d85250ba7cf1e6bd38fa92dd0e625505.ppt
- Количество слайдов: 48
 Challenges in Clinical Documentation: Stories from the Front Line Jon Elion MD, FACC Associate Professor of Medicine, Brown University President and CEO, Chart. Wise Medical Systems j. Elion@chartwisemed. com
Challenges in Clinical Documentation: Stories from the Front Line Jon Elion MD, FACC Associate Professor of Medicine, Brown University President and CEO, Chart. Wise Medical Systems j. Elion@chartwisemed. com
 Jon Elion MD, FACC Five Things to Know about Jon… Jon Elion, M. D. , FACC 1. Medical Computing: Since 1969 2. Clinical: Duke-trained cardiologist 3. Academic: Assoc Prof at Brown 4. Administration: Hospital Boards, Foundation and Finance Committees 5. Commercial: Medical software since 1994. Now President and CEO of Chart. Wise Medical Systems (Computer-Assisted Clinical Documentation Improvement).
Jon Elion MD, FACC Five Things to Know about Jon… Jon Elion, M. D. , FACC 1. Medical Computing: Since 1969 2. Clinical: Duke-trained cardiologist 3. Academic: Assoc Prof at Brown 4. Administration: Hospital Boards, Foundation and Finance Committees 5. Commercial: Medical software since 1994. Now President and CEO of Chart. Wise Medical Systems (Computer-Assisted Clinical Documentation Improvement).

 Clinical Documentation should be a thorough record of the diagnos(es) made, symptoms observed, treatment procedure planned and executed, the care provided, the outcome of treatment and clinical assessment of the entire treatment process. * *From “Guidelines for Improvement in Clinical Documentation” by Tom Bilmore; http: //Ezine. Articles/5034354
Clinical Documentation should be a thorough record of the diagnos(es) made, symptoms observed, treatment procedure planned and executed, the care provided, the outcome of treatment and clinical assessment of the entire treatment process. * *From “Guidelines for Improvement in Clinical Documentation” by Tom Bilmore; http: //Ezine. Articles/5034354
 Clinical Documentation Improvement …improve the accuracy, specificity and completeness of clinical documentation through education, assessment, review, communication, clarification, querying and analysis of clinical documentation patterns…* *From Catholic Health. Care West Clinical Documentation Improvement Program
Clinical Documentation Improvement …improve the accuracy, specificity and completeness of clinical documentation through education, assessment, review, communication, clarification, querying and analysis of clinical documentation patterns…* *From Catholic Health. Care West Clinical Documentation Improvement Program
 Clinical Documentation Specialist …Assess the accuracy, specificity and completeness of physician clinical documentation and to identify if clinical findings suggest the presence of other conditions that are not explicitly documented…* *From Catholic Health. Care West Clinical Documentation Improvement Program
Clinical Documentation Specialist …Assess the accuracy, specificity and completeness of physician clinical documentation and to identify if clinical findings suggest the presence of other conditions that are not explicitly documented…* *From Catholic Health. Care West Clinical Documentation Improvement Program
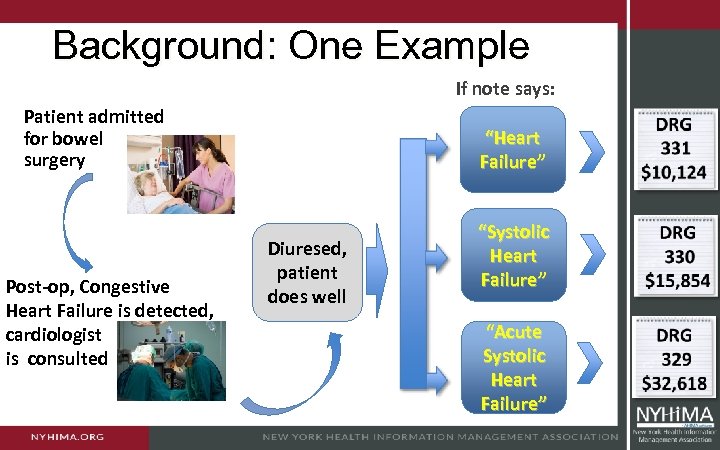 Background: One Example If note says: Patient admitted for bowel surgery Post-op, Congestive Heart Failure is detected, cardiologist is consulted “Heart Failure” Diuresed, patient does well “Systolic Heart Failure” “Acute Systolic Heart Failure”
Background: One Example If note says: Patient admitted for bowel surgery Post-op, Congestive Heart Failure is detected, cardiologist is consulted “Heart Failure” Diuresed, patient does well “Systolic Heart Failure” “Acute Systolic Heart Failure”

 It’s All About Quality… If you pursue reimbursement, you will miss the High Quality Medical Record … but. . . If you pursue the High Quality Medical Record, the proper reimbursement will follow.
It’s All About Quality… If you pursue reimbursement, you will miss the High Quality Medical Record … but. . . If you pursue the High Quality Medical Record, the proper reimbursement will follow.
 …Not Just About Reimbursement Complete and accurate coded data is essential for: ü Improved quality of patient care ü Decision-making on healthcare policies ü Optimizing resource utilization ü Identifying and reducing medical errors ü Clinical research, epidemiological studies Physician documentation is the cornerstone of accurate coding
…Not Just About Reimbursement Complete and accurate coded data is essential for: ü Improved quality of patient care ü Decision-making on healthcare policies ü Optimizing resource utilization ü Identifying and reducing medical errors ü Clinical research, epidemiological studies Physician documentation is the cornerstone of accurate coding
 Don’t fall into this trap! Find an MCC and move on…
Don’t fall into this trap! Find an MCC and move on…
 What Would You Code? ü A 92 year-old woman is admitted to the Coronary Care Unit following a fall at home. She complains of chest and hip pain ü She has an elevated troponin, and her ECG shows new inferior ST elevation. ü The orthopedic resident sees the patient, reviews the xrays of the pelvis and hip. His note says “The ice cream fell off the cone”
What Would You Code? ü A 92 year-old woman is admitted to the Coronary Care Unit following a fall at home. She complains of chest and hip pain ü She has an elevated troponin, and her ECG shows new inferior ST elevation. ü The orthopedic resident sees the patient, reviews the xrays of the pelvis and hip. His note says “The ice cream fell off the cone”
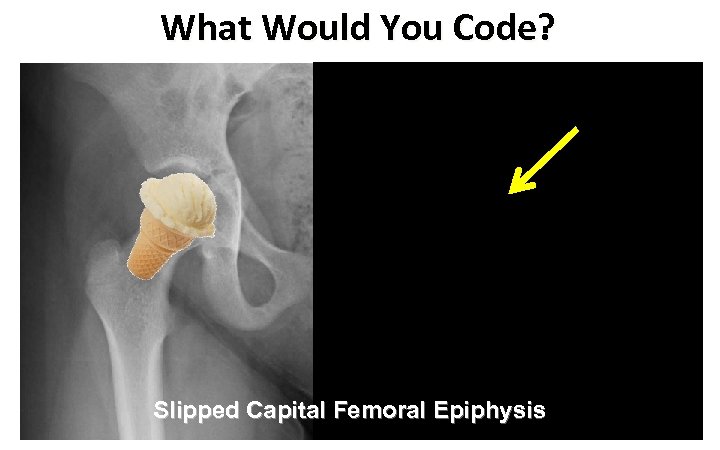 What Would You Code? Slipped Capital Femoral Epiphysis
What Would You Code? Slipped Capital Femoral Epiphysis
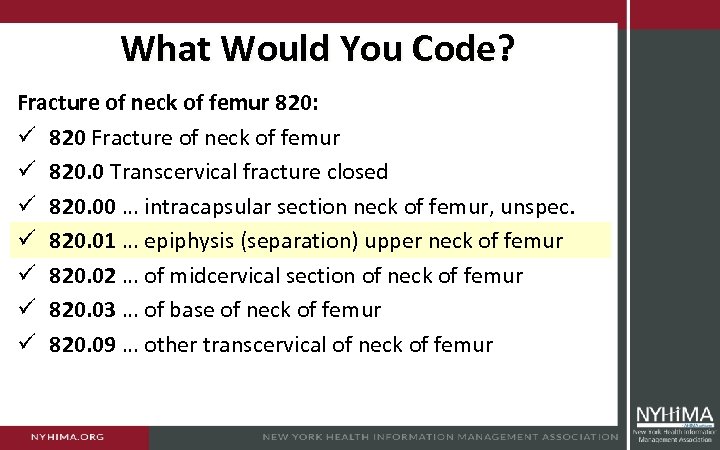 What Would You Code? Fracture of neck of femur 820: ü 820 Fracture of neck of femur ü 820. 0 Transcervical fracture closed ü 820. 00 … intracapsular section neck of femur, unspec. ü 820. 01 … epiphysis (separation) upper neck of femur ü 820. 02 … of midcervical section of neck of femur ü 820. 03 … of base of neck of femur ü 820. 09 … other transcervical of neck of femur
What Would You Code? Fracture of neck of femur 820: ü 820 Fracture of neck of femur ü 820. 0 Transcervical fracture closed ü 820. 00 … intracapsular section neck of femur, unspec. ü 820. 01 … epiphysis (separation) upper neck of femur ü 820. 02 … of midcervical section of neck of femur ü 820. 03 … of base of neck of femur ü 820. 09 … other transcervical of neck of femur
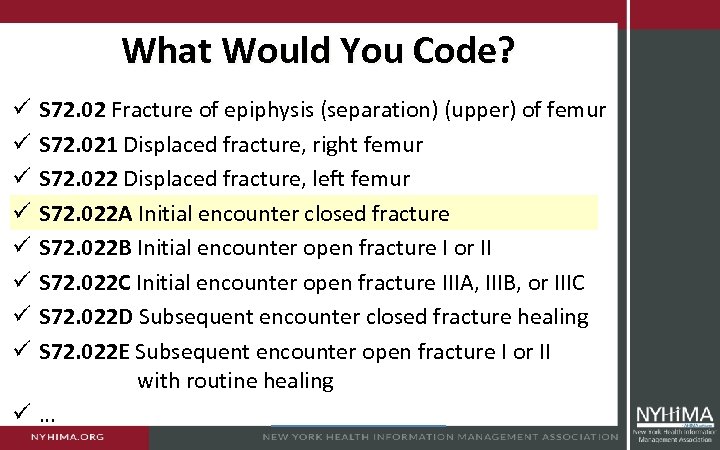 What Would You Code? S 72. 02 Fracture of epiphysis (separation) (upper) of femur S 72. 021 Displaced fracture, right femur S 72. 022 Displaced fracture, left femur S 72. 022 A Initial encounter closed fracture S 72. 022 B Initial encounter open fracture I or II S 72. 022 C Initial encounter open fracture IIIA, IIIB, or IIIC S 72. 022 D Subsequent encounter closed fracture healing S 72. 022 E Subsequent encounter open fracture I or II with routine healing ü… ü ü ü ü
What Would You Code? S 72. 02 Fracture of epiphysis (separation) (upper) of femur S 72. 021 Displaced fracture, right femur S 72. 022 Displaced fracture, left femur S 72. 022 A Initial encounter closed fracture S 72. 022 B Initial encounter open fracture I or II S 72. 022 C Initial encounter open fracture IIIA, IIIB, or IIIC S 72. 022 D Subsequent encounter closed fracture healing S 72. 022 E Subsequent encounter open fracture I or II with routine healing ü… ü ü ü ü
 Documentation: Why Should We Care?
Documentation: Why Should We Care?
 Documentation: Why Should We Care? THEY ARE WATCHING YOU!
Documentation: Why Should We Care? THEY ARE WATCHING YOU!
 Documentation: Why Should We Care? • A patient with cholecystitis undergoes a cholecystectomy • Post-op, the patient spikes a temperature with high WBC • Abdomen tender, diffuse rebound, pulse 110, respirations 22 • KUB and abdominal CT unremarkable • IV Cipro started, Infectious Disease consulted • Patient improves, is discharged on post-op day 6 on oral Cipro
Documentation: Why Should We Care? • A patient with cholecystitis undergoes a cholecystectomy • Post-op, the patient spikes a temperature with high WBC • Abdomen tender, diffuse rebound, pulse 110, respirations 22 • KUB and abdominal CT unremarkable • IV Cipro started, Infectious Disease consulted • Patient improves, is discharged on post-op day 6 on oral Cipro
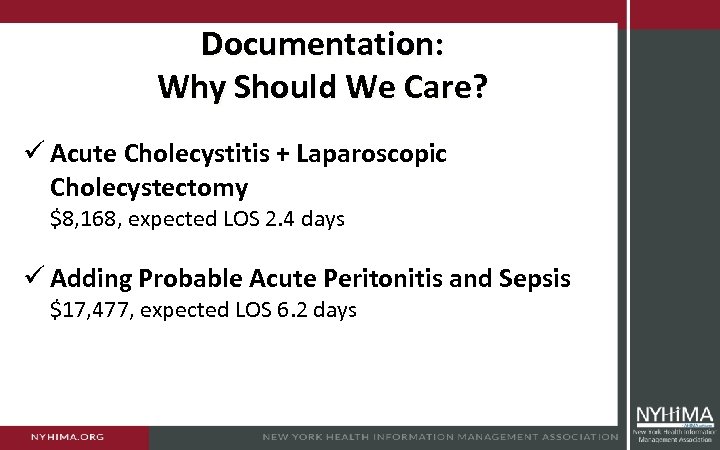 Documentation: Why Should We Care? ü Acute Cholecystitis + Laparoscopic Cholecystectomy $8, 168, expected LOS 2. 4 days ü Adding Probable Acute Peritonitis and Sepsis $17, 477, expected LOS 6. 2 days
Documentation: Why Should We Care? ü Acute Cholecystitis + Laparoscopic Cholecystectomy $8, 168, expected LOS 2. 4 days ü Adding Probable Acute Peritonitis and Sepsis $17, 477, expected LOS 6. 2 days
 Documentation: Why Should We Care? United Healthcare dropping R. I. doctors from Medicare Advantage network October 21, 2013
Documentation: Why Should We Care? United Healthcare dropping R. I. doctors from Medicare Advantage network October 21, 2013
 What Would You Code? ü One of the great mentalists of 1800 s ü A frenetic performance, culminating in a “catalectic fit” ü A note in his pocket stated his catatonic state was not death ü After a fit at a performance in 1889 he was promptly autopsied ü His death certificate officially read “hysterocatalepsy” Washington Irving Bishop 1855 – 1889
What Would You Code? ü One of the great mentalists of 1800 s ü A frenetic performance, culminating in a “catalectic fit” ü A note in his pocket stated his catatonic state was not death ü After a fit at a performance in 1889 he was promptly autopsied ü His death certificate officially read “hysterocatalepsy” Washington Irving Bishop 1855 – 1889
 FYI: Hysterocatalepsy ü Psychogenic non-epileptic seizures are events superficially resembling an epileptic seizure, but without the characteristic electrical discharges associated with epilepsy ü ICD 9: 780. 39 Other Convulsions ü ICD 9: 300. 11 Conversion Disorder ü ICD 10: F 44. 5 Dissociative Convulsions ü Death by Autopsy ? ? ? ü Did they use ICD 1 in 1889 ? ? ?
FYI: Hysterocatalepsy ü Psychogenic non-epileptic seizures are events superficially resembling an epileptic seizure, but without the characteristic electrical discharges associated with epilepsy ü ICD 9: 780. 39 Other Convulsions ü ICD 9: 300. 11 Conversion Disorder ü ICD 10: F 44. 5 Dissociative Convulsions ü Death by Autopsy ? ? ? ü Did they use ICD 1 in 1889 ? ? ?
 Think ICD-10 is Taking a Long Time? ü 1853: The 1 st International Statistical Congress: Resolution requesting the preparation of a uniform classification of causes of death ü 1891: The International Statistical Institute (successor to the International Statistical Congress), charged a committee with the preparation of a classification of causes of death ü 1893: The report of this committee was adopted by the International Statistical Institute ü For all practical purposes, this was “ICD 1” (but never called that)
Think ICD-10 is Taking a Long Time? ü 1853: The 1 st International Statistical Congress: Resolution requesting the preparation of a uniform classification of causes of death ü 1891: The International Statistical Institute (successor to the International Statistical Congress), charged a committee with the preparation of a classification of causes of death ü 1893: The report of this committee was adopted by the International Statistical Institute ü For all practical purposes, this was “ICD 1” (but never called that)
 Near-Death by Autopsy? ü Best remembered for “Paget’s Disease” of the bone ü Considered as the founder of scientific medical pathology ü Developed septicemia after a self-inflicted injury during autopsy ü Thereafter he claimed that he was the first person ever to survive the attention of 10 doctors Sir James Paget 1814 – 1899
Near-Death by Autopsy? ü Best remembered for “Paget’s Disease” of the bone ü Considered as the founder of scientific medical pathology ü Developed septicemia after a self-inflicted injury during autopsy ü Thereafter he claimed that he was the first person ever to survive the attention of 10 doctors Sir James Paget 1814 – 1899
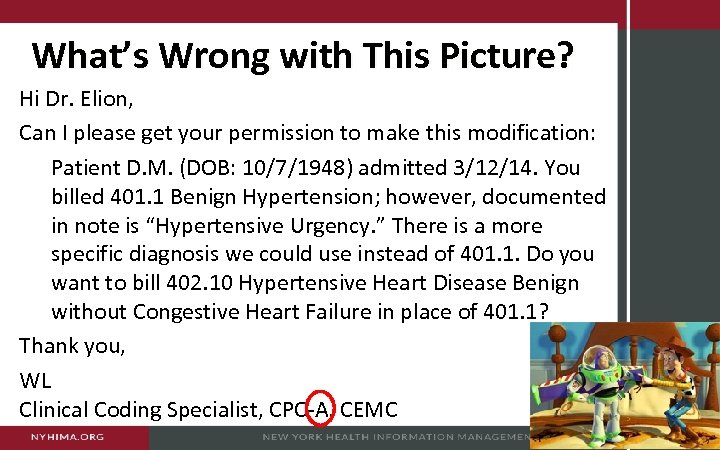 What’s Wrong with This Picture? Hi Dr. Elion, Can I please get your permission to make this modification: Patient D. M. (DOB: 10/7/1948) admitted 3/12/14. You billed 401. 1 Benign Hypertension; however, documented in note is “Hypertensive Urgency. ” There is a more specific diagnosis we could use instead of 401. 1. Do you want to bill 402. 10 Hypertensive Heart Disease Benign without Congestive Heart Failure in place of 401. 1? Thank you, WL Clinical Coding Specialist, CPC-A, CEMC
What’s Wrong with This Picture? Hi Dr. Elion, Can I please get your permission to make this modification: Patient D. M. (DOB: 10/7/1948) admitted 3/12/14. You billed 401. 1 Benign Hypertension; however, documented in note is “Hypertensive Urgency. ” There is a more specific diagnosis we could use instead of 401. 1. Do you want to bill 402. 10 Hypertensive Heart Disease Benign without Congestive Heart Failure in place of 401. 1? Thank you, WL Clinical Coding Specialist, CPC-A, CEMC
 My Reply There is no corresponding ICD 9 code for “Hypertensive Urgency”. If signs of current or impending end-organ damage, then it is one of the variations of “malignant” hypertension. Without that, it is Essential Hypertension, 401. 1. In order the have 402. 10 Hypertensive Heart Disease, there would need to be evidence that the heart was involved in the hypertension process. The echo done January 22, 2014 says: “The left ventricle chamber size, wall thickness, and systolic function are within normal limits” So the patient would not qualify for 402. 10
My Reply There is no corresponding ICD 9 code for “Hypertensive Urgency”. If signs of current or impending end-organ damage, then it is one of the variations of “malignant” hypertension. Without that, it is Essential Hypertension, 401. 1. In order the have 402. 10 Hypertensive Heart Disease, there would need to be evidence that the heart was involved in the hypertension process. The echo done January 22, 2014 says: “The left ventricle chamber size, wall thickness, and systolic function are within normal limits” So the patient would not qualify for 402. 10
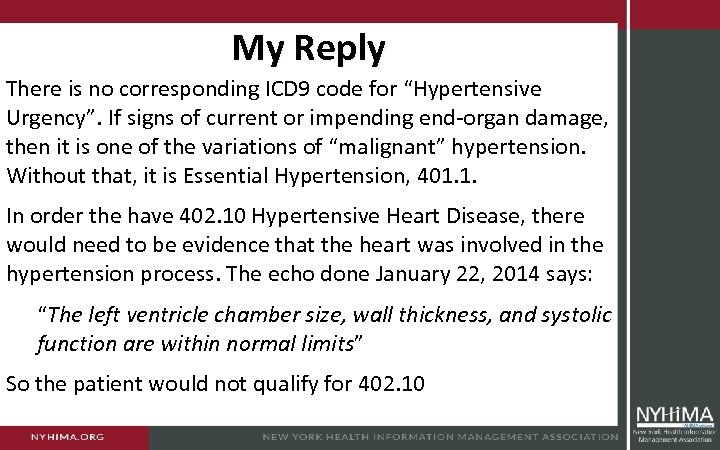
 What’s Wrong with This Picture?
What’s Wrong with This Picture?
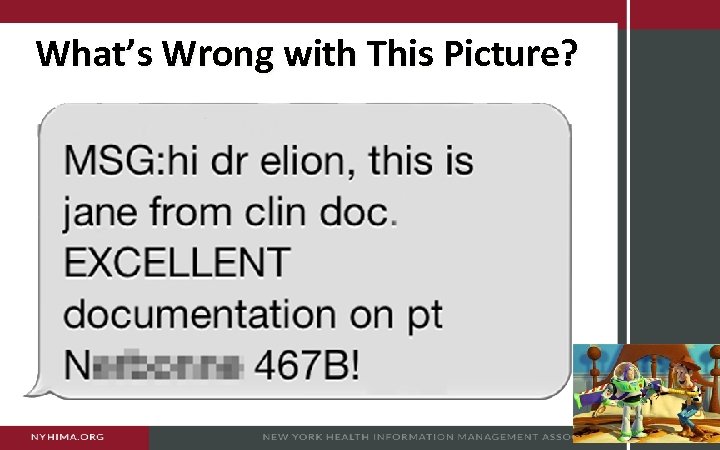
 Due To This patient is known to have severe Aortic Stenosis. Her downhill slide is probably due to dietary indiscretion (she does not follow her diet). She is symptomatically much improved after initial diuresis. Her clinical picture is consistent with acute-onchronic systolic CHF due to Aortic Stenosis.
Due To This patient is known to have severe Aortic Stenosis. Her downhill slide is probably due to dietary indiscretion (she does not follow her diet). She is symptomatically much improved after initial diuresis. Her clinical picture is consistent with acute-onchronic systolic CHF due to Aortic Stenosis.
 Query for Clarification ü Query physicians for clarification and additional documentation when there is conflicting, incomplete, or ambiguous information in the record ü Do not query: Ø when there is no supporting clinical information Ø for gram-negative pneumonia on every pneumonia case, regardless of clinical indicators Ø for sepsis when the clinical indicators are only suggestive of UTI + fever + increased WBCs
Query for Clarification ü Query physicians for clarification and additional documentation when there is conflicting, incomplete, or ambiguous information in the record ü Do not query: Ø when there is no supporting clinical information Ø for gram-negative pneumonia on every pneumonia case, regardless of clinical indicators Ø for sepsis when the clinical indicators are only suggestive of UTI + fever + increased WBCs
 When to Query ü Legibility: Illegible handwritten notes, and cannot determine the provider’s assessment ü Completeness: For example, an abnormal test results without notation of the clinical significance ü Clarity: For example, diagnosis noted without statement of a cause or suspected cause ü Consistency: Disagreement between two or more providers about diagnosis ü Precision: Clinical reports and clinical condition suggest a more specific diagnosis than is documented
When to Query ü Legibility: Illegible handwritten notes, and cannot determine the provider’s assessment ü Completeness: For example, an abnormal test results without notation of the clinical significance ü Clarity: For example, diagnosis noted without statement of a cause or suspected cause ü Consistency: Disagreement between two or more providers about diagnosis ü Precision: Clinical reports and clinical condition suggest a more specific diagnosis than is documented
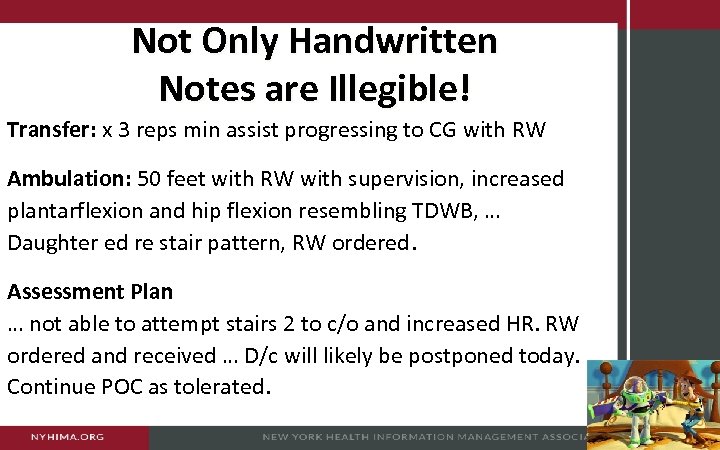 Not Only Handwritten Notes are Illegible! Transfer: x 3 reps min assist progressing to CG with RW Ambulation: 50 feet with RW with supervision, increased plantarflexion and hip flexion resembling TDWB, … Daughter ed re stair pattern, RW ordered. Assessment Plan … not able to attempt stairs 2 to c/o and increased HR. RW ordered and received … D/c will likely be postponed today. Continue POC as tolerated.
Not Only Handwritten Notes are Illegible! Transfer: x 3 reps min assist progressing to CG with RW Ambulation: 50 feet with RW with supervision, increased plantarflexion and hip flexion resembling TDWB, … Daughter ed re stair pattern, RW ordered. Assessment Plan … not able to attempt stairs 2 to c/o and increased HR. RW ordered and received … D/c will likely be postponed today. Continue POC as tolerated.
 Doctors on Strike
Doctors on Strike
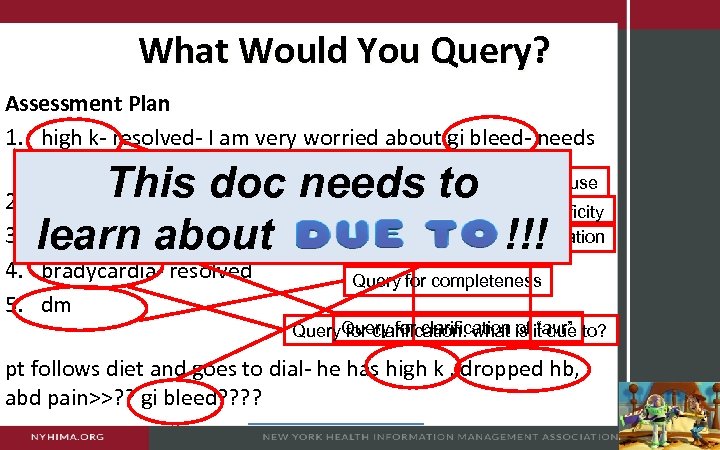 What Would You Query? Assessment Plan 1. high k- resolved- I am very worried about gi bleed- needs stolls- ? gi consult Query for abnormal lab and for cause 2. esrd- hd for wed Query for completeness, specificity 3. avr- on hep> coumadine Query on abnormal lab interpretation 4. bradycardia- resolved Query for completeness 5. dm This doc needs to learn about !!! Query for clarification is it due to? for clarification: what of “avr” pt follows diet and goes to dial- he has high k , dropped hb, abd pain>>? ? gi bleed? ?
What Would You Query? Assessment Plan 1. high k- resolved- I am very worried about gi bleed- needs stolls- ? gi consult Query for abnormal lab and for cause 2. esrd- hd for wed Query for completeness, specificity 3. avr- on hep> coumadine Query on abnormal lab interpretation 4. bradycardia- resolved Query for completeness 5. dm This doc needs to learn about !!! Query for clarification is it due to? for clarification: what of “avr” pt follows diet and goes to dial- he has high k , dropped hb, abd pain>>? ? gi bleed? ?
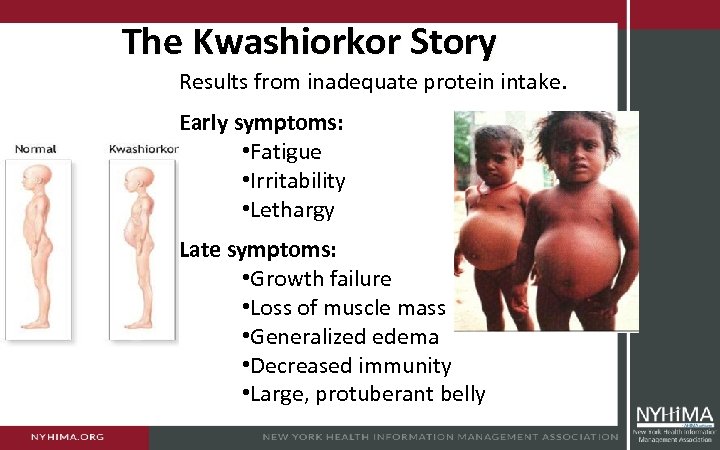 The Kwashiorkor Story Results from inadequate protein intake. Early symptoms: • Fatigue • Irritability • Lethargy Late symptoms: • Growth failure • Loss of muscle mass • Generalized edema • Decreased immunity • Large, protuberant belly
The Kwashiorkor Story Results from inadequate protein intake. Early symptoms: • Fatigue • Irritability • Lethargy Late symptoms: • Growth failure • Loss of muscle mass • Generalized edema • Decreased immunity • Large, protuberant belly
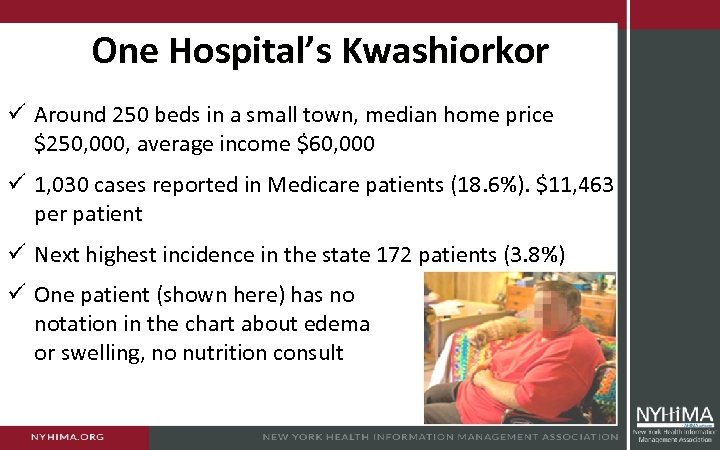 One Hospital’s Kwashiorkor ü Around 250 beds in a small town, median home price $250, 000, average income $60, 000 ü 1, 030 cases reported in Medicare patients (18. 6%). $11, 463 per patient ü Next highest incidence in the state 172 patients (3. 8%) ü One patient (shown here) has no notation in the chart about edema or swelling, no nutrition consult
One Hospital’s Kwashiorkor ü Around 250 beds in a small town, median home price $250, 000, average income $60, 000 ü 1, 030 cases reported in Medicare patients (18. 6%). $11, 463 per patient ü Next highest incidence in the state 172 patients (3. 8%) ü One patient (shown here) has no notation in the chart about edema or swelling, no nutrition consult
 Adult Malnutrition: Two or More Findings ü Insufficient energy intake ü Weight loss ü Loss of muscle mass ü Loss of subcutaneous fat ü Localized or generalized fluid accumulation that may sometimes mask weight loss ü Diminished functional status as measured by hand grip strength
Adult Malnutrition: Two or More Findings ü Insufficient energy intake ü Weight loss ü Loss of muscle mass ü Loss of subcutaneous fat ü Localized or generalized fluid accumulation that may sometimes mask weight loss ü Diminished functional status as measured by hand grip strength
 Adult Malnutrition: Documentation ü History and Clinical Diagnosis: Conditions that might be associated with inflammation and nutritional disturbances ü Clinical Signs and Physical Examination: SIRS, fluid accumulation, signs of weight gain or weight loss. ü Anthropometric Data: Height, weight and weight history, skin folds, circumference, other body composition metrics. ü Laboratory Indicators: Low proteins related to morbidity and mortality. Inflammation, negative nitrogen balance ü Dietary Data: A diet history or 24 -hour dietary recall ü Functional Outcomes: Assessment of strength and physical performance, along with other associated findings.
Adult Malnutrition: Documentation ü History and Clinical Diagnosis: Conditions that might be associated with inflammation and nutritional disturbances ü Clinical Signs and Physical Examination: SIRS, fluid accumulation, signs of weight gain or weight loss. ü Anthropometric Data: Height, weight and weight history, skin folds, circumference, other body composition metrics. ü Laboratory Indicators: Low proteins related to morbidity and mortality. Inflammation, negative nitrogen balance ü Dietary Data: A diet history or 24 -hour dietary recall ü Functional Outcomes: Assessment of strength and physical performance, along with other associated findings.
 Adult Malnutrition: Jon’s Tips ü Be sure that there is a clinical sense of a potential nutritional disturbance before proceeding any further! ü Verify that at least 2 of the 6 characteristics from the ASPEN guidelines are present to further confirm the diagnosis ü Avoid temptation to query about malnutrition (or to code for it) when the only basis is an abnormal lab result ü Use the 6 -point template suggested by the ASPEN guidelines to provide complete documentation ü Look for other conditions and diagnoses that may produce or be associated with malnutrition ü Don’t confuse the need for nutrition for the presence of malnutrition
Adult Malnutrition: Jon’s Tips ü Be sure that there is a clinical sense of a potential nutritional disturbance before proceeding any further! ü Verify that at least 2 of the 6 characteristics from the ASPEN guidelines are present to further confirm the diagnosis ü Avoid temptation to query about malnutrition (or to code for it) when the only basis is an abnormal lab result ü Use the 6 -point template suggested by the ASPEN guidelines to provide complete documentation ü Look for other conditions and diagnoses that may produce or be associated with malnutrition ü Don’t confuse the need for nutrition for the presence of malnutrition
 Encephalopathy ü ü ü ü Rapid involuntary eye movement Inability to swallow or speak Muscle twitching, atrophy, weakness and tremor Memory loss, loss of cognitive ability Personality changes Inability to concentrate Loss of consciousness Dementia, seizures, lethargy
Encephalopathy ü ü ü ü Rapid involuntary eye movement Inability to swallow or speak Muscle twitching, atrophy, weakness and tremor Memory loss, loss of cognitive ability Personality changes Inability to concentrate Loss of consciousness Dementia, seizures, lethargy
 … and at One Hospital ü 36% incidence in elderly Medicare patients at one hospitals ü Other hospitals in the state reported encephalopathy in 3. 6% of that population ü A hospital could earn $7, 000 per case for treating the condition as a complication
… and at One Hospital ü 36% incidence in elderly Medicare patients at one hospitals ü Other hospitals in the state reported encephalopathy in 3. 6% of that population ü A hospital could earn $7, 000 per case for treating the condition as a complication
 Beware! ü Not all Altered Mental Status is encephalopathy ü Some consultants emphasize pursuing this diagnosis as an apparently easy way to increase revenues ü Develop clear criteria for the diagnosis at your hospital ü Anticipate close scrutiny from auditors
Beware! ü Not all Altered Mental Status is encephalopathy ü Some consultants emphasize pursuing this diagnosis as an apparently easy way to increase revenues ü Develop clear criteria for the diagnosis at your hospital ü Anticipate close scrutiny from auditors
 First Document the Cause of AMS ü Neurodegenerative diseases: – Alzheimer’s disease (delusional, depressed, or psychotic) – Lewy body dementia (associated with Parkinson’s disease) ü Psychiatric illnesses: – Mood disorders (unipolar depression or bipolar disorder 1 & 2) – Schizophrenia (specified as to the type) – Chemical dependencies, including drug withdrawal syndrome ü AMS caused by a focal structural problem with the brain; seizure, concussion, stroke, transient ischemic attack, or tumor. ü AMS caused by global dysfunction of the brain (encephalopathy!); toxic, septic, metabolic, hypertensive, or hepatic.
First Document the Cause of AMS ü Neurodegenerative diseases: – Alzheimer’s disease (delusional, depressed, or psychotic) – Lewy body dementia (associated with Parkinson’s disease) ü Psychiatric illnesses: – Mood disorders (unipolar depression or bipolar disorder 1 & 2) – Schizophrenia (specified as to the type) – Chemical dependencies, including drug withdrawal syndrome ü AMS caused by a focal structural problem with the brain; seizure, concussion, stroke, transient ischemic attack, or tumor. ü AMS caused by global dysfunction of the brain (encephalopathy!); toxic, septic, metabolic, hypertensive, or hepatic.

 CDI: It’s Front Page News
CDI: It’s Front Page News
 You May Be Headed for the Front Page… ü If you have a high incidence of Kwashiorkor ü If your CDI consultant promised in writing to increase revenues ü If the first hour of your first day of training is all about encephalopathy ü If you have an high incidence of malignant hypertension ü If you are told: – Find an MCC then move on – Query for reimbursement or SOI
You May Be Headed for the Front Page… ü If you have a high incidence of Kwashiorkor ü If your CDI consultant promised in writing to increase revenues ü If the first hour of your first day of training is all about encephalopathy ü If you have an high incidence of malignant hypertension ü If you are told: – Find an MCC then move on – Query for reimbursement or SOI
 A Few Helpful References ü Consensus Statement of the Academy of Nutrition and Dietetics/American Society for Parenteral and Enteral Nutrition: Characteristics Recommended for the Identification and Documentation of Adult Malnutrition (Undernutrition) J Acad Nutr Diet. 2012; 112: 730 -738. www. wvda. org/meeting 2012/Malnutrition. pdf ü Cut Through the Confusion of Altered Mental Status by Brian Murphy. Association of Clinical Documentation Specialists, June 2009. www. hcpro. com/content/235239. pdf ü Clinical Documentation Intelligence: www. chartwisemed. com
A Few Helpful References ü Consensus Statement of the Academy of Nutrition and Dietetics/American Society for Parenteral and Enteral Nutrition: Characteristics Recommended for the Identification and Documentation of Adult Malnutrition (Undernutrition) J Acad Nutr Diet. 2012; 112: 730 -738. www. wvda. org/meeting 2012/Malnutrition. pdf ü Cut Through the Confusion of Altered Mental Status by Brian Murphy. Association of Clinical Documentation Specialists, June 2009. www. hcpro. com/content/235239. pdf ü Clinical Documentation Intelligence: www. chartwisemed. com