9c59b2d39d6144d52e77e6388c1a8c2a.ppt
- Количество слайдов: 33
 Case Study: Sepsis Jill Collins, Dana Hogan, Louisa Golay, Krystal Morris & Wanda Schumacher December 16, 2010
Case Study: Sepsis Jill Collins, Dana Hogan, Louisa Golay, Krystal Morris & Wanda Schumacher December 16, 2010
 History of Present Illness • 30 y/o pt presents to ED with increasing mental status changes and abdominal pain X 24 hrs per skilled nursing facility – Nursing home staff reports pt had unwitnessed fall last NOC • Patient appears diaphoretic, increased respiratory rate, thready pulses, flushed skin, hot to touch • Pt unable to verbalize pain rating; FACES score of 7 -8 given from observed grimacing and moaning
History of Present Illness • 30 y/o pt presents to ED with increasing mental status changes and abdominal pain X 24 hrs per skilled nursing facility – Nursing home staff reports pt had unwitnessed fall last NOC • Patient appears diaphoretic, increased respiratory rate, thready pulses, flushed skin, hot to touch • Pt unable to verbalize pain rating; FACES score of 7 -8 given from observed grimacing and moaning
 MEDICAL/SOCIAL HISTORY MEDICAL SOCIAL • Medical History • Patient single without children, previously lived alone • Family denies pt using tobacco, alcohol, or recreational drugs • Family unable to report if pt is currently sexually active • Patient appears to have strong support system in place – HIV – End Stage Liver Disease • Liver cirrhosis • Hepatic Encephalopathy – SIADH – Diabetes Mellitus Type 2 • Surgical History – Upper Gastrointestinal Endoscopy – Adenoidectomy
MEDICAL/SOCIAL HISTORY MEDICAL SOCIAL • Medical History • Patient single without children, previously lived alone • Family denies pt using tobacco, alcohol, or recreational drugs • Family unable to report if pt is currently sexually active • Patient appears to have strong support system in place – HIV – End Stage Liver Disease • Liver cirrhosis • Hepatic Encephalopathy – SIADH – Diabetes Mellitus Type 2 • Surgical History – Upper Gastrointestinal Endoscopy – Adenoidectomy
 Previous Admissions • Admitted 6 months ago with hepatic encephalopathy, acute kidney injury, hyperkalemia, EKG changes • Hepatic encephalopathy resolved with lactulose treatments, kidney function improved with short term dialysis • Patient was discharged after a 2 month hospitalization to a skilled nursing facility for rehabilitation
Previous Admissions • Admitted 6 months ago with hepatic encephalopathy, acute kidney injury, hyperkalemia, EKG changes • Hepatic encephalopathy resolved with lactulose treatments, kidney function improved with short term dialysis • Patient was discharged after a 2 month hospitalization to a skilled nursing facility for rehabilitation
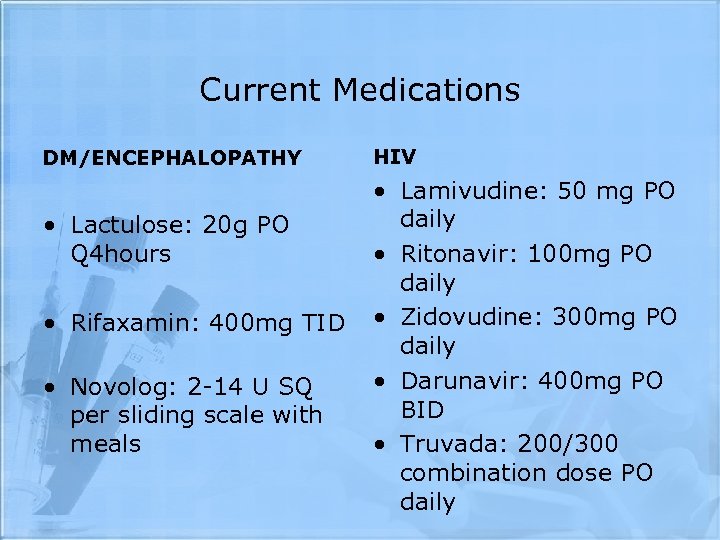 Current Medications DM/ENCEPHALOPATHY • Lactulose: 20 g PO Q 4 hours • Rifaxamin: 400 mg TID • Novolog: 2 -14 U SQ per sliding scale with meals HIV • Lamivudine: 50 mg PO daily • Ritonavir: 100 mg PO daily • Zidovudine: 300 mg PO daily • Darunavir: 400 mg PO BID • Truvada: 200/300 combination dose PO daily
Current Medications DM/ENCEPHALOPATHY • Lactulose: 20 g PO Q 4 hours • Rifaxamin: 400 mg TID • Novolog: 2 -14 U SQ per sliding scale with meals HIV • Lamivudine: 50 mg PO daily • Ritonavir: 100 mg PO daily • Zidovudine: 300 mg PO daily • Darunavir: 400 mg PO BID • Truvada: 200/300 combination dose PO daily
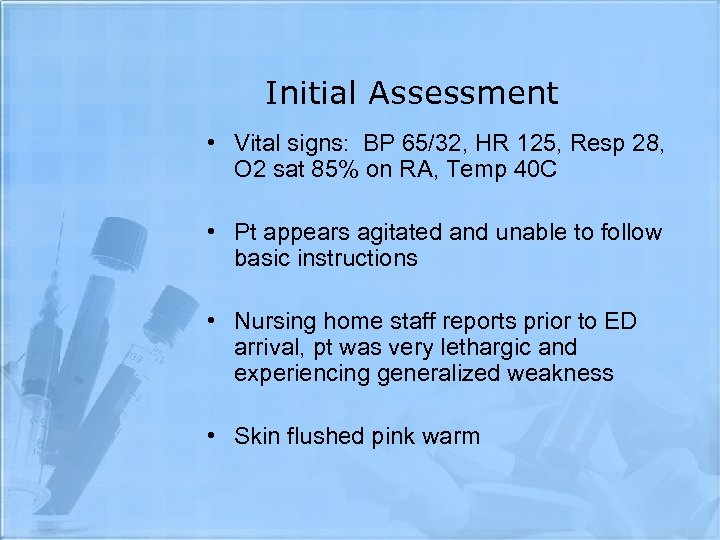 Initial Assessment • Vital signs: BP 65/32, HR 125, Resp 28, O 2 sat 85% on RA, Temp 40 C • Pt appears agitated and unable to follow basic instructions • Nursing home staff reports prior to ED arrival, pt was very lethargic and experiencing generalized weakness • Skin flushed pink warm
Initial Assessment • Vital signs: BP 65/32, HR 125, Resp 28, O 2 sat 85% on RA, Temp 40 C • Pt appears agitated and unable to follow basic instructions • Nursing home staff reports prior to ED arrival, pt was very lethargic and experiencing generalized weakness • Skin flushed pink warm
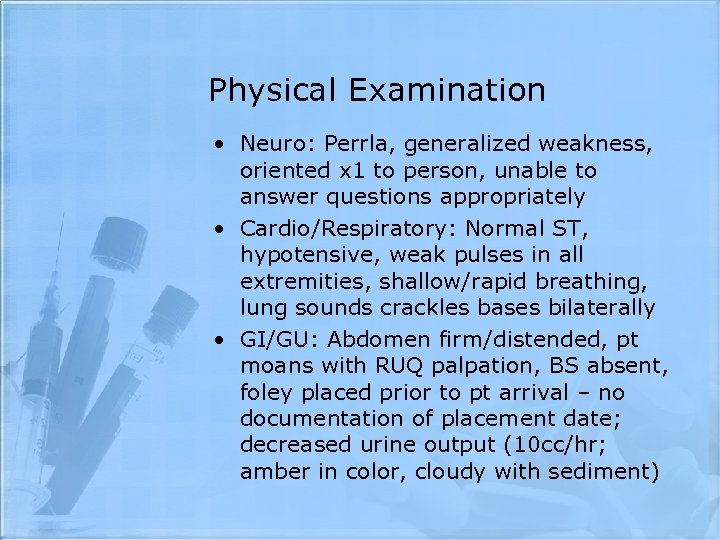 Physical Examination • Neuro: Perrla, generalized weakness, oriented x 1 to person, unable to answer questions appropriately • Cardio/Respiratory: Normal ST, hypotensive, weak pulses in all extremities, shallow/rapid breathing, lung sounds crackles bases bilaterally • GI/GU: Abdomen firm/distended, pt moans with RUQ palpation, BS absent, foley placed prior to pt arrival – no documentation of placement date; decreased urine output (10 cc/hr; amber in color, cloudy with sediment)
Physical Examination • Neuro: Perrla, generalized weakness, oriented x 1 to person, unable to answer questions appropriately • Cardio/Respiratory: Normal ST, hypotensive, weak pulses in all extremities, shallow/rapid breathing, lung sounds crackles bases bilaterally • GI/GU: Abdomen firm/distended, pt moans with RUQ palpation, BS absent, foley placed prior to pt arrival – no documentation of placement date; decreased urine output (10 cc/hr; amber in color, cloudy with sediment)
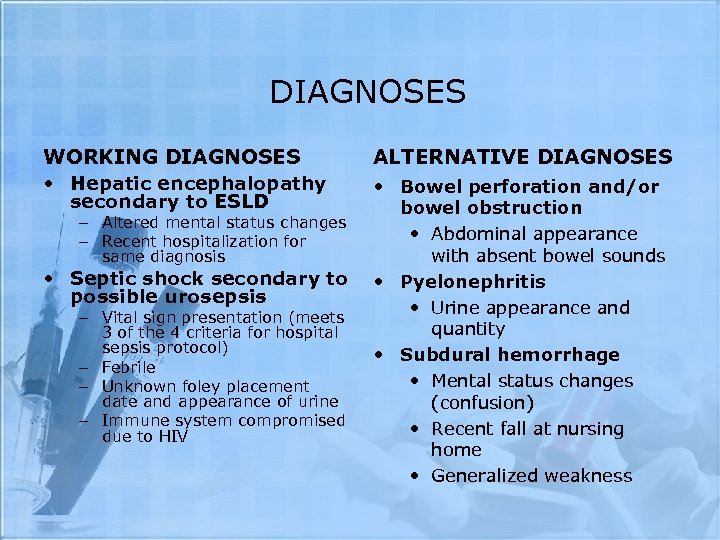 DIAGNOSES WORKING DIAGNOSES • Hepatic encephalopathy secondary to ESLD – Altered mental status changes – Recent hospitalization for same diagnosis • Septic shock secondary to possible urosepsis – Vital sign presentation (meets 3 of the 4 criteria for hospital sepsis protocol) – Febrile – Unknown foley placement date and appearance of urine – Immune system compromised due to HIV ALTERNATIVE DIAGNOSES • Bowel perforation and/or bowel obstruction • Abdominal appearance with absent bowel sounds • Pyelonephritis • Urine appearance and quantity • Subdural hemorrhage • Mental status changes (confusion) • Recent fall at nursing home • Generalized weakness
DIAGNOSES WORKING DIAGNOSES • Hepatic encephalopathy secondary to ESLD – Altered mental status changes – Recent hospitalization for same diagnosis • Septic shock secondary to possible urosepsis – Vital sign presentation (meets 3 of the 4 criteria for hospital sepsis protocol) – Febrile – Unknown foley placement date and appearance of urine – Immune system compromised due to HIV ALTERNATIVE DIAGNOSES • Bowel perforation and/or bowel obstruction • Abdominal appearance with absent bowel sounds • Pyelonephritis • Urine appearance and quantity • Subdural hemorrhage • Mental status changes (confusion) • Recent fall at nursing home • Generalized weakness
 OTHER DIAGNOSES • Pneumonia • Febrile, respiratory status, and recent hospitalization with d/c to nursing facility • Stroke • Altered mental status changes, generalized weakness, and recent fall • Abdominal Aortic Aneurysm • Abdominal assessment & severe hypotension
OTHER DIAGNOSES • Pneumonia • Febrile, respiratory status, and recent hospitalization with d/c to nursing facility • Stroke • Altered mental status changes, generalized weakness, and recent fall • Abdominal Aortic Aneurysm • Abdominal assessment & severe hypotension
 DIAGNOSIS CONT. SEPSIS WORKING DIAGNOSES • Urosepsis • Sepsis caused by pneumocysitc pneumonia • Sepsis caused by bowel perforation or obstruction • SIRS from pancreatitis and ESLD FINAL DIAGNOSIS SEVERE UROSEPSIS
DIAGNOSIS CONT. SEPSIS WORKING DIAGNOSES • Urosepsis • Sepsis caused by pneumocysitc pneumonia • Sepsis caused by bowel perforation or obstruction • SIRS from pancreatitis and ESLD FINAL DIAGNOSIS SEVERE UROSEPSIS
 UROSEPSIS • Definition: Severe Sepsis • Suspected or proven infection, plus a systemic inflammatory response (e. g. fever, tachycardia, tachypnea, elevated white blood cell count, altered mental state, and hyperglycemia in the absence of diabetes) with organ dysfunction (e. g. hypotension, hypoxemia, oliguria, metabolic acidosis, thrombocytopenia, or obtundation). (Porth, 628) • Epidemiology • Estimated that more that 750, 000 cases of sepsis occur each year in the US ultimately leading to approximately 225, 000 deaths. (Porth, 628) • Severe Sepsis is the leading cause of death in non-coronary ICU’s (www. acponline. org) • Sepsis has a mortality rate of about 40% currently in the US (www. merckmanuals. com)
UROSEPSIS • Definition: Severe Sepsis • Suspected or proven infection, plus a systemic inflammatory response (e. g. fever, tachycardia, tachypnea, elevated white blood cell count, altered mental state, and hyperglycemia in the absence of diabetes) with organ dysfunction (e. g. hypotension, hypoxemia, oliguria, metabolic acidosis, thrombocytopenia, or obtundation). (Porth, 628) • Epidemiology • Estimated that more that 750, 000 cases of sepsis occur each year in the US ultimately leading to approximately 225, 000 deaths. (Porth, 628) • Severe Sepsis is the leading cause of death in non-coronary ICU’s (www. acponline. org) • Sepsis has a mortality rate of about 40% currently in the US (www. merckmanuals. com)
 PATHOPHYSIOLOGY • Etiology • Most likely caused by bacterial organism in the urine which most likely developed as a result of a chronic indwelling foley catheter. Most cases of sepsis are caused by hospital-acquired gram-negative bacilli or gram positive cocci and often occur in immunocompromised patients and those with chronic and debilitating diseases (www. merckmanuals. com)
PATHOPHYSIOLOGY • Etiology • Most likely caused by bacterial organism in the urine which most likely developed as a result of a chronic indwelling foley catheter. Most cases of sepsis are caused by hospital-acquired gram-negative bacilli or gram positive cocci and often occur in immunocompromised patients and those with chronic and debilitating diseases (www. merckmanuals. com)
 PATHOPHYSIOLOGY CONT. • Mechanisms of the disease • Immunocompromised by HIV and diabetes mellitus • Chronic indwelling catheter is source for bacterial collection • Decreased food and fluid intake secondary to altered mental status from hepatic encephalopathy • Possible alteration in electrolytes secondary to medication for hepatic encephalopathy (lactulose)
PATHOPHYSIOLOGY CONT. • Mechanisms of the disease • Immunocompromised by HIV and diabetes mellitus • Chronic indwelling catheter is source for bacterial collection • Decreased food and fluid intake secondary to altered mental status from hepatic encephalopathy • Possible alteration in electrolytes secondary to medication for hepatic encephalopathy (lactulose)
 PATHOPHYSIOLOGY CONT. • Pathogenesis of disease • Starts with inflammatory trigger (bacteria) • Proinflammatory mediators are stimulated (tumor necrosis factor and IL-1) • Cytokines cause neutrophil-endothelial cell adhesion, activate the clotting mechanism, and generate microthrombi. • Other mediators released including leukotrienes, lipoxygenase, histamine, bradykinin, serotonin, and IL-2. • These are opposed by anti-inflammatory mediators like IL-4 and IL-10 which results in a negative feedback mechanism. • Vasoactive mediators cause blood flow to bypass capillary exchange vessels. • Poor capillary flow from the shunting along with capillary obstruction by microthrombi decreases the delivery of oxygen and impairs removal of carbon dioxide and waste products. • Decreased perfusion causes dysfunction and sometimes failure of one or more organs, including the kidneys, lungs, liver, brain, and heart. • Coagulopathy can develop because of intravascular coagulation with comsumption of major clotting factors. (www. merckmanuals. com)
PATHOPHYSIOLOGY CONT. • Pathogenesis of disease • Starts with inflammatory trigger (bacteria) • Proinflammatory mediators are stimulated (tumor necrosis factor and IL-1) • Cytokines cause neutrophil-endothelial cell adhesion, activate the clotting mechanism, and generate microthrombi. • Other mediators released including leukotrienes, lipoxygenase, histamine, bradykinin, serotonin, and IL-2. • These are opposed by anti-inflammatory mediators like IL-4 and IL-10 which results in a negative feedback mechanism. • Vasoactive mediators cause blood flow to bypass capillary exchange vessels. • Poor capillary flow from the shunting along with capillary obstruction by microthrombi decreases the delivery of oxygen and impairs removal of carbon dioxide and waste products. • Decreased perfusion causes dysfunction and sometimes failure of one or more organs, including the kidneys, lungs, liver, brain, and heart. • Coagulopathy can develop because of intravascular coagulation with comsumption of major clotting factors. (www. merckmanuals. com)
 PATHOPHYSIOLOGY CONT. • Relation of pathology to history and clinical manifestations • Pt. immunocompromised by HIV, DM and cirrhosis • Indwelling catheter source of bacterial growth and proliferation • Bacteria in urinary tract eventually trigged the pathophysiologic process discussed in previous slide. • Processes eventually lead to decreased perfusion to organs which probably caused the altered mental status and possibly the abdominal pain (also caused by the UTI) • Hypotension occurs secondary to the vasodilation caused by the inflammatory response. Tachycardia then ensues in an attempt to keep blood pressure and cardiac output up. Tachypnea is an attempt of the body to remove excess acid buildup as well as the decreased availabilty of oxygen (hypoxemia)caused by the sepsis process. Fever occurs as a result of the energy expenditure needed to fight the bacterial invasion.
PATHOPHYSIOLOGY CONT. • Relation of pathology to history and clinical manifestations • Pt. immunocompromised by HIV, DM and cirrhosis • Indwelling catheter source of bacterial growth and proliferation • Bacteria in urinary tract eventually trigged the pathophysiologic process discussed in previous slide. • Processes eventually lead to decreased perfusion to organs which probably caused the altered mental status and possibly the abdominal pain (also caused by the UTI) • Hypotension occurs secondary to the vasodilation caused by the inflammatory response. Tachycardia then ensues in an attempt to keep blood pressure and cardiac output up. Tachypnea is an attempt of the body to remove excess acid buildup as well as the decreased availabilty of oxygen (hypoxemia)caused by the sepsis process. Fever occurs as a result of the energy expenditure needed to fight the bacterial invasion.
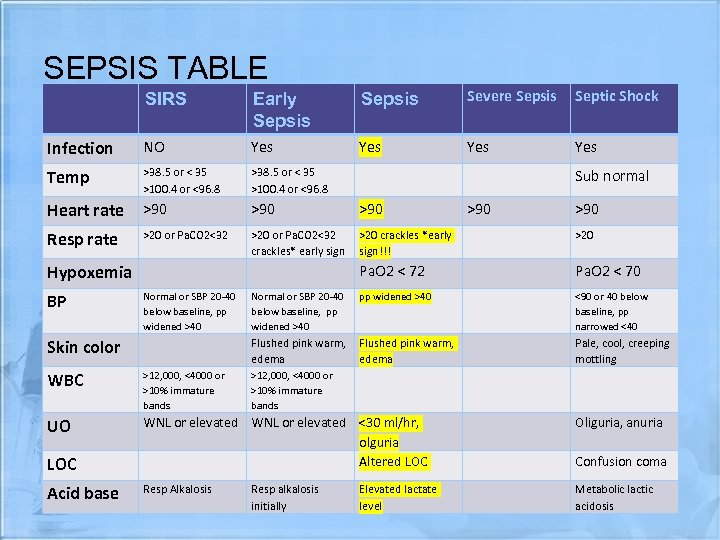 SEPSIS TABLE SIRS Early Sepsis Severe Sepsis Septic Shock Infection NO Yes Yes Temp >38. 5 or < 35 >100. 4 or <96. 8 Heart rate >90 >90 Resp rate >20 or Pa. CO 2<32 crackles* early sign >20 crackles *early sign!!! >20 Pa. O 2 < 72 Pa. O 2 < 70 Normal or SBP 20 -40 below baseline, pp widened >40 <90 or 40 below baseline, pp narrowed <40 Flushed pink warm, edema Pale, cool, creeping mottling Hypoxemia BP Normal or SBP 20 -40 below baseline, pp widened >40 Skin color Sub normal >90 WBC >12, 000, <4000 or >10% immature bands UO WNL or elevated <30 ml/hr, olguria Altered LOC Oliguria, anuria Resp Alkalosis Metabolic lactic acidosis LOC Acid base >12, 000, <4000 or >10% immature bands Resp alkalosis initially Elevated lactate level Confusion coma
SEPSIS TABLE SIRS Early Sepsis Severe Sepsis Septic Shock Infection NO Yes Yes Temp >38. 5 or < 35 >100. 4 or <96. 8 Heart rate >90 >90 Resp rate >20 or Pa. CO 2<32 crackles* early sign >20 crackles *early sign!!! >20 Pa. O 2 < 72 Pa. O 2 < 70 Normal or SBP 20 -40 below baseline, pp widened >40 <90 or 40 below baseline, pp narrowed <40 Flushed pink warm, edema Pale, cool, creeping mottling Hypoxemia BP Normal or SBP 20 -40 below baseline, pp widened >40 Skin color Sub normal >90 WBC >12, 000, <4000 or >10% immature bands UO WNL or elevated <30 ml/hr, olguria Altered LOC Oliguria, anuria Resp Alkalosis Metabolic lactic acidosis LOC Acid base >12, 000, <4000 or >10% immature bands Resp alkalosis initially Elevated lactate level Confusion coma
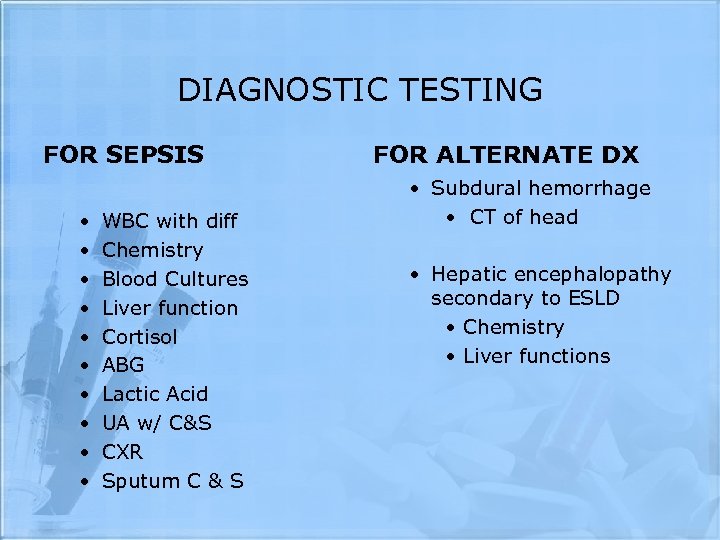 DIAGNOSTIC TESTING FOR SEPSIS • • • WBC with diff Chemistry Blood Cultures Liver function Cortisol ABG Lactic Acid UA w/ C&S CXR Sputum C & S FOR ALTERNATE DX • Subdural hemorrhage • CT of head • Hepatic encephalopathy secondary to ESLD • Chemistry • Liver functions
DIAGNOSTIC TESTING FOR SEPSIS • • • WBC with diff Chemistry Blood Cultures Liver function Cortisol ABG Lactic Acid UA w/ C&S CXR Sputum C & S FOR ALTERNATE DX • Subdural hemorrhage • CT of head • Hepatic encephalopathy secondary to ESLD • Chemistry • Liver functions
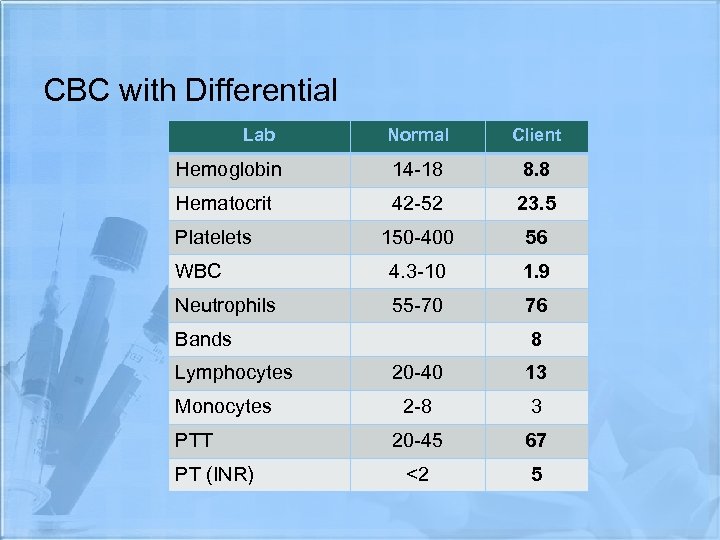 CBC with Differential Lab Normal Client Hemoglobin 14 -18 8. 8 Hematocrit 42 -52 23. 5 150 -400 56 WBC 4. 3 -10 1. 9 Neutrophils 55 -70 76 Platelets Bands Lymphocytes Monocytes PTT PT (INR) 8 20 -40 13 2 -8 3 20 -45 67 <2 5
CBC with Differential Lab Normal Client Hemoglobin 14 -18 8. 8 Hematocrit 42 -52 23. 5 150 -400 56 WBC 4. 3 -10 1. 9 Neutrophils 55 -70 76 Platelets Bands Lymphocytes Monocytes PTT PT (INR) 8 20 -40 13 2 -8 3 20 -45 67 <2 5
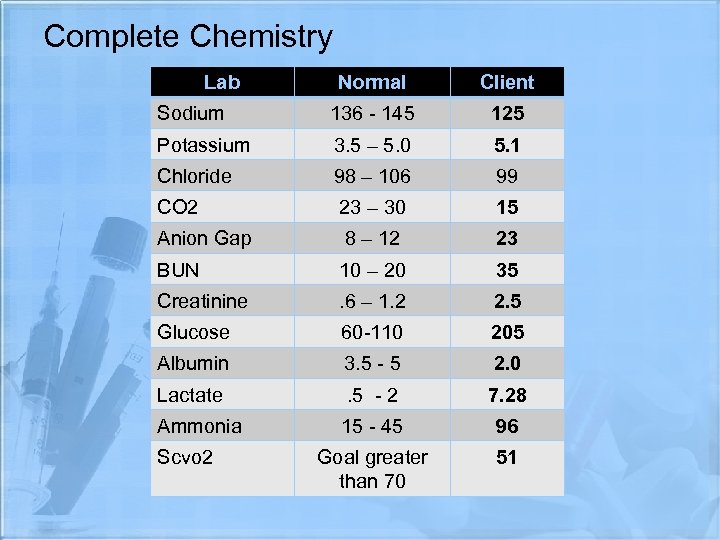 Complete Chemistry Lab Normal Client Sodium 136 - 145 125 Potassium 3. 5 – 5. 0 5. 1 Chloride 98 – 106 99 CO 2 23 – 30 15 Anion Gap 8 – 12 23 BUN 10 – 20 35 Creatinine . 6 – 1. 2 2. 5 Glucose 60 -110 205 Albumin 3. 5 - 5 2. 0 Lactate . 5 - 2 7. 28 Ammonia 15 - 45 96 Goal greater than 70 51 Scvo 2
Complete Chemistry Lab Normal Client Sodium 136 - 145 125 Potassium 3. 5 – 5. 0 5. 1 Chloride 98 – 106 99 CO 2 23 – 30 15 Anion Gap 8 – 12 23 BUN 10 – 20 35 Creatinine . 6 – 1. 2 2. 5 Glucose 60 -110 205 Albumin 3. 5 - 5 2. 0 Lactate . 5 - 2 7. 28 Ammonia 15 - 45 96 Goal greater than 70 51 Scvo 2
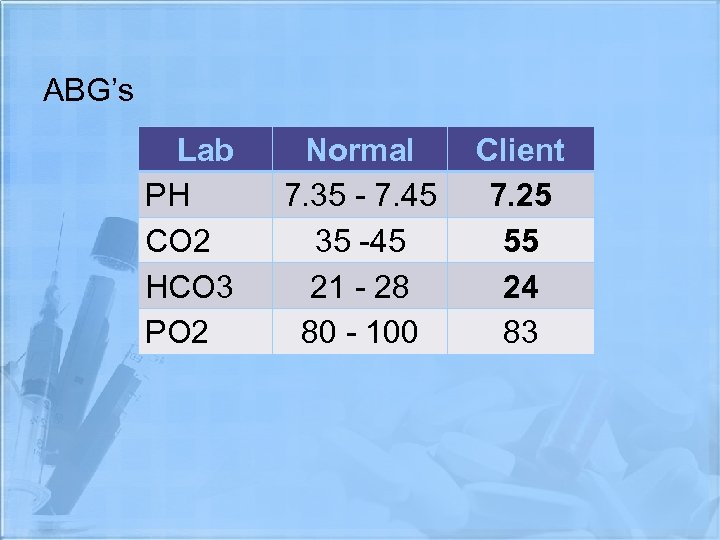 ABG’s Lab PH CO 2 HCO 3 PO 2 Normal 7. 35 - 7. 45 35 -45 21 - 28 80 - 100 Client 7. 25 55 24 83
ABG’s Lab PH CO 2 HCO 3 PO 2 Normal 7. 35 - 7. 45 35 -45 21 - 28 80 - 100 Client 7. 25 55 24 83
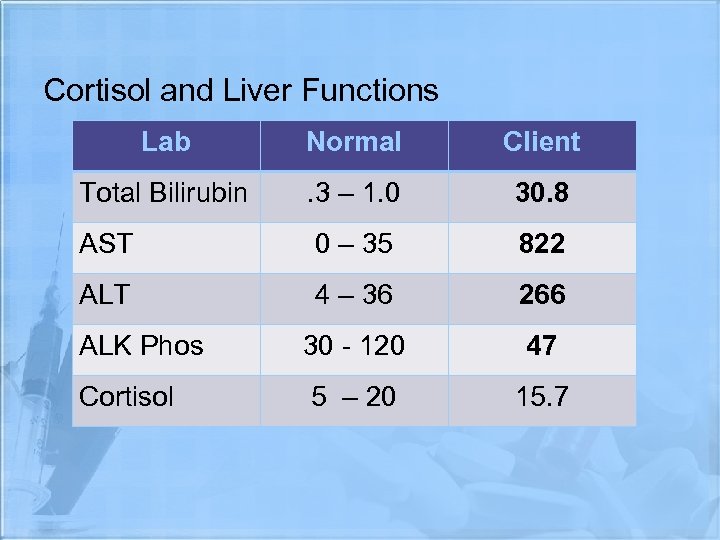 Cortisol and Liver Functions Lab Normal Client Total Bilirubin . 3 – 1. 0 30. 8 AST 0 – 35 822 ALT 4 – 36 266 30 - 120 47 5 – 20 15. 7 ALK Phos Cortisol
Cortisol and Liver Functions Lab Normal Client Total Bilirubin . 3 – 1. 0 30. 8 AST 0 – 35 822 ALT 4 – 36 266 30 - 120 47 5 – 20 15. 7 ALK Phos Cortisol
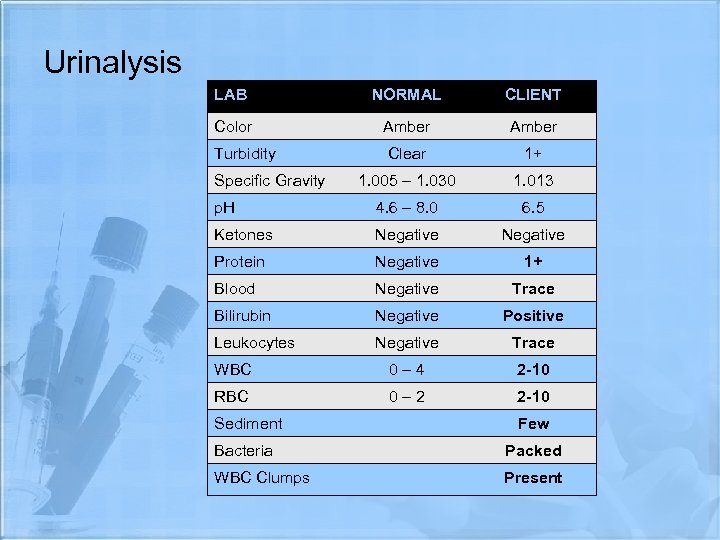 Urinalysis LAB NORMAL CLIENT Color Amber Turbidity Clear 1+ 1. 005 – 1. 030 1. 013 p. H 4. 6 – 8. 0 6. 5 Ketones Negative Protein Negative 1+ Blood Negative Trace Bilirubin Negative Positive Leukocytes Negative Trace WBC 0– 4 2 -10 RBC 0– 2 2 -10 Specific Gravity Sediment Few Bacteria Packed WBC Clumps Present
Urinalysis LAB NORMAL CLIENT Color Amber Turbidity Clear 1+ 1. 005 – 1. 030 1. 013 p. H 4. 6 – 8. 0 6. 5 Ketones Negative Protein Negative 1+ Blood Negative Trace Bilirubin Negative Positive Leukocytes Negative Trace WBC 0– 4 2 -10 RBC 0– 2 2 -10 Specific Gravity Sediment Few Bacteria Packed WBC Clumps Present
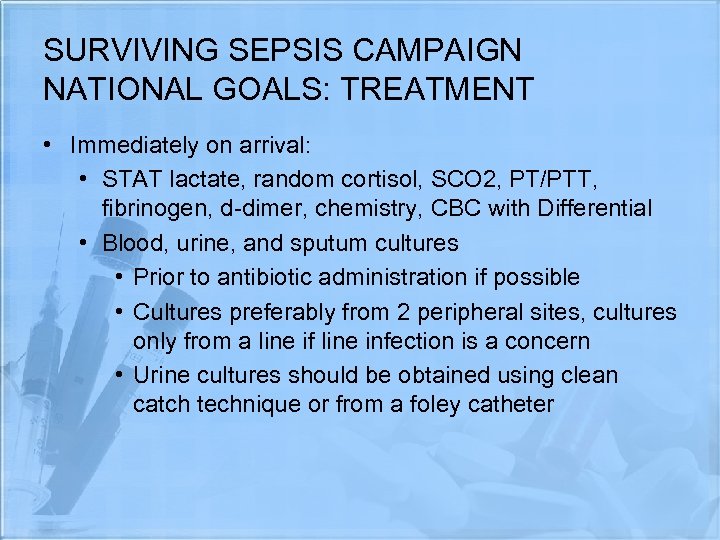 SURVIVING SEPSIS CAMPAIGN NATIONAL GOALS: TREATMENT • Immediately on arrival: • STAT lactate, random cortisol, SCO 2, PT/PTT, fibrinogen, d-dimer, chemistry, CBC with Differential • Blood, urine, and sputum cultures • Prior to antibiotic administration if possible • Cultures preferably from 2 peripheral sites, cultures only from a line if line infection is a concern • Urine cultures should be obtained using clean catch technique or from a foley catheter
SURVIVING SEPSIS CAMPAIGN NATIONAL GOALS: TREATMENT • Immediately on arrival: • STAT lactate, random cortisol, SCO 2, PT/PTT, fibrinogen, d-dimer, chemistry, CBC with Differential • Blood, urine, and sputum cultures • Prior to antibiotic administration if possible • Cultures preferably from 2 peripheral sites, cultures only from a line if line infection is a concern • Urine cultures should be obtained using clean catch technique or from a foley catheter
 SURVIVING SEPSIS CAMPAIGN NATIONAL GOALS: TREATMENT • Early Therapy • Start in ED • Focus on early recognition and TX • Studies show early, appropriate TX (within 6 hrs of ED admission) decreased 28 day mortality rates by 16% • Transfer to ICU • Start with ABC’s • Establish a patent airway (patient lethargic) • Insure proper oxygenation(sats were 85% on RA. ABG’s did not improve on NRB so patient was intubated on placed on ventilator) • Insure proper circulation
SURVIVING SEPSIS CAMPAIGN NATIONAL GOALS: TREATMENT • Early Therapy • Start in ED • Focus on early recognition and TX • Studies show early, appropriate TX (within 6 hrs of ED admission) decreased 28 day mortality rates by 16% • Transfer to ICU • Start with ABC’s • Establish a patent airway (patient lethargic) • Insure proper oxygenation(sats were 85% on RA. ABG’s did not improve on NRB so patient was intubated on placed on ventilator) • Insure proper circulation
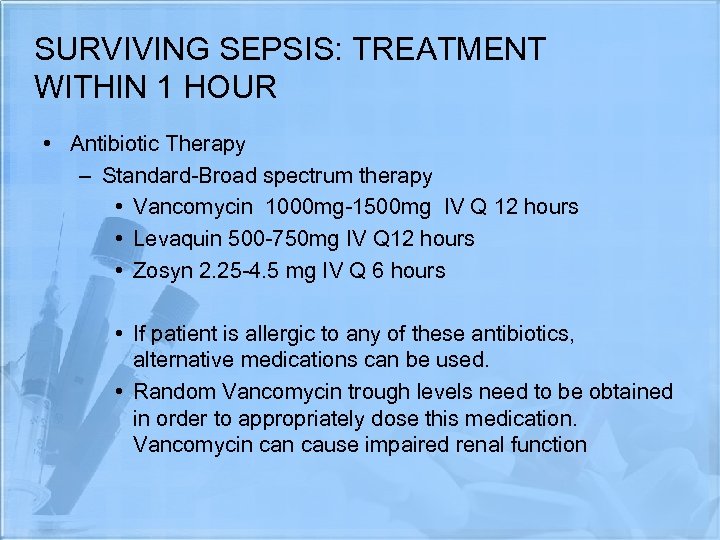 SURVIVING SEPSIS: TREATMENT WITHIN 1 HOUR • Antibiotic Therapy – Standard-Broad spectrum therapy • Vancomycin 1000 mg-1500 mg IV Q 12 hours • Levaquin 500 -750 mg IV Q 12 hours • Zosyn 2. 25 -4. 5 mg IV Q 6 hours • If patient is allergic to any of these antibiotics, alternative medications can be used. • Random Vancomycin trough levels need to be obtained in order to appropriately dose this medication. Vancomycin cause impaired renal function
SURVIVING SEPSIS: TREATMENT WITHIN 1 HOUR • Antibiotic Therapy – Standard-Broad spectrum therapy • Vancomycin 1000 mg-1500 mg IV Q 12 hours • Levaquin 500 -750 mg IV Q 12 hours • Zosyn 2. 25 -4. 5 mg IV Q 6 hours • If patient is allergic to any of these antibiotics, alternative medications can be used. • Random Vancomycin trough levels need to be obtained in order to appropriately dose this medication. Vancomycin cause impaired renal function
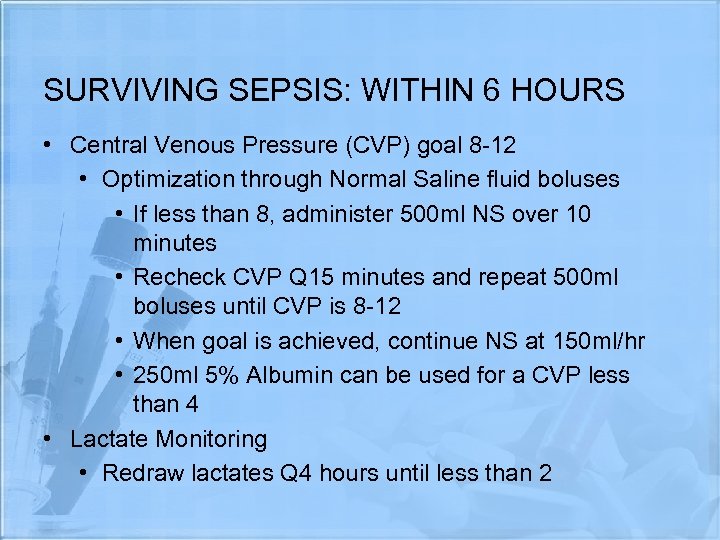 SURVIVING SEPSIS: WITHIN 6 HOURS • Central Venous Pressure (CVP) goal 8 -12 • Optimization through Normal Saline fluid boluses • If less than 8, administer 500 ml NS over 10 minutes • Recheck CVP Q 15 minutes and repeat 500 ml boluses until CVP is 8 -12 • When goal is achieved, continue NS at 150 ml/hr • 250 ml 5% Albumin can be used for a CVP less than 4 • Lactate Monitoring • Redraw lactates Q 4 hours until less than 2
SURVIVING SEPSIS: WITHIN 6 HOURS • Central Venous Pressure (CVP) goal 8 -12 • Optimization through Normal Saline fluid boluses • If less than 8, administer 500 ml NS over 10 minutes • Recheck CVP Q 15 minutes and repeat 500 ml boluses until CVP is 8 -12 • When goal is achieved, continue NS at 150 ml/hr • 250 ml 5% Albumin can be used for a CVP less than 4 • Lactate Monitoring • Redraw lactates Q 4 hours until less than 2
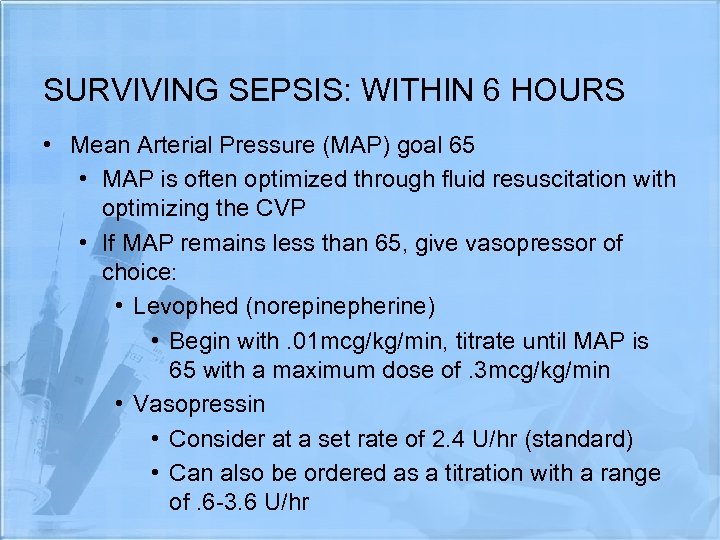 SURVIVING SEPSIS: WITHIN 6 HOURS • Mean Arterial Pressure (MAP) goal 65 • MAP is often optimized through fluid resuscitation with optimizing the CVP • If MAP remains less than 65, give vasopressor of choice: • Levophed (norepinepherine) • Begin with. 01 mcg/kg/min, titrate until MAP is 65 with a maximum dose of. 3 mcg/kg/min • Vasopressin • Consider at a set rate of 2. 4 U/hr (standard) • Can also be ordered as a titration with a range of. 6 -3. 6 U/hr
SURVIVING SEPSIS: WITHIN 6 HOURS • Mean Arterial Pressure (MAP) goal 65 • MAP is often optimized through fluid resuscitation with optimizing the CVP • If MAP remains less than 65, give vasopressor of choice: • Levophed (norepinepherine) • Begin with. 01 mcg/kg/min, titrate until MAP is 65 with a maximum dose of. 3 mcg/kg/min • Vasopressin • Consider at a set rate of 2. 4 U/hr (standard) • Can also be ordered as a titration with a range of. 6 -3. 6 U/hr
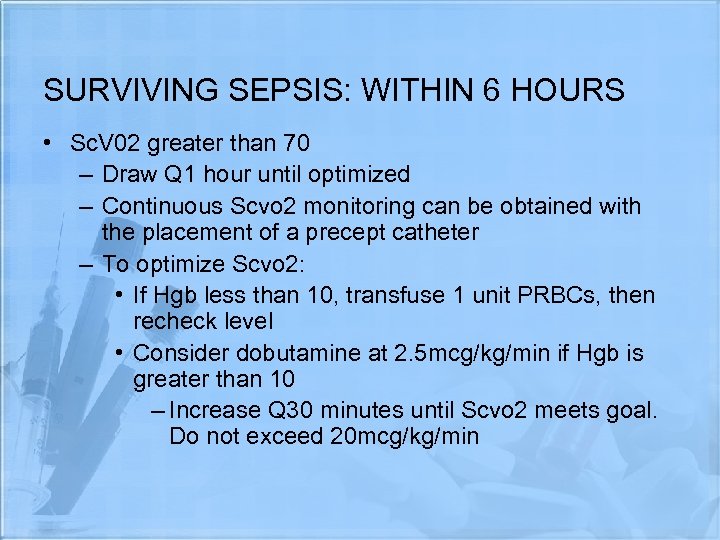 SURVIVING SEPSIS: WITHIN 6 HOURS • Sc. V 02 greater than 70 – Draw Q 1 hour until optimized – Continuous Scvo 2 monitoring can be obtained with the placement of a precept catheter – To optimize Scvo 2: • If Hgb less than 10, transfuse 1 unit PRBCs, then recheck level • Consider dobutamine at 2. 5 mcg/kg/min if Hgb is greater than 10 – Increase Q 30 minutes until Scvo 2 meets goal. Do not exceed 20 mcg/kg/min
SURVIVING SEPSIS: WITHIN 6 HOURS • Sc. V 02 greater than 70 – Draw Q 1 hour until optimized – Continuous Scvo 2 monitoring can be obtained with the placement of a precept catheter – To optimize Scvo 2: • If Hgb less than 10, transfuse 1 unit PRBCs, then recheck level • Consider dobutamine at 2. 5 mcg/kg/min if Hgb is greater than 10 – Increase Q 30 minutes until Scvo 2 meets goal. Do not exceed 20 mcg/kg/min
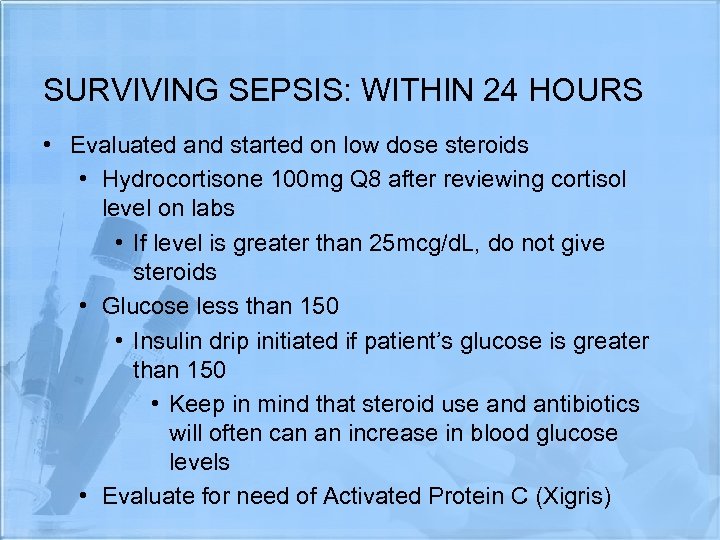 SURVIVING SEPSIS: WITHIN 24 HOURS • Evaluated and started on low dose steroids • Hydrocortisone 100 mg Q 8 after reviewing cortisol level on labs • If level is greater than 25 mcg/d. L, do not give steroids • Glucose less than 150 • Insulin drip initiated if patient’s glucose is greater than 150 • Keep in mind that steroid use and antibiotics will often can an increase in blood glucose levels • Evaluate for need of Activated Protein C (Xigris)
SURVIVING SEPSIS: WITHIN 24 HOURS • Evaluated and started on low dose steroids • Hydrocortisone 100 mg Q 8 after reviewing cortisol level on labs • If level is greater than 25 mcg/d. L, do not give steroids • Glucose less than 150 • Insulin drip initiated if patient’s glucose is greater than 150 • Keep in mind that steroid use and antibiotics will often can an increase in blood glucose levels • Evaluate for need of Activated Protein C (Xigris)
 Treatment • Activated Protein C (Xigris) • • • Steroids • Antibiotics Costly • Remove sources of Decreased mortality infection by 20% • Glycemic Control FDA approved Early administration • Active cooling • Renal function Risk of increased bleeding (consider CRRT if needed)
Treatment • Activated Protein C (Xigris) • • • Steroids • Antibiotics Costly • Remove sources of Decreased mortality infection by 20% • Glycemic Control FDA approved Early administration • Active cooling • Renal function Risk of increased bleeding (consider CRRT if needed)
 Treatment • WASH YOUR HANDS • Strict aseptic/sterile techniques • Safety • BSI • Frequent position changes • Inspect oral cavity QD • Support/Educate Pt and family
Treatment • WASH YOUR HANDS • Strict aseptic/sterile techniques • Safety • BSI • Frequent position changes • Inspect oral cavity QD • Support/Educate Pt and family
 References Ø Porth C. , Matfin G. (2009). Pathophysiology: Concepts of Altered Health States. Philadelphia, PA. Lipppincott Williams & Wilkins. Ø Merck Manual Online. (2010). Retrieved December 4, 2010, from http: //www. merckmanuals. com Ø Harkins M. D. , M. (n. d. ). ACP Online. Retrieved December 4 th, 2010, from http: //www. acponline. org/about_acp/chapters/nm/harkins/ppt Ø The University of Kansas Adult Severe Sepsis/Septic Shock Order Set Dellinger, R. P. , Levy, M. M. , Carlet, J. M. , Bion, J. , Parker, M. M. , Jaeschke, R. , Vincent, J. L. (2008). Surviving sepsis campaign: International guidelines for management of severe sepsis and septic shock: 2008. Intensive Care Ø Medicine, 34, 17 -60. Ø Institute for Healthcare Improvement. (2010). First steps and measures to reduce sepsis mortality. Retrieved from www. ihi. org/IHI/Topics/Critical. Care/Sepsis/Improvement. Stories/First. Stepsan d. Measures. org Ø Institute for Health Care Improvement. (2010). Sepsis. Retrieved from www. ihi. org/Topics/Criticalcare/sepsis
References Ø Porth C. , Matfin G. (2009). Pathophysiology: Concepts of Altered Health States. Philadelphia, PA. Lipppincott Williams & Wilkins. Ø Merck Manual Online. (2010). Retrieved December 4, 2010, from http: //www. merckmanuals. com Ø Harkins M. D. , M. (n. d. ). ACP Online. Retrieved December 4 th, 2010, from http: //www. acponline. org/about_acp/chapters/nm/harkins/ppt Ø The University of Kansas Adult Severe Sepsis/Septic Shock Order Set Dellinger, R. P. , Levy, M. M. , Carlet, J. M. , Bion, J. , Parker, M. M. , Jaeschke, R. , Vincent, J. L. (2008). Surviving sepsis campaign: International guidelines for management of severe sepsis and septic shock: 2008. Intensive Care Ø Medicine, 34, 17 -60. Ø Institute for Healthcare Improvement. (2010). First steps and measures to reduce sepsis mortality. Retrieved from www. ihi. org/IHI/Topics/Critical. Care/Sepsis/Improvement. Stories/First. Stepsan d. Measures. org Ø Institute for Health Care Improvement. (2010). Sepsis. Retrieved from www. ihi. org/Topics/Criticalcare/sepsis
 THANK YOU!!! QUESTIONS? ? ?
THANK YOU!!! QUESTIONS? ? ?


