ab26aa203575e3af0a868af0d85ccbde.ppt
- Количество слайдов: 50
Chapter 16 Enterobacteriaceae MLAB 2434 – Clinical Microbiology Cecile Sanders & Keri Brophy-Martinez
Chapter 16 - Enterics Family Enterobacteriaceae often referred to as “enterics” ¢ Four major features: ¢ All ferment glucose (dextrose) l All reduce nitrates to nitrites l All are oxidase negative l All except Klebsiella, Shigella and Yersinia are motile l
Microscopic and Colony Morphology Gram negative bacilli or coccobacilli ¢ Non-spore forming ¢ Colony morphology on BAP or CA of little value, as they look the same, except for Klebsiella ¢ Selective and differential media are used for initial colony evaluation (ex. Mac. Conkey, HE, XLD agars) ¢
Classification of Enterics Due to the very large number of organisms in the Family Enterobacteriaceae (see Table 1611), species are grouped into Tribes, which have similar characteristics (Table 16 -1, page 466) ¢ Within each Tribe, species are further subgrouped under genera ¢
Virulence and Antigenic Factors of Enterics ¢ ¢ ¢ Ability to colonize, adhere, produce various toxins and invade tissues Some possess plasmids that may mediate resistance to antibiotics Many enterics possess antigens that can be used to identify groups l l l O antigen – somatic, heat-stable antigen located in the cell wall H antigen – flagellar, heat labile antigen K antigen – capsular, heat-labile antigen
Clinical Significance of Enterics are ubiquitous in nature ¢ Except for few, most are present in the intestinal tract of animals and humans as commensal flora; therefore, they are sometimes call “fecal coliforms” ¢ Some live in water, soil and sewage ¢
Clinical Significance of Enterics (cont’d) ¢ Based on clinical infections produced, enterics are divided into two categories: Opportunistic pathogens – normally part of the usual intestinal flora that may produce infection outside the intestine l Primary intestinal pathogens – Salmonella, Shigella, and Yersinia sp. l
Escherichia coli Most significant species in the genus ¢ Important potential pathogen in humans ¢ Common isolate from colon flora ¢
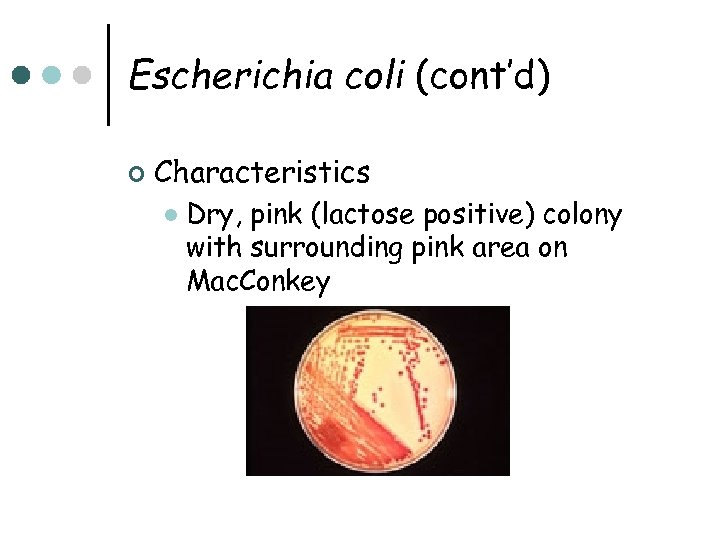
Escherichia coli (cont’d) ¢ Characteristics l Dry, pink (lactose positive) colony with surrounding pink area on Mac. Conkey
Escherichia coli (cont’d) Ferments glucose, lactose, trehalose, & xylose l Positive indole and methyl red tests l Does NOT produce H 2 S or phenylalanine deaminase l Simmons citrate negative l Usually motile l Voges-Proskauer test negative l
Escherichia coli (cont’d) ¢ Infections Wide range including meningitis, gastrointestinal, urinary tract, wound, and bacteremia l Gastrointestinal Infections l • Enteropathogenic (EPEC) – primarily in infants and children; outbreaks in hospital nurseries and day care centers; stool has mucous but not blood; identified by serotyping
Escherichia coli (cont’d) • Enterotoxigenic (ETEC) – “traveler’s diarrhea”; watery diarrhea without blood; self-limiting; usually not identified, other than patient history and lactose-positive organisms cultured on differential media • Enteroinvasive (EIEC) – produce dysentery with bowel penetration, invasion and destruction of intestinal mucosa; watery diarrhea with blood; do NOT ferment lactose; identified via DNA probes
Escherichia coli (cont’d) • Enterohemorrhagic (EHEC serotype 0157: H 7) – associated with hemorrhagic diarrhea and hemolytic-uremic syndrome (HUS), which includes low platelet count, hemolytic anemia, and kidney failure; potentially fatal, especially in young children; undercooked hamburger, unpasteurized milk and apple cider have spread the infection; does NOT ferment sucrose; identified by serotyping
Escherichia coli (cont’d) • Enteroaggregative (Eagg. EC) – cause diarrhea by adhering to the mucosal surface of the intestine; watery diarrhea; symptoms may persist for over two weeks l Urinary Tract Infections • E. coli is most common cause of UTI and kidney infection in humans • Usually originate in the large instestine • Able to adhere to epithelial cells in the urinary tract
Escherichia coli (cont’d) l Septicemia & Meningitis • E. coli is one of the most common causes of septicemia and meningitis among neonates; acquired in the birth canal before or during delivery • E. coli also causes bacteremia in adults, primarily from a genitourinary tract infection or a gastrointestinal source ¢ ¢ Escherichia hermannii – yellow pigmented; isolated from CSF, wounds and blood Escherichia vulneris - wounds
Klebsiella, Enterobacter, Serratia & Hafnia sp. ¢ ¢ ¢ Usually found in intestinal tract Wide variety of infections, primarily pneumonia, wound, and UTI General characteristics: l l l Some species are non-motile Simmons citrate positive H 2 S negative Phenylalanine deaminase negative Some weakly urease positive MR negative; VP positive
Klebsiella species ¢ ¢ ¢ Usually found in GI tract Four major species K. pneumoniae is mostly commonly isolated species l l l Possesses a polysaccharide capsule, which protects against phagocytosis and antibiotics AND makes the colonies moist and mucoid Has a distinctive “yeasty” odor Frequent cause of nosocomial pneumonia
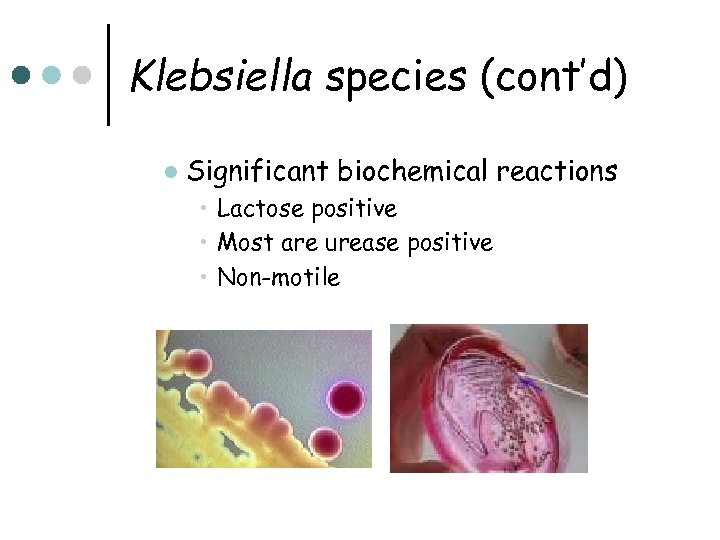
Klebsiella species (cont’d) l Significant biochemical reactions • Lactose positive • Most are urease positive • Non-motile
Enterobacter species Comprised of 12 species; E. cloacae and E. aerogenes are most common ¢ Isolated from wounds, urine, blood and CSF ¢ Major characteristics ¢ Colonies resemble Klebsiella l Motile l MR negative; VP positive l
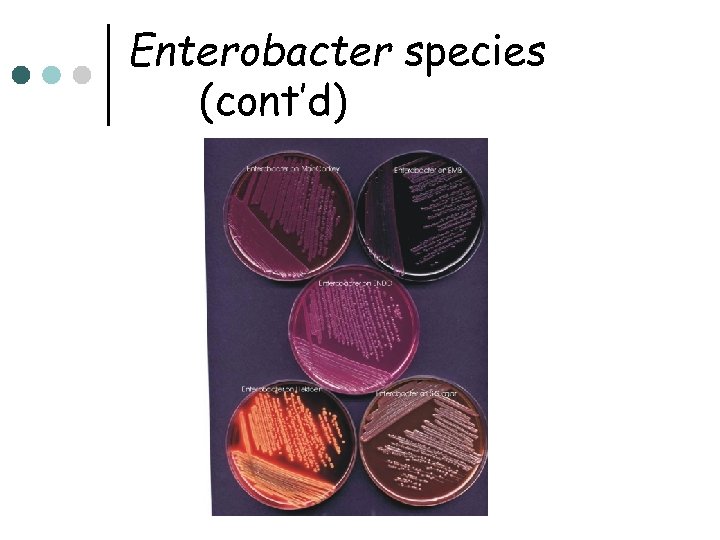
Enterobacter species (cont’d)
Serratia species Seven species, but S. marcescens is the only one clinically important ¢ Frequently found in nosocomial infections of urinary or respiratory tracts ¢ Implicated in bacteremic outbreaks in nurseries, cardiac surgery, and burn units ¢ Fairly resistant to antibiotics ¢
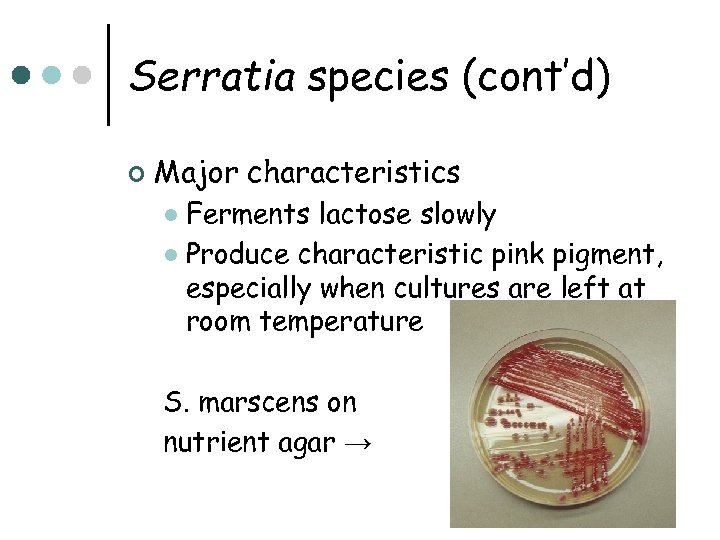
Serratia species (cont’d) ¢ Major characteristics Ferments lactose slowly l Produce characteristic pink pigment, especially when cultures are left at room temperature l S. marscens on nutrient agar →
Hafnia species Hafnia alvei is only species ¢ Has been isolated from many anatomical sites in humans and the environment ¢ Occasionally isolated from stools ¢ Delayed citrate reaction is major characteristic ¢
Proteus, Morganella & Providencia species All are normal intestinal flora ¢ Opportunistic pathogens ¢ Deaminate phenylalanine ¢ All are lactose negative ¢
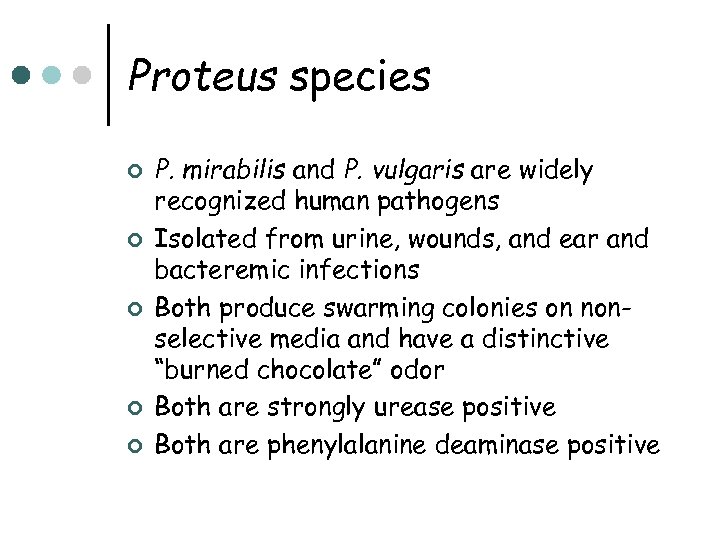
Proteus species ¢ ¢ ¢ P. mirabilis and P. vulgaris are widely recognized human pathogens Isolated from urine, wounds, and ear and bacteremic infections Both produce swarming colonies on nonselective media and have a distinctive “burned chocolate” odor Both are strongly urease positive Both are phenylalanine deaminase positive
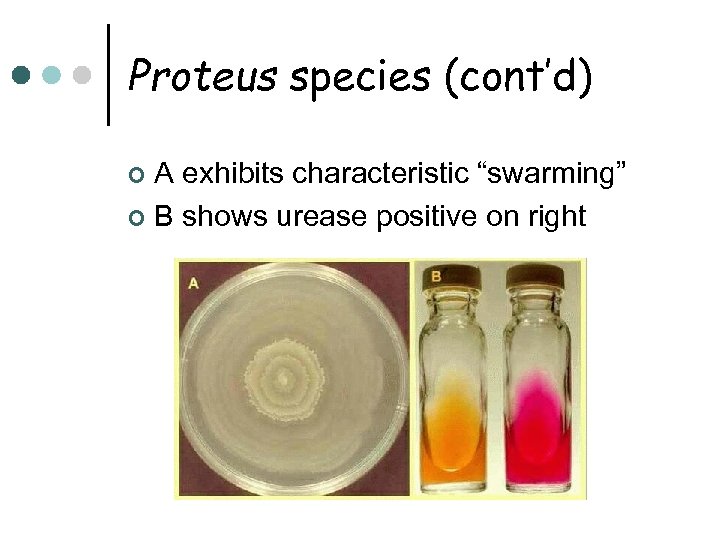
Proteus species (cont’d) A exhibits characteristic “swarming” ¢ B shows urease positive on right ¢
Morganella species Morganella morganii is only species ¢ Documented cause of UTI ¢ Isolated from other anatomical sites ¢ Urease positive ¢ Phenylalanine deaminase positive ¢
Providencia species Providencia rettgeri is pathogen of urinary tract and has caused nosocomial outbreaks ¢ Providenicia stuartii can cause nosocomial outbreaks in burn units and has been isolated from urine ¢ Both are phenylalanine deaminase positive ¢
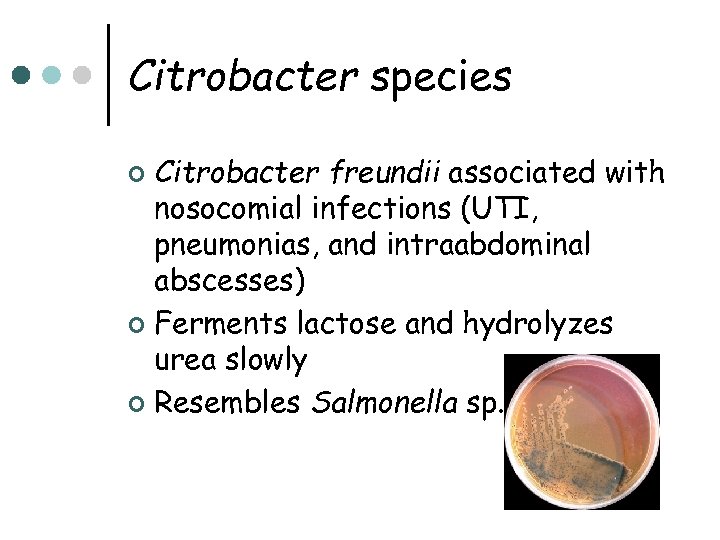
Citrobacter species Citrobacter freundii associated with nosocomial infections (UTI, pneumonias, and intraabdominal abscesses) ¢ Ferments lactose and hydrolyzes urea slowly ¢ Resembles Salmonella sp. ¢
Salmonella Produce significant infections in humans and certain animals ¢ On differential selective agar, produces clear, colorless, nonlactose fermenting colonies with black centers (if media contains indicator for hydrogen sulfide) ¢
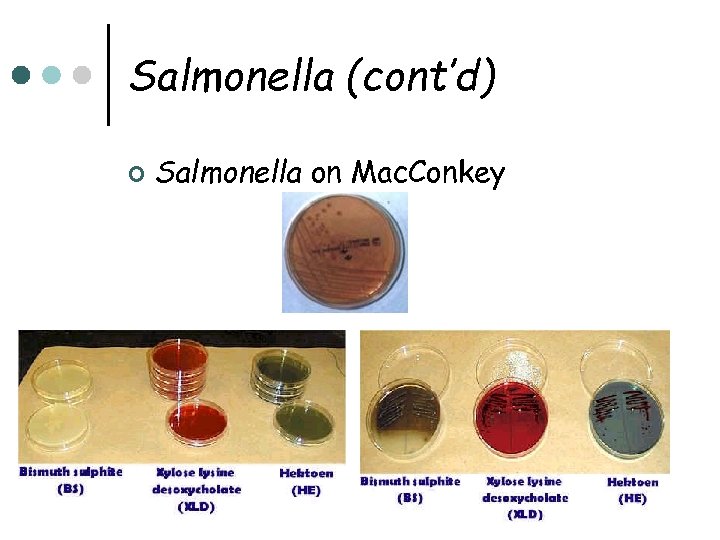
Salmonella (cont’d) ¢ Salmonella on Mac. Conkey
Salmonella (cont’d) Lactose negative ¢ Negative for indole, VP, phenylalanine deaminase, and urease ¢ Most produce H 2 S ¢ Do not grow in potassium cyanide ¢ Large and complex group of organisms; grouped by O, H, and Vi (for virulence) antigens ¢
Salmonella (cont’d) ¢ Clinical Infections l Acute gastroenteritis or food poisoning • Source = handling pets, insufficiently cooked eggs and chicken, and contaminated cooking utensils • Occurs 8 to 36 hours after ingestion • Requires a high microbial load for infection • Self-limiting in health individuals (antibiotics and antidiarrheal agents may prolong symptoms)
Salmonella (cont’d) l Typhoid and Other Enteric Fevers • Prolonged fever • Bacteremia • Involvement of the RE system, particularly liver, spleen, intestines, and mesentery • Dissemination to multiple organs • Occurs more often in tropical and subtropical countries
Salmonella (cont’d) Salmonella Bacteremia l Carrier State l • Organisms shed in feces • Gallbladder is the site of organisms (removal of gallbladder may be the only solution to carrier state)
Shigella species Closely related to the Escherichia ¢ All species cause bacillary dysentery ¢ S. dysenteriae (Group A) ¢ S. flexneri (Group B) ¢ S. boydii (Group C) ¢ S. sonnei (Group D) ¢
Shigella (cont’d) ¢ Characteristics l l l l Non-motile Do not produce gas from glucose Do not hydrolyze urea Do not produce H 2 S on TSI Lysine decarboxylase negative ONPG positive (delayed lactose +) Fragile organisms Possess O and some have K antigens
Shigella (cont’d) ¢ Clinical Infections l l l Cause dysentery (bloody stools, mucous, and numerous WBC) S. sonnei is most common, followed by S. flexneri (“gay bowel syndrome”) Humans are only known reservoir Oral-fecal transmission Fewer than 200 bacilli are needed for infection in health individuals

Shigella (cont’d)
Yersinia species ¢ ¢ Consists of 11 named species Yersinia pestis l l l Causes plague, which is a disease primarily of rodents; transmitted by fleas Two forms of plague, bubonic and pneumonic Gram-negative, short, plump bacillus, exhibiting “safety-pin” or “bipolar” staining
Yersinia species ¢ Yersinia enterocolitica l Most common form of Yersinia l Found worldwide l Found in pigs, cats and dogs l Human also infected by ingestion of contaminated food or water l Some infections result from eating contaminated market meat and vacuum-packed beef l Is able to survive refrigerator temperatures (can use “cold enrichment” to isolate) l Mainly causes acute gastroenteritis with fever
Yersinia species ¢ Yersinia pseudotuberculosis Pathogen of rodents, particularly guinea pigs l Septicemia with mesenteric lymphadenitis, similar to appendicitis l Motile at 18 to 22 degrees C l
Laboratory Diagnosis of Enterics ¢ Collection and Handling l ¢ If not processed quickly, should be collected and transported in Cary. Blair, Amies, or Stuart media Isolation and Identification Site of origin must be considered l Enterics from sterile body sites are highly significant l Routinely cultured from stool l
Laboratory Diagnosis of Enterics (cont’d) ¢ Media for Isolation and Identification of Enterics Most labs use BAP, CA and a selective/differential medium such as Mac. Conkey l On Mac. Conkey, lactose positive are pink; lactose negative are clear and colorless l
Laboratory Diagnosis of Enterics (cont’d) l ¢ For stools, highly selective media, such as Hektoen Enteric (HE), XLD, or SS is used along with Mac. Conkey agar Identification l Most labs use a miniaturized or automated commercial identification system, rather than multiple tubes inoculated manually
Laboratory Diagnosis of Enterics (cont’d) ¢ Identification (cont’d) l All enterics are • Oxidase negative • Ferment glucose • Reduce nitrates to nitrites
Laboratory Diagnosis of Enterics (cont’d) ¢ Common Biochemical Tests Lactose fermentation and utilization of carbohydrates l Triple Sugar Iron (TSI) l ONPG l Glucose metabolism l • Methyl red • Voges-Proskauer
Laboratory Diagnosis of Enterics (cont’d) ¢ Common Biochemical Tests (cont’d) l Miscellaneous Reactions • • • Indole Citrate utilization Urease production Motility Phenylalanine deaminase Decarboxylase tests
Screening Stools for Pathogens Because stools have numerous microbial flora, efficient screening methods must be used to recover any pathogens ¢ Enteric pathogens include Salmonella, Shigella, Aeromonas, Campylobacter, Yersinia, Vibrio, and E. coli 0157: H 7 ¢
Screening Stools for Pathogens (cont’d) Most labs screen for Salmonella, Shigella, and Campylobacter; many screen for E. coli 0157: H 7 ¢ Fecal pathogens are generally lactose-negative (although Proteus, Providencia, Serratia, Citrobacter and Pseudomonas are also lactosenegative) ¢
ab26aa203575e3af0a868af0d85ccbde.ppt