0ca5db8c81decea7582a9a1e1cdcb8d7.ppt
- Количество слайдов: 16
Chaos Waiting for Bad Luck? Medication Reconciliation Should Be Mandatory Roni Cohen, B. Sc. , Inbal Yifrach-Damari, M. Sc. * Dr. Meir Frankel, Prof. Mayer Brezis Hadassah-Hebrew University Hospital, Jerusalem, Israel * Clinical Pharmacist, Pharmacy Division Supported by a joint non-restricted educational grant established by Pfizer, Hadassah Medical Organization and the Hebrew University School of Pharmacy Pharm-D student, School of Pharmacy, Hebrew University With Help From Joint Commission International
Medication Errors · Medication errors are the fourth leading cause of death or major permanent loss of function in hospital patients. · The majority of problems with patient safety occur during the transition from one care setting to another. · Ambulatory-hospital lack of communication is responsible for 50% of medical errors. · To improve patient safety, the Joint Commission on Accreditation of Healthcare Organizations now recommends a procedure designed to minimize errors.
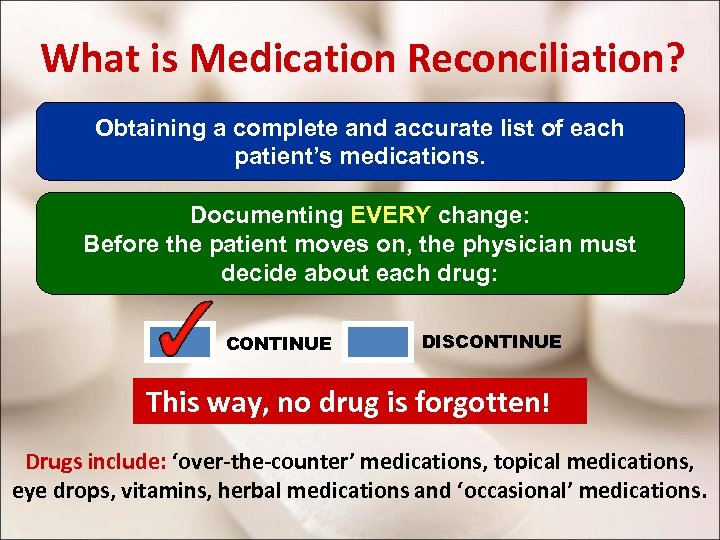
What is Medication Reconciliation? Obtaining a complete and accurate list of each patient’s medications. Documenting EVERY change: Before the patient moves on, the physician must decide about each drug: CONTINUE DISCONTINUE This way, no drug is forgotten! Drugs include: ‘over-the-counter’ medications, topical medications, eye drops, vitamins, herbal medications and ‘occasional’ medications.
Methods for current project · Over 100 adult patients admitted to the ER, on at least 5 regular drugs, underwent medication reconciliation. · Review of medications with patient, family, primary physician and/or database of HMOs (sick funds). · After 24 -48 hours, we checked the list of medications prescribed to the patient by the ward staff. · Our list was then compared with the list in the ward. · If any discrepancy was observed or an error was suspected, the staff was approached to clarify the reason for the change.
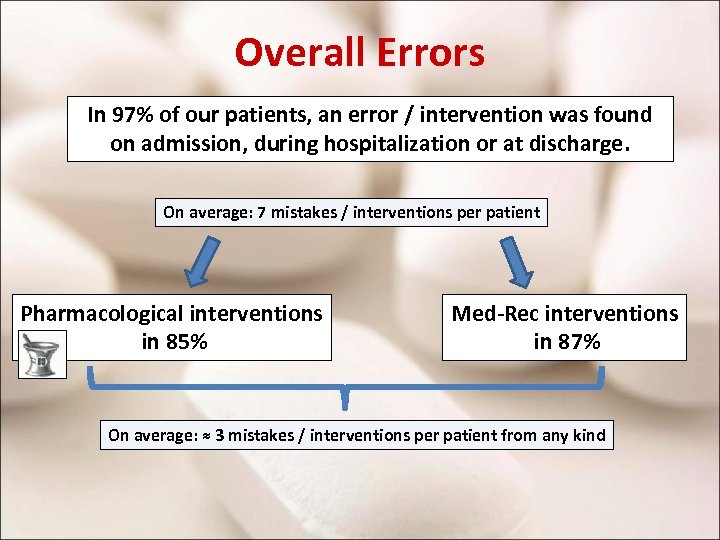
Overall Errors In 97% of our patients, an error / intervention was found on admission, during hospitalization or at discharge. On average: 7 mistakes / interventions per patient Pharmacological interventions in 85% Med-Rec interventions in 87% On average: ≈ 3 mistakes / interventions per patient from any kind
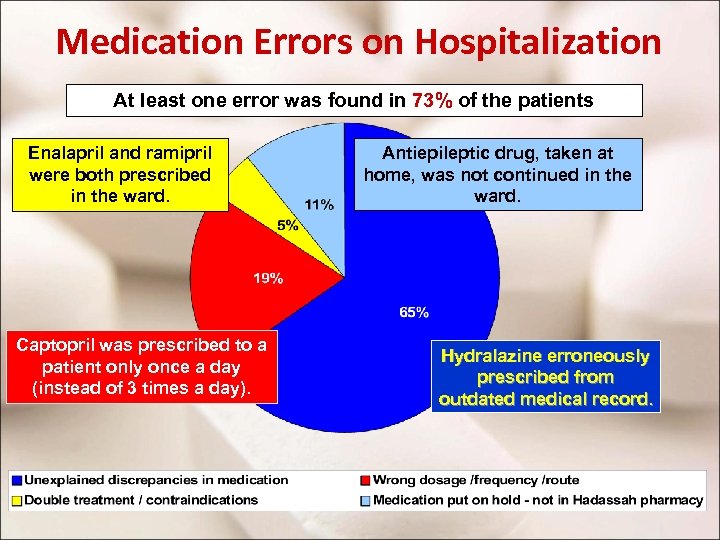
Medication Errors on Hospitalization At least one error was found in 73% of the patients Enalapril and ramipril were both prescribed in the ward. Captopril was prescribed to a patient only once a day (instead of 3 times a day). Antiepileptic drug, taken at home, was not continued in the ward. Hydralazine erroneously prescribed from outdated medical record.
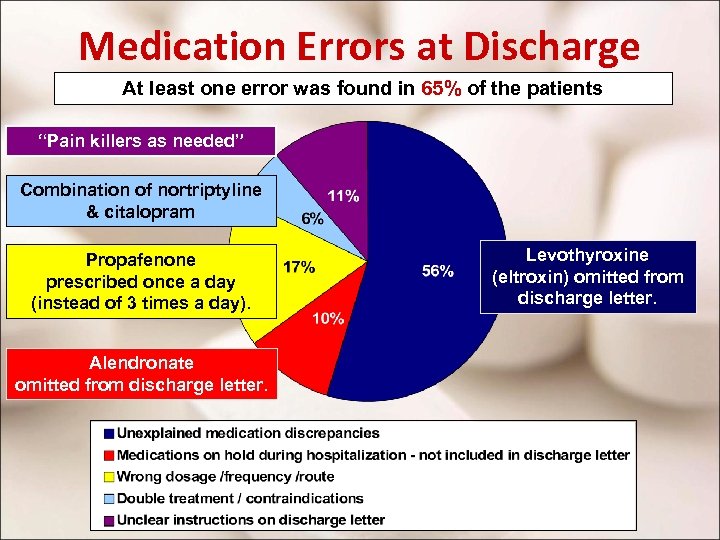
Medication Errors at Discharge At least one error was found in 65% of the patients “Pain killers as needed” Combination of nortriptyline & citalopram Propafenone prescribed once a day (instead of 3 times a day). Alendronate omitted from discharge letter. Levothyroxine (eltroxin) omitted from discharge letter.
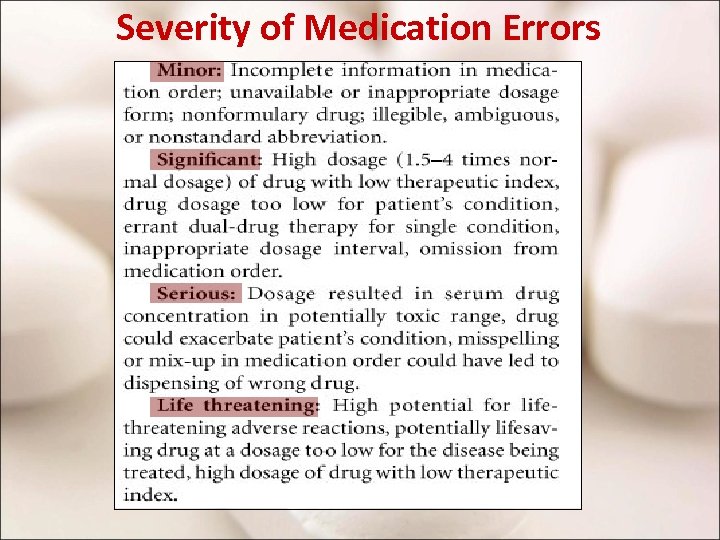
Severity of Medication Errors
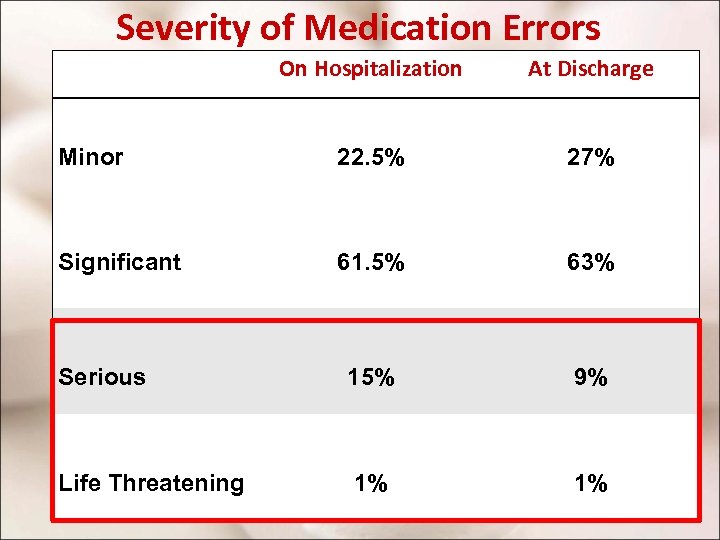
Severity of Medication Errors On Hospitalization At Discharge Minor 22. 5% 27% Significant 61. 5% 63% Serious 15% 9% Life Threatening 1% 1%
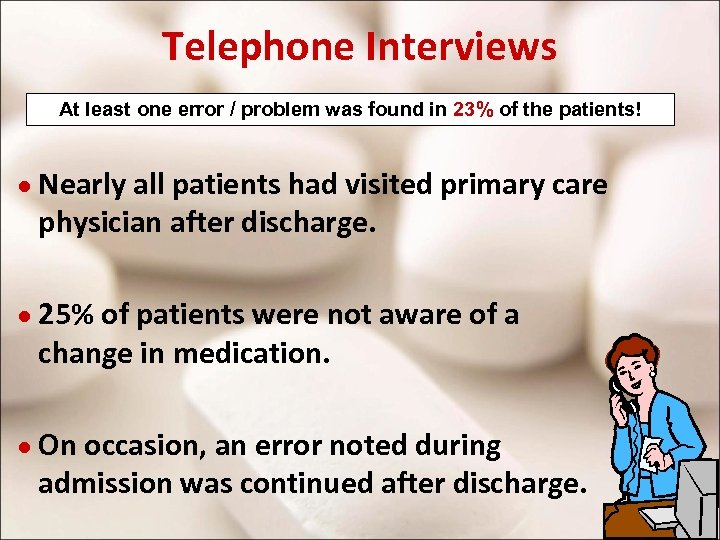
Telephone Interviews At least one error / problem was found in 23% of the patients! ● Nearly all patients had visited primary care physician after discharge. ● 25% of patients were not aware of a change in medication. ● On occasion, an error noted during admission was continued after discharge.
Clinical Pharmacist Service In 85% of patients: • Apply correct indications and contra-indications (≈18%). • Adapt dosage to kidney or liver function (≈15%). • Drug-Drug Interaction (≈37%). • Correct administration: discharge, over 50% of patients were not taking medications correctly. After Polypharmacy
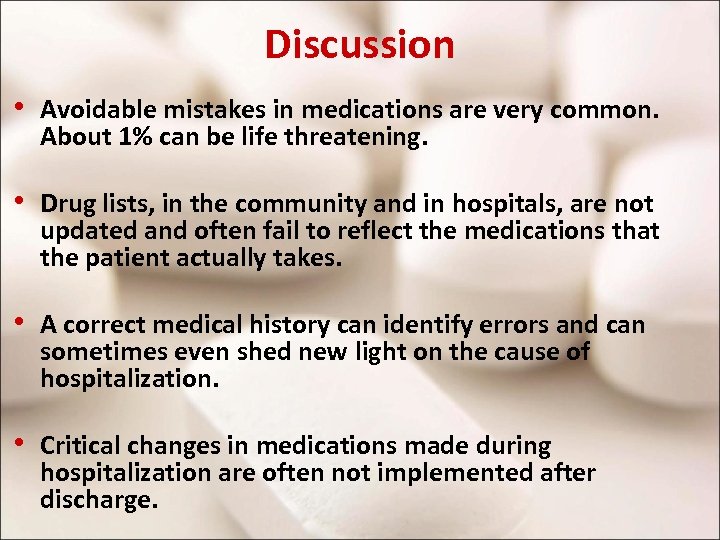
Discussion • Avoidable mistakes in medications are very common. About 1% can be life threatening. • Drug lists, in the community and in hospitals, are not updated and often fail to reflect the medications that the patient actually takes. • A correct medical history can identify errors and can sometimes even shed new light on the cause of hospitalization. • Critical changes in medications made during hospitalization are often not implemented after discharge.
On Medication-Reconciliation Elsewhere Survey of 100 patients at the Mayo Clinic: Inpatient Medication Reconciliation in an Academic Setting American Journal of Health. System Pharmacy 2007 Number of medication discrepancies decreased from 3 per patient in phase 1 to 1. 8 per patient in phase 2 (p = 0. 003) Survey of 180 patients at Brigham and Women’s Hospital, in Boston: Classifying and Predicting Errors of Inpatient Medication Reconciliation. J Gen Intern Med 2008. Ave rage of 1. 5 error per patient with potential for harm. Solutions included development of special software for adapting prescription to the patient’s provider preferred medications outside hospital.
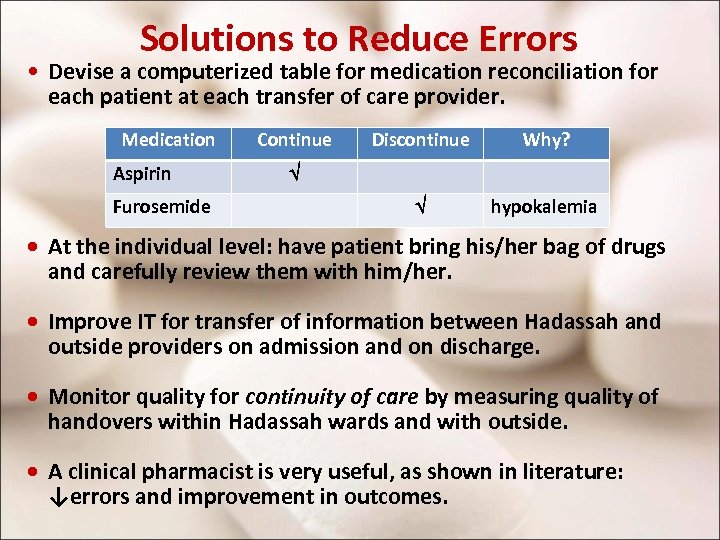
Solutions to Reduce Errors • Devise a computerized table for medication reconciliation for each patient at each transfer of care provider. Medication Aspirin Furosemide Continue Discontinue Why? hypokalemia · At the individual level: have patient bring his/her bag of drugs and carefully review them with him/her. · Improve IT for transfer of information between Hadassah and outside providers on admission and on discharge. · Monitor quality for continuity of care by measuring quality of handovers within Hadassah wards and with outside. · A clinical pharmacist is very useful, as shown in literature: ↓errors and improvement in outcomes.
Conclusion Medication Reconciliation Should Be Mandatory!
Special thanks to Ms. Lois Gordon for graphics assistance.
0ca5db8c81decea7582a9a1e1cdcb8d7.ppt