fa5d1951b0beca6adf9dd46835846a84.ppt
- Количество слайдов: 30

 CASE HISTORY NAME : Age : Sex : Marital Status: Occupation : MARJINA BEGUM About 25 year Female Married House wife.
CASE HISTORY NAME : Age : Sex : Marital Status: Occupation : MARJINA BEGUM About 25 year Female Married House wife.
 Address : Vill : Kujghar, Post : Kujghar, P. S. : Sadar, Dist : Jamalpur. Date of Admission: 08 -11 -2005 Date of Examination: 09 -11 -2005
Address : Vill : Kujghar, Post : Kujghar, P. S. : Sadar, Dist : Jamalpur. Date of Admission: 08 -11 -2005 Date of Examination: 09 -11 -2005
 CHIEF COMPLAINTS Diffuse painful blisters & crusted lesions over scalp, face, trunk, upper extrimities & groin. For about 1½ month. A few small blisters in mouth cavity For 7 days.
CHIEF COMPLAINTS Diffuse painful blisters & crusted lesions over scalp, face, trunk, upper extrimities & groin. For about 1½ month. A few small blisters in mouth cavity For 7 days.
 H/O PRESENT ILLNESS The patient states that she was all right about six months back. Then she developed a few blisters with itching at lower part of back of Lt painful blisters
H/O PRESENT ILLNESS The patient states that she was all right about six months back. Then she developed a few blisters with itching at lower part of back of Lt painful blisters
 side. Subsequently after 4 months she developed various sizedassociated with itching at her chest, back, upper extrimities, scalp, face, groin & a few painful lesions is oral mucous membrane which became crusted,
side. Subsequently after 4 months she developed various sizedassociated with itching at her chest, back, upper extrimities, scalp, face, groin & a few painful lesions is oral mucous membrane which became crusted,
 With above complaints she was admitted in College Hospital Mymensingh for Medical proper management. exfoliative, reddened with moist surface
With above complaints she was admitted in College Hospital Mymensingh for Medical proper management. exfoliative, reddened with moist surface
 H/O PAST ILLNESS. Nothing contributory. Personal History: Married for 4 years. No issue. Menstruation : Regular. Habit chewing of battle nut +
H/O PAST ILLNESS. Nothing contributory. Personal History: Married for 4 years. No issue. Menstruation : Regular. Habit chewing of battle nut +
 Family History: No any of her family members suffered from any such notable disease.
Family History: No any of her family members suffered from any such notable disease.
 Treatment History: Patient was admitted with complaint mentioned in MMCH on 20 -10 -2005 & was treated with long acting steroid triamcinolone acetonide parenterally & was improved.
Treatment History: Patient was admitted with complaint mentioned in MMCH on 20 -10 -2005 & was treated with long acting steroid triamcinolone acetonide parenterally & was improved.
 GENERAL EXAMINATION. Appearance : Body build : Anaemia Jaundice Cyanosis Ill looking. Average. Absent.
GENERAL EXAMINATION. Appearance : Body build : Anaemia Jaundice Cyanosis Ill looking. Average. Absent.
 Oedema Dehydration Clubbing Koilonychia Hair Nail Absent Normal
Oedema Dehydration Clubbing Koilonychia Hair Nail Absent Normal
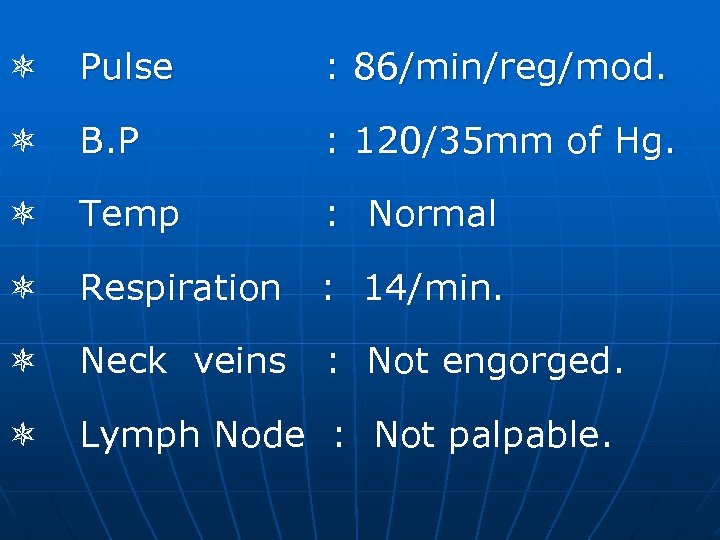 Pulse : 86/min/reg/mod. B. P : 120/35 mm of Hg. Temp : Normal Respiration : 14/min. Neck veins : Not engorged. Lymph Node : Not palpable.
Pulse : 86/min/reg/mod. B. P : 120/35 mm of Hg. Temp : Normal Respiration : 14/min. Neck veins : Not engorged. Lymph Node : Not palpable.
 EXAMINATION OF INTEGUMENTARY SYSTEM. Inspection Vesicles & bulla on scalp, face, chest, back, upper extrimities, groin, some on normal skin & some are erythomatous based.
EXAMINATION OF INTEGUMENTARY SYSTEM. Inspection Vesicles & bulla on scalp, face, chest, back, upper extrimities, groin, some on normal skin & some are erythomatous based.

 Palpation : Vesicles & bullae are flacid, tenderness present NIKOLSKY Sign Present. Bulla – spread plenomenon (The Asboe. Hansen sign) – Present.
Palpation : Vesicles & bullae are flacid, tenderness present NIKOLSKY Sign Present. Bulla – spread plenomenon (The Asboe. Hansen sign) – Present.
 EXAMINATION OF OTHER SYSTEM : NAD lesions. except a few oral mucosal
EXAMINATION OF OTHER SYSTEM : NAD lesions. except a few oral mucosal
 SALIENT FEATURES. Marjina Begum, Age about 25 years of vill Kujghar, Jamalpur was admitted in MMCH on 08 -11 -05 with complaints of progressive development of painful blisters. Crust, erosions & exfoliative lesions associated with itching
SALIENT FEATURES. Marjina Begum, Age about 25 years of vill Kujghar, Jamalpur was admitted in MMCH on 08 -11 -05 with complaints of progressive development of painful blisters. Crust, erosions & exfoliative lesions associated with itching
 over scalp, face, trunk, upper arms, groin & a few small painful blisters in oral cavity. Examination shows flaccid & vesicles, Bullae, crusted & exfoliative lesions with erythomatous base at the mentioned sites. The lesions are
over scalp, face, trunk, upper arms, groin & a few small painful blisters in oral cavity. Examination shows flaccid & vesicles, Bullae, crusted & exfoliative lesions with erythomatous base at the mentioned sites. The lesions are
 tender, moist with malodourous condition & a few superficial erosions in oral mucous membrane. Nikolsky sign – Present Bulla – Spread Phenomenon – Present.
tender, moist with malodourous condition & a few superficial erosions in oral mucous membrane. Nikolsky sign – Present Bulla – Spread Phenomenon – Present.
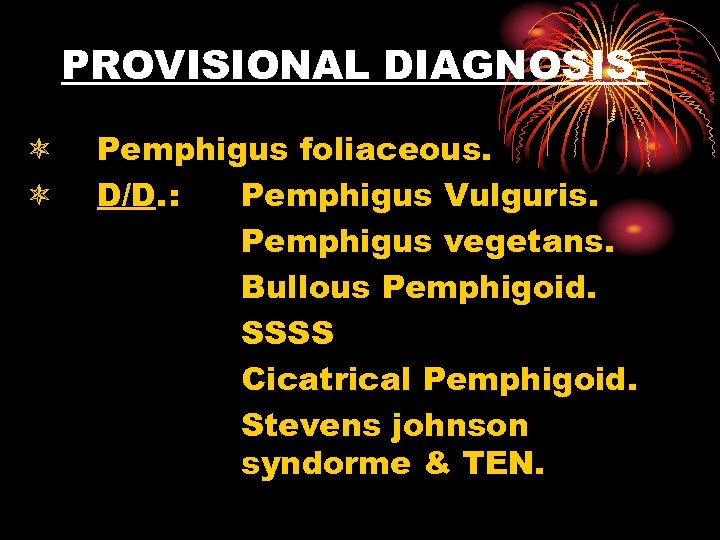 PROVISIONAL DIAGNOSIS. Pemphigus foliaceous. D/D. : Pemphigus Vulguris. Pemphigus vegetans. Bullous Pemphigoid. SSSS Cicatrical Pemphigoid. Stevens johnson syndorme & TEN.
PROVISIONAL DIAGNOSIS. Pemphigus foliaceous. D/D. : Pemphigus Vulguris. Pemphigus vegetans. Bullous Pemphigoid. SSSS Cicatrical Pemphigoid. Stevens johnson syndorme & TEN.
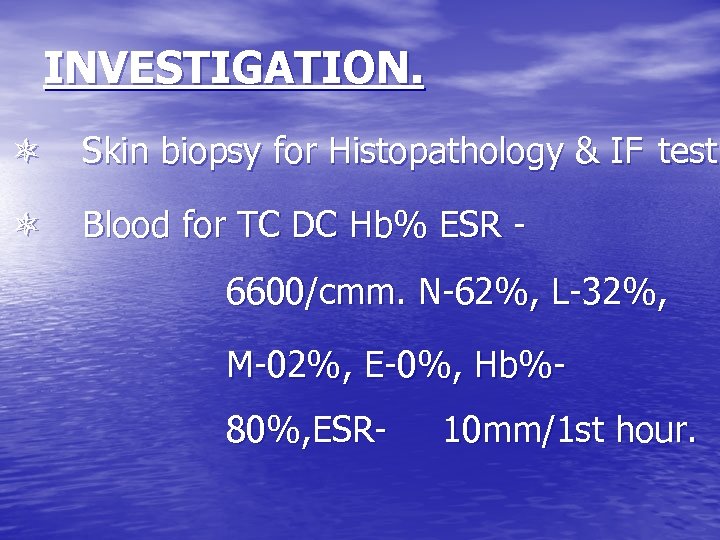 INVESTIGATION. Skin biopsy for Histopathology & IF test. Blood for TC DC Hb% ESR 6600/cmm. N-62%, L-32%, M-02%, E-0%, Hb%80%, ESR- 10 mm/1 st hour.
INVESTIGATION. Skin biopsy for Histopathology & IF test. Blood for TC DC Hb% ESR 6600/cmm. N-62%, L-32%, M-02%, E-0%, Hb%80%, ESR- 10 mm/1 st hour.
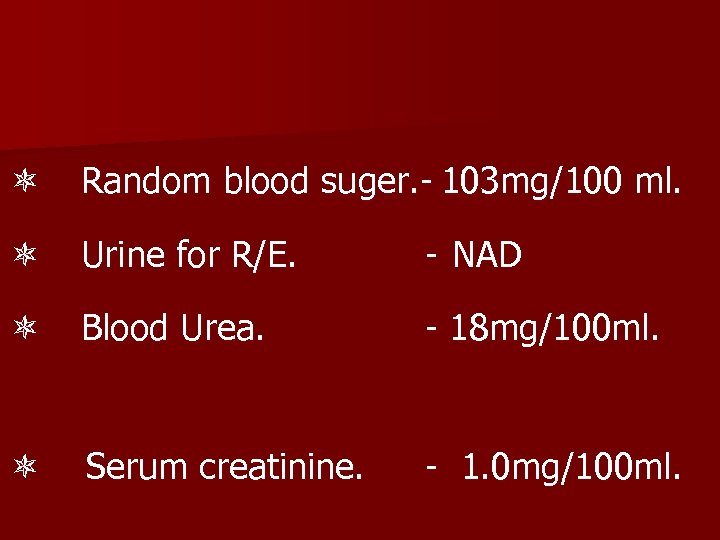 Random blood suger. - 103 mg/100 ml. Urine for R/E. - NAD Blood Urea. - 18 mg/100 ml. Serum creatinine. - 1. 0 mg/100 ml.
Random blood suger. - 103 mg/100 ml. Urine for R/E. - NAD Blood Urea. - 18 mg/100 ml. Serum creatinine. - 1. 0 mg/100 ml.
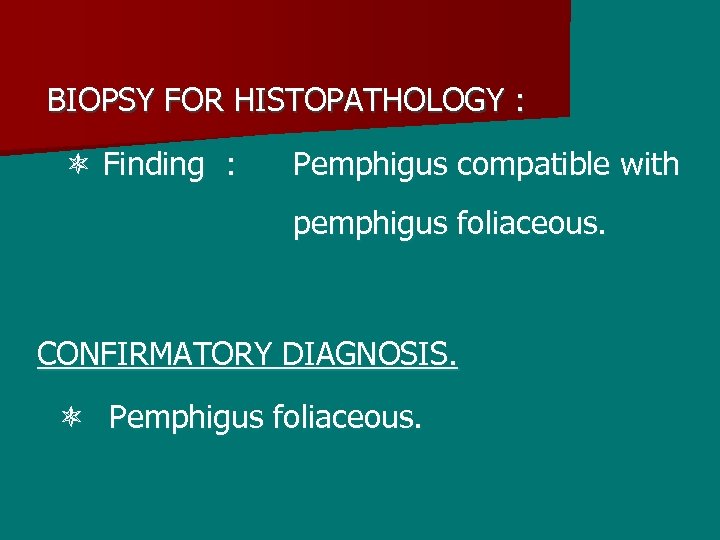 BIOPSY FOR HISTOPATHOLOGY : Finding : Pemphigus compatible with pemphigus foliaceous. CONFIRMATORY DIAGNOSIS. Pemphigus foliaceous.
BIOPSY FOR HISTOPATHOLOGY : Finding : Pemphigus compatible with pemphigus foliaceous. CONFIRMATORY DIAGNOSIS. Pemphigus foliaceous.
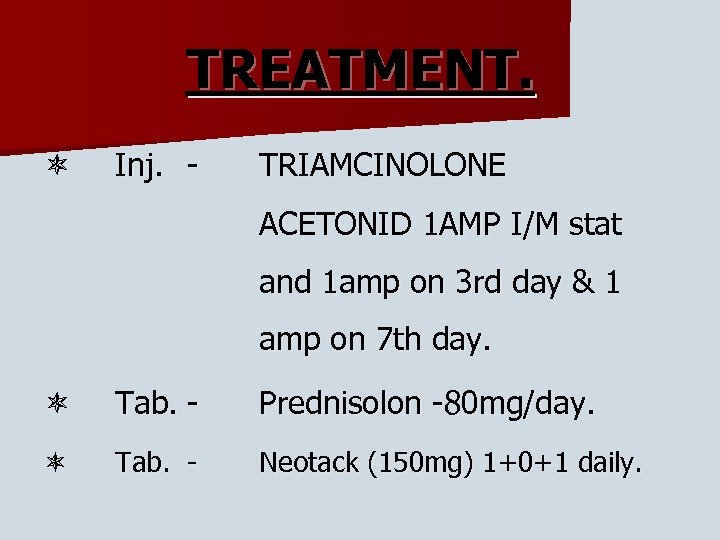 TREATMENT. Inj. - TRIAMCINOLONE ACETONID 1 AMP I/M stat and 1 amp on 3 rd day & 1 amp on 7 th day. Tab. - Prednisolon -80 mg/day. Tab. - Neotack (150 mg) 1+0+1 daily.
TREATMENT. Inj. - TRIAMCINOLONE ACETONID 1 AMP I/M stat and 1 amp on 3 rd day & 1 amp on 7 th day. Tab. - Prednisolon -80 mg/day. Tab. - Neotack (150 mg) 1+0+1 daily.
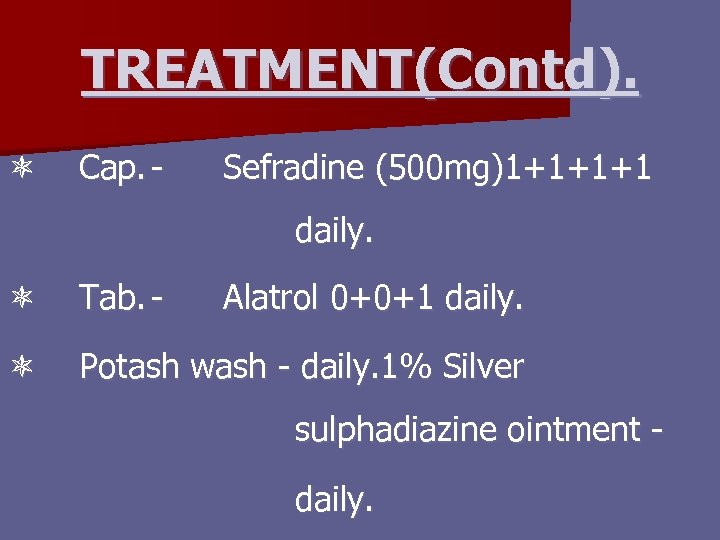 TREATMENT(Contd). Cap. - Sefradine (500 mg)1+1+1+1 daily. Tab. - Alatrol 0+0+1 daily. Potash wash - daily. 1% Silver sulphadiazine ointment daily.
TREATMENT(Contd). Cap. - Sefradine (500 mg)1+1+1+1 daily. Tab. - Alatrol 0+0+1 daily. Potash wash - daily. 1% Silver sulphadiazine ointment daily.
 SALIENT FEATURE. Mr. Sumon Das, son of Dr. Kanu Das, aged 29 years hailing form Jamalpur was admitted in MMCH, Cabin-7 on 28 th November, 2005. He was referred to skin & VD OPD on 30 th Nov. 05 with the complaints of exfoliation of
SALIENT FEATURE. Mr. Sumon Das, son of Dr. Kanu Das, aged 29 years hailing form Jamalpur was admitted in MMCH, Cabin-7 on 28 th November, 2005. He was referred to skin & VD OPD on 30 th Nov. 05 with the complaints of exfoliation of
 skin with generalized mild itching for 20 days, a known case of hypothyroidism due to thyroidectomy 3 months back & bronchial asthma from childhood. On examination we found extensive scaling all over the skin with erythema
skin with generalized mild itching for 20 days, a known case of hypothyroidism due to thyroidectomy 3 months back & bronchial asthma from childhood. On examination we found extensive scaling all over the skin with erythema
 and itching, mild leg oedema & puffy face. Pt’s pulse was 96/min, BP= 120/65 mm of Hg, temp. = 101. 40 F, lungs, heart & urinary output – normal. There was no mucous membrane and nail changes. Pt. also complaints of
and itching, mild leg oedema & puffy face. Pt’s pulse was 96/min, BP= 120/65 mm of Hg, temp. = 101. 40 F, lungs, heart & urinary output – normal. There was no mucous membrane and nail changes. Pt. also complaints of
 chilling & gave H/O taking tab. Ibuprofen 20 days back and also paracetamol & azithromycin. With these above features our diagnosis is drug induced exfoliative dermatitis.
chilling & gave H/O taking tab. Ibuprofen 20 days back and also paracetamol & azithromycin. With these above features our diagnosis is drug induced exfoliative dermatitis.


