b09ee343247d81baf8d0949d62992f14.ppt
- Количество слайдов: 24
 Chapter 38 End-of-Life Carolyne Richardson-Phillips, MS, RN PNU 145 Pages 841 -853
Chapter 38 End-of-Life Carolyne Richardson-Phillips, MS, RN PNU 145 Pages 841 -853
 Learning Outcomes By the end of this session, the PN student will be able to: 1. Define terminal illness 2. List the five stages of dying and give an example of each 3. Describe two methods by which nurses can promote acceptance of death in dying clients 4. Discuss & contrast the available settings that a dying client may choose for care 5. Discuss the philosophy of hospice care 6. Discuss the client’s basic physical needs that are common in terminal care 7. Name at least five signs of multiple organ failure 8. Explain the process of discussing organ donation & why it is important as soon as possible after a client’s death 9. Describe the process of confirming death 10. Discuss what is performed with postmortem care 11. Discuss the components of grieving and describe a sign that may indicate a person is resolving his/her grief 12. Discuss general gerontologic considerations with death and dying 13. Discuss different religious cultural aspects in death & dying of a client 14. Develop a nursing care plan using NANDA approved nursing diagnosis, expected outcomes, interventions & methods of outcome evaluation for a client diagnosed with hopelessness
Learning Outcomes By the end of this session, the PN student will be able to: 1. Define terminal illness 2. List the five stages of dying and give an example of each 3. Describe two methods by which nurses can promote acceptance of death in dying clients 4. Discuss & contrast the available settings that a dying client may choose for care 5. Discuss the philosophy of hospice care 6. Discuss the client’s basic physical needs that are common in terminal care 7. Name at least five signs of multiple organ failure 8. Explain the process of discussing organ donation & why it is important as soon as possible after a client’s death 9. Describe the process of confirming death 10. Discuss what is performed with postmortem care 11. Discuss the components of grieving and describe a sign that may indicate a person is resolving his/her grief 12. Discuss general gerontologic considerations with death and dying 13. Discuss different religious cultural aspects in death & dying of a client 14. Develop a nursing care plan using NANDA approved nursing diagnosis, expected outcomes, interventions & methods of outcome evaluation for a client diagnosed with hopelessness
 Terminal Illness • Condition from which recovery is beyond reasonable expectation • Dr. Elisabeth Kubler-Ross-authority on dying • Stages of Death & Dying: • Denial: psychological defense mechanism; person refuses to believe certain information • Anger: emotional response to feeling victimized-person displaces anger onto someone else or with complaints • Bargaining: psychological mechanism for delaying the inevitable - a process of negotiation, usually with God or some higher power • Depression: (sad mood) indicates the realization that death will come • Acceptance: attitude of complacency
Terminal Illness • Condition from which recovery is beyond reasonable expectation • Dr. Elisabeth Kubler-Ross-authority on dying • Stages of Death & Dying: • Denial: psychological defense mechanism; person refuses to believe certain information • Anger: emotional response to feeling victimized-person displaces anger onto someone else or with complaints • Bargaining: psychological mechanism for delaying the inevitable - a process of negotiation, usually with God or some higher power • Depression: (sad mood) indicates the realization that death will come • Acceptance: attitude of complacency
 Death & Dying (cont’d) • • Not an easy task-Facing death with a client, child, and family Time where patience is stretched, rules fall apart It is tiring, discouraging, sad Requires a profound look at acceptance for the nurse caring for someone who is dying • Self-exploration of one’s self: most important preparation for dealing with the dying • Defense Mechanism Used: Coping
Death & Dying (cont’d) • • Not an easy task-Facing death with a client, child, and family Time where patience is stretched, rules fall apart It is tiring, discouraging, sad Requires a profound look at acceptance for the nurse caring for someone who is dying • Self-exploration of one’s self: most important preparation for dealing with the dying • Defense Mechanism Used: Coping
 Promoting Acceptance • Emotional care: • Helping to choose how & where to receive terminal care • Comfort in preparing an advance directive • Educate about available settings • Dying Person’s Bill of Rights: nurse cares for dying clients with respect, no matter what their emotional, physical or cognitive state; Box 38 -1, pg. 844 • Nurses • Help clients pass thru each stage • Provide Emotional support • Supporting choices with terminal care • Facilitate directives to maintain the client’s personal dignity and focus of control • Listen to feelings & allow client to verbally work through emotions • Become nonjudgmental sounding board • Acknowledge client as unique & worthwhile
Promoting Acceptance • Emotional care: • Helping to choose how & where to receive terminal care • Comfort in preparing an advance directive • Educate about available settings • Dying Person’s Bill of Rights: nurse cares for dying clients with respect, no matter what their emotional, physical or cognitive state; Box 38 -1, pg. 844 • Nurses • Help clients pass thru each stage • Provide Emotional support • Supporting choices with terminal care • Facilitate directives to maintain the client’s personal dignity and focus of control • Listen to feelings & allow client to verbally work through emotions • Become nonjudgmental sounding board • Acknowledge client as unique & worthwhile
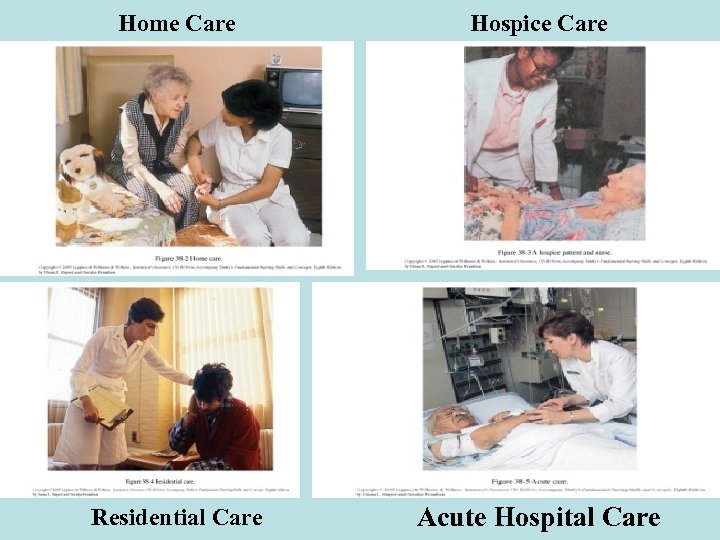 Home Care Hospice Care Residential Care Acute Hospital Care
Home Care Hospice Care Residential Care Acute Hospital Care
 Arrangements For Care • Home care: Remain at home- travel to hospital or clinic for brief treatments, tests, evaluations • Nurses help to secure home equipment, VNA • Respite care Support: Relief for caregiver by someone else • Hospice care: Involves helping clients live their final days in comfort, (relief from distressing symptoms-easing pain), dignity, and in a caring environment • Multidisciplinary team & volunteer support -Provides support for family members significant others-during care & after client’s death • Eligibility: 6 months or less to live; certified by a physician & can be re-certified if continue to meet Hospice and Medicare requirements
Arrangements For Care • Home care: Remain at home- travel to hospital or clinic for brief treatments, tests, evaluations • Nurses help to secure home equipment, VNA • Respite care Support: Relief for caregiver by someone else • Hospice care: Involves helping clients live their final days in comfort, (relief from distressing symptoms-easing pain), dignity, and in a caring environment • Multidisciplinary team & volunteer support -Provides support for family members significant others-during care & after client’s death • Eligibility: 6 months or less to live; certified by a physician & can be re-certified if continue to meet Hospice and Medicare requirements
 Arrangements For Care (cont’d) • Hospice care: Termination of care • Two ways • If withdraw to receive treatment not covered in hospice plan • No longer meets Medicare criteria • Residential care: Form of intermediate care. • Nursing homes or long-term care facilities - usual settings for subacute care • Acute care: Sophisticated technology and labor intensive treatment - when condition is unstable; most expensive care
Arrangements For Care (cont’d) • Hospice care: Termination of care • Two ways • If withdraw to receive treatment not covered in hospice plan • No longer meets Medicare criteria • Residential care: Form of intermediate care. • Nursing homes or long-term care facilities - usual settings for subacute care • Acute care: Sophisticated technology and labor intensive treatment - when condition is unstable; most expensive care
 Nurses Providing Terminal Care • Hydration: adequate fluid volume • Nourishment: little interest in eating -may choose a tube feeding or total parenteral nutrition • Elimination: incontinent of urine/stool or may have retention of urine and constipation • Skin care: very important-potential for skin breakdown R/T incontinence • Hygiene: keep dying clients clean, well groomed, free of unpleasant odors -frequent mouth care • Positioning: lateral position helps prevent choking or aspiration-change & reposition every 2 hours or more if possible • Comfort- goal keep free from pain • Try to prevent dull consciousness, inhibit communication, or suppress respirations • Given non-narcotics initially –then a combination of non-narcotics & narcotics; *may change route from oral to parenteral or transdermal • Analgesia –more effective when meds given on a routine schedule • Ex: Schedule every 4 hours or in a continuous release form through a transdermal patch rather than when necessary (PRN)
Nurses Providing Terminal Care • Hydration: adequate fluid volume • Nourishment: little interest in eating -may choose a tube feeding or total parenteral nutrition • Elimination: incontinent of urine/stool or may have retention of urine and constipation • Skin care: very important-potential for skin breakdown R/T incontinence • Hygiene: keep dying clients clean, well groomed, free of unpleasant odors -frequent mouth care • Positioning: lateral position helps prevent choking or aspiration-change & reposition every 2 hours or more if possible • Comfort- goal keep free from pain • Try to prevent dull consciousness, inhibit communication, or suppress respirations • Given non-narcotics initially –then a combination of non-narcotics & narcotics; *may change route from oral to parenteral or transdermal • Analgesia –more effective when meds given on a routine schedule • Ex: Schedule every 4 hours or in a continuous release form through a transdermal patch rather than when necessary (PRN)
 Nurses Providing Terminal Care (cont’d) • Fear of taking Medications • Addiction should not interfere with efforts to relieve pain • Develop tolerance to pain-relieving property of analgesic drugs • Some who are tolerant to opioids (narcotic meds)-develop resistance to respiratory depression • If client is alert & does not become sedated from medrespiratory depression is minimized • Constipation another common consequence of narcotic analgesia • Other medications given: Anti-anxiety, tranquilizers, antidepressants • Family involvement: care by family tends to maintain bonds and help survivors cope with future grief • Welcome the opportunity to assist • Dying Person: • Waiting for permission phenomenon • Some clients forestall dying when thy feel their loved ones not ready to accept their death-once they do-then die shortly after
Nurses Providing Terminal Care (cont’d) • Fear of taking Medications • Addiction should not interfere with efforts to relieve pain • Develop tolerance to pain-relieving property of analgesic drugs • Some who are tolerant to opioids (narcotic meds)-develop resistance to respiratory depression • If client is alert & does not become sedated from medrespiratory depression is minimized • Constipation another common consequence of narcotic analgesia • Other medications given: Anti-anxiety, tranquilizers, antidepressants • Family involvement: care by family tends to maintain bonds and help survivors cope with future grief • Welcome the opportunity to assist • Dying Person: • Waiting for permission phenomenon • Some clients forestall dying when thy feel their loved ones not ready to accept their death-once they do-then die shortly after
 Approaching Death • Dealing with death-two major fears the dying person has: • Fear of pain • Fear of being alone • Pain-accepted as being “whatever the experiencing person says it is and existing whenever he says it does” • Need reassurance- comfort needs will be met • Two or more organ systems gradually cease to function • Oxygen begins to fall below levels required to sustain life, cells, followed by tissues and organs ----begin to deteriorate • Heart • Skin • Liver • Lungs • Kidneys • Brain
Approaching Death • Dealing with death-two major fears the dying person has: • Fear of pain • Fear of being alone • Pain-accepted as being “whatever the experiencing person says it is and existing whenever he says it does” • Need reassurance- comfort needs will be met • Two or more organ systems gradually cease to function • Oxygen begins to fall below levels required to sustain life, cells, followed by tissues and organs ----begin to deteriorate • Heart • Skin • Liver • Lungs • Kidneys • Brain
 Approaching Death: Family Notification • NOTIFY physician first • Then Nurse informs family that death is approaching • If death has occurred already--- physician is responsible for notifying family • Nurse: meeting family/relatives • Nurse or other support person- meets family and informs them • Private room if possible or client’s bedside • Be aware that people show their grief in different ways
Approaching Death: Family Notification • NOTIFY physician first • Then Nurse informs family that death is approaching • If death has occurred already--- physician is responsible for notifying family • Nurse: meeting family/relatives • Nurse or other support person- meets family and informs them • Private room if possible or client’s bedside • Be aware that people show their grief in different ways
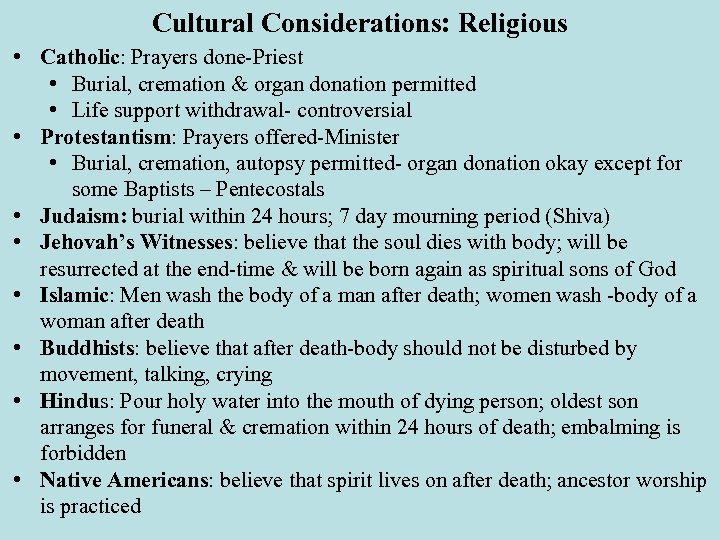 Cultural Considerations: Religious • Catholic: Prayers done-Priest • Burial, cremation & organ donation permitted • Life support withdrawal- controversial • Protestantism: Prayers offered-Minister • Burial, cremation, autopsy permitted- organ donation okay except for some Baptists – Pentecostals • Judaism: burial within 24 hours; 7 day mourning period (Shiva) • Jehovah’s Witnesses: believe that the soul dies with body; will be resurrected at the end-time & will be born again as spiritual sons of God • Islamic: Men wash the body of a man after death; women wash -body of a woman after death • Buddhists: believe that after death-body should not be disturbed by movement, talking, crying • Hindus: Pour holy water into the mouth of dying person; oldest son arranges for funeral & cremation within 24 hours of death; embalming is forbidden • Native Americans: believe that spirit lives on after death; ancestor worship is practiced
Cultural Considerations: Religious • Catholic: Prayers done-Priest • Burial, cremation & organ donation permitted • Life support withdrawal- controversial • Protestantism: Prayers offered-Minister • Burial, cremation, autopsy permitted- organ donation okay except for some Baptists – Pentecostals • Judaism: burial within 24 hours; 7 day mourning period (Shiva) • Jehovah’s Witnesses: believe that the soul dies with body; will be resurrected at the end-time & will be born again as spiritual sons of God • Islamic: Men wash the body of a man after death; women wash -body of a woman after death • Buddhists: believe that after death-body should not be disturbed by movement, talking, crying • Hindus: Pour holy water into the mouth of dying person; oldest son arranges for funeral & cremation within 24 hours of death; embalming is forbidden • Native Americans: believe that spirit lives on after death; ancestor worship is practiced
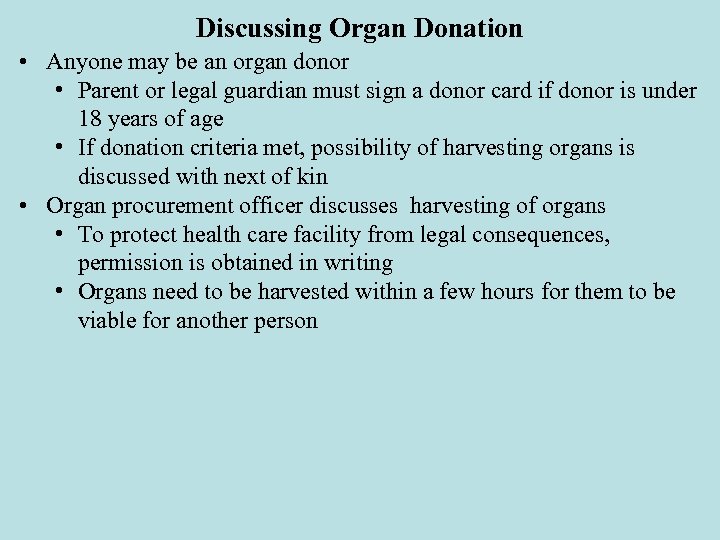 Discussing Organ Donation • Anyone may be an organ donor • Parent or legal guardian must sign a donor card if donor is under 18 years of age • If donation criteria met, possibility of harvesting organs is discussed with next of kin • Organ procurement officer discusses harvesting of organs • To protect health care facility from legal consequences, permission is obtained in writing • Organs need to be harvested within a few hours for them to be viable for another person
Discussing Organ Donation • Anyone may be an organ donor • Parent or legal guardian must sign a donor card if donor is under 18 years of age • If donation criteria met, possibility of harvesting organs is discussed with next of kin • Organ procurement officer discusses harvesting of organs • To protect health care facility from legal consequences, permission is obtained in writing • Organs need to be harvested within a few hours for them to be viable for another person
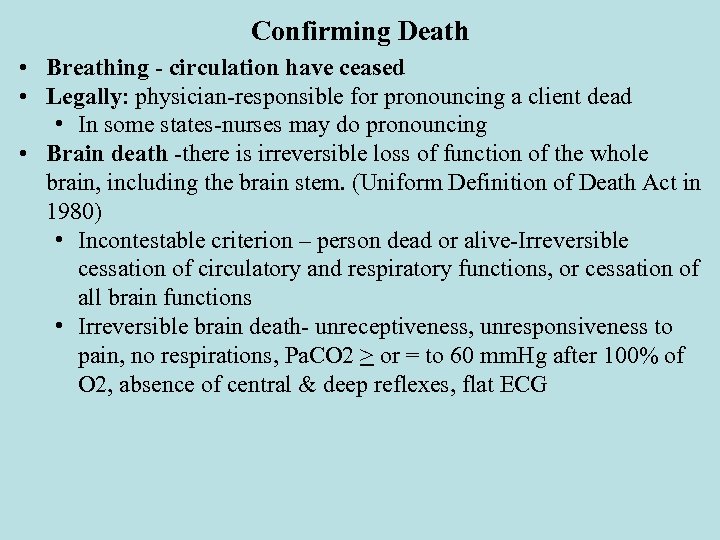 Confirming Death • Breathing - circulation have ceased • Legally: physician-responsible for pronouncing a client dead • In some states-nurses may do pronouncing • Brain death -there is irreversible loss of function of the whole brain, including the brain stem. (Uniform Definition of Death Act in 1980) • Incontestable criterion – person dead or alive-Irreversible cessation of circulatory and respiratory functions, or cessation of all brain functions • Irreversible brain death- unreceptiveness, unresponsiveness to pain, no respirations, Pa. CO 2 > or = to 60 mm. Hg after 100% of O 2, absence of central & deep reflexes, flat ECG
Confirming Death • Breathing - circulation have ceased • Legally: physician-responsible for pronouncing a client dead • In some states-nurses may do pronouncing • Brain death -there is irreversible loss of function of the whole brain, including the brain stem. (Uniform Definition of Death Act in 1980) • Incontestable criterion – person dead or alive-Irreversible cessation of circulatory and respiratory functions, or cessation of all brain functions • Irreversible brain death- unreceptiveness, unresponsiveness to pain, no respirations, Pa. CO 2 > or = to 60 mm. Hg after 100% of O 2, absence of central & deep reflexes, flat ECG
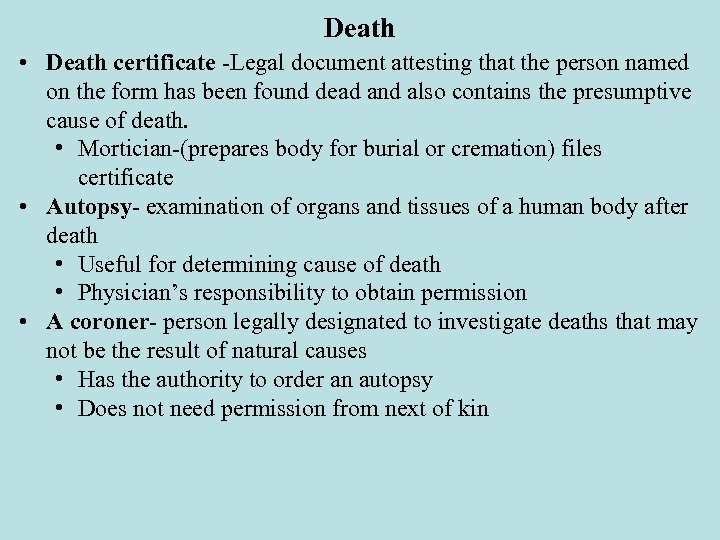 Death • Death certificate -Legal document attesting that the person named on the form has been found dead and also contains the presumptive cause of death. • Mortician-(prepares body for burial or cremation) files certificate • Autopsy- examination of organs and tissues of a human body after death • Useful for determining cause of death • Physician’s responsibility to obtain permission • A coroner- person legally designated to investigate deaths that may not be the result of natural causes • Has the authority to order an autopsy • Does not need permission from next of kin
Death • Death certificate -Legal document attesting that the person named on the form has been found dead and also contains the presumptive cause of death. • Mortician-(prepares body for burial or cremation) files certificate • Autopsy- examination of organs and tissues of a human body after death • Useful for determining cause of death • Physician’s responsibility to obtain permission • A coroner- person legally designated to investigate deaths that may not be the result of natural causes • Has the authority to order an autopsy • Does not need permission from next of kin
 Postmortem Care • Care of body after death • Involves cleaning –preparing body to enhance appearance during family viewing • May need to replace hospital gown, clothes, clean client of incontinence • Facility may have a postmortem kit
Postmortem Care • Care of body after death • Involves cleaning –preparing body to enhance appearance during family viewing • May need to replace hospital gown, clothes, clean client of incontinence • Facility may have a postmortem kit
 Grieving • Grieving- Process of feeling acute sorrow over a loss • Painful but Helps survivors to resolve the loss • Anticipatory grieving –before loss occurs experienced by family, friends & client • Grief work-activities involving grieving (burial preparation etc. ) • Grief response –universal –psychological & physical phenomena • Psychological reactions – Stages of Grief • Shock and disbelief • Developing awareness (feeling sick, sad, empty, angry) • Restitution period (recognition of loss) • Idealization (exaggeration of the good qualities of deceased • Pathologic grief-Dysfunctional: may keep possessions of a deceased loved one exactly as they were at the time of death for a prolonged period of time---may attempt to contact the deceased with séances
Grieving • Grieving- Process of feeling acute sorrow over a loss • Painful but Helps survivors to resolve the loss • Anticipatory grieving –before loss occurs experienced by family, friends & client • Grief work-activities involving grieving (burial preparation etc. ) • Grief response –universal –psychological & physical phenomena • Psychological reactions – Stages of Grief • Shock and disbelief • Developing awareness (feeling sick, sad, empty, angry) • Restitution period (recognition of loss) • Idealization (exaggeration of the good qualities of deceased • Pathologic grief-Dysfunctional: may keep possessions of a deceased loved one exactly as they were at the time of death for a prolonged period of time---may attempt to contact the deceased with séances
 Grieving (cont’d) • Paranormal experience-Outside scientific explanation • Seeing, hearing, feeling continued presence of deceased • Pathologic or Dysfunctional Grief • Cannot accept someone’s death • Manifest bizarre or morbid behaviors • Resolution of Grief • No standard length of time for “normal” grieving • Signs of resolving grief: • Abe to talk about the deceased without becoming too emotional • Describing the deceased good and bad qualities • Important to accept and support all in whatever stage they are in –try not to direct progress • Nurses: need to be available for comfort
Grieving (cont’d) • Paranormal experience-Outside scientific explanation • Seeing, hearing, feeling continued presence of deceased • Pathologic or Dysfunctional Grief • Cannot accept someone’s death • Manifest bizarre or morbid behaviors • Resolution of Grief • No standard length of time for “normal” grieving • Signs of resolving grief: • Abe to talk about the deceased without becoming too emotional • Describing the deceased good and bad qualities • Important to accept and support all in whatever stage they are in –try not to direct progress • Nurses: need to be available for comfort
 Nursing Interventions with Grieving Clients • Use skills that are most effective and appropriate for client & family • Attentive listening • Silence • Open and closed questioning • Paraphrasing • Clarifying and reflecting feelings • Summarizing • Use therapeutic communication relevant to client’s stage of grief
Nursing Interventions with Grieving Clients • Use skills that are most effective and appropriate for client & family • Attentive listening • Silence • Open and closed questioning • Paraphrasing • Clarifying and reflecting feelings • Summarizing • Use therapeutic communication relevant to client’s stage of grief
 Nursing Process • • • Assessment Diagnoses (Review page 851) Plan Interventions Supportive care—Be there for client-family • Assist with ADLs • Turn & reposition at least q 2 hours • Monitor VS, skin, I & O • Assess cognitive status, depression, anxiety • Administer pain meds-monitor effectiveness & side effects • Provide nutrition & fluids • Allow client/family to express fears • Provide education & information
Nursing Process • • • Assessment Diagnoses (Review page 851) Plan Interventions Supportive care—Be there for client-family • Assist with ADLs • Turn & reposition at least q 2 hours • Monitor VS, skin, I & O • Assess cognitive status, depression, anxiety • Administer pain meds-monitor effectiveness & side effects • Provide nutrition & fluids • Allow client/family to express fears • Provide education & information
 Gerontological & Others for Considerations • Allow dying client to continue to have interpersonal relationships • Some develop illness & die within 6 months of the death of a spouse • Encourage the individual who has experienced death to discuss their feelings • Elderly read obituaries to learn what is happening to their friends (a form of effective coping mechanism) • Death--individualized experience influenced by prior experiences, cultural practices & personal development • Encourage Hospice if meet criteria • Include client in all aspects of care-helps to maintain self-esteem & dignity • Many older adults & others prepare advanced directives concerning health care and identify a durable power of attorney • Health care-evaluate use of antidepressants & otherapies for older adults who have depression • Older adults have the highest rate of suicide • Important for health care personnel to assess suicide risk & to implement appropriate precautions
Gerontological & Others for Considerations • Allow dying client to continue to have interpersonal relationships • Some develop illness & die within 6 months of the death of a spouse • Encourage the individual who has experienced death to discuss their feelings • Elderly read obituaries to learn what is happening to their friends (a form of effective coping mechanism) • Death--individualized experience influenced by prior experiences, cultural practices & personal development • Encourage Hospice if meet criteria • Include client in all aspects of care-helps to maintain self-esteem & dignity • Many older adults & others prepare advanced directives concerning health care and identify a durable power of attorney • Health care-evaluate use of antidepressants & otherapies for older adults who have depression • Older adults have the highest rate of suicide • Important for health care personnel to assess suicide risk & to implement appropriate precautions
 Legal Definitions • End of Life Treatment Decisions • Advanced Health Care Directives • Durable Power of Attorney-Health Care Proxy • Appoints an agent the person trusts to make decisions in the event of incapacity • Living Will: provides specific instructions about kinds of healthcare that should be provided or foregone • DO-NOT-Resuscitate (DNR): no attempts to be made to resuscitate a client who stops breathing or whose heart stops beating • End of Life Treatment Decisions • DNI – Do Not Intubate: Not Inserting a tube in the trachea for continue life support • Comfort Measures Only: Goal of treatment is a comfortable dignified death with no life-sustaining measure • Do-Not-Hospitalize: used in nursing homes and residential settings
Legal Definitions • End of Life Treatment Decisions • Advanced Health Care Directives • Durable Power of Attorney-Health Care Proxy • Appoints an agent the person trusts to make decisions in the event of incapacity • Living Will: provides specific instructions about kinds of healthcare that should be provided or foregone • DO-NOT-Resuscitate (DNR): no attempts to be made to resuscitate a client who stops breathing or whose heart stops beating • End of Life Treatment Decisions • DNI – Do Not Intubate: Not Inserting a tube in the trachea for continue life support • Comfort Measures Only: Goal of treatment is a comfortable dignified death with no life-sustaining measure • Do-Not-Hospitalize: used in nursing homes and residential settings
 References • Timby, B. K. (2013) (10 th ed. ). Fundamental Nursing Skills and Concepts. Philadelphia: PA. , Lippincott Williams & Wilkins • Images retrieved from we site www. http: // googleimages. com in September 2015 • Taylor, C. , Lillis, C. , Le. Mone, P. , Lynn, P. , (2011) (7 th ed. ) Fundamentals of Nursing The Art and Science of Nursing Care Lippincott Williams & Wilkins, Philadelphia: PA.
References • Timby, B. K. (2013) (10 th ed. ). Fundamental Nursing Skills and Concepts. Philadelphia: PA. , Lippincott Williams & Wilkins • Images retrieved from we site www. http: // googleimages. com in September 2015 • Taylor, C. , Lillis, C. , Le. Mone, P. , Lynn, P. , (2011) (7 th ed. ) Fundamentals of Nursing The Art and Science of Nursing Care Lippincott Williams & Wilkins, Philadelphia: PA.


