b629c7f875e9f0310c8c62aab20d9b95.ppt
- Количество слайдов: 60
Case Based Peds in your ED My kid is seizing Ø My kid is vomiting Ø My kid is having trouble breathing Ø My baby stopped breathing Ø 20 cases over the next 90 minutes Ø Audience participation is requested Ø
Case Based Peds in your ED My kid is seizing Ø My kid is vomiting Ø My kid is having trouble breathing Ø My baby stopped breathing Ø 20 cases over the next 90 minutes Ø Audience participation is required Ø
Managing Seizures in Pediatric Patients in your ED Frank Overly, MD Assistant Professor Emergency Medicine and Pediatrics Alpert Medical School of Brown University
Overview Ø Case based Ø Presentation of illness Ø Important questions to ask Ø Management Ø Physical findings Ø Work up Ø Summary
Pediatric Seizures Ø Most common neurologic disorder in childhood Ø 4 -6% of all kids will have 1 seizure before 16 y/o
Ø 5 year old female Case One Ø GTC seizure Ø Started 15 minutes ago Ø T-101, P-155, RR-40, BP-110/80, Ox Sat-89% Ø What would you like to do? Ø What history do you want to know?
Useful History for Seizure Ø Ø Ø Ø Does s/he have a fever? Does s/he have a seizure disorder? Ø If yes, is s/he on anti-seizure meds? Ø If yes, is s/he taking them, or any recent changes? Any trauma? Any medicines s/he had access to? How was s/he before the seizure started? Is s/he developmentally normal? Bottle or breast? Did you have a party last night?
Case One PMHx former 27 week’er Ø Has a known seizure disorder Ø On phenobarb Ø Has a fever and is seizing
Case One Getting started Ø Oxygen, NPA Ø Ask for IV access and d-stick Ø Ask to draw up Benzo (or phenobarb)
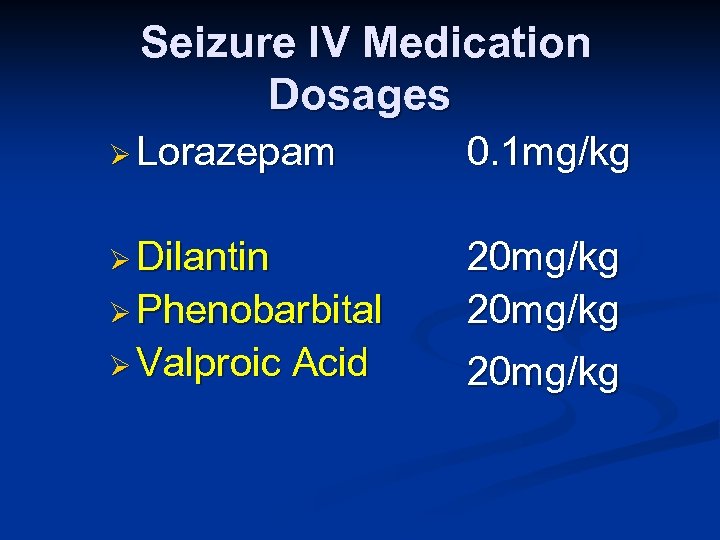
Seizure IV Medication Dosages Ø Lorazepam 0. 1 mg/kg Ø Dilantin Ø Phenobarbital 20 mg/kg Ø Valproic 20 mg/kg Acid

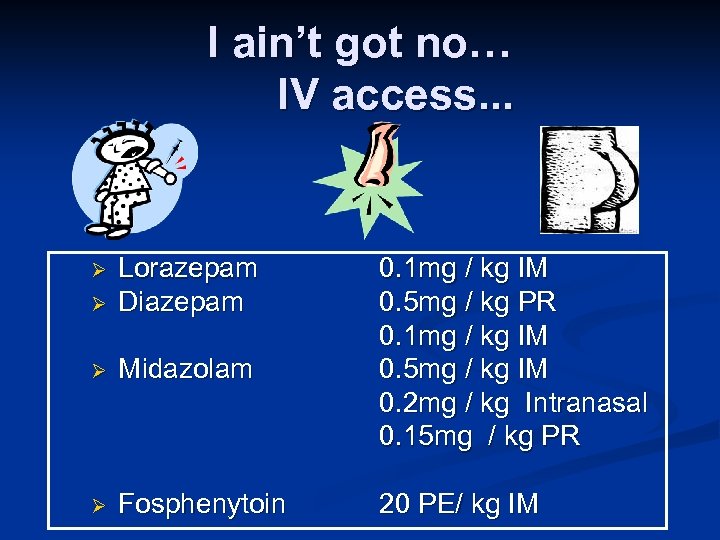
I ain’t got no… IV access. . . Ø Lorazepam Diazepam Ø Midazolam Ø Fosphenytoin Ø 0. 1 mg / kg IM 0. 5 mg / kg PR 0. 1 mg / kg IM 0. 5 mg / kg IM 0. 2 mg / kg Intranasal 0. 15 mg / kg PR 20 PE/ kg IM
Case One Ø Seizure Ø What Stops would you like to know and do?
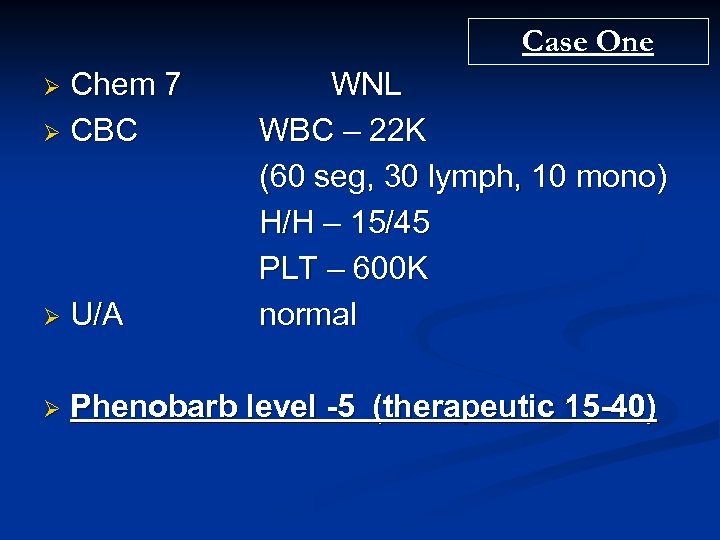
Case One Chem 7 Ø CBC Ø WNL WBC – 22 K (60 seg, 30 lymph, 10 mono) H/H – 15/45 PLT – 600 K normal Ø U/A Ø Phenobarb level -5 (therapeutic 15 -40)
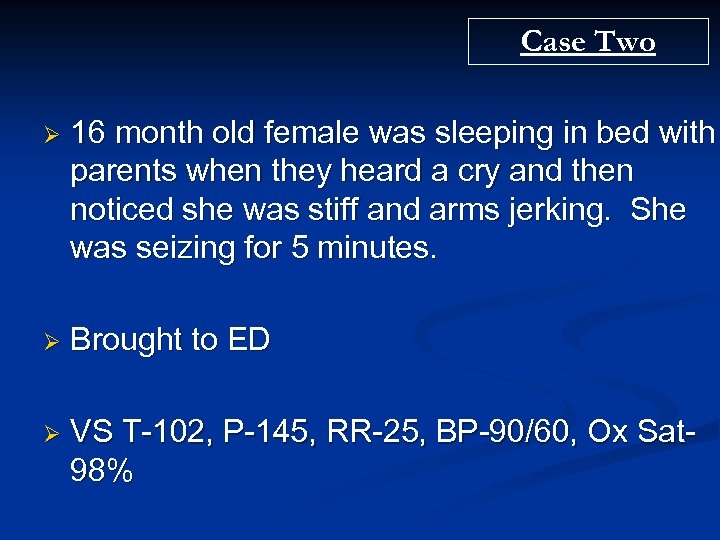
Case Two Ø 16 month old female was sleeping in bed with parents when they heard a cry and then noticed she was stiff and arms jerking. She was seizing for 5 minutes. Ø Brought to ED Ø VS T-102, P-145, RR-25, BP-90/60, Ox Sat 98%
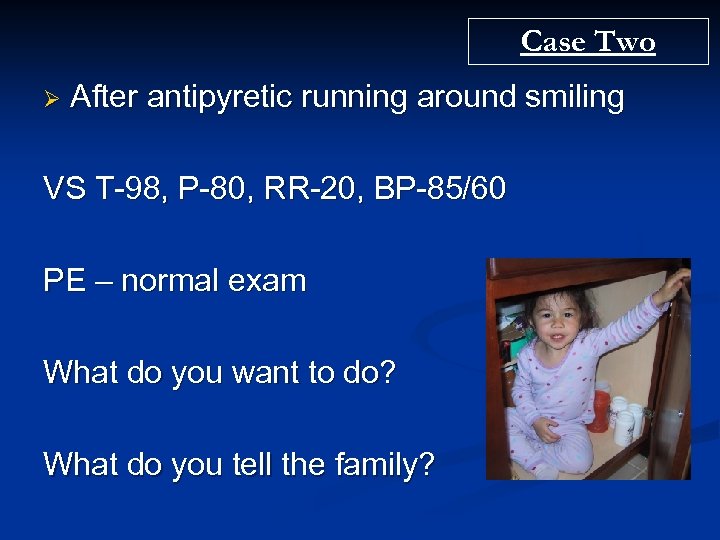
Case Two Ø After antipyretic running around smiling VS T-98, P-80, RR-20, BP-85/60 PE – normal exam What do you want to do? What do you tell the family?
Febrile Seizures Ø Simple Ø Generalized Ø Less than 15 -20 minutes Ø One in 24 hour period Ø Complex Ø Anything that is not simple
Febrile Seizures 6 months to 6 years Ø 2 -5 % of kids have a febrile seizure Ø 33% will have a second Ø 10% will have 3 or more Ø No proven increase risk of epilepsy in “normal” kids Ø
Simple Febrile Seizures Ø Work-up Ø Find Ø If source of fever and treat it you think they have meningitis tap them ØLow threshold to tap kids less than 12 months
Complex Febrile Seizures Ø Work-up Ø Find source of fever and treat it Ø Work up for seizure
Febrile Seizures Antipyretics (what do you tell parents? ) Ø Worth giving, but no study shows you can prevent future febrile seizures
Case Three Ø 6 month old female, brought in by rescue. Mother called and felt the child was having trouble breathing. Ø Seizing, GTC activity Ø T-95, P– 180, RR– 40, BP– 80/50, Ox Sat– 95% Ø What would you like to know and do?
Case Three Ø PE Ø No sign of trauma Ø Fontanelle flat Ø No rashes Ø Rhythmic jerking of arms bilaterally Ø Eyes rolled back Ø Not responding
Case Three Oxygen, NPA Saturation 100% Ø IV access nice work! Ø D-stick 100 good to know Ø Lorazepam 0. 1 mg/kg X 2 doses thank you! Ø Ø Still seizing? ? ?
Case Three Oxygen, NPA Saturation 100% Ø IV access nice work! Ø D-stick 100 good to know Ø Lorazepam 0. 1 mg/kg X 2 doses thank you! Ø Ø Still seizing? ? ?
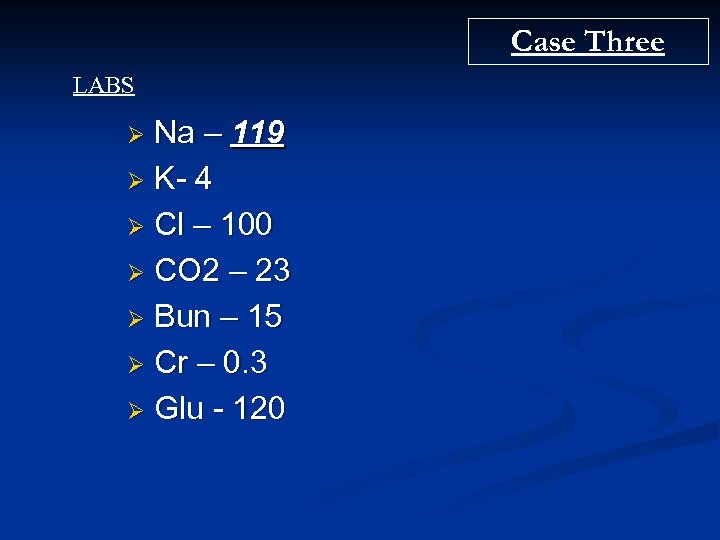
Case Three LABS Na – 119 Ø K- 4 Ø Cl – 100 Ø CO 2 – 23 Ø Bun – 15 Ø Cr – 0. 3 Ø Glu - 120 Ø
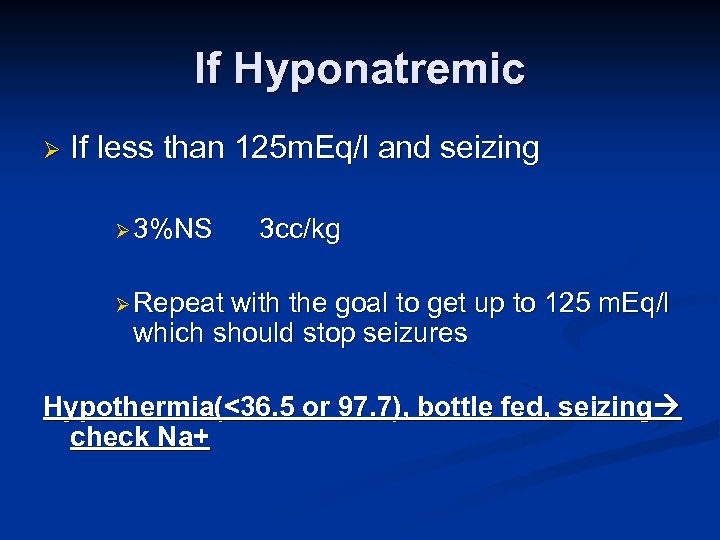
If Hyponatremic Ø If less than 125 m. Eq/l and seizing Ø 3%NS 3 cc/kg Ø Repeat with the goal to get up to 125 m. Eq/l which should stop seizures Hypothermia(<36. 5 or 97. 7), bottle fed, seizing check Na+
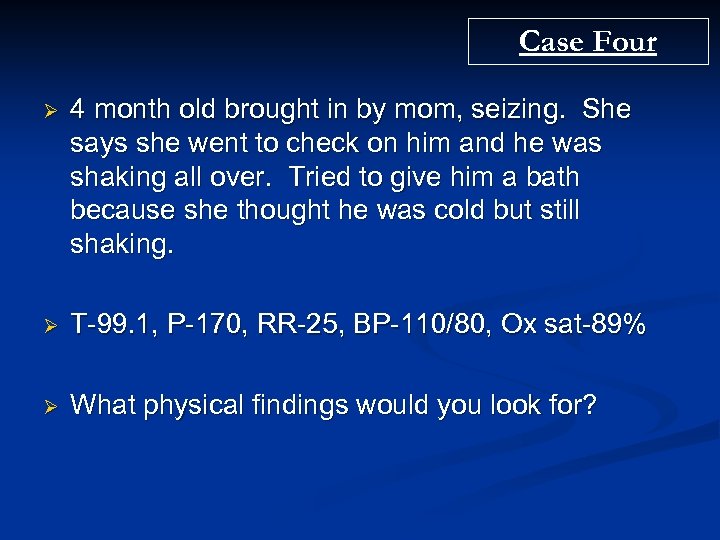
Case Four Ø 4 month old brought in by mom, seizing. She says she went to check on him and he was shaking all over. Tried to give him a bath because she thought he was cold but still shaking. Ø T-99. 1, P-170, RR-25, BP-110/80, Ox sat-89% Ø What physical findings would you look for?
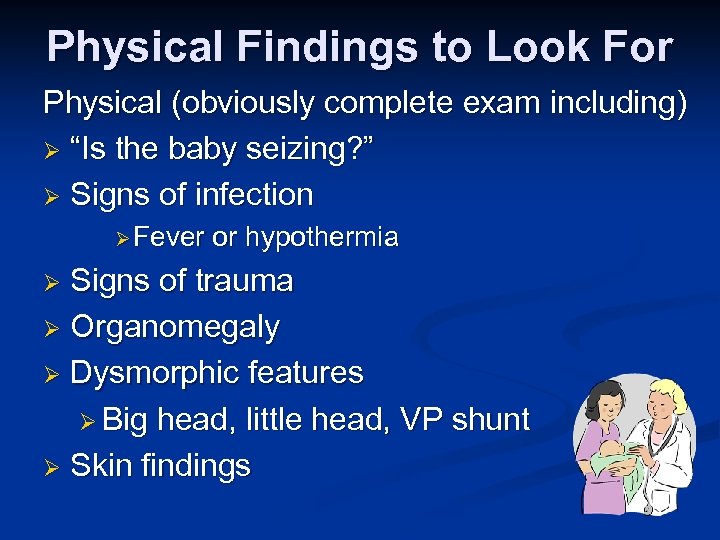
Physical Findings to Look For Physical (obviously complete exam including) Ø “Is the baby seizing? ” Ø Signs of infection Ø Fever or hypothermia Signs of trauma Ø Organomegaly Ø Dysmorphic features Ø Big head, little head, VP shunt Ø Skin findings Ø
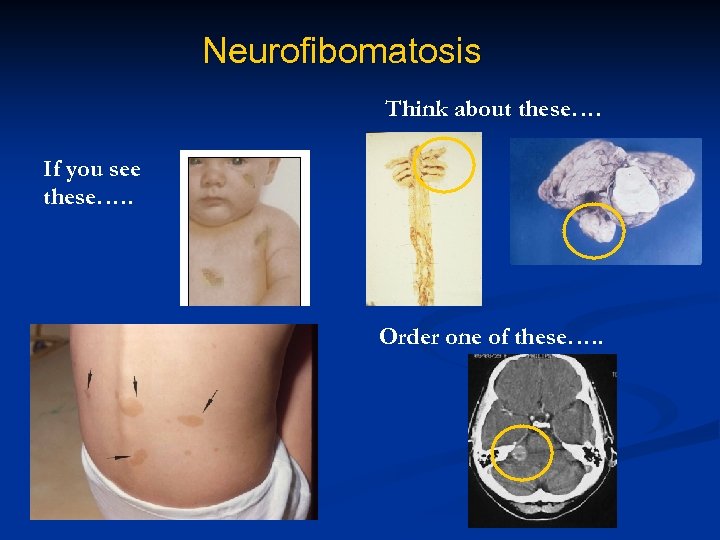
Neurofibomatosis Think about these…. If you see these…. . Order one of these…. .
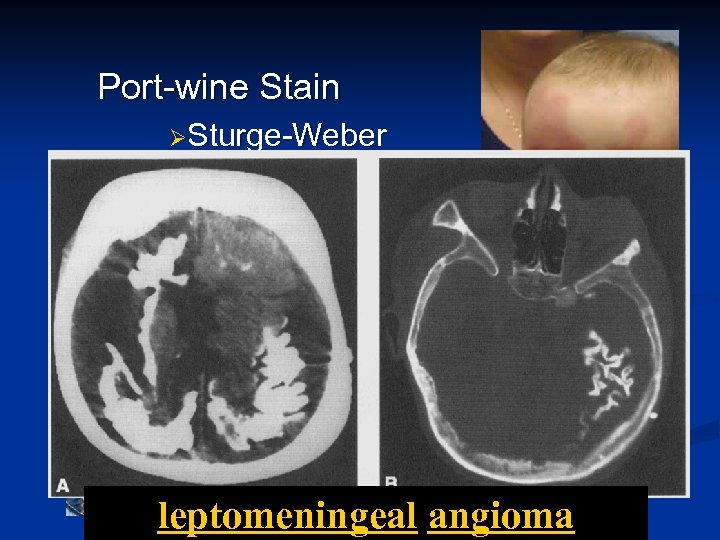
Port-wine Stain ØSturge-Weber leptomeningeal angioma
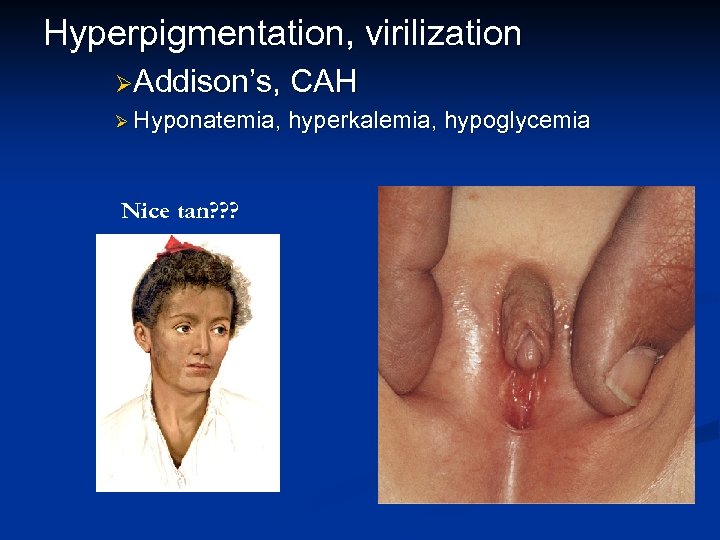
Hyperpigmentation, virilization ØAddison’s, CAH Ø Hyponatemia, hyperkalemia, hypoglycemia Nice tan? ? ? What the ? ? ?
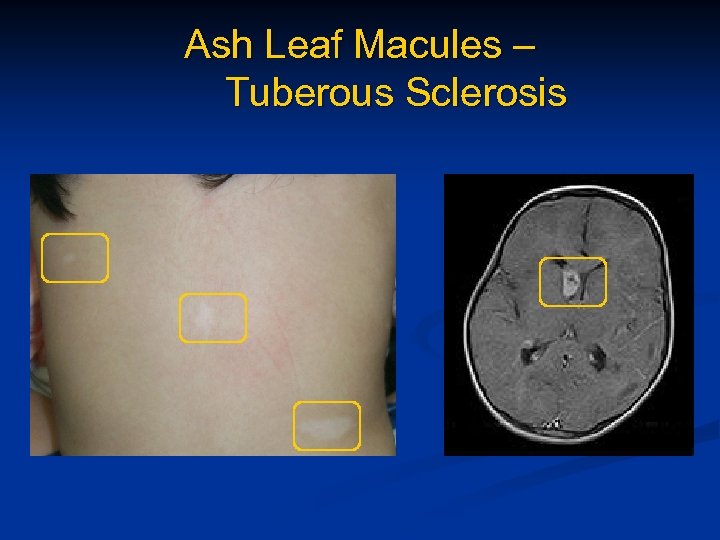
Ash Leaf Macules – Tuberous Sclerosis
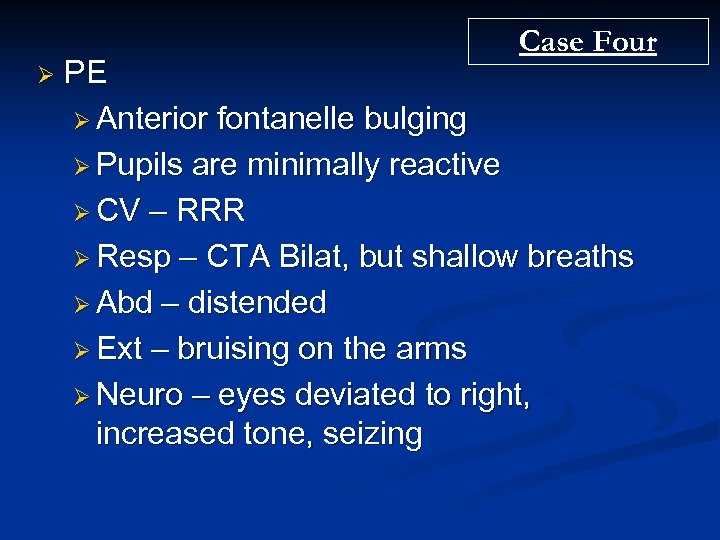
Case Four Ø PE Ø Anterior fontanelle bulging Ø Pupils are minimally reactive Ø CV – RRR Ø Resp – CTA Bilat, but shallow breaths Ø Abd – distended Ø Ext – bruising on the arms Ø Neuro – eyes deviated to right, increased tone, seizing

Case Four
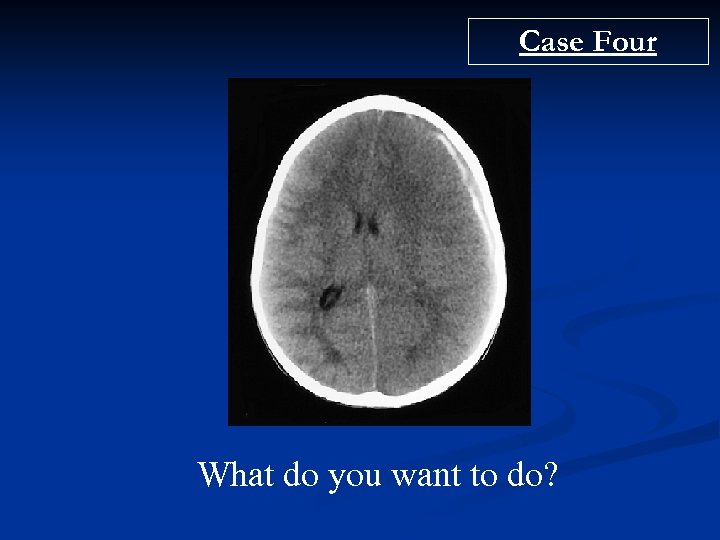
Case Four What do you want to do?
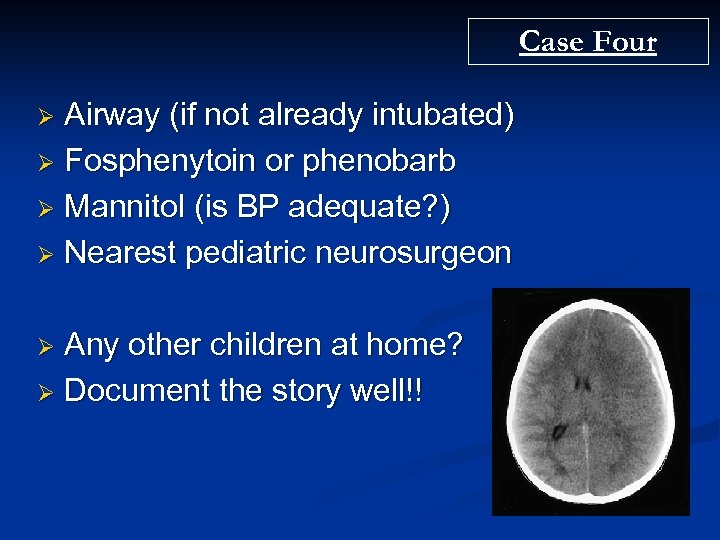
Case Four Airway (if not already intubated) Ø Fosphenytoin or phenobarb Ø Mannitol (is BP adequate? ) Ø Nearest pediatric neurosurgeon Ø Any other children at home? Ø Document the story well!! Ø
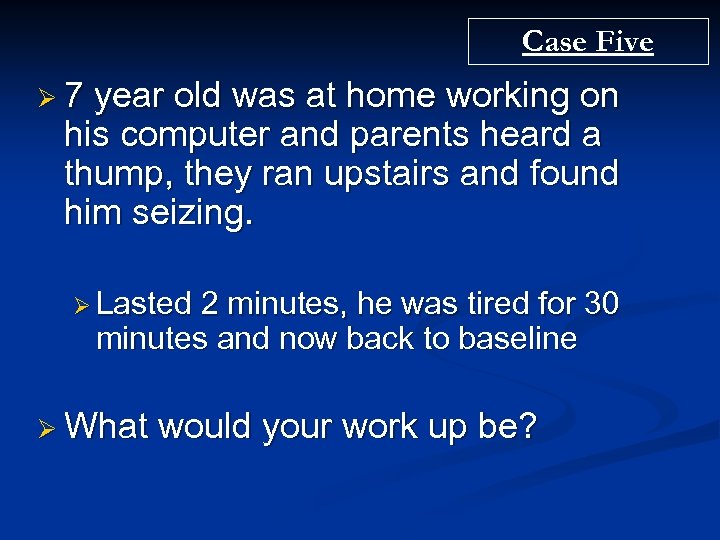
Case Five Ø 7 year old was at home working on his computer and parents heard a thump, they ran upstairs and found him seizing. Ø Lasted 2 minutes, he was tired for 30 minutes and now back to baseline Ø What would your work up be?

Case Five Ø If normal exam and no significant PMHx Ø Will need outpatient EEG, outpatient neurology Ø Possibly an MRI of brain Ø No Head CT Ø (some say 1/1000 mortality for each pediatric head CT) Ø No Blood work
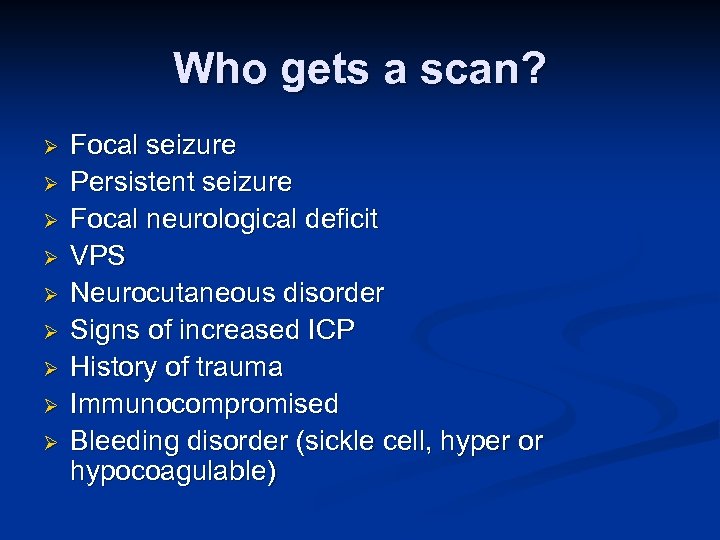
Who gets a scan? Ø Ø Ø Ø Ø Focal seizure Persistent seizure Focal neurological deficit VPS Neurocutaneous disorder Signs of increased ICP History of trauma Immunocompromised Bleeding disorder (sickle cell, hyper or hypocoagulable)
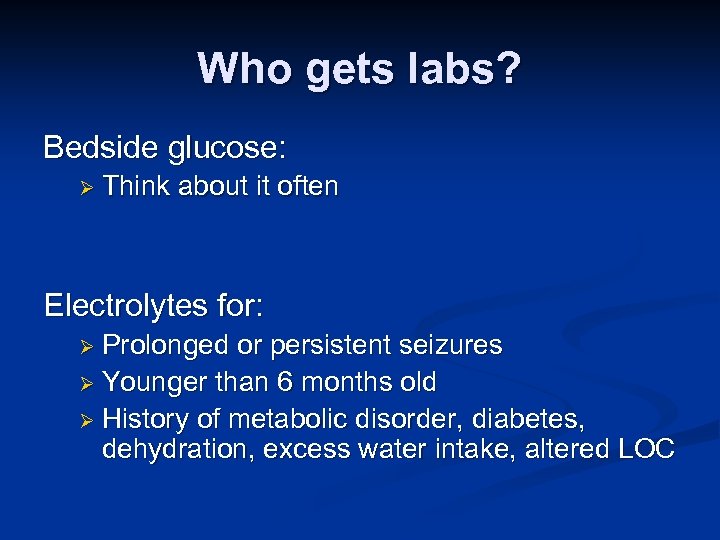
Who gets labs? Bedside glucose: Ø Think about it often Electrolytes for: Ø Prolonged or persistent seizures Ø Younger than 6 months old Ø History of metabolic disorder, diabetes, dehydration, excess water intake, altered LOC
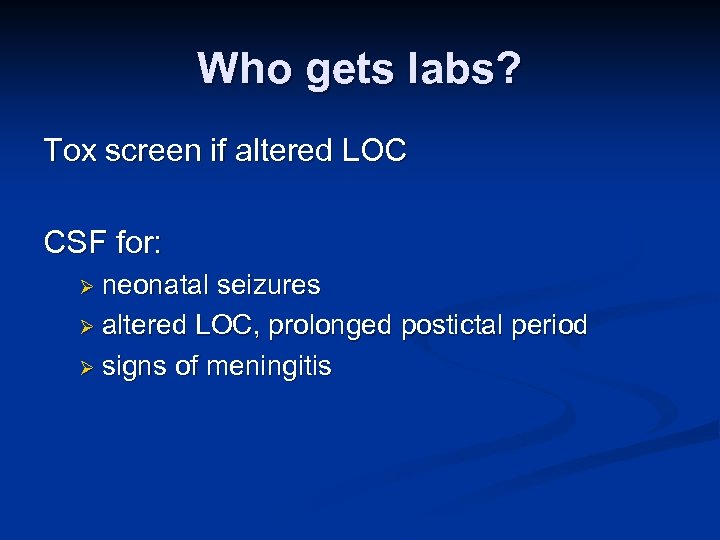
Who gets labs? Tox screen if altered LOC CSF for: Ø neonatal seizures Ø altered LOC, prolonged postictal period Ø signs of meningitis
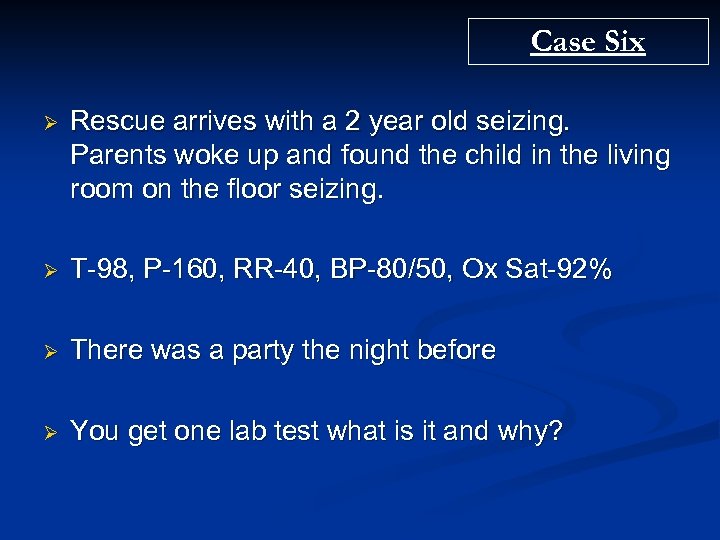
Case Six Ø Rescue arrives with a 2 year old seizing. Parents woke up and found the child in the living room on the floor seizing. Ø T-98, P-160, RR-40, BP-80/50, Ox Sat-92% Ø There was a party the night before Ø You get one lab test what is it and why?
Case Six Ø the parents did not clean up the mixed drinks laying around the house.
Maybe Miller had a Miller!

Case Six ØD-stick 35
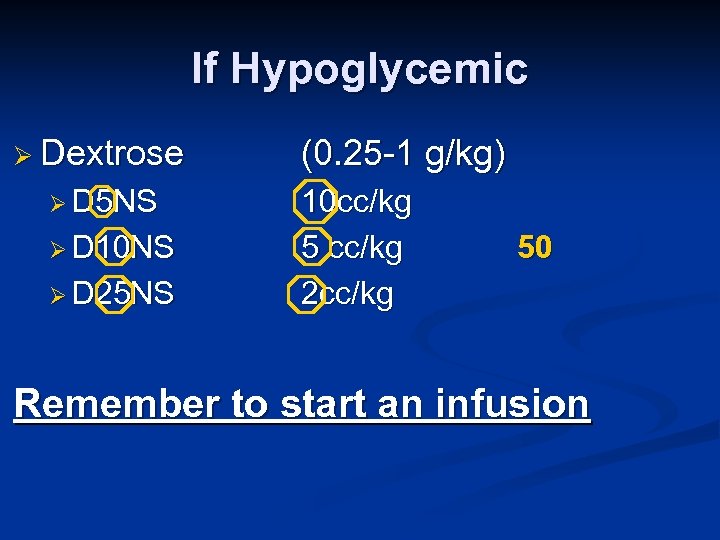
If Hypoglycemic Ø Dextrose Ø D 5 NS Ø D 10 NS Ø D 25 NS (0. 25 -1 g/kg) 10 cc/kg 5 cc/kg 2 cc/kg 50 Remember to start an infusion
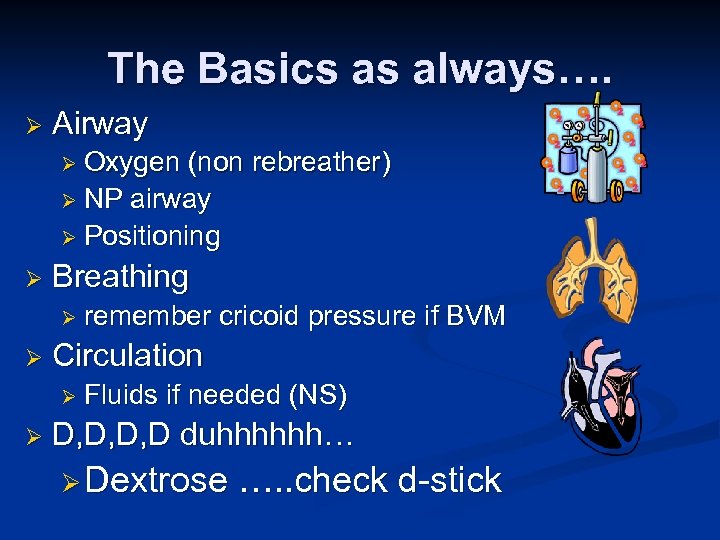
The Basics as always…. Ø Airway Ø Oxygen (non rebreather) Ø NP airway Ø Positioning Ø Breathing Ø remember Ø Circulation Ø Fluids Ø cricoid pressure if BVM if needed (NS) D, D, D, D duhhhhhh… Ø Dextrose …. . check d-stick
Access Ø Ø Ø Three attempts at IV Ø Consider other routes Think IM, PR, intranasal Ø IM Lorazepam Ø IM, PR, Intranasal Midazolam Ø PR Diazapam (Diastat) Agree on a weight and ask for meds early Ø Broslow? Other routine? Ø Not the best time to be practicing multiplication
Additional Pearls
Pyridoxine (Vit B 6) Ø Consider for persistent seizures in patient <1 yr Ø 50 -100 mg IV Ø Consider in suspected Isoniazid toxicity Ø Initial dose 70 mg/kg
Fosphenytoin Nicer to veins Ø Can be infused rapidly with less hypotension Ø 20 Phenytoin equivalents/kg load Ø
Case Seven Ø 4 day old is brought into your ED for poor feeding. You notice this……. . Ø VS T-99, P-165, RR-35, BP-70/45, Ox Sat 99%
Case Seven Ø PE Ø No sign of trauma Ø No rashes Ø Well hydrated Ø No dysmorphic features Ø Normal tone Ø Eyes deviated to the left Ø Persistent lip smacking/sucking/chewing Ø What would you like to do?
Neonatal Seizures Ø Rare to have GTC movements Ø Immature Ø Can cortical development be subtle focal findings Ø Repetitive movements ØEye blinking ØEye deviation ØChewing ØLip smacking ØBicycling
Neonatal Seizures § Can be focal tonic or clonic seizures Ø Sustained posturing of one or more extremities Ø Possibly just rhythmic jerking of single extremity
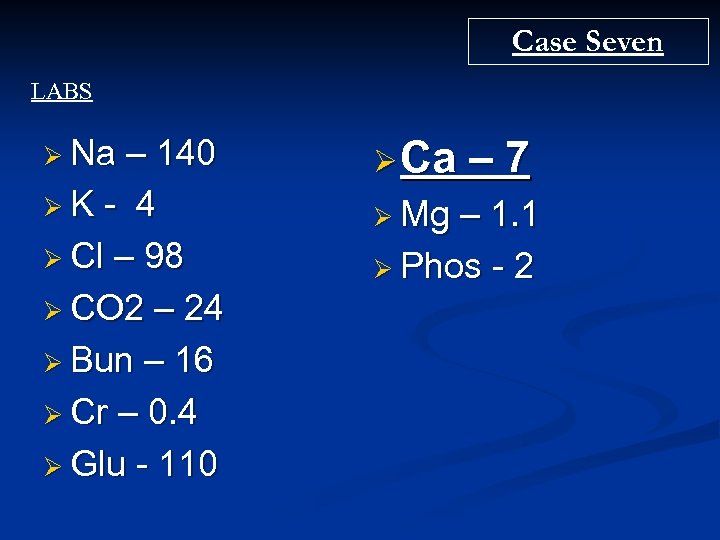
Case Seven LABS Ø Na – 140 ØK - 4 Ø Cl – 98 Ø CO 2 – 24 Ø Bun – 16 Ø Cr – 0. 4 Ø Glu - 110 Ø Ca Ø Mg – 7 – 1. 1 Ø Phos - 2
Hypocalcemia Serum calcium < 7 -8 mg/dl Ø 10% Ca. Gluconate 1 -2 ml/kg slow IV infusion Ø 10% Ca. Cl 0. 2 ml/kg slow IV infusion Ø Ø Continuous Ø ECG monitoring Chest x-ray looking for thymus
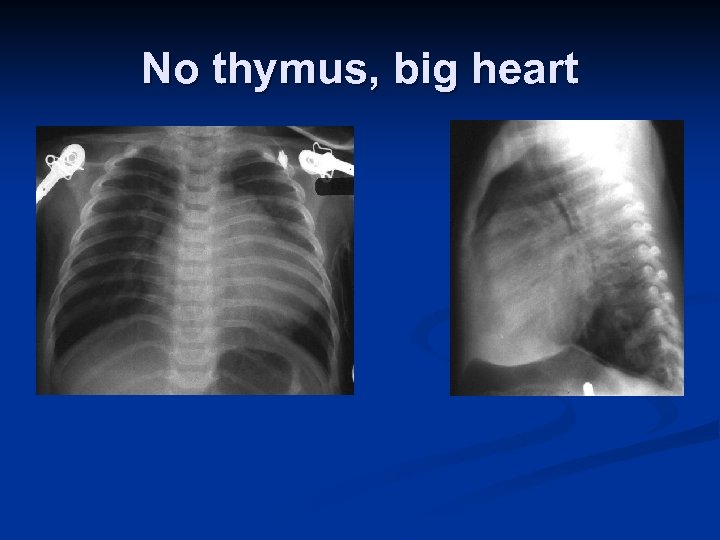
No thymus, big heart
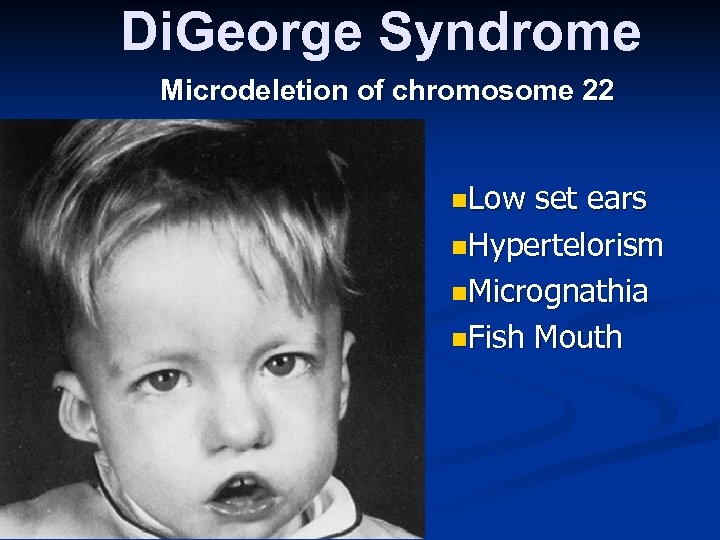
Di. George Syndrome Microdeletion of chromosome 22 n. Low set ears n. Hypertelorism n. Micrognathia n. Fish Mouth
b629c7f875e9f0310c8c62aab20d9b95.ppt