4b2f46b5e9676620b0284dd86cdccaf6.ppt
- Количество слайдов: 79
Chapter 6 Bones and Skeletal Tissues J. F. Thompson, Ph. D. & J. R. Schiller, Ph. D. & G. Pitts, Ph. D.
Functions of Bones • Support – a framework for the body • Protection – bones protect many internal organs – cranial bones surround the brain; vertebrae surround the spinal cord; pelvic girdle surrounds the reproductive organs • Movement - muscles attach to bones • Mineral homeostasis - Ca++, PO-4 storage • Site of blood cell production - hematopoiesis in red bone marrow

Macroscopic Bone Structure • Diaphysis – the shaft of a long bone – contains medullary or marrow cavity • infants have considerable red (hematopoietic) bone marrow • red marrow is gradually replaced by yellow (fatty) bone marrow throughout life • Epiphysis (epiphyses) – ends of a long bone – epiphyseal plate - growth plate made of cartilage – nutrient foramen - site of blood vessel entry into bone – articular cartilage - hyaline cartilage covering epiphysis
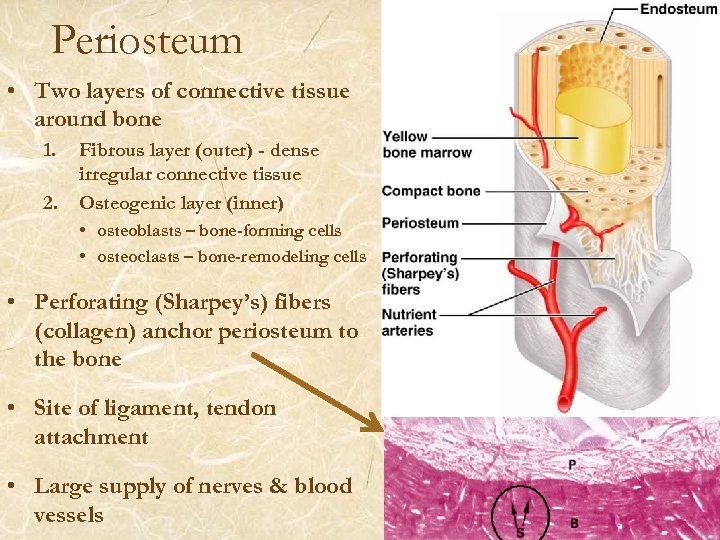
Periosteum • Two layers of connective tissue around bone 1. 2. Fibrous layer (outer) - dense irregular connective tissue Osteogenic layer (inner) • osteoblasts – bone-forming cells • osteoclasts – bone-remodeling cells • Perforating (Sharpey’s) fibers (collagen) anchor periosteum to the bone • Site of ligament, tendon attachment • Large supply of nerves & blood vessels
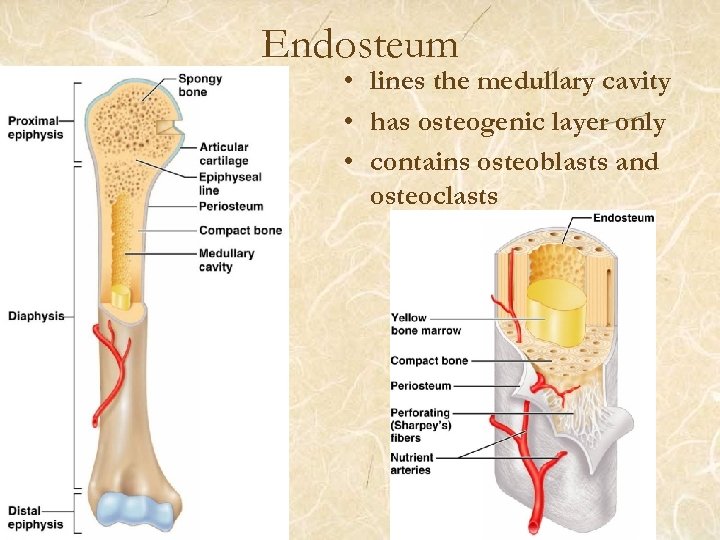
Endosteum • lines the medullary cavity • has osteogenic layer only • contains osteoblasts and osteoclasts
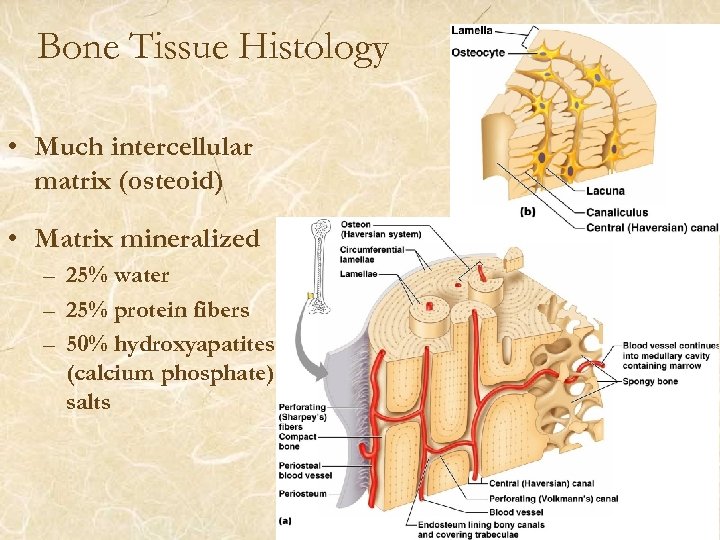
Bone Tissue Histology • Much intercellular matrix (osteoid) • Matrix mineralized – 25% water – 25% protein fibers – 50% hydroxyapatites (calcium phosphate) salts
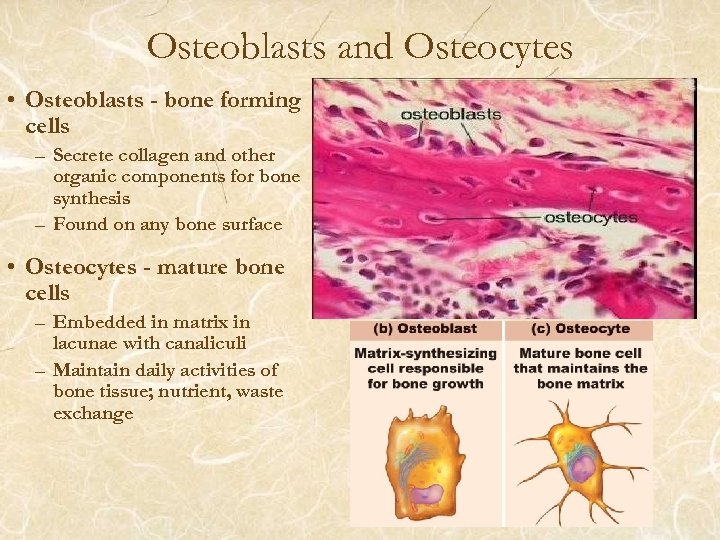
Osteoblasts and Osteocytes • Osteoblasts - bone forming cells – Secrete collagen and other organic components for bone synthesis – Found on any bone surface • Osteocytes - mature bone cells – Embedded in matrix in lacunae with canaliculi – Maintain daily activities of bone tissue; nutrient, waste exchange
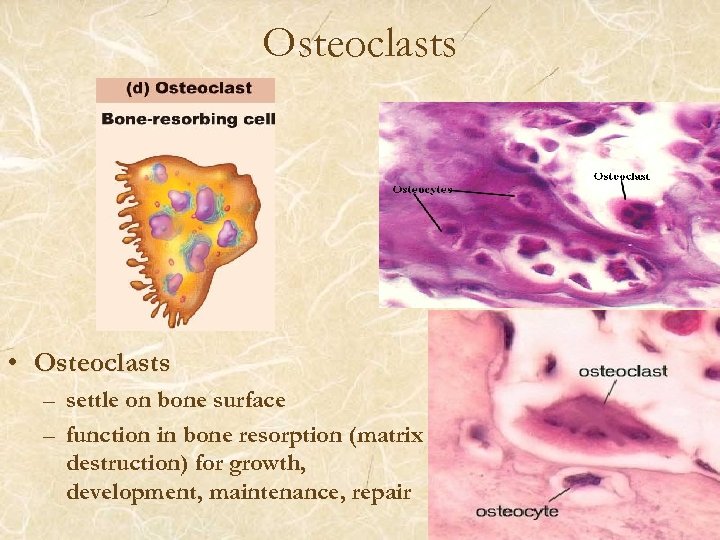
Osteoclasts • Osteoclasts – settle on bone surface – function in bone resorption (matrix destruction) for growth, development, maintenance, repair
Histology of Bone Tissue • Maturation – matrix secretion – ground substance & collagen – crystallization = calcification = mineralization • hydroxyapatite (calcium phosphate salt) • other salts – hardness vs. flexibility • collagen fibers • mineralization – crystallization develops around collagen fibers – stronger than egg shells which have no collagen – matrix is not continuous, because many vascular passageways penetrate the mineralized matrix – size and distribution of these vascular channels determines the type of bone - spongy or compact
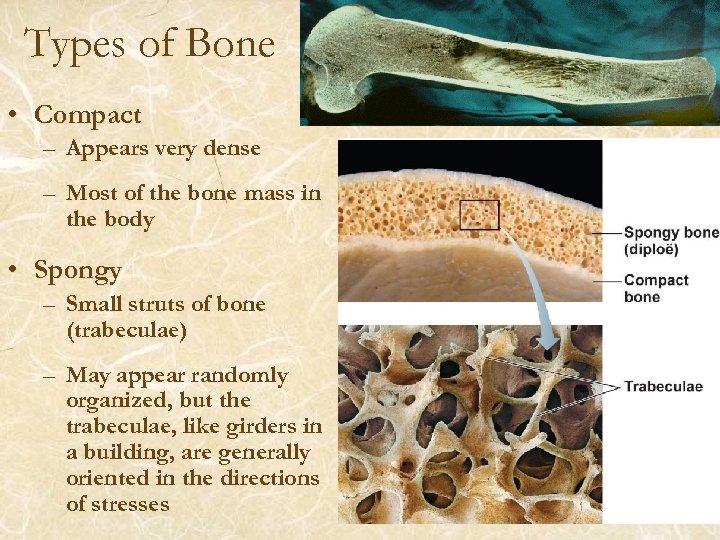
Types of Bone • Compact – Appears very dense – Most of the bone mass in the body • Spongy – Small struts of bone (trabeculae) – May appear randomly organized, but the trabeculae, like girders in a building, are generally oriented in the directions of stresses
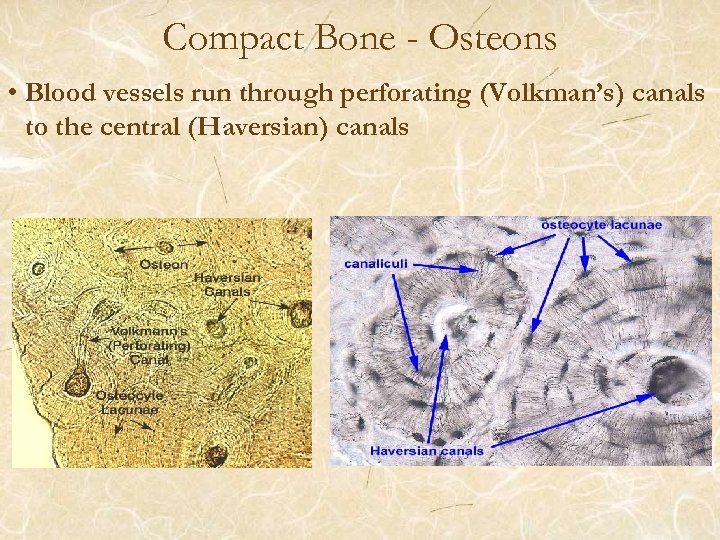
Compact Bone - Osteons • Blood vessels run through perforating (Volkman’s) canals to the central (Haversian) canals
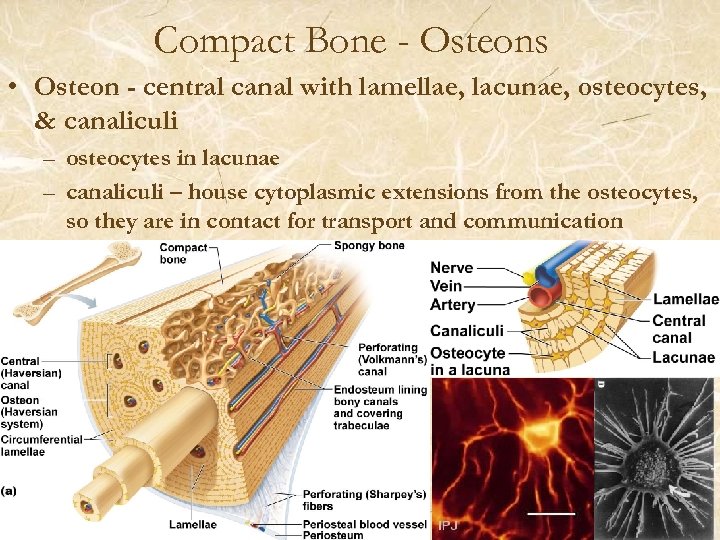
Compact Bone - Osteons • Osteon - central canal with lamellae, lacunae, osteocytes, & canaliculi – osteocytes in lacunae – canaliculi – house cytoplasmic extensions from the osteocytes, so they are in contact for transport and communication
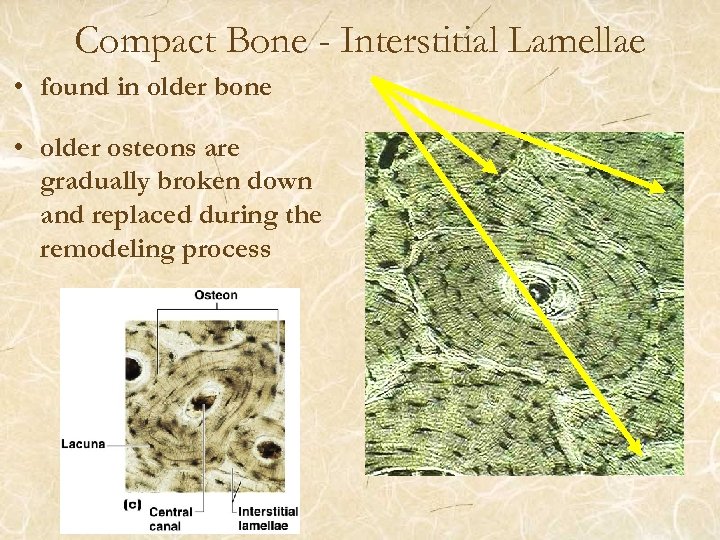
Compact Bone - Interstitial Lamellae • found in older bone • older osteons are gradually broken down and replaced during the remodeling process
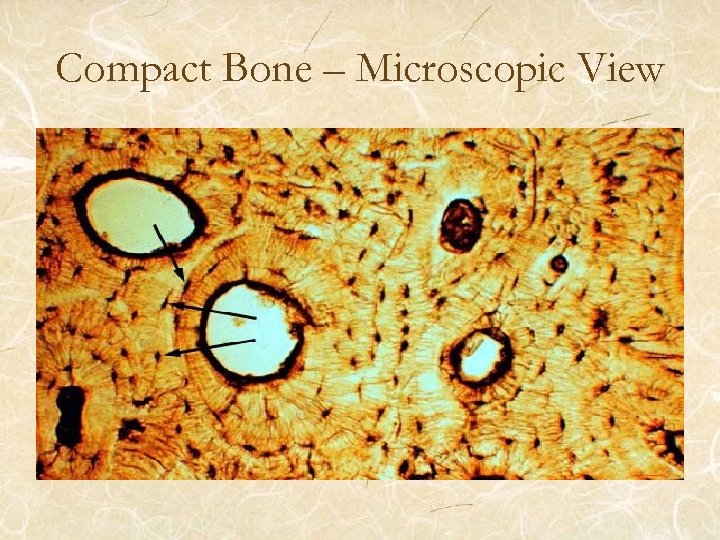
Compact Bone – Microscopic View
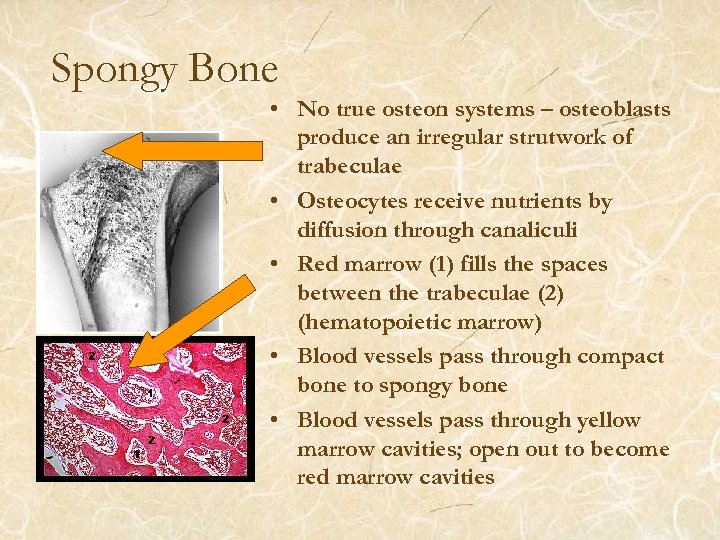
Spongy Bone • No true osteon systems – osteoblasts produce an irregular strutwork of trabeculae • Osteocytes receive nutrients by diffusion through canaliculi • Red marrow (1) fills the spaces between the trabeculae (2) (hematopoietic marrow) • Blood vessels pass through compact bone to spongy bone • Blood vessels pass through yellow marrow cavities; open out to become red marrow cavities
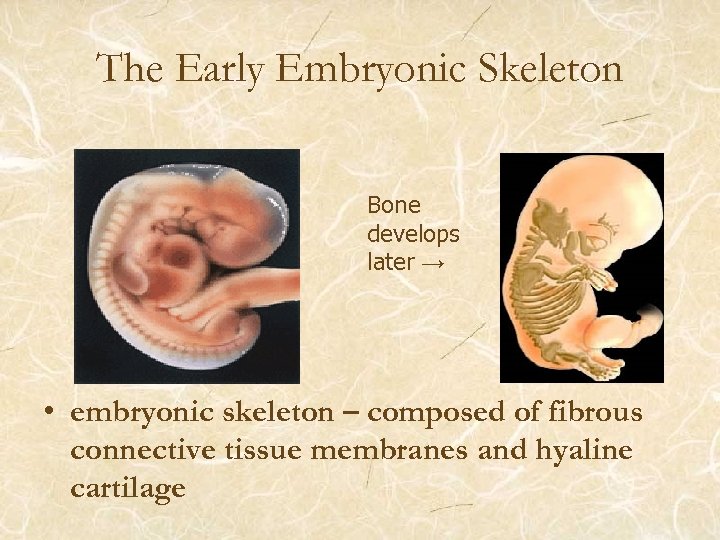
The Early Embryonic Skeleton Bone develops later → • embryonic skeleton – composed of fibrous connective tissue membranes and hyaline cartilage
Bone Formation and Growth • Ossification/osteogenesis • Begins at week 4 of development • There are two different types of bone formation – Each process leads to the formation of mature compact and spongy bones – Fibrous membrane model - intramembranous ossification – “membrane bones” – Hyaline cartilage model - endochondral ossification • the initial cartilage is transformed to become “endochondral bones”
Intramembranous Ossification • Results in the formation of cranial bones and the clavicles. – All are flat bones • At the site of bone development – Ossification begins in fibrous connective tissue membranes formed by mesenchymal cells. – Osteoprogenitor cells (osteoblasts): clusters of embryonic cells • become centers of ossification, secrete matrix until they are surrounded
Intramembranous Ossification • As the matrix forms, trabeculae form, joining together, forming the lattice of spongy bone • Outside vascularized connective tissue develops into the periosteum • Bone collar of compact bone forms, and red marrow appears • Most of this bone will be remodeled into compact bone over time
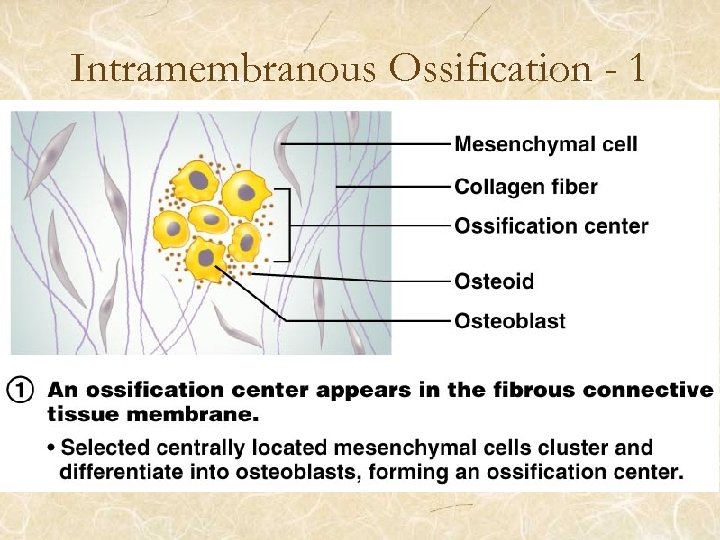
Intramembranous Ossification - 1
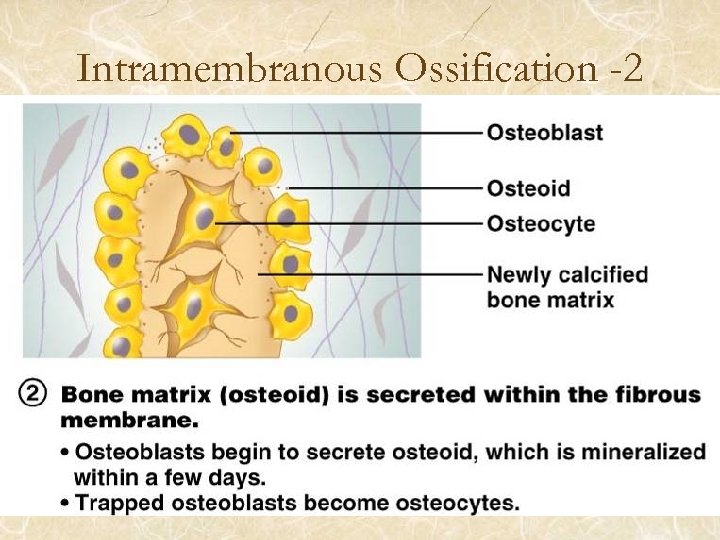
Intramembranous Ossification -2
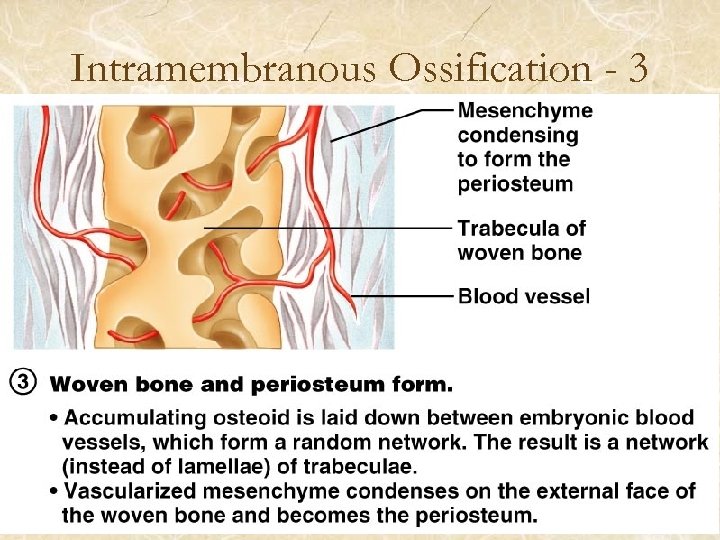
Intramembranous Ossification - 3
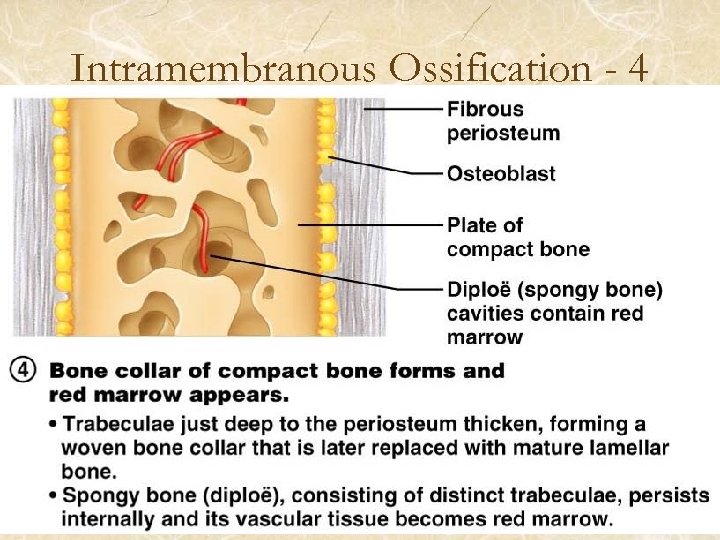
Intramembranous Ossification - 4
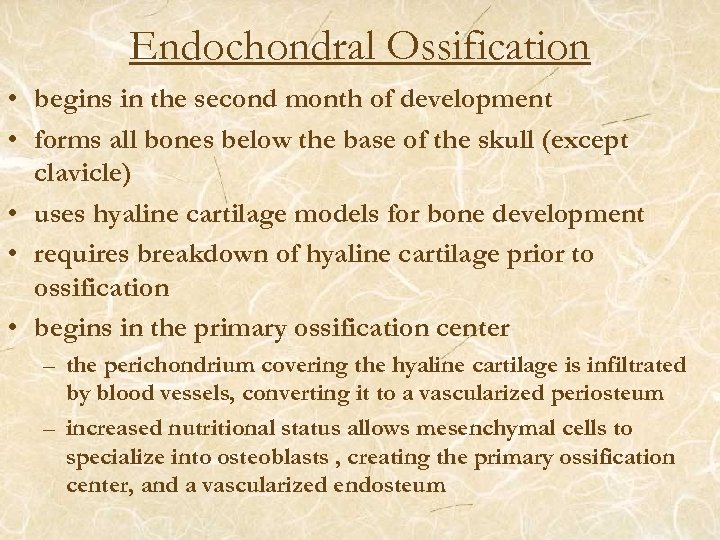
Endochondral Ossification • begins in the second month of development • forms all bones below the base of the skull (except clavicle) • uses hyaline cartilage models for bone development • requires breakdown of hyaline cartilage prior to ossification • begins in the primary ossification center – the perichondrium covering the hyaline cartilage is infiltrated by blood vessels, converting it to a vascularized periosteum – increased nutritional status allows mesenchymal cells to specialize into osteoblasts , creating the primary ossification center, and a vascularized endosteum
Stages of Endochondral Ossification • formation of bone collar • cavitation of the hyaline cartilage • invasion of internal cavities by the periosteal bud, and spongy bone formation • formation of the medullary cavity; appearance of secondary ossification centers in the epiphyses • ossification of the epiphyses, with hyaline cartilage remaining only in the epiphyseal plates
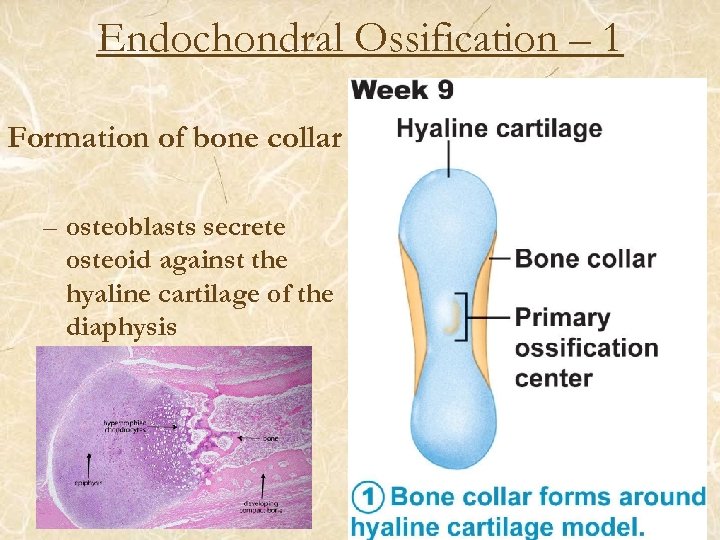
Endochondral Ossification – 1 Formation of bone collar – osteoblasts secrete osteoid against the hyaline cartilage of the diaphysis
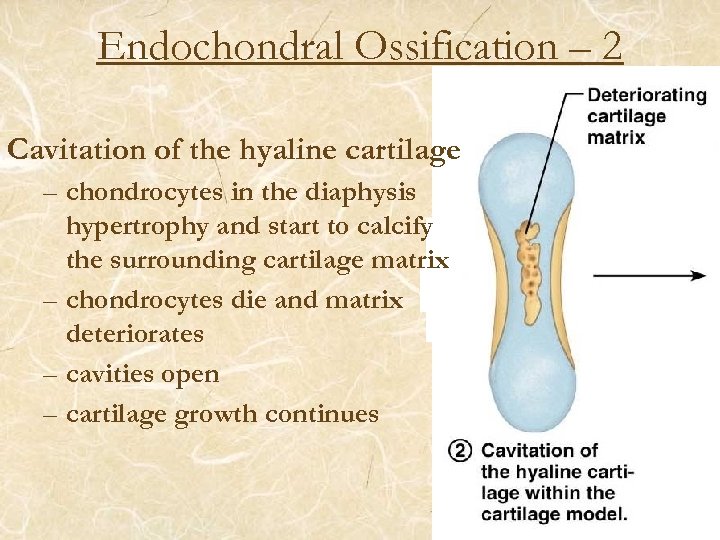
Endochondral Ossification – 2 Cavitation of the hyaline cartilage – chondrocytes in the diaphysis hypertrophy and start to calcify the surrounding cartilage matrix – chondrocytes die and matrix deteriorates – cavities open – cartilage growth continues
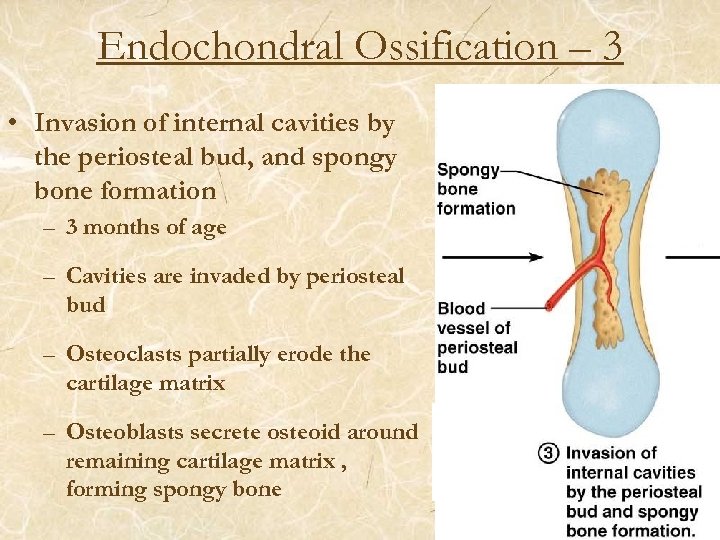
Endochondral Ossification – 3 • Invasion of internal cavities by the periosteal bud, and spongy bone formation – 3 months of age – Cavities are invaded by periosteal bud – Osteoclasts partially erode the cartilage matrix – Osteoblasts secrete osteoid around remaining cartilage matrix , forming spongy bone
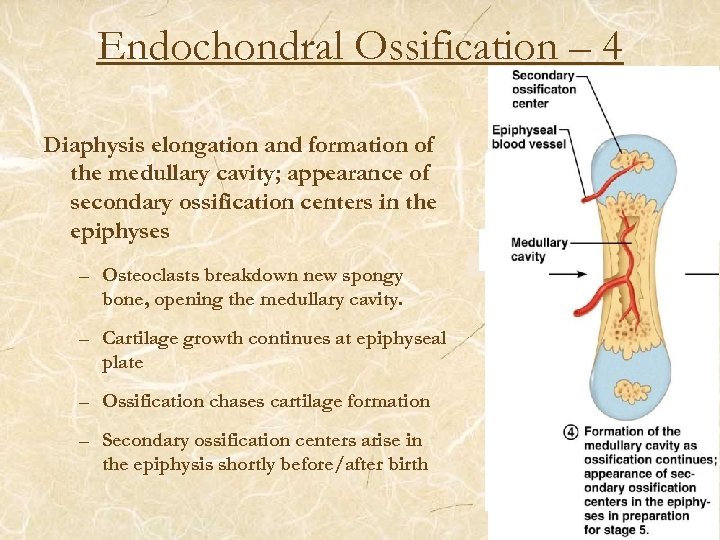
Endochondral Ossification – 4 Diaphysis elongation and formation of the medullary cavity; appearance of secondary ossification centers in the epiphyses – Osteoclasts breakdown new spongy bone, opening the medullary cavity. – Cartilage growth continues at epiphyseal plate – Ossification chases cartilage formation – Secondary ossification centers arise in the epiphysis shortly before/after birth
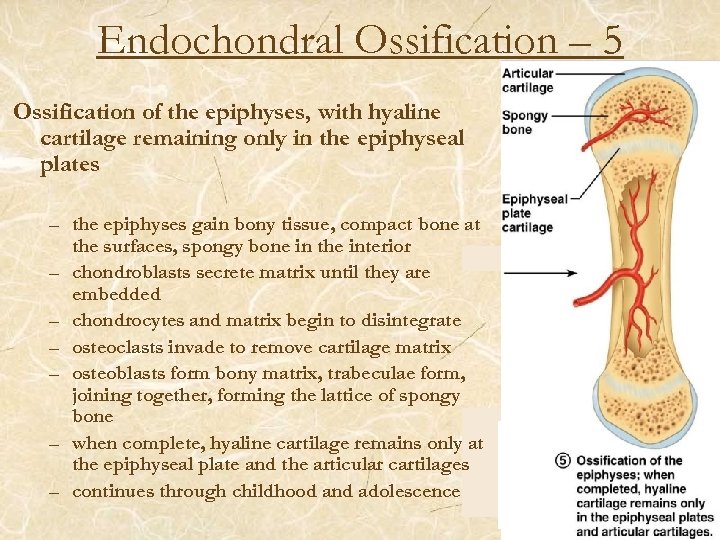
Endochondral Ossification – 5 Ossification of the epiphyses, with hyaline cartilage remaining only in the epiphyseal plates – the epiphyses gain bony tissue, compact bone at the surfaces, spongy bone in the interior – chondroblasts secrete matrix until they are embedded – chondrocytes and matrix begin to disintegrate – osteoclasts invade to remove cartilage matrix – osteoblasts form bony matrix, trabeculae form, joining together, forming the lattice of spongy bone – when complete, hyaline cartilage remains only at the epiphyseal plate and the articular cartilages – continues through childhood and adolescence
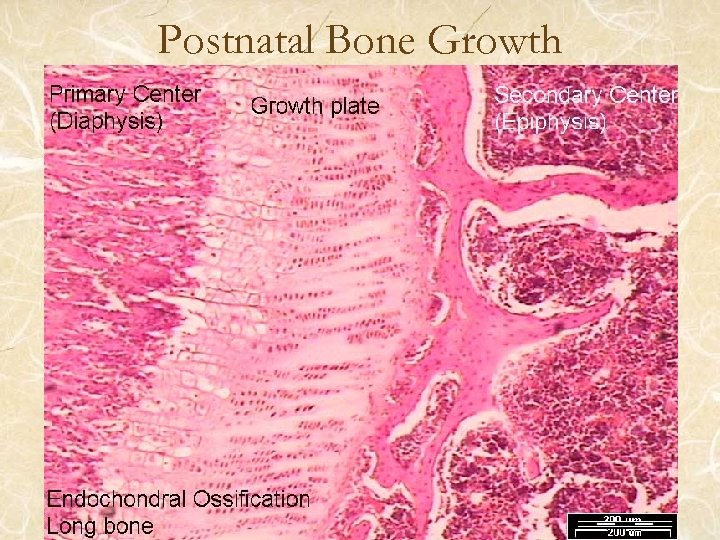
Postnatal Bone Growth
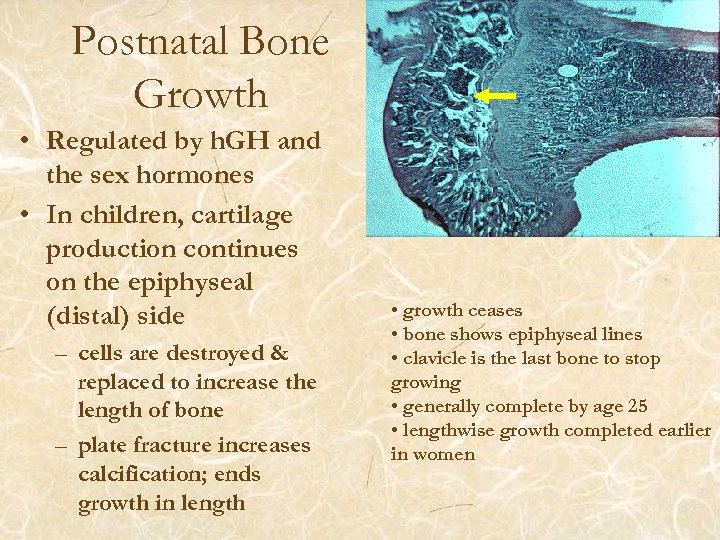
Postnatal Bone Growth • Regulated by h. GH and the sex hormones • In children, cartilage production continues on the epiphyseal (distal) side – cells are destroyed & replaced to increase the length of bone – plate fracture increases calcification; ends growth in length • growth ceases • bone shows epiphyseal lines • clavicle is the last bone to stop growing • generally complete by age 25 • lengthwise growth completed earlier in women
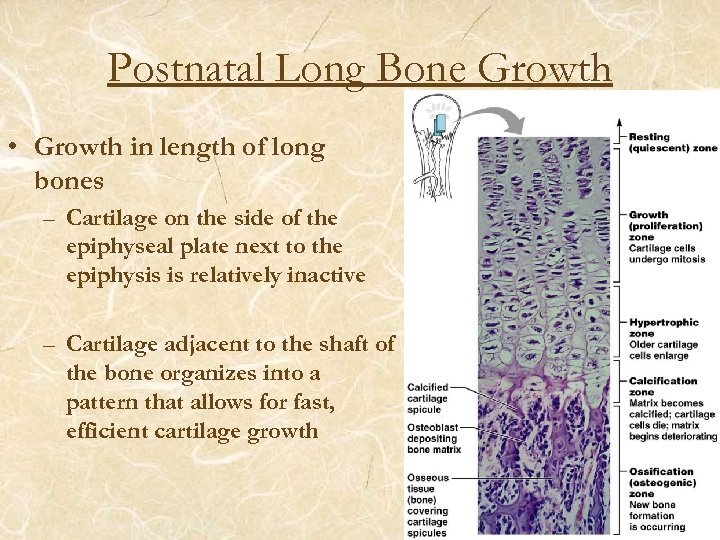
Postnatal Long Bone Growth • Growth in length of long bones – Cartilage on the side of the epiphyseal plate next to the epiphysis is relatively inactive – Cartilage adjacent to the shaft of the bone organizes into a pattern that allows for fast, efficient cartilage growth
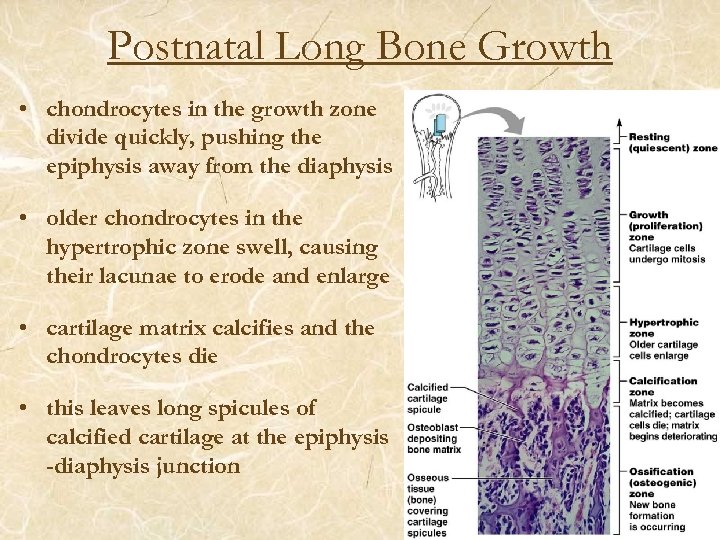
Postnatal Long Bone Growth • chondrocytes in the growth zone divide quickly, pushing the epiphysis away from the diaphysis • older chondrocytes in the hypertrophic zone swell, causing their lacunae to erode and enlarge • cartilage matrix calcifies and the chondrocytes die • this leaves long spicules of calcified cartilage at the epiphysis -diaphysis junction
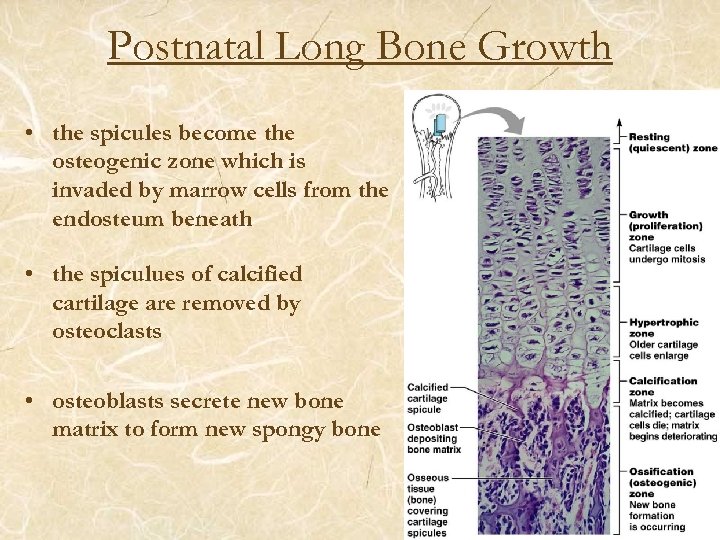
Postnatal Long Bone Growth • the spicules become the osteogenic zone which is invaded by marrow cells from the endosteum beneath • the spiculues of calcified cartilage are removed by osteoclasts • osteoblasts secrete new bone matrix to form new spongy bone
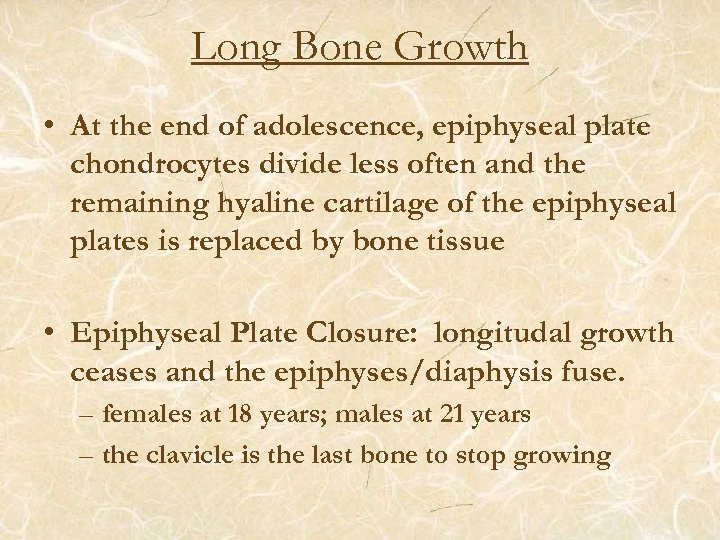
Long Bone Growth • At the end of adolescence, epiphyseal plate chondrocytes divide less often and the remaining hyaline cartilage of the epiphyseal plates is replaced by bone tissue • Epiphyseal Plate Closure: longitudal growth ceases and the epiphyses/diaphysis fuse. – females at 18 years; males at 21 years – the clavicle is the last bone to stop growing
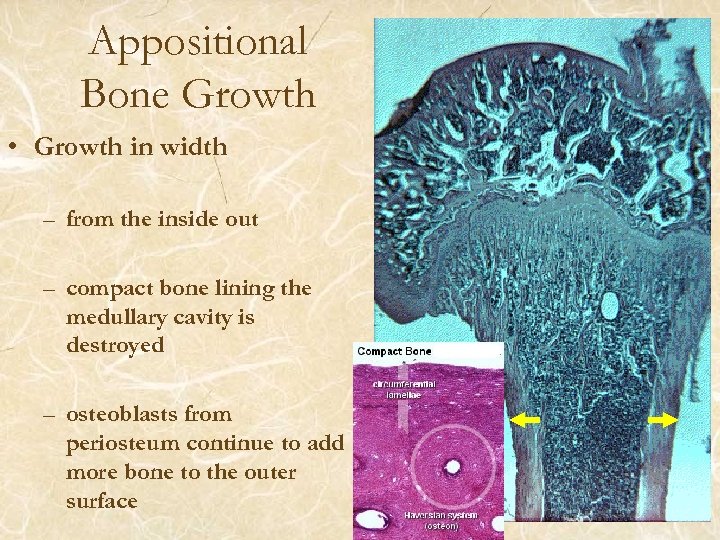
Appositional Bone Growth • Growth in width – from the inside out – compact bone lining the medullary cavity is destroyed – osteoblasts from periosteum continue to add more bone to the outer surface
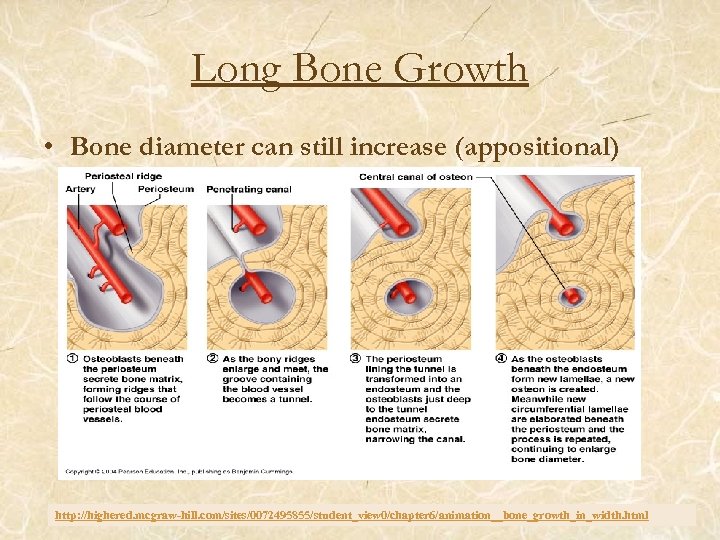
Long Bone Growth • Bone diameter can still increase (appositional) http: //highered. mcgraw-hill. com/sites/0072495855/student_view 0/chapter 6/animation__bone_growth_in_width. html
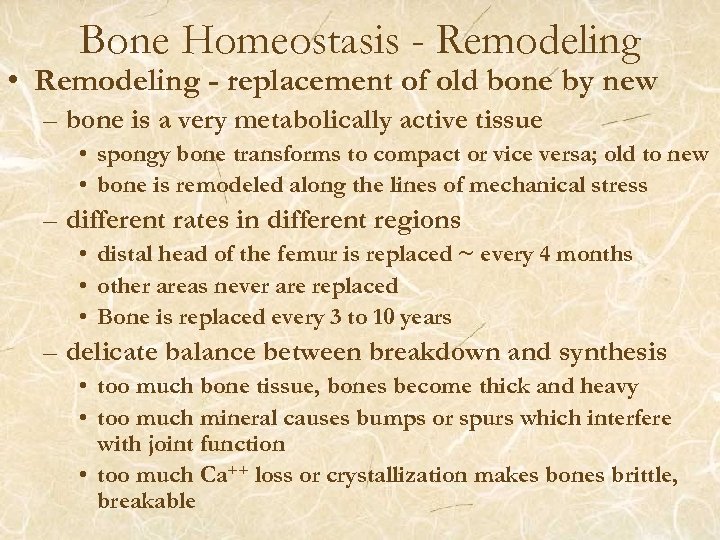
Bone Homeostasis - Remodeling • Remodeling - replacement of old bone by new – bone is a very metabolically active tissue • spongy bone transforms to compact or vice versa; old to new • bone is remodeled along the lines of mechanical stress – different rates in different regions • distal head of the femur is replaced ~ every 4 months • other areas never are replaced • Bone is replaced every 3 to 10 years – delicate balance between breakdown and synthesis • too much bone tissue, bones become thick and heavy • too much mineral causes bumps or spurs which interfere with joint function • too much Ca++ loss or crystallization makes bones brittle, breakable
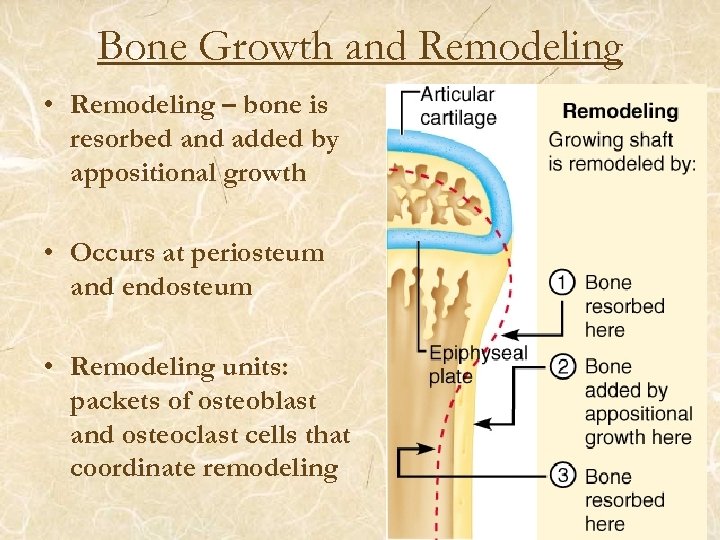
Bone Growth and Remodeling • Remodeling – bone is resorbed and added by appositional growth • Occurs at periosteum and endosteum • Remodeling units: packets of osteoblast and osteoclast cells that coordinate remodeling
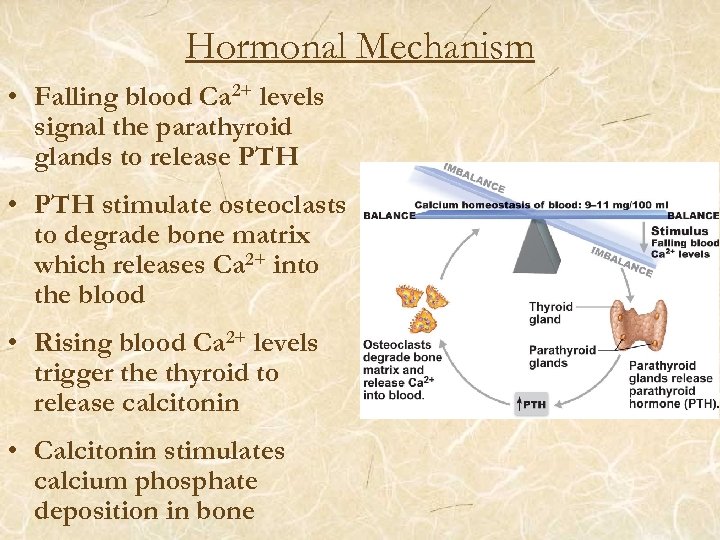
Hormonal Mechanism • Falling blood Ca 2+ levels signal the parathyroid glands to release PTH • PTH stimulate osteoclasts to degrade bone matrix which releases Ca 2+ into the blood • Rising blood Ca 2+ levels trigger the thyroid to release calcitonin • Calcitonin stimulates calcium phosphate deposition in bone
Response to Mechanical Stress • Wolff’s law – a bone grows or remodels in response to the forces or demands placed upon it • Observations supporting Wolff’s law include – Long bones are thickest midway along the shaft (where bending stress is greatest) – Curved bones are thickest where they are most likely to buckle
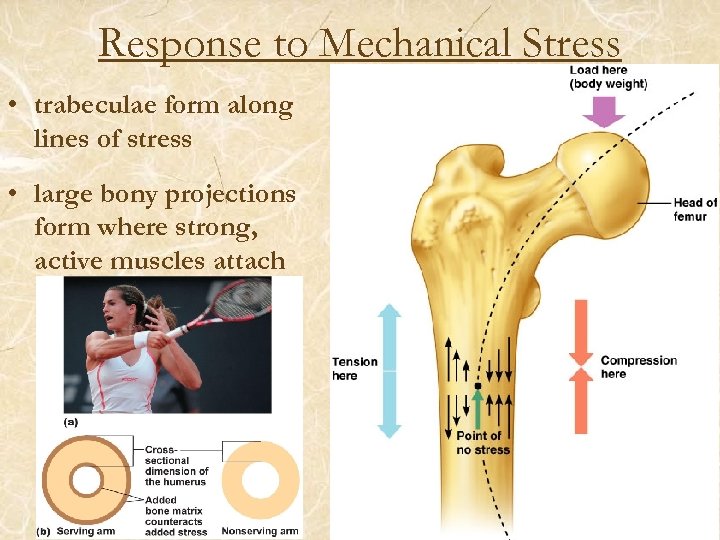
Response to Mechanical Stress • trabeculae form along lines of stress • large bony projections form where strong, active muscles attach
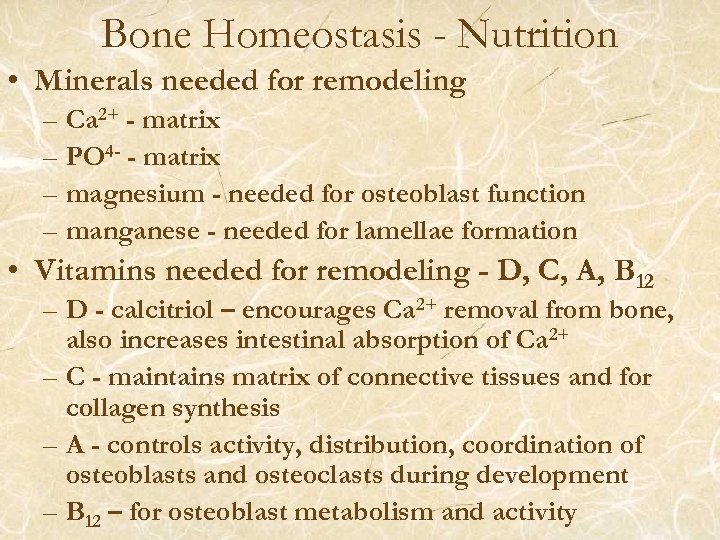
Bone Homeostasis - Nutrition • Minerals needed for remodeling – Ca 2+ - matrix – PO 4 - - matrix – magnesium - needed for osteoblast function – manganese - needed for lamellae formation • Vitamins needed for remodeling - D, C, A, B 12 – D - calcitriol – encourages Ca 2+ removal from bone, also increases intestinal absorption of Ca 2+ – C - maintains matrix of connective tissues and for collagen synthesis – A - controls activity, distribution, coordination of osteoblasts and osteoclasts during development – B 12 – for osteoblast metabolism and activity
Bone Homeostasis - Regulation • Hormonal regulation of bone growth and remodeling – h. GH = human growth hormone • • • responsible for general growth of all body tissues becoming tall or short depends on h. GH levels works with the sex hormones aids in the growth of new bone causes degeneration of cartilage cells in epiphyseal plates – sex hormones – androgens and estrogens - important for normal bone growth & development – insulin and thyroid hormones - important for bone and connective tissue growth & metabolism
Calcium Homeostasis • Bones are important for Ca 2+ homeostasis – bone tissue is the main reservoir for Ca 2+ ions in the body (500 -1000 times more calcium is in bone than in the rest of the tissues) – blood levels are regulated very tightly by the endocrine system – bone serves as a “buffer” to prevent sudden changes in blood Ca 2+ levels • too much blood Ca 2+ (hypercalcemia) - heart stops • too little blood Ca 2+ (hypocalcemia) - breathing stops
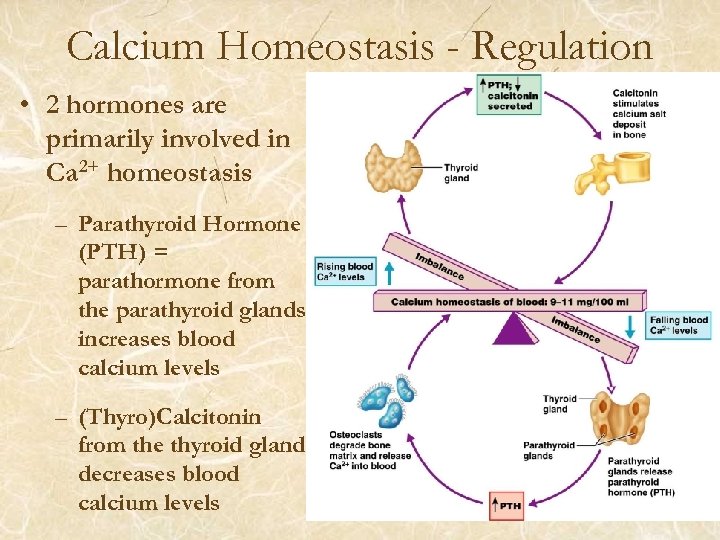
Calcium Homeostasis - Regulation • 2 hormones are primarily involved in Ca 2+ homeostasis – Parathyroid Hormone (PTH) = parathormone from the parathyroid glands increases blood calcium levels – (Thyro)Calcitonin from the thyroid gland decreases blood calcium levels
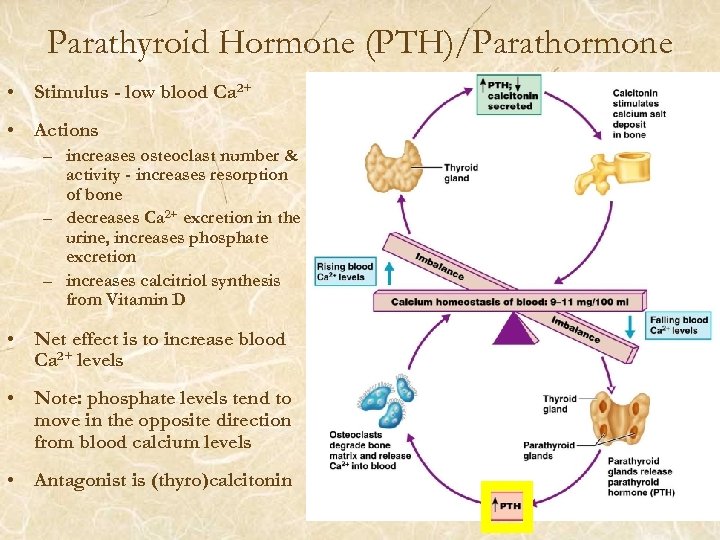
Parathyroid Hormone (PTH)/Parathormone • Stimulus - low blood Ca 2+ • Actions – increases osteoclast number & activity - increases resorption of bone – decreases Ca 2+ excretion in the urine, increases phosphate excretion – increases calcitriol synthesis from Vitamin D • Net effect is to increase blood Ca 2+ levels • Note: phosphate levels tend to move in the opposite direction from blood calcium levels • Antagonist is (thyro)calcitonin
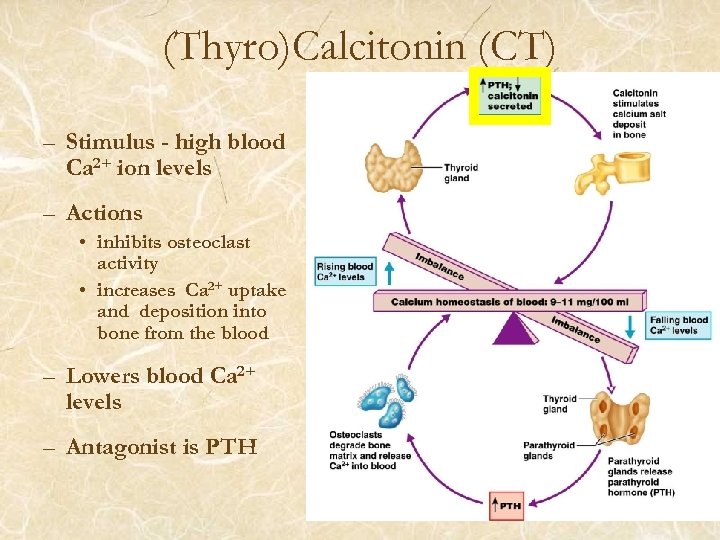
(Thyro)Calcitonin (CT) – Stimulus - high blood Ca 2+ ion levels – Actions • inhibits osteoclast activity • increases Ca 2+ uptake and deposition into bone from the blood – Lowers blood Ca 2+ levels – Antagonist is PTH
Bone Fractures (Breaks) • Bone fractures are classified by: – The position of the bone ends after fracture – The completeness of the break – The orientation of the bone to the long axis – Whether or not the bones ends penetrate the skin
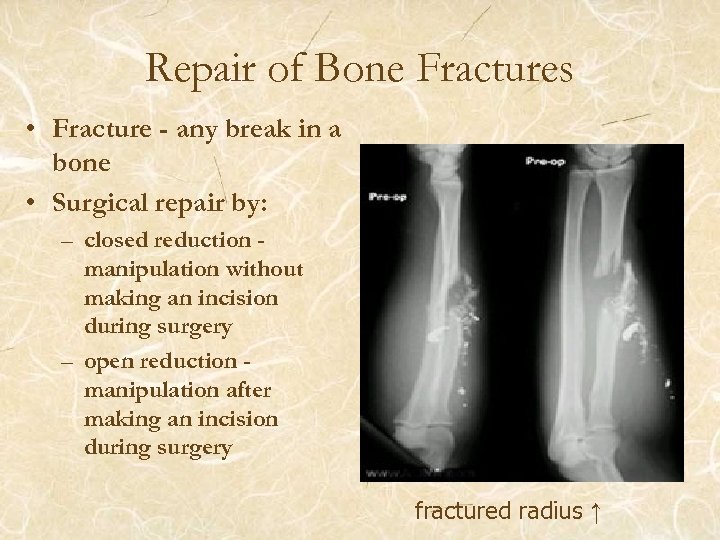
Repair of Bone Fractures • Fracture - any break in a bone • Surgical repair by: – closed reduction manipulation without making an incision during surgery – open reduction manipulation after making an incision during surgery fractured radius ↑
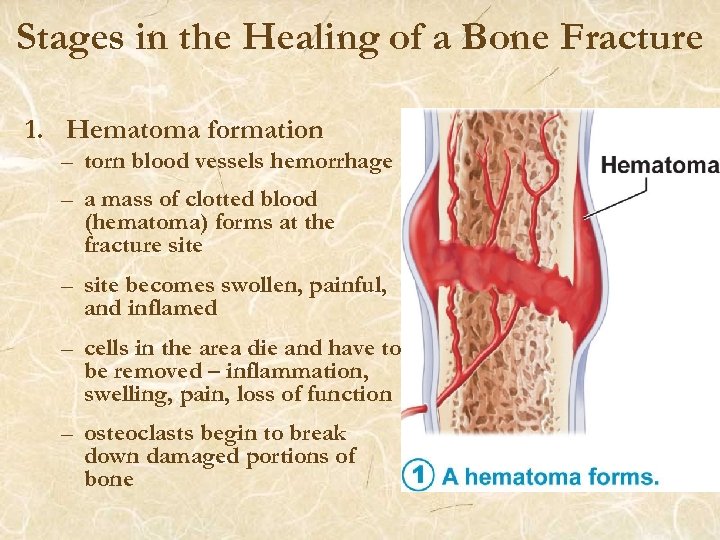
Stages in the Healing of a Bone Fracture 1. Hematoma formation – torn blood vessels hemorrhage – a mass of clotted blood (hematoma) forms at the fracture site – site becomes swollen, painful, and inflamed – cells in the area die and have to be removed – inflammation, swelling, pain, loss of function – osteoclasts begin to break down damaged portions of bone
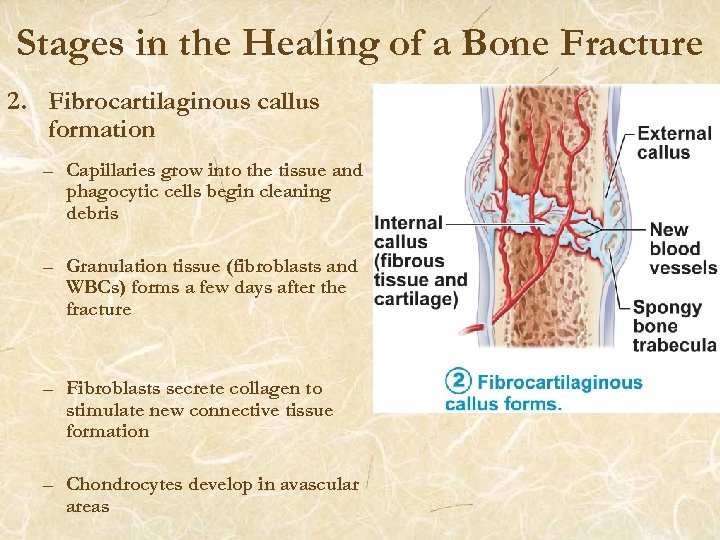
Stages in the Healing of a Bone Fracture 2. Fibrocartilaginous callus formation – Capillaries grow into the tissue and phagocytic cells begin cleaning debris – Granulation tissue (fibroblasts and WBCs) forms a few days after the fracture – Fibroblasts secrete collagen to stimulate new connective tissue formation – Chondrocytes develop in avascular areas
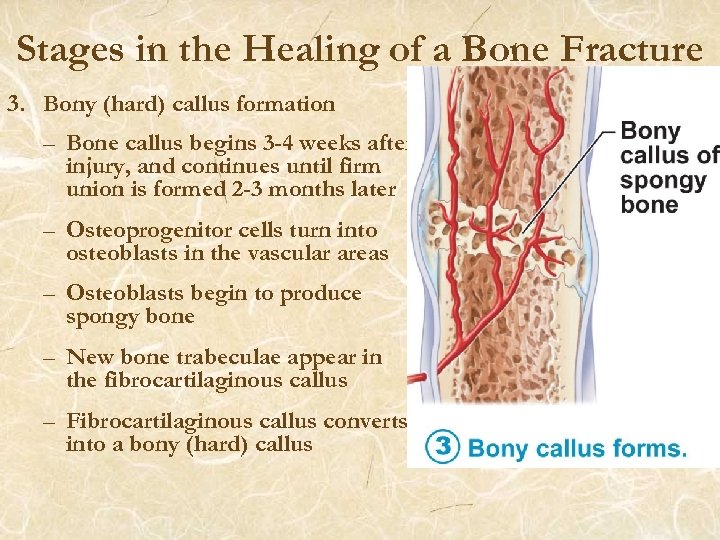
Stages in the Healing of a Bone Fracture 3. Bony (hard) callus formation – Bone callus begins 3 -4 weeks after injury, and continues until firm union is formed 2 -3 months later – Osteoprogenitor cells turn into osteoblasts in the vascular areas – Osteoblasts begin to produce spongy bone – New bone trabeculae appear in the fibrocartilaginous callus – Fibrocartilaginous callus converts into a bony (hard) callus
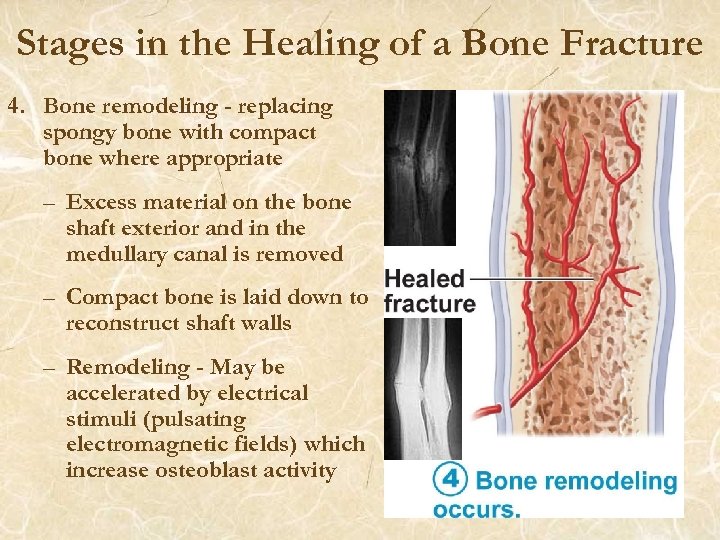
Stages in the Healing of a Bone Fracture 4. Bone remodeling - replacing spongy bone with compact bone where appropriate – Excess material on the bone shaft exterior and in the medullary canal is removed – Compact bone is laid down to reconstruct shaft walls – Remodeling - May be accelerated by electrical stimuli (pulsating electromagnetic fields) which increase osteoblast activity
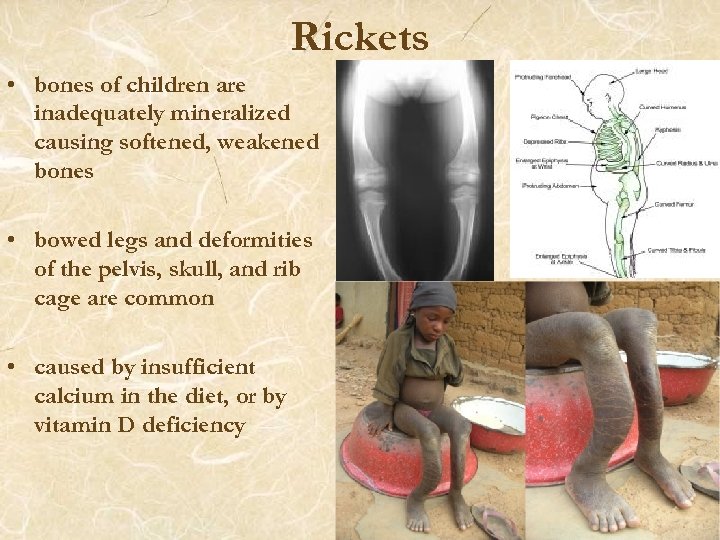
Rickets • bones of children are inadequately mineralized causing softened, weakened bones • bowed legs and deformities of the pelvis, skull, and rib cage are common • caused by insufficient calcium in the diet, or by vitamin D deficiency
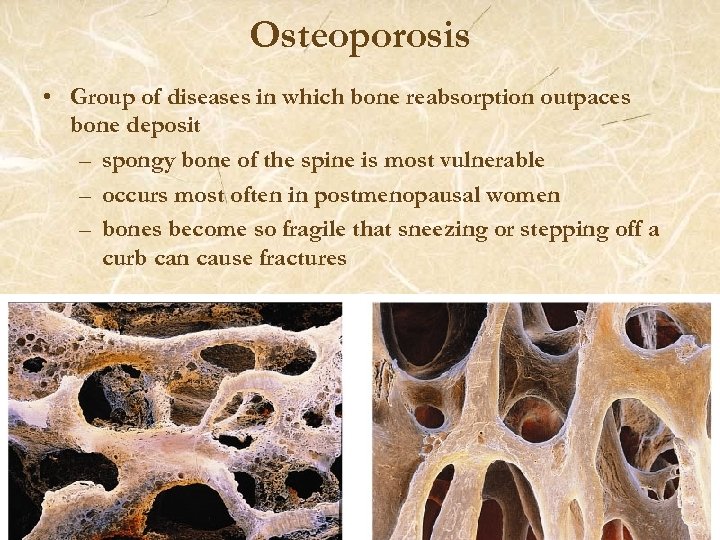
Osteoporosis • Group of diseases in which bone reabsorption outpaces bone deposit – spongy bone of the spine is most vulnerable – occurs most often in postmenopausal women – bones become so fragile that sneezing or stepping off a curb can cause fractures
Osteoporosis: Treatment • Calcium and vitamin D supplements • Increased weight-bearing exercise • Hormone (estrogen) replacement therapy (HRT) slows bone loss • Natural progesterone cream prompts new bone growth • Statins increase bone mineral density
End Chapter 6. There are some additional review slides for you after this slide.
Postnatal Bone Growth • Growth in length of long bones – cells of the epiphyseal plate proximal to the resting cartilage form three functionally different zones: growth, transformation, and osteogenic – most bone growth stops during adolescence – continued growth of nose and lower jaw – accompanied by significant remodeling in order to maintain the proper shape of the epiphysis and diaphysis
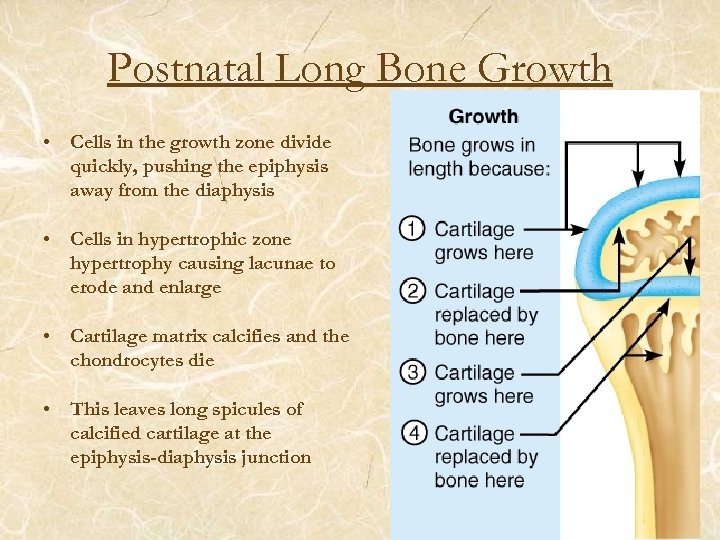
Postnatal Long Bone Growth • Cells in the growth zone divide quickly, pushing the epiphysis away from the diaphysis • Cells in hypertrophic zone hypertrophy causing lacunae to erode and enlarge • Cartilage matrix calcifies and the chondrocytes die • This leaves long spicules of calcified cartilage at the epiphysis-diaphysis junction
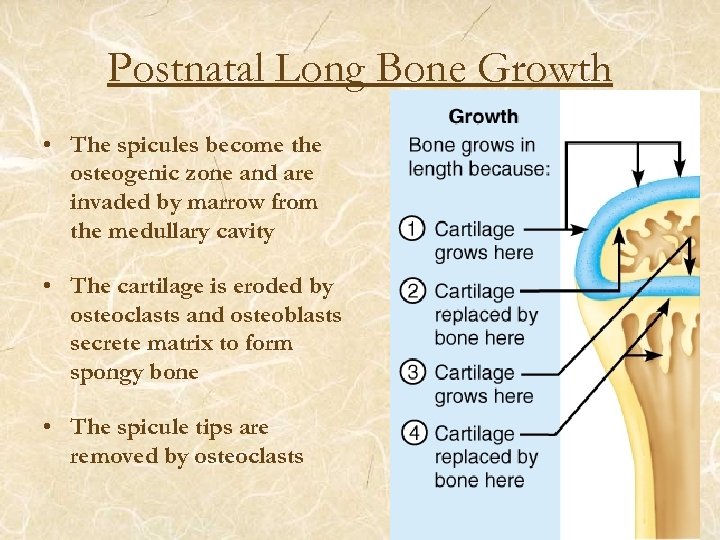
Postnatal Long Bone Growth • The spicules become the osteogenic zone and are invaded by marrow from the medullary cavity • The cartilage is eroded by osteoclasts and osteoblasts secrete matrix to form spongy bone • The spicule tips are removed by osteoclasts
Bone Resorption • Accomplished by osteoclasts • Resorption bays – grooves formed by osteoclasts as they break down bone matrix • Resorption involves osteoclast secretion of: – Lysosomal enzymes that digest organic matrix – Acids that convert calcium salts into soluble forms • Dissolved matrix is transcytosed across the osteoclast’s cell where it is secreted into the interstitial fluid and then into the blood • Two control mechanisms
Hormonal Regulation of Bone Growth During Youth • During infancy and childhood, epiphyseal plate activity is stimulated by growth hormone • During puberty, testosterone and estrogens: – Initially promote adolescent growth spurts – Cause masculinization and feminization of specific parts of the skeleton – Later induce epiphyseal plate closure, ending longitudinal bone growth
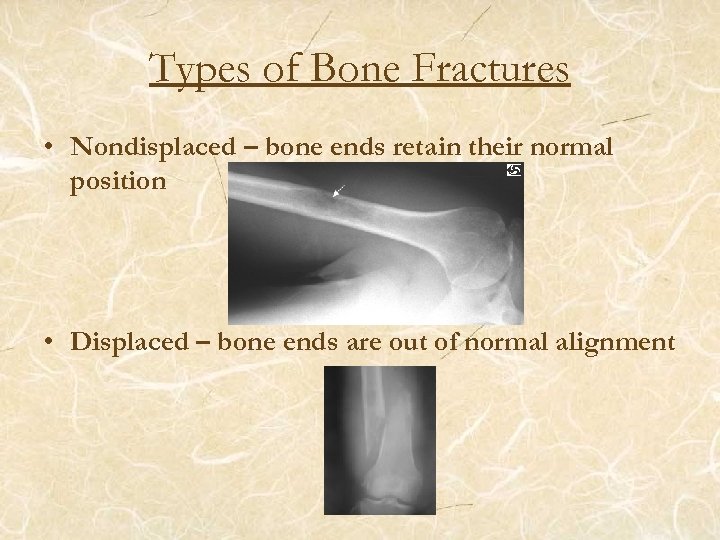
Types of Bone Fractures • Nondisplaced – bone ends retain their normal position • Displaced – bone ends are out of normal alignment
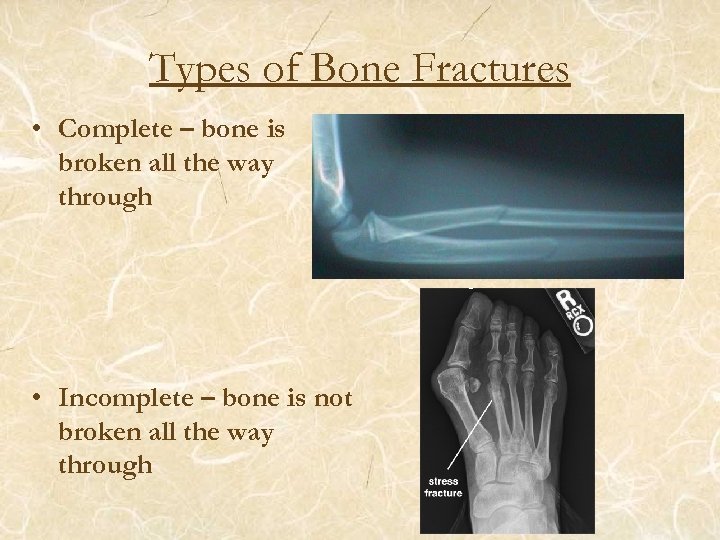
Types of Bone Fractures • Complete – bone is broken all the way through • Incomplete – bone is not broken all the way through
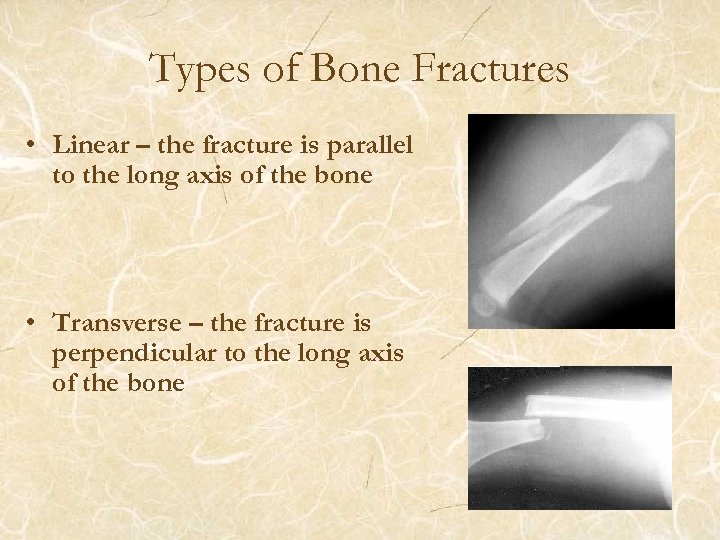
Types of Bone Fractures • Linear – the fracture is parallel to the long axis of the bone • Transverse – the fracture is perpendicular to the long axis of the bone
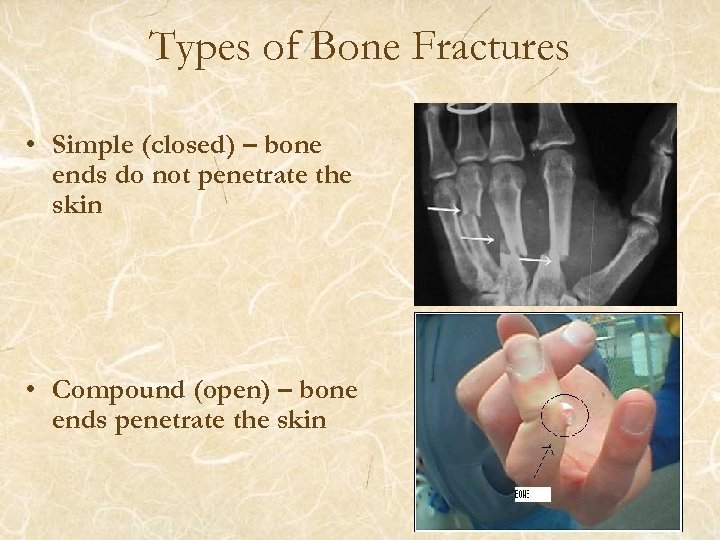
Types of Bone Fractures • Simple (closed) – bone ends do not penetrate the skin • Compound (open) – bone ends penetrate the skin
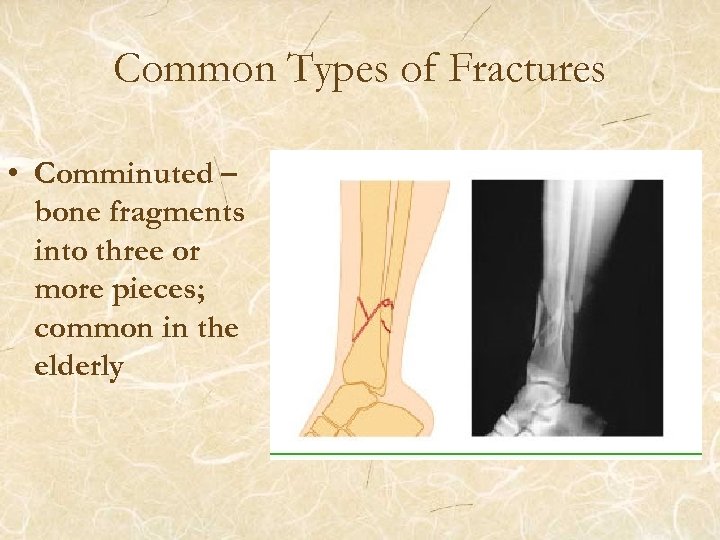
Common Types of Fractures • Comminuted – bone fragments into three or more pieces; common in the elderly
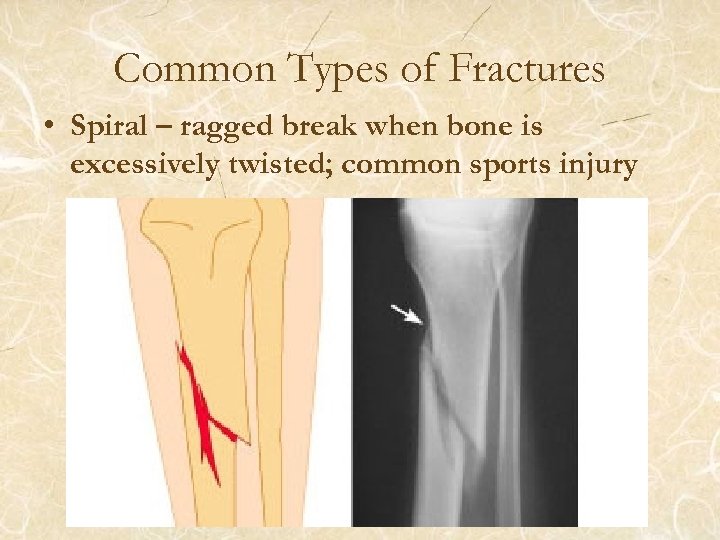
Common Types of Fractures • Spiral – ragged break when bone is excessively twisted; common sports injury
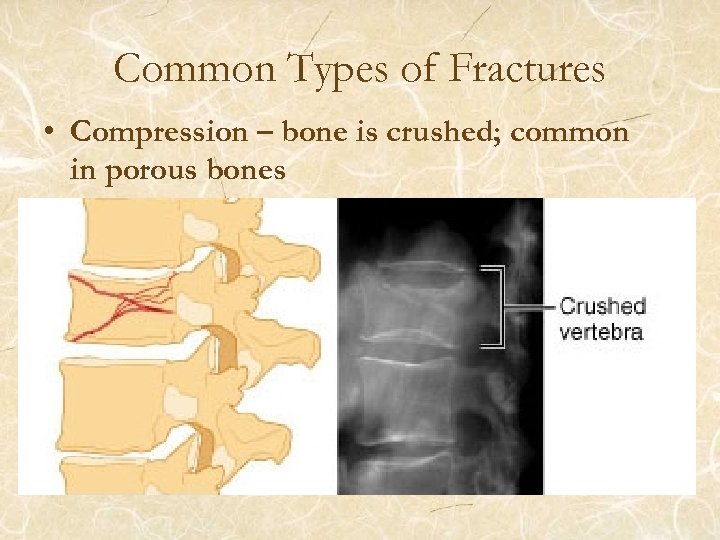
Common Types of Fractures • Compression – bone is crushed; common in porous bones
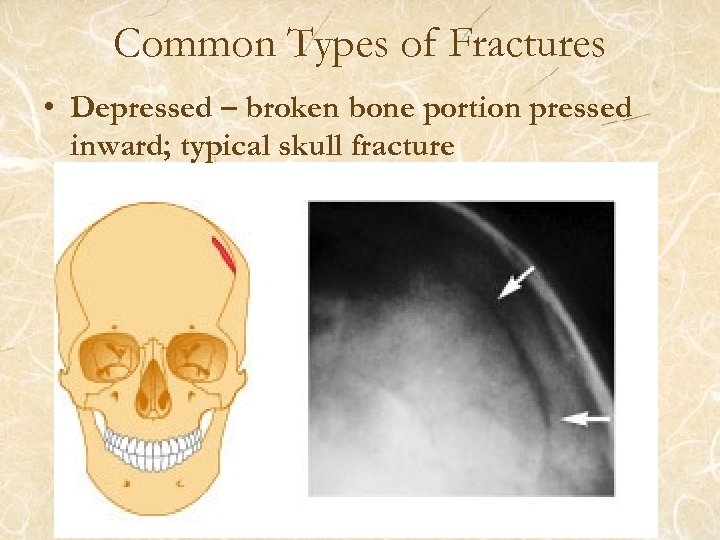
Common Types of Fractures • Depressed – broken bone portion pressed inward; typical skull fracture
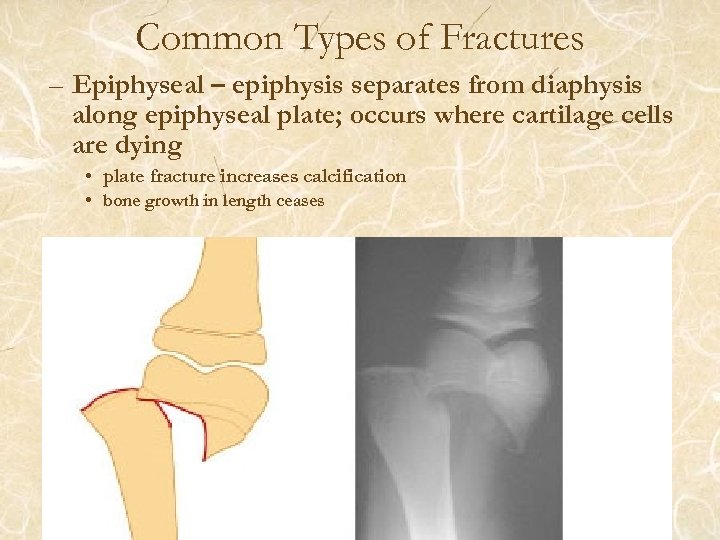
Common Types of Fractures – Epiphyseal – epiphysis separates from diaphysis along epiphyseal plate; occurs where cartilage cells are dying • plate fracture increases calcification • bone growth in length ceases
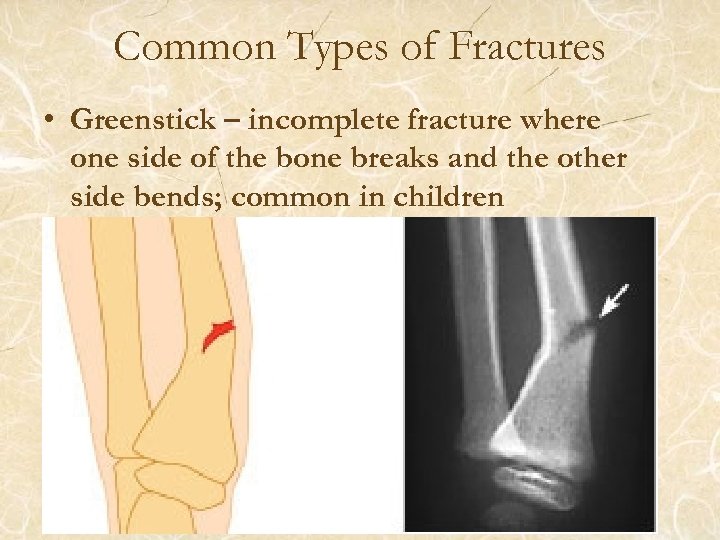
Common Types of Fractures • Greenstick – incomplete fracture where one side of the bone breaks and the other side bends; common in children
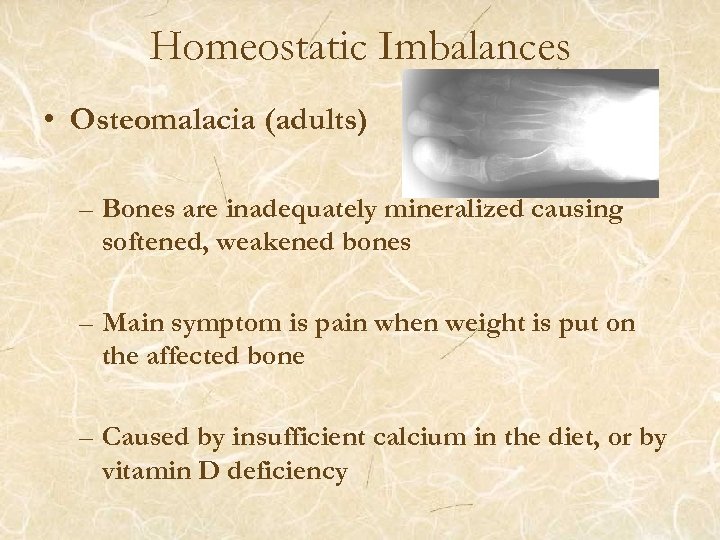
Homeostatic Imbalances • Osteomalacia (adults) – Bones are inadequately mineralized causing softened, weakened bones – Main symptom is pain when weight is put on the affected bone – Caused by insufficient calcium in the diet, or by vitamin D deficiency
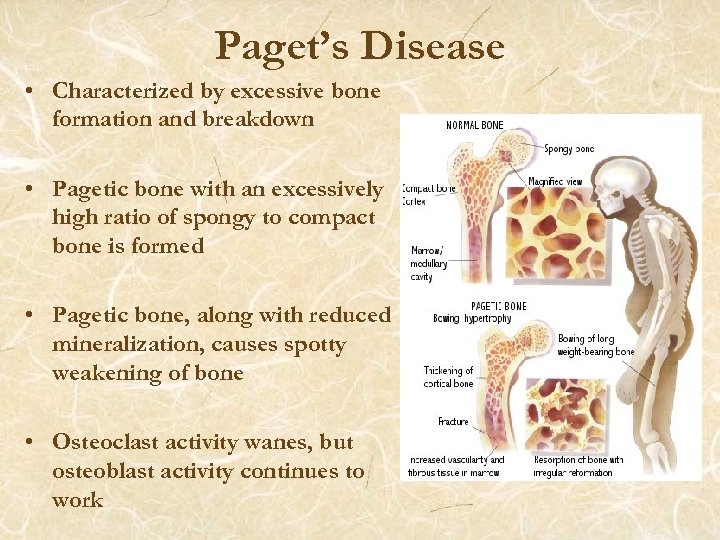
Paget’s Disease • Characterized by excessive bone formation and breakdown • Pagetic bone with an excessively high ratio of spongy to compact bone is formed • Pagetic bone, along with reduced mineralization, causes spotty weakening of bone • Osteoclast activity wanes, but osteoblast activity continues to work
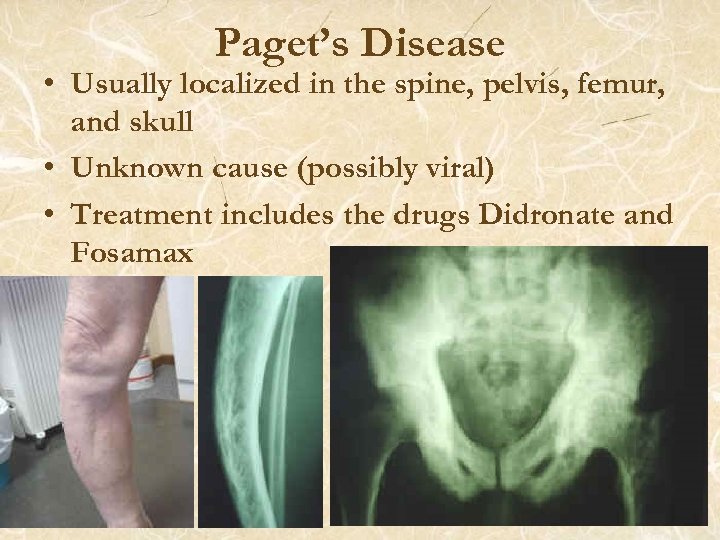
Paget’s Disease • Usually localized in the spine, pelvis, femur, and skull • Unknown cause (possibly viral) • Treatment includes the drugs Didronate and Fosamax
End Chapter 6. End of the additional review slides.
4b2f46b5e9676620b0284dd86cdccaf6.ppt