7ead267cd0fc665efa3113ade18baca7.ppt
- Количество слайдов: 62
CCM Specialty Board Tutorial RRT in ICU Yan Wing Wa Department of Intensive Care PYNEH 22 April 2008 1
Indications of RRT 2
Indications for acute dialysis JT Daugirdas, Handbook of Dialysis 3 rd Ed. • Impaired RFT (Creatinine Cl < 20 -25 ml/min/1. 73 m 2) – Symptoms of Uremia, e. g. GI upset, dec. consciousness, pericarditis or bleeding diathesis – Refractory or progressive fluid overload – Uncontrollable hyperkalemia – Severe metabolic acidosis • Steady worsening of renal function with – Urea > 25 -36 mmol/l or – Creatinine Cl < 15 -20 ml/min 3
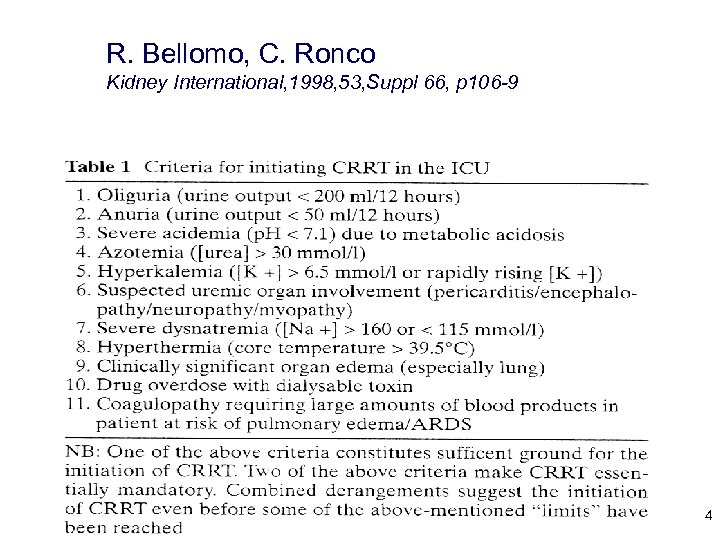
R. Bellomo, C. Ronco Kidney International, 1998, 53, Suppl 66, p 106 -9 4
Anticoagulation strategies 5
Extracorporeal circuit patency • Systemic anticoagulation • No anticoagulation • Regional anticoagulation 6
Systemic anticoagulation Oudemans-van. Straaten etal, Intensive Care Med 2006, 32, 188 -202 – Unfractionated Heparin (HIT 2. 6%) – LMWH (HIT 0. 2%) – Heparinoids – Danaparoid (cross react with HIT Abs in ~10%) – Factor Xa inhibitor – Fondaparinux – Direct thrombin inhibitor – r-Hirudin – Argatroban – Dermatan sulfate – Prostacyclin & prostaglandin E 1(hypotension) – Protease inhibitors – nafamostat mesilate (anaphylaxis, only a/v in Japan) 7
No anticoagulation • For patients in whom systemic anticoagulation is contraindicated • Frequent circuit clotting 8
Regional anticoagulation • Regional anticoagulation using UFH with protamine – UFH side effect (HIT) and Protamine side effects (platelet and inflammatory mediators activation, hypotension & pulmonary hypertension) 9
Regional citrate anticoagulation (RCA) Indicated in patients with bleeding risk • thrombocytopenia • coagulopathy • pericarditis • recent surgery with bleeding complications • recent surgery after which bleeding would be very dangerous – brain surgery – vascular or cardiac surgery – renal transplant 10
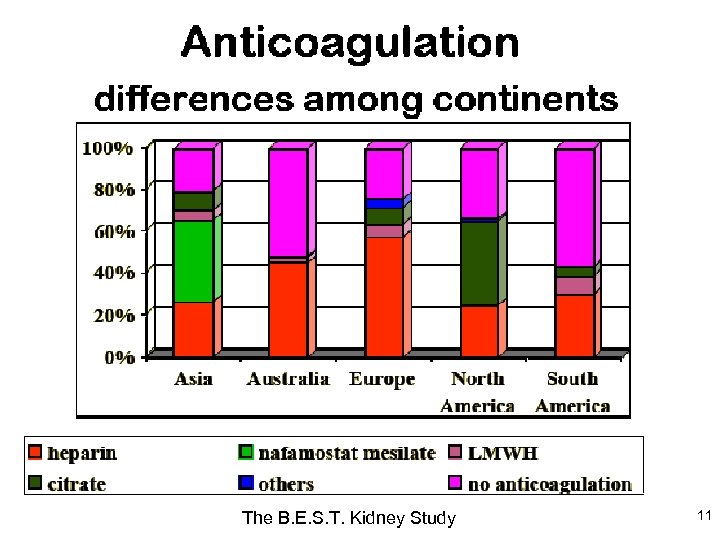
The B. E. S. T. Kidney Study 11
12
Citrate Metabolism • Half-life 5 mins • Metabolized by liver, kidney & muscle • 1 citrate molecule will form 3 HCO 3 molecules 13
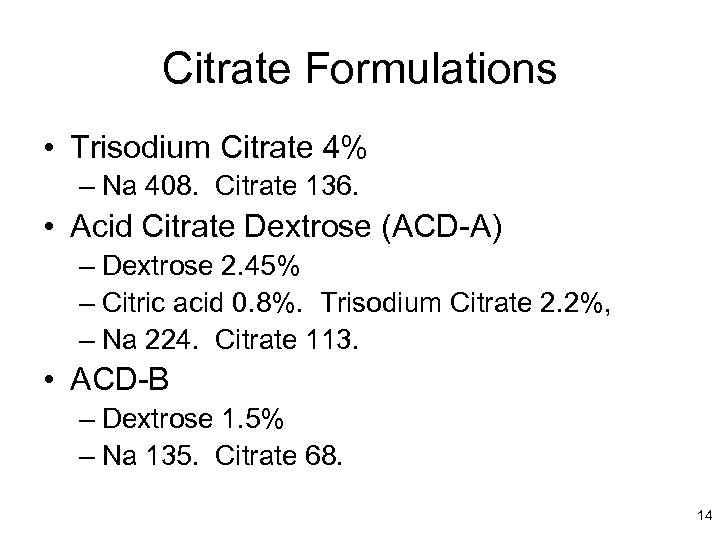
Citrate Formulations • Trisodium Citrate 4% – Na 408. Citrate 136. • Acid Citrate Dextrose (ACD-A) – Dextrose 2. 45% – Citric acid 0. 8%. Trisodium Citrate 2. 2%, – Na 224. Citrate 113. • ACD-B – Dextrose 1. 5% – Na 135. Citrate 68. 14
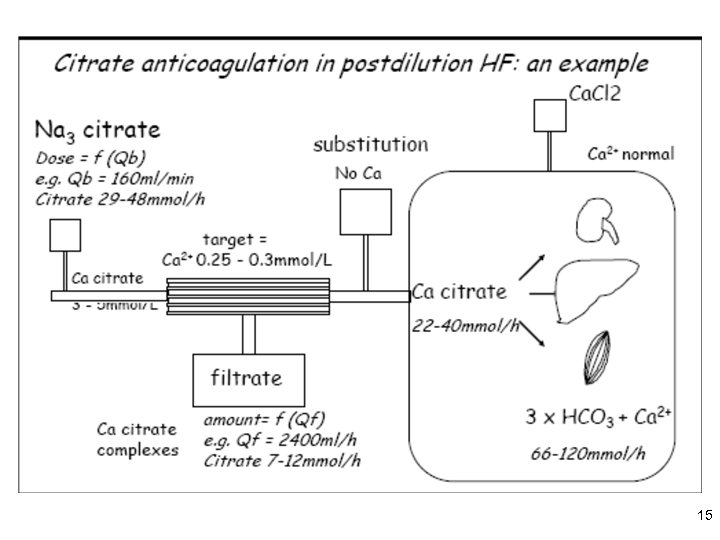
15
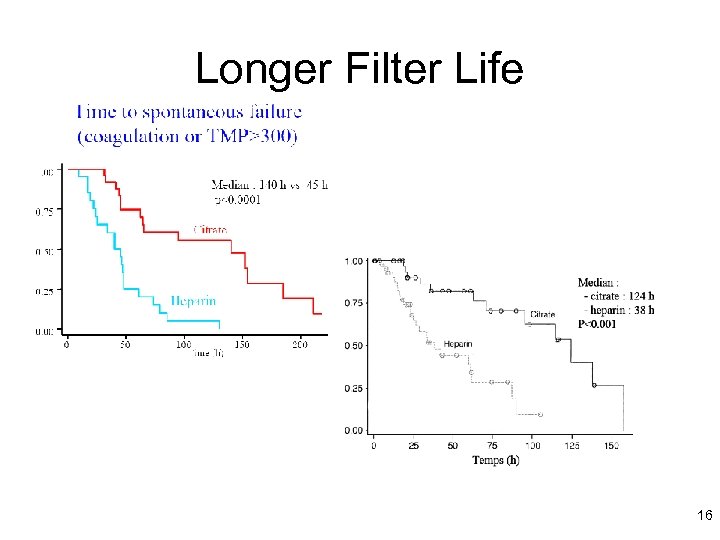
Longer Filter Life 16
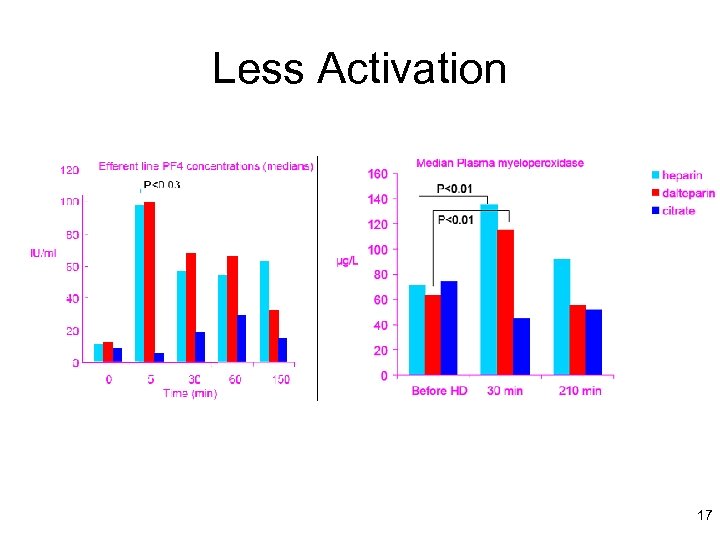
Less Activation 17
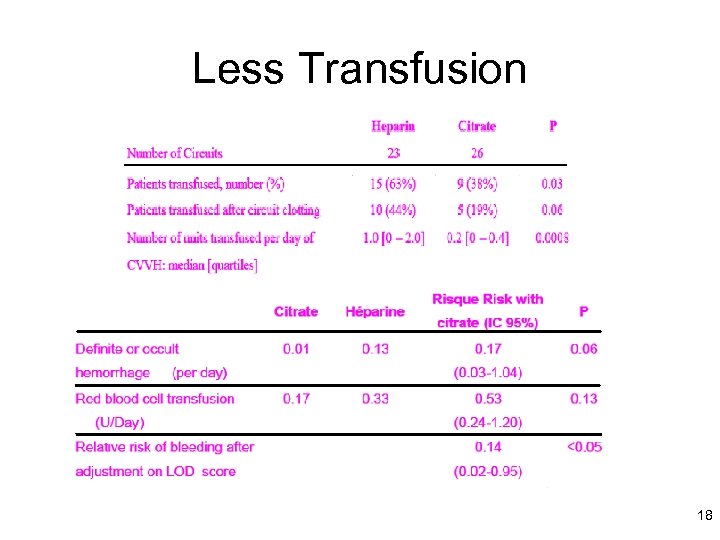
Less Transfusion 18
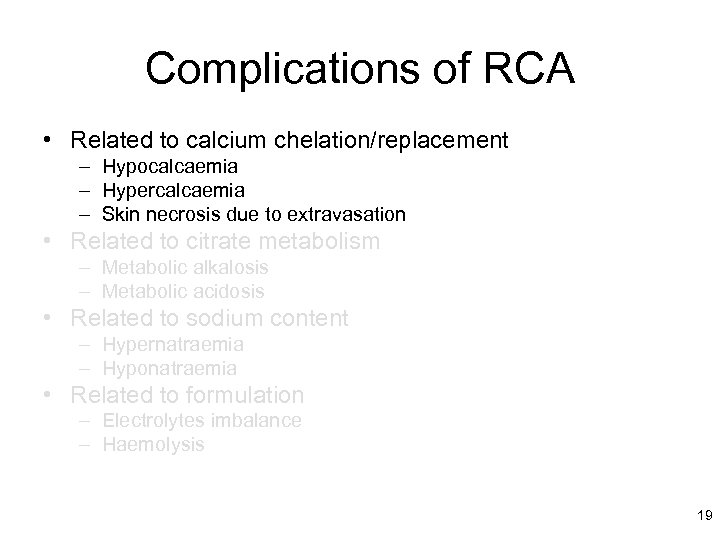
Complications of RCA • Related to calcium chelation/replacement – Hypocalcaemia – Hypercalcaemia – Skin necrosis due to extravasation • Related to citrate metabolism – Metabolic alkalosis – Metabolic acidosis • Related to sodium content – Hypernatraemia – Hyponatraemia • Related to formulation – Electrolytes imbalance – Haemolysis 19
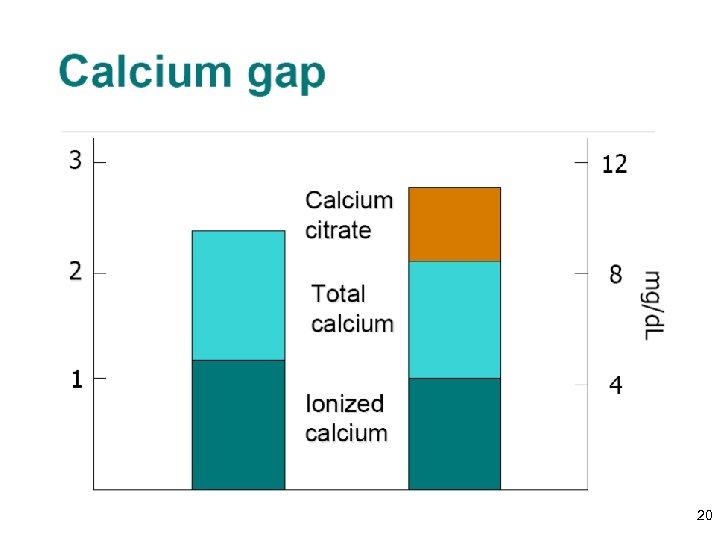
20
Complications of RCA • Related to calcium chelation/replacement – Hypocalcaemia – Hypercalcaemia – Skin necrosis due to extravasation • Related to citrate metabolism – Metabolic alkalosis – Metabolic acidosis • Related to sodium content – Hypernatraemia – Hyponatraemia • Related to formulation – Electrolytes imbalance – Haemolysis 21
Complications of RCA • Related to calcium chelation/replacement – Hypocalcaemia – Hypercalcaemia – Skin necrosis due to extravasation • Related to citrate metabolism – Metabolic alkalosis – Metabolic acidosis • Related to sodium content – Hypernatraemia – Hyponatraemia • Related to formulation – Electrolytes imbalance – Haemolysis 22
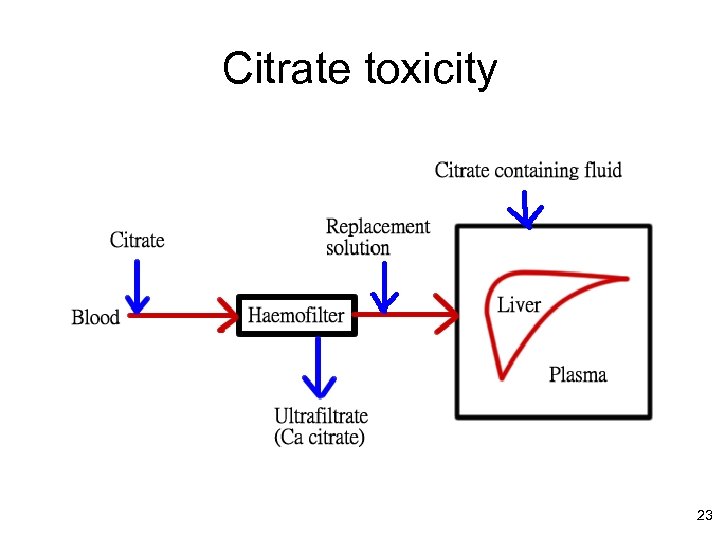
Citrate toxicity 23
Dose of RRT 24
Q. How should one prescribe and dose acute RRT to optimize patient outcomes? 25
Pesacreta et al. • 27 academic centres involved with the Acute Renal Failure Trial Network (ATN) study • Cross sectional survey of acute RRT prescribing practices circa 2003 -2004 • Do practitioners dose acute RRT? Pesacreta etal, J Am Soc Nephrol, Vol 15, pp 350 A, 2004 26
Pesacreta et al. i. HD • 31% of respondents targeted URR ≥ 0. 65 • 7% of respondents targeted Kt/V≥ 1. 2 • 56% of respondents did not target any specific i. HD dose • Fewer than one-quarter of respondents routinely assess delivered i. HD dose Pesacreta etal, J Am Soc Nephrol, Vol 15, pp 350 A, 2004 27
Pesacreta et al. CRRT • 14% of respondents dosed CRRT indexed to weight (more than three-quarters of these respondents prescribed an effluent rate of ≥ 35 m. L/kg/hour) • 66% of remaining respondents prescribed fixed effluent rates of ≤ 2 L/hour • Remainder did not target any specific dose Pesacreta etal, J Am Soc Nephrol, Vol 15, pp 350 A, 2004 28
Overview • Revisiting of dose and outcomes • Patient and treatment related factors affecting dose prescription and delivery • Therapy-specific dose-outcome data • Approach to prescription and quantification of acute RRT dose 29
Overview • Revisiting of dose and outcomes • Patient and treatment related factors affecting dose prescription and delivery • Therapy-specific dose-outcome data • Approach to prescription and quantification of acute RRT dose 30
“Patient are dying with renal failure, rather than of renal failure in the ICU” (AKI an indicator of disease) 31
“Patient are dying of renal failure, rather than with renal failure in the ICU” (AKI a mediator of disease) 32
AKI and Mortality Risk • AKI in critically ill patients still associated with a disappointingly high mortality risk • “Corrected” mortality is that attributable to AKI rather than the underlying illness (Kennedy, 1973) – “Corrected” mortality minimal for low illness severity, ~50% at the severe end – Main contributors to “corrected” mortality are haemorrhage, non-resolving shock and infection Uchino et al, JAMA, Vol 294, pp 813 -818, 2005 Kennedy et al, QJM, Vol 42, pp 73 -86, 1973 Liano et al, Vol 63, S 16 -S 24, 1998 33
34
Metnitz et al. • Prospective, observational, cohort study • Is there as independent association between AKI and patient mortality risk? • 30 medical, surgical, and mixed ICUs in • Austria using a national ICU registry • 17, 126 consecutive patients • 01. 03. 98 to 28. 02. 00 35
Metnitz et al. • Usual predictors of mortality e. g. age, illness severity, septic or cardiogenic shock, etc • Case-control analysis to examine independent association between AKI (defined as requiring RRT) and mortality risk • Exposure group (AKI) versus matched control group by age, SAPS II, and ICU 36
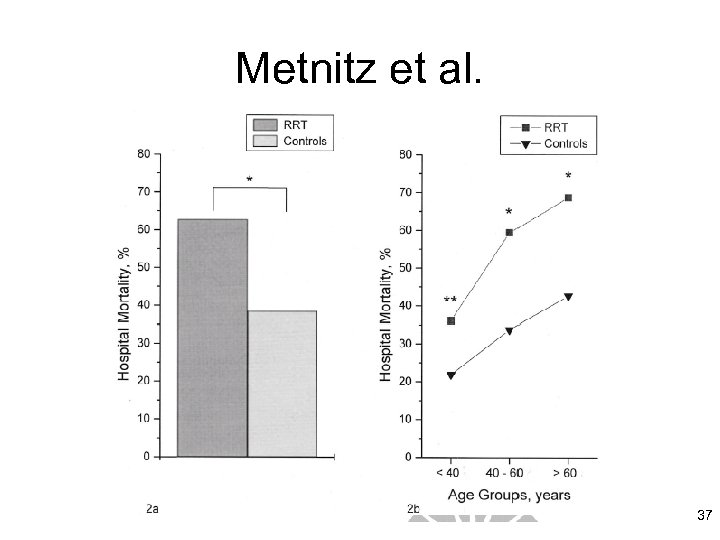
Metnitz et al. 37
How should one prescribe and dose acute RRT to optimize patient outcomes? Individually, according to the requirements of the patient 38
Overview • Revisiting of dose and outcomes • Patient and treatment related factors affecting dose prescription and delivery • Therapy-specific dose-outcome data • Approach to prescription and quantification of acute RRT dose 39
Expressions of Acute RRT Dose • Studies using urea kinetic methods to quantify dose have successfully related dose to outcomes in i. HD • Studies using effluent (filtration) rate to quantify dose have successfully related dose to outcomes in CRRT 40
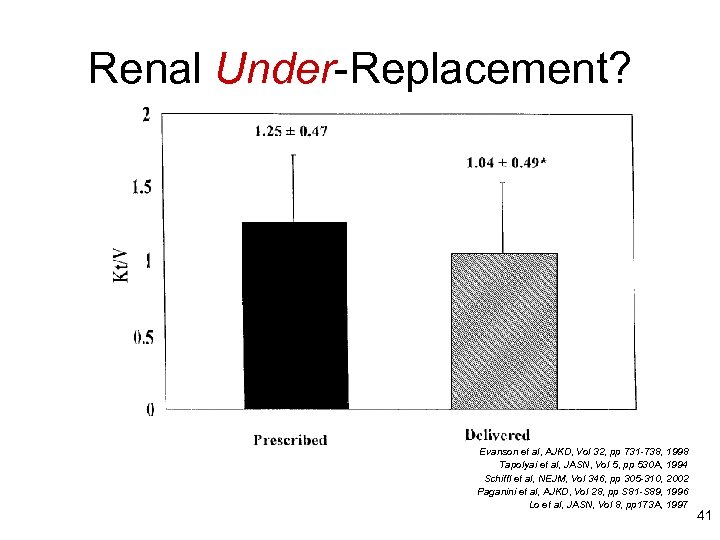
Renal Under-Replacement? Evanson et al, AJKD, Vol 32, pp 731 -738, 1998 Tapolyai et al, JASN, Vol 5, pp 530 A, 1994 Schiffl et al, NEJM, Vol 346, pp 305 -310, 2002 Paganini et al, AJKD, Vol 28, pp S 81 -S 89, 1996 Lo et al, JASN, Vol 8, pp 173 A, 1997 41
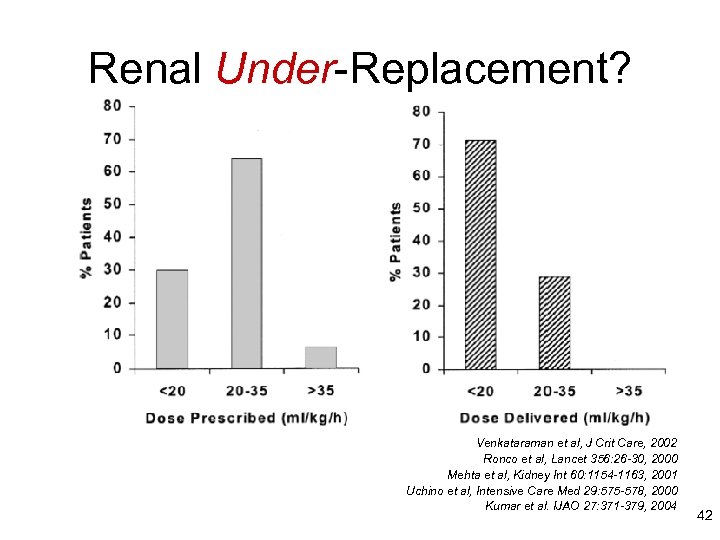
Renal Under-Replacement? Venkataraman et al, J Crit Care, 2002 Ronco et al, Lancet 356: 26 -30, 2000 Mehta et al, Kidney Int 60: 1154 -1163, 2001 Uchino et al, Intensive Care Med 29: 575 -578, 2000 Kumar et al. IJAO 27: 371 -379, 2004 42
43

44
45
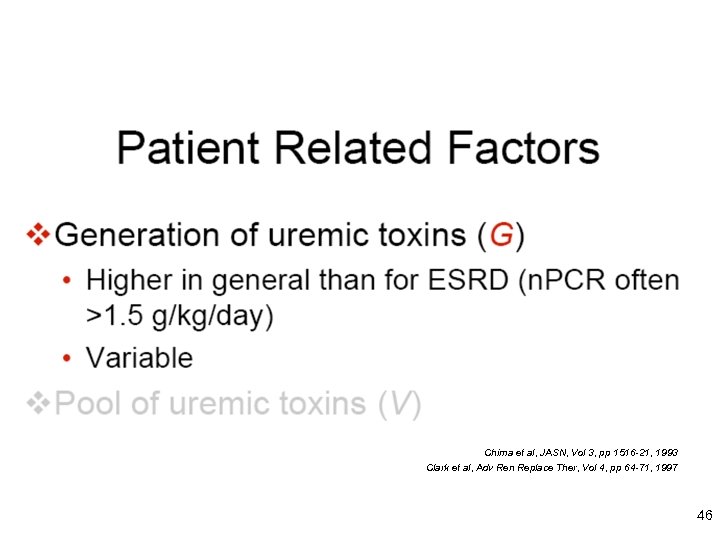
Chima et al, JASN, Vol 3, pp 1516 -21, 1993 Clark et al, Adv Ren Replace Ther, Vol 4, pp 64 -71, 1997 46
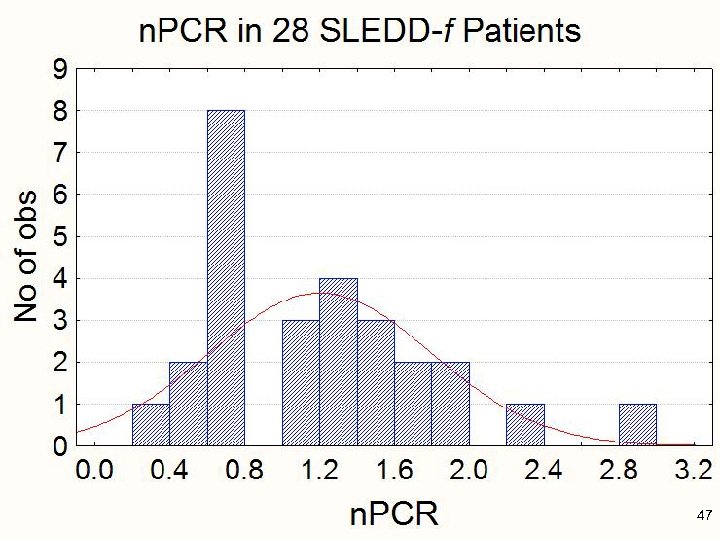
47
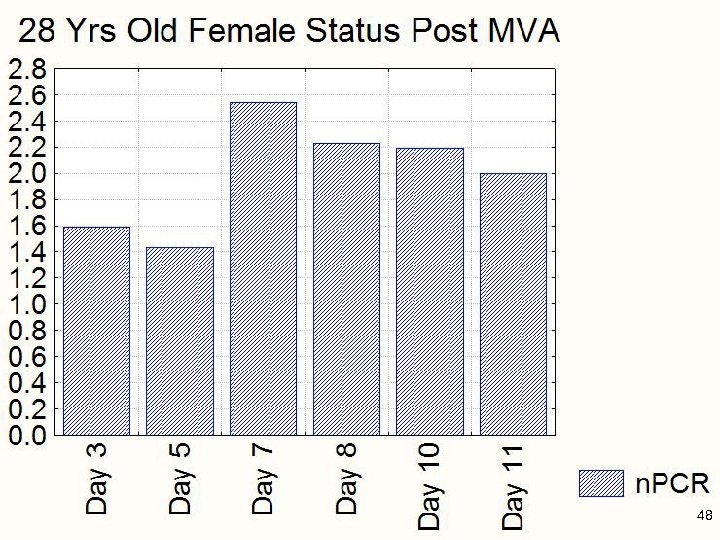
48
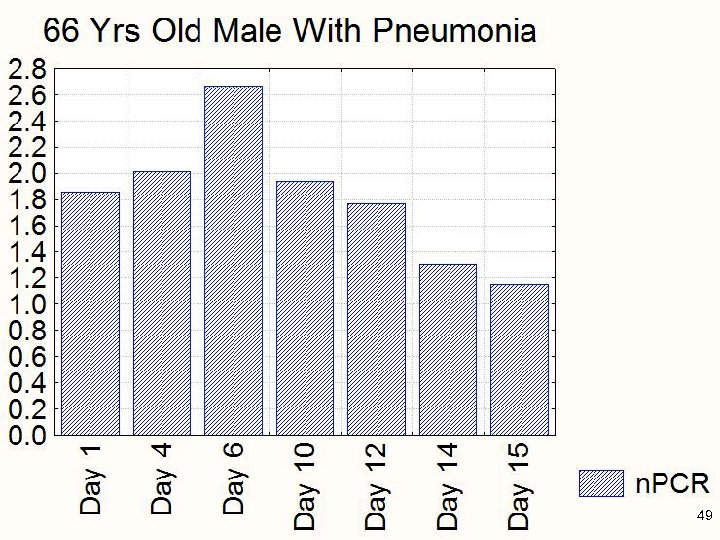
49
50
51
52
53
54
55
56
57
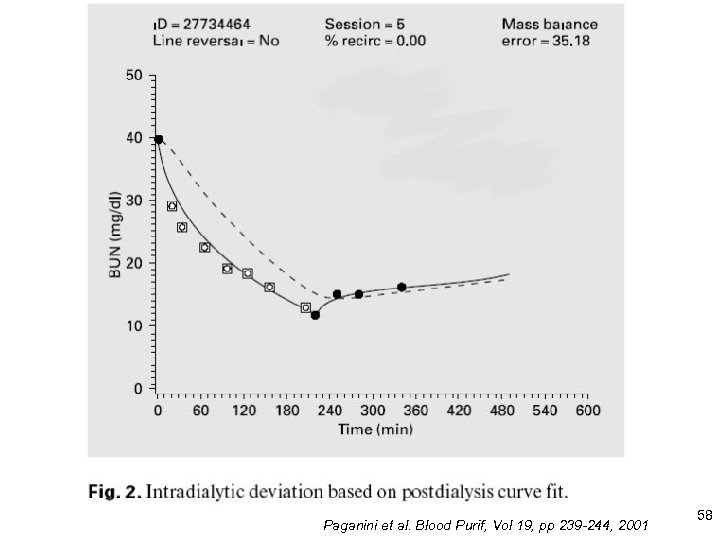
Paganini et al. Blood Purif, Vol 19, pp 239 -244, 2001 58
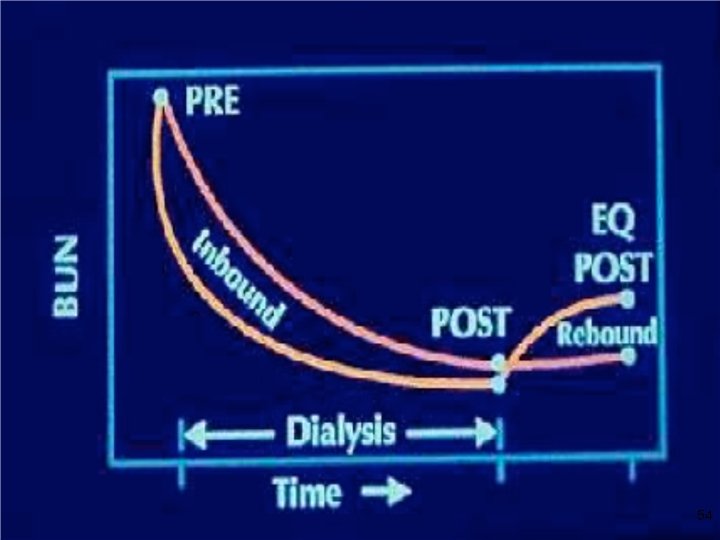
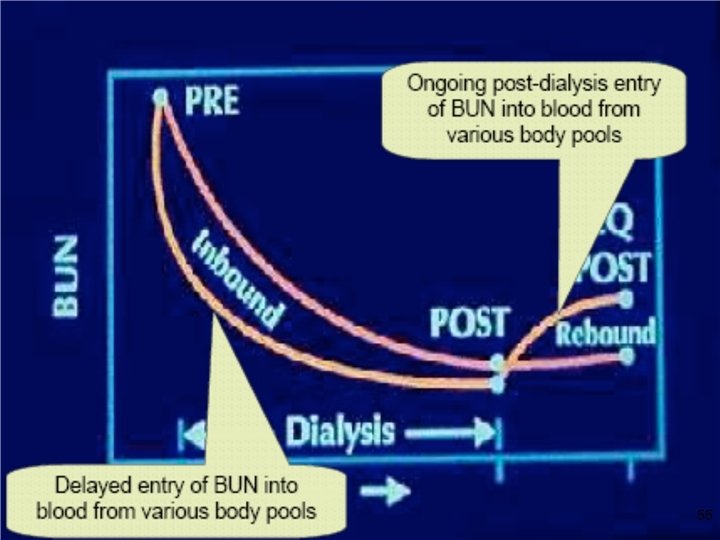
Patient Related Factors • A smaller acute RRT dose than desired is both prescribed and delivered to AKI patients • AKI patients are not in steady state 59
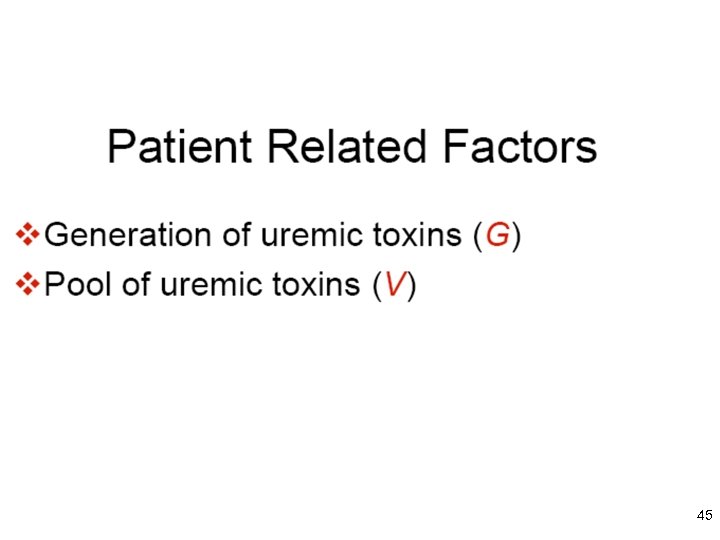
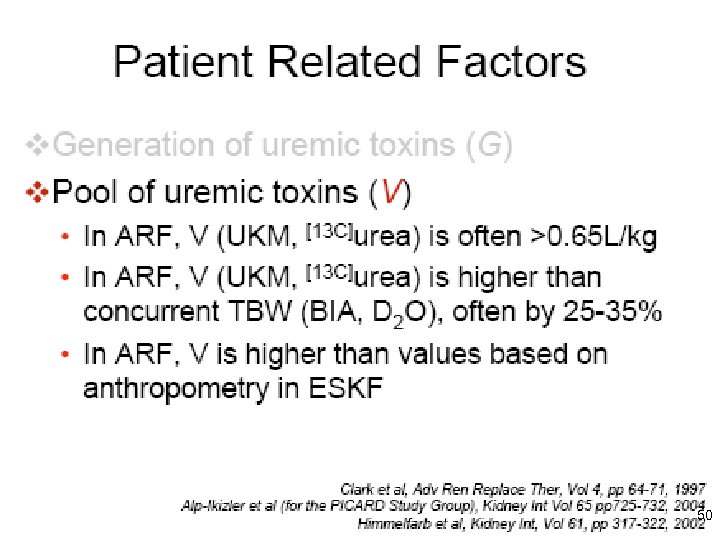
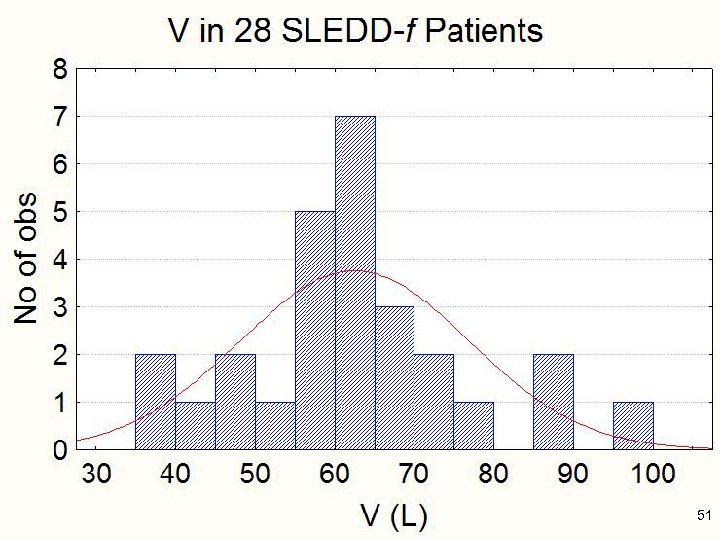
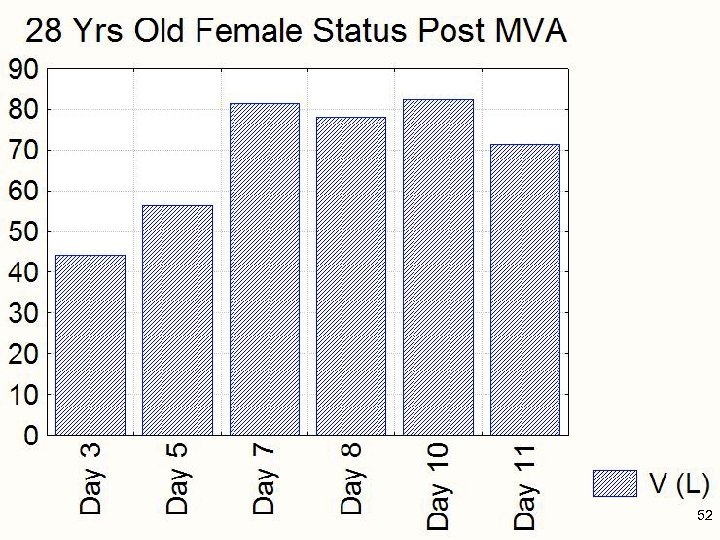
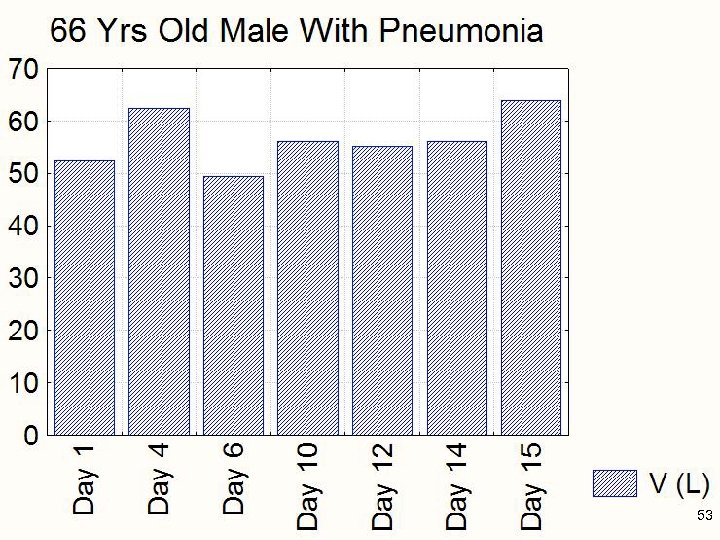
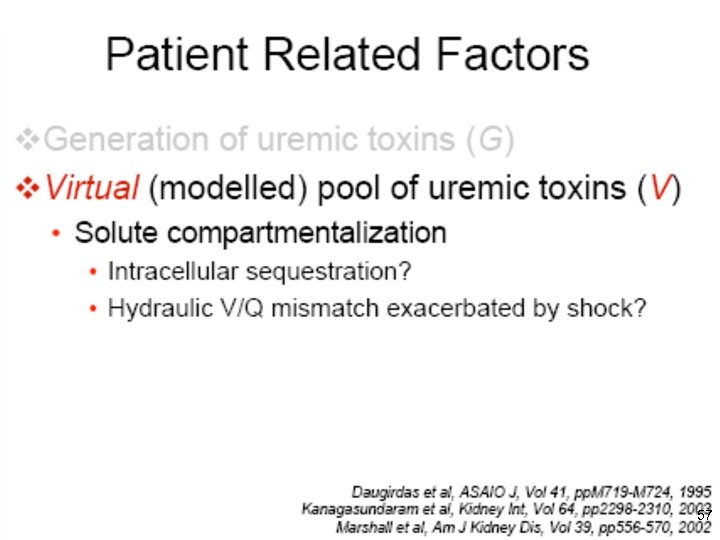
Patient Related Factors • AKI patients generate more uremic toxins than expected (higher G) • AKI patients have a greater pool (higher V) of uremic toxins than expected for unknown reasons, and one should account for this pool by formal UKM rather than anthropometry 60
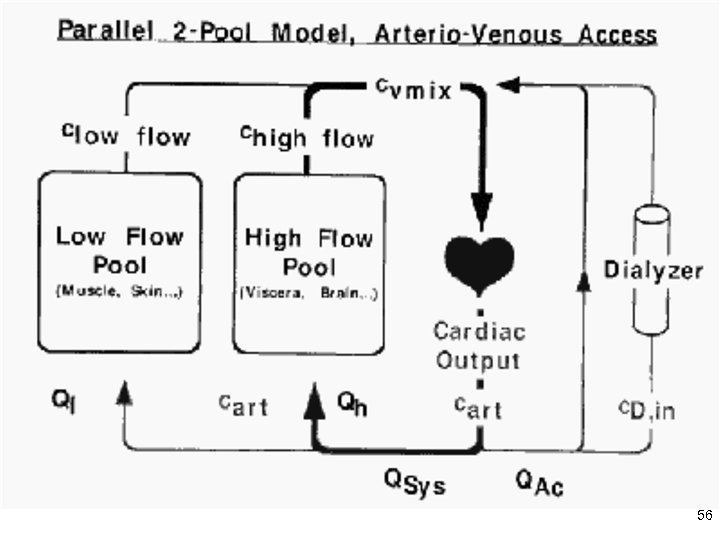
Patient Related Factors Solute compartmentalization may be a little (but not a lot) greater in AKI than ESKF • Solute compartmentalization increases with efficiency of solute removal (i. e. important for i. HD, not for hybrid or CRRT) • Estimation of e. Kt/V or dp. Kt/V for i. HD is necessary, utilizing using the Daugirdas, Garred, or Tattersall rate equations • Leblanc et al. Adv Ren Replace Ther, Vol 2, pp 255 -264, 1995 Paganini et al. Blood Purif, Vol 19, pp 239 -244, 2001 Marshall et al, Am J Kidney Dis, Vol 35, pp. A 19, 2000. 61
Treatment Related Factors • Catheter performance • Dialyzer/filter performance 62
7ead267cd0fc665efa3113ade18baca7.ppt