c97bbffc9200effaa6ab0be5c59ee702.ppt
- Количество слайдов: 66
 Chapter 20 Care of Patients with Arthritis and Other Connective Tissue Diseases
Chapter 20 Care of Patients with Arthritis and Other Connective Tissue Diseases
 Rheumatology • Connective tissue disease (CTD) is a major focus of rheumatology. • Rheumatic disease is any disease or condition involving the musculoskeletal system. • Arthritis means inflammation of one or more joints.
Rheumatology • Connective tissue disease (CTD) is a major focus of rheumatology. • Rheumatic disease is any disease or condition involving the musculoskeletal system. • Arthritis means inflammation of one or more joints.
 Rheumatology (Cont’d) • Noninflammatory arthritis (osteoarthritis) is not systemic. OA is not an autoimmune disease. • Inflammatory arthritis: – Rheumatoid arthritis – Systemic lupus erythematosus – Autoimmune disease – Connective tissue disease that is inflammatory
Rheumatology (Cont’d) • Noninflammatory arthritis (osteoarthritis) is not systemic. OA is not an autoimmune disease. • Inflammatory arthritis: – Rheumatoid arthritis – Systemic lupus erythematosus – Autoimmune disease – Connective tissue disease that is inflammatory
 Osteoarthritis • Most common type of arthritis • Joint pain and loss of function characterized by progressive deterioration and loss of cartilage in the joints • Osteophytes • Synovitis • Subluxation
Osteoarthritis • Most common type of arthritis • Joint pain and loss of function characterized by progressive deterioration and loss of cartilage in the joints • Osteophytes • Synovitis • Subluxation
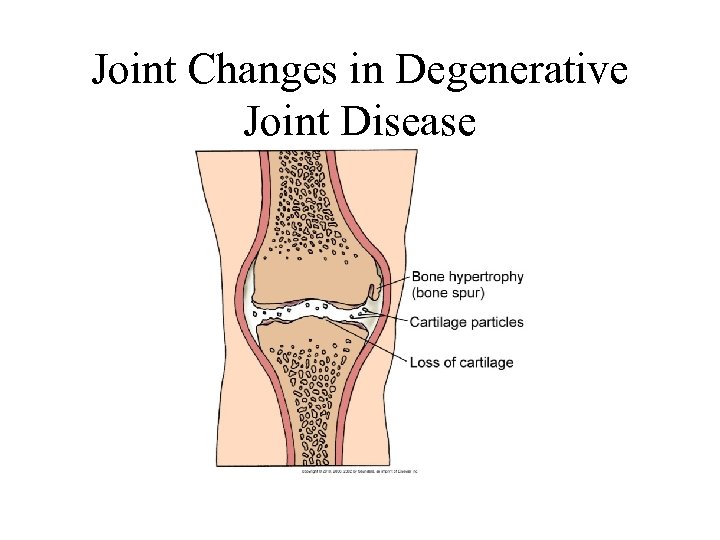 Joint Changes in Degenerative Joint Disease
Joint Changes in Degenerative Joint Disease
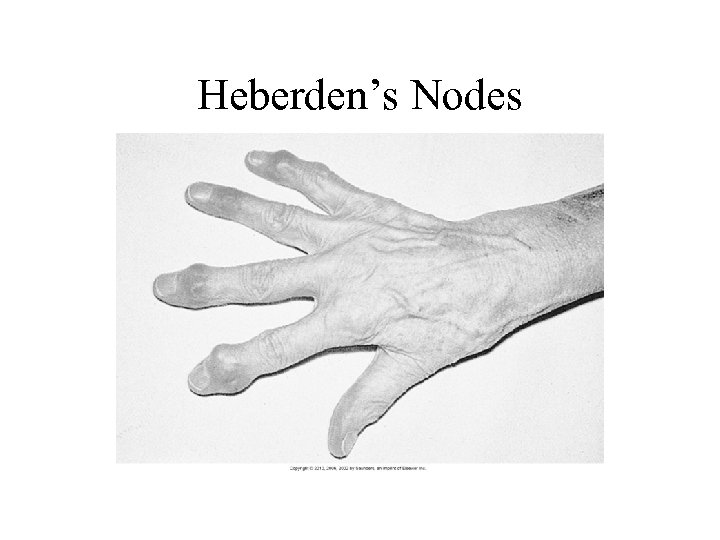
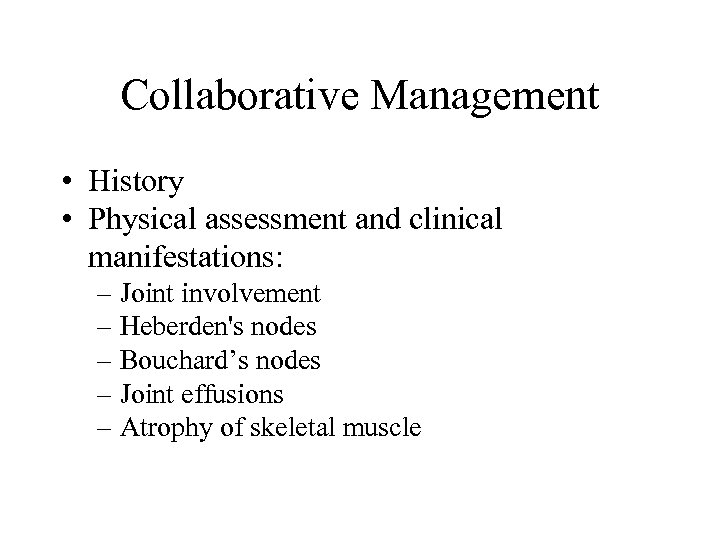 Collaborative Management • History • Physical assessment and clinical manifestations: – Joint involvement – Heberden's nodes – Bouchard’s nodes – Joint effusions – Atrophy of skeletal muscle
Collaborative Management • History • Physical assessment and clinical manifestations: – Joint involvement – Heberden's nodes – Bouchard’s nodes – Joint effusions – Atrophy of skeletal muscle
 Heberden’s Nodes
Heberden’s Nodes
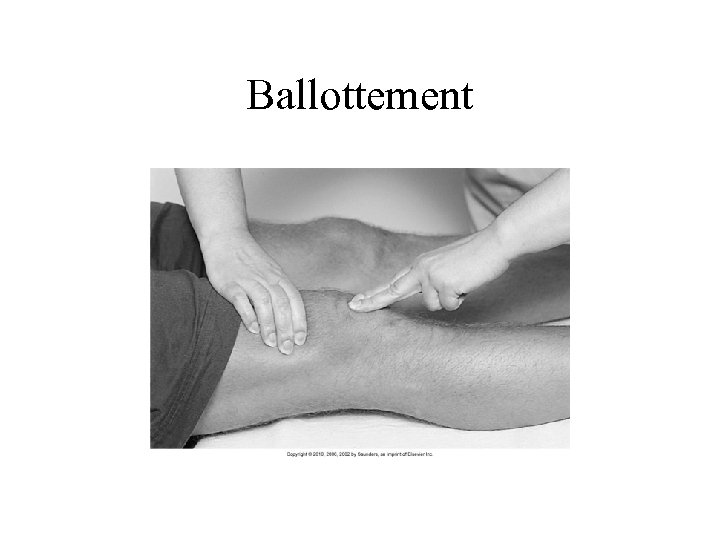 Ballottement
Ballottement
 Assessments • Psychosocial • Laboratory assessment of erythrocyte sedimentation rate and C-reactive protein (may be slightly elevated) • Radiographic assessment • Other diagnostic assessments: – MR imaging – CT studies
Assessments • Psychosocial • Laboratory assessment of erythrocyte sedimentation rate and C-reactive protein (may be slightly elevated) • Radiographic assessment • Other diagnostic assessments: – MR imaging – CT studies
 Chronic Pain: Nonsurgical Management • • • Analgesics Rest Positioning Thermal modalities Weight control Integrative therapies
Chronic Pain: Nonsurgical Management • • • Analgesics Rest Positioning Thermal modalities Weight control Integrative therapies
 Chronic Pain: Surgical Management • • Total joint arthroplasty (TJA) Total joint replacement (TJR) Arthroscopy Osteotomy
Chronic Pain: Surgical Management • • Total joint arthroplasty (TJA) Total joint replacement (TJR) Arthroscopy Osteotomy
 Total Hip Arthroplasty • Preoperative care • Operative procedures • Postoperative care: – Prevention of dislocation, infection, and thromboembolic complications – Assessment of bleeding – Management of anemia
Total Hip Arthroplasty • Preoperative care • Operative procedures • Postoperative care: – Prevention of dislocation, infection, and thromboembolic complications – Assessment of bleeding – Management of anemia
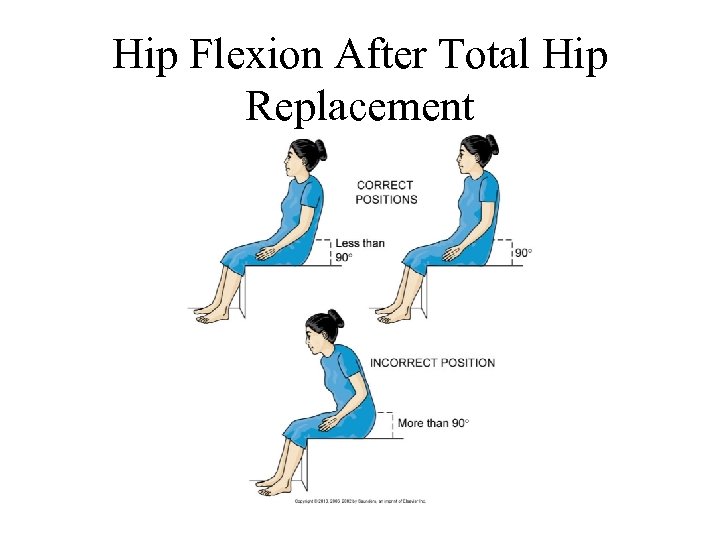 Hip Flexion After Total Hip Replacement
Hip Flexion After Total Hip Replacement
 Prevention of Complications • • Assessment for neurovascular compromise Management of pain Progression of activity Promotion of self-care
Prevention of Complications • • Assessment for neurovascular compromise Management of pain Progression of activity Promotion of self-care
 Total Knee Arthroplasty • Preoperative care • Operative procedures • Postoperative care: – Continuous passive motion machine – Hot/ice device – Pain management – Neurovascular assessment
Total Knee Arthroplasty • Preoperative care • Operative procedures • Postoperative care: – Continuous passive motion machine – Hot/ice device – Pain management – Neurovascular assessment
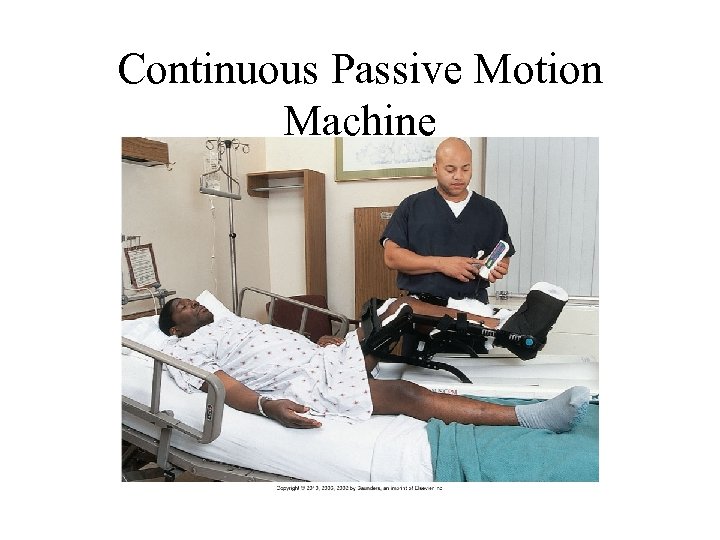 Continuous Passive Motion Machine
Continuous Passive Motion Machine
 Rheumatoid Arthritis • One of the most common connective tissue diseases and the most destructive to the joints • Chronic, progressive, systemic inflammatory autoimmune disease affecting primarily the synovial joints • Autoantibodies (rheumatoid factors) formed that attack healthy tissue, especially synovium, causing inflammation • Affects synovial tissue of any organ or body system
Rheumatoid Arthritis • One of the most common connective tissue diseases and the most destructive to the joints • Chronic, progressive, systemic inflammatory autoimmune disease affecting primarily the synovial joints • Autoantibodies (rheumatoid factors) formed that attack healthy tissue, especially synovium, causing inflammation • Affects synovial tissue of any organ or body system
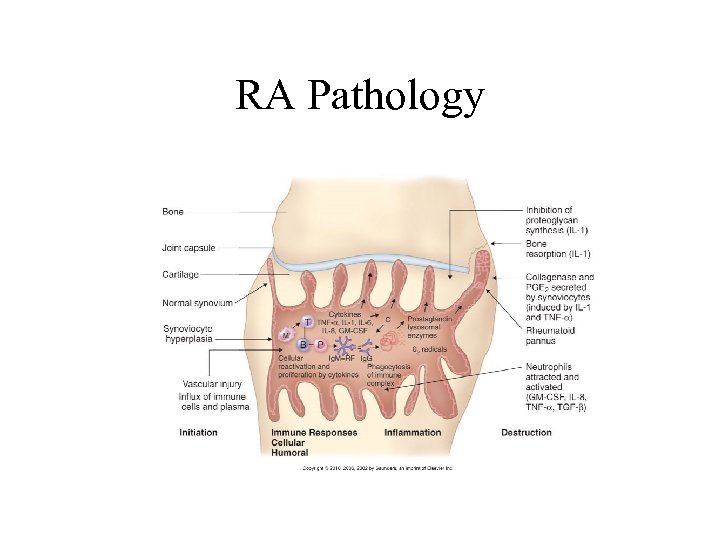 RA Pathology
RA Pathology
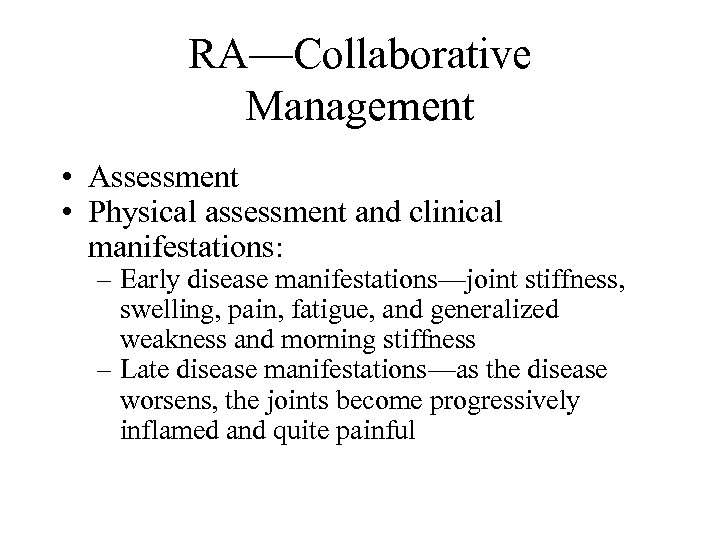 RA—Collaborative Management • Assessment • Physical assessment and clinical manifestations: – Early disease manifestations—joint stiffness, swelling, pain, fatigue, and generalized weakness and morning stiffness – Late disease manifestations—as the disease worsens, the joints become progressively inflamed and quite painful
RA—Collaborative Management • Assessment • Physical assessment and clinical manifestations: – Early disease manifestations—joint stiffness, swelling, pain, fatigue, and generalized weakness and morning stiffness – Late disease manifestations—as the disease worsens, the joints become progressively inflamed and quite painful
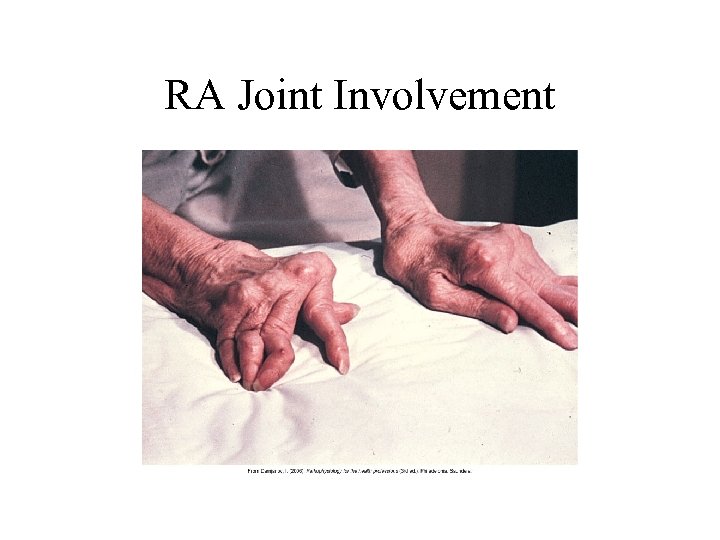 RA Joint Involvement
RA Joint Involvement
 RA Systemic Complications • • Weight loss, fever, and extreme fatigue Exacerbations Subcutaneous nodules Pulmonary complications Vasculitis Periungual lesions Paresthesias Cardiac complications
RA Systemic Complications • • Weight loss, fever, and extreme fatigue Exacerbations Subcutaneous nodules Pulmonary complications Vasculitis Periungual lesions Paresthesias Cardiac complications
 RA—Assessments • Psychosocial assessment • Laboratory assessment—rheumatoid factor, antinuclear antibody titer, erythrocyte sedimentation rate, serum complement, serum protein electrophoresis, serum immunoglobulins • Other diagnostic assessments—x-ray, CT, arthrocentesis, bone scan
RA—Assessments • Psychosocial assessment • Laboratory assessment—rheumatoid factor, antinuclear antibody titer, erythrocyte sedimentation rate, serum complement, serum protein electrophoresis, serum immunoglobulins • Other diagnostic assessments—x-ray, CT, arthrocentesis, bone scan
 RA—Drug Therapy • • Disease-modifying antirheumatic drugs NSAIDs Biologic response modifiers Other drugs: – Glucocorticoids – Immunosuppressive agents – Gold therapy – Analgesic drugs
RA—Drug Therapy • • Disease-modifying antirheumatic drugs NSAIDs Biologic response modifiers Other drugs: – Glucocorticoids – Immunosuppressive agents – Gold therapy – Analgesic drugs
 RA—Nonpharmacologic Interventions • • Adequate rest Proper positioning Ice and heat applications Plasmapheresis Gene therapy Complementary and alternative therapies Promotion of self-care
RA—Nonpharmacologic Interventions • • Adequate rest Proper positioning Ice and heat applications Plasmapheresis Gene therapy Complementary and alternative therapies Promotion of self-care
 RA—Nonpharmacologic Interventions (Cont’d) • Management of fatigue • Enhancement of body image • Community-based care: – Home care management – Health teaching – Health care resources
RA—Nonpharmacologic Interventions (Cont’d) • Management of fatigue • Enhancement of body image • Community-based care: – Home care management – Health teaching – Health care resources
 Lupus Erythematosus • Chronic, progressive, inflammatory connective tissue disorder that can cause major body organs and systems to fail. • Characterized by spontaneous remissions and exacerbations. • Autoimmune process. • Autoimmune complexes tend to be attracted to the glomeruli of the kidneys. • Many patients with SLE have some degree of kidney involvement.
Lupus Erythematosus • Chronic, progressive, inflammatory connective tissue disorder that can cause major body organs and systems to fail. • Characterized by spontaneous remissions and exacerbations. • Autoimmune process. • Autoimmune complexes tend to be attracted to the glomeruli of the kidneys. • Many patients with SLE have some degree of kidney involvement.
 Lupus Erythematosus— Clinical Manifestations • • • Skin involvement Polyarthritis Osteonecrosis Muscle atrophy Fever and fatigue
Lupus Erythematosus— Clinical Manifestations • • • Skin involvement Polyarthritis Osteonecrosis Muscle atrophy Fever and fatigue
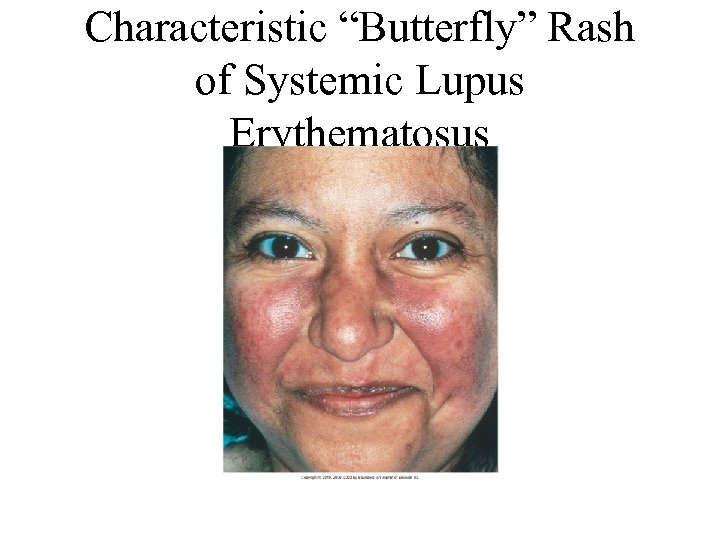 Characteristic “Butterfly” Rash of Systemic Lupus Erythematosus
Characteristic “Butterfly” Rash of Systemic Lupus Erythematosus
 LE—Clinical Manifestations • • • Renal involvement Pleural effusions Pericarditis Raynaud’s phenomenon Neurologic manifestation Serositis
LE—Clinical Manifestations • • • Renal involvement Pleural effusions Pericarditis Raynaud’s phenomenon Neurologic manifestation Serositis
 Assessments for Lupus • Psychosocial results can be devastating. • Laboratory: – Skin biopsy (only significant test to confirm diagnosis) – Immunologic-based laboratory tests – Complete blood count – Body system function assessment
Assessments for Lupus • Psychosocial results can be devastating. • Laboratory: – Skin biopsy (only significant test to confirm diagnosis) – Immunologic-based laboratory tests – Complete blood count – Body system function assessment
 SLE—Drug Therapy • • • Topical drugs Plaquenil Tylenol or NSAIDs Chronic steroid therapy Immunosuppressive agents
SLE—Drug Therapy • • • Topical drugs Plaquenil Tylenol or NSAIDs Chronic steroid therapy Immunosuppressive agents
 Scleroderma (Systemic Sclerosis) • Chronic, inflammatory, autoimmune connective tissue disease • Not always progressive • Hardening of the skin
Scleroderma (Systemic Sclerosis) • Chronic, inflammatory, autoimmune connective tissue disease • Not always progressive • Hardening of the skin
 Scleroderma
Scleroderma
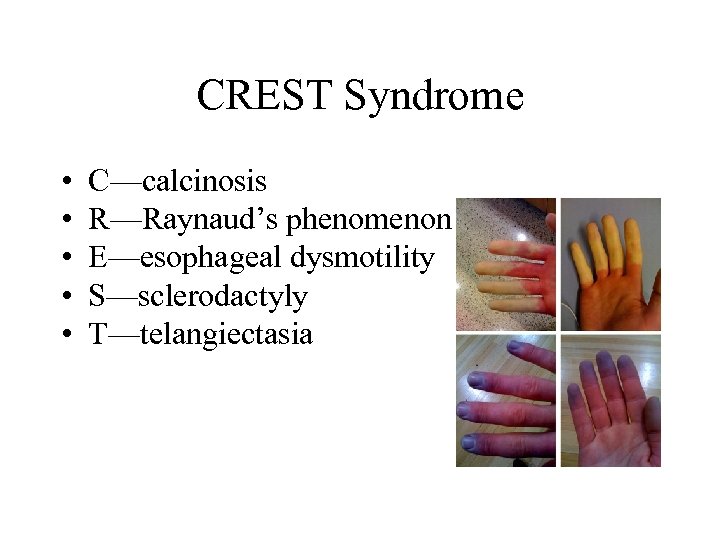 CREST Syndrome • • • C—calcinosis R—Raynaud’s phenomenon E—esophageal dysmotility S—sclerodactyly T—telangiectasia
CREST Syndrome • • • C—calcinosis R—Raynaud’s phenomenon E—esophageal dysmotility S—sclerodactyly T—telangiectasia
 Scleroderma—Clinical Manifestations • • • Arthralgia GI tract Cardiovascular system Pulmonary system Renal system
Scleroderma—Clinical Manifestations • • • Arthralgia GI tract Cardiovascular system Pulmonary system Renal system
 Scleroderma—Interventions • • • Drug therapy Identify early organ involvement Skin protective measures Comfort GI manifestation Mobility
Scleroderma—Interventions • • • Drug therapy Identify early organ involvement Skin protective measures Comfort GI manifestation Mobility
 Gout • Also called gouty arthritis, a systemic disease in which urate crystals deposit in the joints and other body tissues, causing inflammation • Primary gout • Secondary gout—hyperuricemia
Gout • Also called gouty arthritis, a systemic disease in which urate crystals deposit in the joints and other body tissues, causing inflammation • Primary gout • Secondary gout—hyperuricemia
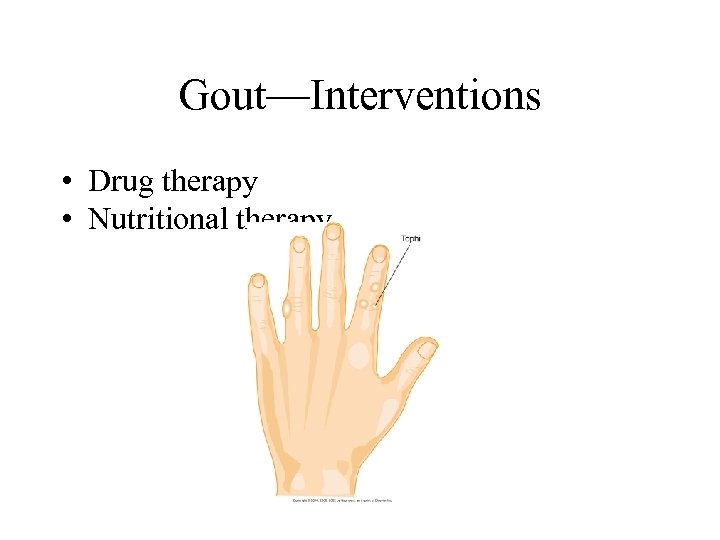 Gout—Interventions • Drug therapy • Nutritional therapy
Gout—Interventions • Drug therapy • Nutritional therapy
 Other Connective Tissue Diseases • Polymyositis • Systemic necrotizing vasculitis • Polymyalgia rheumatica and temporal arteritis • Ankylosing spondylitis • Reiter’s syndrome • Marfan syndrome • Infectious arthritis
Other Connective Tissue Diseases • Polymyositis • Systemic necrotizing vasculitis • Polymyalgia rheumatica and temporal arteritis • Ankylosing spondylitis • Reiter’s syndrome • Marfan syndrome • Infectious arthritis
 Lyme Disease • Reportable systemic infectious disease caused by the spirochete Borrelia burgdorferi, resulting from the bite of an infected deer tick. • Stages I and II. • If not diagnosed and treated in early stages, chronic complications such as arthralgias, fatigue, and memory and thinking problems can result. • For some patients, the first and only sign of Lyme disease is arthritis.
Lyme Disease • Reportable systemic infectious disease caused by the spirochete Borrelia burgdorferi, resulting from the bite of an infected deer tick. • Stages I and II. • If not diagnosed and treated in early stages, chronic complications such as arthralgias, fatigue, and memory and thinking problems can result. • For some patients, the first and only sign of Lyme disease is arthritis.
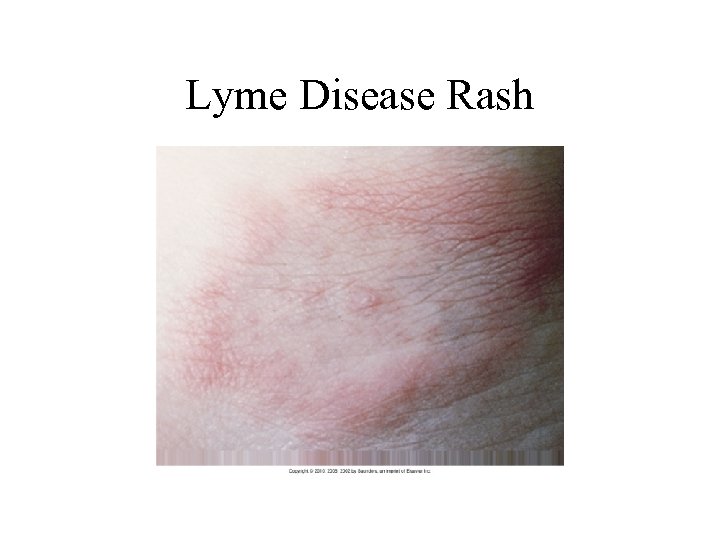 Lyme Disease Rash
Lyme Disease Rash
 Fibromyalgia Syndrome • Chronic pain syndrome, not an inflammatory disease
Fibromyalgia Syndrome • Chronic pain syndrome, not an inflammatory disease
 Chronic Fatigue Syndromes • Chronic illness in which patients have severe fatigue for 6 months or longer, usually following flu-like symptoms • Sore throat; substantial impairment in short-term memory or concentration; tender lymph nodes; muscle pain; multiple joint pain with redness or swelling; headaches of a new type, pattern, or severity; unrefreshing sleep; and postexertional malaise lasting more than 24 hours
Chronic Fatigue Syndromes • Chronic illness in which patients have severe fatigue for 6 months or longer, usually following flu-like symptoms • Sore throat; substantial impairment in short-term memory or concentration; tender lymph nodes; muscle pain; multiple joint pain with redness or swelling; headaches of a new type, pattern, or severity; unrefreshing sleep; and postexertional malaise lasting more than 24 hours
 Chapter 22 Care of Patients with Immune Function Excess: Hypersensitivity (Allergy) and Autoimmunity
Chapter 22 Care of Patients with Immune Function Excess: Hypersensitivity (Allergy) and Autoimmunity
 Hypersensitivities/Allergies • Increased or excessive response to the presence of an antigen to which the patient has been exposed • Degree of reaction ranging from uncomfortable to life threatening
Hypersensitivities/Allergies • Increased or excessive response to the presence of an antigen to which the patient has been exposed • Degree of reaction ranging from uncomfortable to life threatening
 Type I: Rapid Hypersensitivity Reactions • Also called atopic allergy, this is the most common type of hypersensitivity. • Some reactions occur just in the areas exposed to the antigen.
Type I: Rapid Hypersensitivity Reactions • Also called atopic allergy, this is the most common type of hypersensitivity. • Some reactions occur just in the areas exposed to the antigen.
 Type I: Rapid Hypersensitivity Reactions (Cont’d) • Allergens can be contacted in these ways: – Inhaled (plant pollens, fungal spores, animal dander, house dust, grass, ragweed) – Ingested (foods, food additives, drugs) – Injected (bee venom, drugs, biologic substances)
Type I: Rapid Hypersensitivity Reactions (Cont’d) • Allergens can be contacted in these ways: – Inhaled (plant pollens, fungal spores, animal dander, house dust, grass, ragweed) – Ingested (foods, food additives, drugs) – Injected (bee venom, drugs, biologic substances)
 Type I: Rapid Hypersensitivity Reactions (Cont’d) – Contacted (pollens, foods, environmental proteins) • Other reactions may involve all blood vessels and bronchiolar smooth muscle, causing widespread blood vessel dilation, decreased cardiac output, and bronchoconstriction, which is known as anaphylaxis
Type I: Rapid Hypersensitivity Reactions (Cont’d) – Contacted (pollens, foods, environmental proteins) • Other reactions may involve all blood vessels and bronchiolar smooth muscle, causing widespread blood vessel dilation, decreased cardiac output, and bronchoconstriction, which is known as anaphylaxis
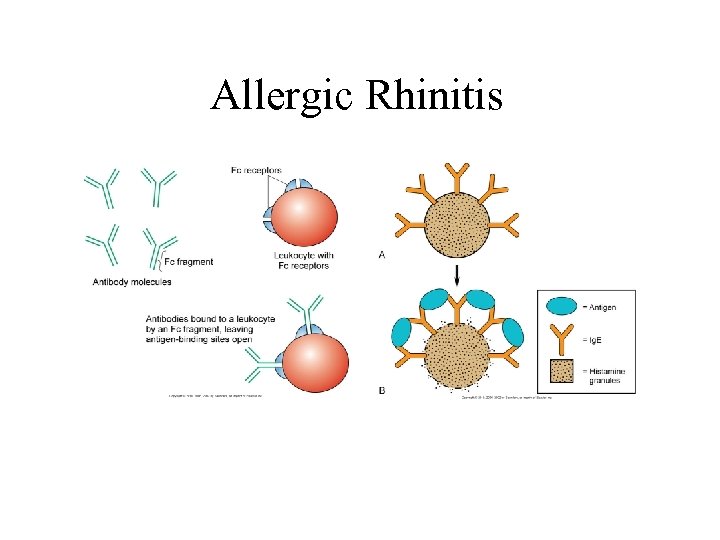 Allergic Rhinitis
Allergic Rhinitis
 Patient-Centered Collaborative Care • History • Laboratory assessment—increased eosinophils, immunoglobulin E (Ig. E), RAST • Allergy testing – Patient preparation – Procedure – Follow-up care • Oral food challenges
Patient-Centered Collaborative Care • History • Laboratory assessment—increased eosinophils, immunoglobulin E (Ig. E), RAST • Allergy testing – Patient preparation – Procedure – Follow-up care • Oral food challenges
 Interventions • Avoidance therapy: – Environmental changes: • • Air-conditioning and air-cleaning units Cloth drapes Upholstered furniture Carpeting – Pet-induced allergies
Interventions • Avoidance therapy: – Environmental changes: • • Air-conditioning and air-cleaning units Cloth drapes Upholstered furniture Carpeting – Pet-induced allergies
 Drug Therapy • • Decongestants Antihistamines Corticosteroids Mast cell stabilizers Leukotriene antagonists Complementary and alternative therapy Desensitization therapy
Drug Therapy • • Decongestants Antihistamines Corticosteroids Mast cell stabilizers Leukotriene antagonists Complementary and alternative therapy Desensitization therapy
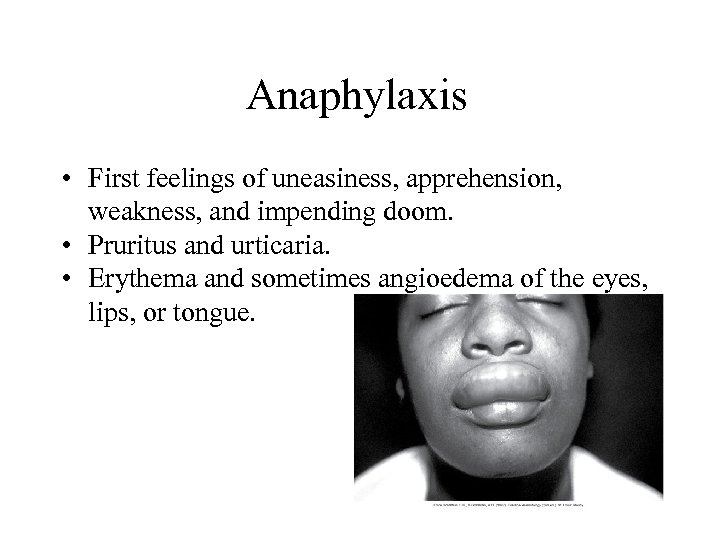 Anaphylaxis • First feelings of uneasiness, apprehension, weakness, and impending doom. • Pruritus and urticaria. • Erythema and sometimes angioedema of the eyes, lips, or tongue.
Anaphylaxis • First feelings of uneasiness, apprehension, weakness, and impending doom. • Pruritus and urticaria. • Erythema and sometimes angioedema of the eyes, lips, or tongue.
 Anaphylaxis (Cont’d) • Histamine causes capillary leak, bronchoconstriction, mucosal edema, and excess mucus secretion. • Congestion, rhinorrhea, dyspnea, and increasing respiratory distress with audible wheezing result. • Anaphylaxis can be fatal.
Anaphylaxis (Cont’d) • Histamine causes capillary leak, bronchoconstriction, mucosal edema, and excess mucus secretion. • Congestion, rhinorrhea, dyspnea, and increasing respiratory distress with audible wheezing result. • Anaphylaxis can be fatal.
 Interventions • First assess respiratory function; an airway must be established. • CPR may be needed. • Epinephrine (1: 1000) 0. 3 to 0. 5 m. L subcutaneous is given as soon as symptoms appear. • Antihistamines treat angioedema and urticaria. • Oxygen. • Treat bronchospasm. • IV fluids.
Interventions • First assess respiratory function; an airway must be established. • CPR may be needed. • Epinephrine (1: 1000) 0. 3 to 0. 5 m. L subcutaneous is given as soon as symptoms appear. • Antihistamines treat angioedema and urticaria. • Oxygen. • Treat bronchospasm. • IV fluids.
 Type II: Cytotoxic Reactions • The body makes special autoantibodies directed against self cells that have some form of foreign protein attached to them. • Clinical examples include hemolytic anemias, thrombocytopenic purpura, hemolytic transfusion reactions, Goodpasture’s syndrome, and drug-induced hemolytic anemia.
Type II: Cytotoxic Reactions • The body makes special autoantibodies directed against self cells that have some form of foreign protein attached to them. • Clinical examples include hemolytic anemias, thrombocytopenic purpura, hemolytic transfusion reactions, Goodpasture’s syndrome, and drug-induced hemolytic anemia.
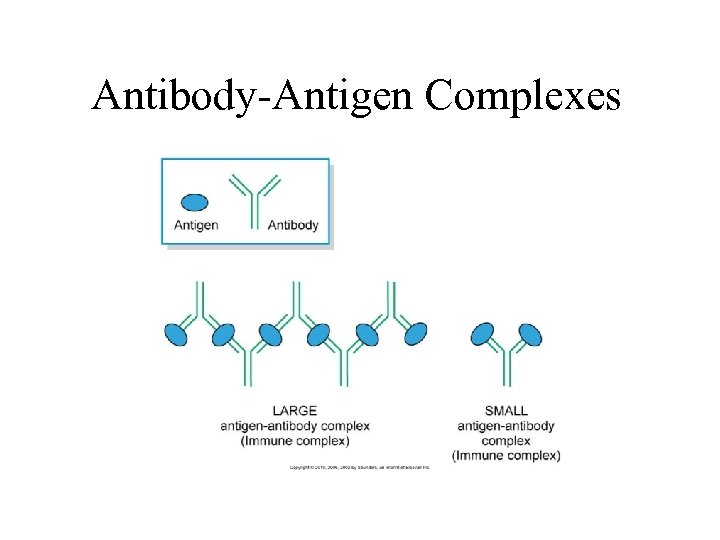 Antibody-Antigen Complexes
Antibody-Antigen Complexes
 Type III: Immune Complex Reactions • Excess antigens cause immune complexes to form in the blood. These circulating complexes usually lodge in small blood vessels. • Usual sites include the kidneys, skin, joints, and small blood vessels.
Type III: Immune Complex Reactions • Excess antigens cause immune complexes to form in the blood. These circulating complexes usually lodge in small blood vessels. • Usual sites include the kidneys, skin, joints, and small blood vessels.
 Type III: Immune Complex Reactions (Cont’d) • Deposited complexes trigger inflammation, resulting in tissue or vessel damage. • Rheumatoid arthritis, systemic lupus erythematosus, and serum sickness occur.
Type III: Immune Complex Reactions (Cont’d) • Deposited complexes trigger inflammation, resulting in tissue or vessel damage. • Rheumatoid arthritis, systemic lupus erythematosus, and serum sickness occur.
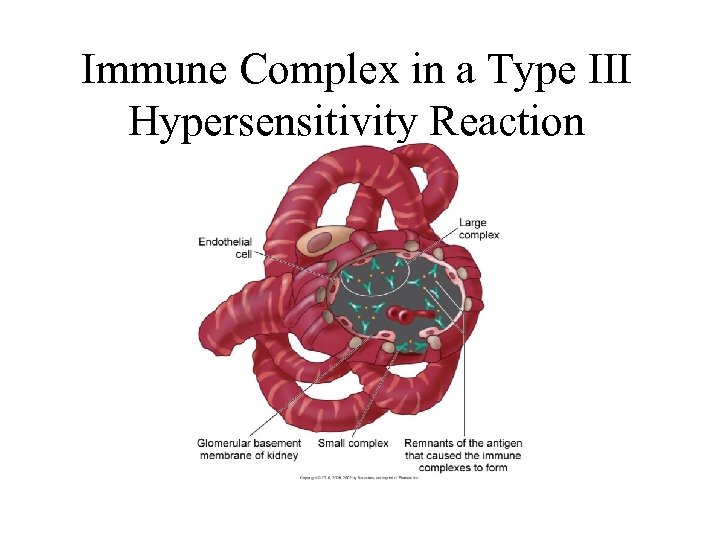 Immune Complex in a Type III Hypersensitivity Reaction
Immune Complex in a Type III Hypersensitivity Reaction
 Type IV: Delayed Hypersensitivity Reactions • In a type IV reaction, the reactive cell is the T-lymphocyte (T-cell). • Antibodies and complement are not involved. • Local collection of lymphocytes and macrophages causes edema, induration, ischemia, and tissue damage at the site.
Type IV: Delayed Hypersensitivity Reactions • In a type IV reaction, the reactive cell is the T-lymphocyte (T-cell). • Antibodies and complement are not involved. • Local collection of lymphocytes and macrophages causes edema, induration, ischemia, and tissue damage at the site.
 Type IV: Delayed Hypersensitivity Reactions (Cont’d) • Other examples include positive purified protein derivative, contact dermatitis, poison ivy skin rashes, insect stings, tissue transplant rejection, and sarcoidosis.
Type IV: Delayed Hypersensitivity Reactions (Cont’d) • Other examples include positive purified protein derivative, contact dermatitis, poison ivy skin rashes, insect stings, tissue transplant rejection, and sarcoidosis.
 Type V: Stimulatory Reaction • Excess stimulation of a normal cell surface receptor by an autoantibody, resulting in a continuous “turned-on” state for the cell. • Graves’ disease.
Type V: Stimulatory Reaction • Excess stimulation of a normal cell surface receptor by an autoantibody, resulting in a continuous “turned-on” state for the cell. • Graves’ disease.
 Autoimmunity • Autoimmunity is the process whereby a person develops an inappropriate immune response. • Antibodies and/or lymphocytes are directed against healthy normal cells and tissues. • For unknown reasons, the immune system fails to recognize certain body cells or tissues as self and triggers immune reactions.
Autoimmunity • Autoimmunity is the process whereby a person develops an inappropriate immune response. • Antibodies and/or lymphocytes are directed against healthy normal cells and tissues. • For unknown reasons, the immune system fails to recognize certain body cells or tissues as self and triggers immune reactions.
 Sjögren’s Syndrome • Group of problems that often appear with other autoimmune disorders • Dry eyes, dry mucous membranes of the nose and mouth (xerostomia), and vaginal dryness • Insufficient tears causing inflammation and ulceration of the cornea • No cure; intensity and progression can be slowed by suppressing immune and inflammatory responses
Sjögren’s Syndrome • Group of problems that often appear with other autoimmune disorders • Dry eyes, dry mucous membranes of the nose and mouth (xerostomia), and vaginal dryness • Insufficient tears causing inflammation and ulceration of the cornea • No cure; intensity and progression can be slowed by suppressing immune and inflammatory responses
 Goodpasture’s Syndrome • Autoimmune disorder in which autoantibodies are made against the glomerular basement membrane and neutrophils • Lungs and kidneys • Shortness of breath, hemoptysis, decreased urine output, weight gain, edema, hypertension, and tachycardia • Treatment—high-dose corticosteroids
Goodpasture’s Syndrome • Autoimmune disorder in which autoantibodies are made against the glomerular basement membrane and neutrophils • Lungs and kidneys • Shortness of breath, hemoptysis, decreased urine output, weight gain, edema, hypertension, and tachycardia • Treatment—high-dose corticosteroids


