f3486174efc0a18d7069287434c50a31.ppt
- Количество слайдов: 140

 Chair: Dr. Allan Gunning Joint Chair of National Steering Group for Joint Strategic Commissioning
Chair: Dr. Allan Gunning Joint Chair of National Steering Group for Joint Strategic Commissioning

 Professor Jim Mc. Goldrick Chair Joint Improvement Partnership Board
Professor Jim Mc. Goldrick Chair Joint Improvement Partnership Board
 Joint Strategic Commissioning Improvement Agenda Jim Mc. Goldrick
Joint Strategic Commissioning Improvement Agenda Jim Mc. Goldrick
 Joint Improvement Partnership Board • • • NHS Scotland Scottish Government COSLA Third Sector Independent Sector
Joint Improvement Partnership Board • • • NHS Scotland Scottish Government COSLA Third Sector Independent Sector
 Board and JIT will work with other improvement bodies to: • Accelerate the pace of transformational change • Support and challenge improvement in the delivery of integrated health and social care • Particular challenge of joint strategic commissioning
Board and JIT will work with other improvement bodies to: • Accelerate the pace of transformational change • Support and challenge improvement in the delivery of integrated health and social care • Particular challenge of joint strategic commissioning
 Need for improvement • Need “new commissioning models based on partnership and delivery of personalised outcomes” Changing Lives; report of the 21 Century Social Work Review, 2006 • “Little evidence …of significant improvement and limited progress on joint commissioning” st Audit Scotland 2012 • “Very few examples of good joint planning and a slowness to develop strategic commissioning” Scottish Parliament Finance Committee 2013
Need for improvement • Need “new commissioning models based on partnership and delivery of personalised outcomes” Changing Lives; report of the 21 Century Social Work Review, 2006 • “Little evidence …of significant improvement and limited progress on joint commissioning” st Audit Scotland 2012 • “Very few examples of good joint planning and a slowness to develop strategic commissioning” Scottish Parliament Finance Committee 2013

 • Analysis is one of the most important activities in the commissioning cycle. Poor analysis of past or future trends will result in flawed commissioning decisions and wasted resources”. • SWIA guide to Strategic Commissioning
• Analysis is one of the most important activities in the commissioning cycle. Poor analysis of past or future trends will result in flawed commissioning decisions and wasted resources”. • SWIA guide to Strategic Commissioning
 Supporting the analysis • Individual level linked health and social care data • Centrally funded team • Joint Improvement Team • Across all partnerships by 2015
Supporting the analysis • Individual level linked health and social care data • Centrally funded team • Joint Improvement Team • Across all partnerships by 2015
 • “One of the opportunities with which integration provides us is that it will allow us to ensure through joint commissioning that we bring those services together in a much more targeted and focused way with a clear focus on the long term outcomes” • Michael Matheson MSP, Minister for Public Health, Scottish Parliament, 8 May 2013 • “Each Health and Social Care Partnership will be expected to produce joint commissioning strategies and delivery plans over the medium and long-term • Integration of Adult Health and Social Care Consultation Proposals
• “One of the opportunities with which integration provides us is that it will allow us to ensure through joint commissioning that we bring those services together in a much more targeted and focused way with a clear focus on the long term outcomes” • Michael Matheson MSP, Minister for Public Health, Scottish Parliament, 8 May 2013 • “Each Health and Social Care Partnership will be expected to produce joint commissioning strategies and delivery plans over the medium and long-term • Integration of Adult Health and Social Care Consultation Proposals

 • “Councils and NHS Boards do not always involve voluntary and private providers in planning which services are needed in the local area” Audit Scotland, 2012 • A significant part of the expertise required to commission and provide services…. sits with the providers of service rather than the commissioners” Changing Lives, 2009
• “Councils and NHS Boards do not always involve voluntary and private providers in planning which services are needed in the local area” Audit Scotland, 2012 • A significant part of the expertise required to commission and provide services…. sits with the providers of service rather than the commissioners” Changing Lives, 2009

 Councillor Peter Johnston Health and Well-being Spokesperson COSLA
Councillor Peter Johnston Health and Well-being Spokesperson COSLA
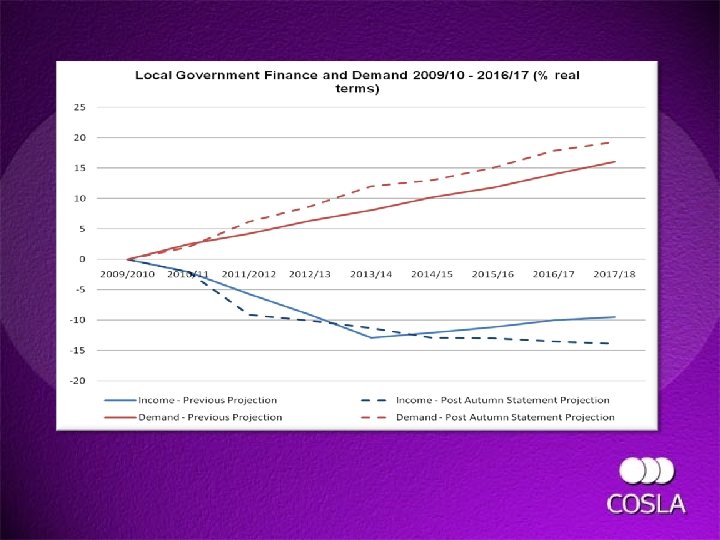
 Health and Social Care Integration: Today’s Reality, Tomorrow’s Vision Cllr Peter Johnston Health and Well-being Spokesperson COSLA
Health and Social Care Integration: Today’s Reality, Tomorrow’s Vision Cllr Peter Johnston Health and Well-being Spokesperson COSLA
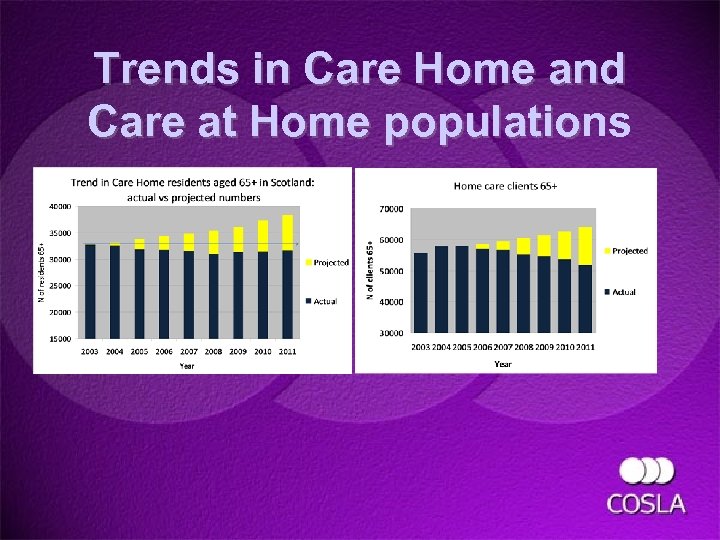 Trends in Care Home and Care at Home populations populatio
Trends in Care Home and Care at Home populations populatio
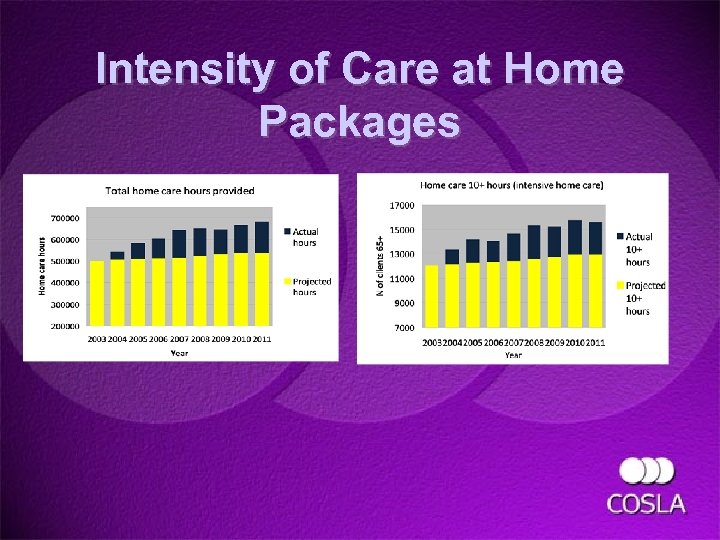 Intensity of Care at Home Packages
Intensity of Care at Home Packages
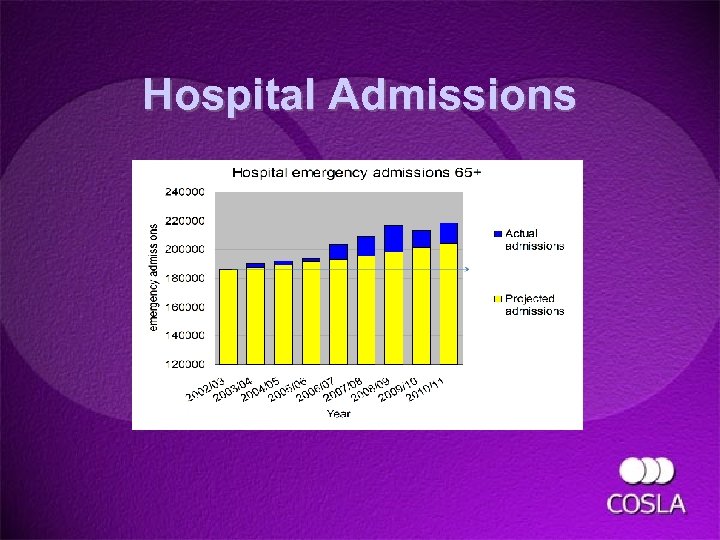 Hospital Admissions
Hospital Admissions
 What is to be Done? • • • More Personalised Support Shift the Balance of Care Develop Strategic Commissioning Health and Social Care Integration Find a Funding Solution
What is to be Done? • • • More Personalised Support Shift the Balance of Care Develop Strategic Commissioning Health and Social Care Integration Find a Funding Solution
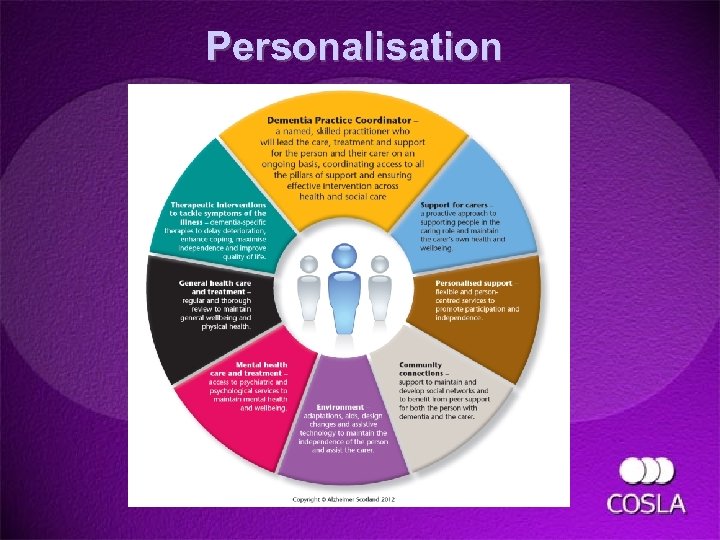 Personalisation
Personalisation

 Strategic Commissioning
Strategic Commissioning
 Health and Social Care Integration
Health and Social Care Integration
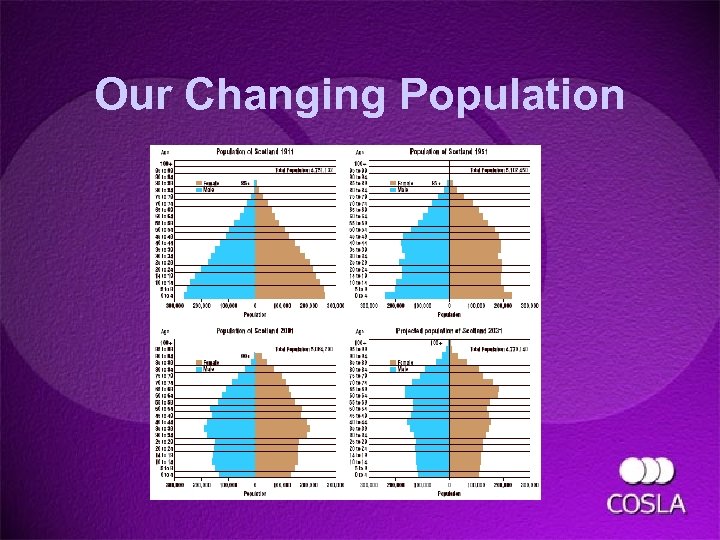 Our Changing Population
Our Changing Population
 What is to be Done? • • • More Personalised Support Shift the Balance of Care Develop Strategic Commissioning Health and Social Care Integration Find a Funding Solution
What is to be Done? • • • More Personalised Support Shift the Balance of Care Develop Strategic Commissioning Health and Social Care Integration Find a Funding Solution
 Questions
Questions

 Tony Homer Joint Strategic Commissioning Lead Joint Improvement Team
Tony Homer Joint Strategic Commissioning Lead Joint Improvement Team
 Joint Strategic Commissioning Plans for Older People 2013 Overview of Self Assessments, Improvement Themes and the Support Agenda May 2013 Tony Homer JIT National Lead, Joint Strategic Commissioning
Joint Strategic Commissioning Plans for Older People 2013 Overview of Self Assessments, Improvement Themes and the Support Agenda May 2013 Tony Homer JIT National Lead, Joint Strategic Commissioning
 Commissioning Context > Requirements: • • Self evaluation return to SG Preparation of JSC Plans > National drivers: • • • Policy – personalisation and prevention Demographics – population levels and health profiles Public sector finances – focus on efficiencies > Integration context: • • • All adult and older people care groups Minimum level of acute spend into integrated budgets Locality planning > Purpose of the review: understanding progress and challenges and preparing for further change
Commissioning Context > Requirements: • • Self evaluation return to SG Preparation of JSC Plans > National drivers: • • • Policy – personalisation and prevention Demographics – population levels and health profiles Public sector finances – focus on efficiencies > Integration context: • • • All adult and older people care groups Minimum level of acute spend into integrated budgets Locality planning > Purpose of the review: understanding progress and challenges and preparing for further change
 National partner review process > Who was involved? > Review timetable > Core review of plans > Thematic review of plans: > > > > Partnership working Outcomes Co-production Information Housing Intermediate Care Telehealthcare > Round table discussions Workforce Self Directed Support Community Capacity Building Financials Dementia Carers
National partner review process > Who was involved? > Review timetable > Core review of plans > Thematic review of plans: > > > > Partnership working Outcomes Co-production Information Housing Intermediate Care Telehealthcare > Round table discussions Workforce Self Directed Support Community Capacity Building Financials Dementia Carers
 Review reporting > Presentation – key themes and support priorities > Thematic reports > Individual partnership feedback > Incorporation into planned improvement support priorities and shared learning
Review reporting > Presentation – key themes and support priorities > Thematic reports > Individual partnership feedback > Incorporation into planned improvement support priorities and shared learning
 JSC Plan - Structure Analysis > 24 out of 31 plans (77%) were available to be reviewed > Most of the other 7 are well progressed and/or are awaiting sign off > 10 year horizon 15 health and social care partnership plans/frameworks with 1 being a pan health board strategic framework and 1 a joint plan across 2 Council areas > 3 year horizon 9 health and social care partnership strategies/plans and 7 implementation plans relating to a 10 year strategy > 1 year Change Plans – all available > Housing Contribution Statements – all available
JSC Plan - Structure Analysis > 24 out of 31 plans (77%) were available to be reviewed > Most of the other 7 are well progressed and/or are awaiting sign off > 10 year horizon 15 health and social care partnership plans/frameworks with 1 being a pan health board strategic framework and 1 a joint plan across 2 Council areas > 3 year horizon 9 health and social care partnership strategies/plans and 7 implementation plans relating to a 10 year strategy > 1 year Change Plans – all available > Housing Contribution Statements – all available
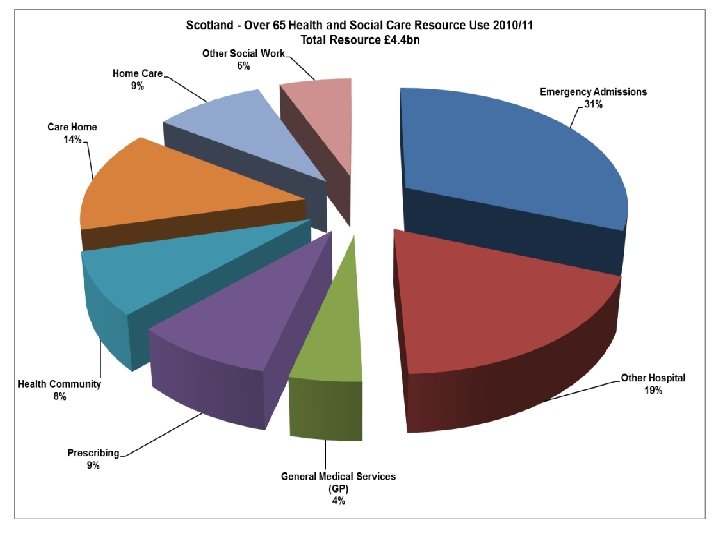
 Whole system overview > The challenge of scaling up from Change Plans > Scoping of the available resource pot did include acute hospital activity but the detail varied > Analysis of acute hospital activity absent beyond the brief description of services included in the scope > Nothing about how the acute spend will be used > Limited presentation and analysis of community assets and less traditional activities/approaches
Whole system overview > The challenge of scaling up from Change Plans > Scoping of the available resource pot did include acute hospital activity but the detail varied > Analysis of acute hospital activity absent beyond the brief description of services included in the scope > Nothing about how the acute spend will be used > Limited presentation and analysis of community assets and less traditional activities/approaches
 Following some golden threads. . . > Personal outcomes > Partnership working > Leadership > Information and Analysis
Following some golden threads. . . > Personal outcomes > Partnership working > Leadership > Information and Analysis
 Personal outcomes Recognised in the self evaluation as the area of greatest challenge – and confirmed to be so by the review Examples of how this was most apparent: > > ‘When is a vision not a vision. . . ’ Recognising, capturing and applying personal outcomes data Using outcomes to shape re-design activity Understanding and addressing the culture change implications in single agencies and particularly across partners > Securing services that will deliver improved outcomes – contracts and commissioning / procurement links > Personalisation and SDS?
Personal outcomes Recognised in the self evaluation as the area of greatest challenge – and confirmed to be so by the review Examples of how this was most apparent: > > ‘When is a vision not a vision. . . ’ Recognising, capturing and applying personal outcomes data Using outcomes to shape re-design activity Understanding and addressing the culture change implications in single agencies and particularly across partners > Securing services that will deliver improved outcomes – contracts and commissioning / procurement links > Personalisation and SDS?
 Partnership working Considered in the self evaluation to be one of the areas of greatest progress but important gaps emerged from the review Basic governance and commissioning processes in place but examples of gaps concerned: > Comprehensive engagement strategies > Co-production with all partners and stakeholders > Clear processes and joint accountability for prioritisation and decision making > Little evidence of a culture of data sharing across sectors > Joint approaches to Organisational Development > Locality/total place approaches that bring shared insights / ownership
Partnership working Considered in the self evaluation to be one of the areas of greatest progress but important gaps emerged from the review Basic governance and commissioning processes in place but examples of gaps concerned: > Comprehensive engagement strategies > Co-production with all partners and stakeholders > Clear processes and joint accountability for prioritisation and decision making > Little evidence of a culture of data sharing across sectors > Joint approaches to Organisational Development > Locality/total place approaches that bring shared insights / ownership
 Leadership Considered in the self evaluation to be an area of strength but limited evidence emerged to support this: Evidence of enabling leadership through practitioners and staff but examples of the following were scarce: > Visible senior corporate leadership through sponsorship of overall programme and key workstreams > Explicit referencing of high level corporate strategic drivers and cross sector priorities to evidence buy-in > Driving forward on known aspects and direction of travel whilst managing the present uncertainty around integration
Leadership Considered in the self evaluation to be an area of strength but limited evidence emerged to support this: Evidence of enabling leadership through practitioners and staff but examples of the following were scarce: > Visible senior corporate leadership through sponsorship of overall programme and key workstreams > Explicit referencing of high level corporate strategic drivers and cross sector priorities to evidence buy-in > Driving forward on known aspects and direction of travel whilst managing the present uncertainty around integration
 Information and Analysis Considered in the self evaluation to be one of the areas of strength but variable evidence emerged from the review Strong contextualisation through use of population health and well-being profiles and good focus on key points, analysis and interpretation but examples of outstanding limitations included: > > Limited referencing of health inequalities Access to common local data/analyses for shared use Limited application of robust option appraisal methodologies Little analysis of expenditure patterns with a view to modelling the impact of re-design > Limited use of national mapping data
Information and Analysis Considered in the self evaluation to be one of the areas of strength but variable evidence emerged from the review Strong contextualisation through use of population health and well-being profiles and good focus on key points, analysis and interpretation but examples of outstanding limitations included: > > Limited referencing of health inequalities Access to common local data/analyses for shared use Limited application of robust option appraisal methodologies Little analysis of expenditure patterns with a view to modelling the impact of re-design > Limited use of national mapping data
 Thematic support priorities 1 CARERS > Mapping the future carer population > Developing an integrated approach to requirements regarding indirect/direct support, personal outcomes and carer support SDS > Drawing evidence from current support packages and PSP initiatives about the impact of SDS > Improving knowledge of what works in order to grow the ambition of plans for SDS DEMENTIA > More detailed work concerning dementia on support for carers and for specialist groups of OP (eg. people with a LD) > Use of the NES/SSSC ‘Promoting Excellence model’ and of dementia tools and evaluating the impact of service changes
Thematic support priorities 1 CARERS > Mapping the future carer population > Developing an integrated approach to requirements regarding indirect/direct support, personal outcomes and carer support SDS > Drawing evidence from current support packages and PSP initiatives about the impact of SDS > Improving knowledge of what works in order to grow the ambition of plans for SDS DEMENTIA > More detailed work concerning dementia on support for carers and for specialist groups of OP (eg. people with a LD) > Use of the NES/SSSC ‘Promoting Excellence model’ and of dementia tools and evaluating the impact of service changes
 Thematic support priorities 2 CO-PRODUCTION > A greater emphasis and focus on the application and utility of coproduction in health and social care HOUSING > Improving links between housing and H&SC data > Developing the focus on the role of housing in delivering improved prevention INTERMEDIATE CARE > Aligning initiatives as a comprehensive framework of IC tailored to the locality > Development of practitioner capability for enhanced roles in the community > TELEHEALTHCARE > Despite recent progress and ongoing investment scant referencing in plans and little sign of strategic grasp of its ongoing role
Thematic support priorities 2 CO-PRODUCTION > A greater emphasis and focus on the application and utility of coproduction in health and social care HOUSING > Improving links between housing and H&SC data > Developing the focus on the role of housing in delivering improved prevention INTERMEDIATE CARE > Aligning initiatives as a comprehensive framework of IC tailored to the locality > Development of practitioner capability for enhanced roles in the community > TELEHEALTHCARE > Despite recent progress and ongoing investment scant referencing in plans and little sign of strategic grasp of its ongoing role
 Commissioning in practice – where are we now: > Largely treading water on progress in implementing a personal outcomes approach to commissioning – except for a very few notable exceptions > Formal partnership arrangements are being sustained but not all partners are embedded within many important JSC roles/tasks - and they need to be > Clear, consistent senior leadership is too often noticeable by it’s absence > Use of information and our analysis of it is improving but we are not making best use of available national data and are slow at growing local information > We are not making investment decisions on the basis of clear criteria, a robust decision making process and the application of relevant and focussed information > Important progress in many areas of practice/re-design but little grasp as yet of how to enable communities and local assets to engage and contribute to the strategic agenda These will form key elements of the ongoing improvement support agenda
Commissioning in practice – where are we now: > Largely treading water on progress in implementing a personal outcomes approach to commissioning – except for a very few notable exceptions > Formal partnership arrangements are being sustained but not all partners are embedded within many important JSC roles/tasks - and they need to be > Clear, consistent senior leadership is too often noticeable by it’s absence > Use of information and our analysis of it is improving but we are not making best use of available national data and are slow at growing local information > We are not making investment decisions on the basis of clear criteria, a robust decision making process and the application of relevant and focussed information > Important progress in many areas of practice/re-design but little grasp as yet of how to enable communities and local assets to engage and contribute to the strategic agenda These will form key elements of the ongoing improvement support agenda

 Professor John Bolton Independent Consultant
Professor John Bolton Independent Consultant
 What does good look like if we are to manage demand in health and social care? From strategy to reality. Professor John Bolton Consultant JRFB Ltd
What does good look like if we are to manage demand in health and social care? From strategy to reality. Professor John Bolton Consultant JRFB Ltd
 Challenges for Health and Care Demographic pressure leading to more demand (unless we do something about it) – already happening in health but not consistently in social care. In England accompanied by significant financial challenges – focuses the mind Policy demand to integrate two different sets of values – medical model – eliminate and proscribe vs care model – assess and maximise independence– (evidence not really on our side) Focus on outcomes – can we agree on the outcomes that we want to achieve – What does good look like?
Challenges for Health and Care Demographic pressure leading to more demand (unless we do something about it) – already happening in health but not consistently in social care. In England accompanied by significant financial challenges – focuses the mind Policy demand to integrate two different sets of values – medical model – eliminate and proscribe vs care model – assess and maximise independence– (evidence not really on our side) Focus on outcomes – can we agree on the outcomes that we want to achieve – What does good look like?
 Different levels of Prevention (Source Institute of Public Care) Universal provision (the preventative aspects of universally available services) Preventative provision for populations that contain some elements of vulnerability (specialist services that may tackle some aspects of need but not ones which would have led to an assessed social care intervention or an acute episode of health care). Targeted restorative interventions (interventions targeted on very particular populations in the evidence based belief that if successful they will lessen potential future demand for high intensity care). Deferred interventions (interventions that are preventative in that they defer people for a time from a poorer outcome). 55
Different levels of Prevention (Source Institute of Public Care) Universal provision (the preventative aspects of universally available services) Preventative provision for populations that contain some elements of vulnerability (specialist services that may tackle some aspects of need but not ones which would have led to an assessed social care intervention or an acute episode of health care). Targeted restorative interventions (interventions targeted on very particular populations in the evidence based belief that if successful they will lessen potential future demand for high intensity care). Deferred interventions (interventions that are preventative in that they defer people for a time from a poorer outcome). 55
 Universality – health and social care Public Health – health of the nation/ deprivation / prevent or cure for health – “well-being” – tackling inequalities in life expectation and outcomes Reducing dementia risks through exercise Does everyone get the same health care? Priorities for Health - You don’t suffer from the same things that make you die Dementia – Incontinence – Falls – Stroke Recovery vs Cancers and Heart Failure. A little bit of social care may be bad for you! Active citizenship is good for you – tackling social isolation
Universality – health and social care Public Health – health of the nation/ deprivation / prevent or cure for health – “well-being” – tackling inequalities in life expectation and outcomes Reducing dementia risks through exercise Does everyone get the same health care? Priorities for Health - You don’t suffer from the same things that make you die Dementia – Incontinence – Falls – Stroke Recovery vs Cancers and Heart Failure. A little bit of social care may be bad for you! Active citizenship is good for you – tackling social isolation
 Housing Related Support Former Supporting People funded services e. g. Tackling Homelessness; Community Living schemes; Domestic Violence Cap Gemini identified preventive interventions Move to Payments by Results or Outcome Based Commissioning – invest in schemes that will deliver the preventive outcomes that you seek – be specific for each scheme
Housing Related Support Former Supporting People funded services e. g. Tackling Homelessness; Community Living schemes; Domestic Violence Cap Gemini identified preventive interventions Move to Payments by Results or Outcome Based Commissioning – invest in schemes that will deliver the preventive outcomes that you seek – be specific for each scheme
 Assistive Technology Community Alarms Gadgets that aid daily living (stand-alone) Gadgets that aid daily living (connected by sensors to a centre) Tracking or monitoring devices Health monitoring (vital signs) and Interactive products linked to risk management Communication Devices Information and Advice
Assistive Technology Community Alarms Gadgets that aid daily living (stand-alone) Gadgets that aid daily living (connected by sensors to a centre) Tracking or monitoring devices Health monitoring (vital signs) and Interactive products linked to risk management Communication Devices Information and Advice
 New rules of practice for health and social care Don’t assess someone when they are in a crisis e. g. a hospital bed/ in bereavement – you will get in wrong for 1 in 3 people Ensure that you manage the crisis and offer short term help to assist the person or divert away from formal care Only assess after short term help has completed its natural course (which isn't always 6 weeks)
New rules of practice for health and social care Don’t assess someone when they are in a crisis e. g. a hospital bed/ in bereavement – you will get in wrong for 1 in 3 people Ensure that you manage the crisis and offer short term help to assist the person or divert away from formal care Only assess after short term help has completed its natural course (which isn't always 6 weeks)
 Restorative interventions Joint Commissioning a Health and Care system Therapists and reablement Out of hospital care –recuperation through Intermediate Care Mental Health Recovery Model Rehabilitation
Restorative interventions Joint Commissioning a Health and Care system Therapists and reablement Out of hospital care –recuperation through Intermediate Care Mental Health Recovery Model Rehabilitation
 Deferred Interventions Much we can do to identify people who are not doing well and get the services right to reduce the acceleration of the condition – a combination of better management and better self-management Managing a Long-term condition – most persistent readmissions Challenge from professionals (virtual ward) Consistent messages
Deferred Interventions Much we can do to identify people who are not doing well and get the services right to reduce the acceleration of the condition – a combination of better management and better self-management Managing a Long-term condition – most persistent readmissions Challenge from professionals (virtual ward) Consistent messages
 Good reablement has………. A clear process that enables people to access the service and that can cope with flows of demand A well trained workforce who are clear on the outcomes that are expected A set of measurements which helps demonstrate which people are benefitting from the approach and is able to indicate if any staff need further support and training in the work (it is easy when under pressure for some staff to return to old ways). A clear set of business plans which monitor both the financial flows (in relation to any savings made against the investment) alongside a performance framework that monitor the delivery of these plans. Leadership within the Organisation which is making sure that the service is delivering what might be expected. A clear link between therapists working within the service and the staff delivering the day to day re-ablement. A clarity of where the re-ablement programme sits within the care pathway. The opportunity for follow up and sustained action by customers after the service has ended e. g. opportunity to participate in exercise classes or to take regular exercise. A focus on the emotional as well as the practical and physical needs of older people.
Good reablement has………. A clear process that enables people to access the service and that can cope with flows of demand A well trained workforce who are clear on the outcomes that are expected A set of measurements which helps demonstrate which people are benefitting from the approach and is able to indicate if any staff need further support and training in the work (it is easy when under pressure for some staff to return to old ways). A clear set of business plans which monitor both the financial flows (in relation to any savings made against the investment) alongside a performance framework that monitor the delivery of these plans. Leadership within the Organisation which is making sure that the service is delivering what might be expected. A clear link between therapists working within the service and the staff delivering the day to day re-ablement. A clarity of where the re-ablement programme sits within the care pathway. The opportunity for follow up and sustained action by customers after the service has ended e. g. opportunity to participate in exercise classes or to take regular exercise. A focus on the emotional as well as the practical and physical needs of older people.
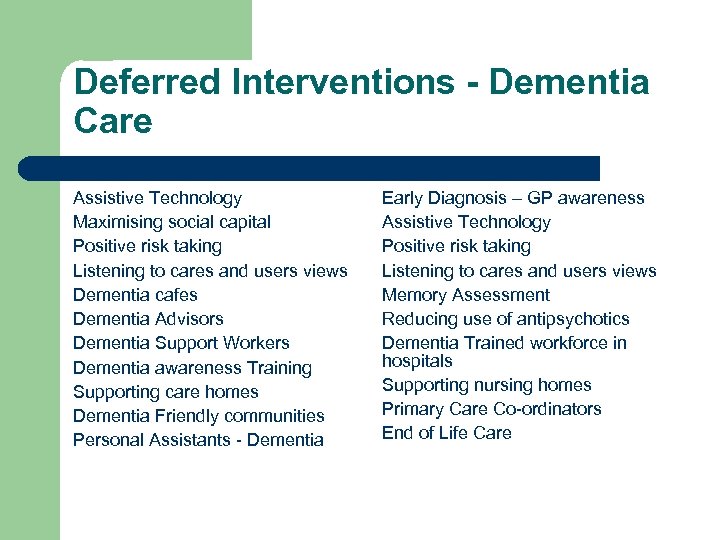 Deferred Interventions - Dementia Care Assistive Technology Maximising social capital Positive risk taking Listening to cares and users views Dementia cafes Dementia Advisors Dementia Support Workers Dementia awareness Training Supporting care homes Dementia Friendly communities Personal Assistants - Dementia Early Diagnosis – GP awareness Assistive Technology Positive risk taking Listening to cares and users views Memory Assessment Reducing use of antipsychotics Dementia Trained workforce in hospitals Supporting nursing homes Primary Care Co-ordinators End of Life Care
Deferred Interventions - Dementia Care Assistive Technology Maximising social capital Positive risk taking Listening to cares and users views Dementia cafes Dementia Advisors Dementia Support Workers Dementia awareness Training Supporting care homes Dementia Friendly communities Personal Assistants - Dementia Early Diagnosis – GP awareness Assistive Technology Positive risk taking Listening to cares and users views Memory Assessment Reducing use of antipsychotics Dementia Trained workforce in hospitals Supporting nursing homes Primary Care Co-ordinators End of Life Care
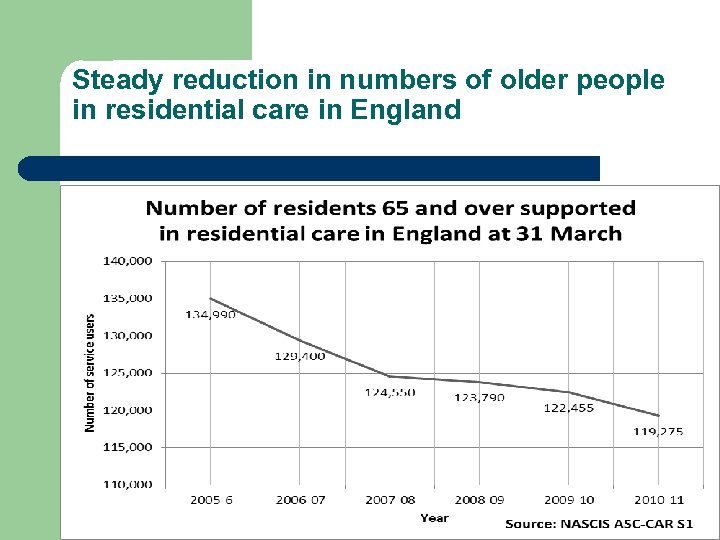 Steady reduction in numbers of older people in residential care in England
Steady reduction in numbers of older people in residential care in England
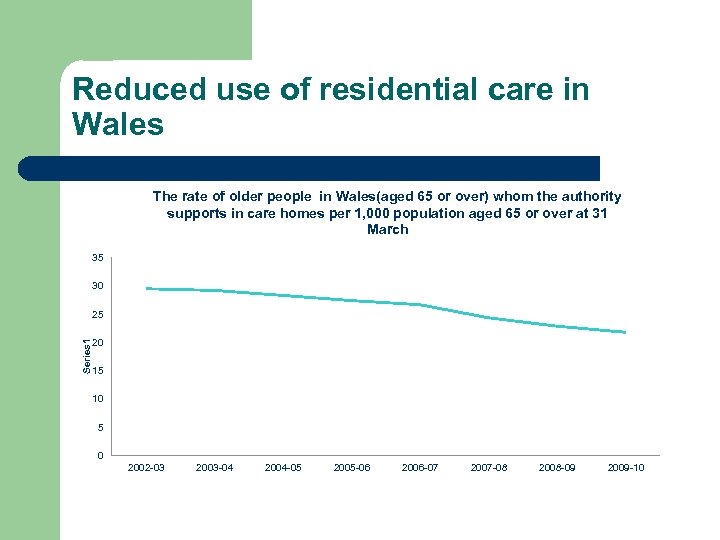 Reduced use of residential care in Wales The rate of older people in Wales(aged 65 or over) whom the authority supports in care homes per 1, 000 population aged 65 or over at 31 March 35 30 Series 1 25 20 15 10 5 0 2002 -03 2003 -04 2004 -05 2005 -06 2006 -07 2007 -08 2008 -09 2009 -10
Reduced use of residential care in Wales The rate of older people in Wales(aged 65 or over) whom the authority supports in care homes per 1, 000 population aged 65 or over at 31 March 35 30 Series 1 25 20 15 10 5 0 2002 -03 2003 -04 2004 -05 2005 -06 2006 -07 2007 -08 2008 -09 2009 -10
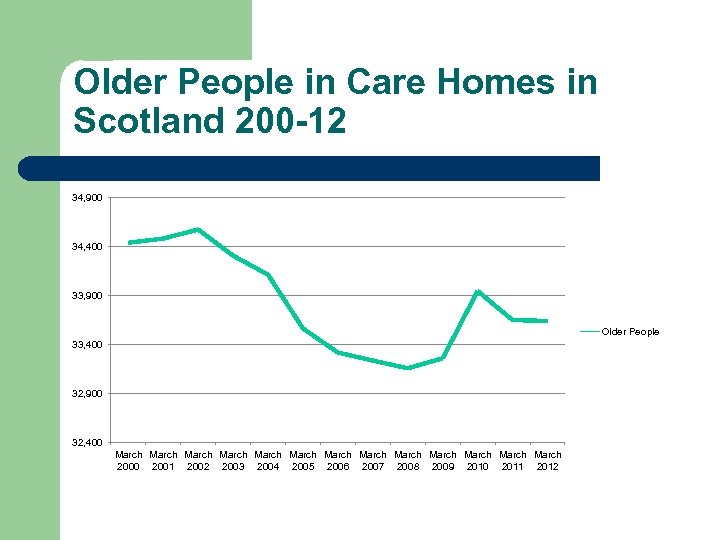 Older People in Care Homes in Scotland 200 -12 34, 900 34, 400 33, 900 Older People 33, 400 32, 900 32, 400 March March March March 2000 2001 2002 2003 2004 2005 2006 2007 2008 2009 2010 2011 2012
Older People in Care Homes in Scotland 200 -12 34, 900 34, 400 33, 900 Older People 33, 400 32, 900 32, 400 March March March March 2000 2001 2002 2003 2004 2005 2006 2007 2008 2009 2010 2011 2012
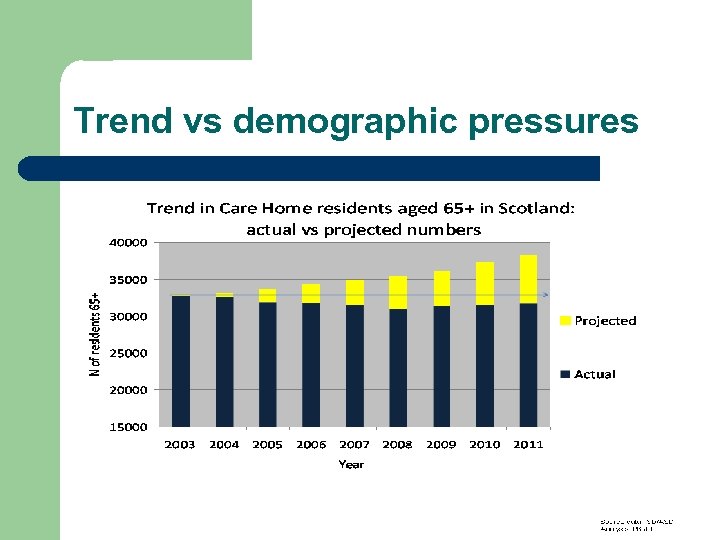 Trend vs demographic pressures
Trend vs demographic pressures
 What does good look like? Reduced admissions to residential care (nil from acute hospital) Reduced numbers needing longer term care High numbers supported through reablement/recovery to need no further care Reduced emergency readmissions Reduced non-elective admissions Reduced delayed discharges of care
What does good look like? Reduced admissions to residential care (nil from acute hospital) Reduced numbers needing longer term care High numbers supported through reablement/recovery to need no further care Reduced emergency readmissions Reduced non-elective admissions Reduced delayed discharges of care
 With an ageing population can we manage demand for services through better interventions? The need for new solutions to meet people’s needs through emergence of recovery based and outcome based models of care: Build on evidence from public health Build on management and self-management with multi-disciplinary team Building on the evidence from re-ablement with health partners Improving health outcomes for older people – Dementia care with early diagnosis- Falls prevention Managing continence - Stroke recovery services Focus on the evidence from housing solutions (care and repair, DFGs (Neath), extra care housing (IPC). Focus on the evidence from new technologies Focus on the evidence for tackling social isolation Focus on assessments that improve outcomes
With an ageing population can we manage demand for services through better interventions? The need for new solutions to meet people’s needs through emergence of recovery based and outcome based models of care: Build on evidence from public health Build on management and self-management with multi-disciplinary team Building on the evidence from re-ablement with health partners Improving health outcomes for older people – Dementia care with early diagnosis- Falls prevention Managing continence - Stroke recovery services Focus on the evidence from housing solutions (care and repair, DFGs (Neath), extra care housing (IPC). Focus on the evidence from new technologies Focus on the evidence for tackling social isolation Focus on assessments that improve outcomes
 For more help………. John Bolton Independent Consultant 07789748166 john. bolton@jrfb. co. uk
For more help………. John Bolton Independent Consultant 07789748166 john. bolton@jrfb. co. uk

 Lunch
Lunch

 Chair: Peter Mac. Leod Joint Chair of National Steering Group for Joint Strategic Commissioning
Chair: Peter Mac. Leod Joint Chair of National Steering Group for Joint Strategic Commissioning

 Keith Moultrie Director Institute of Public Care
Keith Moultrie Director Institute of Public Care
 Mature Integrated Commissioning – Joining the Dots JIT Conference May 2013
Mature Integrated Commissioning – Joining the Dots JIT Conference May 2013
 About IPC n We work for well run evidence based public care n We are part of Oxford Brookes University n We work with national and local government, the NHS and private, community and voluntary sectors n We work across the United Kingdom and undertake consultancy, applied research, management development, publications, seminars and software n We were formed in 1987, and have a team of 40 staff and Fellows, based in Oxford and Bath 79
About IPC n We work for well run evidence based public care n We are part of Oxford Brookes University n We work with national and local government, the NHS and private, community and voluntary sectors n We work across the United Kingdom and undertake consultancy, applied research, management development, publications, seminars and software n We were formed in 1987, and have a team of 40 staff and Fellows, based in Oxford and Bath 79
 Basis of presentation n Scottish Govt JIT National Joint Commissioning Learning Framework n Welsh Government SSIA national commissioning guidance and implementation programme n Df. E national Commissioning Support Programme for England n IPC academic partner programme n DH Developing Care Markets for Quality and Choice n Mc. Intyre, Saga, Somerset Care, Essex, Moray, Lancashire, Guinness, Swansea, Renfrewshire n Post graduate certificates programme 80
Basis of presentation n Scottish Govt JIT National Joint Commissioning Learning Framework n Welsh Government SSIA national commissioning guidance and implementation programme n Df. E national Commissioning Support Programme for England n IPC academic partner programme n DH Developing Care Markets for Quality and Choice n Mc. Intyre, Saga, Somerset Care, Essex, Moray, Lancashire, Guinness, Swansea, Renfrewshire n Post graduate certificates programme 80
 Outline n The basic ideas are well established – don’t waste too much time reinventing these n The real challenge now is about the scope, approach and energy you will bring to the commissioning task n There are 5 key tactical issues you need to address locally to deliver successful change through joint strategic commissioning 81
Outline n The basic ideas are well established – don’t waste too much time reinventing these n The real challenge now is about the scope, approach and energy you will bring to the commissioning task n There are 5 key tactical issues you need to address locally to deliver successful change through joint strategic commissioning 81
 The basic ideas are established. . n COSLA (2008) Guidance for Community Planning Partnerships on Single Outcome Agreements n Social Work Inspection Agency (Sept 2009) Guide to Strategic Commissioning n Scottish Government, COSLA, NHS Scotland (2011) Reshaping Care for Older People n Scottish Government (Sept 2010) Procurement of Care and Support Services n Public Services Commission (June 2011) Commission on the Future Delivery of Public Services n Scottish Government Joint Improvement Team (August 2011), Preparing your Joint Commissioning Strategy for Older People n Scottish Government Joint Improvement Team (Sept 2011), Preparing your Joint Strategic Commissioning Plan for Older People n Audit Scotland (March 2012) Commissioning Social Care n Scottish Government (Sept 2012) Integration of Health and Social Care in Scotland response to consultation (2013) 82
The basic ideas are established. . n COSLA (2008) Guidance for Community Planning Partnerships on Single Outcome Agreements n Social Work Inspection Agency (Sept 2009) Guide to Strategic Commissioning n Scottish Government, COSLA, NHS Scotland (2011) Reshaping Care for Older People n Scottish Government (Sept 2010) Procurement of Care and Support Services n Public Services Commission (June 2011) Commission on the Future Delivery of Public Services n Scottish Government Joint Improvement Team (August 2011), Preparing your Joint Commissioning Strategy for Older People n Scottish Government Joint Improvement Team (Sept 2011), Preparing your Joint Strategic Commissioning Plan for Older People n Audit Scotland (March 2012) Commissioning Social Care n Scottish Government (Sept 2012) Integration of Health and Social Care in Scotland response to consultation (2013) 82
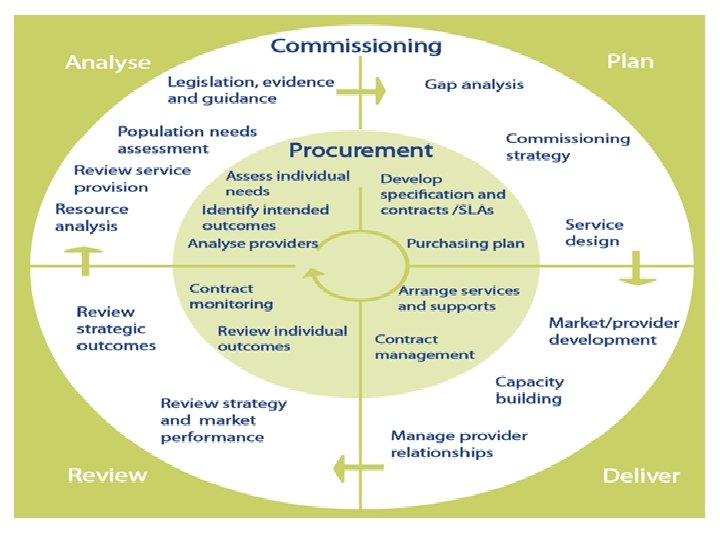
 The basic ideas are clear n Strategic commissioning is the term used for all the activities involved in assessing and forecasting needs, linking investment to agreed desired outcomes, considering options, planning the nature, range and quality of future services and working in partnership to put these in place. n Joint commissioning is where these actions are undertaken by two or more agencies working together, typically health and local government, and often from a pooled or aligned budget. 83
The basic ideas are clear n Strategic commissioning is the term used for all the activities involved in assessing and forecasting needs, linking investment to agreed desired outcomes, considering options, planning the nature, range and quality of future services and working in partnership to put these in place. n Joint commissioning is where these actions are undertaken by two or more agencies working together, typically health and local government, and often from a pooled or aligned budget. 83
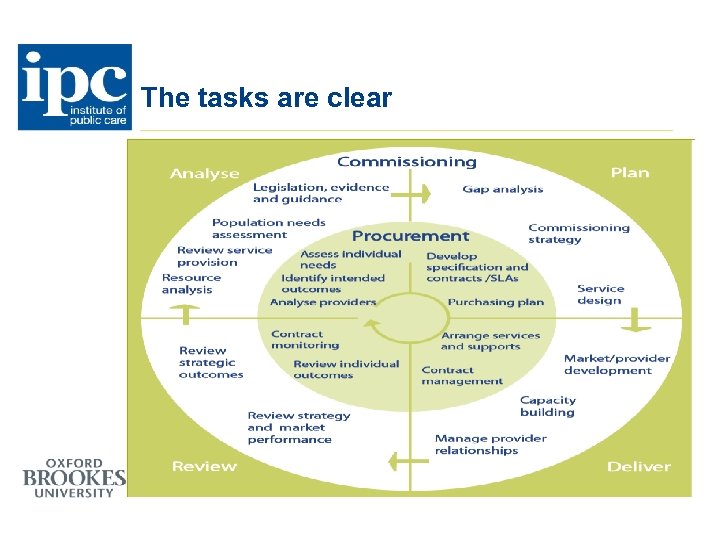 The tasks are clear
The tasks are clear
 The rationale is clear n Strategic commissioning is about taking a systematic, unbiased, in depth look at the needs of a local population, and configuring all the resources at your disposal to make sure you get the best possible outcomes for that population. n It is ONLY a methodology, a way of doing things. n It can be used in lots of different circumstances, but there are some basic principles: 85
The rationale is clear n Strategic commissioning is about taking a systematic, unbiased, in depth look at the needs of a local population, and configuring all the resources at your disposal to make sure you get the best possible outcomes for that population. n It is ONLY a methodology, a way of doing things. n It can be used in lots of different circumstances, but there are some basic principles: 85
 The basic principles are clear n Focus on a defined population, not limited to a service perspective. n Be systematic – analyse, plan, deliver, review – its a package. n Apply to all relevant resources. n It is a costly change management approach focusing on both human and technical systems – don’t do it if you don’t want or can’t achieve change. 86
The basic principles are clear n Focus on a defined population, not limited to a service perspective. n Be systematic – analyse, plan, deliver, review – its a package. n Apply to all relevant resources. n It is a costly change management approach focusing on both human and technical systems – don’t do it if you don’t want or can’t achieve change. 86
 The value of JSC is clear n It starts and ends with the overall needs of the population – individual services and individual professionals can’t do this. n It requires a systematic approach - most change programmes fail to deliver. n It involves understanding the whole system involved in meeting people’s needs and the inter-relationship between different agencies, services, people and pathways – most redesign programmes fail to consider these. n It requires a focus on evidence and analysis rather than political preference. . . 87
The value of JSC is clear n It starts and ends with the overall needs of the population – individual services and individual professionals can’t do this. n It requires a systematic approach - most change programmes fail to deliver. n It involves understanding the whole system involved in meeting people’s needs and the inter-relationship between different agencies, services, people and pathways – most redesign programmes fail to consider these. n It requires a focus on evidence and analysis rather than political preference. . . 87
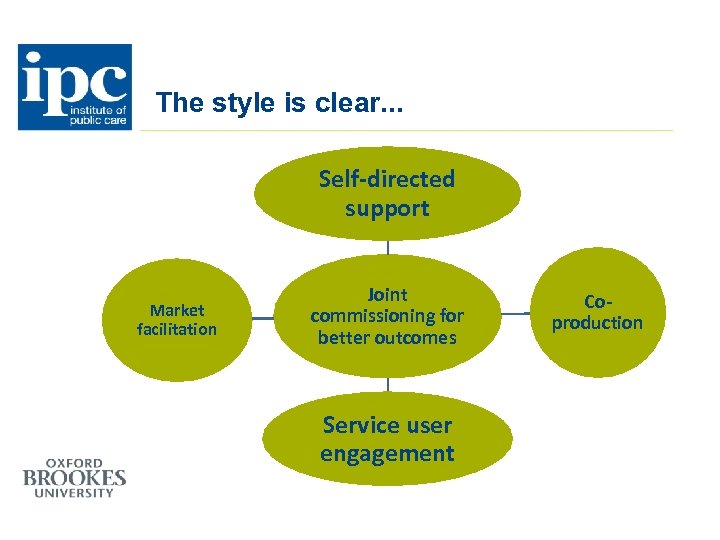 The style is clear. . . Self-directed support Market facilitation Joint commissioning for better outcomes Service user engagement Coproduction
The style is clear. . . Self-directed support Market facilitation Joint commissioning for better outcomes Service user engagement Coproduction
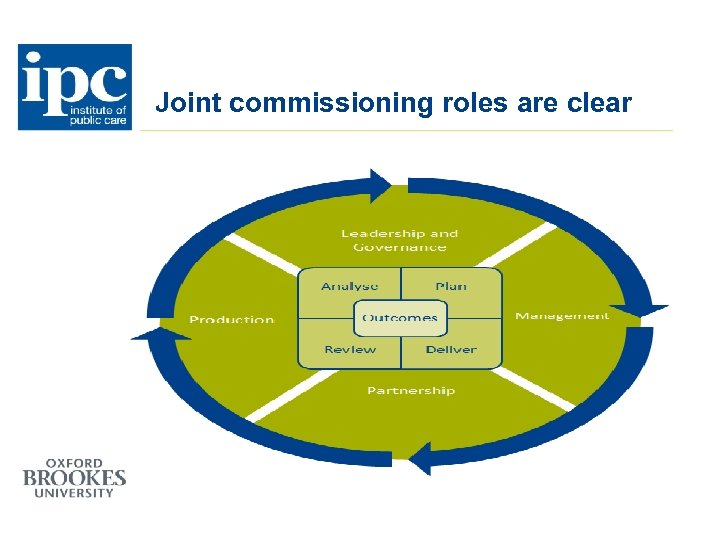 Joint commissioning roles are clear
Joint commissioning roles are clear
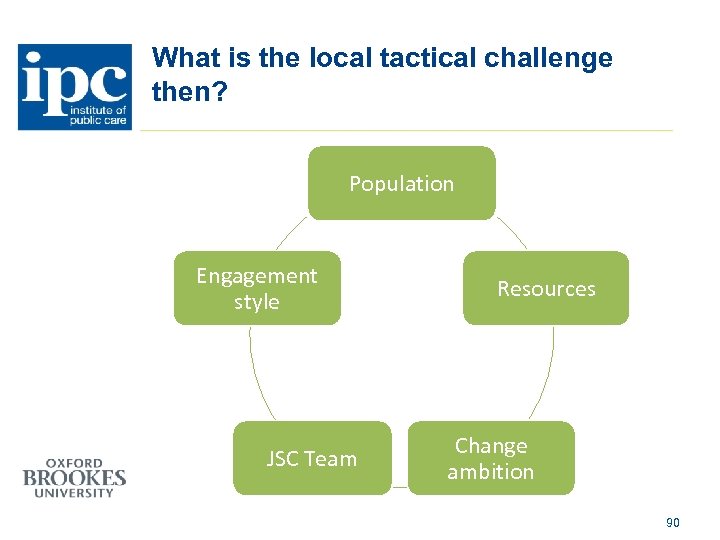 What is the local tactical challenge then? Population Engagement style JSC Team Resources Change ambition 90
What is the local tactical challenge then? Population Engagement style JSC Team Resources Change ambition 90
 Population n Needs to be local decision based on local priorities n Focus on POPULATIONS and their needs, not conditions, services or pathways n Be clear about geographic and age boundaries and their rationale n Tactically unrealistic to consider all age populations – unless focused on a very local geographical boundary, and drawing in all public, private and community resources 91
Population n Needs to be local decision based on local priorities n Focus on POPULATIONS and their needs, not conditions, services or pathways n Be clear about geographic and age boundaries and their rationale n Tactically unrealistic to consider all age populations – unless focused on a very local geographical boundary, and drawing in all public, private and community resources 91
 Population n Not enough, for example, in your strategy to focus only on: n Reducing acute demand n Reducing residential demand n Reducing length of stays n Improving discharge n Early years support n Fostering n Respire care n Although these might be very legitimate agendas for your procurement plans, SLAs, or Market Position Statements 92
Population n Not enough, for example, in your strategy to focus only on: n Reducing acute demand n Reducing residential demand n Reducing length of stays n Improving discharge n Early years support n Fostering n Respire care n Although these might be very legitimate agendas for your procurement plans, SLAs, or Market Position Statements 92
 Services and Resources n Impact of joint strategic commissioning relies on the extent to which resources are ‘in the pot’. n Secure commitment and agreement at the front end of the work to the services and resources to be considered. n Don’t go ahead without that commitment - rescope. n This commitment dictates the ambition of the work, we have never been involved in a strategic commissioning project which has increased the span of resources in the course of a project successfully without a complete rescope. 93
Services and Resources n Impact of joint strategic commissioning relies on the extent to which resources are ‘in the pot’. n Secure commitment and agreement at the front end of the work to the services and resources to be considered. n Don’t go ahead without that commitment - rescope. n This commitment dictates the ambition of the work, we have never been involved in a strategic commissioning project which has increased the span of resources in the course of a project successfully without a complete rescope. 93
 Ambition n Key stakeholder s need to understand the service implications of a joint strategic commissioning approach from the start. n We use ‘hypotheses’ to stimulate this understanding - key questions about services which need to be answered by the approach. n Stakeholders also need to decide HOW they will use JSC. . 94
Ambition n Key stakeholder s need to understand the service implications of a joint strategic commissioning approach from the start. n We use ‘hypotheses’ to stimulate this understanding - key questions about services which need to be answered by the approach. n Stakeholders also need to decide HOW they will use JSC. . 94
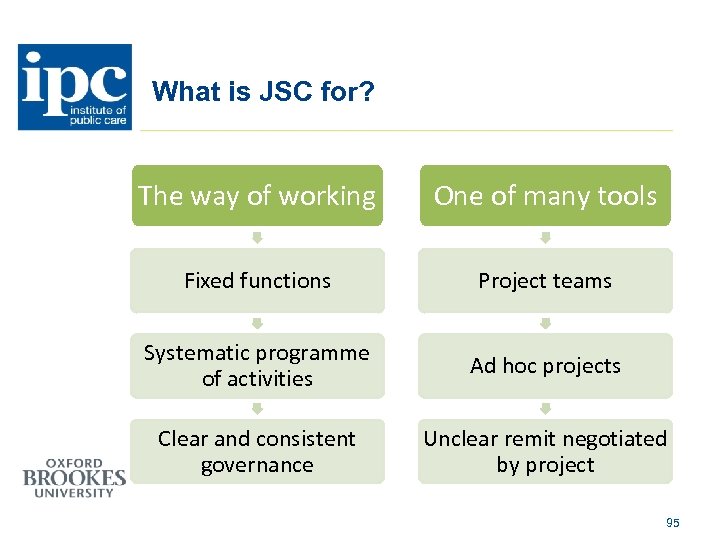 What is JSC for? The way of working One of many tools Fixed functions Project teams Systematic programme of activities Ad hoc projects Clear and consistent governance Unclear remit negotiated by project 95
What is JSC for? The way of working One of many tools Fixed functions Project teams Systematic programme of activities Ad hoc projects Clear and consistent governance Unclear remit negotiated by project 95
 JSC Team n Fixed or project based approach is first key decision n Whether the function leads or supports JSC is second key decision n Must have technical (needs, research, procurement) and field credibility between them n Best balance is combination of fixed resource and seconded / project based teams n Must be led by or report to most senior executives responsible for services to the relevant population 96
JSC Team n Fixed or project based approach is first key decision n Whether the function leads or supports JSC is second key decision n Must have technical (needs, research, procurement) and field credibility between them n Best balance is combination of fixed resource and seconded / project based teams n Must be led by or report to most senior executives responsible for services to the relevant population 96
 Engagement style n Extent to which strategic decision making processes are separate, parallel or integrated n Relative influence of professionals, service users and carers, service providers, politicians, the public n Balance usually depends on extent to which changes need to focus on service provision, service quality or systems and pathways n Design projects which draw on best change management approaches – be very deliberate in their application n If you want mature relationships you need mature approaches to change 97
Engagement style n Extent to which strategic decision making processes are separate, parallel or integrated n Relative influence of professionals, service users and carers, service providers, politicians, the public n Balance usually depends on extent to which changes need to focus on service provision, service quality or systems and pathways n Design projects which draw on best change management approaches – be very deliberate in their application n If you want mature relationships you need mature approaches to change 97
 Example 1. Project set-up n Purpose and priorities, people and framework 2. Analyse priorities / evidence n Research and best practice evidence n Key national drivers and local priorities n Stakeholder consensus 3. Analyse need n Population analyses and prediction of future needs n Service user analysis n Stakeholder consensus 98
Example 1. Project set-up n Purpose and priorities, people and framework 2. Analyse priorities / evidence n Research and best practice evidence n Key national drivers and local priorities n Stakeholder consensus 3. Analyse need n Population analyses and prediction of future needs n Service user analysis n Stakeholder consensus 98
 Example (cont) 4. Analyse services and resources n Market mapping, benchmarking n Contracting arrangements n Resource analyses n Stakeholders consensus 5. Analyse service quality n Illustrative case studies n Stakeholder interviews 6. Analyse strengths and gaps n Draft findings n Analysis testing n Stakeholder consensus 7. Plan n Design, consensus and risk testing n Commissioning Strategy 99
Example (cont) 4. Analyse services and resources n Market mapping, benchmarking n Contracting arrangements n Resource analyses n Stakeholders consensus 5. Analyse service quality n Illustrative case studies n Stakeholder interviews 6. Analyse strengths and gaps n Draft findings n Analysis testing n Stakeholder consensus 7. Plan n Design, consensus and risk testing n Commissioning Strategy 99
 Example (cont) 8. Deliver n Communicate intentions including MPS n Service specifications n Tendering n Contracts n SLAs 9. Monitor and Review n User feedback n Performance indicators n Activity information n Changes in need 100
Example (cont) 8. Deliver n Communicate intentions including MPS n Service specifications n Tendering n Contracts n SLAs 9. Monitor and Review n User feedback n Performance indicators n Activity information n Changes in need 100
 Challenges n Commissioning model proposed is based on joint planning , co-production and involvement of all stakeholders, not a simplistic separation of purchasers/providers. Engagement is time consuming and expensive and might not be worth it for individual services. Will all sectors want to engage? n Outcomes must be the starting point and drivers for change. Services based on reward for outcomes carry significant business risk n SDS will have a very significant impact. Public sector will have less influence over purchasing of services. Big businesses will have more routes to market and capacity to invest. They see longer term opportunities. Smaller providers are experiencing cash flow squeeze. 101
Challenges n Commissioning model proposed is based on joint planning , co-production and involvement of all stakeholders, not a simplistic separation of purchasers/providers. Engagement is time consuming and expensive and might not be worth it for individual services. Will all sectors want to engage? n Outcomes must be the starting point and drivers for change. Services based on reward for outcomes carry significant business risk n SDS will have a very significant impact. Public sector will have less influence over purchasing of services. Big businesses will have more routes to market and capacity to invest. They see longer term opportunities. Smaller providers are experiencing cash flow squeeze. 101
 Challenges n Mature commissioning is going to mean market facilitation – MPS is first step to understanding what information providers need to operate effectively n To secure a shift to prevention, acute sector services and budgets will need to be considered with community health and social care n What if what individual citizens want is NOT the same as what the population ‘needs’? n Community based services do not inevitably result in prevention – they may actually draw people into acute or substitute care. n Financial climate is challenging everyone. Don’t assume it will look the same at the end of the recession. 102
Challenges n Mature commissioning is going to mean market facilitation – MPS is first step to understanding what information providers need to operate effectively n To secure a shift to prevention, acute sector services and budgets will need to be considered with community health and social care n What if what individual citizens want is NOT the same as what the population ‘needs’? n Community based services do not inevitably result in prevention – they may actually draw people into acute or substitute care. n Financial climate is challenging everyone. Don’t assume it will look the same at the end of the recession. 102
 Contact us n n http: //ipc. brookes. ac. uk ipc@brookes. ac. uk kmoultrie@brookes. ac. uk 01225 484088 103
Contact us n n http: //ipc. brookes. ac. uk ipc@brookes. ac. uk kmoultrie@brookes. ac. uk 01225 484088 103

 Michelle Sutherland Partnership Facilitator North Ayrshire CHCP
Michelle Sutherland Partnership Facilitator North Ayrshire CHCP
 A Partnership approach to Joint Commissioning Planning -An Ayrshire perspective
A Partnership approach to Joint Commissioning Planning -An Ayrshire perspective

 Rationale • Existing Pan Ayrshire Change fund activities • Existing relationships with our third and independent sector • Capitalised on existing governance arrangements to Health Board, Councils and CPP • Reducing duplication of effort across whole system • Single whole system performance using Covalent
Rationale • Existing Pan Ayrshire Change fund activities • Existing relationships with our third and independent sector • Capitalised on existing governance arrangements to Health Board, Councils and CPP • Reducing duplication of effort across whole system • Single whole system performance using Covalent
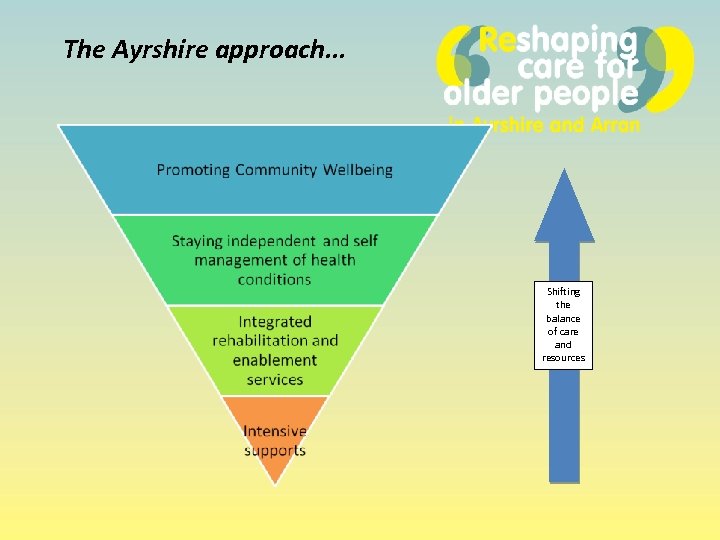 The Ayrshire approach. . . Shifting the balance of care and resources
The Ayrshire approach. . . Shifting the balance of care and resources
 What did we do? • Managing Successful Programme approach • Programme Board established • Senior responsible officers x 2 (NHS and local authorities) • Finance, communication and workforce sub groups established. • CHPs agreed as delivery vehicles
What did we do? • Managing Successful Programme approach • Programme Board established • Senior responsible officers x 2 (NHS and local authorities) • Finance, communication and workforce sub groups established. • CHPs agreed as delivery vehicles
 What worked? • Strengthened Relationships • Common vision and ambition with local priorities • Single engagement message across partnerships, with staff and communities • Allowed us to consider good practice across Ayrshire as our wicked problems are common • Agreed pooled budget and financial model • Governance
What worked? • Strengthened Relationships • Common vision and ambition with local priorities • Single engagement message across partnerships, with staff and communities • Allowed us to consider good practice across Ayrshire as our wicked problems are common • Agreed pooled budget and financial model • Governance
 What didn’t work so well? • Pan Ayrshire Programme Board large • Resource intensive but additional support provided by partners • Focus moved to strategic and required balance with front line service change • Local Partnership Commissioning not moved to Pan Ayrshire joint commissioning yet
What didn’t work so well? • Pan Ayrshire Programme Board large • Resource intensive but additional support provided by partners • Focus moved to strategic and required balance with front line service change • Local Partnership Commissioning not moved to Pan Ayrshire joint commissioning yet
 Phil White Partnership Facilitator South Ayrshire CHCP
Phil White Partnership Facilitator South Ayrshire CHCP
 Communication and engagement • Substantive engagement strategy developed • Opted for continuous engagement process • All partners engaged • Supported by partnership communications teams • Pan Ayrshire message delivered with locality focus • Sharing of public information across systems • Standardised engagement tool kit • DVD developed, and booklet developed – widely disseminated
Communication and engagement • Substantive engagement strategy developed • Opted for continuous engagement process • All partners engaged • Supported by partnership communications teams • Pan Ayrshire message delivered with locality focus • Sharing of public information across systems • Standardised engagement tool kit • DVD developed, and booklet developed – widely disseminated
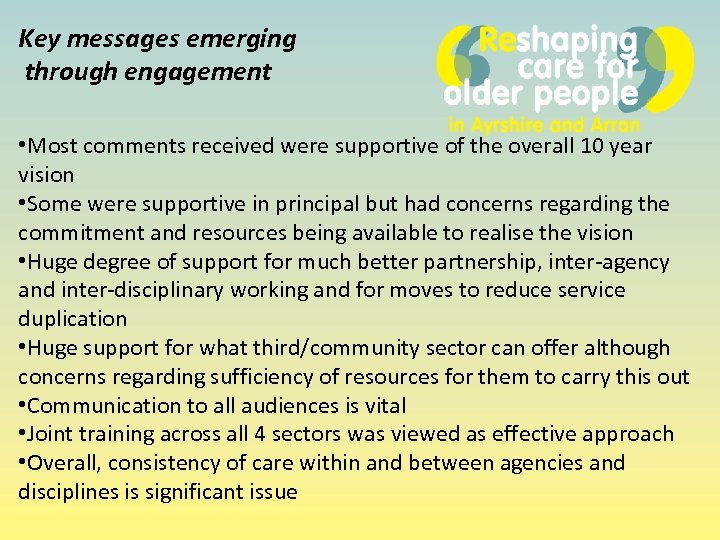 Key messages emerging through engagement • Most comments received were supportive of the overall 10 year vision • Some were supportive in principal but had concerns regarding the commitment and resources being available to realise the vision • Huge degree of support for much better partnership, inter-agency and inter-disciplinary working and for moves to reduce service duplication • Huge support for what third/community sector can offer although concerns regarding sufficiency of resources for them to carry this out • Communication to all audiences is vital • Joint training across all 4 sectors was viewed as effective approach • Overall, consistency of care within and between agencies and disciplines is significant issue
Key messages emerging through engagement • Most comments received were supportive of the overall 10 year vision • Some were supportive in principal but had concerns regarding the commitment and resources being available to realise the vision • Huge degree of support for much better partnership, inter-agency and inter-disciplinary working and for moves to reduce service duplication • Huge support for what third/community sector can offer although concerns regarding sufficiency of resources for them to carry this out • Communication to all audiences is vital • Joint training across all 4 sectors was viewed as effective approach • Overall, consistency of care within and between agencies and disciplines is significant issue
 What didn’t work so well? • Tight timetable – including Christmas • Community groups already had agendas arranged • Not all groups participated in engagement – despite mechanisms in place Also. . . We still need to ensure ongoing dialogue
What didn’t work so well? • Tight timetable – including Christmas • Community groups already had agendas arranged • Not all groups participated in engagement – despite mechanisms in place Also. . . We still need to ensure ongoing dialogue
 Embedding Community Capacity and Co-production in Reshaping Care
Embedding Community Capacity and Co-production in Reshaping Care
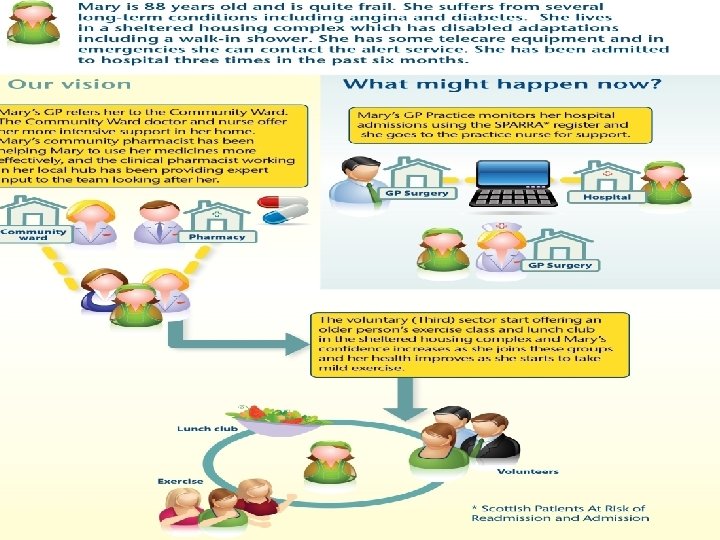
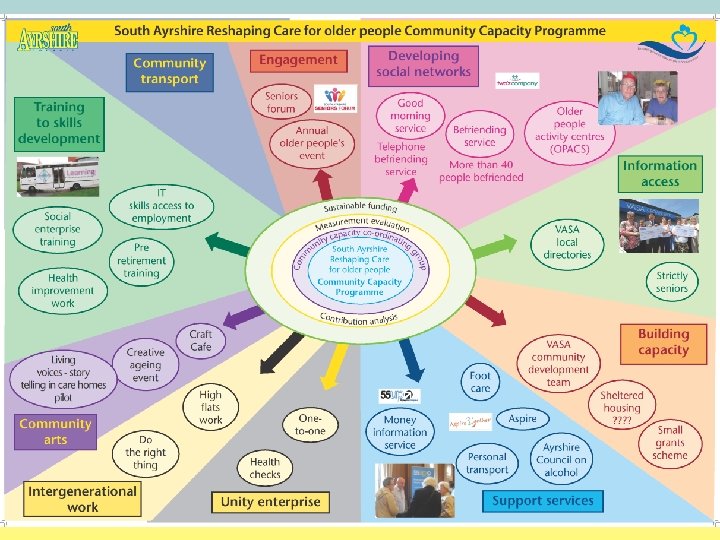
 In Ayrshire partnerships the third and independent sectors have been viewed as essential partners in delivering our strategic plans (both in relation to Change Fund and the longer term Reshaping Care 10 year plans). In relation to the Community Capacity Building part of the planning the third sector interfaces have been vital players in relation to this. The next slide shows a summary of the Community Capacity programme within South Ayrshire illustrating the breadth and importance of this work strand as a discrete entity but also contributing to the other tiers of work.
In Ayrshire partnerships the third and independent sectors have been viewed as essential partners in delivering our strategic plans (both in relation to Change Fund and the longer term Reshaping Care 10 year plans). In relation to the Community Capacity Building part of the planning the third sector interfaces have been vital players in relation to this. The next slide shows a summary of the Community Capacity programme within South Ayrshire illustrating the breadth and importance of this work strand as a discrete entity but also contributing to the other tiers of work.
 Michelle Sutherland – Partnership Facilitator North Ayrshire Community Health Partnership Phil White – Partnership Facilitator South Ayrshire Community Health Partnership and. . . Shiona Johnstone – Partnership Facilitator East Ayrshire Community Health Partnership
Michelle Sutherland – Partnership Facilitator North Ayrshire Community Health Partnership Phil White – Partnership Facilitator South Ayrshire Community Health Partnership and. . . Shiona Johnstone – Partnership Facilitator East Ayrshire Community Health Partnership

 Dr. Erik Sutherland Planning and Performance Manager East Renfrewshire CHCP
Dr. Erik Sutherland Planning and Performance Manager East Renfrewshire CHCP
 Co-producing our Joint Strategic Commissioning Plan East Renfrewshire Reshaping Care for Older People Erik Sutherland 14 th May 2013
Co-producing our Joint Strategic Commissioning Plan East Renfrewshire Reshaping Care for Older People Erik Sutherland 14 th May 2013
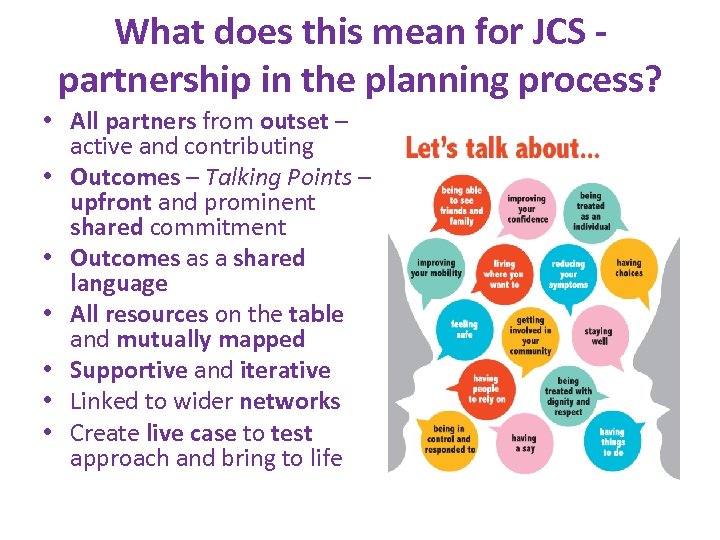 What does this mean for JCS partnership in the planning process? • All partners from outset – active and contributing • Outcomes – Talking Points – upfront and prominent shared commitment • Outcomes as a shared language • All resources on the table and mutually mapped • Supportive and iterative • Linked to wider networks • Create live case to test approach and bring to life
What does this mean for JCS partnership in the planning process? • All partners from outset – active and contributing • Outcomes – Talking Points – upfront and prominent shared commitment • Outcomes as a shared language • All resources on the table and mutually mapped • Supportive and iterative • Linked to wider networks • Create live case to test approach and bring to life
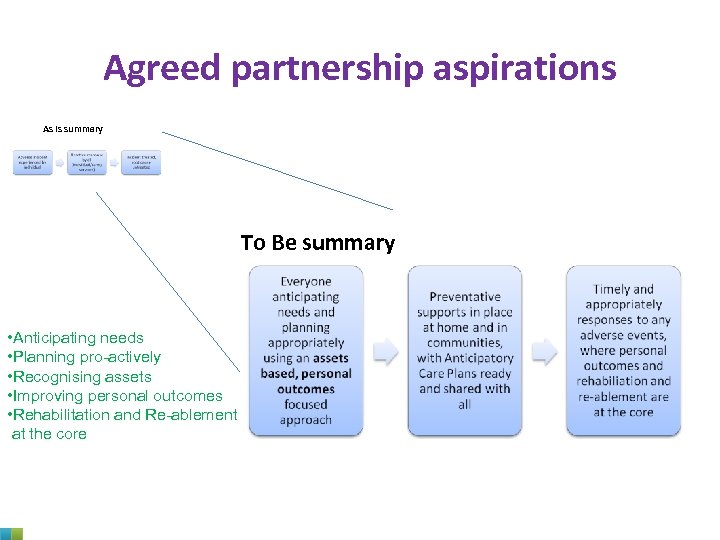 Agreed partnership aspirations As Is summary To Be summary • Anticipating needs • Planning pro-actively • Recognising assets • Improving personal outcomes • Rehabilitation and Re-ablement at the core
Agreed partnership aspirations As Is summary To Be summary • Anticipating needs • Planning pro-actively • Recognising assets • Improving personal outcomes • Rehabilitation and Re-ablement at the core
 Conclusions and organisational learning • ‘Limited’ extent of co-production to strategic commissioning plan but principal plan shaping direction over long-term • Live and purposeful approach which generates fresh thinking and new ideas • More comprehensive ‘model of care’ from all partner perspectives • Approach itself can strengthen relationships • Need for building on these foundations • Broaden and deepen co-production in implementation phase
Conclusions and organisational learning • ‘Limited’ extent of co-production to strategic commissioning plan but principal plan shaping direction over long-term • Live and purposeful approach which generates fresh thinking and new ideas • More comprehensive ‘model of care’ from all partner perspectives • Approach itself can strengthen relationships • Need for building on these foundations • Broaden and deepen co-production in implementation phase


 Dr. Margaret Whoriskey Director Joint Improvement Team
Dr. Margaret Whoriskey Director Joint Improvement Team
 Chaired by: Dr. Margaret Whoriskey, JIT Ron Culley, COSLA Ranald Mair, Scottish Care Annie Gunner Logan, CCPS Keith Moultrie, IPC Heather Kelman, NHS Grampian
Chaired by: Dr. Margaret Whoriskey, JIT Ron Culley, COSLA Ranald Mair, Scottish Care Annie Gunner Logan, CCPS Keith Moultrie, IPC Heather Kelman, NHS Grampian
 • Is your partnership shifting activity to community upstream ? Yes or No
• Is your partnership shifting activity to community upstream ? Yes or No
 • Is your partnership shifting the resources ? Yes or No
• Is your partnership shifting the resources ? Yes or No
 • Are you confident that your partnership is doing enough of the right things to meet the challenges ? Yes or No
• Are you confident that your partnership is doing enough of the right things to meet the challenges ? Yes or No
 • Do you feel your partnership is enthusiastically embracing shift towards co production and community capacity ? Yes or No
• Do you feel your partnership is enthusiastically embracing shift towards co production and community capacity ? Yes or No
 • Are you clearer now about the areas for improvement needed to strengthen your local joint strategic community approval? Yes or No
• Are you clearer now about the areas for improvement needed to strengthen your local joint strategic community approval? Yes or No

 Close of Conference
Close of Conference



