Main protein in mature human milk – Facilitates calcium absorption
Proteins in Human Milk • Total proteins – Lower than in whole cow’s milk (0. 32 vs. 0. 98 g/oz) – Have antiviral & antimicrobial effects • Casein – Main protein in mature human milk – Facilitates calcium absorption
 Proteins in Human Milk • Whey – A soluble protein that precipitates by acid or enzyme – Some minerals, hormones & vitamin binding proteins are part of whey • Non-protein nitrogen – ~20 -25% nitrogen in human milk – Used to make non-essential amino acids
Proteins in Human Milk • Whey – A soluble protein that precipitates by acid or enzyme – Some minerals, hormones & vitamin binding proteins are part of whey • Non-protein nitrogen – ~20 -25% nitrogen in human milk – Used to make non-essential amino acids
 Milk Carbohydrates • Lactose – Dominant CHO – Enhances calcium absorption • Oligosaccharides – A medium-length CHO – Prevent binding of pathogenic microorganisms to gut, which prevents infection & diarrhea
Milk Carbohydrates • Lactose – Dominant CHO – Enhances calcium absorption • Oligosaccharides – A medium-length CHO – Prevent binding of pathogenic microorganisms to gut, which prevents infection & diarrhea
 Fat-Soluble Vitamins in Human Milk • Vitamin A – Content in colostrum is ~double that of mature milk – Yellow color from beta-carotene • Vitamin D – Most as 25 -OH 2 vitamin D – Content reflective of mother’s exposure to sun
Fat-Soluble Vitamins in Human Milk • Vitamin A – Content in colostrum is ~double that of mature milk – Yellow color from beta-carotene • Vitamin D – Most as 25 -OH 2 vitamin D – Content reflective of mother’s exposure to sun
 Fat-Soluble Vitamins • Vitamin E – Level linked to milk’s fat content – Level not adequate to meet needs of preterm infants • Vitamin K – ~5% of breastfed infants at risk for K deficiency based on clotting factors – Infants who did not receive K injection at birth may be deficient
Fat-Soluble Vitamins • Vitamin E – Level linked to milk’s fat content – Level not adequate to meet needs of preterm infants • Vitamin K – ~5% of breastfed infants at risk for K deficiency based on clotting factors – Infants who did not receive K injection at birth may be deficient
 Water-Soluble Vitamins in Human Milk • Water soluble in general – Content reflective of mother’s diet – Vitamin most likely to be deficient is B 6 • Vitamin B 12 and folate – Bound to whey proteins – Low B 12 seen in women who: • Have hypothyroidism or latent pernicious anemia • Are vegans or malnourished • Have had gastric bypass
Water-Soluble Vitamins in Human Milk • Water soluble in general – Content reflective of mother’s diet – Vitamin most likely to be deficient is B 6 • Vitamin B 12 and folate – Bound to whey proteins – Low B 12 seen in women who: • Have hypothyroidism or latent pernicious anemia • Are vegans or malnourished • Have had gastric bypass
 Minerals in Human Milk • Minerals contribute to osmolality – Content related to growth of infant – Concentration decreases over 1 st 4 months, except for magnesium • Bioavailability – Most have high bioavailability – Exclusively breastfed infants have very low risk of anemia despite low iron content of human milk
Minerals in Human Milk • Minerals contribute to osmolality – Content related to growth of infant – Concentration decreases over 1 st 4 months, except for magnesium • Bioavailability – Most have high bioavailability – Exclusively breastfed infants have very low risk of anemia despite low iron content of human milk
 Trace Minerals in Human Milk • Zinc – Bound to protein & highly available – Rare defect in mammary gland uptake of zinc may cause zinc deficiency that appears as diaper rash • Other trace minerals – In general, trace minerals are not altered by mother’s diet, excepting Fluoride
Trace Minerals in Human Milk • Zinc – Bound to protein & highly available – Rare defect in mammary gland uptake of zinc may cause zinc deficiency that appears as diaper rash • Other trace minerals – In general, trace minerals are not altered by mother’s diet, excepting Fluoride
 Taste of Human Milk • Flavor of foods in mother’s diet influences taste of breast milk – Infants seem more interested in mother’s milk if flavor is new • Exposure to a variety of flavors may contribute to infant’s interest & acceptance of new flavors in solid foods
Taste of Human Milk • Flavor of foods in mother’s diet influences taste of breast milk – Infants seem more interested in mother’s milk if flavor is new • Exposure to a variety of flavors may contribute to infant’s interest & acceptance of new flavors in solid foods
 Benefits of Breastfeeding for Women • Hormonal benefits – Increased oxytocin stimulates uterus to return to prepregnancy status • Physical benefits – Delay in monthly ovulation resulting in longer intervals between pregnancies • Psychosocial benefits – Increased self-confidence & bonding with infant
Benefits of Breastfeeding for Women • Hormonal benefits – Increased oxytocin stimulates uterus to return to prepregnancy status • Physical benefits – Delay in monthly ovulation resulting in longer intervals between pregnancies • Psychosocial benefits – Increased self-confidence & bonding with infant
 Benefits of Breastfeeding for Infants • Nutritional benefits – Widely recognized – HMS (Human Milk Subs) are created to meet the standards of Human Milk – Nutrients are balanced – Human milk is isotonic – Meets infants’ protein needs without overloading the kidneys – Contains soft, easily digestible curd – Provides generous amounts of the right lipids – Minerals more bioavailable
Benefits of Breastfeeding for Infants • Nutritional benefits – Widely recognized – HMS (Human Milk Subs) are created to meet the standards of Human Milk – Nutrients are balanced – Human milk is isotonic – Meets infants’ protein needs without overloading the kidneys – Contains soft, easily digestible curd – Provides generous amounts of the right lipids – Minerals more bioavailable
 Benefits of Breastfeeding for Infants • Immunological benefits – Lower infant mortality in developing countries – Fewer acute illnesses • Reductions in chronic illnesses – Reduce risk of celiac disease, IBS – Reduce risk of allergies and asthmatic disease • Breastfeeding & childhood overweight – Typically breastfed infants are leaner at 1 year of age
Benefits of Breastfeeding for Infants • Immunological benefits – Lower infant mortality in developing countries – Fewer acute illnesses • Reductions in chronic illnesses – Reduce risk of celiac disease, IBS – Reduce risk of allergies and asthmatic disease • Breastfeeding & childhood overweight – Typically breastfed infants are leaner at 1 year of age
 Benefits of Breastfeeding for Infants • Cognitive benefits – Studies show an increase even after adjusting for family environment as assessed by IQ • Socioeconomic benefits – Decrease need for medical care • Analgesic effects – Reduction of infant pain
Benefits of Breastfeeding for Infants • Cognitive benefits – Studies show an increase even after adjusting for family environment as assessed by IQ • Socioeconomic benefits – Decrease need for medical care • Analgesic effects – Reduction of infant pain
 Breast Milk Supply and Demand • Can women make enough milk? – Milk synthesis is related to: • How vigorously an infant nurses • How much time the infant is at the breast • How many times per day infant nurses • The size of the breast does NOT limit a woman’s ability to nurse • Is feeding frequency related to the amount of milk a woman makes? – Rate of milk synthesis is variable between breasts & between feedings
Breast Milk Supply and Demand • Can women make enough milk? – Milk synthesis is related to: • How vigorously an infant nurses • How much time the infant is at the breast • How many times per day infant nurses • The size of the breast does NOT limit a woman’s ability to nurse • Is feeding frequency related to the amount of milk a woman makes? – Rate of milk synthesis is variable between breasts & between feedings
 Breast Milk Supply and Demand • Pumping or expressing milk – Several different methods are available • • Manually Hand pumps Commercial electric pumps Hospital grade electric pumps – To stimulate adequate milk may require 8 -12 expressions per day
Breast Milk Supply and Demand • Pumping or expressing milk – Several different methods are available • • Manually Hand pumps Commercial electric pumps Hospital grade electric pumps – To stimulate adequate milk may require 8 -12 expressions per day
 Breast Milk Supply and Demand • Can women breastfeed after breast reduction/augmentation? – The type of surgery determines the ability to breastfeed • Does silicone from breast implants leach into the milk? – There is no evidence of direct toxicity to the infant
Breast Milk Supply and Demand • Can women breastfeed after breast reduction/augmentation? – The type of surgery determines the ability to breastfeed • Does silicone from breast implants leach into the milk? – There is no evidence of direct toxicity to the infant
 The Breastfeeding Infant • Optimal duration of breastfeeding – AAP 1 year or longer – U. S. Surgeon General exclusively for 6 months & best to breastfeed for 12 months • Reflexes – Gag reflex—prevents infant from taking things into lungs – Oral search reflex—infant opens mouth wide when close to breast & thrusts tongue forward – Rooting reflex—infant turns to side when stimulated on that side
The Breastfeeding Infant • Optimal duration of breastfeeding – AAP 1 year or longer – U. S. Surgeon General exclusively for 6 months & best to breastfeed for 12 months • Reflexes – Gag reflex—prevents infant from taking things into lungs – Oral search reflex—infant opens mouth wide when close to breast & thrusts tongue forward – Rooting reflex—infant turns to side when stimulated on that side
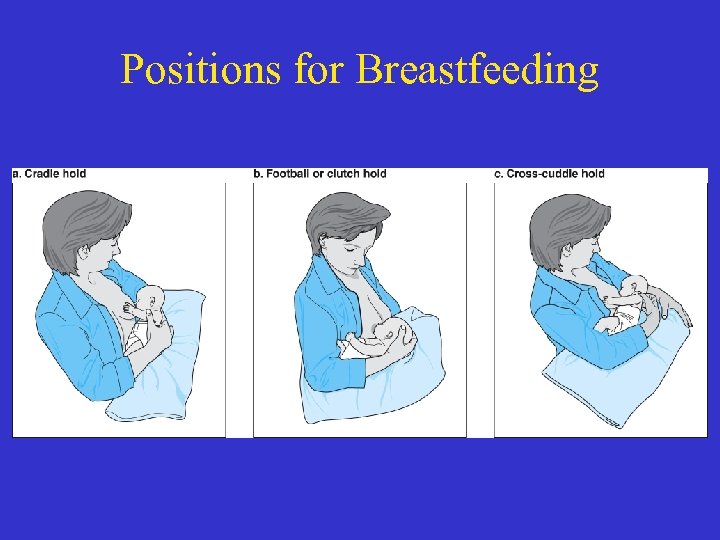 Positions for Breastfeeding
Positions for Breastfeeding
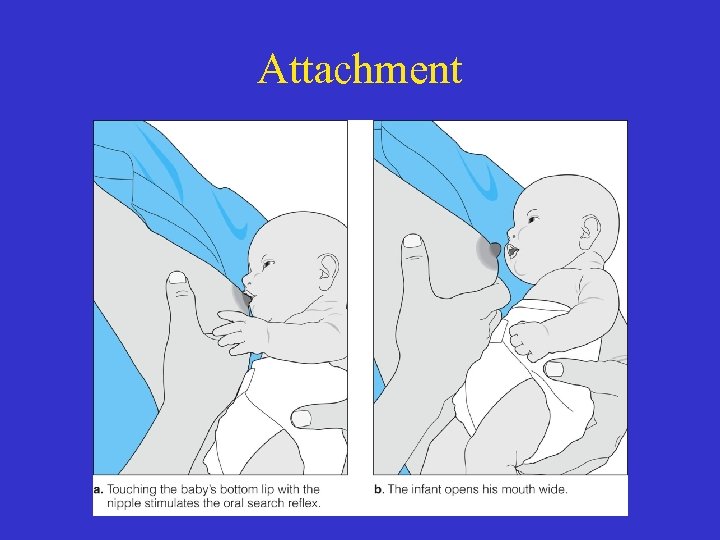 Attachment
Attachment
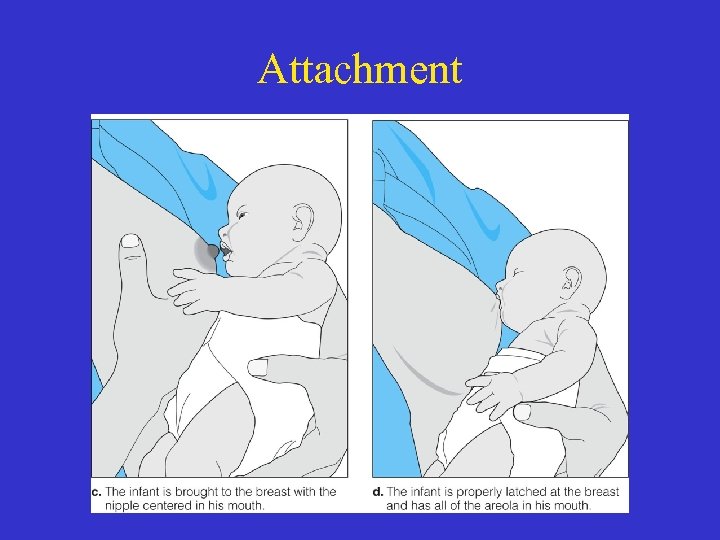 Attachment
Attachment
 The Breastfeeding Infant • Identifying hunger and satiety – Hunger is signaled by infant bringing hands to mouth, sucking on them, & moving head from side to side – Crying is late sign of hunger – Allow infant to nurse on one breast as long as they want to ensure they get hindmilk with its high fat content that provides satiety • Note: High lactose content of foremilk may cause diarrhea
The Breastfeeding Infant • Identifying hunger and satiety – Hunger is signaled by infant bringing hands to mouth, sucking on them, & moving head from side to side – Crying is late sign of hunger – Allow infant to nurse on one breast as long as they want to ensure they get hindmilk with its high fat content that provides satiety • Note: High lactose content of foremilk may cause diarrhea
 The Breastfeeding Infant • Feeding frequency – 10 -12 feedings/day are normal for newborns – Stomach emptying occurs in ~1½ hours • Vitamin supplements for breastfeeding infants – Vitamin K—all U. S. infants receive injections at birth – Vitamin D—exclusively breastfed infants need supplements at 2 months
The Breastfeeding Infant • Feeding frequency – 10 -12 feedings/day are normal for newborns – Stomach emptying occurs in ~1½ hours • Vitamin supplements for breastfeeding infants – Vitamin K—all U. S. infants receive injections at birth – Vitamin D—exclusively breastfed infants need supplements at 2 months
 Identifying Breastfeeding Malnutrition • Normal weight loss for newborns – ~7% of birthweight in 1 st week – Weight loss of 10% needs evaluation by lactation consultant • Malnourished infants become sleepy, nonresponsive, have a weak cry, & wet few diapers – By day 5 to 7, infants should have 6 wet diapers & 3 -4 soiled diapers
Identifying Breastfeeding Malnutrition • Normal weight loss for newborns – ~7% of birthweight in 1 st week – Weight loss of 10% needs evaluation by lactation consultant • Malnourished infants become sleepy, nonresponsive, have a weak cry, & wet few diapers – By day 5 to 7, infants should have 6 wet diapers & 3 -4 soiled diapers
 Tooth Decay • Caries can occur in children who are breastfed • Risk factor is frequent nursing at night after 1 year • All children should be seen 6 months after 1 st tooth erupts or at 1 year of age
Tooth Decay • Caries can occur in children who are breastfed • Risk factor is frequent nursing at night after 1 year • All children should be seen 6 months after 1 st tooth erupts or at 1 year of age
 Maternal Diet • My. Pyramid Food Guide has been adapted for pregnant and breastfeeding women – Dietary Guidelines • Moderate weight reduction can be achieved without compromising the weight gain of the infant – Diets formed around a My. Pyramid Moms food plan provide • Healthy assortment of nutrients at specified calorie levels for each stage of breastfeeding
Maternal Diet • My. Pyramid Food Guide has been adapted for pregnant and breastfeeding women – Dietary Guidelines • Moderate weight reduction can be achieved without compromising the weight gain of the infant – Diets formed around a My. Pyramid Moms food plan provide • Healthy assortment of nutrients at specified calorie levels for each stage of breastfeeding
 Energy and Nutrient Needs for Lactation • Energy needs vary by activity level • DRI is 500 kcal/day for the 1 st 6 months & 400 kcal/day afterward • A single recommendation for energy needs could never address all of the individual variation in energy needs
Energy and Nutrient Needs for Lactation • Energy needs vary by activity level • DRI is 500 kcal/day for the 1 st 6 months & 400 kcal/day afterward • A single recommendation for energy needs could never address all of the individual variation in energy needs
 Maternal Energy Balance and Milk Composition • Protein-calorie malnutrition – Results in reduction in milk volume but not quality • Weight loss during breastfeeding – Theoretically, the caloric DRI assume a loss of 0. 8 kg/month – Most women do not reach prepregnancy weight by 1 year after birth – Modest or short-term energy reductions do not decrease milk production
Maternal Energy Balance and Milk Composition • Protein-calorie malnutrition – Results in reduction in milk volume but not quality • Weight loss during breastfeeding – Theoretically, the caloric DRI assume a loss of 0. 8 kg/month – Most women do not reach prepregnancy weight by 1 year after birth – Modest or short-term energy reductions do not decrease milk production
 Exercising and Breastfeeding • Modest energy restriction combined with increased activity may help women lose weight & body fat • Exercise does not inhibit milk production or infant growth
Exercising and Breastfeeding • Modest energy restriction combined with increased activity may help women lose weight & body fat • Exercise does not inhibit milk production or infant growth
 Other Factors of Maternal Diet • Vitamin and mineral supplements – Not needed in well-nourished women • Functional foods – No adverse effects based on studies to date
Other Factors of Maternal Diet • Vitamin and mineral supplements – Not needed in well-nourished women • Functional foods – No adverse effects based on studies to date
 Other Factors of Maternal Diet • Fluids – Women should drink to thirst • Alternative diets – Type diet determines supplement that may be needed
Other Factors of Maternal Diet • Fluids – Women should drink to thirst • Alternative diets – Type diet determines supplement that may be needed
 Other Factors of Maternal Diet • Infant Colic – Defined as crying for more than 3 hours a day – no medical cause – Components of maternal diet may be related to infant colic – More likely with • Cow’s milk, onions, cabbage, broccoli, & chocolate
Other Factors of Maternal Diet • Infant Colic – Defined as crying for more than 3 hours a day – no medical cause – Components of maternal diet may be related to infant colic – More likely with • Cow’s milk, onions, cabbage, broccoli, & chocolate
 Factors Influencing Breastfeeding Initiation and Duration • Obesity and breastfeeding – Overweight & obesity prior to pregnancy & excess prenatal weight gain breastfeed for shorter duration • Socioeconomic – Both low-income & more affluent mothers need breastfeeding support
Factors Influencing Breastfeeding Initiation and Duration • Obesity and breastfeeding – Overweight & obesity prior to pregnancy & excess prenatal weight gain breastfeed for shorter duration • Socioeconomic – Both low-income & more affluent mothers need breastfeeding support
 Barriers to Breastfeeding Initiation • • • Embarrassment Time & social constraints Lack of support from family & friends Lack of confidence Concerns about diet & health Fear of pain
Barriers to Breastfeeding Initiation • • • Embarrassment Time & social constraints Lack of support from family & friends Lack of confidence Concerns about diet & health Fear of pain
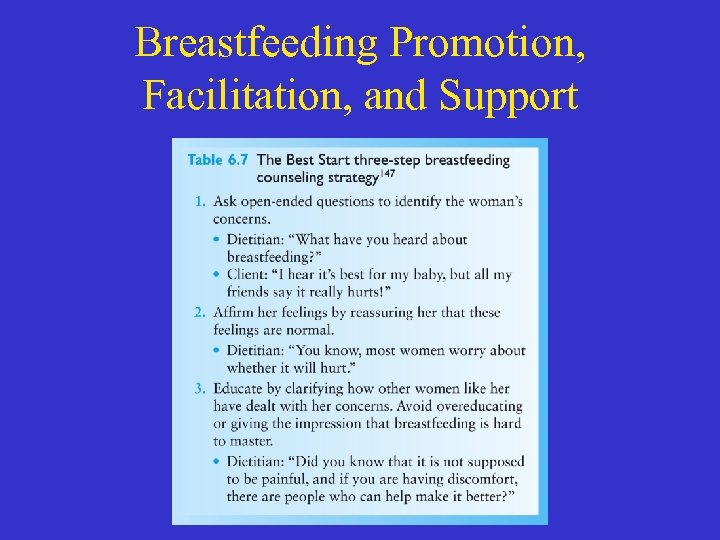
 Breastfeeding Promotion, Facilitation, and Support • Role of the health care system in supporting breastfeeding – Health care system plays an influential role • Prenatal breastfeeding education and support – The Best Start Approach (see Table 6. 7) – Prenatal education is effective in increasing number who chose to breastfeed
Breastfeeding Promotion, Facilitation, and Support • Role of the health care system in supporting breastfeeding – Health care system plays an influential role • Prenatal breastfeeding education and support – The Best Start Approach (see Table 6. 7) – Prenatal education is effective in increasing number who chose to breastfeed
 Breastfeeding Promotion, Facilitation, and Support
Breastfeeding Promotion, Facilitation, and Support
 Breastfeeding Promotion, Facilitation, and Support • Lactation support in hospitals and birthing centers – Hospital practices can influence breastfeeding – Distribution of free formula samples is discouraged – Baby Friendly Hospital Initiative established in 1992
Breastfeeding Promotion, Facilitation, and Support • Lactation support in hospitals and birthing centers – Hospital practices can influence breastfeeding – Distribution of free formula samples is discouraged – Baby Friendly Hospital Initiative established in 1992
 Lactation Support after Discharge • A pediatrician, nurse or other knowledgeable health care practitioner should see all breastfed infants at 2 -4 days of age • Le Leche League – Founded in 1956 – International organization that provides education, information, support & encouragement to women who want to breastfeed
Lactation Support after Discharge • A pediatrician, nurse or other knowledgeable health care practitioner should see all breastfed infants at 2 -4 days of age • Le Leche League – Founded in 1956 – International organization that provides education, information, support & encouragement to women who want to breastfeed
 Breastfeeding Promotion, Facilitation, and Support • Lactation support after discharge – Breastfeeding support is essential in the first few weeks after delivery, as lactation is being established • The work place – Barriers exist such as lack of on-site day care – Insufficiently paid maternity leave – Rigid work schedules – Lack of understanding/knowledge by employers
Breastfeeding Promotion, Facilitation, and Support • Lactation support after discharge – Breastfeeding support is essential in the first few weeks after delivery, as lactation is being established • The work place – Barriers exist such as lack of on-site day care – Insufficiently paid maternity leave – Rigid work schedules – Lack of understanding/knowledge by employers
 Breastfeeding Promotion, Facilitation, and Support • The community – Community attitudes and obstacles to breastfeeding need to be assessed – Barriers to breastfeeding may include • Lack of access to reliable & culturally appropriate sources of information and social support • Cultural perceptions of bottle feeding as norm • Aggressive marketing by formula companies • Laws that prohibit breastfeeding in public
Breastfeeding Promotion, Facilitation, and Support • The community – Community attitudes and obstacles to breastfeeding need to be assessed – Barriers to breastfeeding may include • Lack of access to reliable & culturally appropriate sources of information and social support • Cultural perceptions of bottle feeding as norm • Aggressive marketing by formula companies • Laws that prohibit breastfeeding in public
 The Community • Establish a multidisciplinary breastfeeding task force with representatives from: – Physicians – Hospitals and birthing centers – Public health – Home visitors – La Leche League – Government, industry, & school boards – Journalists
The Community • Establish a multidisciplinary breastfeeding task force with representatives from: – Physicians – Hospitals and birthing centers – Public health – Home visitors – La Leche League – Government, industry, & school boards – Journalists
 Public Food and Nutrition Programs • National Breastfeeding Policy – Title V Maternal and Child Health programs of the Health Resources and Services Administration provide substantial support services, training, and research for breastfeeding
Public Food and Nutrition Programs • National Breastfeeding Policy – Title V Maternal and Child Health programs of the Health Resources and Services Administration provide substantial support services, training, and research for breastfeeding
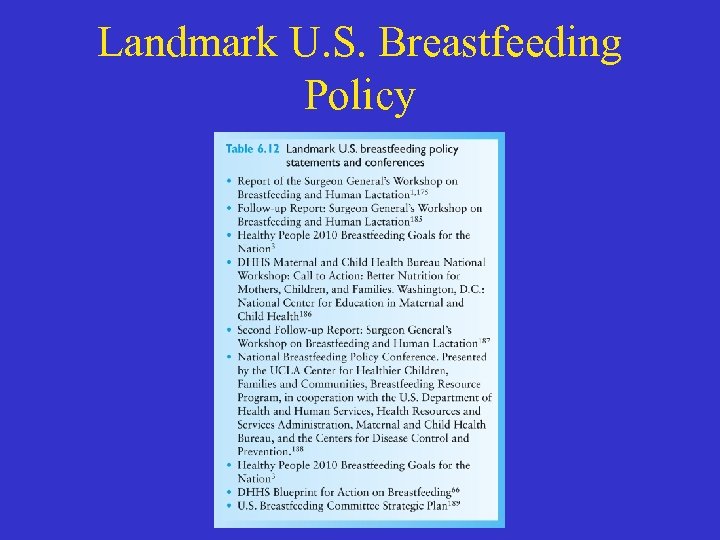 Landmark U. S. Breastfeeding Policy
Landmark U. S. Breastfeeding Policy
 Public Food and Nutrition Programs • USDA WIC Program • Model Breastfeeding Programs – WIC National Breastfeeding Promotion Project— Loving Support Makes Breastfeeding Work – Wellstart International
Public Food and Nutrition Programs • USDA WIC Program • Model Breastfeeding Programs – WIC National Breastfeeding Promotion Project— Loving Support Makes Breastfeeding Work – Wellstart International


