11e59d8dd9aa4ed4f3fc772ed64a43f8.ppt
- Количество слайдов: 26
CASE STUDY IN SYSTEMS FAILURE Ethan Cumbler M. D. Assistant Professor of Medicine Hospitalist Section University of Colorado Hospital 2007 Case represents an example based on real case. Some details have been changed and case de-identified to preserve patient confidentiality
Case-Background Ø 78 y/o with multiple comorbidities including afib, DM II, CHF and CAD Ø Pt was taken off warfarin 2 months before admission due to falls. Ø Underwent gallbladder removal for symptomatic gallstones one month PTA. Ø Two days PTA left lower extremity swelling begins. Pt c/o pain from left knee to groin.
What Diagnosis Do You Suspect?
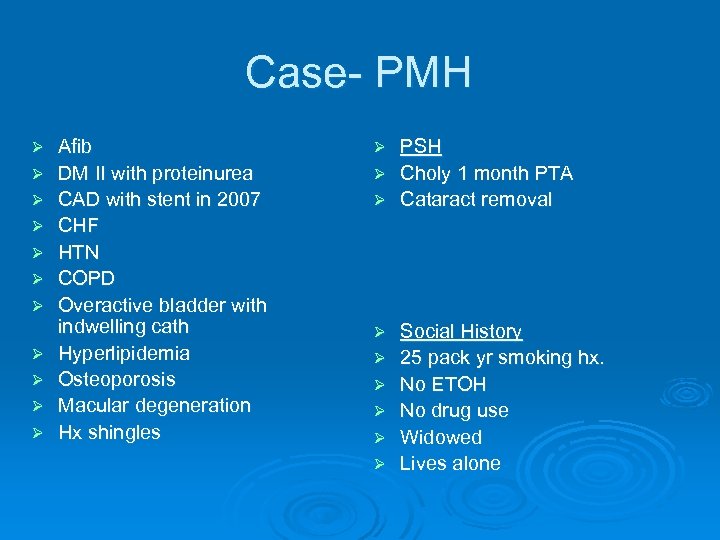
Case- PMH Ø Ø Ø Afib DM II with proteinurea CAD with stent in 2007 CHF HTN COPD Overactive bladder with indwelling cath Hyperlipidemia Osteoporosis Macular degeneration Hx shingles PSH Ø Choly 1 month PTA Ø Cataract removal Ø Ø Ø Ø Social History 25 pack yr smoking hx. No ETOH No drug use Widowed Lives alone
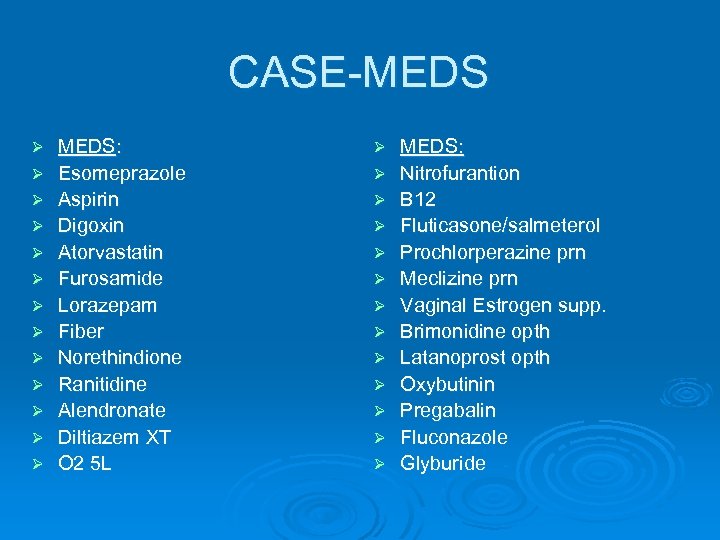
CASE-MEDS Ø Ø Ø Ø MEDS: Esomeprazole Aspirin Digoxin Atorvastatin Furosamide Lorazepam Fiber Norethindione Ranitidine Alendronate Diltiazem XT O 2 5 L Ø Ø Ø Ø MEDS: Nitrofurantion B 12 Fluticasone/salmeterol Prochlorperazine prn Meclizine prn Vaginal Estrogen supp. Brimonidine opth Latanoprost opth Oxybutinin Pregabalin Fluconazole Glyburide
What About This Case Already Creates Higher Than Average Risk for Adverse Events and Medical Error?
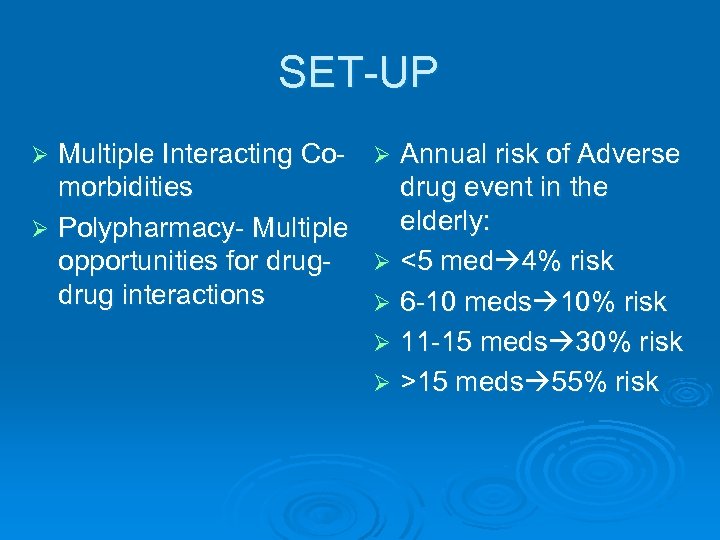
SET-UP Multiple Interacting Co- Ø Annual risk of Adverse morbidities drug event in the elderly: Ø Polypharmacy- Multiple opportunities for drug- Ø <5 med 4% risk drug interactions Ø 6 -10 meds 10% risk Ø 11 -15 meds 30% risk Ø >15 meds 55% risk Ø
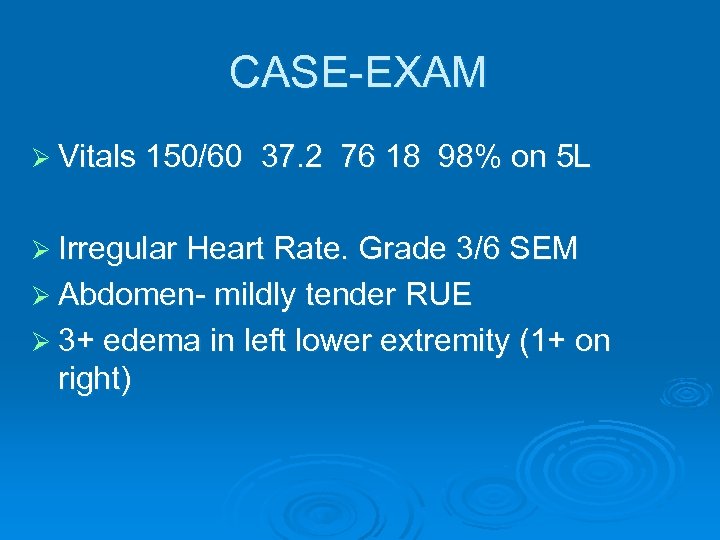
CASE-EXAM Ø Vitals 150/60 37. 2 76 18 98% on 5 L Ø Irregular Heart Rate. Grade 3/6 SEM Ø Abdomen- mildly tender RUE Ø 3+ edema in left lower extremity (1+ on right)
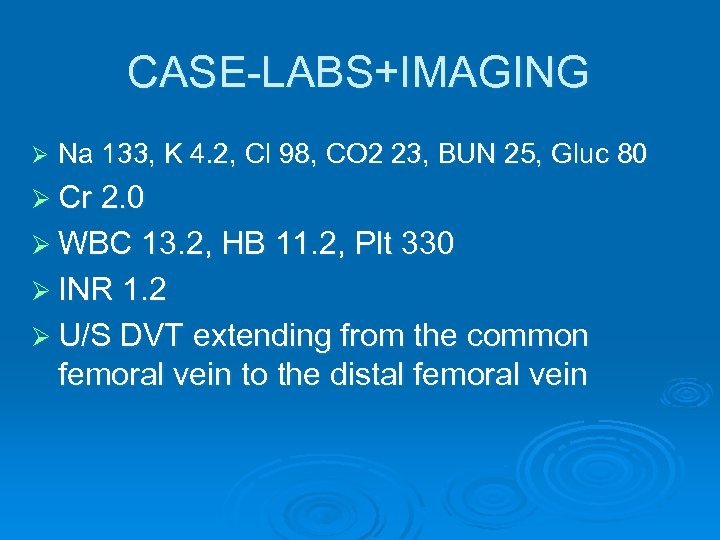
CASE-LABS+IMAGING Ø Na 133, K 4. 2, Cl 98, CO 2 23, BUN 25, Gluc 80 Ø Cr 2. 0 Ø WBC 13. 2, HB 11. 2, Plt 330 Ø INR 1. 2 Ø U/S DVT extending from the common femoral vein to the distal femoral vein
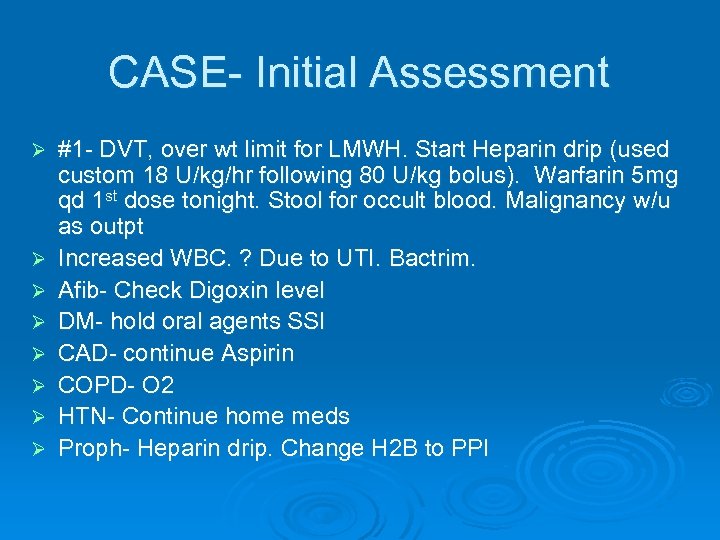
CASE- Initial Assessment Ø Ø Ø Ø #1 - DVT, over wt limit for LMWH. Start Heparin drip (used custom 18 U/kg/hr following 80 U/kg bolus). Warfarin 5 mg qd 1 st dose tonight. Stool for occult blood. Malignancy w/u as outpt Increased WBC. ? Due to UTI. Bactrim. Afib- Check Digoxin level DM- hold oral agents SSI CAD- continue Aspirin COPD- O 2 HTN- Continue home meds Proph- Heparin drip. Change H 2 B to PPI
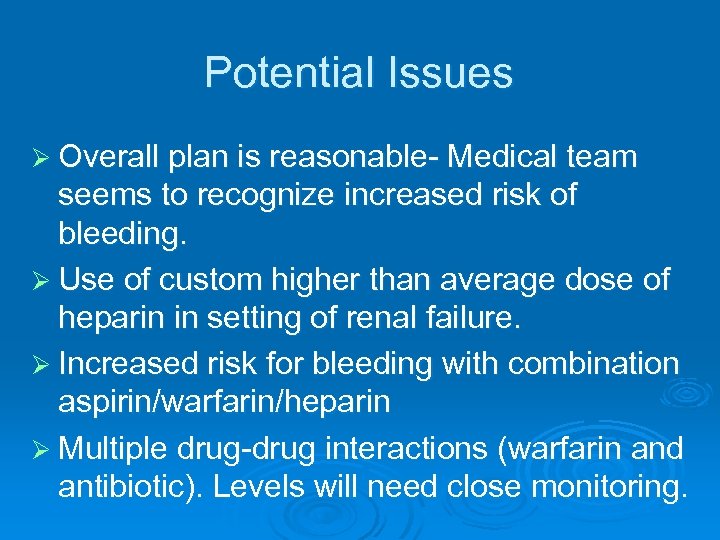
Potential Issues Ø Overall plan is reasonable- Medical team seems to recognize increased risk of bleeding. Ø Use of custom higher than average dose of heparin in setting of renal failure. Ø Increased risk for bleeding with combination aspirin/warfarin/heparin Ø Multiple drug-drug interactions (warfarin and antibiotic). Levels will need close monitoring.
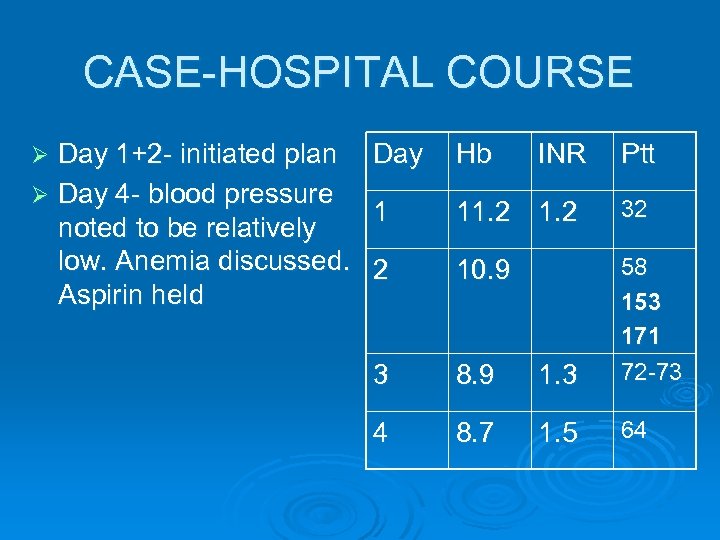
CASE-HOSPITAL COURSE Day 1+2 - initiated plan Ø Day 4 - blood pressure noted to be relatively low. Anemia discussed. Aspirin held Ø Day Hb INR Ptt 1 11. 2 32 2 10. 9 3 8. 9 1. 3 58 153 171 72 -73 4 8. 7 1. 5 64
CASE-HOSPITAL COURSE Ø Day 5 - Hb drops to 7. 8. Ø Assessment notes drop in Hb. Attributes to likely acute/subacute bleed. CT abdomen ordered Ø (Note later in day comments on CT finding of rectus sheath hematoma)
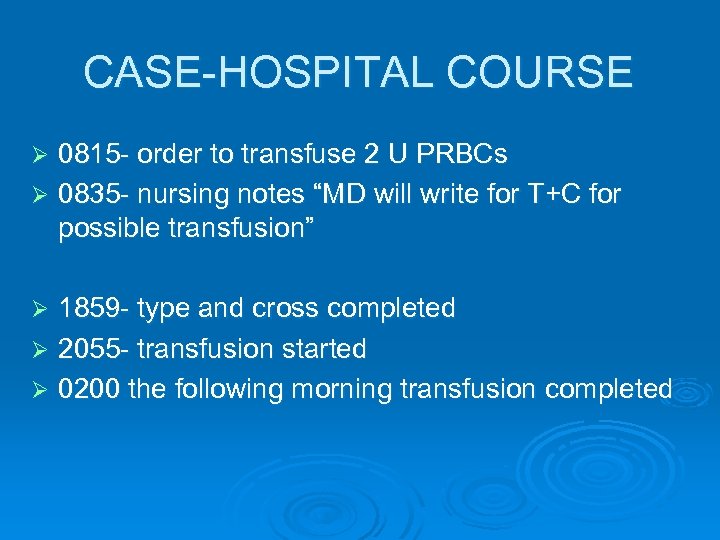
CASE-HOSPITAL COURSE 0815 - order to transfuse 2 U PRBCs Ø 0835 - nursing notes “MD will write for T+C for possible transfusion” Ø 1859 - type and cross completed Ø 2055 - transfusion started Ø 0200 the following morning transfusion completed Ø
Analysis of Case Ø Use (Systematic Analysis of a Medical Error form to guide discussion)
Step 1 Adverse event, Medical error, Causation Ø Ø Ø Was there an adverse event? Yes- the bleed represented an adverse drug event. Was there a medical error? Yes- 17 hour 45 min delay between ordering a transfusion and the completion of the transfusion Significant delay in transfusion represents a delay between intent and outcome (Remember that the definition of medical error does not require harm to occur) Did the medical error cause the adverse event- No. In this case there is an adverse drug event but the medical error occurred during the treatment of the adverse event and was not a causal factor.
Step 2 Did system errors contribute to medical error? Which types? Ø Type and Cross blood sample was lost Ø No feedback mechanism to trigger investigation when blood did not arrive Ø This error represents both problems with information management and with communication Ø To determine exactly what in the system failed, a more detailed process map was required.
Failure Analysis Ø Process Mapping l l Between Order and Transfusion > 20 nodes Where did things go wrong? • Failure at Nodes l l Tech drawing multiple blood samples before sending Blood sent by tube system to wrong location by nurse • Lack of Nodes l No feedback mechanism, when blood has not arrived • Lack of Communication l Pt sent for CT Scan before type and cross drawn
Step 3 List Individual Errors + Type Individual error included nurse sending type and cross to wrong location via intra-hospital tube system Ø This represented a Skill-based Error on the part of the nurse who accidentally sent the blood to the wrong location. Ø Looking back there was probably also opportunity for earlier recognition of the adverse drug event (bleeding) by the physicians with the drop in blood counts on day #3 Ø
Step 4 List Heuristic Failures Leading to Individual Judgment Error Ø None related directly to the medical error which was the delay between ordering the transfusion and the blood being transfused
Step 5 What Level Harm Occurred As a Result of The Adverse Event? Ø Rectus sheath bleed in patient on heparin/coumadin/and aspirin is an adverse drug event Ø Harm occurred- major temporary harm Ø The adverse event was probably not directly related to the medical error in this case. Ø No evidence that harm was worsened by delay in transfusion
Step 6 What Would You Disclose? In a case such as this where the process has broken down but no harm is occurring it is appropriate to keep the patient informed that the transfusion is still planned but has been delayed by difficulty processing the blood. Ø A simple apology for the delay is usually sufficient when no harm is occurring. Ø A commitment to keep the patient updated is important. Ø
Step 7 What Could Be Done To Prevent This In The Future?
What Could Be Done To Prevent This In The Future? Involve risk management to assist in creating new feedback nodes between the floor nurses and the laboratory. Ø This involves change in system of care and requires multi-disciplinary approach to creating a solution Ø Follow-up by physician to assure that ordered events are occurring (active step which is significantly less reliable then the system solution described above) Ø
References 1. 2. 3. 4. 5. Pierluissi E, Fischer MA, Campbell AR, Landefeld CS. Discussion of Medical Errors in Morbidity and Mortality Conferences. JAMA 2003; 290: 2838 -2842 C. K. Hofling et al. An Experimental Study in Nurse-Physician Relationships. Journal of Nervous and Mental Disease 143; 1966: 171 -80 (as quoted in The Lucifer Effect. Understanding how Good People turn Evil. Philip Zimbardo Random House New York 2007) Blumenthal D, Ferris TG. Safety in the Academic Medical Center: Transforming Challenges Into Ingredients For Improvement. Academic Medicine 2006; 81: 817 -822 Murayama KM, Derossis AM, Da. Rosa DA, Sherman HB, Fryer JP. A Critical Evaluation of the Morbidity and Mortality Conference. Am J Surg 2002; 183: 246 -250 Spencer FC. Human Error in Hospitals and Industrial Accidents: Current Concepts. J Am Coll Surg 2000: 191: 410 -418
References 6. 7. 8. 9. Buetow S, Elwyn G. Patient Safety and Patient Error. Lancet 2007; 369: 158 -161 Jagsi R, Kitch BT, Weinstein DF, Campbell EG, Hutter M, Weissman JS. Residents Report on Adverse Events and Their Causes. Arch Intern Med 2005; 165: 2607 -2613 Patient Safety: Past, Present, and Future. Clinical Orthopaedics and Related Research 2005; 440: P 242 -250 James Reason. Human Error. Cambridge University Press. Cambridge. 1990
11e59d8dd9aa4ed4f3fc772ed64a43f8.ppt