c8ae79fe3591fbfb2d1107a110eb64d9.ppt
- Количество слайдов: 33
 Central Venous Access Office of Graduate Medical Education Perelman School of Medicine University of Pennsylvania Slides Courtesy of : Joan Hoch Kinniry ACNP-BC Lead Practitioner , Critical Care Medicine, Procedure and Resuscitation Service
Central Venous Access Office of Graduate Medical Education Perelman School of Medicine University of Pennsylvania Slides Courtesy of : Joan Hoch Kinniry ACNP-BC Lead Practitioner , Critical Care Medicine, Procedure and Resuscitation Service
 Central Venous Line Placement n Goals n n Reduce anxiety about procedures Review basics n n n n Indications Complications Mechanics Improve familiarity with various catheter types Establish good habits and solid foundation Improve confidence and competency Ensure safe and sterile catheter placement
Central Venous Line Placement n Goals n n Reduce anxiety about procedures Review basics n n n n Indications Complications Mechanics Improve familiarity with various catheter types Establish good habits and solid foundation Improve confidence and competency Ensure safe and sterile catheter placement
 Central Venous Line Placement n Indications n Hemodynamic monitoring n n n CVP / Scv 02 PA-Catheters (Swan-Ganz, RHC) Administration of hyperosmolar agents, vasopressors and other medications Temporary transvenous cardiac pacing Hemodialysis and plasmapheresis Lack of peripheral access
Central Venous Line Placement n Indications n Hemodynamic monitoring n n n CVP / Scv 02 PA-Catheters (Swan-Ganz, RHC) Administration of hyperosmolar agents, vasopressors and other medications Temporary transvenous cardiac pacing Hemodialysis and plasmapheresis Lack of peripheral access
 Central Venous Line Placement n Absolute contraindications n n None Relative contraindications n n n Coagulopathy / thrombocytopenia Anatomic abnormalities Thrombus / stenosis Localized infection over insertion site Recent pacemaker insertion
Central Venous Line Placement n Absolute contraindications n n None Relative contraindications n n n Coagulopathy / thrombocytopenia Anatomic abnormalities Thrombus / stenosis Localized infection over insertion site Recent pacemaker insertion
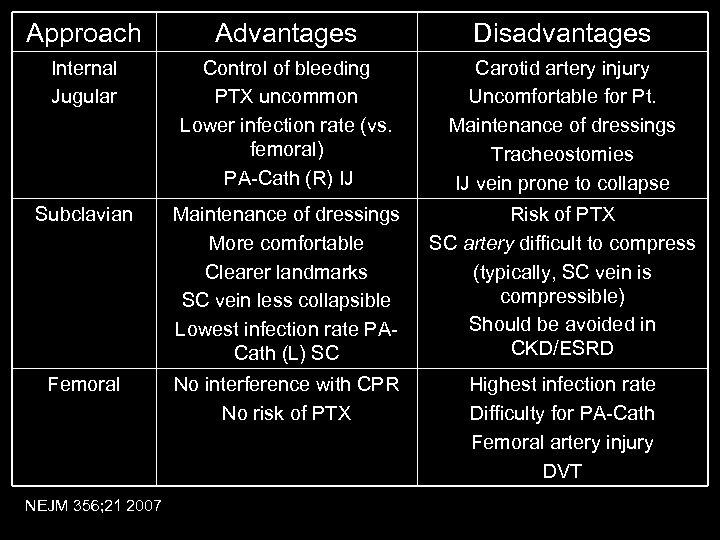 Approach Advantages Disadvantages Internal Jugular Control of bleeding PTX uncommon Lower infection rate (vs. femoral) PA-Cath (R) IJ Carotid artery injury Uncomfortable for Pt. Maintenance of dressings Tracheostomies IJ vein prone to collapse Subclavian Maintenance of dressings More comfortable Clearer landmarks SC vein less collapsible Lowest infection rate PACath (L) SC Risk of PTX SC artery difficult to compress (typically, SC vein is compressible) Should be avoided in CKD/ESRD Femoral No interference with CPR No risk of PTX Highest infection rate Difficulty for PA-Cath Femoral artery injury DVT NEJM 356; 21 2007
Approach Advantages Disadvantages Internal Jugular Control of bleeding PTX uncommon Lower infection rate (vs. femoral) PA-Cath (R) IJ Carotid artery injury Uncomfortable for Pt. Maintenance of dressings Tracheostomies IJ vein prone to collapse Subclavian Maintenance of dressings More comfortable Clearer landmarks SC vein less collapsible Lowest infection rate PACath (L) SC Risk of PTX SC artery difficult to compress (typically, SC vein is compressible) Should be avoided in CKD/ESRD Femoral No interference with CPR No risk of PTX Highest infection rate Difficulty for PA-Cath Femoral artery injury DVT NEJM 356; 21 2007
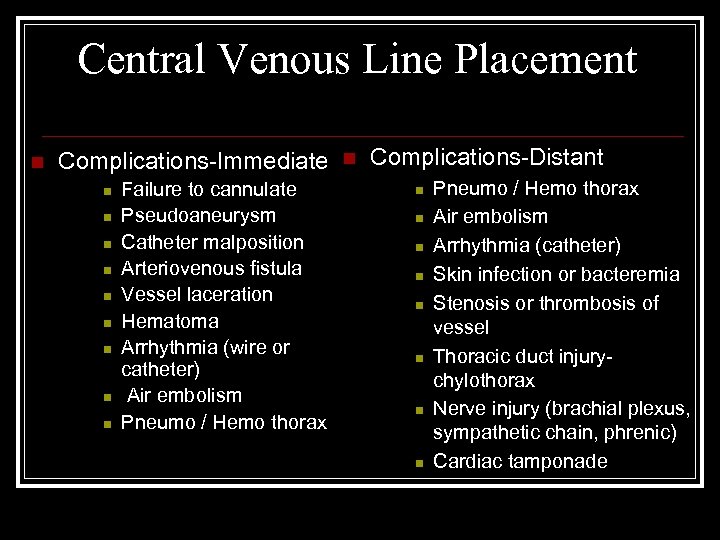 Central Venous Line Placement n Complications-Immediate n n n n n Failure to cannulate Pseudoaneurysm Catheter malposition Arteriovenous fistula Vessel laceration Hematoma Arrhythmia (wire or catheter) Air embolism Pneumo / Hemo thorax n Complications-Distant n n n n Pneumo / Hemo thorax Air embolism Arrhythmia (catheter) Skin infection or bacteremia Stenosis or thrombosis of vessel Thoracic duct injurychylothorax Nerve injury (brachial plexus, sympathetic chain, phrenic) Cardiac tamponade
Central Venous Line Placement n Complications-Immediate n n n n n Failure to cannulate Pseudoaneurysm Catheter malposition Arteriovenous fistula Vessel laceration Hematoma Arrhythmia (wire or catheter) Air embolism Pneumo / Hemo thorax n Complications-Distant n n n n Pneumo / Hemo thorax Air embolism Arrhythmia (catheter) Skin infection or bacteremia Stenosis or thrombosis of vessel Thoracic duct injurychylothorax Nerve injury (brachial plexus, sympathetic chain, phrenic) Cardiac tamponade
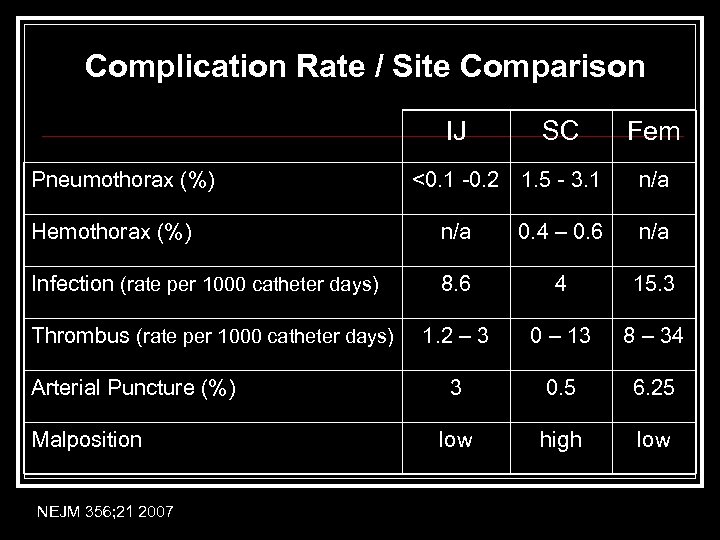 Complication Rate / Site Comparison IJ Pneumothorax (%) SC <0. 1 -0. 2 1. 5 - 3. 1 Fem n/a Hemothorax (%) n/a 0. 4 – 0. 6 n/a Infection (rate per 1000 catheter days) 8. 6 4 15. 3 1. 2 – 3 0 – 13 8 – 34 3 0. 5 6. 25 low high low Thrombus (rate per 1000 catheter days) Arterial Puncture (%) Malposition NEJM 356; 21 2007
Complication Rate / Site Comparison IJ Pneumothorax (%) SC <0. 1 -0. 2 1. 5 - 3. 1 Fem n/a Hemothorax (%) n/a 0. 4 – 0. 6 n/a Infection (rate per 1000 catheter days) 8. 6 4 15. 3 1. 2 – 3 0 – 13 8 – 34 3 0. 5 6. 25 low high low Thrombus (rate per 1000 catheter days) Arterial Puncture (%) Malposition NEJM 356; 21 2007
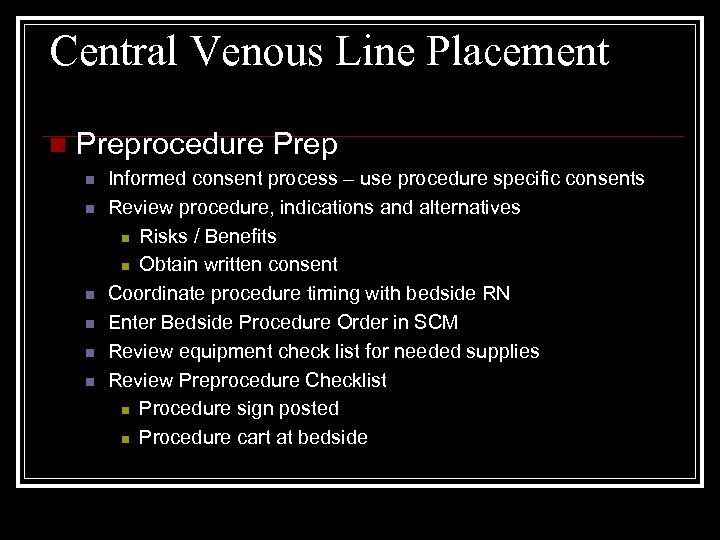 Central Venous Line Placement n Preprocedure Prep n n n Informed consent process – use procedure specific consents Review procedure, indications and alternatives n Risks / Benefits n Obtain written consent Coordinate procedure timing with bedside RN Enter Bedside Procedure Order in SCM Review equipment check list for needed supplies Review Preprocedure Checklist n Procedure sign posted n Procedure cart at bedside
Central Venous Line Placement n Preprocedure Prep n n n Informed consent process – use procedure specific consents Review procedure, indications and alternatives n Risks / Benefits n Obtain written consent Coordinate procedure timing with bedside RN Enter Bedside Procedure Order in SCM Review equipment check list for needed supplies Review Preprocedure Checklist n Procedure sign posted n Procedure cart at bedside
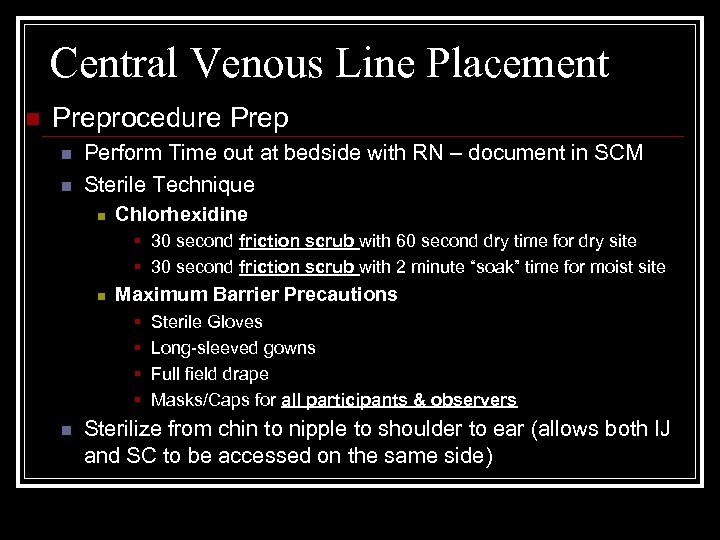 Central Venous Line Placement n Preprocedure Prep n n Perform Time out at bedside with RN – document in SCM Sterile Technique n Chlorhexidine § 30 second friction scrub with 60 second dry time for dry site § 30 second friction scrub with 2 minute “soak” time for moist site n Maximum Barrier Precautions § § n Sterile Gloves Long-sleeved gowns Full field drape Masks/Caps for all participants & observers Sterilize from chin to nipple to shoulder to ear (allows both IJ and SC to be accessed on the same side)
Central Venous Line Placement n Preprocedure Prep n n Perform Time out at bedside with RN – document in SCM Sterile Technique n Chlorhexidine § 30 second friction scrub with 60 second dry time for dry site § 30 second friction scrub with 2 minute “soak” time for moist site n Maximum Barrier Precautions § § n Sterile Gloves Long-sleeved gowns Full field drape Masks/Caps for all participants & observers Sterilize from chin to nipple to shoulder to ear (allows both IJ and SC to be accessed on the same side)
 Central Venous Line Placement PROCEDURE n All IJ lines must be done with US guidance n All lines must be transduced before dilation (verified by performing MD and RN) DOCUMENTATION n Consent n Bedside Procedure Order in (SCM) n Time Out (SCM) n US vessel evaluation note n Procedure Note
Central Venous Line Placement PROCEDURE n All IJ lines must be done with US guidance n All lines must be transduced before dilation (verified by performing MD and RN) DOCUMENTATION n Consent n Bedside Procedure Order in (SCM) n Time Out (SCM) n US vessel evaluation note n Procedure Note
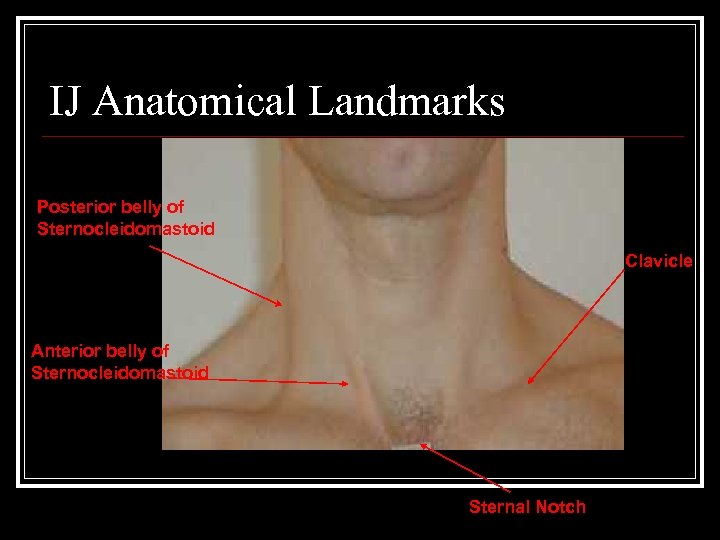 IJ Anatomical Landmarks Posterior belly of Sternocleidomastoid Clavicle Anterior belly of Sternocleidomastoid Sternal Notch
IJ Anatomical Landmarks Posterior belly of Sternocleidomastoid Clavicle Anterior belly of Sternocleidomastoid Sternal Notch
 Subclavian Anatomical Landmarks Clavicle Turn Insertion Point and Trajectory Sternal Notch
Subclavian Anatomical Landmarks Clavicle Turn Insertion Point and Trajectory Sternal Notch
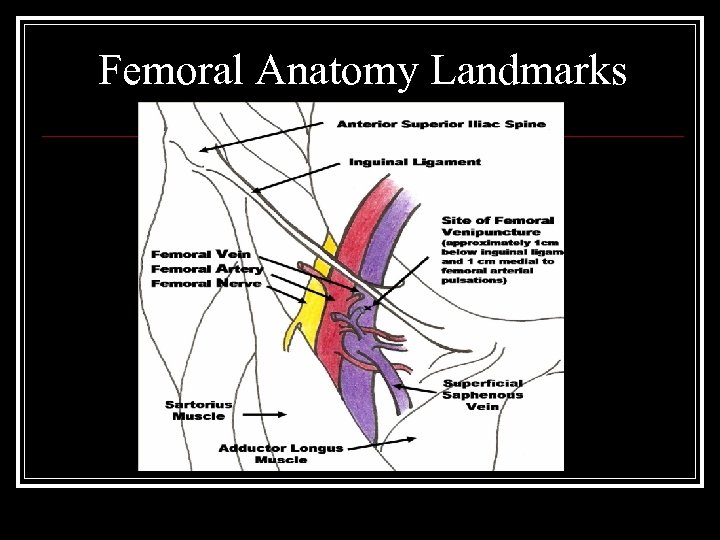 Femoral Anatomy Landmarks
Femoral Anatomy Landmarks
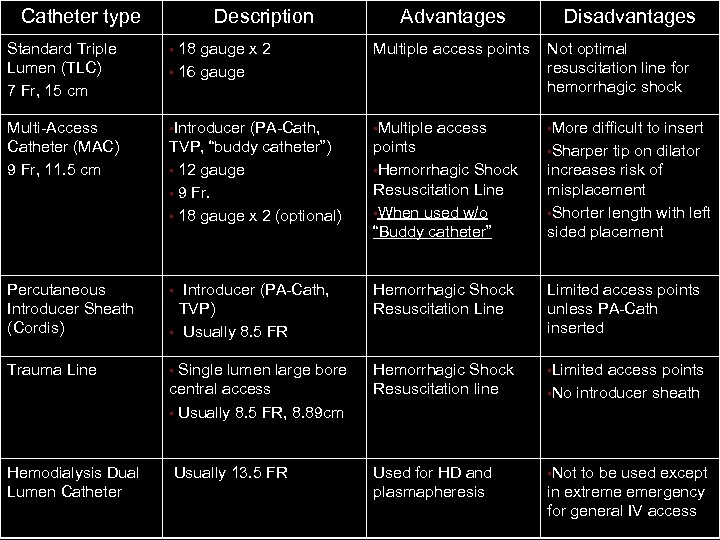 Catheter type Description Advantages Disadvantages Standard Triple Lumen (TLC) 7 Fr, 15 cm • 18 gauge x 2 • 16 gauge Multiple access points Not optimal resuscitation line for hemorrhagic shock Multi-Access Catheter (MAC) 9 Fr, 11. 5 cm • Introducer • Multiple • More Percutaneous Introducer Sheath (Cordis) • Trauma Line • Hemodialysis Dual Lumen Catheter (PA-Cath, TVP, “buddy catheter”) • 12 gauge • 9 Fr. • 18 gauge x 2 (optional) access points • Hemorrhagic Shock Resuscitation Line • When used w/o “Buddy catheter” difficult to insert • Sharper tip on dilator increases risk of misplacement • Shorter length with left sided placement Introducer (PA-Cath, TVP) Usually 8. 5 FR Hemorrhagic Shock Resuscitation Line Limited access points unless PA-Cath inserted Single lumen large bore central access • Usually 8. 5 FR, 8. 89 cm Hemorrhagic Shock Resuscitation line • Limited Usually 13. 5 FR Used for HD and plasmapheresis • Not • access points • No introducer sheath to be used except in extreme emergency for general IV access
Catheter type Description Advantages Disadvantages Standard Triple Lumen (TLC) 7 Fr, 15 cm • 18 gauge x 2 • 16 gauge Multiple access points Not optimal resuscitation line for hemorrhagic shock Multi-Access Catheter (MAC) 9 Fr, 11. 5 cm • Introducer • Multiple • More Percutaneous Introducer Sheath (Cordis) • Trauma Line • Hemodialysis Dual Lumen Catheter (PA-Cath, TVP, “buddy catheter”) • 12 gauge • 9 Fr. • 18 gauge x 2 (optional) access points • Hemorrhagic Shock Resuscitation Line • When used w/o “Buddy catheter” difficult to insert • Sharper tip on dilator increases risk of misplacement • Shorter length with left sided placement Introducer (PA-Cath, TVP) Usually 8. 5 FR Hemorrhagic Shock Resuscitation Line Limited access points unless PA-Cath inserted Single lumen large bore central access • Usually 8. 5 FR, 8. 89 cm Hemorrhagic Shock Resuscitation line • Limited Usually 13. 5 FR Used for HD and plasmapheresis • Not • access points • No introducer sheath to be used except in extreme emergency for general IV access
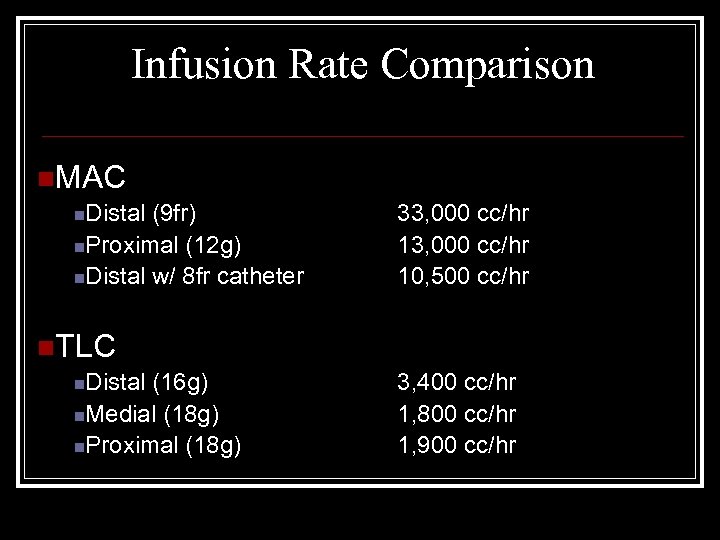 Infusion Rate Comparison n. MAC n. Distal (9 fr) n. Proximal (12 g) n. Distal w/ 8 fr catheter 33, 000 cc/hr 10, 500 cc/hr n. TLC n. Distal (16 g) n. Medial (18 g) n. Proximal (18 g) 3, 400 cc/hr 1, 800 cc/hr 1, 900 cc/hr
Infusion Rate Comparison n. MAC n. Distal (9 fr) n. Proximal (12 g) n. Distal w/ 8 fr catheter 33, 000 cc/hr 10, 500 cc/hr n. TLC n. Distal (16 g) n. Medial (18 g) n. Proximal (18 g) 3, 400 cc/hr 1, 800 cc/hr 1, 900 cc/hr
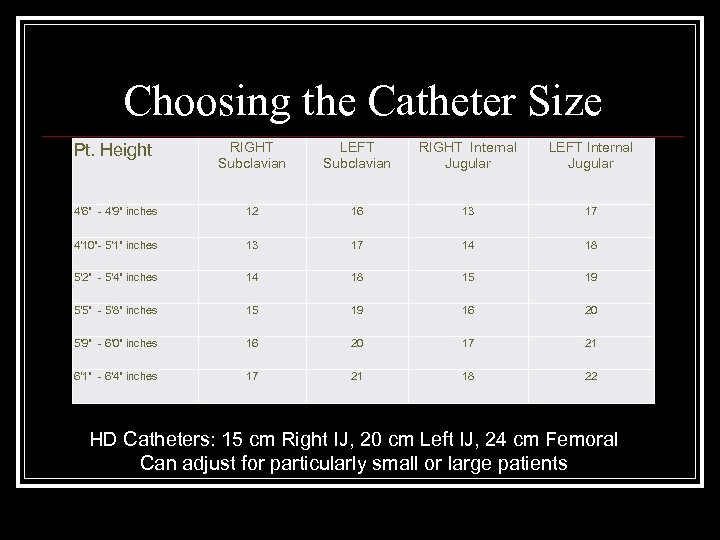 Choosing the Catheter Size Pt. Height RIGHT Subclavian LEFT Subclavian RIGHT Internal Jugular LEFT Internal Jugular 4'6" - 4'9" inches 12 16 13 17 4'10"- 5'1" inches 13 17 14 18 5'2" - 5'4" inches 14 18 15 19 5'5" - 5'8" inches 15 19 16 20 5'9" - 6'0" inches 16 20 17 21 6'1" - 6'4" inches 17 21 18 22 HD Catheters: 15 cm Right IJ, 20 cm Left IJ, 24 cm Femoral Can adjust for particularly small or large patients
Choosing the Catheter Size Pt. Height RIGHT Subclavian LEFT Subclavian RIGHT Internal Jugular LEFT Internal Jugular 4'6" - 4'9" inches 12 16 13 17 4'10"- 5'1" inches 13 17 14 18 5'2" - 5'4" inches 14 18 15 19 5'5" - 5'8" inches 15 19 16 20 5'9" - 6'0" inches 16 20 17 21 6'1" - 6'4" inches 17 21 18 22 HD Catheters: 15 cm Right IJ, 20 cm Left IJ, 24 cm Femoral Can adjust for particularly small or large patients
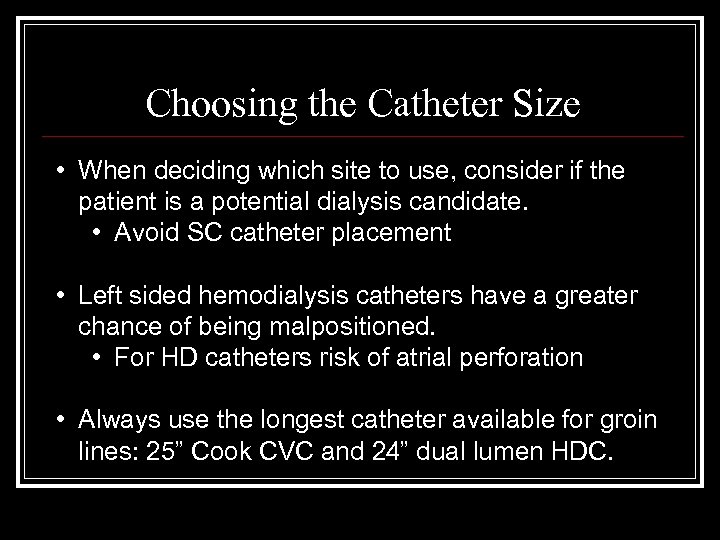 Choosing the Catheter Size • When deciding which site to use, consider if the patient is a potential dialysis candidate. • Avoid SC catheter placement • Left sided hemodialysis catheters have a greater chance of being malpositioned. • For HD catheters risk of atrial perforation • Always use the longest catheter available for groin lines: 25” Cook CVC and 24” dual lumen HDC.
Choosing the Catheter Size • When deciding which site to use, consider if the patient is a potential dialysis candidate. • Avoid SC catheter placement • Left sided hemodialysis catheters have a greater chance of being malpositioned. • For HD catheters risk of atrial perforation • Always use the longest catheter available for groin lines: 25” Cook CVC and 24” dual lumen HDC.
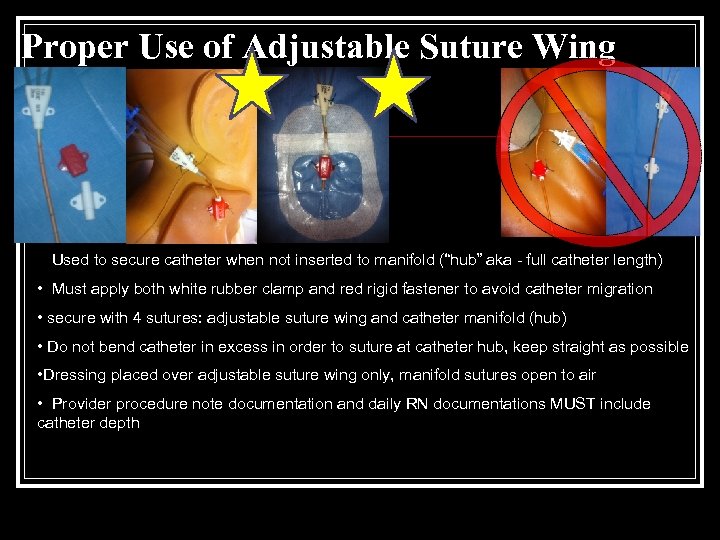 Proper Use of Adjustable Suture Wing • Used to secure catheter when not inserted to manifold (“hub” aka - full catheter length) • Must apply both white rubber clamp and red rigid fastener to avoid catheter migration • secure with 4 sutures: adjustable suture wing and catheter manifold (hub) • Do not bend catheter in excess in order to suture at catheter hub, keep straight as possible • Dressing placed over adjustable suture wing only, manifold sutures open to air • Provider procedure note documentation and daily RN documentations MUST include catheter depth • catheter depth or securement concerns
Proper Use of Adjustable Suture Wing • Used to secure catheter when not inserted to manifold (“hub” aka - full catheter length) • Must apply both white rubber clamp and red rigid fastener to avoid catheter migration • secure with 4 sutures: adjustable suture wing and catheter manifold (hub) • Do not bend catheter in excess in order to suture at catheter hub, keep straight as possible • Dressing placed over adjustable suture wing only, manifold sutures open to air • Provider procedure note documentation and daily RN documentations MUST include catheter depth • catheter depth or securement concerns
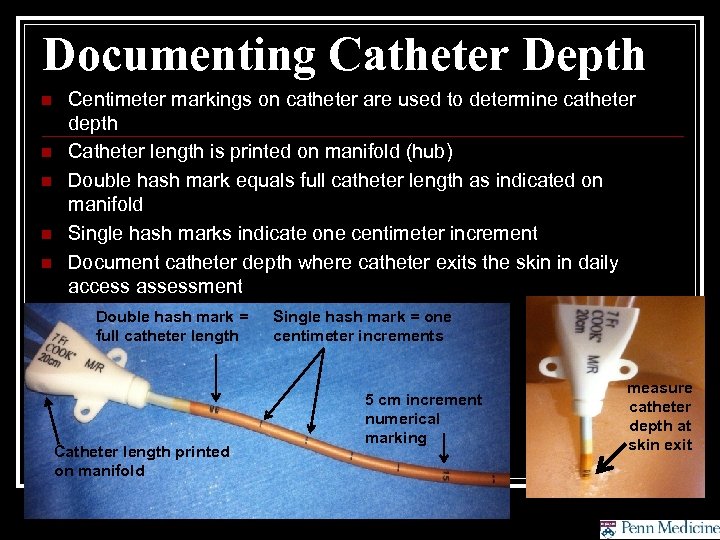 Documenting Catheter Depth n n n Centimeter markings on catheter are used to determine catheter depth Catheter length is printed on manifold (hub) Double hash mark equals full catheter length as indicated on manifold Single hash marks indicate one centimeter increment Document catheter depth where catheter exits the skin in daily access assessment Double hash mark = full catheter length Catheter length printed on manifold Single hash mark = one centimeter increments 5 cm increment numerical marking measure catheter depth at skin exit
Documenting Catheter Depth n n n Centimeter markings on catheter are used to determine catheter depth Catheter length is printed on manifold (hub) Double hash mark equals full catheter length as indicated on manifold Single hash marks indicate one centimeter increment Document catheter depth where catheter exits the skin in daily access assessment Double hash mark = full catheter length Catheter length printed on manifold Single hash mark = one centimeter increments 5 cm increment numerical marking measure catheter depth at skin exit
 Post-Line Insertion Chest X-ray n n Delayed PTX is not unusal – have low threshold to obtain repeat CXR if clinical s/s PTX Single plane view of ICU CXR is suboptimal to evaluate catheter malposition n Transduce waveform via monitor --(can be done without CXR, will demonstrate intravascular placement and arterial vs venous vessel or extravascular placement) Blood gas if intravascular may be useful but clinical conditions can confound interpretation If extravascular catheter is suspected t/c Chest CT w/ contrast
Post-Line Insertion Chest X-ray n n Delayed PTX is not unusal – have low threshold to obtain repeat CXR if clinical s/s PTX Single plane view of ICU CXR is suboptimal to evaluate catheter malposition n Transduce waveform via monitor --(can be done without CXR, will demonstrate intravascular placement and arterial vs venous vessel or extravascular placement) Blood gas if intravascular may be useful but clinical conditions can confound interpretation If extravascular catheter is suspected t/c Chest CT w/ contrast
 Coagulopathic Patients n Caution with INR > 2. 5, PT or PTT > 2 x normal, Plt < 50 k, or untreated uremia (not on HD). The more parameters fulfilled, increases the cumulative effect on hemostasis. n Consider correction (FFP, platelets, ddavp, HD) n Consider IJ placement under US over SC n Coagulopathic state and /or thrombocytopenia are RELATIVE CONTRAINDICATIONS and warrant a risk/benefit discussion with attending
Coagulopathic Patients n Caution with INR > 2. 5, PT or PTT > 2 x normal, Plt < 50 k, or untreated uremia (not on HD). The more parameters fulfilled, increases the cumulative effect on hemostasis. n Consider correction (FFP, platelets, ddavp, HD) n Consider IJ placement under US over SC n Coagulopathic state and /or thrombocytopenia are RELATIVE CONTRAINDICATIONS and warrant a risk/benefit discussion with attending
 Helpful Reminders n n n Recommend restraining all patients during central line placement. (even awake or intact) Keep everything within reach (needles, wire, catheter, flush) Always place patient in trendelenberg (>15 degrees) For SC catheters, placing a rolled towel/sheet in between the scapulae can help “open” the clavicular angle & allow easier passage of the needle underneath the clavicle If wire does not pass: n Re-attach syringe and aspirate (see if still in vessel) n Lower angle of needle (and aspirate) n If wire “clears” the tip of the needle, then consider structural reason (thrombus, anatomic abnormality, ect. ) If the wire does not come out easily, give GENTLE traction and try rotating the wire. DO NOT pull firmly on the wire! n Remove catheter and wire together if able n If unable to remove wire call vascular
Helpful Reminders n n n Recommend restraining all patients during central line placement. (even awake or intact) Keep everything within reach (needles, wire, catheter, flush) Always place patient in trendelenberg (>15 degrees) For SC catheters, placing a rolled towel/sheet in between the scapulae can help “open” the clavicular angle & allow easier passage of the needle underneath the clavicle If wire does not pass: n Re-attach syringe and aspirate (see if still in vessel) n Lower angle of needle (and aspirate) n If wire “clears” the tip of the needle, then consider structural reason (thrombus, anatomic abnormality, ect. ) If the wire does not come out easily, give GENTLE traction and try rotating the wire. DO NOT pull firmly on the wire! n Remove catheter and wire together if able n If unable to remove wire call vascular
 Ultrasound Guided Vascular Access
Ultrasound Guided Vascular Access
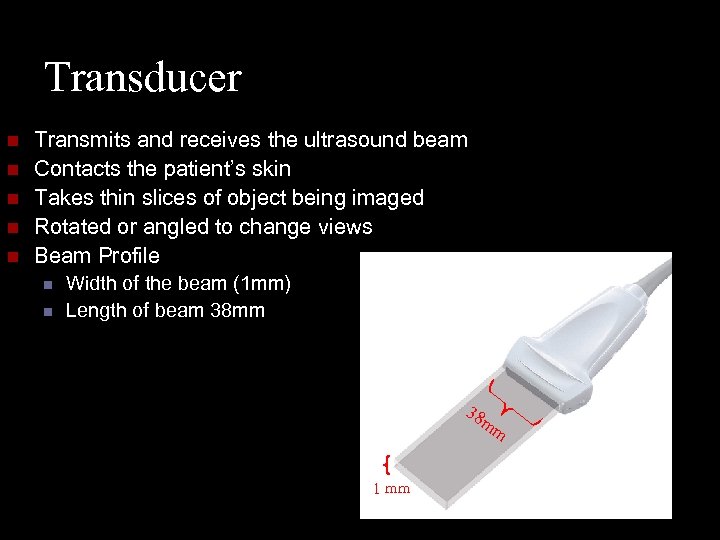 Transducer n n n Transmits and receives the ultrasound beam Contacts the patient’s skin Takes thin slices of object being imaged Rotated or angled to change views Beam Profile n n Width of the beam (1 mm) Length of beam 38 mm 38 mm 1 mm
Transducer n n n Transmits and receives the ultrasound beam Contacts the patient’s skin Takes thin slices of object being imaged Rotated or angled to change views Beam Profile n n Width of the beam (1 mm) Length of beam 38 mm 38 mm 1 mm
 Ultrasound Basics Fluid (i. e. blood) is black b/c near complete transmission of U/S waves occurs n Bone and air cause marked reflection and appear white (in B – mode) n Strong reflection creates an acoustic shadow obscuring distal imaging (bone shadow) n
Ultrasound Basics Fluid (i. e. blood) is black b/c near complete transmission of U/S waves occurs n Bone and air cause marked reflection and appear white (in B – mode) n Strong reflection creates an acoustic shadow obscuring distal imaging (bone shadow) n
 Ultrasound Basics n Most large vessels are easily visualized with U/S probes n n Arteries are pulsatile, difficult to compress and thick walled Veins are non-pulsatile, easily compressible, engorge w/ Trendelenburg or Valsalva and thin walled
Ultrasound Basics n Most large vessels are easily visualized with U/S probes n n Arteries are pulsatile, difficult to compress and thick walled Veins are non-pulsatile, easily compressible, engorge w/ Trendelenburg or Valsalva and thin walled
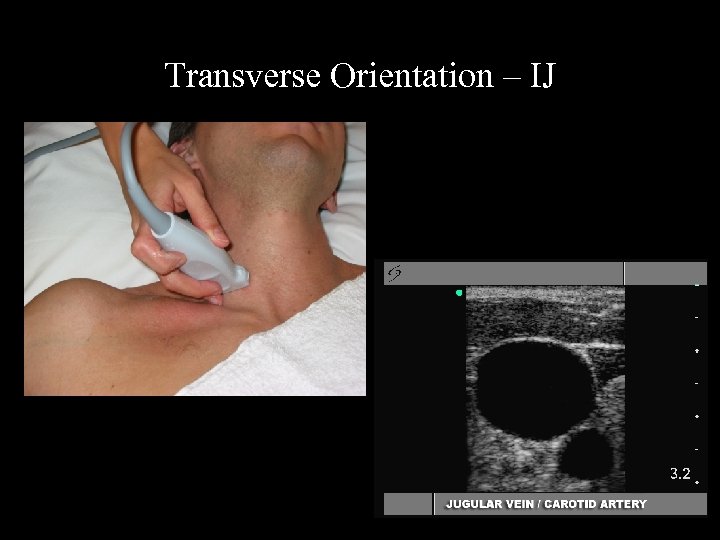 Transverse Orientation – IJ
Transverse Orientation – IJ
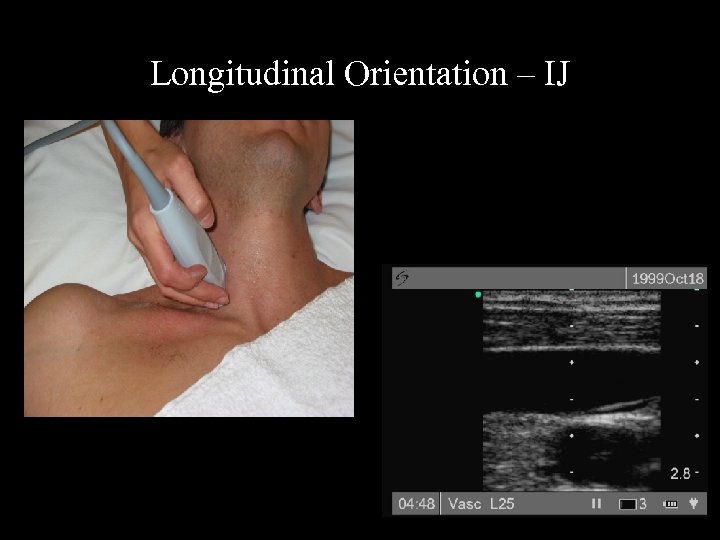 Longitudinal Orientation – IJ
Longitudinal Orientation – IJ
 Transverse Orientation – Subclavian
Transverse Orientation – Subclavian
 Longitudinal Orientation: Subclavian
Longitudinal Orientation: Subclavian
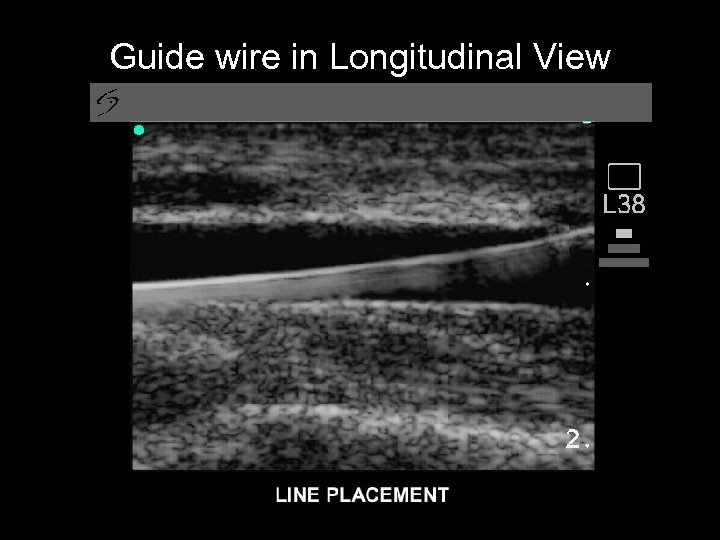 Guide wire in Longitudinal View
Guide wire in Longitudinal View
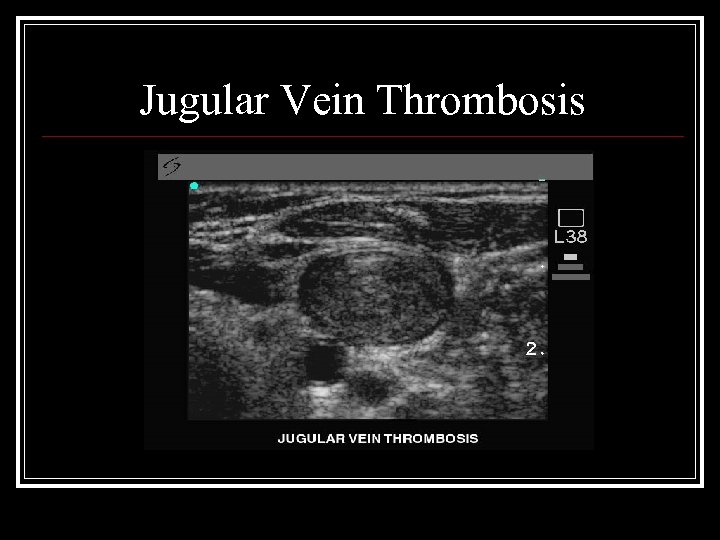 Jugular Vein Thrombosis
Jugular Vein Thrombosis
 Jugular Vein Thrombosis Acute thrombus can appear “black” or “cloudy” on US exam n Always evaluate the whole neck ensuring IJ is fully compressible along the entire length n Presence of small caliber anomalous vessels can be indicative of past or present clot or stenosis n
Jugular Vein Thrombosis Acute thrombus can appear “black” or “cloudy” on US exam n Always evaluate the whole neck ensuring IJ is fully compressible along the entire length n Presence of small caliber anomalous vessels can be indicative of past or present clot or stenosis n


