494bf206488afbee0ae0ca46218ddf9e.ppt
- Количество слайдов: 77
 Chapter 14: Circulatory System • Internal and external factors influence heart function. • The blood system continuously transports substances to cells and simultaneously collects waste products.
Chapter 14: Circulatory System • Internal and external factors influence heart function. • The blood system continuously transports substances to cells and simultaneously collects waste products.
 I. Circulatory System A. Different systems 1. Cardiovascular system : blood, heart, and blood vessels 2. Lymphatic system: lymph, lymph nodes, and lymph vessels 3. Circulatory system: cardiovascular and lymphatic systems together
I. Circulatory System A. Different systems 1. Cardiovascular system : blood, heart, and blood vessels 2. Lymphatic system: lymph, lymph nodes, and lymph vessels 3. Circulatory system: cardiovascular and lymphatic systems together
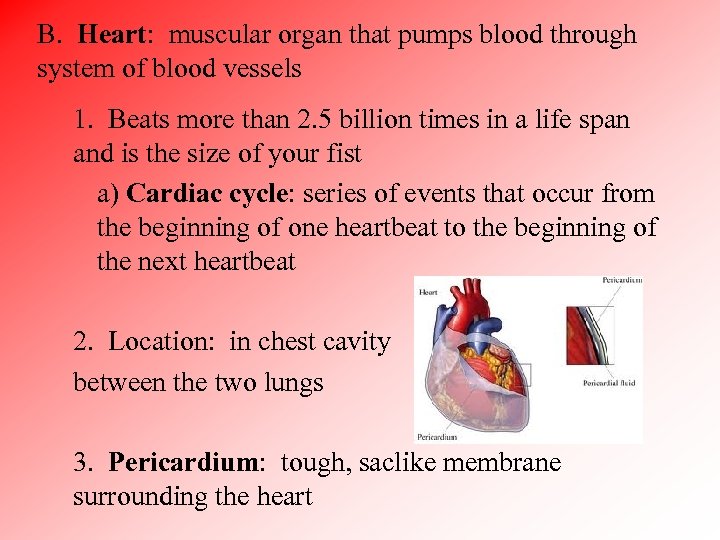 B. Heart: muscular organ that pumps blood through system of blood vessels 1. Beats more than 2. 5 billion times in a life span and is the size of your fist a) Cardiac cycle: series of events that occur from the beginning of one heartbeat to the beginning of the next heartbeat 2. Location: in chest cavity between the two lungs 3. Pericardium: tough, saclike membrane surrounding the heart
B. Heart: muscular organ that pumps blood through system of blood vessels 1. Beats more than 2. 5 billion times in a life span and is the size of your fist a) Cardiac cycle: series of events that occur from the beginning of one heartbeat to the beginning of the next heartbeat 2. Location: in chest cavity between the two lungs 3. Pericardium: tough, saclike membrane surrounding the heart
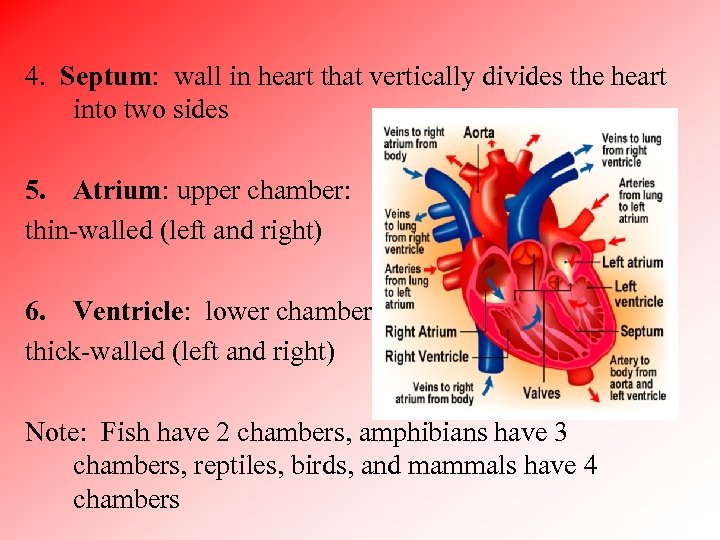 4. Septum: wall in heart that vertically divides the heart into two sides 5. Atrium: upper chamber: thin-walled (left and right) 6. Ventricle: lower chamber: thick-walled (left and right) Note: Fish have 2 chambers, amphibians have 3 chambers, reptiles, birds, and mammals have 4 chambers
4. Septum: wall in heart that vertically divides the heart into two sides 5. Atrium: upper chamber: thin-walled (left and right) 6. Ventricle: lower chamber: thick-walled (left and right) Note: Fish have 2 chambers, amphibians have 3 chambers, reptiles, birds, and mammals have 4 chambers
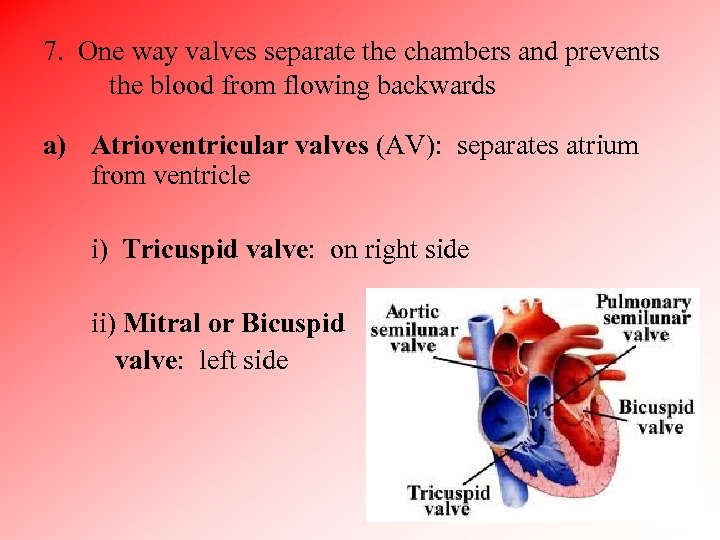 7. One way valves separate the chambers and prevents the blood from flowing backwards a) Atrioventricular valves (AV): separates atrium from ventricle i) Tricuspid valve: on right side ii) Mitral or Bicuspid valve: left side
7. One way valves separate the chambers and prevents the blood from flowing backwards a) Atrioventricular valves (AV): separates atrium from ventricle i) Tricuspid valve: on right side ii) Mitral or Bicuspid valve: left side
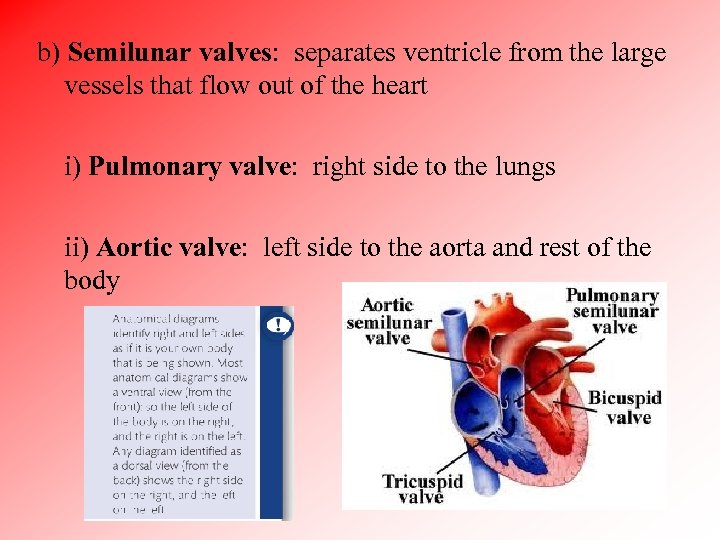 b) Semilunar valves: separates ventricle from the large vessels that flow out of the heart i) Pulmonary valve: right side to the lungs ii) Aortic valve: left side to the aorta and rest of the body
b) Semilunar valves: separates ventricle from the large vessels that flow out of the heart i) Pulmonary valve: right side to the lungs ii) Aortic valve: left side to the aorta and rest of the body

 Note: There are no valves into the atria from the vena cava or the pulmonary vein What prevents blood from flowing back? 1. Veins have internal, passive flap valves that close if blood starts to flow backwards 2. Atrial systole (contractions) does not build up very much pressure 3. Combination of low pressure and passive flap valves means that no heart valve is necessary into each atrium
Note: There are no valves into the atria from the vena cava or the pulmonary vein What prevents blood from flowing back? 1. Veins have internal, passive flap valves that close if blood starts to flow backwards 2. Atrial systole (contractions) does not build up very much pressure 3. Combination of low pressure and passive flap valves means that no heart valve is necessary into each atrium
 8. Heart is composed of cardiac muscle cells a) Skeletal muscle: muscle that moves your bones to create various body motions and many individual cells are fused together to make a fiber i) Fibers are multinucleate (many nuclei) and makes it easier for the fiber to act as a single unit when contracting
8. Heart is composed of cardiac muscle cells a) Skeletal muscle: muscle that moves your bones to create various body motions and many individual cells are fused together to make a fiber i) Fibers are multinucleate (many nuclei) and makes it easier for the fiber to act as a single unit when contracting
 ii) Sarcomeres: actin and myosin proteins in contracting units b)Cardiac and skeletal muscle have similar arrangements of sarcomeres c) Intercalated discs: interconnects the cardiac muscle cells containing sarcomeres i) Disc-shaped areas contain openings called gap junctions where cytoplasm from one cell freely passes to the next cell
ii) Sarcomeres: actin and myosin proteins in contracting units b)Cardiac and skeletal muscle have similar arrangements of sarcomeres c) Intercalated discs: interconnects the cardiac muscle cells containing sarcomeres i) Disc-shaped areas contain openings called gap junctions where cytoplasm from one cell freely passes to the next cell
 ii) Gap junction: protein-lined channels that allow direct transmission of the nerve impulse from cell to cell so that cells contract in unison (muscle is said to be “electrically coupled”) iii) Sharing of the cytoplasm allows the cardiac muscle cells to pass an electrical signal quickly from cell to cells iv)Without gap junctions the impulse to begin a heart beat would spread too slowly through the tissue to result in a unified event
ii) Gap junction: protein-lined channels that allow direct transmission of the nerve impulse from cell to cell so that cells contract in unison (muscle is said to be “electrically coupled”) iii) Sharing of the cytoplasm allows the cardiac muscle cells to pass an electrical signal quickly from cell to cells iv)Without gap junctions the impulse to begin a heart beat would spread too slowly through the tissue to result in a unified event
 d) Cardiac muscle cells that are joined together by intercalated discs form fibrous units that repeatedly branch so the cells works together as a unit as long as they get a signal to synchronize their contractions e) Muscle tissue has a large number of mitochondria and blood supply (highly vascular) to prevent muscle fatigue
d) Cardiac muscle cells that are joined together by intercalated discs form fibrous units that repeatedly branch so the cells works together as a unit as long as they get a signal to synchronize their contractions e) Muscle tissue has a large number of mitochondria and blood supply (highly vascular) to prevent muscle fatigue
 Interactive slide
Interactive slide
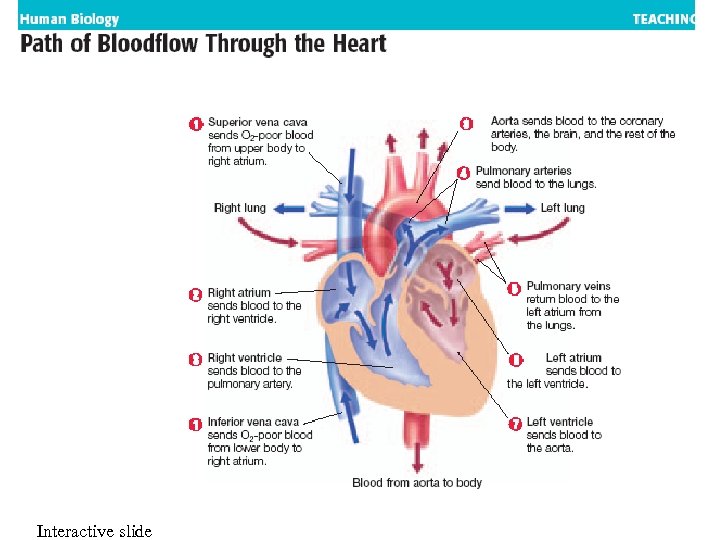
 C. Circulation in the heart Overview 1. Blood returns from the rest of the body with little oxygen and high concentration of carbon dioxide through the vena cava 2. Deoxygenated blood enters the right atrium 3. Right atrium pumps blood into right ventricle 4. Right ventricle pumps into pulmonary artery
C. Circulation in the heart Overview 1. Blood returns from the rest of the body with little oxygen and high concentration of carbon dioxide through the vena cava 2. Deoxygenated blood enters the right atrium 3. Right atrium pumps blood into right ventricle 4. Right ventricle pumps into pulmonary artery
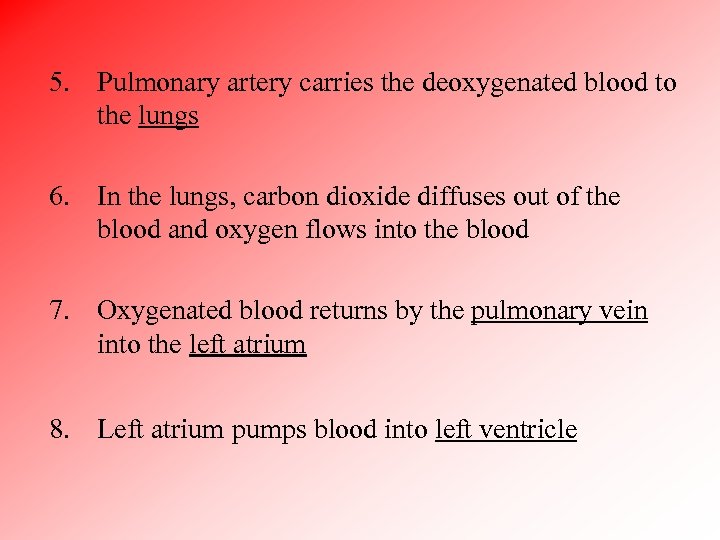 5. Pulmonary artery carries the deoxygenated blood to the lungs 6. In the lungs, carbon dioxide diffuses out of the blood and oxygen flows into the blood 7. Oxygenated blood returns by the pulmonary vein into the left atrium 8. Left atrium pumps blood into left ventricle
5. Pulmonary artery carries the deoxygenated blood to the lungs 6. In the lungs, carbon dioxide diffuses out of the blood and oxygen flows into the blood 7. Oxygenated blood returns by the pulmonary vein into the left atrium 8. Left atrium pumps blood into left ventricle
 9. Left ventricle pumps blood into aorta 10. Aorta: large blood vessel that carries oxygenated blood to the rest of the body
9. Left ventricle pumps blood into aorta 10. Aorta: large blood vessel that carries oxygenated blood to the rest of the body

 Summary 1. Pulmonary circulation: route of blood flow from the right side of the heart to the lungs to release carbon dioxide and pick-up oxygen 2. Systemic circulation: route of blood flow from the left side of the heart through the aorta to the rest of body delivering oxygen to organs and tissues and picking up carbon dioxide
Summary 1. Pulmonary circulation: route of blood flow from the right side of the heart to the lungs to release carbon dioxide and pick-up oxygen 2. Systemic circulation: route of blood flow from the left side of the heart through the aorta to the rest of body delivering oxygen to organs and tissues and picking up carbon dioxide
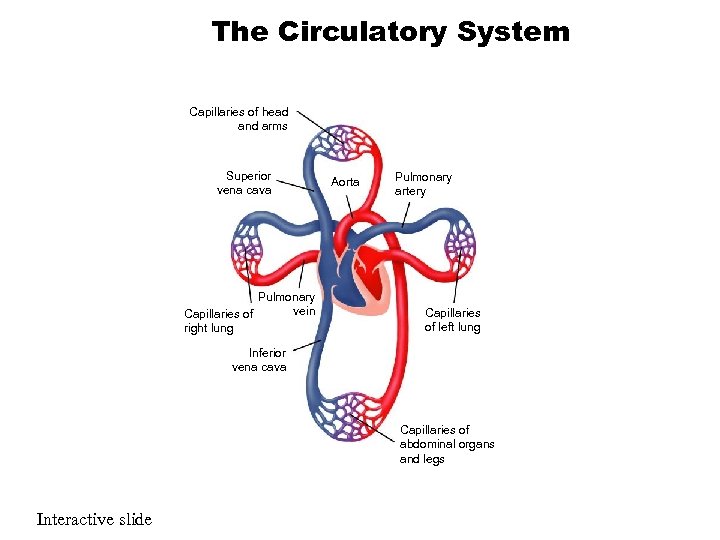 The Circulatory System Capillaries of head and arms Superior vena cava Pulmonary vein Capillaries of right lung Aorta Pulmonary artery Capillaries of left lung Inferior vena cava Capillaries of abdominal organs and legs Interactive slide
The Circulatory System Capillaries of head and arms Superior vena cava Pulmonary vein Capillaries of right lung Aorta Pulmonary artery Capillaries of left lung Inferior vena cava Capillaries of abdominal organs and legs Interactive slide
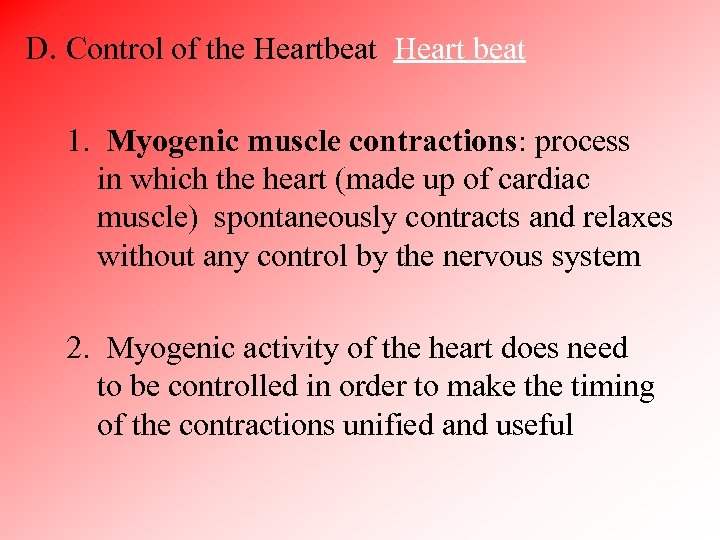 D. Control of the Heartbeat Heart beat 1. Myogenic muscle contractions: process in which the heart (made up of cardiac muscle) spontaneously contracts and relaxes without any control by the nervous system 2. Myogenic activity of the heart does need to be controlled in order to make the timing of the contractions unified and useful
D. Control of the Heartbeat Heart beat 1. Myogenic muscle contractions: process in which the heart (made up of cardiac muscle) spontaneously contracts and relaxes without any control by the nervous system 2. Myogenic activity of the heart does need to be controlled in order to make the timing of the contractions unified and useful
 3. Sinoatrial node (SA): group of specialized heart muscle cells located in the right atrium with properties of both muscle and nervous system cells a) Starts their own electrical impulse and contract b) Pacemaker: regulates the rate of contraction of the entire heart by sending out an “electrical” signal to initiate the contraction of both atria c) With a resting heart rate of 72 beats a minute, the SA node sends out a signal every 0. 8 seconds
3. Sinoatrial node (SA): group of specialized heart muscle cells located in the right atrium with properties of both muscle and nervous system cells a) Starts their own electrical impulse and contract b) Pacemaker: regulates the rate of contraction of the entire heart by sending out an “electrical” signal to initiate the contraction of both atria c) With a resting heart rate of 72 beats a minute, the SA node sends out a signal every 0. 8 seconds
 The Sinoatrial Node Contraction of Atria Contraction of Ventricles Sinoatrial (SA) node Conducting fibers Atrioventricular (AV) node
The Sinoatrial Node Contraction of Atria Contraction of Ventricles Sinoatrial (SA) node Conducting fibers Atrioventricular (AV) node
 4. Atrioventricular node (AV): impulse from SA reaches AV and it relays the electrical impulse to the muscle cells of the ventricles in order to contract a) Located in septum between the atria b) AV node receives impulse and then delays form 0. 1 seconds, and then sends out another “electrical” signal (action potential) c) The second signal goes to the ventricles and causes them to contract
4. Atrioventricular node (AV): impulse from SA reaches AV and it relays the electrical impulse to the muscle cells of the ventricles in order to contract a) Located in septum between the atria b) AV node receives impulse and then delays form 0. 1 seconds, and then sends out another “electrical” signal (action potential) c) The second signal goes to the ventricles and causes them to contract
 i) Conducting fibers: system of fibers that are used in order for the action potentials to reach all the muscle cells of the ventricle efficiently since the walls of the ventricle are thick ii) Conducting fibers begin at the AV node and travel down the septum between the two ventricles iii) Purkinje fibers: branches of the conducting fibers that spread out into the thick cardiac muscle tissue iv) Gap junctions within the intercalated discs of the cardiac muscle cells finish conducting the impulse
i) Conducting fibers: system of fibers that are used in order for the action potentials to reach all the muscle cells of the ventricle efficiently since the walls of the ventricle are thick ii) Conducting fibers begin at the AV node and travel down the septum between the two ventricles iii) Purkinje fibers: branches of the conducting fibers that spread out into the thick cardiac muscle tissue iv) Gap junctions within the intercalated discs of the cardiac muscle cells finish conducting the impulse

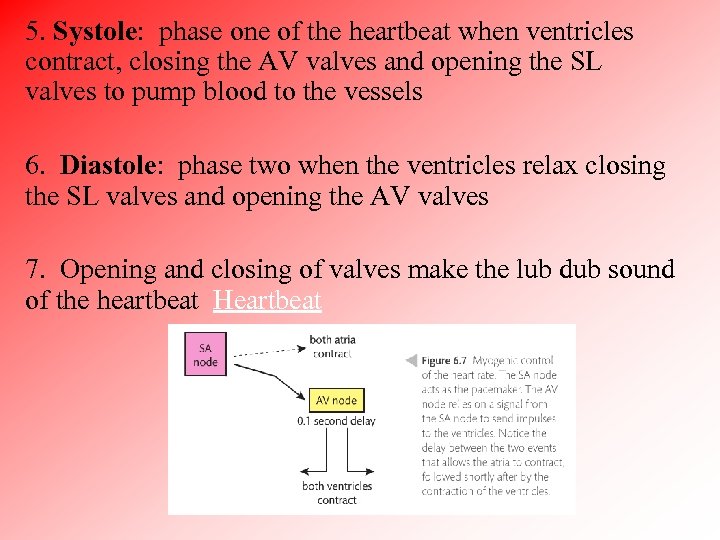 5. Systole: phase one of the heartbeat when ventricles contract, closing the AV valves and opening the SL valves to pump blood to the vessels 6. Diastole: phase two when the ventricles relax closing the SL valves and opening the AV valves 7. Opening and closing of valves make the lub dub sound of the heartbeat Heartbeat
5. Systole: phase one of the heartbeat when ventricles contract, closing the AV valves and opening the SL valves to pump blood to the vessels 6. Diastole: phase two when the ventricles relax closing the SL valves and opening the AV valves 7. Opening and closing of valves make the lub dub sound of the heartbeat Heartbeat
 E. Changes in pressure within the heart chambers keep the blood moving 1. Heart valves open and close depending on the pressure of the blood on each side of the valve 2. The change in pressure also explains the movement of blood through and out of each chamber of the heart
E. Changes in pressure within the heart chambers keep the blood moving 1. Heart valves open and close depending on the pressure of the blood on each side of the valve 2. The change in pressure also explains the movement of blood through and out of each chamber of the heart
 3. Both chambers are at rest: diastole a) Numbers inside each chamber or blood vessel represent the pressure measured in mm. Hg b) The atrial pressure is just slightly higher than ventricular pressure and this keeps the atrioventricular valve open
3. Both chambers are at rest: diastole a) Numbers inside each chamber or blood vessel represent the pressure measured in mm. Hg b) The atrial pressure is just slightly higher than ventricular pressure and this keeps the atrioventricular valve open
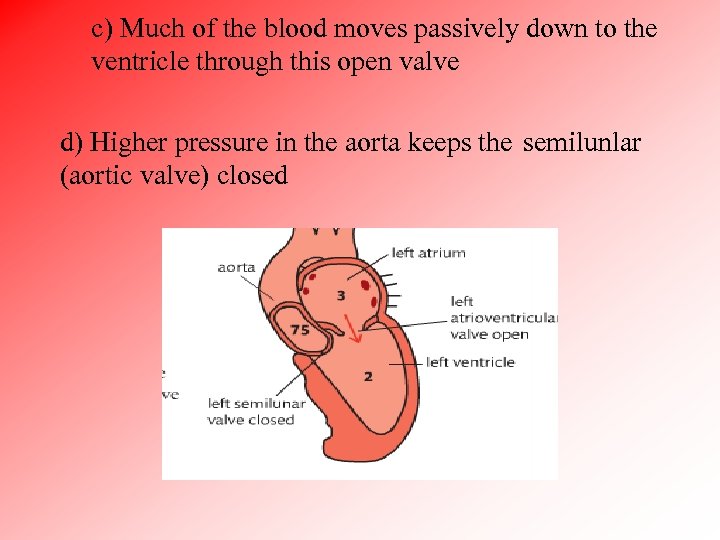 c) Much of the blood moves passively down to the ventricle through this open valve d) Higher pressure in the aorta keeps the semilunlar (aortic valve) closed
c) Much of the blood moves passively down to the ventricle through this open valve d) Higher pressure in the aorta keeps the semilunlar (aortic valve) closed
 4. Atria in systole and ventricles are in diastole a) Atrium is undergoing systole (contraction) b) Pressure produced is not very high since the atrium walls is a thin muscle and there is no need for a great pressure since much of the blood moved passively
4. Atria in systole and ventricles are in diastole a) Atrium is undergoing systole (contraction) b) Pressure produced is not very high since the atrium walls is a thin muscle and there is no need for a great pressure since much of the blood moved passively
 5. Atria are in diastole and ventricles are in systole a) Pressure inside the ventricle increases to be greater than in the atrium, so atrioventricular valve closes to prevent backflow to atrium (lub sound) b) Pressure continues to build as a large volume of blood increases and pressure becomes greater than pressure in aorta c) Semilunar valve opens and blood is pumped into aorta
5. Atria are in diastole and ventricles are in systole a) Pressure inside the ventricle increases to be greater than in the atrium, so atrioventricular valve closes to prevent backflow to atrium (lub sound) b) Pressure continues to build as a large volume of blood increases and pressure becomes greater than pressure in aorta c) Semilunar valve opens and blood is pumped into aorta
 d) Pressure decreases as the contraction is finished and semilunar valve closes (dub sound) e) Both chambers go back into diastole and the cardiac cycle repeats itself
d) Pressure decreases as the contraction is finished and semilunar valve closes (dub sound) e) Both chambers go back into diastole and the cardiac cycle repeats itself
 F. Increased body activity leads to the heart rate increasing 1. Increased demand for oxygen for cell respiration during times of heavy exercise or activity and need to get rid of carbon dioxide 2. Medulla in the brainstem can chemically sense the increase in carbon dioxide 3. Medulla sends a signal through the cranial nerve called the cardiac nerve, to increase the heart rate to the correct level
F. Increased body activity leads to the heart rate increasing 1. Increased demand for oxygen for cell respiration during times of heavy exercise or activity and need to get rid of carbon dioxide 2. Medulla in the brainstem can chemically sense the increase in carbon dioxide 3. Medulla sends a signal through the cranial nerve called the cardiac nerve, to increase the heart rate to the correct level
 4. Signal is sent to the SA node. It doesn’t change the mechanisms of the heart beats, just the timing 5. After exercise, the carbon dioxide levels decrease and another signal is sent from the medulla through the vagus nerve 6. Electrical signal from the vagus nerve results in the SA node adjusting the heart rate back to its resting rate
4. Signal is sent to the SA node. It doesn’t change the mechanisms of the heart beats, just the timing 5. After exercise, the carbon dioxide levels decrease and another signal is sent from the medulla through the vagus nerve 6. Electrical signal from the vagus nerve results in the SA node adjusting the heart rate back to its resting rate
 7. Chemicals can change the heart rate a) Epinephrine (adrenaline): hormone that causes the SA node to fire more frequently to increase the heart rate b) Released by the adrenal gland during periods of high stress, danger, or excitement
7. Chemicals can change the heart rate a) Epinephrine (adrenaline): hormone that causes the SA node to fire more frequently to increase the heart rate b) Released by the adrenal gland during periods of high stress, danger, or excitement
 G. Mapping the cardiac cycle to a normal ECG trace 1. Electrocardiogram (ECG): graph plotted in real time, with electrical activity from the SA and AV nodes plotted on they y-axis and time on the x-axis 2. Electrical leads are placed in a variety of places on the skin in order to measure the small voltage given off by these two nodes of the heart 3. One cardiac cycle is shown with each repeating pattern
G. Mapping the cardiac cycle to a normal ECG trace 1. Electrocardiogram (ECG): graph plotted in real time, with electrical activity from the SA and AV nodes plotted on they y-axis and time on the x-axis 2. Electrical leads are placed in a variety of places on the skin in order to measure the small voltage given off by these two nodes of the heart 3. One cardiac cycle is shown with each repeating pattern
 4. Reading a normal ECG trace a) P wave: voltage given off by the SA node and shows the atrial systole b) Point Q: AV node sends its impulse c) QRS complex: impulse from AV node spreads down the conducting fibers and to Purkinje fibers within the ventricles (ventricular systole) d) T wave: AV node is repolarizing (returning to resting potential), getting ready to send next impulse
4. Reading a normal ECG trace a) P wave: voltage given off by the SA node and shows the atrial systole b) Point Q: AV node sends its impulse c) QRS complex: impulse from AV node spreads down the conducting fibers and to Purkinje fibers within the ventricles (ventricular systole) d) T wave: AV node is repolarizing (returning to resting potential), getting ready to send next impulse

 Notes: 1. SA node also has to repolarize, but the electrical activity is hidden behind the QRS complex 2. ECG shows the delay between the firing of the SA node and the firing of the AV node. Shows the time separation between the systolic contractions of the atria and ventricles
Notes: 1. SA node also has to repolarize, but the electrical activity is hidden behind the QRS complex 2. ECG shows the delay between the firing of the SA node and the firing of the AV node. Shows the time separation between the systolic contractions of the atria and ventricles
 II. Blood vessels: network that contains the blood and keeps it flowing in one direction A. Arteries: large muscular vessels that carry blood away from the heart 1. Smooth, think, strong, and elastic to withstand the force of the blood 2. Stretching of the arteries is your pulse 3. Muscle layer is used by autonomic nervous system to change the inside diameter (lumen) of the blood vessel
II. Blood vessels: network that contains the blood and keeps it flowing in one direction A. Arteries: large muscular vessels that carry blood away from the heart 1. Smooth, think, strong, and elastic to withstand the force of the blood 2. Stretching of the arteries is your pulse 3. Muscle layer is used by autonomic nervous system to change the inside diameter (lumen) of the blood vessel
 4. Arteries have elastic fibers that help maintain the high blood pressure achieved by the contractions of the ventricles a) Blood is pumped into an artery, the elastic fibers are stretched b) Contraction is over, the elastic fibers provide another source of pressure as they return to their original position which helps to maintain the blood pressure between pump cycles
4. Arteries have elastic fibers that help maintain the high blood pressure achieved by the contractions of the ventricles a) Blood is pumped into an artery, the elastic fibers are stretched b) Contraction is over, the elastic fibers provide another source of pressure as they return to their original position which helps to maintain the blood pressure between pump cycles
 B. Blood pressure: force that blood exerts against walls of blood vessel 1. Systolic pressure: pressure of blood when ventricles contract usually 110 - 120 2. Diastolic pressure: pressure when ventricles relax usually 70 – 80 3. Hypertension: high blood pressure, places a strain on the walls of the arteries
B. Blood pressure: force that blood exerts against walls of blood vessel 1. Systolic pressure: pressure of blood when ventricles contract usually 110 - 120 2. Diastolic pressure: pressure when ventricles relax usually 70 – 80 3. Hypertension: high blood pressure, places a strain on the walls of the arteries
 C. Capillaries: tiny vessels that travel to individual cells 1. Much of the blood pressure is lost when blood enters capillaries 2. Blood cells travel one cell at a time through capillaries 3. Chemical exchanges always occur through capillaries (Ex: moving of O 2 and CO 2)
C. Capillaries: tiny vessels that travel to individual cells 1. Much of the blood pressure is lost when blood enters capillaries 2. Blood cells travel one cell at a time through capillaries 3. Chemical exchanges always occur through capillaries (Ex: moving of O 2 and CO 2)

 D. Vein: large blood vessel that carries blood to the heart bringing usually deoxygenated blood 1. Blood is at low pressure from capillaries, so the flow is slower 2. Thin walls and larger diameter, and don’t have to be as strong 3. Valves to prevent blood from moving backwards Blood vessels
D. Vein: large blood vessel that carries blood to the heart bringing usually deoxygenated blood 1. Blood is at low pressure from capillaries, so the flow is slower 2. Thin walls and larger diameter, and don’t have to be as strong 3. Valves to prevent blood from moving backwards Blood vessels
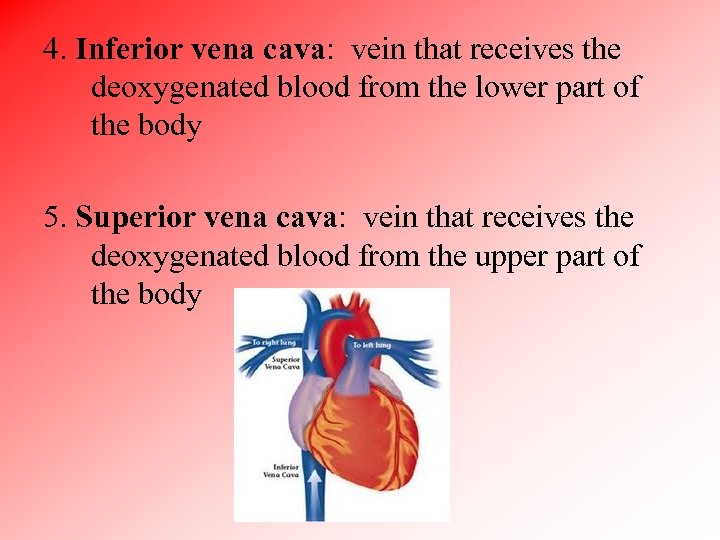 4. Inferior vena cava: vein that receives the deoxygenated blood from the lower part of the body 5. Superior vena cava: vein that receives the deoxygenated blood from the upper part of the body
4. Inferior vena cava: vein that receives the deoxygenated blood from the lower part of the body 5. Superior vena cava: vein that receives the deoxygenated blood from the upper part of the body
 Major road: arteriole Highway: Artery Neighborhood street Driveway: Capillary Heart Highway: Vein Cell Major road: Venule
Major road: arteriole Highway: Artery Neighborhood street Driveway: Capillary Heart Highway: Vein Cell Major road: Venule
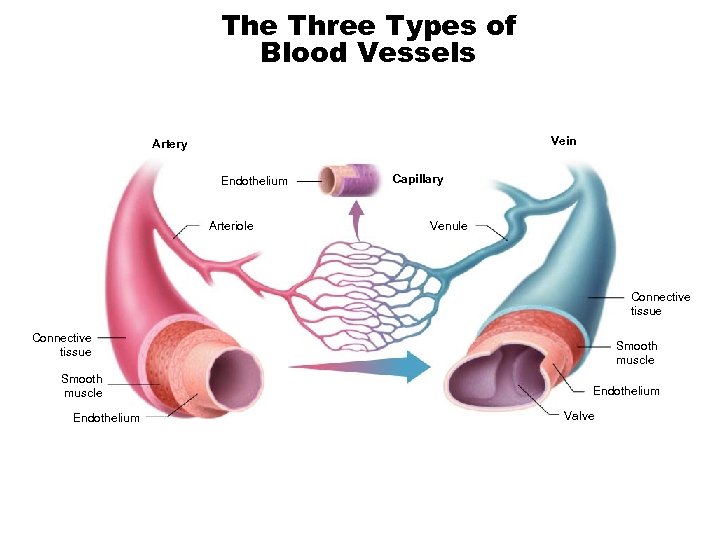 The Three Types of Blood Vessels Vein Artery Endothelium Arteriole Capillary Venule Connective tissue Smooth muscle Endothelium Valve
The Three Types of Blood Vessels Vein Artery Endothelium Arteriole Capillary Venule Connective tissue Smooth muscle Endothelium Valve

 III. Common heart problems and their treatment A. Atherosclerosis: disease characterized by buildup of fatty materials on the interior walls of arteries called plaque (lipids, cholesterol, cell debris, and calcium 1. Can block or reduce flow of blood to the heart and cause the arteries to become harder and less flexible 2. Endothelium: inside lining of artery 3. Endothelium is smooth and no plaque in young person 4. Build-up of plaque due to genetics and eating habits
III. Common heart problems and their treatment A. Atherosclerosis: disease characterized by buildup of fatty materials on the interior walls of arteries called plaque (lipids, cholesterol, cell debris, and calcium 1. Can block or reduce flow of blood to the heart and cause the arteries to become harder and less flexible 2. Endothelium: inside lining of artery 3. Endothelium is smooth and no plaque in young person 4. Build-up of plaque due to genetics and eating habits
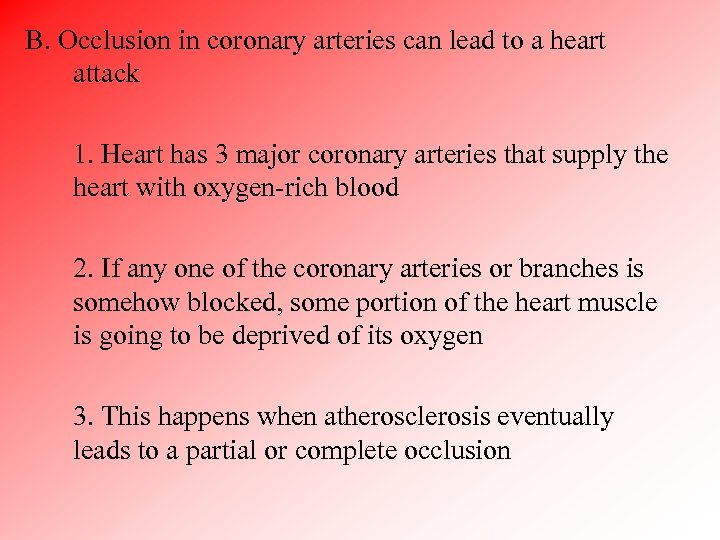 B. Occlusion in coronary arteries can lead to a heart attack 1. Heart has 3 major coronary arteries that supply the heart with oxygen-rich blood 2. If any one of the coronary arteries or branches is somehow blocked, some portion of the heart muscle is going to be deprived of its oxygen 3. This happens when atherosclerosis eventually leads to a partial or complete occlusion
B. Occlusion in coronary arteries can lead to a heart attack 1. Heart has 3 major coronary arteries that supply the heart with oxygen-rich blood 2. If any one of the coronary arteries or branches is somehow blocked, some portion of the heart muscle is going to be deprived of its oxygen 3. This happens when atherosclerosis eventually leads to a partial or complete occlusion
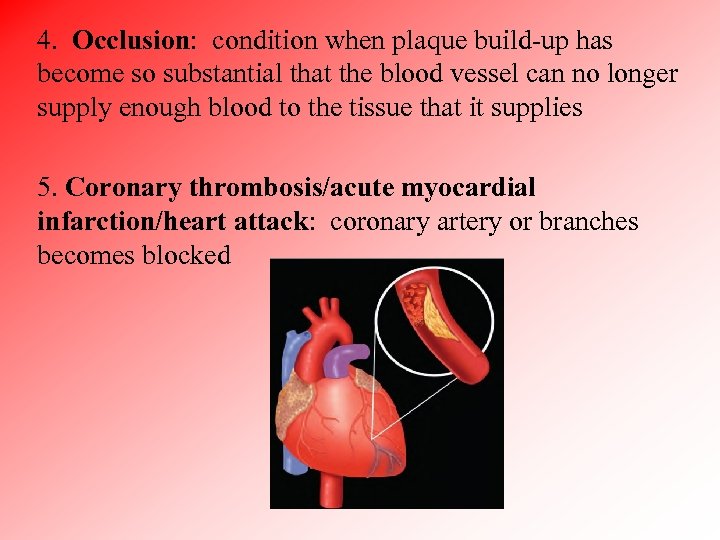 4. Occlusion: condition when plaque build-up has become so substantial that the blood vessel can no longer supply enough blood to the tissue that it supplies 5. Coronary thrombosis/acute myocardial infarction/heart attack: coronary artery or branches becomes blocked
4. Occlusion: condition when plaque build-up has become so substantial that the blood vessel can no longer supply enough blood to the tissue that it supplies 5. Coronary thrombosis/acute myocardial infarction/heart attack: coronary artery or branches becomes blocked
 C. Use of defibrillation device 1. Person with a heart attack may have a cardiac arrest (heart has stopped) or arrhythmia (heart that is not in sequence with set of typical electrical impulses) 2. Both cases the blood is not being pumped effectively to organs 3. Defibrillation: process carried out using a device that delivers an electric shock to the heart to reset the electrical signals with the SA node
C. Use of defibrillation device 1. Person with a heart attack may have a cardiac arrest (heart has stopped) or arrhythmia (heart that is not in sequence with set of typical electrical impulses) 2. Both cases the blood is not being pumped effectively to organs 3. Defibrillation: process carried out using a device that delivers an electric shock to the heart to reset the electrical signals with the SA node
 4. If successful, the heart will continue beating on its own 5. Automated external defibrillators (AEDs): small portable defibrillators are carried by medical first responders and are in areas like schools, sports stadium, shopping centers a) Audible instructions are given through the machine so anyone can use the machine to help someone
4. If successful, the heart will continue beating on its own 5. Automated external defibrillators (AEDs): small portable defibrillators are carried by medical first responders and are in areas like schools, sports stadium, shopping centers a) Audible instructions are given through the machine so anyone can use the machine to help someone
 D. Use of artificial pacemakers to regulate heart rate 1. Artificial pacemaker: small battery-operated device that is implanted under the skin in the upper chest 2. Function is to set the heart rate in the same as a healthy SA node 3. Connected to wires (leads) that are threaded into a blood vessel that leads into the interior of the heart and the placement of the leads depends on the patient’s problem 4. Device delivers a small electrical shock at regular intervals to trigger a cardiac cycle
D. Use of artificial pacemakers to regulate heart rate 1. Artificial pacemaker: small battery-operated device that is implanted under the skin in the upper chest 2. Function is to set the heart rate in the same as a healthy SA node 3. Connected to wires (leads) that are threaded into a blood vessel that leads into the interior of the heart and the placement of the leads depends on the patient’s problem 4. Device delivers a small electrical shock at regular intervals to trigger a cardiac cycle
 5. Used in patients with slow heart rates, fast heart rates, irregular heartbeats, and other problems 6. Batteries last 7 years and then a new pacemaker is usually given
5. Used in patients with slow heart rates, fast heart rates, irregular heartbeats, and other problems 6. Batteries last 7 years and then a new pacemaker is usually given
 E. Thrombosis: condition in which a clot (thrombus) forms within a blood vessel 1. Deep vein thrombosis (DVT): thrombus develops in one of the larger veins (usually leg) and often occurs when a person has been sitting for a long time (plane or car) a) Dangerous when the clot breaks loose and travels to smaller veins when total blockage can occur b) Especially dangerous when clot gets into the lungs
E. Thrombosis: condition in which a clot (thrombus) forms within a blood vessel 1. Deep vein thrombosis (DVT): thrombus develops in one of the larger veins (usually leg) and often occurs when a person has been sitting for a long time (plane or car) a) Dangerous when the clot breaks loose and travels to smaller veins when total blockage can occur b) Especially dangerous when clot gets into the lungs
 c) Treated with anticoagulant medications (blood thinners): do not actually “thin” the blood but it helps prevent blood clotting from occurring as quickly 2. Coronary thrombosis: thrombus occurs in coronary arteries that are used to deliver blood to the heart muscle cells a) Plaque can build up in one or more of the coronary arteries to the point where a substantial narrowing of the lumen (inside) of the artery occurs b) Can lead to myocardial infarction (heart attack)
c) Treated with anticoagulant medications (blood thinners): do not actually “thin” the blood but it helps prevent blood clotting from occurring as quickly 2. Coronary thrombosis: thrombus occurs in coronary arteries that are used to deliver blood to the heart muscle cells a) Plaque can build up in one or more of the coronary arteries to the point where a substantial narrowing of the lumen (inside) of the artery occurs b) Can lead to myocardial infarction (heart attack)
 F. Hypertension: higher than “normal” blood pressure 1. No single blood pressure value that is the norm, since a person’s blood pressure can be highly variable depending on many factors, so it is important to monitor blood pressure for increasing trend 2. Blood pressure measures the force of the blood pushing outwards on the wall of the arteries a) More blood your heart pumps, and the narrower your arteries, the higher the blood pressure
F. Hypertension: higher than “normal” blood pressure 1. No single blood pressure value that is the norm, since a person’s blood pressure can be highly variable depending on many factors, so it is important to monitor blood pressure for increasing trend 2. Blood pressure measures the force of the blood pushing outwards on the wall of the arteries a) More blood your heart pumps, and the narrower your arteries, the higher the blood pressure
 3. Loss of elasticity and build-up of plaque are the main causes of hypertension 4. Blood pressure reading: 115 (systolic) 68 (diastolic) a) Units are mm of Hg b) Systolic: pressure in the arteries when heart contracts c) Diastolic: pressure in arteries when heart is resting and refilling with blood
3. Loss of elasticity and build-up of plaque are the main causes of hypertension 4. Blood pressure reading: 115 (systolic) 68 (diastolic) a) Units are mm of Hg b) Systolic: pressure in the arteries when heart contracts c) Diastolic: pressure in arteries when heart is resting and refilling with blood

 G. Risk factors affecting coronary heart disease 1. Coronary heart disease (CHD): slow progression of plaque build-up in arteries and the problems that can result a) Can have CHD for many years without obvious symptoms b) Factors that determine plaque build-up are in two categories (those that cannot be controlled and that can be controlled)
G. Risk factors affecting coronary heart disease 1. Coronary heart disease (CHD): slow progression of plaque build-up in arteries and the problems that can result a) Can have CHD for many years without obvious symptoms b) Factors that determine plaque build-up are in two categories (those that cannot be controlled and that can be controlled)
 2. Difficult to measure the effects of any one factor and its impact on other factors and the incidence of CHD a) Overweight people often have problems with high blood pressure and cholesterol b) Sedentary lifestyle may lead to obesity c) Stress may lead to smoking and overeating and thus high blood pressure and cholesterol problems
2. Difficult to measure the effects of any one factor and its impact on other factors and the incidence of CHD a) Overweight people often have problems with high blood pressure and cholesterol b) Sedentary lifestyle may lead to obesity c) Stress may lead to smoking and overeating and thus high blood pressure and cholesterol problems
 i. Pad Activities Human • My human (upper left) • Heart anatomy • Rotate, tap, click the scalpel to dissect • Lines on bottom will bring up a description Build a body • Circulatory system Visible Body Atlas • Animations • Heart function Human body: Girl • Go to heart
i. Pad Activities Human • My human (upper left) • Heart anatomy • Rotate, tap, click the scalpel to dissect • Lines on bottom will bring up a description Build a body • Circulatory system Visible Body Atlas • Animations • Heart function Human body: Girl • Go to heart
 III. Blood A. Composition of blood: liquid medium and blood solids: 4 -5 Liters of blood in body 1. Plasma: liquid medium that is sticky and strawcolored a) 90% water b) 10% vitamins, minerals, hormones, waste products, and proteins
III. Blood A. Composition of blood: liquid medium and blood solids: 4 -5 Liters of blood in body 1. Plasma: liquid medium that is sticky and strawcolored a) 90% water b) 10% vitamins, minerals, hormones, waste products, and proteins
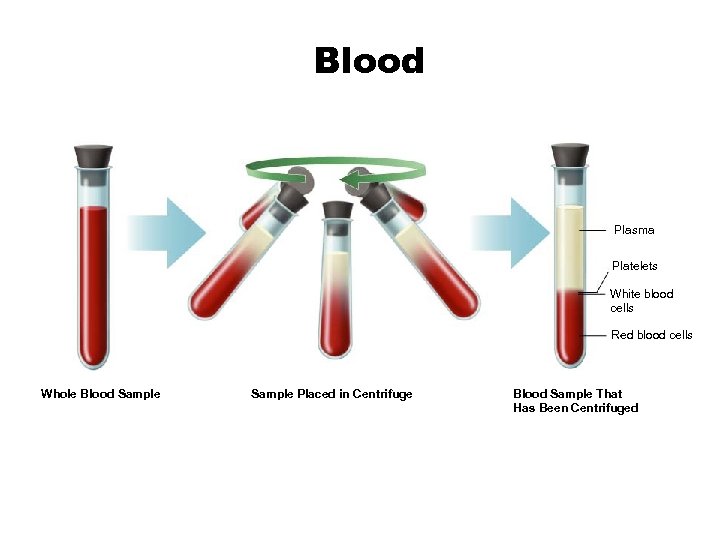 Blood Plasma Platelets White blood cells Red blood cells Whole Blood Sample Placed in Centrifuge Blood Sample That Has Been Centrifuged
Blood Plasma Platelets White blood cells Red blood cells Whole Blood Sample Placed in Centrifuge Blood Sample That Has Been Centrifuged
 2. Red blood cells: (erythrocytes) transport oxygen to cells in all parts of the body a) Hemoglobin: iron containing protein that transports the oxygen b) No nucleus c) Live 120 days
2. Red blood cells: (erythrocytes) transport oxygen to cells in all parts of the body a) Hemoglobin: iron containing protein that transports the oxygen b) No nucleus c) Live 120 days
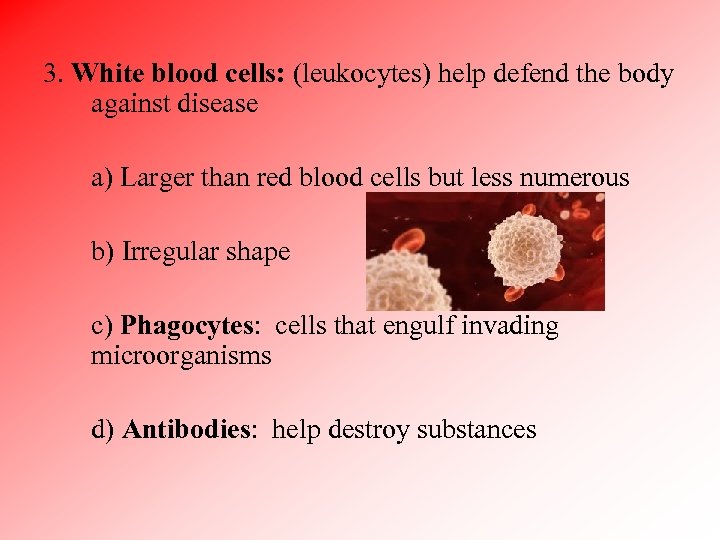 3. White blood cells: (leukocytes) help defend the body against disease a) Larger than red blood cells but less numerous b) Irregular shape c) Phagocytes: cells that engulf invading microorganisms d) Antibodies: help destroy substances
3. White blood cells: (leukocytes) help defend the body against disease a) Larger than red blood cells but less numerous b) Irregular shape c) Phagocytes: cells that engulf invading microorganisms d) Antibodies: help destroy substances
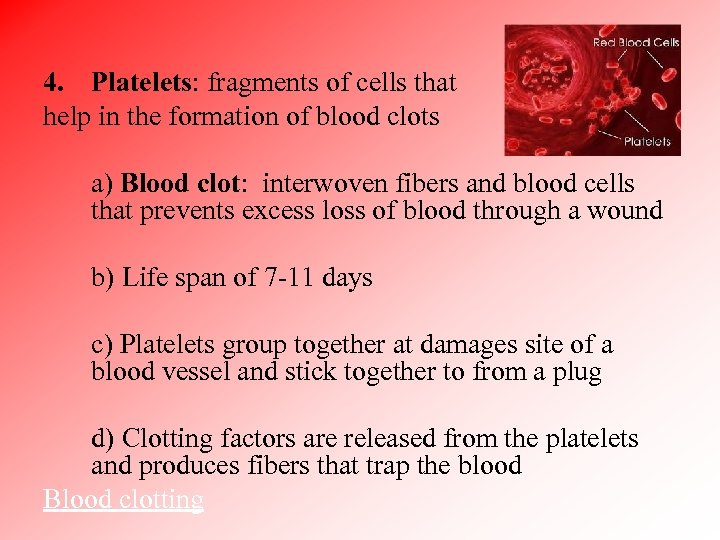 4. Platelets: fragments of cells that help in the formation of blood clots a) Blood clot: interwoven fibers and blood cells that prevents excess loss of blood through a wound b) Life span of 7 -11 days c) Platelets group together at damages site of a blood vessel and stick together to from a plug d) Clotting factors are released from the platelets and produces fibers that trap the blood Blood clotting
4. Platelets: fragments of cells that help in the formation of blood clots a) Blood clot: interwoven fibers and blood cells that prevents excess loss of blood through a wound b) Life span of 7 -11 days c) Platelets group together at damages site of a blood vessel and stick together to from a plug d) Clotting factors are released from the platelets and produces fibers that trap the blood Blood clotting
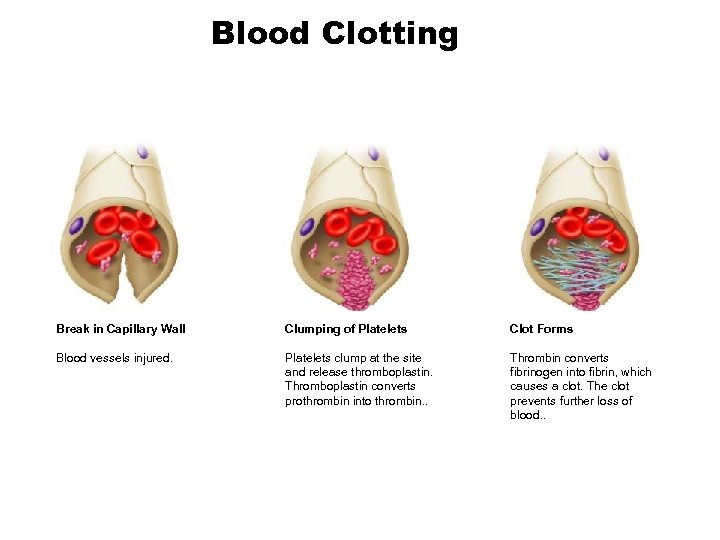 Blood Clotting Break in Capillary Wall Clumping of Platelets Clot Forms Blood vessels injured. Platelets clump at the site and release thromboplastin. Thromboplastin converts prothrombin into thrombin. . Thrombin converts fibrinogen into fibrin, which causes a clot. The clot prevents further loss of blood. .
Blood Clotting Break in Capillary Wall Clumping of Platelets Clot Forms Blood vessels injured. Platelets clump at the site and release thromboplastin. Thromboplastin converts prothrombin into thrombin. . Thrombin converts fibrinogen into fibrin, which causes a clot. The clot prevents further loss of blood. .
 B. Blood type: determined by the type of antigen present on the surface of red blood cells 1. Antigen: protein or carbohydrate that acts as a signal, enabling the body to recognize foreign substances a) Foreign antigens enters the body, the body responds by producing antibodies to fight the invaders 2. 4 groups of blood types 3. When two different blood types are mixed, reactions occur between antigen and antibodies
B. Blood type: determined by the type of antigen present on the surface of red blood cells 1. Antigen: protein or carbohydrate that acts as a signal, enabling the body to recognize foreign substances a) Foreign antigens enters the body, the body responds by producing antibodies to fight the invaders 2. 4 groups of blood types 3. When two different blood types are mixed, reactions occur between antigen and antibodies
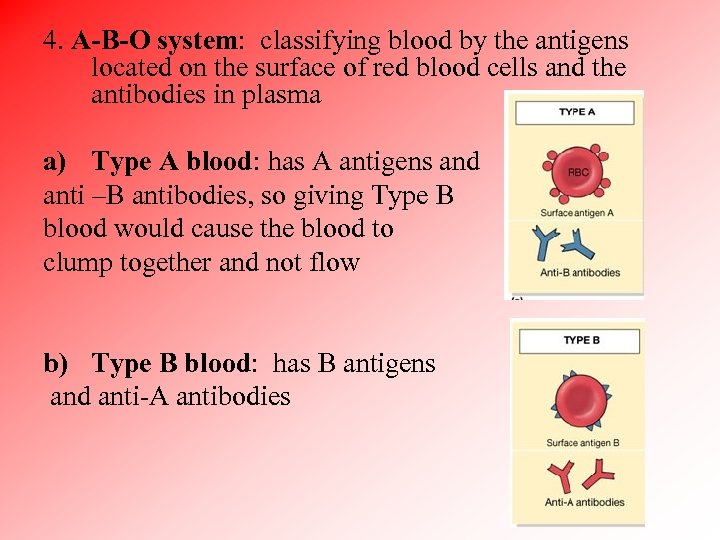 4. A-B-O system: classifying blood by the antigens located on the surface of red blood cells and the antibodies in plasma a) Type A blood: has A antigens and anti –B antibodies, so giving Type B blood would cause the blood to clump together and not flow b) Type B blood: has B antigens and anti-A antibodies
4. A-B-O system: classifying blood by the antigens located on the surface of red blood cells and the antibodies in plasma a) Type A blood: has A antigens and anti –B antibodies, so giving Type B blood would cause the blood to clump together and not flow b) Type B blood: has B antigens and anti-A antibodies
 c) Type AB: has A and B antigens and no antibodies, so can receive blood from any type d) Type O: has no antigens and anti-A and anti-B antibodies, so can get blood from just Type O, but they can give blood to all because they have no antigens
c) Type AB: has A and B antigens and no antibodies, so can receive blood from any type d) Type O: has no antigens and anti-A and anti-B antibodies, so can get blood from just Type O, but they can give blood to all because they have no antigens

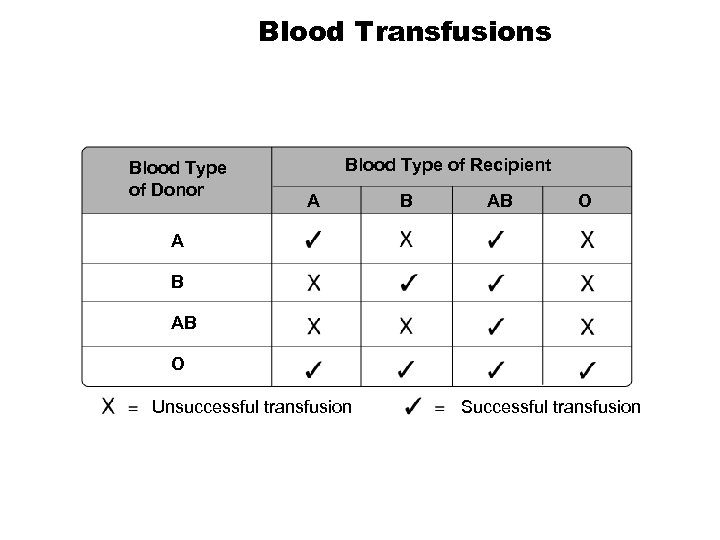 Blood Transfusions Blood Type of Donor Blood Type of Recipient A B AB O Unsuccessful transfusion Successful transfusion
Blood Transfusions Blood Type of Donor Blood Type of Recipient A B AB O Unsuccessful transfusion Successful transfusion
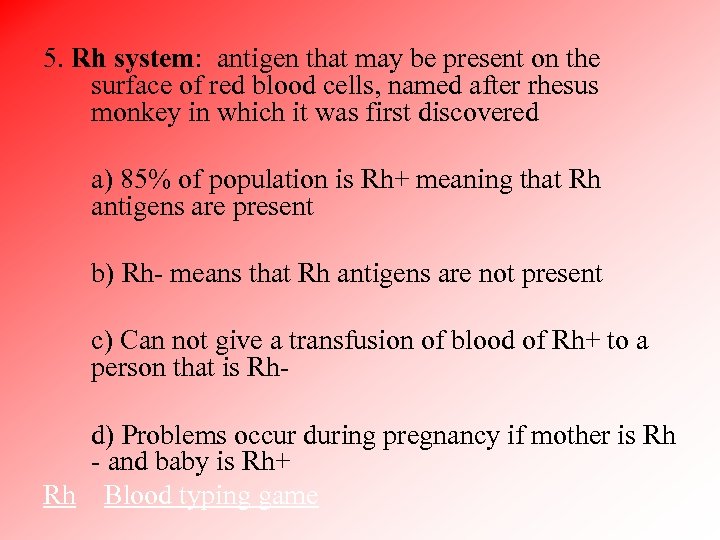 5. Rh system: antigen that may be present on the surface of red blood cells, named after rhesus monkey in which it was first discovered a) 85% of population is Rh+ meaning that Rh antigens are present b) Rh- means that Rh antigens are not present c) Can not give a transfusion of blood of Rh+ to a person that is Rhd) Problems occur during pregnancy if mother is Rh - and baby is Rh+ Rh Blood typing game
5. Rh system: antigen that may be present on the surface of red blood cells, named after rhesus monkey in which it was first discovered a) 85% of population is Rh+ meaning that Rh antigens are present b) Rh- means that Rh antigens are not present c) Can not give a transfusion of blood of Rh+ to a person that is Rhd) Problems occur during pregnancy if mother is Rh - and baby is Rh+ Rh Blood typing game



