StaphStrPseu.ppt
- Количество слайдов: 50
 Causative agents of inflammatory, suppurative and septical infections DEPARTMENT OF MICROBIOLOGY AND VIROLOGY PIROGOV’S RSMU
Causative agents of inflammatory, suppurative and septical infections DEPARTMENT OF MICROBIOLOGY AND VIROLOGY PIROGOV’S RSMU
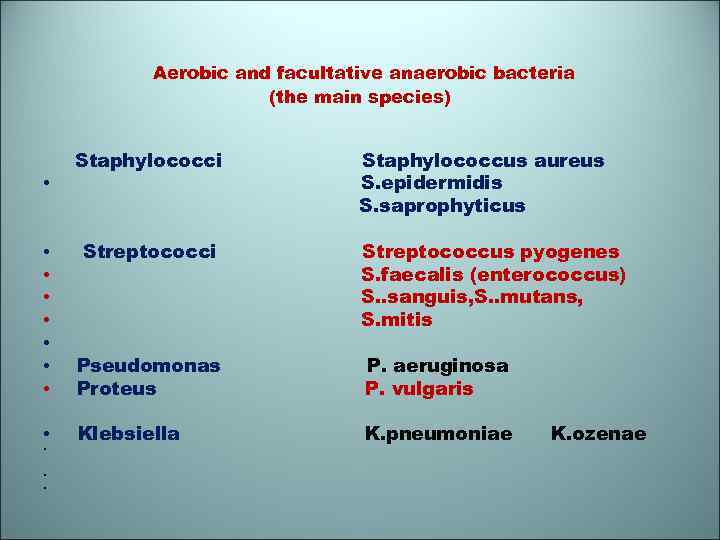 Aerobic and facultative anaerobic bacteria (the main species) Staphylococci • Streptococci • • • • • Pseudomonas Proteus Klebsiella Staphylococcus aureus S. epidermidis S. saprophyticus Streptococcus pyogenes S. faecalis (enterococcus) S. . sanguis, S. . mutans, S. mitis P. aeruginosa P. vulgaris K. pneumoniae K. ozenae
Aerobic and facultative anaerobic bacteria (the main species) Staphylococci • Streptococci • • • • • Pseudomonas Proteus Klebsiella Staphylococcus aureus S. epidermidis S. saprophyticus Streptococcus pyogenes S. faecalis (enterococcus) S. . sanguis, S. . mutans, S. mitis P. aeruginosa P. vulgaris K. pneumoniae K. ozenae
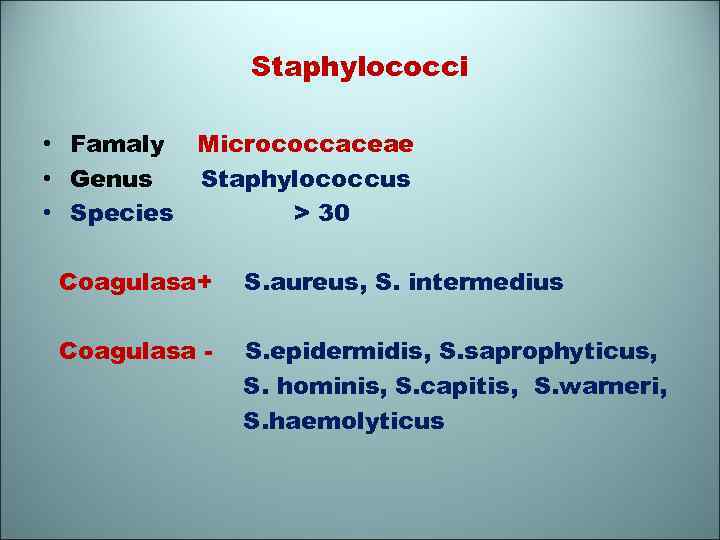 Staphylococci • Famaly Micrococcaceae • Genus Staphylococсus • Species > 30 Coagulasa+ S. aureus, S. intermedius Coagulasa - S. epidermidis, S. saprophyticus, S. hominis, S. capitis, S. warneri, S. haemolyticus
Staphylococci • Famaly Micrococcaceae • Genus Staphylococсus • Species > 30 Coagulasa+ S. aureus, S. intermedius Coagulasa - S. epidermidis, S. saprophyticus, S. hominis, S. capitis, S. warneri, S. haemolyticus
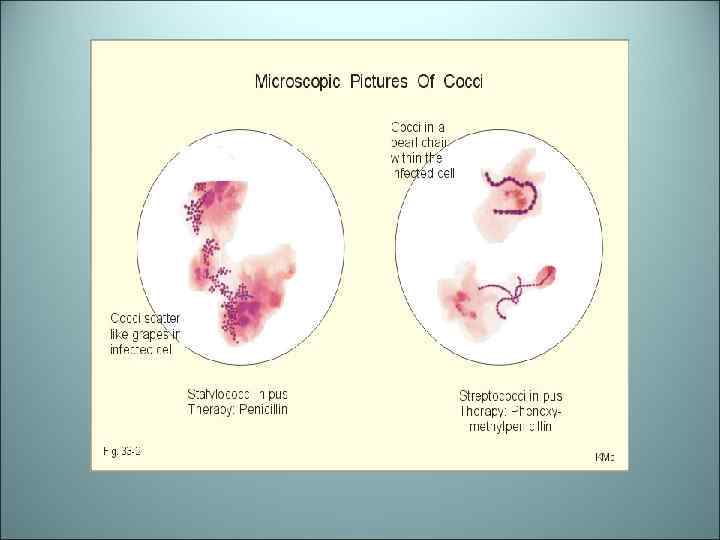
 Staphylococci • Staphylococcus aureus The name aureus means “golden" refers to bronze pigmentation of colonies (other are white). • S. saprophyticus is unique in that it apparently causes only urinary tract infections. • In Gram stain Staphylococcus look like clusters of grapes (staphylo from Greek word for grape clusters)
Staphylococci • Staphylococcus aureus The name aureus means “golden" refers to bronze pigmentation of colonies (other are white). • S. saprophyticus is unique in that it apparently causes only urinary tract infections. • In Gram stain Staphylococcus look like clusters of grapes (staphylo from Greek word for grape clusters)
 Staphylococcus aureus
Staphylococcus aureus
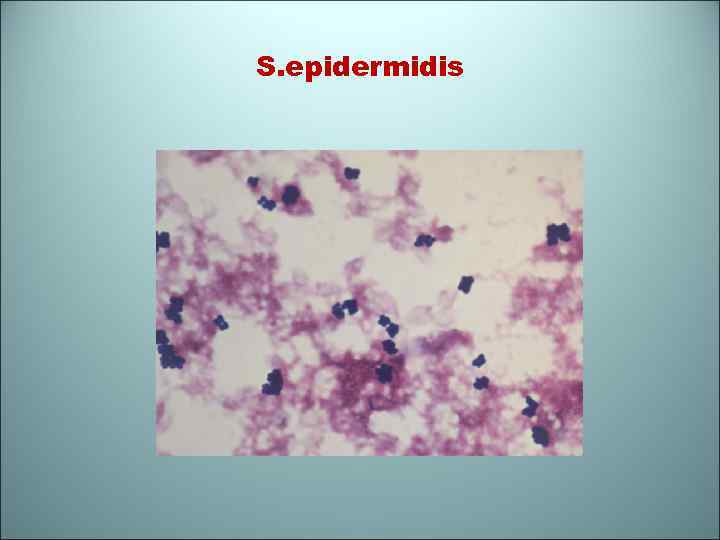 S. epidermidis
S. epidermidis
 S. aureus S. epidermidis
S. aureus S. epidermidis
 Disease caused by Staphylococci • • • Skin and soft tissue infection Furuncles Wound infections (traumatic, surgical) Endocarditis Cellulites Brain abscess Central nervous system infections Osteomyelitis Arthritis Musculoskeletal infection
Disease caused by Staphylococci • • • Skin and soft tissue infection Furuncles Wound infections (traumatic, surgical) Endocarditis Cellulites Brain abscess Central nervous system infections Osteomyelitis Arthritis Musculoskeletal infection
 Pus-producing
Pus-producing
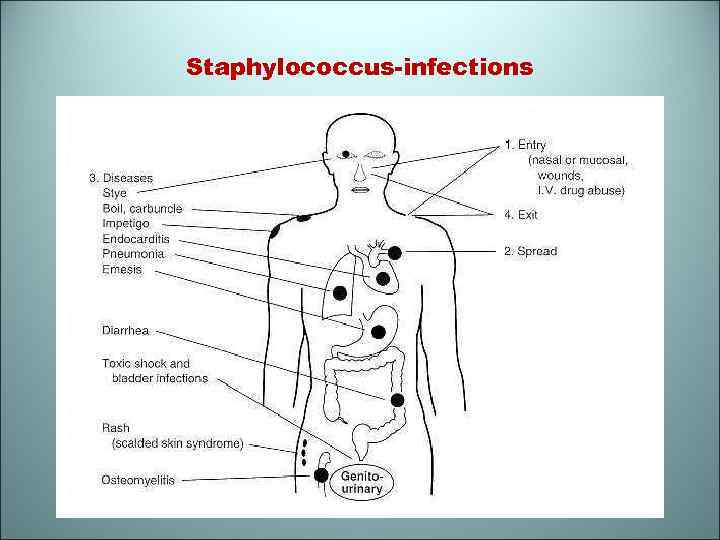 Staphylococcus-infections
Staphylococcus-infections
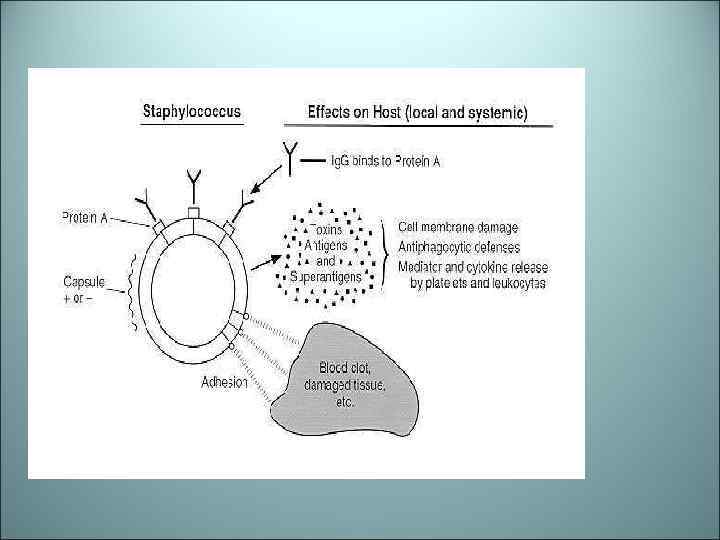
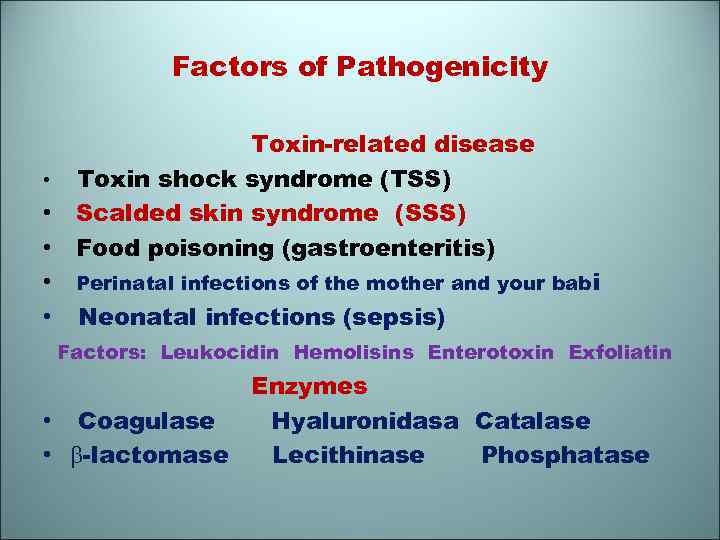 Factors of Pathogenicity • • • Toxin-related disease Toxin shock syndrome (TSS) Scalded skin syndrome (SSS) Food poisoning (gastroenteritis) Perinatal infections of the mother and your babi Neonatal infections (sepsis) Factors: Leukocidin Hemolisins Enterotoxin Exfoliatin Enzymes • Coagulase Hyaluronidasa Catalase • -lactomase Lecithinase Phosphatase
Factors of Pathogenicity • • • Toxin-related disease Toxin shock syndrome (TSS) Scalded skin syndrome (SSS) Food poisoning (gastroenteritis) Perinatal infections of the mother and your babi Neonatal infections (sepsis) Factors: Leukocidin Hemolisins Enterotoxin Exfoliatin Enzymes • Coagulase Hyaluronidasa Catalase • -lactomase Lecithinase Phosphatase
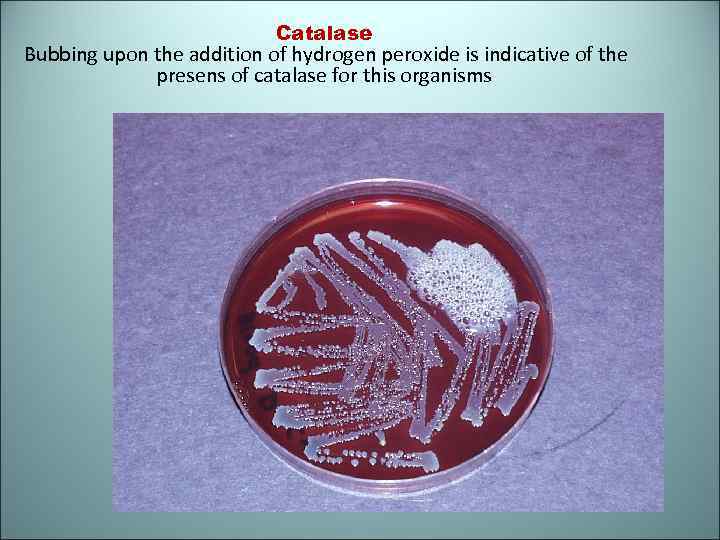 Catalase Bubbing upon the addition of hydrogen peroxide is indicative of the presens of catalase for this organisms
Catalase Bubbing upon the addition of hydrogen peroxide is indicative of the presens of catalase for this organisms
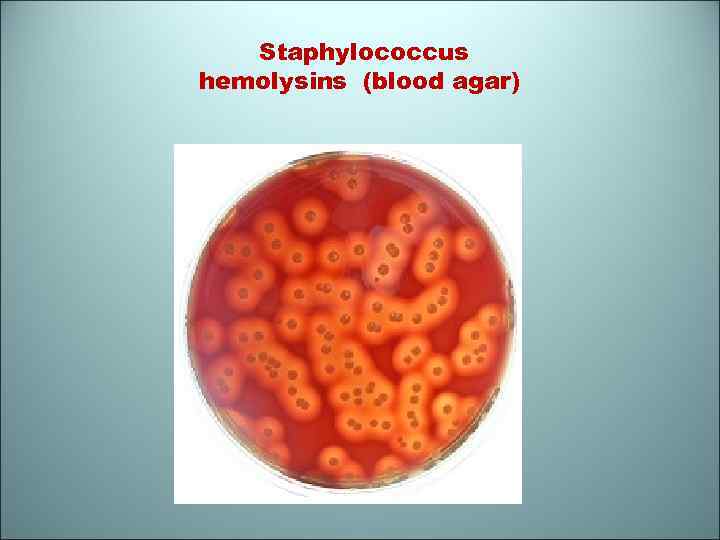 Staphylococcus hemolysins (blood agar)
Staphylococcus hemolysins (blood agar)
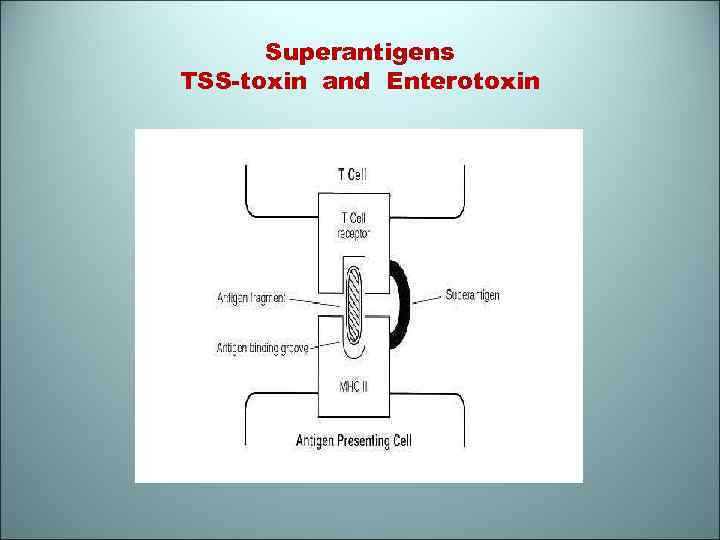 Superantigens TSS-toxin and Enterotoxin
Superantigens TSS-toxin and Enterotoxin
 The diagnostic tests • Morphology: cluster of large Gram-positiv cocci. A few strains possess microscopiccally visible capsules. • Bacteriology: culturing a specimen of pas on agg yolk with salt. • Biochemical testing: Staphylococci ferment a number sugars, producing acid but no gas • VPT+, indol-negativ, liquefy gelatin • Serological test: the reaction of toxin-neutralisation
The diagnostic tests • Morphology: cluster of large Gram-positiv cocci. A few strains possess microscopiccally visible capsules. • Bacteriology: culturing a specimen of pas on agg yolk with salt. • Biochemical testing: Staphylococci ferment a number sugars, producing acid but no gas • VPT+, indol-negativ, liquefy gelatin • Serological test: the reaction of toxin-neutralisation
 Treatment • Staphylococci are resistent to penicillin • Semisynthetic penicillins and cephalosporins are resistant to -lactomase and may be useful. Methicillin - with this property • However, methicillin-resistance has shreed to all hospitals and ofen requeresthe use of • vancomycin • cyprofloxacin, • rifampicin
Treatment • Staphylococci are resistent to penicillin • Semisynthetic penicillins and cephalosporins are resistant to -lactomase and may be useful. Methicillin - with this property • However, methicillin-resistance has shreed to all hospitals and ofen requeresthe use of • vancomycin • cyprofloxacin, • rifampicin
 Prevention • Antiserum (immune globulin) • Vaccine (toxoid) • Anti-staphylococcal bacteriophage
Prevention • Antiserum (immune globulin) • Vaccine (toxoid) • Anti-staphylococcal bacteriophage
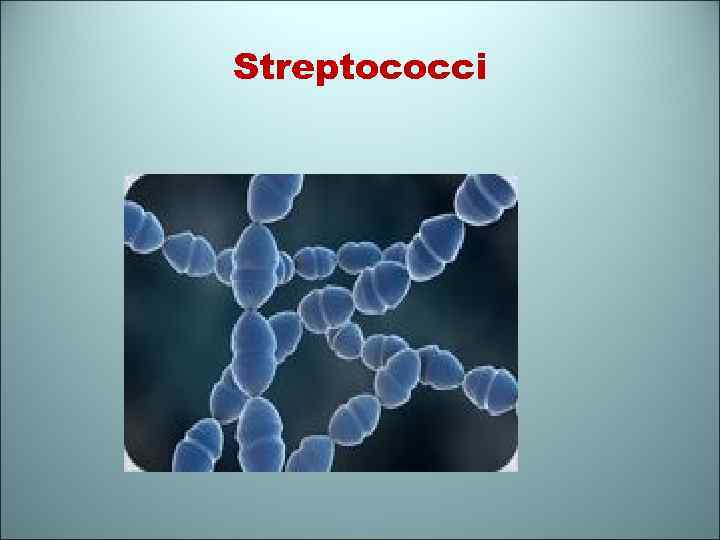 Streptococci
Streptococci
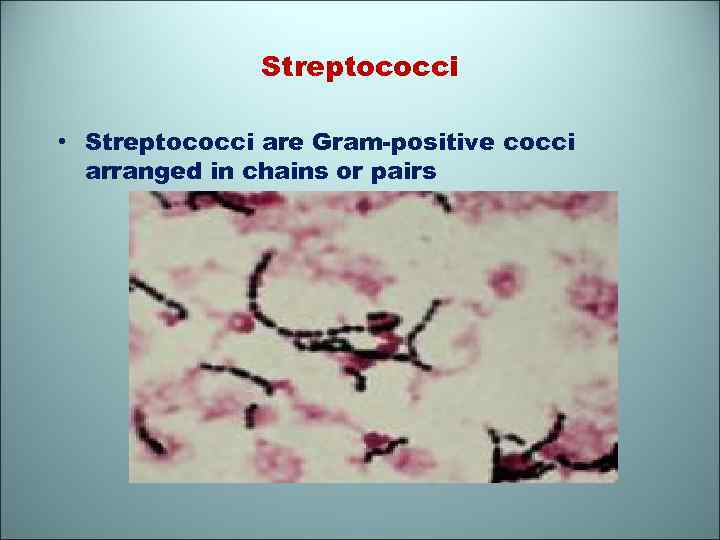 Streptococci • Streptococci are Gram-positive cocci arranged in chains or pairs
Streptococci • Streptococci are Gram-positive cocci arranged in chains or pairs
 The classification • I. Streptococci are divided by the type of hemolysis: • Alpha- hemolytic produce a greenish discoloration with partial hemolysis (S. pneumoniae, viridans-group) • Beta- hemolytic produce a sharply defined clear, colourless zone (S. agalactiae) • Gamma or nonhemolytic streptococci (S. fecalis – Enterococci)
The classification • I. Streptococci are divided by the type of hemolysis: • Alpha- hemolytic produce a greenish discoloration with partial hemolysis (S. pneumoniae, viridans-group) • Beta- hemolytic produce a sharply defined clear, colourless zone (S. agalactiae) • Gamma or nonhemolytic streptococci (S. fecalis – Enterococci)
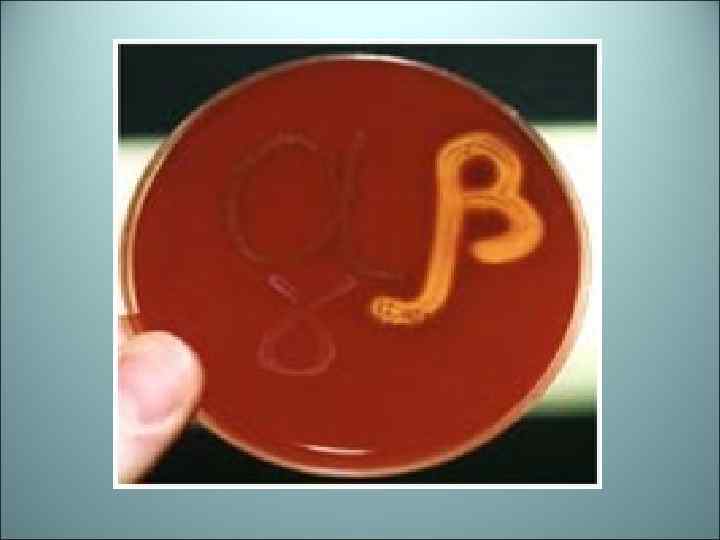
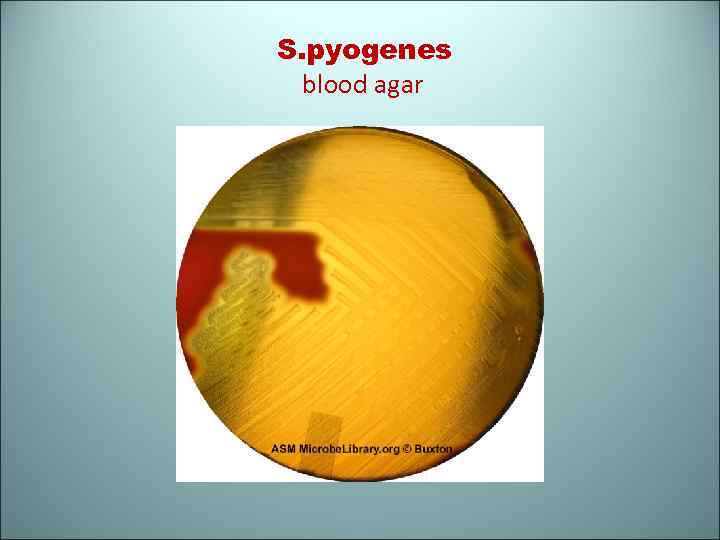 S. pyogenes blood agar
S. pyogenes blood agar
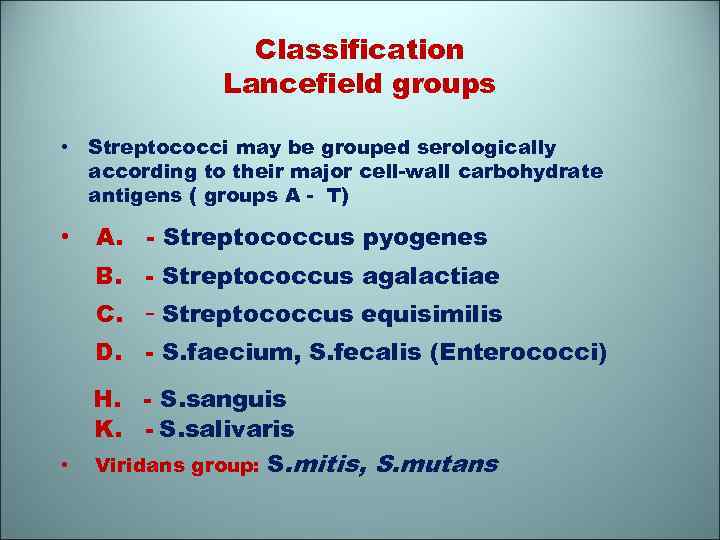 Classification Lancefield groups • Streptococci may be grouped serologically according to their major cell-wall carbohydrate antigens ( groups A - T) • A. - Streptococcus pyogenes B. - Streptococcus agalactiae D. H. - S. faecium, S. fecalis (Enterococci) C. - Streptococcus equisimilis - S. sanguis K. - S. salivaris • Viridans group: S. mitis, S. mutans
Classification Lancefield groups • Streptococci may be grouped serologically according to their major cell-wall carbohydrate antigens ( groups A - T) • A. - Streptococcus pyogenes B. - Streptococcus agalactiae D. H. - S. faecium, S. fecalis (Enterococci) C. - Streptococcus equisimilis - S. sanguis K. - S. salivaris • Viridans group: S. mitis, S. mutans
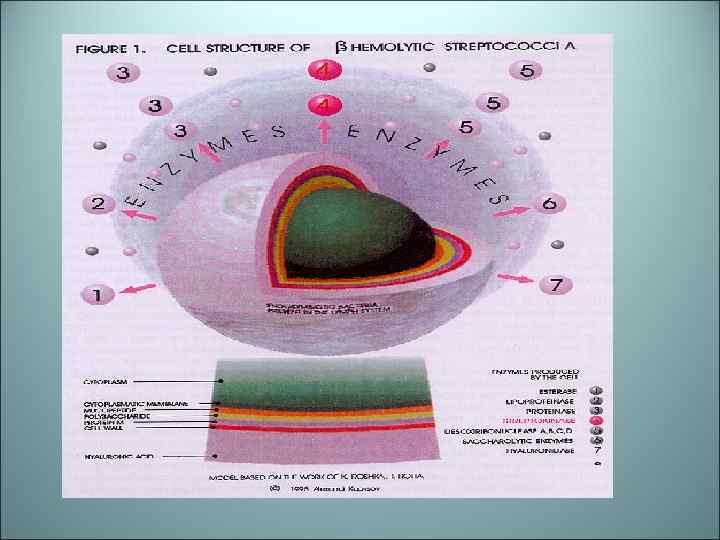
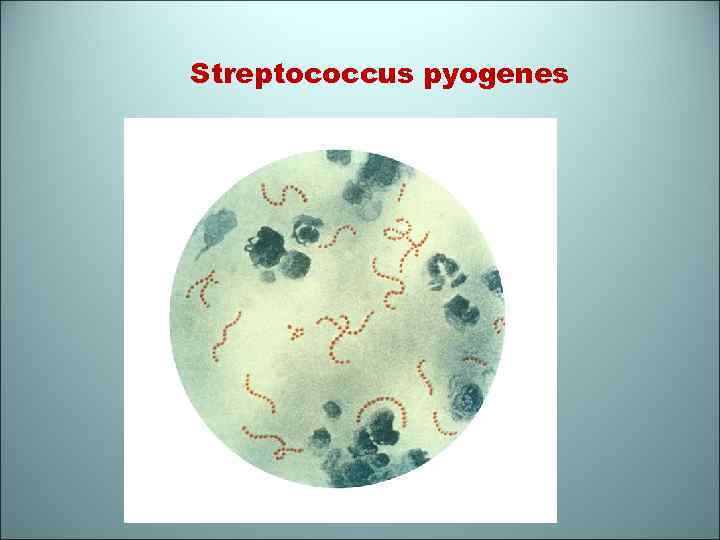 Streptococcus pyogenes
Streptococcus pyogenes
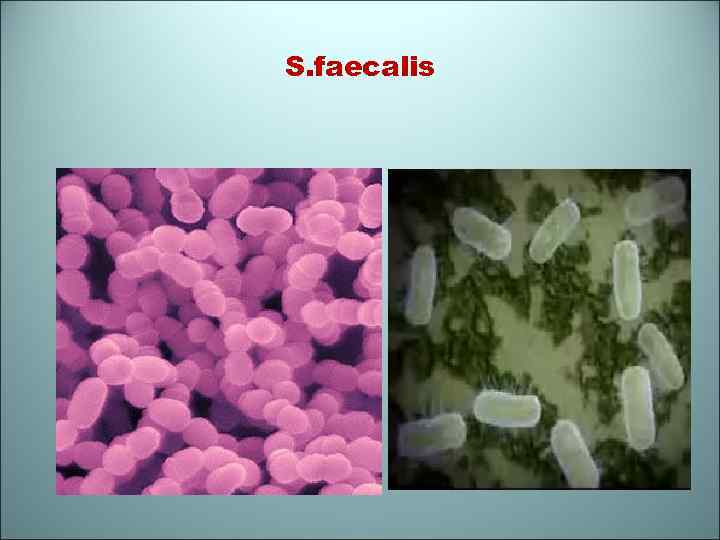 S. faecalis
S. faecalis
 Disease caused by streptococci • Group A S. pyogenus causes upper respiratory tract infections, “strep throat”, scarlet fever, rheumatic fever, pyoderma • Group B S. agalactiae causes neonatal sepsis • Group C and G cause abscess • Group D causes bacterial endocarditis and dental caries
Disease caused by streptococci • Group A S. pyogenus causes upper respiratory tract infections, “strep throat”, scarlet fever, rheumatic fever, pyoderma • Group B S. agalactiae causes neonatal sepsis • Group C and G cause abscess • Group D causes bacterial endocarditis and dental caries
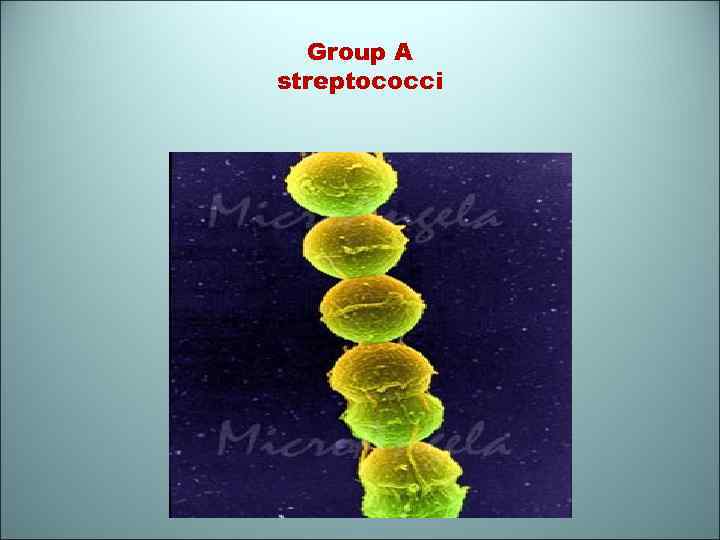 Group A streptococci
Group A streptococci
 Group B
Group B
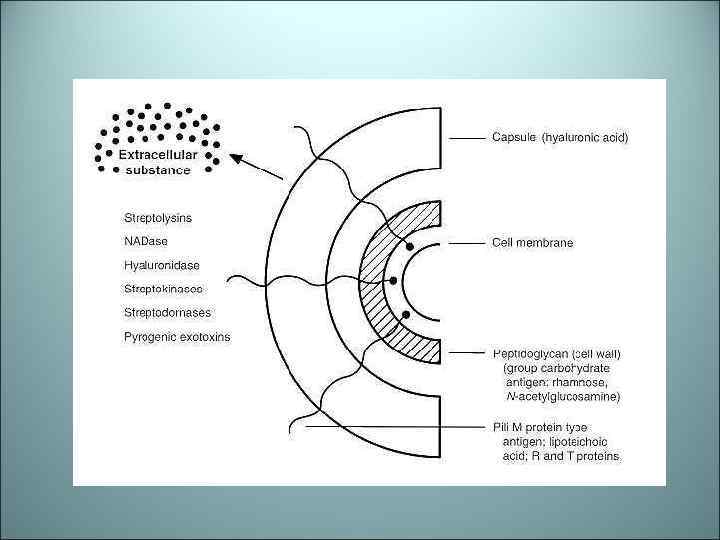
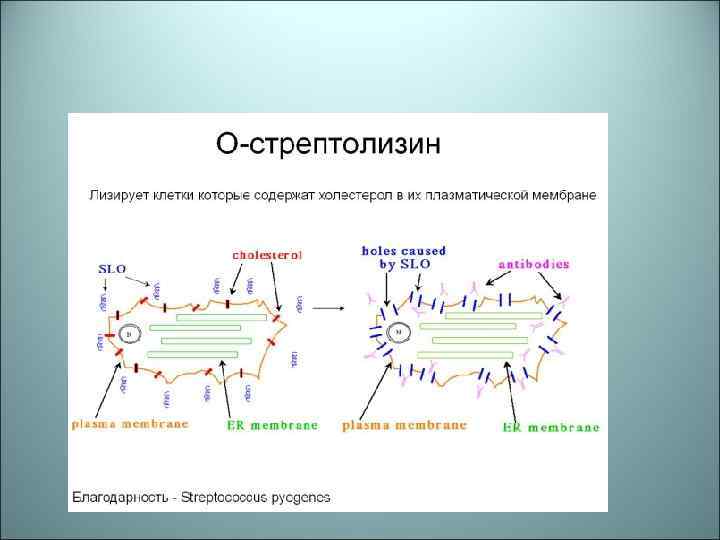
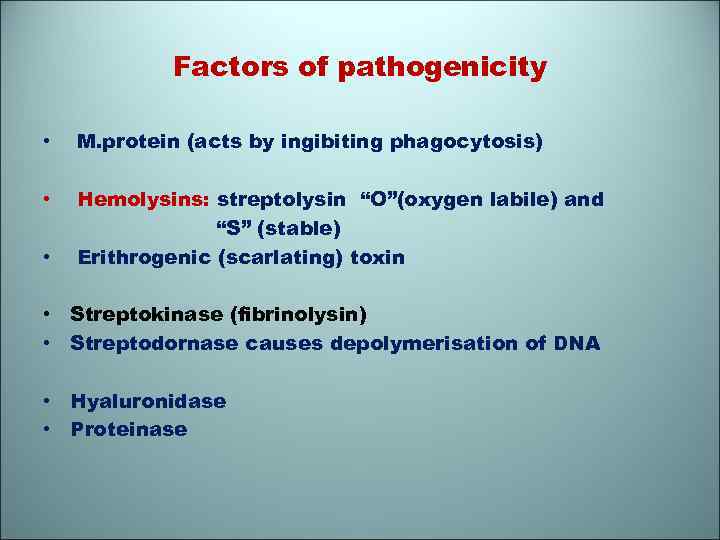 Factors of pathogenicity • M. protein (acts by ingibiting phagocytosis) • Hemolysins: streptolysin “O”(oxygen labile) and “S” (stable) Erithrogenic (scarlating) toxin • • Streptokinase (fibrinolysin) • Streptodornase causes depolymerisation of DNA • Hyaluronidase • Proteinase
Factors of pathogenicity • M. protein (acts by ingibiting phagocytosis) • Hemolysins: streptolysin “O”(oxygen labile) and “S” (stable) Erithrogenic (scarlating) toxin • • Streptokinase (fibrinolysin) • Streptodornase causes depolymerisation of DNA • Hyaluronidase • Proteinase
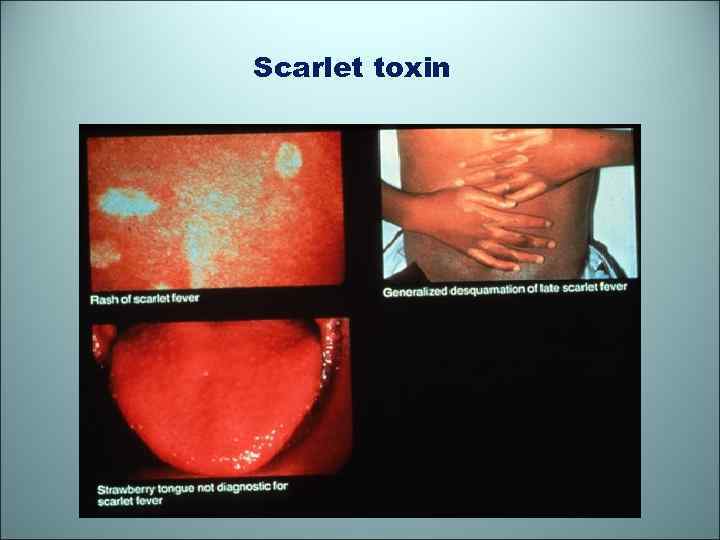 Scarlet toxin
Scarlet toxin
 Abscess
Abscess
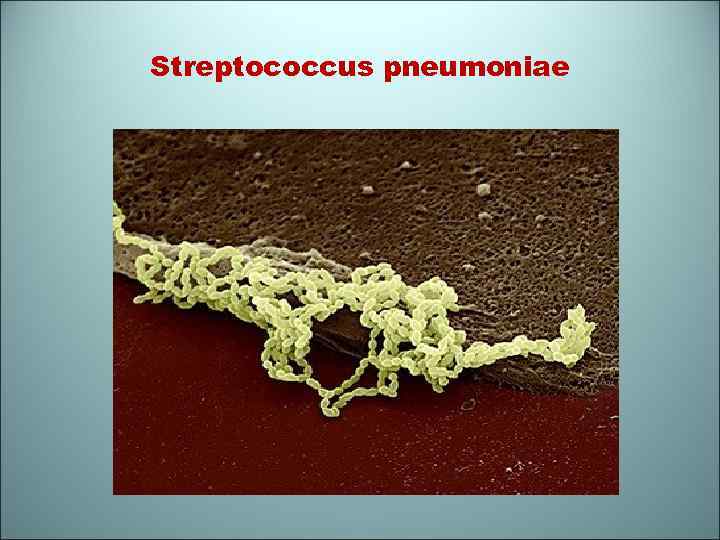 Streptococcus pneumoniae
Streptococcus pneumoniae
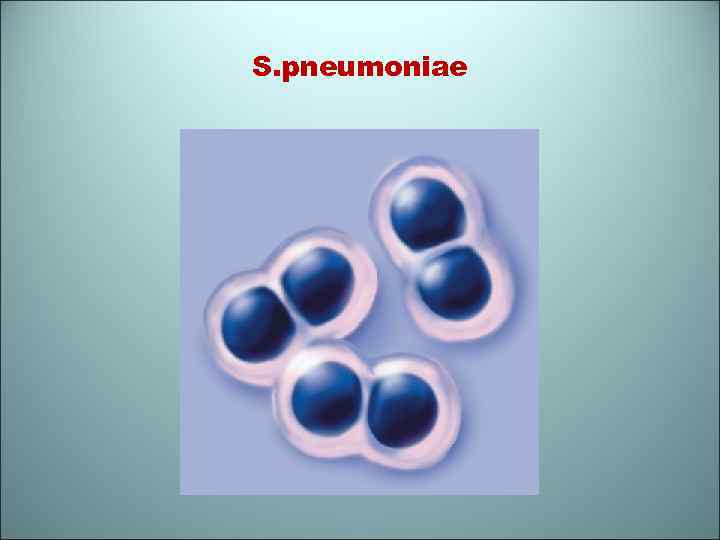 S. pneumoniae
S. pneumoniae
 Pleuritis S. pneumoniae
Pleuritis S. pneumoniae
 rheumfev
rheumfev
 Impetigo
Impetigo
 Keratit
Keratit
 Erysipelas
Erysipelas
 Scarlet (S. pyogenes)
Scarlet (S. pyogenes)
 Pseudomonas aeruginosa • P. aeruginosa is ubiquitous opportunistic pathogen (in soil, water) • P. aeruginosa produced a number of pigments the best known being pyocyanin. • The infections caused by P. aeruginosa: • osteomyelitis, burn wound infection, • urinary tract infection (predisposing factor – kidney stones), • septicemia, pneumoniae, • meningitis (neurosurgical operations)
Pseudomonas aeruginosa • P. aeruginosa is ubiquitous opportunistic pathogen (in soil, water) • P. aeruginosa produced a number of pigments the best known being pyocyanin. • The infections caused by P. aeruginosa: • osteomyelitis, burn wound infection, • urinary tract infection (predisposing factor – kidney stones), • septicemia, pneumoniae, • meningitis (neurosurgical operations)
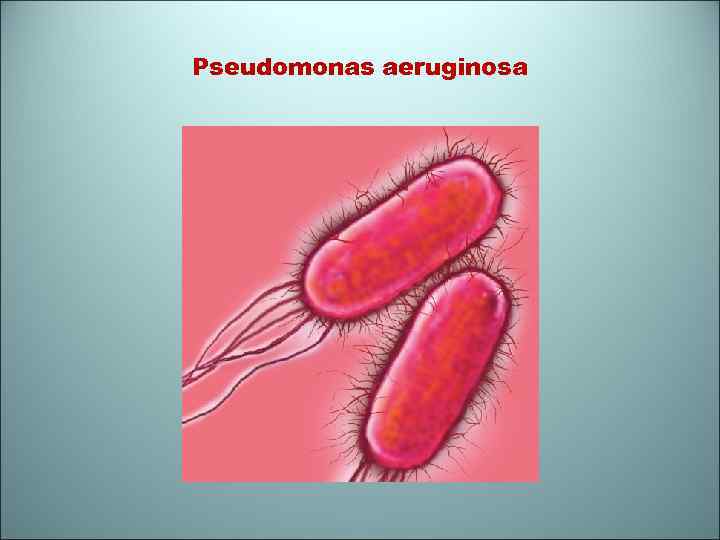 Pseudomonas aeruginosa
Pseudomonas aeruginosa
 Factors of Pathogenicity • Pili (adherence, colonisation) • Flagellum (motility) • Endotoxin (stimulates vasoactive peptides, activates clotting) • Exotoxin A – histo- or cytotoxin (tissue damage, shock) • Elastase (cleavage of elastin, collagen, Ig) • Phospholipase C (tissue damage)
Factors of Pathogenicity • Pili (adherence, colonisation) • Flagellum (motility) • Endotoxin (stimulates vasoactive peptides, activates clotting) • Exotoxin A – histo- or cytotoxin (tissue damage, shock) • Elastase (cleavage of elastin, collagen, Ig) • Phospholipase C (tissue damage)
 The diagnostic tests • Morphology: they are Gram-negative rods • Diagnosis by cultere: P. aeruginosa is obligate aerobe, grows well on ordinary media, producing colonies with bluish green pigment • Biochemical testing: catalase+, oxidase+, indol-, H 2 S-
The diagnostic tests • Morphology: they are Gram-negative rods • Diagnosis by cultere: P. aeruginosa is obligate aerobe, grows well on ordinary media, producing colonies with bluish green pigment • Biochemical testing: catalase+, oxidase+, indol-, H 2 S-
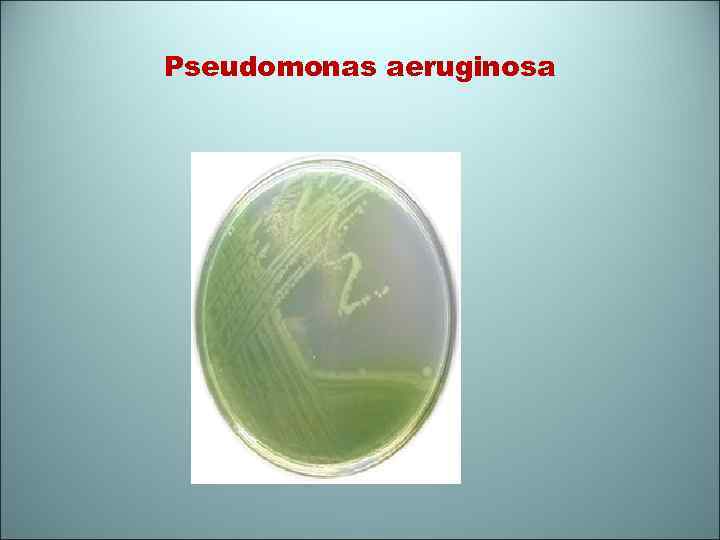 Pseudomonas aeruginosa
Pseudomonas aeruginosa
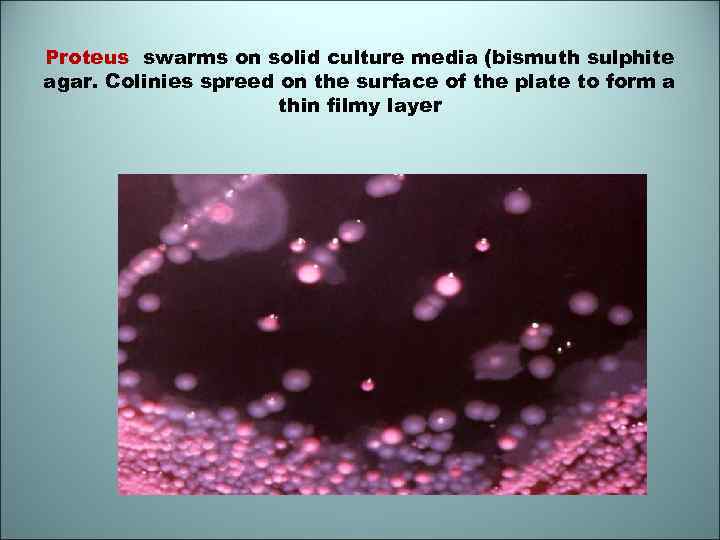 Proteus swarms on solid culture media (bismuth sulphite agar. Colinies spreed on the surface of the plate to form a thin filmy layer
Proteus swarms on solid culture media (bismuth sulphite agar. Colinies spreed on the surface of the plate to form a thin filmy layer


