3c3c3eac2e8e8cec0bf52b59e6c2dbf1.ppt
- Количество слайдов: 70
 Chapter 18 *Lecture Outline *See separate Flex. Art Power. Point slides for all figures and tables pre-inserted into Power. Point without notes. Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display.
Chapter 18 *Lecture Outline *See separate Flex. Art Power. Point slides for all figures and tables pre-inserted into Power. Point without notes. Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display.
 Chapter 18 Outline • Comparison of the Somatic and Autonomic Nervous Systems • Overview of the Autonomic Nervous System • Parasympathetic Division • Sympathetic Division • Other Features of the Autonomic Nervous System • CNS Control of Autonomic Function • Development of the Autonomic Nervous System
Chapter 18 Outline • Comparison of the Somatic and Autonomic Nervous Systems • Overview of the Autonomic Nervous System • Parasympathetic Division • Sympathetic Division • Other Features of the Autonomic Nervous System • CNS Control of Autonomic Function • Development of the Autonomic Nervous System
 Autonomic Nervous System • The autonomic nervous system (ANS) is a complex system of nerves that govern involuntary actions. • The ANS works constantly with the somatic nervous system (SNS) to regulate body organs and maintain normal internal functions.
Autonomic Nervous System • The autonomic nervous system (ANS) is a complex system of nerves that govern involuntary actions. • The ANS works constantly with the somatic nervous system (SNS) to regulate body organs and maintain normal internal functions.
 Autonomic Nervous System • The ANS and SNS are part of both the central nervous system and the peripheral nervous system. • The SNS operates under our conscious control. The ANS functions are involuntary and we are usually unaware of them.
Autonomic Nervous System • The ANS and SNS are part of both the central nervous system and the peripheral nervous system. • The SNS operates under our conscious control. The ANS functions are involuntary and we are usually unaware of them.
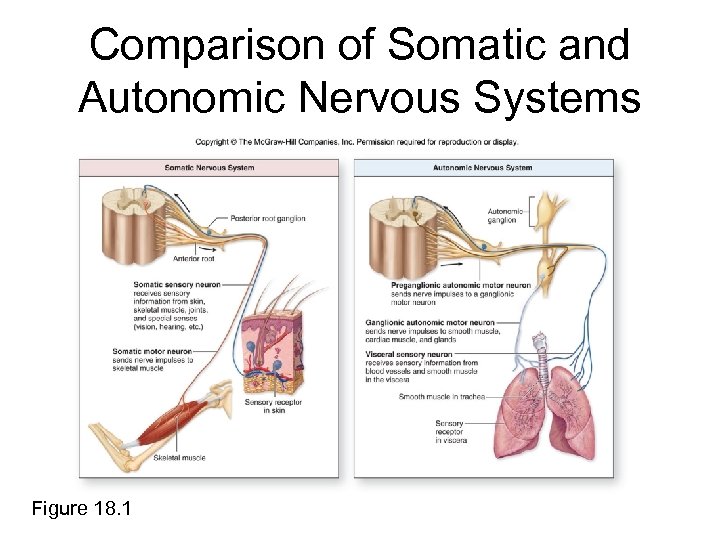 Comparison of Somatic and Autonomic Nervous Systems Figure 18. 1
Comparison of Somatic and Autonomic Nervous Systems Figure 18. 1
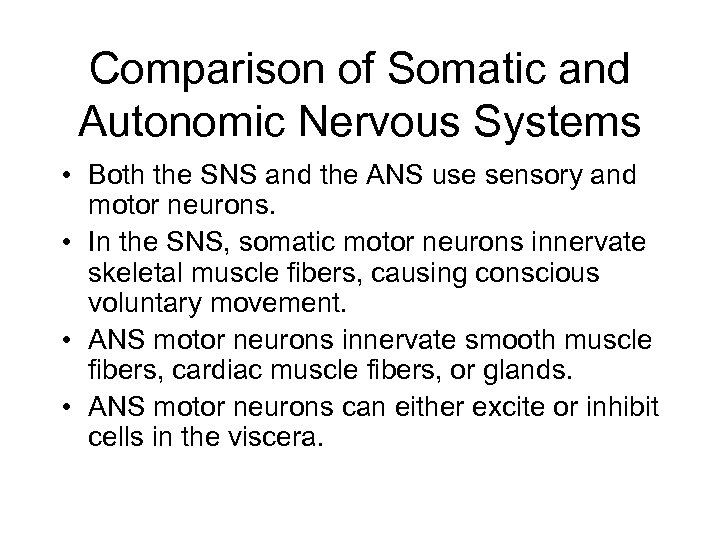 Comparison of Somatic and Autonomic Nervous Systems • Both the SNS and the ANS use sensory and motor neurons. • In the SNS, somatic motor neurons innervate skeletal muscle fibers, causing conscious voluntary movement. • ANS motor neurons innervate smooth muscle fibers, cardiac muscle fibers, or glands. • ANS motor neurons can either excite or inhibit cells in the viscera.
Comparison of Somatic and Autonomic Nervous Systems • Both the SNS and the ANS use sensory and motor neurons. • In the SNS, somatic motor neurons innervate skeletal muscle fibers, causing conscious voluntary movement. • ANS motor neurons innervate smooth muscle fibers, cardiac muscle fibers, or glands. • ANS motor neurons can either excite or inhibit cells in the viscera.
 Comparison of Somatic and Autonomic Nervous Systems • SNS—single lower motor neuron axon extends uninterrupted from the spinal cord to one or more muscle fibers • ANS—two-neuron chain innervates muscles and glands
Comparison of Somatic and Autonomic Nervous Systems • SNS—single lower motor neuron axon extends uninterrupted from the spinal cord to one or more muscle fibers • ANS—two-neuron chain innervates muscles and glands
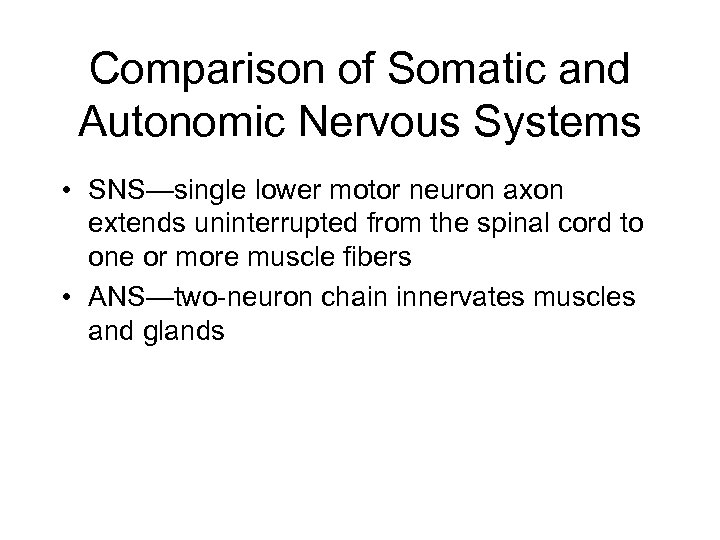
 Components of the Autonomic Nervous System Figure 18. 2
Components of the Autonomic Nervous System Figure 18. 2
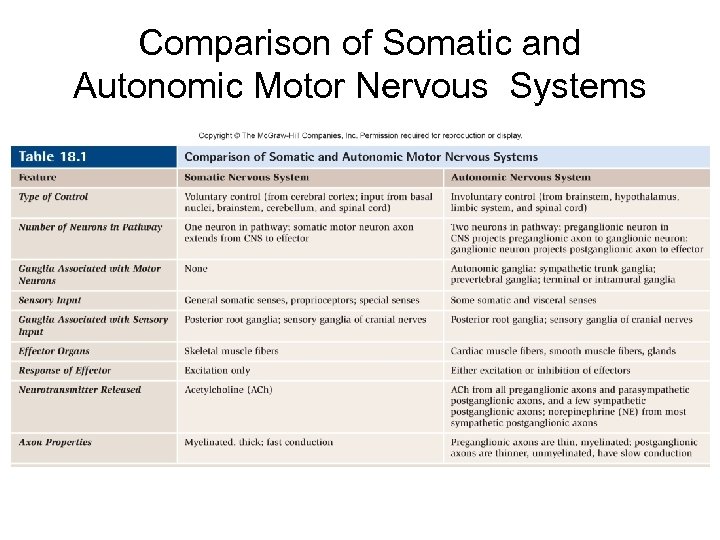 Comparison of Somatic and Autonomic Motor Nervous Systems
Comparison of Somatic and Autonomic Motor Nervous Systems
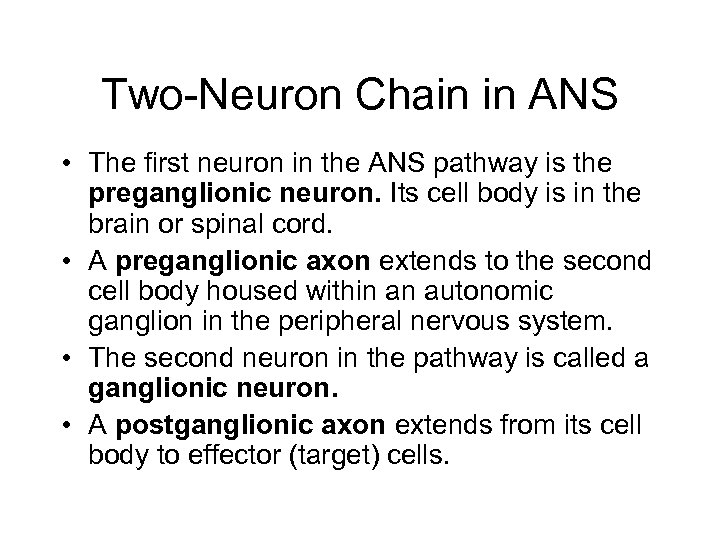 Two-Neuron Chain in ANS • The first neuron in the ANS pathway is the preganglionic neuron. Its cell body is in the brain or spinal cord. • A preganglionic axon extends to the second cell body housed within an autonomic ganglion in the peripheral nervous system. • The second neuron in the pathway is called a ganglionic neuron. • A postganglionic axon extends from its cell body to effector (target) cells.
Two-Neuron Chain in ANS • The first neuron in the ANS pathway is the preganglionic neuron. Its cell body is in the brain or spinal cord. • A preganglionic axon extends to the second cell body housed within an autonomic ganglion in the peripheral nervous system. • The second neuron in the pathway is called a ganglionic neuron. • A postganglionic axon extends from its cell body to effector (target) cells.
 Two-Neuron Chain in ANS • Neuronal convergence—axons from numerous preganglionic cells synapse on a single ganglionic cell • Neuronal divergence—axons from one preganglionic cell synapse on numerous ganglionic cells
Two-Neuron Chain in ANS • Neuronal convergence—axons from numerous preganglionic cells synapse on a single ganglionic cell • Neuronal divergence—axons from one preganglionic cell synapse on numerous ganglionic cells
 Divisions of Autonomic Nervous System • Parasympathetic division—conservation of energy and replenishment of nutrient stores (“rest-and-digest”) • Sympathetic division—preparation of body for emergencies (“fight-or-flight”); increased activity of this division results in increased alertness and metabolic activity
Divisions of Autonomic Nervous System • Parasympathetic division—conservation of energy and replenishment of nutrient stores (“rest-and-digest”) • Sympathetic division—preparation of body for emergencies (“fight-or-flight”); increased activity of this division results in increased alertness and metabolic activity
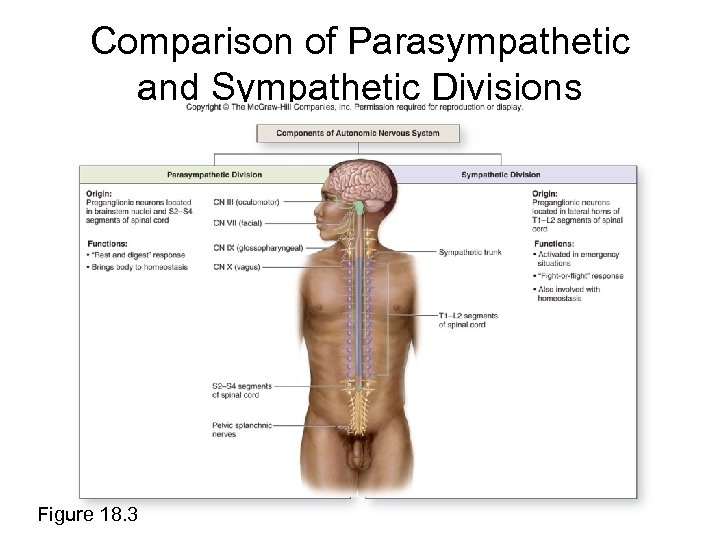 Comparison of Parasympathetic and Sympathetic Divisions Figure 18. 3
Comparison of Parasympathetic and Sympathetic Divisions Figure 18. 3
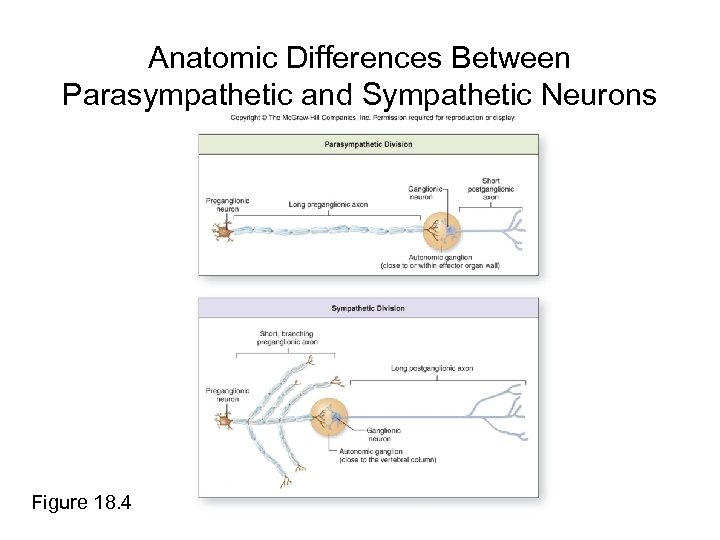 Anatomic Differences Between Parasympathetic and Sympathetic Neurons Figure 18. 4
Anatomic Differences Between Parasympathetic and Sympathetic Neurons Figure 18. 4
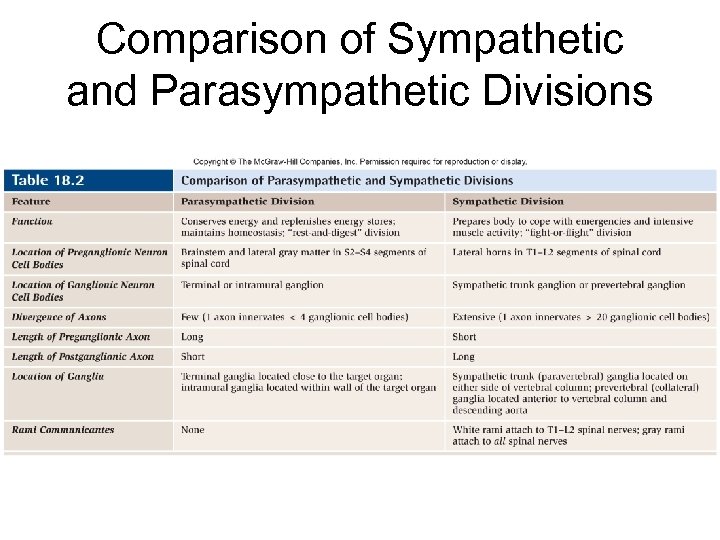 Comparison of Sympathetic and Parasympathetic Divisions
Comparison of Sympathetic and Parasympathetic Divisions
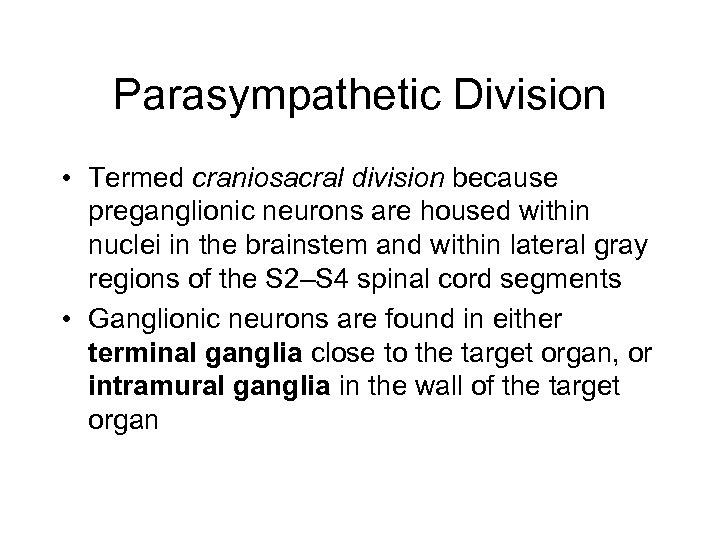 Parasympathetic Division • Termed craniosacral division because preganglionic neurons are housed within nuclei in the brainstem and within lateral gray regions of the S 2–S 4 spinal cord segments • Ganglionic neurons are found in either terminal ganglia close to the target organ, or intramural ganglia in the wall of the target organ
Parasympathetic Division • Termed craniosacral division because preganglionic neurons are housed within nuclei in the brainstem and within lateral gray regions of the S 2–S 4 spinal cord segments • Ganglionic neurons are found in either terminal ganglia close to the target organ, or intramural ganglia in the wall of the target organ
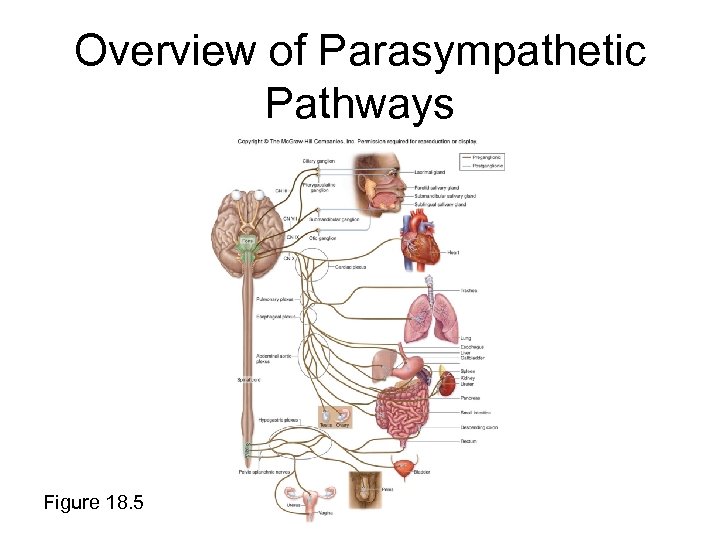 Overview of Parasympathetic Pathways Figure 18. 5
Overview of Parasympathetic Pathways Figure 18. 5
 Four Cranial Nerves of Parasympathetic Division 1. 2. 3. 4. Oculomotor (CN III) Facial (CN VII) Glossopharyngeal (CN IX) Vagus (CN X)
Four Cranial Nerves of Parasympathetic Division 1. 2. 3. 4. Oculomotor (CN III) Facial (CN VII) Glossopharyngeal (CN IX) Vagus (CN X)
 Oculomotor Nerve (CN III) • Preganglionic cell bodies housed in nuclei in mesencephalon • Postganglionic cell bodies located in ciliary ganglion within the orbit • Postganglionic axons project to the ciliary muscle and to the pupillary constrictor muscle of iris
Oculomotor Nerve (CN III) • Preganglionic cell bodies housed in nuclei in mesencephalon • Postganglionic cell bodies located in ciliary ganglion within the orbit • Postganglionic axons project to the ciliary muscle and to the pupillary constrictor muscle of iris
 Facial Nerve (VII) Two branches of preganglionic axons in the facial nerve (VII) exit the pons: 1. greater petrosal nerve 2. chorda tympani
Facial Nerve (VII) Two branches of preganglionic axons in the facial nerve (VII) exit the pons: 1. greater petrosal nerve 2. chorda tympani
 Facial Nerve (VII) Greater petrosal nerve: • terminates at the pterygopalatine ganglion • postganglionic axons project to lacrimal glands and small glands of nasal cavity, oral cavity, and palate
Facial Nerve (VII) Greater petrosal nerve: • terminates at the pterygopalatine ganglion • postganglionic axons project to lacrimal glands and small glands of nasal cavity, oral cavity, and palate
 Facial Nerve (VII) Chorda tympani: • terminates at the submandibular ganglion – postganglionic axons project to submandibular and sublingual salivary glands in the floor of the mouth
Facial Nerve (VII) Chorda tympani: • terminates at the submandibular ganglion – postganglionic axons project to submandibular and sublingual salivary glands in the floor of the mouth
 Glossopharyngeal Nerve (CN IX) • Preganglionic axons exit brainstem • Preganglionic axons branch and synapse on ganglionic neurons in the otic ganglion • Postganglionic axons cause increase in secretion from parotid salivary glands
Glossopharyngeal Nerve (CN IX) • Preganglionic axons exit brainstem • Preganglionic axons branch and synapse on ganglionic neurons in the otic ganglion • Postganglionic axons cause increase in secretion from parotid salivary glands
 Vagus Nerve (CN X) • Projects inferiorly through neck to supply innervation to thoracic organs and most abdominal organs • Multiple branches extend to thoracic organs to increase mucous production and decrease diameter of airways, and to decrease heart rate and force of heart contraction
Vagus Nerve (CN X) • Projects inferiorly through neck to supply innervation to thoracic organs and most abdominal organs • Multiple branches extend to thoracic organs to increase mucous production and decrease diameter of airways, and to decrease heart rate and force of heart contraction
 Vagus Nerve (CN X) • Vagal trunks pass through diaphragm, associate with the abdominal aorta, and project branches to ganglia located adjacent to or within wall of target organs • Increases smooth muscle motility and secretory activity in digestive tract organs
Vagus Nerve (CN X) • Vagal trunks pass through diaphragm, associate with the abdominal aorta, and project branches to ganglia located adjacent to or within wall of target organs • Increases smooth muscle motility and secretory activity in digestive tract organs
 Spinal Sacral Nerves • Preganglionic neuron cell bodies are housed within lateral gray regions of S 2–S 4 spinal cord segments. • Preganglionic axons branch to form pelvic splanchnic nerves, which contribute to the superior and inferior hypogastric plexus. • Preganglionic fibers project to ganglionic neurons within terminal or intramural ganglia of large intestine, rectum, reproductive organs, urinary bladder, and distal ureter.
Spinal Sacral Nerves • Preganglionic neuron cell bodies are housed within lateral gray regions of S 2–S 4 spinal cord segments. • Preganglionic axons branch to form pelvic splanchnic nerves, which contribute to the superior and inferior hypogastric plexus. • Preganglionic fibers project to ganglionic neurons within terminal or intramural ganglia of large intestine, rectum, reproductive organs, urinary bladder, and distal ureter.
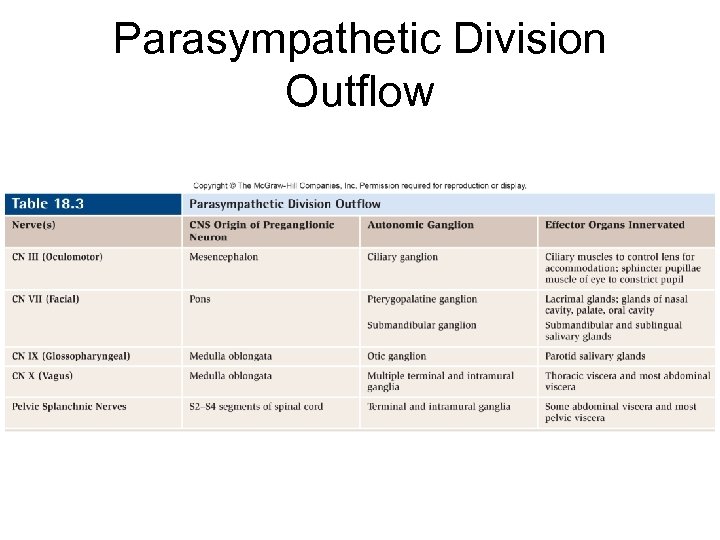 Parasympathetic Division Outflow
Parasympathetic Division Outflow
 Sympathetic Division • Also termed thoracolumbar division because preganglionic neuron cell bodies are housed in lateral horn between first thoracic (T 1) and second lumbar (L 2) spinal segments • Preganglionic axons travel with somatic motor neuron axons to exit the spinal cord and enter the anterior roots and then the T 1–L 2 spinal nerves
Sympathetic Division • Also termed thoracolumbar division because preganglionic neuron cell bodies are housed in lateral horn between first thoracic (T 1) and second lumbar (L 2) spinal segments • Preganglionic axons travel with somatic motor neuron axons to exit the spinal cord and enter the anterior roots and then the T 1–L 2 spinal nerves
 Right and Left Sympathetic Trunks • Sympathetic trunks are located anterior to spinal nerves and immediately lateral to vertebral column. • Sympathetic trunk ganglia (paravertebral or chain ganglia) house sympathetic ganglionic neuron cell bodies. One sympathetic ganglion is approximately associated with each spinal nerve. • Cervical portion of each sympathetic trunk is partitioned into three ganglia: the superior, middle, and inferior ganglia.
Right and Left Sympathetic Trunks • Sympathetic trunks are located anterior to spinal nerves and immediately lateral to vertebral column. • Sympathetic trunk ganglia (paravertebral or chain ganglia) house sympathetic ganglionic neuron cell bodies. One sympathetic ganglion is approximately associated with each spinal nerve. • Cervical portion of each sympathetic trunk is partitioned into three ganglia: the superior, middle, and inferior ganglia.
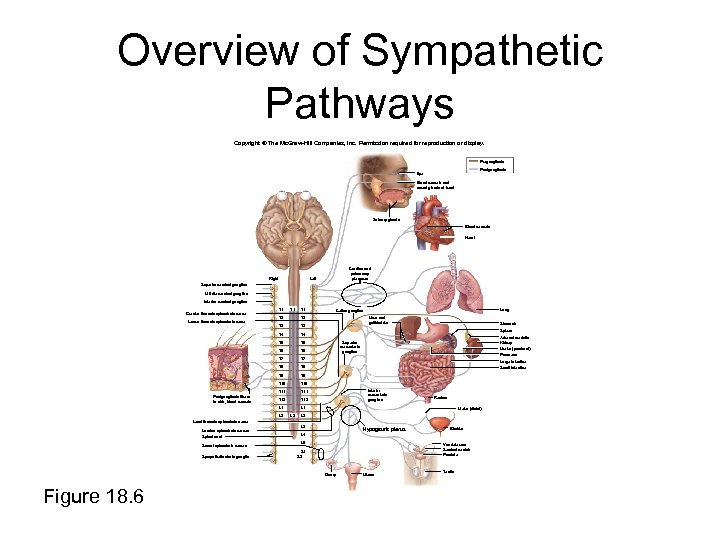 Overview of Sympathetic Pathways Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display. Preganglionic Postganglionic Eye Blood vessels and sweat glands of head Salivary glands Blood vessels Heart Right Cardiac and pulmonary plexuses Left Superior cervical ganglion Middle cervical ganglion Inferior cervical ganglion T 1 Greater thoracic splanchnic nerve T 1 T 3 T 4 T 5 T 6 T 7 T 8 T 9 T 10 T 11 T 12 L 1 Lung Celiac ganglion T 2 T 4 Postganglionic fibers to skin, blood vessels T 2 T 3 Lesser thoracic splanchnic nerve L 1 L 2 Liver and gallbladder Stomach Spleen Adrenal medulla Kidney Superior mesenteric ganglion Ureter (proximal) Pancreas Large intestine Small intestine Inferior mesenteric ganglion Rectum Ureter (distal) L 2 Least thoracic splanchnic nerve Lumbar splanchnic nerves Spinal cord Sacral splanchnic nerves Sympathetic chain ganglia L 3 Hypogastric plexus L 5 Vas deferens Seminal vesicle Prostate S 1 S 2 Ovary Figure 18. 6 Bladder L 4 Uterus Testis
Overview of Sympathetic Pathways Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display. Preganglionic Postganglionic Eye Blood vessels and sweat glands of head Salivary glands Blood vessels Heart Right Cardiac and pulmonary plexuses Left Superior cervical ganglion Middle cervical ganglion Inferior cervical ganglion T 1 Greater thoracic splanchnic nerve T 1 T 3 T 4 T 5 T 6 T 7 T 8 T 9 T 10 T 11 T 12 L 1 Lung Celiac ganglion T 2 T 4 Postganglionic fibers to skin, blood vessels T 2 T 3 Lesser thoracic splanchnic nerve L 1 L 2 Liver and gallbladder Stomach Spleen Adrenal medulla Kidney Superior mesenteric ganglion Ureter (proximal) Pancreas Large intestine Small intestine Inferior mesenteric ganglion Rectum Ureter (distal) L 2 Least thoracic splanchnic nerve Lumbar splanchnic nerves Spinal cord Sacral splanchnic nerves Sympathetic chain ganglia L 3 Hypogastric plexus L 5 Vas deferens Seminal vesicle Prostate S 1 S 2 Ovary Figure 18. 6 Bladder L 4 Uterus Testis
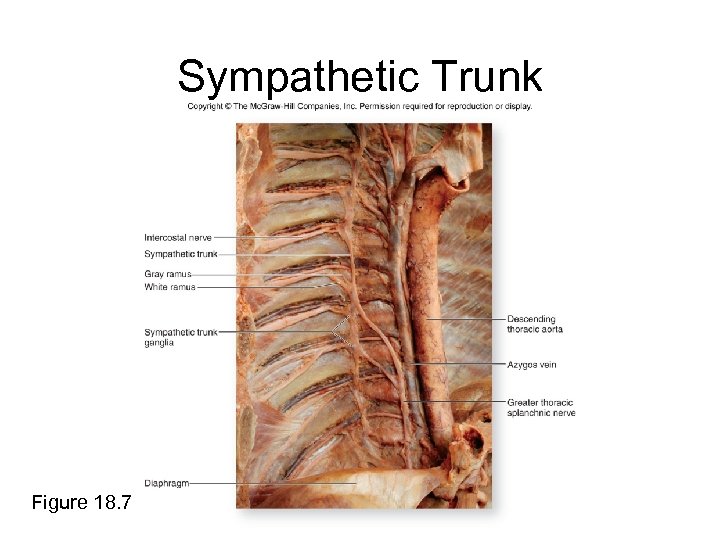 Sympathetic Trunk Figure 18. 7
Sympathetic Trunk Figure 18. 7
 Cervical Sympathetic Ganglia • Postganglionic axons from cell bodies in the superior cervical ganglion distribute to structures in the head and neck. Axons innervate sweat glands, smooth muscle in blood vessels, dilator pupillae muscle of the eye, and the superior tarsal muscle of the eye. • Middle and inferior cervical ganglia house neuron cell bodies that extend postganglionic axons to the thoracic viscera.
Cervical Sympathetic Ganglia • Postganglionic axons from cell bodies in the superior cervical ganglion distribute to structures in the head and neck. Axons innervate sweat glands, smooth muscle in blood vessels, dilator pupillae muscle of the eye, and the superior tarsal muscle of the eye. • Middle and inferior cervical ganglia house neuron cell bodies that extend postganglionic axons to the thoracic viscera.
 Rami Communicantes • Connect sympathetic trunk to each spinal nerve • Preganglionic sympathetic axons of T 1– L 2 spinal nerves are carried by white rami communicantes (or white rami)
Rami Communicantes • Connect sympathetic trunk to each spinal nerve • Preganglionic sympathetic axons of T 1– L 2 spinal nerves are carried by white rami communicantes (or white rami)
 Rami Communicantes • Postganglionic sympathetic axons are carried from the sympathetic trunk to the spinal nerve by gray rami communicantes (or gray rami). Gray rami connect to all spinal nerves including cervical, sacral, and coccygeal spinal nerves. • Preganglionic axons of white rami are myelinated and postganglionic axons of gray rami are unmyelinated.
Rami Communicantes • Postganglionic sympathetic axons are carried from the sympathetic trunk to the spinal nerve by gray rami communicantes (or gray rami). Gray rami connect to all spinal nerves including cervical, sacral, and coccygeal spinal nerves. • Preganglionic axons of white rami are myelinated and postganglionic axons of gray rami are unmyelinated.
 Splanchnic Nerves • Composed of preganglionic sympathetic axons that did not synapse in a sympathetic trunk ganglion • Run anteriorly from sympathetic trunk to most of viscera
Splanchnic Nerves • Composed of preganglionic sympathetic axons that did not synapse in a sympathetic trunk ganglion • Run anteriorly from sympathetic trunk to most of viscera
 Splanchnic Nerves • Larger nerves are preganglionic axons that extend from sympathetic trunk ganglia: – – – Greater thoracic splanchnic nerves: T 5–T 9 Lesser thoracic splanchnic nerves: T 10–T 11 Least thoracic splanchnic nerves: T 12 Lumbar splanchnic nerves: L 1 and L 2 Sacral splanchnic nerves: sacral sympathetic ganglia
Splanchnic Nerves • Larger nerves are preganglionic axons that extend from sympathetic trunk ganglia: – – – Greater thoracic splanchnic nerves: T 5–T 9 Lesser thoracic splanchnic nerves: T 10–T 11 Least thoracic splanchnic nerves: T 12 Lumbar splanchnic nerves: L 1 and L 2 Sacral splanchnic nerves: sacral sympathetic ganglia
 Prevertebral (Collateral) Ganglia • Splanchnic nerves typically terminate in prevertebral ganglia. • Ganglia are unpaired and immediately anterior to the vertebral column on the anterolateral surface of the aorta in the abdominopelvic cavity.
Prevertebral (Collateral) Ganglia • Splanchnic nerves typically terminate in prevertebral ganglia. • Ganglia are unpaired and immediately anterior to the vertebral column on the anterolateral surface of the aorta in the abdominopelvic cavity.
 Prevertebral (Collateral) Ganglia • Ganglia typically cluster around the major abdominal arteries and are named for the arteries. • Sympathetic postganglionic axons extend away from the ganglionic neuron cell bodies in the ganglia and innervate many of the abdominal organs.
Prevertebral (Collateral) Ganglia • Ganglia typically cluster around the major abdominal arteries and are named for the arteries. • Sympathetic postganglionic axons extend away from the ganglionic neuron cell bodies in the ganglia and innervate many of the abdominal organs.
 Prevertebral Ganglia Prevertebral ganglia include: • Celiac ganglion • Superior mesenteric ganglion • Inferior mesenteric ganglion
Prevertebral Ganglia Prevertebral ganglia include: • Celiac ganglion • Superior mesenteric ganglion • Inferior mesenteric ganglion
 Celiac Ganglion • Location—adjacent to origin of celiac artery • Preganglion axons—greater thoracic splanchnic nerves (T 5–T 9 segment of spinal cord) • Postganglionic axons—innervate stomach, spleen, liver, gallbladder, proximal duodenum, part of pancreas
Celiac Ganglion • Location—adjacent to origin of celiac artery • Preganglion axons—greater thoracic splanchnic nerves (T 5–T 9 segment of spinal cord) • Postganglionic axons—innervate stomach, spleen, liver, gallbladder, proximal duodenum, part of pancreas
 Superior Mesenteric Ganglion • Location—adjacent to origin of superior mesenteric artery • Preganglionic axons—lesser and least thoracic splanchnic nerves (T 10–T 12 segment of spinal cord) • Postganglionic axons—innervate distal duodenum, part of pancreas, remainder of small intestine, proximal large intestine, kidneys, proximal part of ureters
Superior Mesenteric Ganglion • Location—adjacent to origin of superior mesenteric artery • Preganglionic axons—lesser and least thoracic splanchnic nerves (T 10–T 12 segment of spinal cord) • Postganglionic axons—innervate distal duodenum, part of pancreas, remainder of small intestine, proximal large intestine, kidneys, proximal part of ureters
 Inferior Mesenteric Ganglion • Location—adjacent to the origin of the inferior mesenteric artery • Preganglionic axons—lumbar splanchnic nerves (L 1–L 2 segment of spinal cord) • Postganglionic axons—innervate the distal colon, rectum, urinary bladder, distal ureter, and most of reproductive organs
Inferior Mesenteric Ganglion • Location—adjacent to the origin of the inferior mesenteric artery • Preganglionic axons—lumbar splanchnic nerves (L 1–L 2 segment of spinal cord) • Postganglionic axons—innervate the distal colon, rectum, urinary bladder, distal ureter, and most of reproductive organs
 Sympathetic Pathways • All preganglionic neurons originate in lateral gray horns of T 1–L 2 regions of the spinal cord. • Preganglionic axons travel with T 1–L 2 spinal nerves. • Preganglionic axons immediately leave spinal nerve and travel through white rami to enter sympathetic trunk.
Sympathetic Pathways • All preganglionic neurons originate in lateral gray horns of T 1–L 2 regions of the spinal cord. • Preganglionic axons travel with T 1–L 2 spinal nerves. • Preganglionic axons immediately leave spinal nerve and travel through white rami to enter sympathetic trunk.
 Sympathetic Pathways • Once inside the sympathetic trunk preganglionic axons may remain at the level of entry or travel superiorly or inferiorly within the sympathetic trunk. • Axons exit sympathetic trunk ganglia by: – – spinal nerve pathway postganglionic sympathetic nerve pathway splanchnic nerve pathway adrenal medulla pathway
Sympathetic Pathways • Once inside the sympathetic trunk preganglionic axons may remain at the level of entry or travel superiorly or inferiorly within the sympathetic trunk. • Axons exit sympathetic trunk ganglia by: – – spinal nerve pathway postganglionic sympathetic nerve pathway splanchnic nerve pathway adrenal medulla pathway
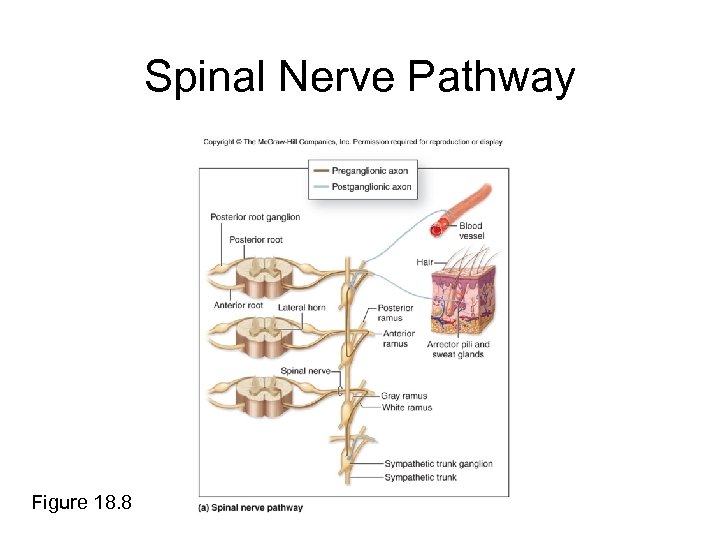 Spinal Nerve Pathway Figure 18. 8
Spinal Nerve Pathway Figure 18. 8
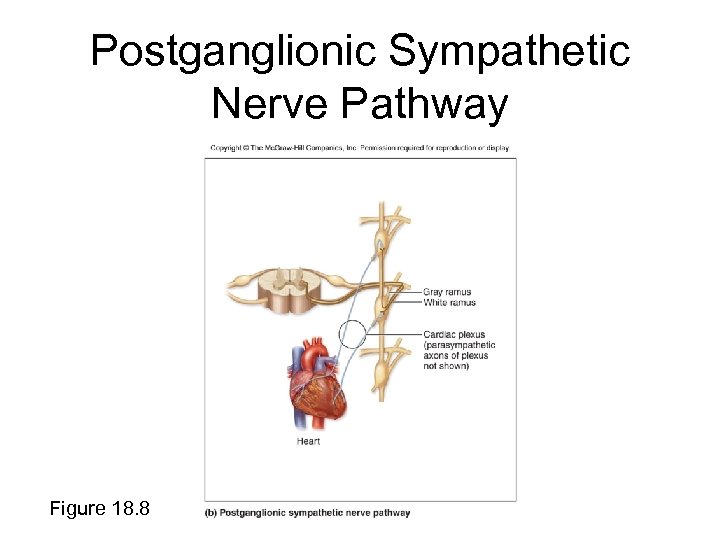 Postganglionic Sympathetic Nerve Pathway Figure 18. 8
Postganglionic Sympathetic Nerve Pathway Figure 18. 8
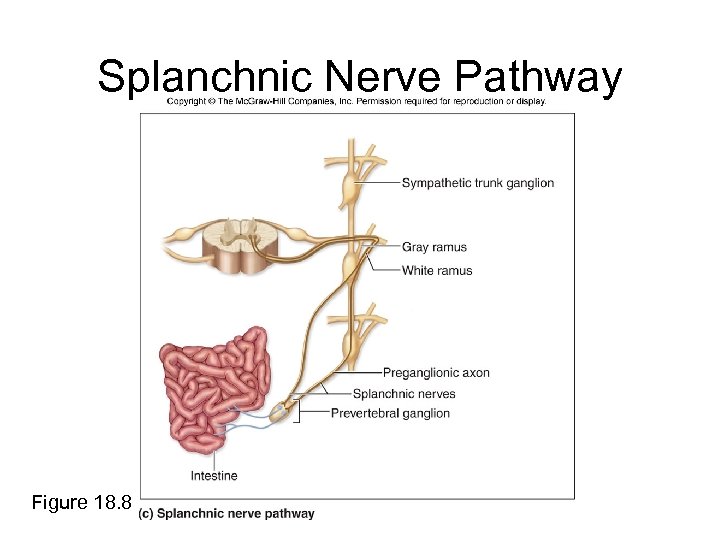 Splanchnic Nerve Pathway Figure 18. 8
Splanchnic Nerve Pathway Figure 18. 8
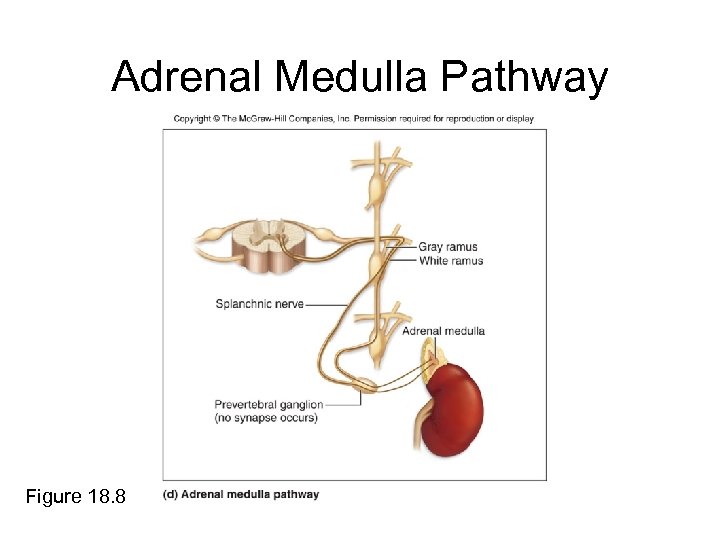 Adrenal Medulla Pathway Figure 18. 8
Adrenal Medulla Pathway Figure 18. 8
 Adrenal Medulla Pathway • Adrenal medulla—the internal region of adrenal gland that releases hormones within the bloodstream to help promote fight-or-flight response – The hormones are epinephrine and, to a lesser degree, norepinephrine
Adrenal Medulla Pathway • Adrenal medulla—the internal region of adrenal gland that releases hormones within the bloodstream to help promote fight-or-flight response – The hormones are epinephrine and, to a lesser degree, norepinephrine
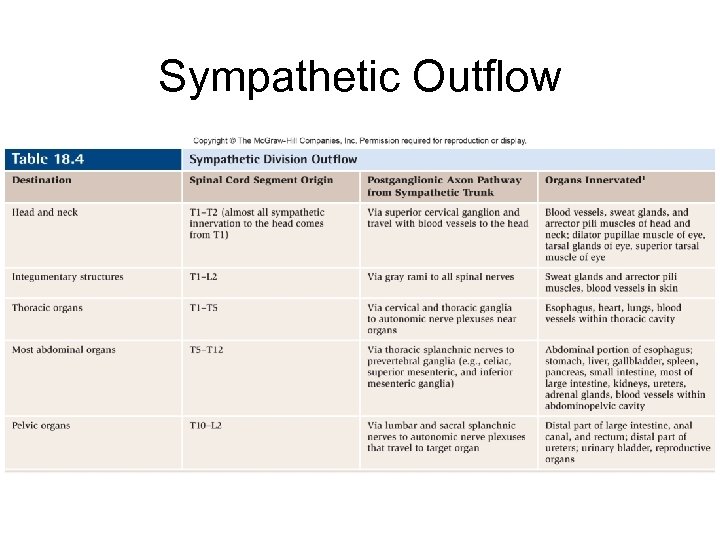 Sympathetic Outflow
Sympathetic Outflow
 Autonomic Plexuses • Collections of sympathetic postganglionic axons, parasympathetic preganglionic axons, and visceral sensory axons • Sympathetic and parasympathetic axons are close to one another
Autonomic Plexuses • Collections of sympathetic postganglionic axons, parasympathetic preganglionic axons, and visceral sensory axons • Sympathetic and parasympathetic axons are close to one another
 Autonomic Plexuses • • Cardiac plexus Pulmonary plexus Esophageal plexus Abdominal aortic plexus consists of celiac plexus, superior mesenteric plexus, inferior mesenteric plexus, • Hypogastric plexus
Autonomic Plexuses • • Cardiac plexus Pulmonary plexus Esophageal plexus Abdominal aortic plexus consists of celiac plexus, superior mesenteric plexus, inferior mesenteric plexus, • Hypogastric plexus
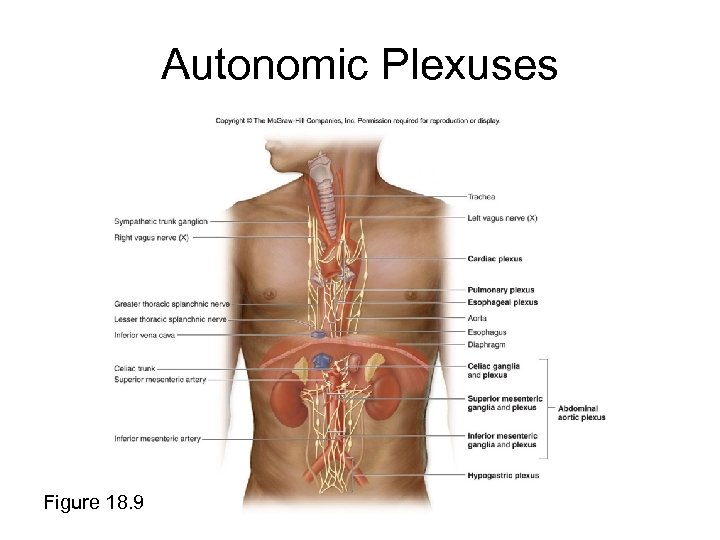 Autonomic Plexuses Figure 18. 9
Autonomic Plexuses Figure 18. 9
 Cardiac Plexus • In mediastinum of thoracic cavity • Consists of postganglionic sympathetic axons from thoracic sympathetic trunk ganglia and preganglionic axons of vagus nerve • Increased sympathetic activity increases heart rate and blood pressure • Increased parasympathetic activity decreases heart rate
Cardiac Plexus • In mediastinum of thoracic cavity • Consists of postganglionic sympathetic axons from thoracic sympathetic trunk ganglia and preganglionic axons of vagus nerve • Increased sympathetic activity increases heart rate and blood pressure • Increased parasympathetic activity decreases heart rate
 Pulmonary Plexus • Consists of postganglionic sympathetic axons from thoracic sympathetic trunk ganglia and preganglionic axons from the vagus nerve • Axons project to bronchi and blood vessels of the lungs • Parasympathetic stimulation reduces bronchial diameter (bronchoconstriction) and increases mucous gland secretion in bronchial tree • Sympathetic innervation causes bronchodilation (increase bronchial diameter)
Pulmonary Plexus • Consists of postganglionic sympathetic axons from thoracic sympathetic trunk ganglia and preganglionic axons from the vagus nerve • Axons project to bronchi and blood vessels of the lungs • Parasympathetic stimulation reduces bronchial diameter (bronchoconstriction) and increases mucous gland secretion in bronchial tree • Sympathetic innervation causes bronchodilation (increase bronchial diameter)
 Esophageal Plexus • Consists of preganglionic axons from the vagus nerve • Parasympathetic activity coordinates smooth muscle activity during swallowing reflex in inferior wall and cardiac sphincter in inferior esophagus
Esophageal Plexus • Consists of preganglionic axons from the vagus nerve • Parasympathetic activity coordinates smooth muscle activity during swallowing reflex in inferior wall and cardiac sphincter in inferior esophagus
 Abdominal Aortic Plexus • Consists of celiac plexus, superior mesenteric plexus, and inferior mesenteric plexus • Composed of postganglionic axons projecting from the prevertebral ganglia and preganglionic axons from the vagus nerve
Abdominal Aortic Plexus • Consists of celiac plexus, superior mesenteric plexus, and inferior mesenteric plexus • Composed of postganglionic axons projecting from the prevertebral ganglia and preganglionic axons from the vagus nerve
 Hypogastric Plexus • Complex meshwork of postganglionic sympathetic axons (from the aortic plexus and the lumbar region of the sympathetic trunk) and preganglionic parasympathetic axons from the pelvic splanchnic nerve • Axons innervate viscera within the pelvic region
Hypogastric Plexus • Complex meshwork of postganglionic sympathetic axons (from the aortic plexus and the lumbar region of the sympathetic trunk) and preganglionic parasympathetic axons from the pelvic splanchnic nerve • Axons innervate viscera within the pelvic region
 Neurotransmitters and Receptors • All preganglionic axons release acetylcholine (ACh), which has an excitatory effect on the ganglionic cell. • All postganglionic parasympathetic axons and a few postganglionic sympathetic axons release ACh on the effector. • Depending on the receptor, ACh from parasympathetic axons may have either an inhibitory or excitatory effect on the effector.
Neurotransmitters and Receptors • All preganglionic axons release acetylcholine (ACh), which has an excitatory effect on the ganglionic cell. • All postganglionic parasympathetic axons and a few postganglionic sympathetic axons release ACh on the effector. • Depending on the receptor, ACh from parasympathetic axons may have either an inhibitory or excitatory effect on the effector.
 Neurotransmitters and Receptors • Ach released from sympathetic axons is excitatory only. • Most postganglionic sympathetic axons release norepinephrine on the effector. • Depending on the receptor, the effects of norepinephrine has an inhibitory or an excitatory effect.
Neurotransmitters and Receptors • Ach released from sympathetic axons is excitatory only. • Most postganglionic sympathetic axons release norepinephrine on the effector. • Depending on the receptor, the effects of norepinephrine has an inhibitory or an excitatory effect.
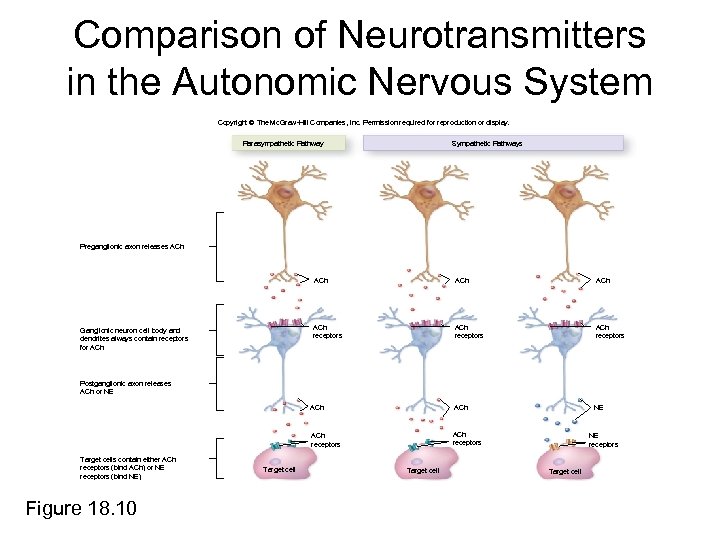 Comparison of Neurotransmitters in the Autonomic Nervous System Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display. Parasympathetic Pathway Sympathetic Pathways Preganglionic axon releases ACh ACh receptors ACh NE ACh receptors Ganglionic neuron cell body and dendrites always contain receptors for ACh ACh receptors Postganglionic axon releases ACh or NE Target cells contain either ACh receptors (bind ACh) or NE receptors (bind NE) Figure 18. 10 Target cell NE receptors Target cell
Comparison of Neurotransmitters in the Autonomic Nervous System Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display. Parasympathetic Pathway Sympathetic Pathways Preganglionic axon releases ACh ACh receptors ACh NE ACh receptors Ganglionic neuron cell body and dendrites always contain receptors for ACh ACh receptors Postganglionic axon releases ACh or NE Target cells contain either ACh receptors (bind ACh) or NE receptors (bind NE) Figure 18. 10 Target cell NE receptors Target cell
 Dual Innervation • Many visceral effectors have dual innervation, meaning innervation by postganglionic axons from both ANS divisions. • The actions of the divisions usually oppose each other (antagonistic effects).
Dual Innervation • Many visceral effectors have dual innervation, meaning innervation by postganglionic axons from both ANS divisions. • The actions of the divisions usually oppose each other (antagonistic effects).
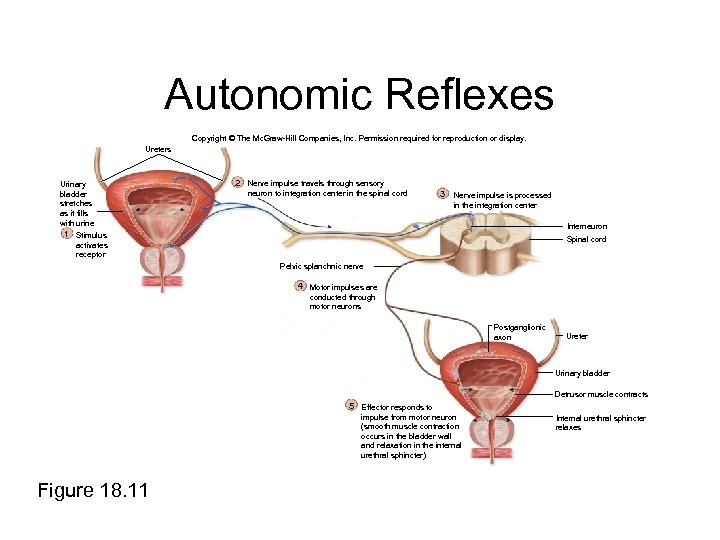 Autonomic Reflexes Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display. Ureters Urinary bladder stretches as it fills with urine 2 Nerve impulse travels through sensory neuron to integration center in the spinal cord 3 Nerve impulse is processed in the integration center Interneuron 1 Stimulus Spinal cord activates receptor Pelvic splanchnic nerve 4 Motor impulses are conducted through motor neurons Postganglionic axon Ureter Urinary bladder Detrusor muscle contracts 5 Effector responds to impulse from motor neuron (smooth muscle contraction occurs in the bladder wall and relaxation in the internal urethral sphincter) Figure 18. 11 Internal urethral sphincter relaxes
Autonomic Reflexes Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display. Ureters Urinary bladder stretches as it fills with urine 2 Nerve impulse travels through sensory neuron to integration center in the spinal cord 3 Nerve impulse is processed in the integration center Interneuron 1 Stimulus Spinal cord activates receptor Pelvic splanchnic nerve 4 Motor impulses are conducted through motor neurons Postganglionic axon Ureter Urinary bladder Detrusor muscle contracts 5 Effector responds to impulse from motor neuron (smooth muscle contraction occurs in the bladder wall and relaxation in the internal urethral sphincter) Figure 18. 11 Internal urethral sphincter relaxes
 CNS Control of Autonomic Function Autonomic function is influenced by the: • cerebrum • hypothalamus • brainstem • spinal cord
CNS Control of Autonomic Function Autonomic function is influenced by the: • cerebrum • hypothalamus • brainstem • spinal cord
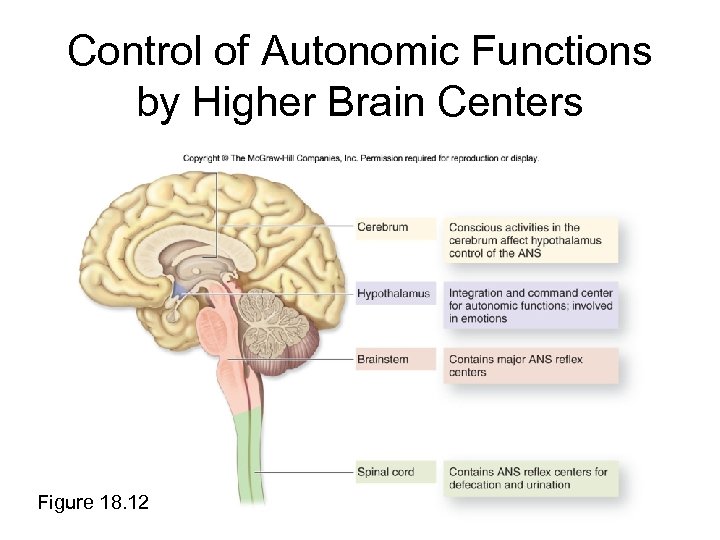 Control of Autonomic Functions by Higher Brain Centers Figure 18. 12
Control of Autonomic Functions by Higher Brain Centers Figure 18. 12
 CNS Control of Autonomic Function Cerebrum: • ANS activities are affected by conscious activities in cerebral cortex and subconscious communication between association areas in the cortex with centers of sympathetic and parasympathetic control in the hypothalamus. • Sensory processing in the thalamus and emotional states controlled in the limbic system directly affect the hypothalamus.
CNS Control of Autonomic Function Cerebrum: • ANS activities are affected by conscious activities in cerebral cortex and subconscious communication between association areas in the cortex with centers of sympathetic and parasympathetic control in the hypothalamus. • Sensory processing in the thalamus and emotional states controlled in the limbic system directly affect the hypothalamus.
 CNS Control of Autonomic Function Hypothalamus: • Integration and command center for autonomic functions • Contains nuclei that control visceral functions in both divisions of the ANS • Communicates with other CNS regions, including cerebral cortex, thalamus, brainstem, cerebellum, and spinal cord • Central brain structure involved in emotions and drives that act through the ANS
CNS Control of Autonomic Function Hypothalamus: • Integration and command center for autonomic functions • Contains nuclei that control visceral functions in both divisions of the ANS • Communicates with other CNS regions, including cerebral cortex, thalamus, brainstem, cerebellum, and spinal cord • Central brain structure involved in emotions and drives that act through the ANS
 CNS Control of Autonomic Function Brainstem: • Nuclei in the mesencephalon, pons, medulla oblongata mediate visceral reflexes. • Reflex centers control accommodation of the lens, blood pressure changes, blood vessel diameter changes, digestive activities, heart rate changes, and pupil size. • Centers for cardiac, digestive, and vasomotor functions are housed within the brainstem.
CNS Control of Autonomic Function Brainstem: • Nuclei in the mesencephalon, pons, medulla oblongata mediate visceral reflexes. • Reflex centers control accommodation of the lens, blood pressure changes, blood vessel diameter changes, digestive activities, heart rate changes, and pupil size. • Centers for cardiac, digestive, and vasomotor functions are housed within the brainstem.
 CNS Control of Autonomic Function Spinal Cord: • Processes some autonomic responses, notably the parasympathetic activities associated with defecation and urination, without involvement of the brain • Higher centers in the brain may consciously inhibit these reflex activities
CNS Control of Autonomic Function Spinal Cord: • Processes some autonomic responses, notably the parasympathetic activities associated with defecation and urination, without involvement of the brain • Higher centers in the brain may consciously inhibit these reflex activities
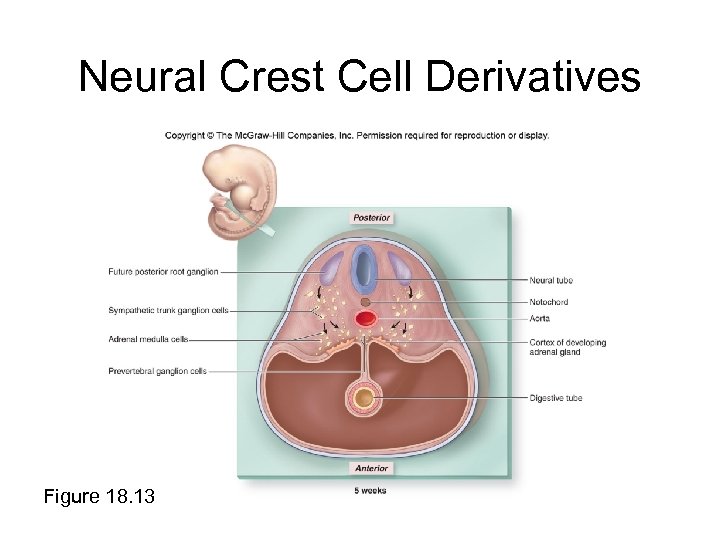 Neural Crest Cell Derivatives Figure 18. 13
Neural Crest Cell Derivatives Figure 18. 13


