МИ от Шишова (англ. +русск.).pptx
- Количество слайдов: 48
Causes of childhood acute bacterial meningitis. • In children aged > 1 month two pathogens predominate in unvaccinated populations usually accounting for >80% of cases outside the meningitis belt: – Strep. Pneumoniae – H. influenzae • In children < 1 month the range of pathogens is wider with common ones being: – Group B Streptococcus – E. coli – Klebsiella spp.
Neisseria meningitidis • Severe acute bacterial infection • Cause of meningitis, sepsis, and focal infections • Epidemic disease in sub-Saharan Africa • Current polysaccharide vaccine licensed in 1978 • Conjugate vaccine licensed in 2005
Neisseria meningitidis • Aerobic gram-negative bacteria • At least 13 serogroups based on characteristics of the polysaccharide capsule • Most invasive disease caused by serogroups A, B, C, Y, and W-135 • Relative importance of serogroups depends on geographic location and other factors (e. g. age)
Meningococcal Disease Clinical Features • Incubation period 3 -4 days (range 2 -10 days) • Abrupt onset of fever, meningeal symptoms, hypotension, and rash • Fatality rate 9%-12%; up to 40% in meningococcemia
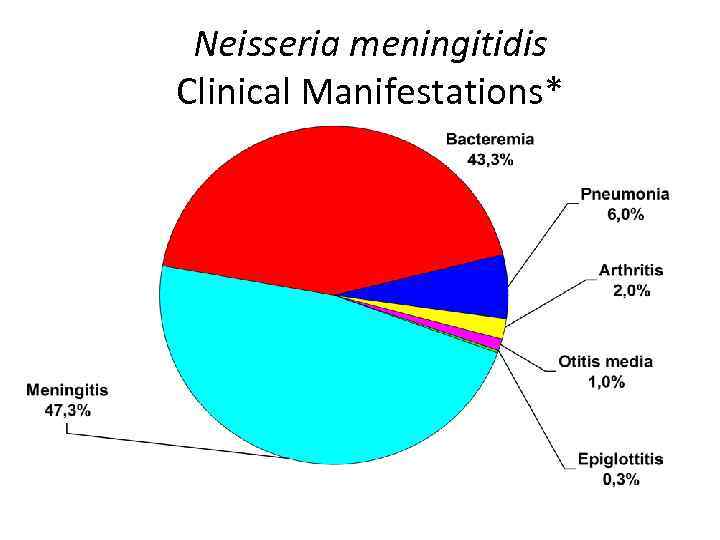
Neisseria meningitidis Clinical Manifestations* *1992 -1996 data
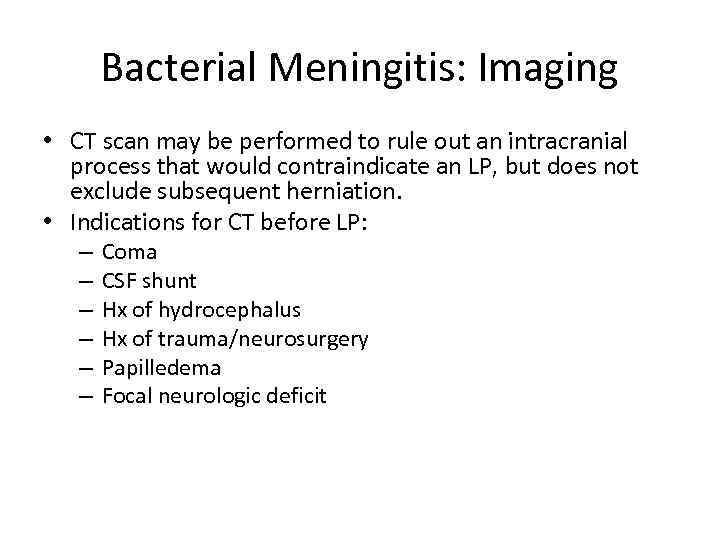
Bacterial Meningitis: Imaging • CT scan may be performed to rule out an intracranial process that would contraindicate an LP, but does not exclude subsequent herniation. • Indications for CT before LP: – – – Coma CSF shunt Hx of hydrocephalus Hx of trauma/neurosurgery Papilledema Focal neurologic deficit
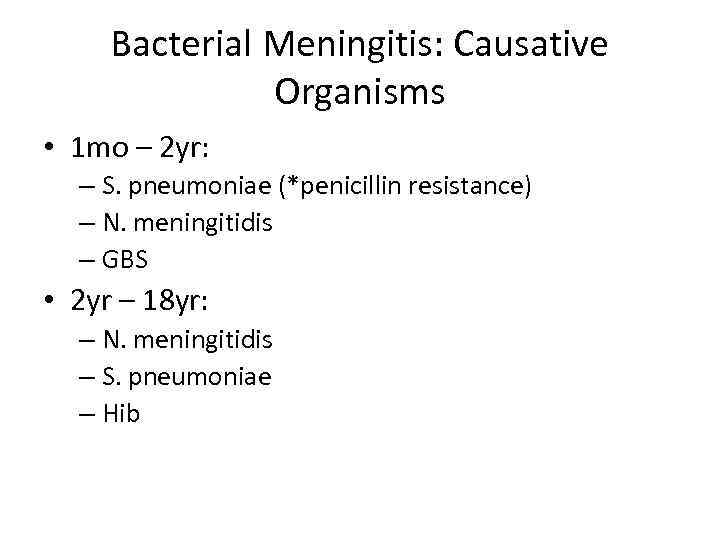
Bacterial Meningitis: Causative Organisms • 1 mo – 2 yr: – S. pneumoniae (*penicillin resistance) – N. meningitidis – GBS • 2 yr – 18 yr: – N. meningitidis – S. pneumoniae – Hib
Viral Meningitis: Causative Organisms • • Enteroviruses Herpesviruses Arboviruses Influenza
Viral Meningitis: Treatment • Herpes meningitis in children is treated with Acyclovir 30 mg/kg/day, or 10 mg/kg/dose IV Q 8 hrs, for a minimum of 14 -21 days – Neonatal dosing is 60 mg/kg/day, or 20 mg/kg/dose IV Q 8 hrs for 21 days. • EV infections are treated symptomatically and rarely require hospitalization beyond the neonatal period. • Treatment for EBV, Arbovirus, and Influenza meningitis is mainly supportive.
Lumbar Puncture: Contraindications • Absolute: – Increased ICP • Relative: – Cardiopulmonary instability – Soft tissue infection at puncture site – Bleeding diathesis: • Active bleeding • Platelet count <50, 000 • INR > 1. 4
Lumbar Puncture: Patient Counseling • Your job is to provide a clear explanation of the urgent indications of the procedure, as well as the details of the procedure itself. • In order to obtain informed consent, you must list both risks and benefits.
Lumbar Puncture: Patient Counseling cont. • Risks: – – – Postspinal headache Epidermoid tumor Infection Cerebral herniation Spinal hematoma • Benefits: – The benefit of early diagnosis far outweighs the risk of the procedure if there are no contraindications.
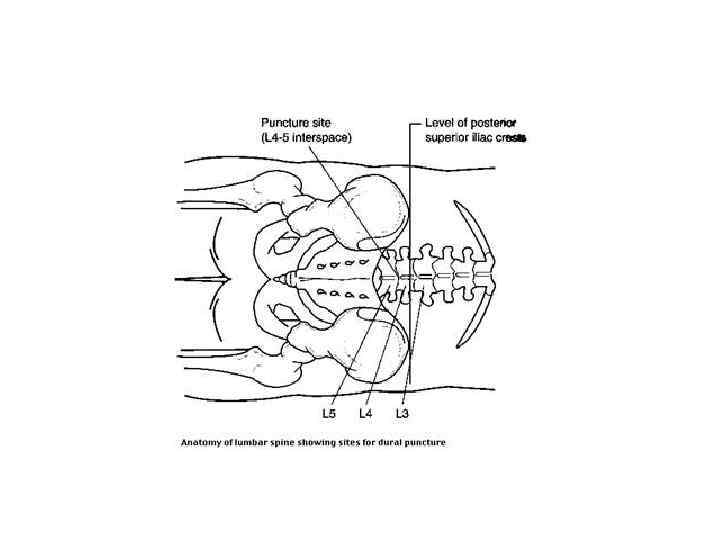
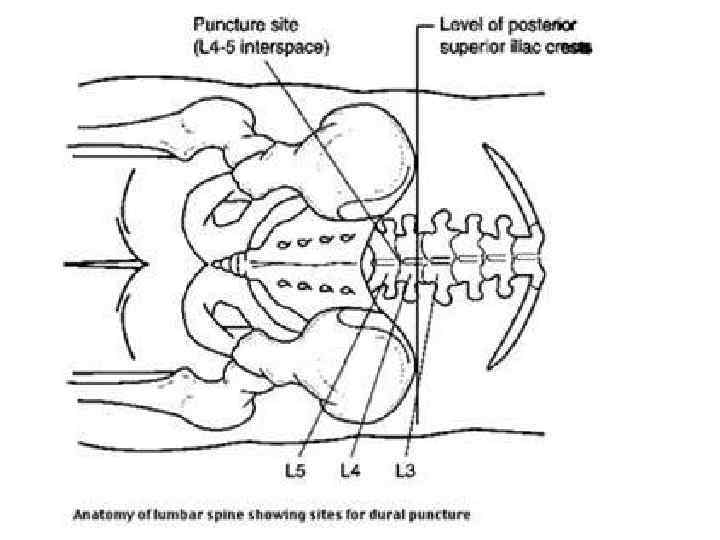
Lumbar Puncture: Anatomy • In older children, LP can be performed from the L 2 -L 3 interspace to the L 5 -S 1 interspace. In children younger than 12 mo, LP must be performed below the L 2 -L 3 interspace. • An imaginary line that connects the 2 PSIC intersects the spine at approximately L 4.

Lumbar Puncture: Misc. • Please be courteous and clean up your own mess. Dispose of all unused sharps before throwing away the kit.
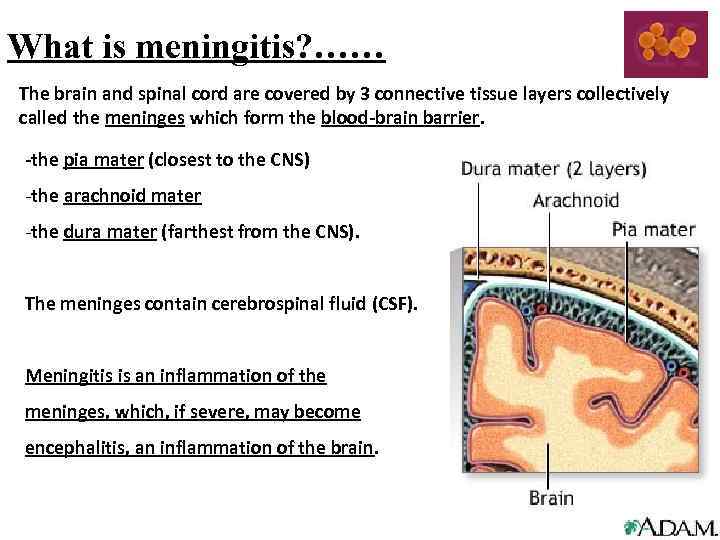
What is meningitis? …… The brain and spinal cord are covered by 3 connective tissue layers collectively called the meninges which form the blood-brain barrier. -the pia mater (closest to the CNS) -the arachnoid mater -the dura mater (farthest from the CNS). The meninges contain cerebrospinal fluid (CSF). Meningitis is an inflammation of the meninges, which, if severe, may become encephalitis, an inflammation of the brain.
Meningitis…… Definition Meningitis is an infection which causes inflammation of the membranes covering the brain and spinal cord. Non-bacterial meningitis is often referred to as ‘aseptic meningitis’ – eg. viral meningitis Bacterial meningitis may be referred to as ‘purulent meningitis’. Causes and risks The most common causes of meningitis are viral infections that usually resolve without treatment. Bacterial infections of the meninges are extremely serious illnesses, and may result in death or brain damage even if treated.
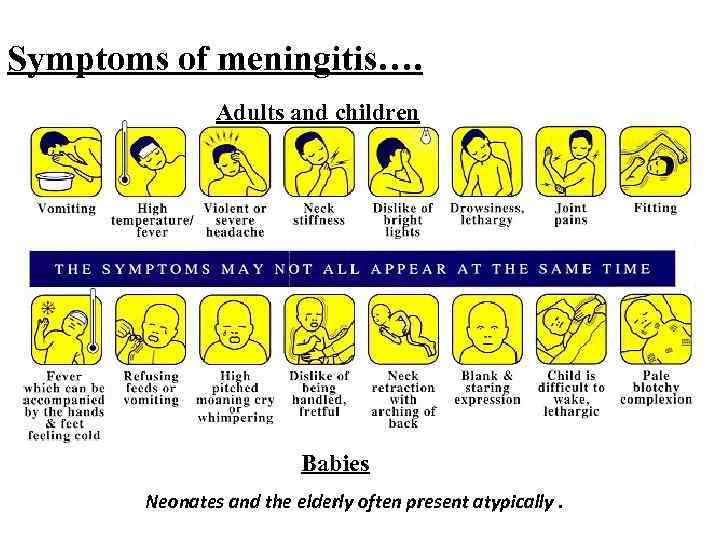
Symptoms of meningitis…. Adults and children Babies Neonates and the elderly often present atypically.
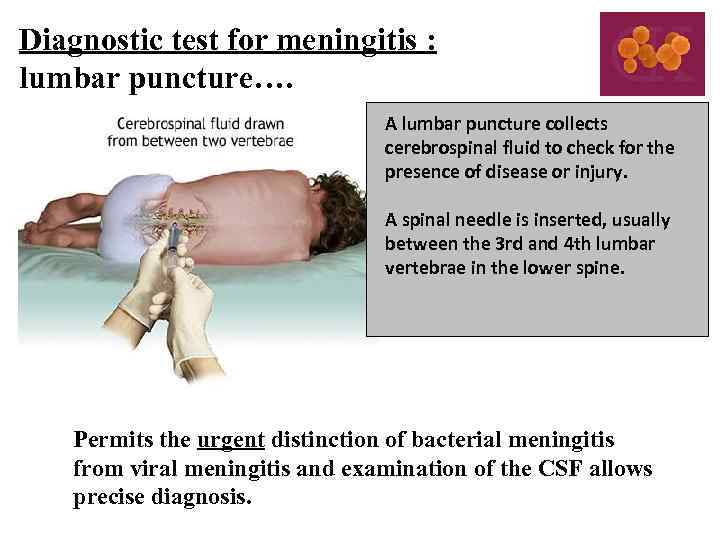
Diagnostic test for meningitis : lumbar puncture…. A lumbar puncture collects cerebrospinal fluid to check for the presence of disease or injury. A spinal needle is inserted, usually between the 3 rd and 4 th lumbar vertebrae in the lower spine. Permits the urgent distinction of bacterial meningitis from viral meningitis and examination of the CSF allows precise diagnosis.
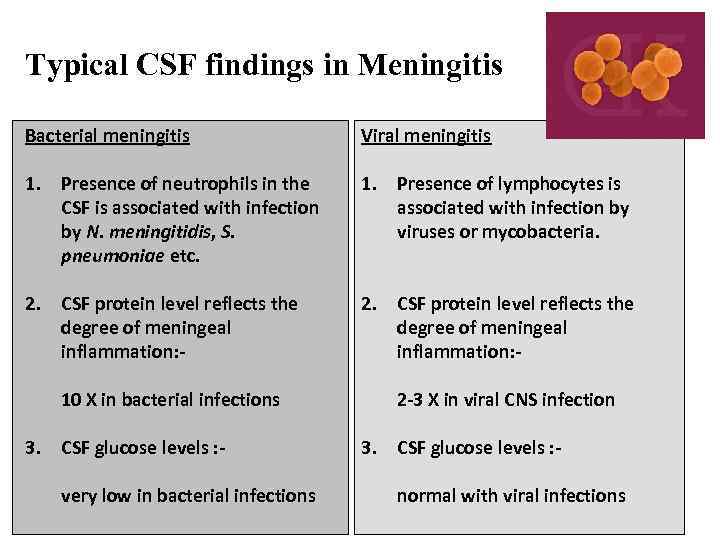
Typical CSF findings in Meningitis Bacterial meningitis Viral meningitis 1. Presence of neutrophils in the CSF is associated with infection by N. meningitidis, S. pneumoniae etc. 1. Presence of lymphocytes is associated with infection by viruses or mycobacteria. 2. CSF protein level reflects the degree of meningeal inflammation: 10 X in bacterial infections 2. CSF protein level reflects the degree of meningeal inflammation: 2 -3 X in viral CNS infection 3. CSF glucose levels : very low in bacterial infections 3. CSF glucose levels : normal with viral infections
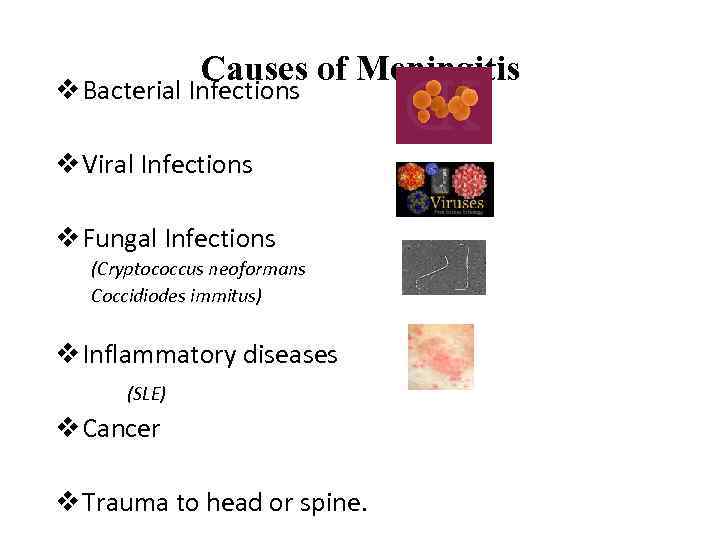
Causes of Meningitis v Bacterial Infections v Viral Infections v Fungal Infections (Cryptococcus neoformans Coccidiodes immitus) v Inflammatory diseases (SLE) v Cancer v Trauma to head or spine.
Bacterial meningitis…. . Etiological Agents: -Pneumococcal, Streptococcus pneumoniae (38%) -Meningococcal, Neisseria meningitidis (14%) -Haemophilus influenzae (4%) -Staphylococcal, Staphylococcus aureus (5%) -Tuberculous, Mycobacterium tuberculosis
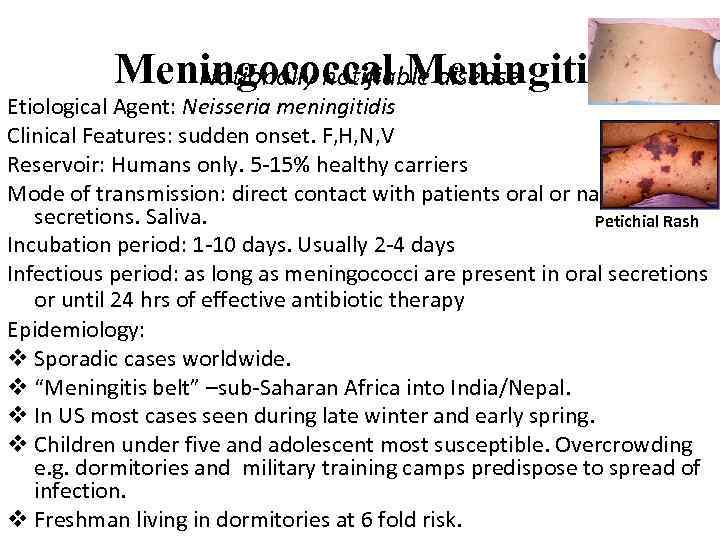
Meningococcal Meningitis Nationally notifiable disease Etiological Agent: Neisseria meningitidis Clinical Features: sudden onset. F, H, N, V Reservoir: Humans only. 5 -15% healthy carriers Mode of transmission: direct contact with patients oral or nasal secretions. Saliva. Petichial Rash Incubation period: 1 -10 days. Usually 2 -4 days Infectious period: as long as meningococci are present in oral secretions or until 24 hrs of effective antibiotic therapy Epidemiology: v Sporadic cases worldwide. v “Meningitis belt” –sub-Saharan Africa into India/Nepal. v In US most cases seen during late winter and early spring. v Children under five and adolescent most susceptible. Overcrowding e. g. dormitories and military training camps predispose to spread of infection. v Freshman living in dormitories at 6 fold risk.
Aseptic Meningitis Definition: A syndrome characterized by acute onset of meningeal symptoms, fever, and cerebrospinal fluid pleocytosis, with bacteriologically sterile cultures. Laboratory criteria for diagnosis: No evidence of bacterial or fungal meningitis Case classification Confirmed: a clinically compatible illness diagnosed by a physician as aseptic meningitis, with no laboratory evidence of bacterial or fungal meningitis Comment Aseptic meningitis is a syndrome of multiple etiologies, but most cases are caused by a viral agent.
MPSV Recommendations • Approved for persons 2 years of age and older • Not recommended for routine vaccination of civilians • Should be used only for persons at increased risk of N. meningiditis infection who are 56 years of age or older, or if MCV is not available
MCV Recommendations • Routinely recommended for: – All children at 11 -18 years of age – All college freshmen living in a dormitory – Other persons 2 through 55 years of age at increased risk of invasive meningococcal disease MMWR 2005; 54(RR-7); 1 -21
Meningococcal Vaccine Recommendations • Use of MCV is preferred for persons 2 through 55 years of age for whom meningococcal vaccine is recommended • MPSV should be used for persons 56 years and older MMWR 2005; 54(RR-7); 1 -21
Meningococcal Vaccine Recommendations • Recommended for persons at increased risk of meningococcal disease: – Microbiologists who are routinely exposed to isolates of N. meningitidis – Military recruits – Persons who travel to and U. S. citizens who reside in countries in which N. meningitidis is hyperendemic or epidemic – terminal complement component deficiency – functional or anatomic asplenia MMWR 2005; 54(RR-7); 1 -21
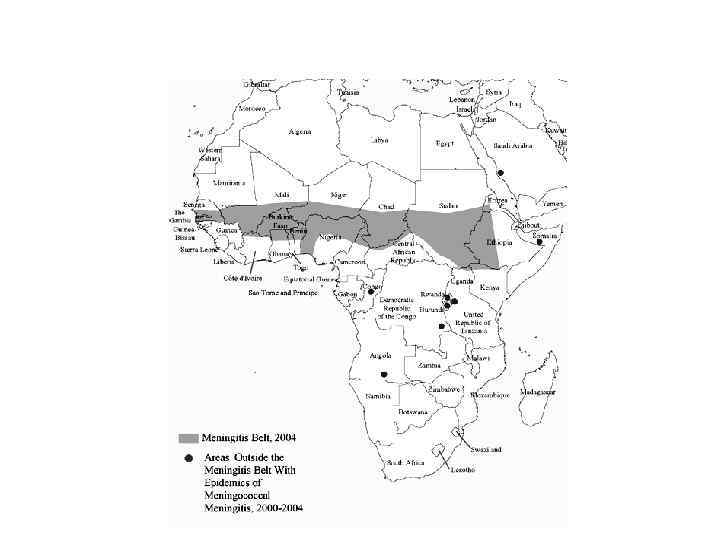
Meningococcal Endemic Areas 2004
Meningococcal Vaccine Recommendations • Both MCV and MPSV recommended for control of outbreaks caused by vaccine-preventable serogroups • Outbreak definition: – 3 or more confirmed or probable primary cases – Period <3 months – Primary attack rate >10 cases per 100, 000 population* *Population-based rates should be used rather than age-specific attack rates
Meningococcal Vaccine Revaccination • Revaccination may be indicated for persons at increased risk for infection* • Revaccination may be considered 5 years after receipt of the MPSV • MCV is recommended for revaccination of persons 2 through 55 years of age although use of MPSV is acceptable • Revaccination after receipt of MCV is not recommended at this time *e. g. , asplenic persons and those who reside in areas in which disease is endemic (does not include college settings)
Meningococcal Vaccines Adverse Reactions MPSV • Local reactions 4%-48% 11%-59% for 1 -2 days • Fever >100 o. F 3% 5% • Systemic reactions 3%-60% 4%-62% (headache, malaise fatigue) MCV
Meningococcal Vaccines Contraindications and Precautions • Severe allergic reaction to vaccine component or following prior dose of vaccine • Moderate or severe acute illness
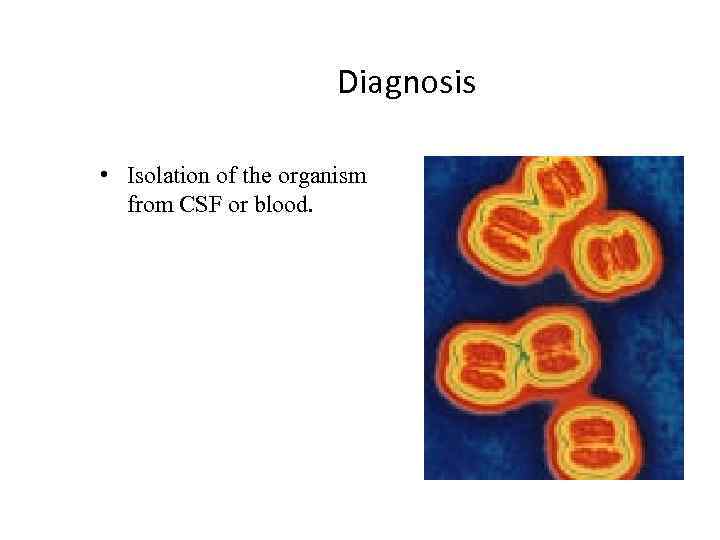
Diagnosis • Isolation of the organism from CSF or blood.
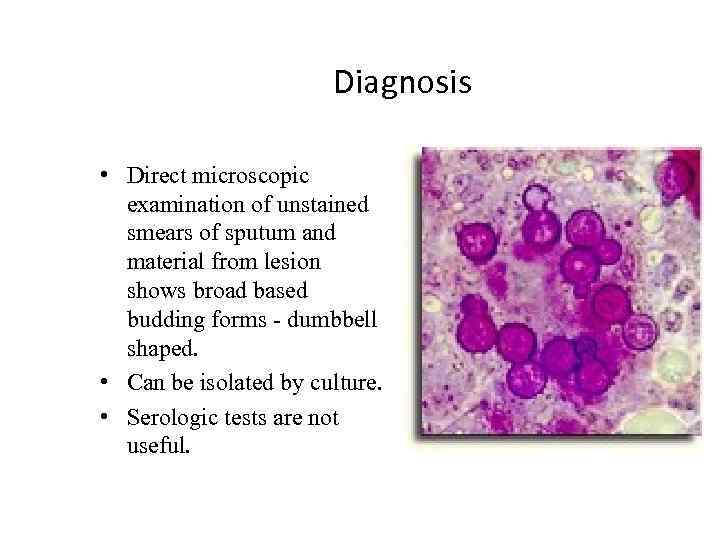
Diagnosis • Direct microscopic examination of unstained smears of sputum and material from lesion shows broad based budding forms - dumbbell shaped. • Can be isolated by culture. • Serologic tests are not useful.
Diagnosis • Increase in specific serum antibodies. • Fluorescent Antibody test on ulcer exudate, lymph node aspirate, etc. , yields rapid results. • Culture.
Менингит, люмбальная пункция
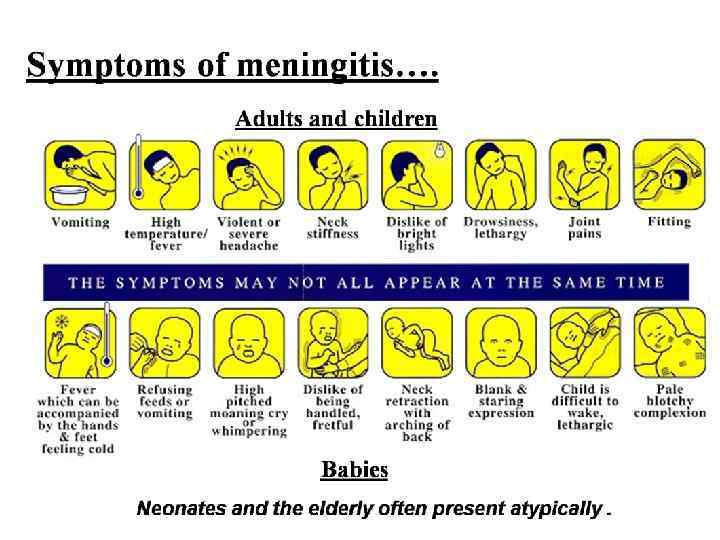

Симптомы менингита Взрослые и дети старшего возраста Дети младшего возраста У новорожденных и детей 1 -го года жизни часто протекает атипично

Симптомы менингита Взрослые и дети старшего возраста Дети младшего возраста У новорожденных и детей 1 -го года жизни часто протекает атипично
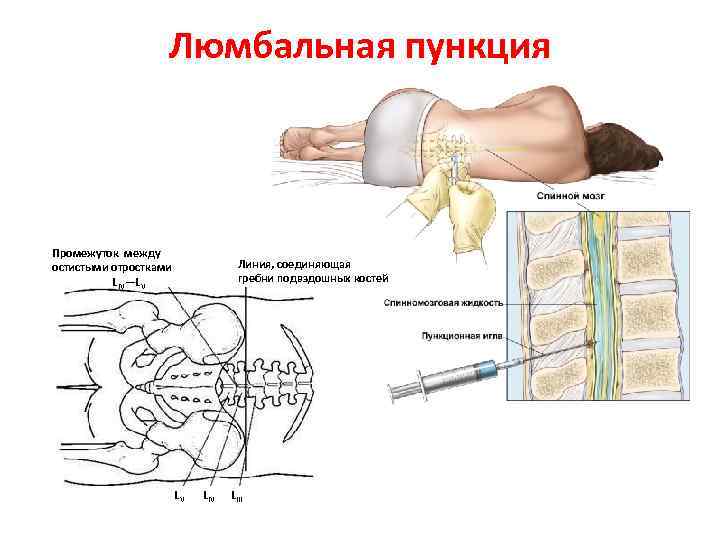
Люмбальная пункция Промежуток между остистыми отростками L IV—LV Линия, соединяющая гребни подвздошных костей LV LIII

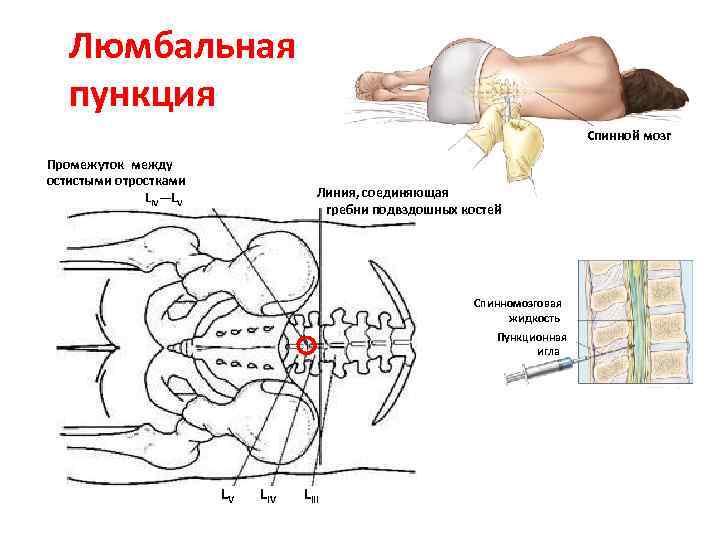
Люмбальная пункция Спинной мозг Промежуток между остистыми отростками LIV—LV Линия, соединяющая гребни подвздошных костей Спинномозговая жидкость Пункционная игла LV LIV LIII

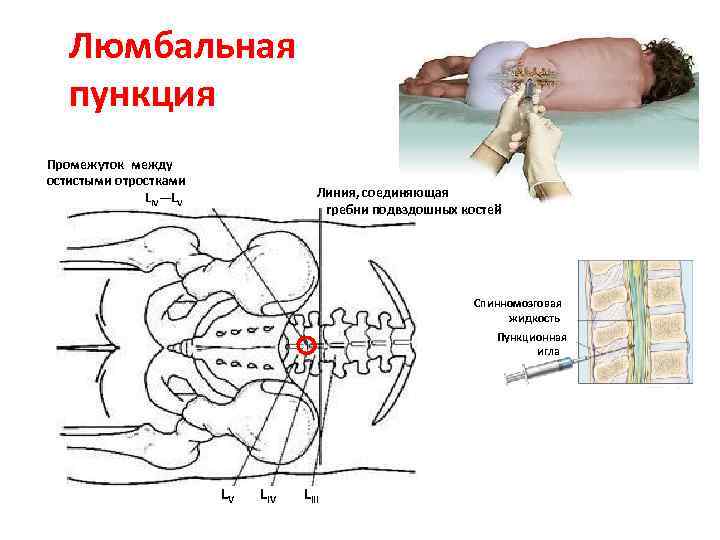
Люмбальная пункция Промежуток между остистыми отростками LIV—LV Линия, соединяющая гребни подвздошных костей Спинномозговая жидкость Пункционная игла LV LIV LIII
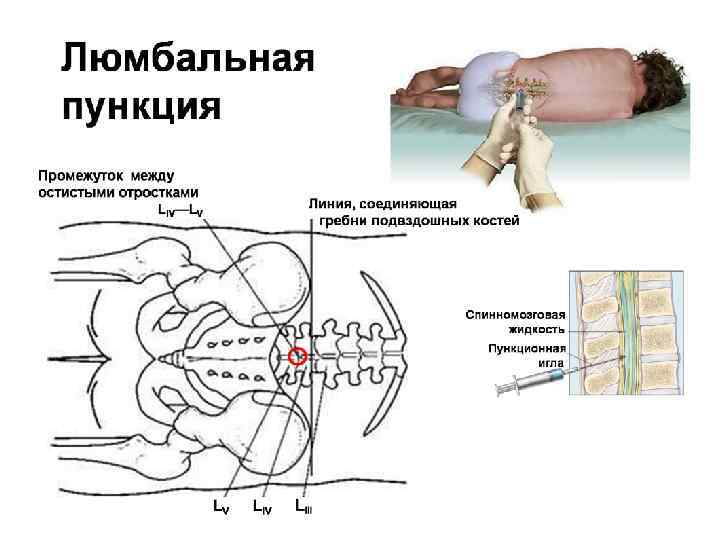

Люмбальная пункция
МИ от Шишова (англ. +русск.).pptx