c701638879e3735416c95e968ebfdcb8.ppt
- Количество слайдов: 32
 Chapter 23 The Child with a Sensory or Neurological Condition
Chapter 23 The Child with a Sensory or Neurological Condition
 Ears • 2 main functions: – hearing & balance • 3 divisions: – External, middle, inner – Eustachian tubes: for ventilation, protection, drainage • Assessment: – Examine ears for alignment – Low-set ears may be assoc with kidney dx and mental retardation
Ears • 2 main functions: – hearing & balance • 3 divisions: – External, middle, inner – Eustachian tubes: for ventilation, protection, drainage • Assessment: – Examine ears for alignment – Low-set ears may be assoc with kidney dx and mental retardation
 Otitis Externa & Media (AOM) • Otitis Externa – acute infection of outer ear; also called swimmer’s ear – S/S: Pain on touching the outer ear; erythema of ear canal – R/O other causes. Tx: irrigation, topical antibiotics • Otitis Media – inflammation of middle ear. – More common in children because of short or blocked eustachian tubes. – Occurs most often after URI – Affects children between 6 & 24 mo. • S/S: fever (may be high); pain, N/V, diarrhea • Treatment: antibiotics & analgesics. – Surgical tx: myringotomy » incision into eardrum to relieve pressure; tympanic tubes for ventilation – avoid water in ears
Otitis Externa & Media (AOM) • Otitis Externa – acute infection of outer ear; also called swimmer’s ear – S/S: Pain on touching the outer ear; erythema of ear canal – R/O other causes. Tx: irrigation, topical antibiotics • Otitis Media – inflammation of middle ear. – More common in children because of short or blocked eustachian tubes. – Occurs most often after URI – Affects children between 6 & 24 mo. • S/S: fever (may be high); pain, N/V, diarrhea • Treatment: antibiotics & analgesics. – Surgical tx: myringotomy » incision into eardrum to relieve pressure; tympanic tubes for ventilation – avoid water in ears
 Ear Infections • S/S – – – – – Rubbing or pulling @ear Rolling head side to side Don’t sleep well Hearing loss Loud speech Inattentive behavior Articulation problems Speech dev. Problems Red/bulging eardrum
Ear Infections • S/S – – – – – Rubbing or pulling @ear Rolling head side to side Don’t sleep well Hearing loss Loud speech Inattentive behavior Articulation problems Speech dev. Problems Red/bulging eardrum
 Hearing Deficit & Ear Trauma • Hearing Deficit • Can affect speech, language, social & emotional develpment – Congenital • hearing loss present @ birth – Acquired • infectious diseases, allergies, meds • Degrees of hearing loss – Complete • difficulty communicating, behavior problems, may be aggressive – Partial • most commonly caused by chronic ear infections or blockage of eustachian tubes • Lack of response by infant to sounds, music or the startle reflex are first signs of possible hearing impairment
Hearing Deficit & Ear Trauma • Hearing Deficit • Can affect speech, language, social & emotional develpment – Congenital • hearing loss present @ birth – Acquired • infectious diseases, allergies, meds • Degrees of hearing loss – Complete • difficulty communicating, behavior problems, may be aggressive – Partial • most commonly caused by chronic ear infections or blockage of eustachian tubes • Lack of response by infant to sounds, music or the startle reflex are first signs of possible hearing impairment
 Nursing Care • Be aware of signs & symptoms of hearing problems – – – Behavior problems Indifference to sound Poor school performance Moro reflex lasting more than 4 months No verbal attempts @ age 18 months • If suspect hearing loss make appropriate referrals
Nursing Care • Be aware of signs & symptoms of hearing problems – – – Behavior problems Indifference to sound Poor school performance Moro reflex lasting more than 4 months No verbal attempts @ age 18 months • If suspect hearing loss make appropriate referrals
 Nursing Care of Hearing-Impaired • • • Be at eye-level with child Be face-to-face with child Establish eye contact Talk in short sentences Avoid using exaggerated lip or face movement
Nursing Care of Hearing-Impaired • • • Be at eye-level with child Be face-to-face with child Establish eye contact Talk in short sentences Avoid using exaggerated lip or face movement
 Eye • Visual acuity: @ birth is about 20/400 but matures to 20/30 to 20/20 by age 23 • Eyes may appear crossed in early weeks of life Depth perception @ 9 months
Eye • Visual acuity: @ birth is about 20/400 but matures to 20/30 to 20/20 by age 23 • Eyes may appear crossed in early weeks of life Depth perception @ 9 months
 Eye Disorders • Dyslexia – a reading disability involving a defect in the brain cortex • Amblyopia (Lazy Eye) – A strong preference for one eye over the other – Tx: patch the good eye to force use of affected eye • Strabismus – cross-eye due to lack of coordination between eye muscles – s/s: eye squinting or frowning to focus • Missed objects reached for • Covering one eye to see • Tilting head to see • Dizziness and/or HA
Eye Disorders • Dyslexia – a reading disability involving a defect in the brain cortex • Amblyopia (Lazy Eye) – A strong preference for one eye over the other – Tx: patch the good eye to force use of affected eye • Strabismus – cross-eye due to lack of coordination between eye muscles – s/s: eye squinting or frowning to focus • Missed objects reached for • Covering one eye to see • Tilting head to see • Dizziness and/or HA
 Eye Infections & Tumors • Conjunctivitis (Pink Eye) – inflammation of the conjunctiva – caused by: viral or bacterial agents, allergens, toxins, irritants, systemic dx. or blockage of tear duct. – Tx: warm compresses, antibiotic eye ointments or drops. – Spreads easily - Use good hand washing and separate towel – N. I. : teach parents & children to wipe secretions from inner canthus downward & away from other eye
Eye Infections & Tumors • Conjunctivitis (Pink Eye) – inflammation of the conjunctiva – caused by: viral or bacterial agents, allergens, toxins, irritants, systemic dx. or blockage of tear duct. – Tx: warm compresses, antibiotic eye ointments or drops. – Spreads easily - Use good hand washing and separate towel – N. I. : teach parents & children to wipe secretions from inner canthus downward & away from other eye
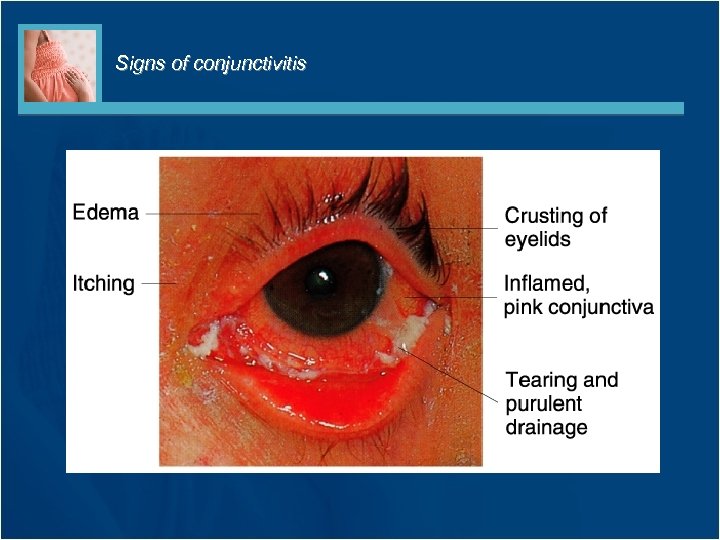 Signs of conjunctivitis
Signs of conjunctivitis
 More Stuff • Retinoblastoma – malignant tumor of retina – S/S: yellowish white reflex is seen in the pupil because of tumor behind lens; also loss of vision, strabismus, pain. – Treatment: Enucleation (removal of eye) if vision cannot be saved. Small tumors treated with laser
More Stuff • Retinoblastoma – malignant tumor of retina – S/S: yellowish white reflex is seen in the pupil because of tumor behind lens; also loss of vision, strabismus, pain. – Treatment: Enucleation (removal of eye) if vision cannot be saved. Small tumors treated with laser
 Reyes Syndrome • Reyes Syndrome – an acute encephalopathy & hepatopathy (pathology of liver) following a viral infection in children – Discourage the use of aspirin & other medications that contain salicylates in children with flu-like s/s.
Reyes Syndrome • Reyes Syndrome – an acute encephalopathy & hepatopathy (pathology of liver) following a viral infection in children – Discourage the use of aspirin & other medications that contain salicylates in children with flu-like s/s.
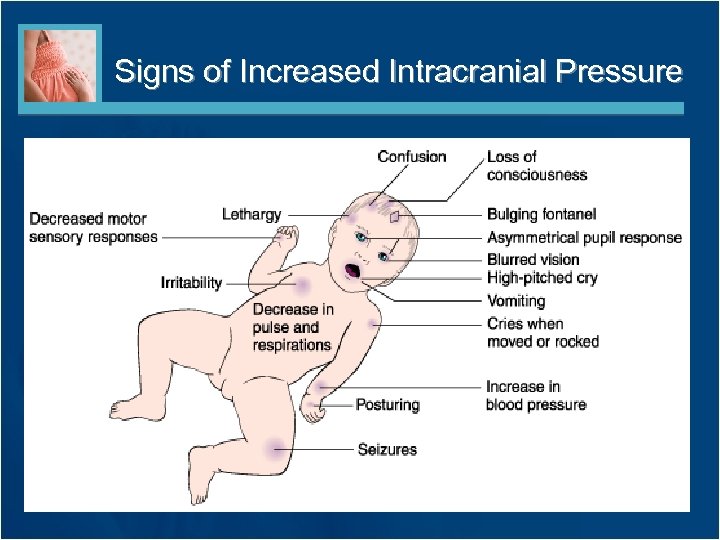 Signs of Increased Intracranial Pressure
Signs of Increased Intracranial Pressure
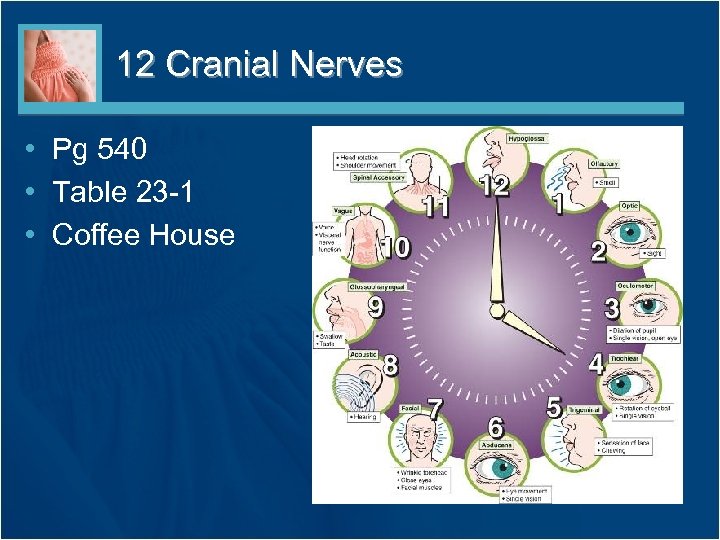 12 Cranial Nerves • Pg 540 • Table 23 -1 • Coffee House
12 Cranial Nerves • Pg 540 • Table 23 -1 • Coffee House
 Meningitis: Inflammation of the Meninges • Bacterial – Indirectly (sepsis) r/t teeth, sinuses, tonsils, lungs; or directly – through ear or skull fx – Peak age is between 6 & 12 months • Viral – Readily transmitted to others – Less common in children older than 4 – S/S: May be preceded by URI & poor feeding. Severe HA, drowsiness, delirium, irritability, fever, vomiting, neck stiffness; convulsions are common; coma. – Infants will have high-pitched cry – Treatment: At first indication, a spinal tap (lumbar puncture) will be performed to test CSF – Nursing Care: frequent VS Slowed P, irreg. resp. & ^B/P could indicate increased ICP and are reported immediately
Meningitis: Inflammation of the Meninges • Bacterial – Indirectly (sepsis) r/t teeth, sinuses, tonsils, lungs; or directly – through ear or skull fx – Peak age is between 6 & 12 months • Viral – Readily transmitted to others – Less common in children older than 4 – S/S: May be preceded by URI & poor feeding. Severe HA, drowsiness, delirium, irritability, fever, vomiting, neck stiffness; convulsions are common; coma. – Infants will have high-pitched cry – Treatment: At first indication, a spinal tap (lumbar puncture) will be performed to test CSF – Nursing Care: frequent VS Slowed P, irreg. resp. & ^B/P could indicate increased ICP and are reported immediately
 Brain Tumors • The second most common type of neoplasm in children (1 st is leukemia) • The majority of childhood tumors occur in the lower part of the brain (cerebellum or brain stem) • Symptoms are directly related to the location and size of the tumor – Most tumors cause increased ICP with hallmark symptoms of headache, vomiting, drowsiness, and seizures
Brain Tumors • The second most common type of neoplasm in children (1 st is leukemia) • The majority of childhood tumors occur in the lower part of the brain (cerebellum or brain stem) • Symptoms are directly related to the location and size of the tumor – Most tumors cause increased ICP with hallmark symptoms of headache, vomiting, drowsiness, and seizures
 Seizure Disorders • Seizures – May be febrile ( rapid rise in temperature) or due to ^ICP – Common in children 6 months to 5 yo – Parents should be reassured that it is self-limiting – Table 23 -2 types of seizures & response, pg 545 • Epilepsy – recurrent attacks of unconsciousness or impaired consciousness followed by tonic-clonic behavior • a disorder of the CNS r/t neurons firing improperly
Seizure Disorders • Seizures – May be febrile ( rapid rise in temperature) or due to ^ICP – Common in children 6 months to 5 yo – Parents should be reassured that it is self-limiting – Table 23 -2 types of seizures & response, pg 545 • Epilepsy – recurrent attacks of unconsciousness or impaired consciousness followed by tonic-clonic behavior • a disorder of the CNS r/t neurons firing improperly
 Seizures, cont. • Grand mal – 3 phases: aura, tonic/clonic seizure, lethargy • Petit mal (absence seizure) – temporary loss of awareness • Partial – jerking in one part of body – pt. awake & alert • Complex partial – blank stare followed by random activity – pt. unaware • Atonic – sudden collapse
Seizures, cont. • Grand mal – 3 phases: aura, tonic/clonic seizure, lethargy • Petit mal (absence seizure) – temporary loss of awareness • Partial – jerking in one part of body – pt. awake & alert • Complex partial – blank stare followed by random activity – pt. unaware • Atonic – sudden collapse
 Treatment of Seizures • EEG to determine type of seizure • Anticonvulsant meds – Nursing Interventions (know med side-effects) • • Phenobarbitol causes drowsiness Dilantin causes gum hyperplasia (massage gums) Depakene needs to be taken with food Mysoline can cause aggressive behavior • Ketogenic Diet – high fat, low carbs to produce ketoacidosis & reduce seizures • N. I. during a seizure, protect patient from nearby hazards
Treatment of Seizures • EEG to determine type of seizure • Anticonvulsant meds – Nursing Interventions (know med side-effects) • • Phenobarbitol causes drowsiness Dilantin causes gum hyperplasia (massage gums) Depakene needs to be taken with food Mysoline can cause aggressive behavior • Ketogenic Diet – high fat, low carbs to produce ketoacidosis & reduce seizures • N. I. during a seizure, protect patient from nearby hazards
 Cerebral palsy • Disorders of the motor center of brain – One of most common disabling conditions – s/s range from mild to severe – Goal of treatment is to assist child in making the most of their assets, perform at their maximum ability, become well-adjusted adults – Help parents to accept the child & guide them to community resources – Good skin care, prevention of contractures
Cerebral palsy • Disorders of the motor center of brain – One of most common disabling conditions – s/s range from mild to severe – Goal of treatment is to assist child in making the most of their assets, perform at their maximum ability, become well-adjusted adults – Help parents to accept the child & guide them to community resources – Good skin care, prevention of contractures
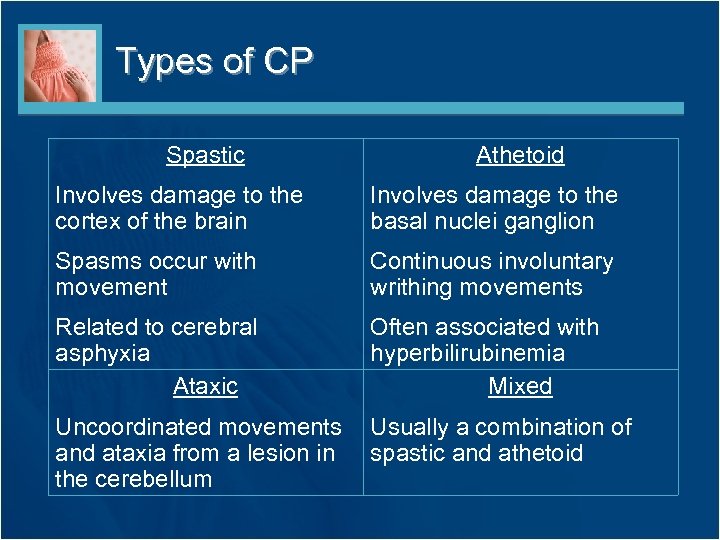 Types of CP Spastic Athetoid Involves damage to the cortex of the brain Involves damage to the basal nuclei ganglion Spasms occur with movement Continuous involuntary writhing movements Related to cerebral asphyxia Ataxic Often associated with hyperbilirubinemia Mixed Uncoordinated movements and ataxia from a lesion in the cerebellum Usually a combination of spastic and athetoid
Types of CP Spastic Athetoid Involves damage to the cortex of the brain Involves damage to the basal nuclei ganglion Spasms occur with movement Continuous involuntary writhing movements Related to cerebral asphyxia Ataxic Often associated with hyperbilirubinemia Mixed Uncoordinated movements and ataxia from a lesion in the cerebellum Usually a combination of spastic and athetoid
 Treatment of CP • Botulinum toxin has been used to manage spasticity problems • Levodopa has helped to control some of the athetoid problems • Specific treatment is highly individualized – Good skin care is essential – All precautions taken to prevent contractures • Braces are often used to treat these • Orthopedic surgery is sometimes indicated
Treatment of CP • Botulinum toxin has been used to manage spasticity problems • Levodopa has helped to control some of the athetoid problems • Specific treatment is highly individualized – Good skin care is essential – All precautions taken to prevent contractures • Braces are often used to treat these • Orthopedic surgery is sometimes indicated
 Treatment Protocol for CP • • • Establish communication Establish locomotion Use and optimize existing motor functions Provide intellectual stimulation Promote socialization Provide technology to encourage self-care and promote growth and development • Provide multidisciplinary approach to care
Treatment Protocol for CP • • • Establish communication Establish locomotion Use and optimize existing motor functions Provide intellectual stimulation Promote socialization Provide technology to encourage self-care and promote growth and development • Provide multidisciplinary approach to care
 Mental Retardation • Below-average mental functioning (IQ below 75) • Nursing Interventions – – – emphasize the strengths Communicate with family Avoid labels, use simple terms Contact school nurse & plan ahead Provide daily opportunities for success Refer to support groups
Mental Retardation • Below-average mental functioning (IQ below 75) • Nursing Interventions – – – emphasize the strengths Communicate with family Avoid labels, use simple terms Contact school nurse & plan ahead Provide daily opportunities for success Refer to support groups
 Head Injuries • Major cause of death in children older than 1 year • Concussion – temporary disturbance of brain, usually followed by period of unconsciousness – Loss of memory for events that happened immediately before, during and after accident
Head Injuries • Major cause of death in children older than 1 year • Concussion – temporary disturbance of brain, usually followed by period of unconsciousness – Loss of memory for events that happened immediately before, during and after accident
 Shaken Baby Syndrome • Infants who are roughly • Symptoms shaken can sustain – Headache (manifested as fussiness in a retinal, subarachnoid, and toddler) subdural hemorrhages in – Drowsiness the brain, as well as high– Blurred vision level cervical spine – Vomiting injuries – Dyspnea • Can result in permanent • In severe cases child brain injury or death may be completely unconscious
Shaken Baby Syndrome • Infants who are roughly • Symptoms shaken can sustain – Headache (manifested as fussiness in a retinal, subarachnoid, and toddler) subdural hemorrhages in – Drowsiness the brain, as well as high– Blurred vision level cervical spine – Vomiting injuries – Dyspnea • Can result in permanent • In severe cases child brain injury or death may be completely unconscious
 Neurological Monitoring of Infants and Children • • Pain stimuli response LOC Arousal awareness Cranial nerve response • Motor response • Posturing • Vital Signs • Pupil response of the eyes • Bulging fontanels • Scalp vein distention • Ataxia; spasticity of lower extremities • Moro/tonic neck withdrawal reflexes
Neurological Monitoring of Infants and Children • • Pain stimuli response LOC Arousal awareness Cranial nerve response • Motor response • Posturing • Vital Signs • Pupil response of the eyes • Bulging fontanels • Scalp vein distention • Ataxia; spasticity of lower extremities • Moro/tonic neck withdrawal reflexes
 Posturing • Often seen with severe brain injury • Decerebrate – Rigidity with all 4 limbs extended & hands pronated – May indicate brainstem injury • Decorticate – Arms, wrists & fingers are flexed; feet show plantar flexion – May indicate damage to cortex of brain
Posturing • Often seen with severe brain injury • Decerebrate – Rigidity with all 4 limbs extended & hands pronated – May indicate brainstem injury • Decorticate – Arms, wrists & fingers are flexed; feet show plantar flexion – May indicate damage to cortex of brain
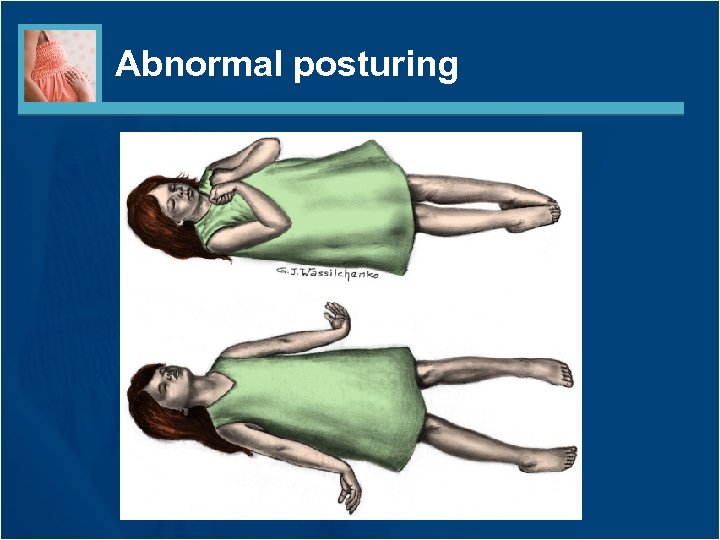 Abnormal posturing
Abnormal posturing
 Near-Drowning • Accidental or near-drowning is the fourth leading cause of death in children under 19 years of age • Near-drowning is defined as survival beyond 24 hours after submersion • Priorities include immediate treatment of – Hypoxia – Aspiration – Hypothermia • CNS injury remains the major cause of death or long-term disability
Near-Drowning • Accidental or near-drowning is the fourth leading cause of death in children under 19 years of age • Near-drowning is defined as survival beyond 24 hours after submersion • Priorities include immediate treatment of – Hypoxia – Aspiration – Hypothermia • CNS injury remains the major cause of death or long-term disability
 Elsevier items and derived items © 2011, 2007, 2006 by Saunders, an imprint of Elsevier Inc. 32
Elsevier items and derived items © 2011, 2007, 2006 by Saunders, an imprint of Elsevier Inc. 32


