bdfad623ee92303f7323b386a9168560.ppt
- Количество слайдов: 70
 CARIES DIAGNOSIS
CARIES DIAGNOSIS
 What is diagnosis? Diagnosis is an art and science that results from the synthesis of scientific knowledge, clinical experience, intuition & common sense Caries diagnosis implies deciding whether a lesion is active, progressing rapidly or slowly or whether is already arrested.
What is diagnosis? Diagnosis is an art and science that results from the synthesis of scientific knowledge, clinical experience, intuition & common sense Caries diagnosis implies deciding whether a lesion is active, progressing rapidly or slowly or whether is already arrested.
 ASSESSMENT TOOLS Stepwise progression toward diagnosis & treatment planning depends on thorough assessment of the following Patient History Clinical examination Nutritional analysis Salivary analysis Radiographic assessment
ASSESSMENT TOOLS Stepwise progression toward diagnosis & treatment planning depends on thorough assessment of the following Patient History Clinical examination Nutritional analysis Salivary analysis Radiographic assessment
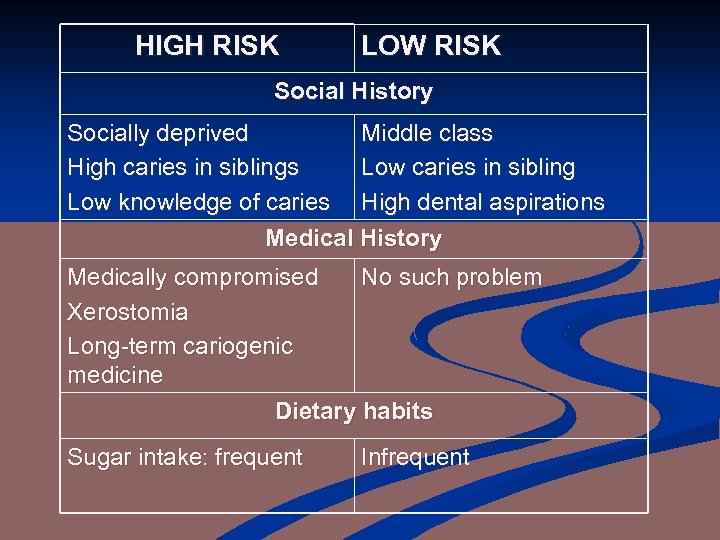 HIGH RISK LOW RISK Social History Socially deprived Middle class High caries in siblings Low caries in sibling Low knowledge of caries High dental aspirations Medical History Medically compromised No such problem Xerostomia Long-term cariogenic medicine Dietary habits Sugar intake: frequent Infrequent
HIGH RISK LOW RISK Social History Socially deprived Middle class High caries in siblings Low caries in sibling Low knowledge of caries High dental aspirations Medical History Medically compromised No such problem Xerostomia Long-term cariogenic medicine Dietary habits Sugar intake: frequent Infrequent
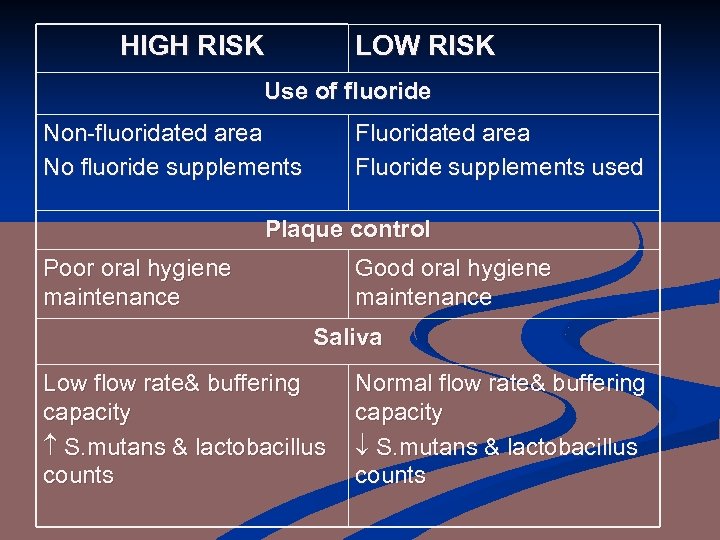 HIGH RISK LOW RISK Use of fluoride Non-fluoridated area No fluoride supplements Fluoridated area Fluoride supplements used Plaque control Poor oral hygiene maintenance Good oral hygiene maintenance Saliva Low flow rate& buffering capacity S. mutans & lactobacillus counts Normal flow rate& buffering capacity S. mutans & lactobacillus counts
HIGH RISK LOW RISK Use of fluoride Non-fluoridated area No fluoride supplements Fluoridated area Fluoride supplements used Plaque control Poor oral hygiene maintenance Good oral hygiene maintenance Saliva Low flow rate& buffering capacity S. mutans & lactobacillus counts Normal flow rate& buffering capacity S. mutans & lactobacillus counts
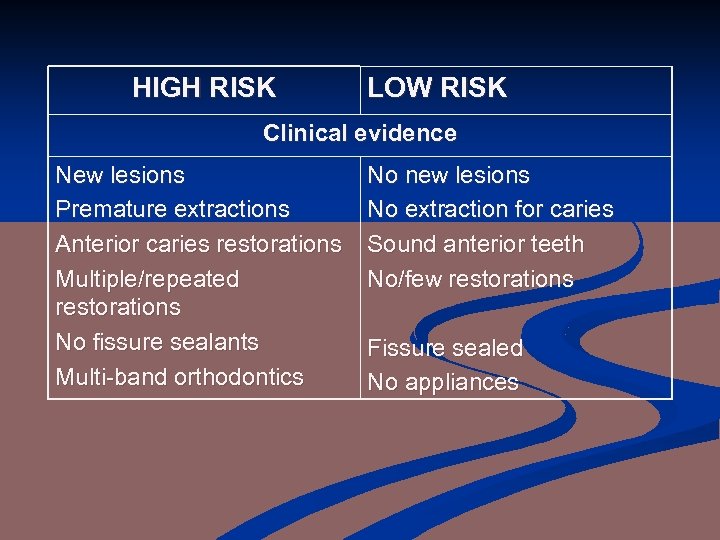 HIGH RISK LOW RISK Clinical evidence New lesions Premature extractions Anterior caries restorations Multiple/repeated restorations No fissure sealants Multi-band orthodontics No new lesions No extraction for caries Sound anterior teeth No/few restorations Fissure sealed No appliances
HIGH RISK LOW RISK Clinical evidence New lesions Premature extractions Anterior caries restorations Multiple/repeated restorations No fissure sealants Multi-band orthodontics No new lesions No extraction for caries Sound anterior teeth No/few restorations Fissure sealed No appliances
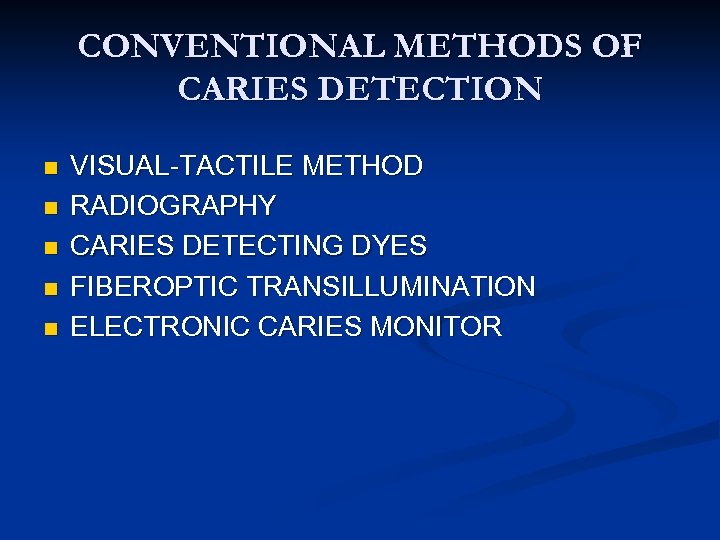 CONVENTIONAL METHODS OF CARIES DETECTION n n n VISUAL-TACTILE METHOD RADIOGRAPHY CARIES DETECTING DYES FIBEROPTIC TRANSILLUMINATION ELECTRONIC CARIES MONITOR
CONVENTIONAL METHODS OF CARIES DETECTION n n n VISUAL-TACTILE METHOD RADIOGRAPHY CARIES DETECTING DYES FIBEROPTIC TRANSILLUMINATION ELECTRONIC CARIES MONITOR
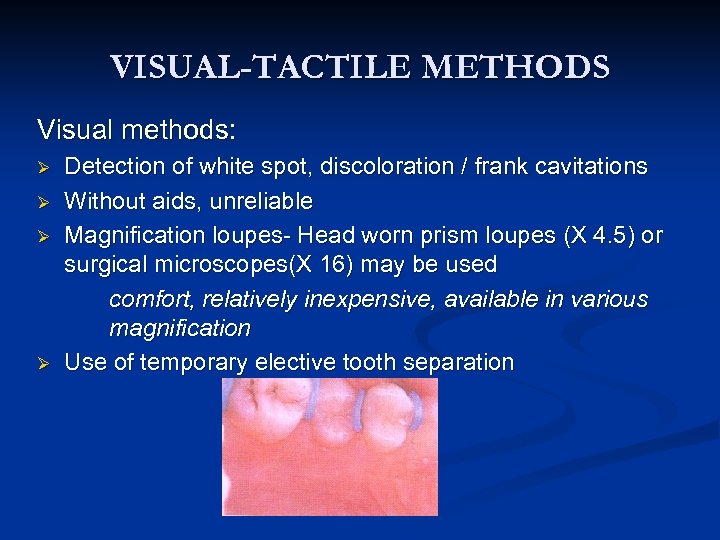 VISUAL-TACTILE METHODS Visual methods: Ø Ø Detection of white spot, discoloration / frank cavitations Without aids, unreliable Magnification loupes- Head worn prism loupes (X 4. 5) or surgical microscopes(X 16) may be used comfort, relatively inexpensive, available in various magnification Use of temporary elective tooth separation
VISUAL-TACTILE METHODS Visual methods: Ø Ø Detection of white spot, discoloration / frank cavitations Without aids, unreliable Magnification loupes- Head worn prism loupes (X 4. 5) or surgical microscopes(X 16) may be used comfort, relatively inexpensive, available in various magnification Use of temporary elective tooth separation
 Tactile methods: Ø Ø Explorers are widely used for the detection of carious tooth structure - Right angled probe- no. 6 - Back action probe- no. 17 - Shepherd's crook- no. 23 - Cowhorn with curved ends- no. 2 Dental floss
Tactile methods: Ø Ø Explorers are widely used for the detection of carious tooth structure - Right angled probe- no. 6 - Back action probe- no. 17 - Shepherd's crook- no. 23 - Cowhorn with curved ends- no. 2 Dental floss
![Use of explorer is not advocated because; ] Sharp tips physically damage small lesions Use of explorer is not advocated because; ] Sharp tips physically damage small lesions](https://present5.com/presentation/bdfad623ee92303f7323b386a9168560/image-10.jpg) Use of explorer is not advocated because; ] Sharp tips physically damage small lesions with intact surfaces ] Probing can cause fracture & cavitation of incipient lesion. It may spread the organism in the mouth ] Mechanical binding may be due to noncarious reasons Shape of fissure Sharpness of explorer Force of application Path of explorer placement
Use of explorer is not advocated because; ] Sharp tips physically damage small lesions with intact surfaces ] Probing can cause fracture & cavitation of incipient lesion. It may spread the organism in the mouth ] Mechanical binding may be due to noncarious reasons Shape of fissure Sharpness of explorer Force of application Path of explorer placement
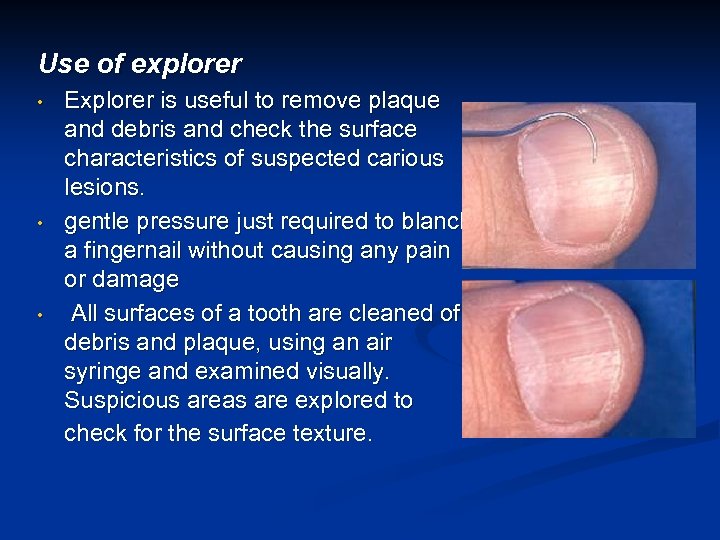 Use of explorer • • • Explorer is useful to remove plaque and debris and check the surface characteristics of suspected carious lesions. gentle pressure just required to blanch a fingernail without causing any pain or damage All surfaces of a tooth are cleaned of debris and plaque, using an air syringe and examined visually. Suspicious areas are explored to check for the surface texture.
Use of explorer • • • Explorer is useful to remove plaque and debris and check the surface characteristics of suspected carious lesions. gentle pressure just required to blanch a fingernail without causing any pain or damage All surfaces of a tooth are cleaned of debris and plaque, using an air syringe and examined visually. Suspicious areas are explored to check for the surface texture.
 SMOOTH SURFACE CARIES Non- cavitated: n n n No signs of cavitation after visual or tactile examination. Location: where dental plaque accumulates (gingival margin). Surface characteristics: Matted (not glossy) when a tooth is dried.
SMOOTH SURFACE CARIES Non- cavitated: n n n No signs of cavitation after visual or tactile examination. Location: where dental plaque accumulates (gingival margin). Surface characteristics: Matted (not glossy) when a tooth is dried.
 Areas of demineralization not in close proximity to the gingival margin not covered by plaque smooth and glossy are non-cavitated not active non-cavitated carious lesions. n Visual enamel opacity under sound marginal ridge indicate undermined enamel due to dental caries non-cavitated carious lesion in dentin n
Areas of demineralization not in close proximity to the gingival margin not covered by plaque smooth and glossy are non-cavitated not active non-cavitated carious lesions. n Visual enamel opacity under sound marginal ridge indicate undermined enamel due to dental caries non-cavitated carious lesion in dentin n
 Non-cavitated carious lesion ENAMEL DENTIN
Non-cavitated carious lesion ENAMEL DENTIN
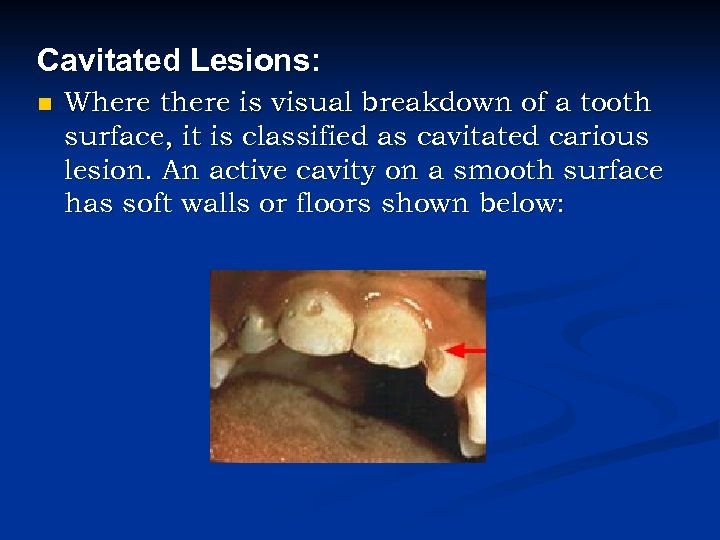 Cavitated Lesions: n Where there is visual breakdown of a tooth surface, it is classified as cavitated carious lesion. An active cavity on a smooth surface has soft walls or floors shown below:
Cavitated Lesions: n Where there is visual breakdown of a tooth surface, it is classified as cavitated carious lesion. An active cavity on a smooth surface has soft walls or floors shown below:
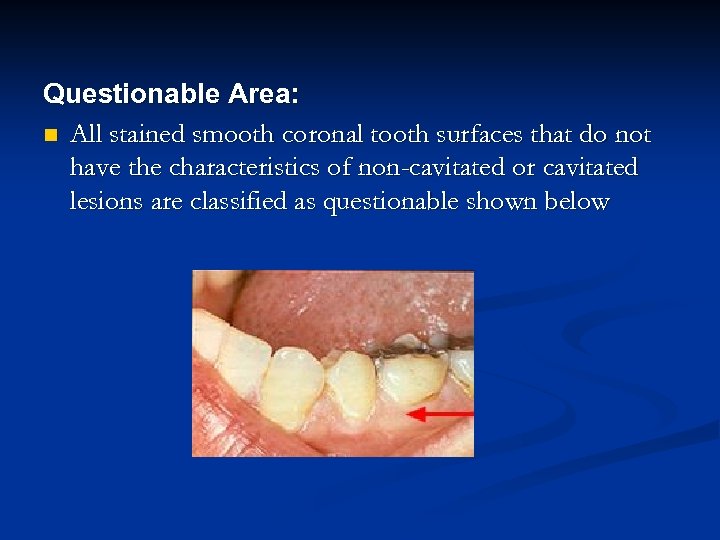 Questionable Area: n All stained smooth coronal tooth surfaces that do not have the characteristics of non-cavitated or cavitated lesions are classified as questionable shown below
Questionable Area: n All stained smooth coronal tooth surfaces that do not have the characteristics of non-cavitated or cavitated lesions are classified as questionable shown below
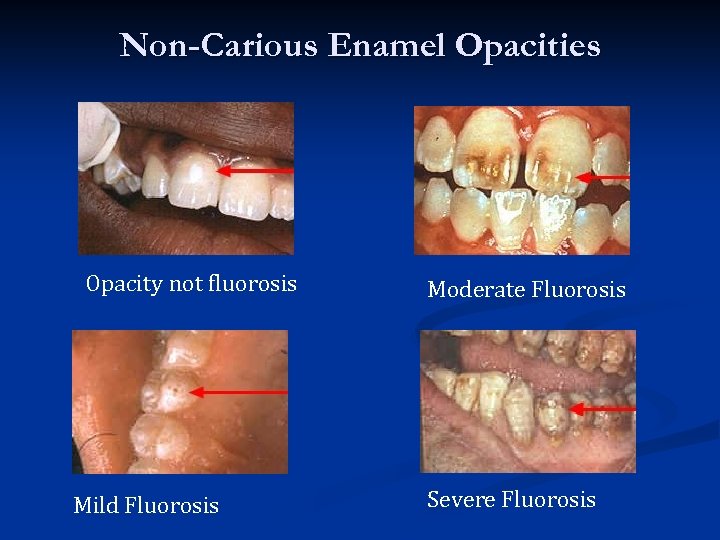 Non-Carious Enamel Opacities Opacity not fluorosis Mild Fluorosis Moderate Fluorosis Severe Fluorosis
Non-Carious Enamel Opacities Opacity not fluorosis Mild Fluorosis Moderate Fluorosis Severe Fluorosis
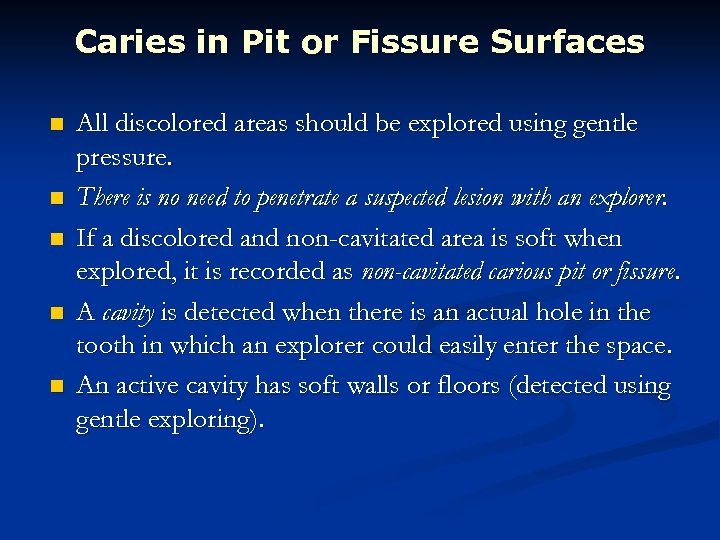 Caries in Pit or Fissure Surfaces n n n All discolored areas should be explored using gentle pressure. There is no need to penetrate a suspected lesion with an explorer. If a discolored and non-cavitated area is soft when explored, it is recorded as non-cavitated carious pit or fissure. A cavity is detected when there is an actual hole in the tooth in which an explorer could easily enter the space. An active cavity has soft walls or floors (detected using gentle exploring).
Caries in Pit or Fissure Surfaces n n n All discolored areas should be explored using gentle pressure. There is no need to penetrate a suspected lesion with an explorer. If a discolored and non-cavitated area is soft when explored, it is recorded as non-cavitated carious pit or fissure. A cavity is detected when there is an actual hole in the tooth in which an explorer could easily enter the space. An active cavity has soft walls or floors (detected using gentle exploring).
 n If there is visual enamel opacity under an ostensibly sound or stained pit or fissure, then the enamel is undermined because of dental caries and the tooth surface is classified with a non-cavitated carious lesion in dentin.
n If there is visual enamel opacity under an ostensibly sound or stained pit or fissure, then the enamel is undermined because of dental caries and the tooth surface is classified with a non-cavitated carious lesion in dentin.
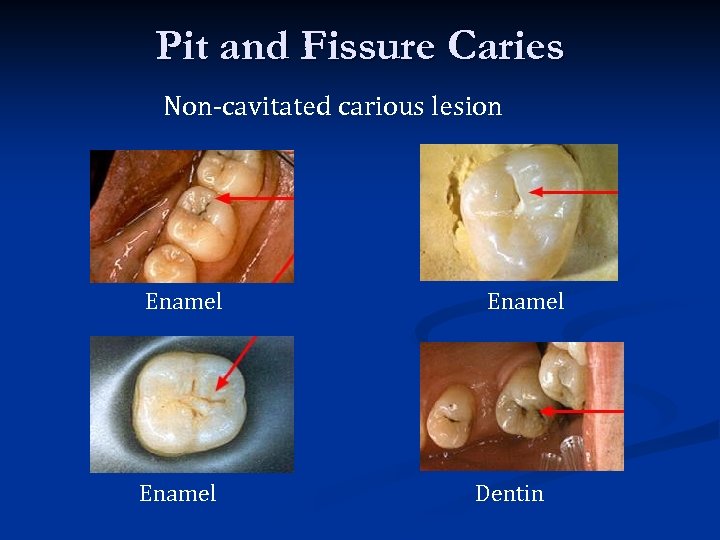 Pit and Fissure Caries Non-cavitated carious lesion Enamel Dentin
Pit and Fissure Caries Non-cavitated carious lesion Enamel Dentin
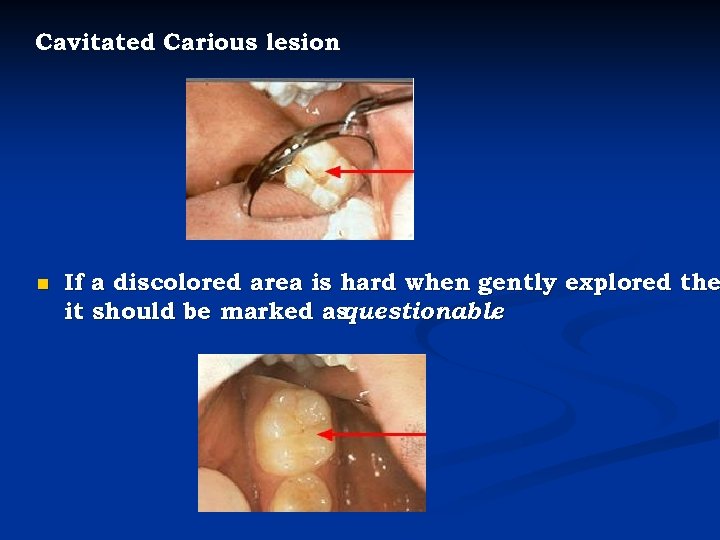 Cavitated Carious lesion n If a discolored area is hard when gently explored the it should be marked as questionable.
Cavitated Carious lesion n If a discolored area is hard when gently explored the it should be marked as questionable.
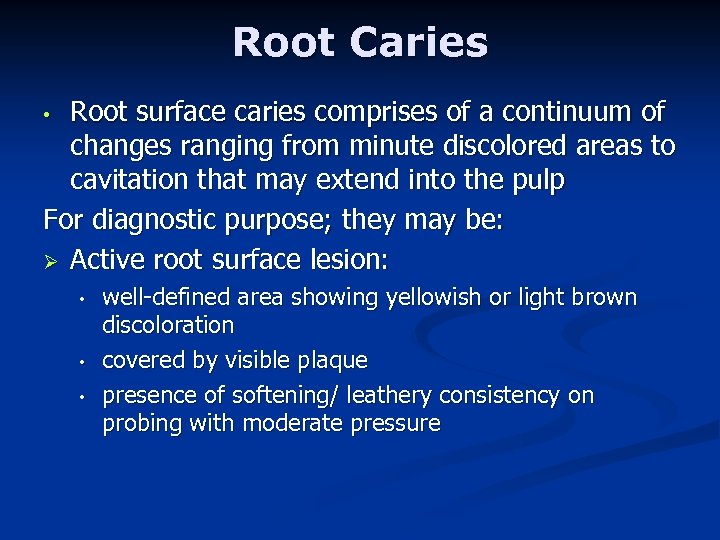 Root Caries Root surface caries comprises of a continuum of changes ranging from minute discolored areas to cavitation that may extend into the pulp For diagnostic purpose; they may be: Ø Active root surface lesion: • • well-defined area showing yellowish or light brown discoloration covered by visible plaque presence of softening/ leathery consistency on probing with moderate pressure
Root Caries Root surface caries comprises of a continuum of changes ranging from minute discolored areas to cavitation that may extend into the pulp For diagnostic purpose; they may be: Ø Active root surface lesion: • • well-defined area showing yellowish or light brown discoloration covered by visible plaque presence of softening/ leathery consistency on probing with moderate pressure
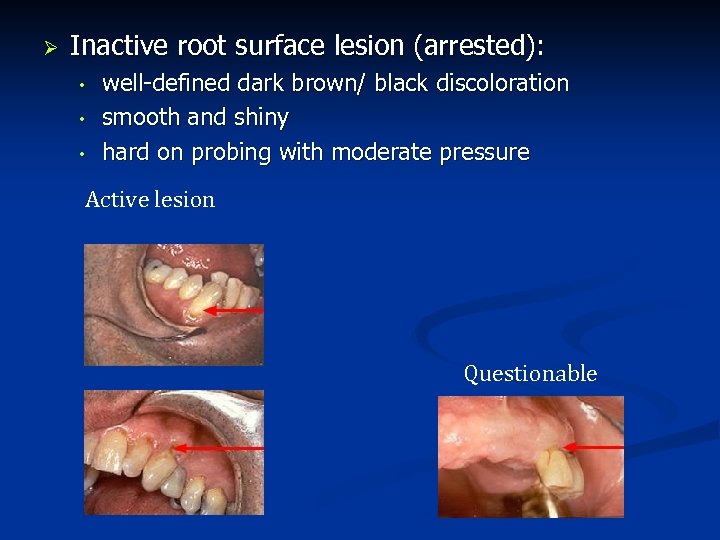 Ø Inactive root surface lesion (arrested): • • • well-defined dark brown/ black discoloration smooth and shiny hard on probing with moderate pressure Active lesion Questionable
Ø Inactive root surface lesion (arrested): • • • well-defined dark brown/ black discoloration smooth and shiny hard on probing with moderate pressure Active lesion Questionable
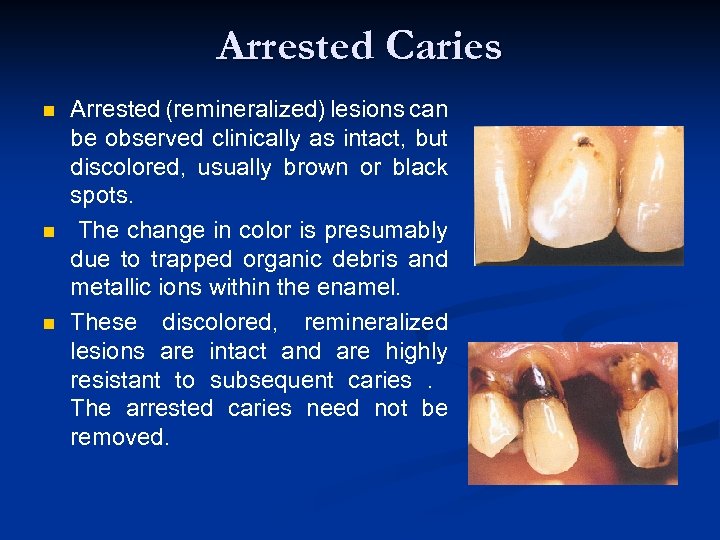 Arrested Caries n n n Arrested (remineralized) lesions can be observed clinically as intact, but discolored, usually brown or black spots. The change in color is presumably due to trapped organic debris and metallic ions within the enamel. These discolored, remineralized lesions are intact and are highly resistant to subsequent caries. The arrested caries need not be removed.
Arrested Caries n n n Arrested (remineralized) lesions can be observed clinically as intact, but discolored, usually brown or black spots. The change in color is presumably due to trapped organic debris and metallic ions within the enamel. These discolored, remineralized lesions are intact and are highly resistant to subsequent caries. The arrested caries need not be removed.
 Recurrent caries n n It is diagnosed whenever there is softness due to caries at a defective margin, and when the tip of a periodontal probe can enter the defect without any resistance. A restoration with a discolored margin or a small marginal ditch (<0. 5 mm or the head of the probe) is recorded as an early recurrent carious area. A larger defect should be classified as advanced recurrent carious area
Recurrent caries n n It is diagnosed whenever there is softness due to caries at a defective margin, and when the tip of a periodontal probe can enter the defect without any resistance. A restoration with a discolored margin or a small marginal ditch (<0. 5 mm or the head of the probe) is recorded as an early recurrent carious area. A larger defect should be classified as advanced recurrent carious area
 Ø There are two valid indicators of recurrent (secondary) caries: • • softness at the margin of a filling that is detected using an explorer or presence of a large defect (a minimum diameter of 0. 4 mm) at a margin of a filling with softness in the area. Ø Large defects are associated with a high level of colonization with cariogenic bacteria. Marginal discoloration by itself is not a valid sign for dental caries.
Ø There are two valid indicators of recurrent (secondary) caries: • • softness at the margin of a filling that is detected using an explorer or presence of a large defect (a minimum diameter of 0. 4 mm) at a margin of a filling with softness in the area. Ø Large defects are associated with a high level of colonization with cariogenic bacteria. Marginal discoloration by itself is not a valid sign for dental caries.
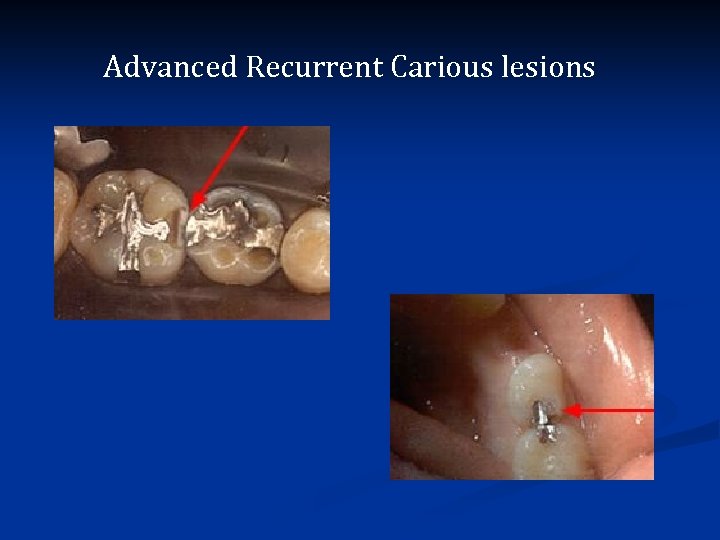 Advanced Recurrent Carious lesions
Advanced Recurrent Carious lesions
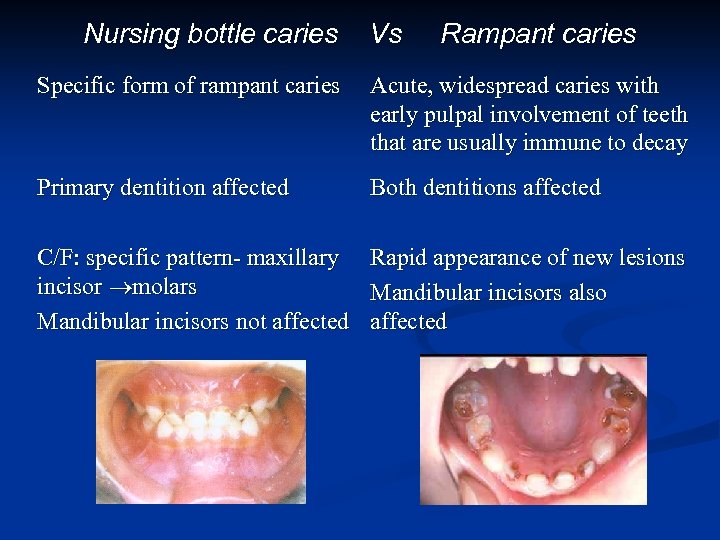 Nursing bottle caries Vs Rampant caries Specific form of rampant caries Acute, widespread caries with early pulpal involvement of teeth that are usually immune to decay Primary dentition affected Both dentitions affected C/F: specific pattern- maxillary incisor molars Mandibular incisors not affected Rapid appearance of new lesions Mandibular incisors also affected
Nursing bottle caries Vs Rampant caries Specific form of rampant caries Acute, widespread caries with early pulpal involvement of teeth that are usually immune to decay Primary dentition affected Both dentitions affected C/F: specific pattern- maxillary incisor molars Mandibular incisors not affected Rapid appearance of new lesions Mandibular incisors also affected
 RADIOGRAPHY § § Carious lesions are detectable radiographically when there has been enough demineralization to allow it to be differentiate from normal They are valuable in detecting proximal caries which may go undetected during clinical examination. On average they have around 50% to 70% sensitivity in detecting carious lesions. 40% demineralization is required for definitive decision on caries
RADIOGRAPHY § § Carious lesions are detectable radiographically when there has been enough demineralization to allow it to be differentiate from normal They are valuable in detecting proximal caries which may go undetected during clinical examination. On average they have around 50% to 70% sensitivity in detecting carious lesions. 40% demineralization is required for definitive decision on caries
 § Radiographic examinations include; Bitewing radiographs IOPA radiographs using paralleling technique Dental panoramic tomograph § The two important decisions related to radiographic examination are (1) when to take a radiograph and (2) how to evaluate a radiograph for presence of signs of dental caries.
§ Radiographic examinations include; Bitewing radiographs IOPA radiographs using paralleling technique Dental panoramic tomograph § The two important decisions related to radiographic examination are (1) when to take a radiograph and (2) how to evaluate a radiograph for presence of signs of dental caries.
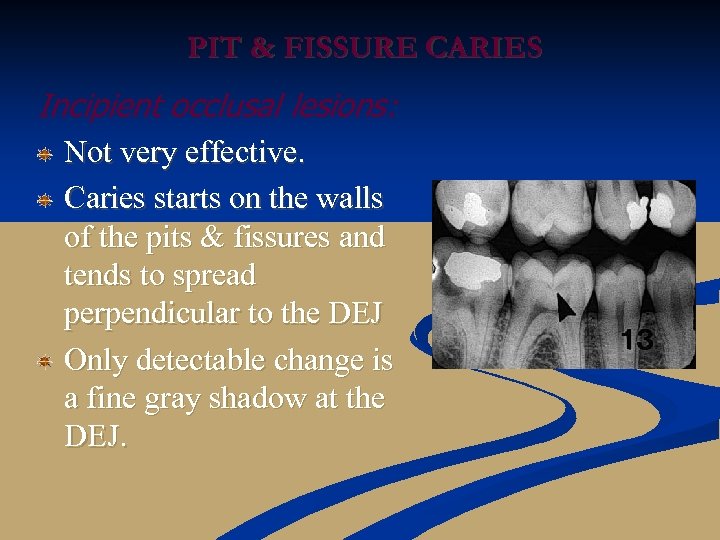 PIT & FISSURE CARIES Incipient occlusal lesions: Not very effective. Caries starts on the walls of the pits & fissures and tends to spread perpendicular to the DEJ Only detectable change is a fine gray shadow at the DEJ.
PIT & FISSURE CARIES Incipient occlusal lesions: Not very effective. Caries starts on the walls of the pits & fissures and tends to spread perpendicular to the DEJ Only detectable change is a fine gray shadow at the DEJ.
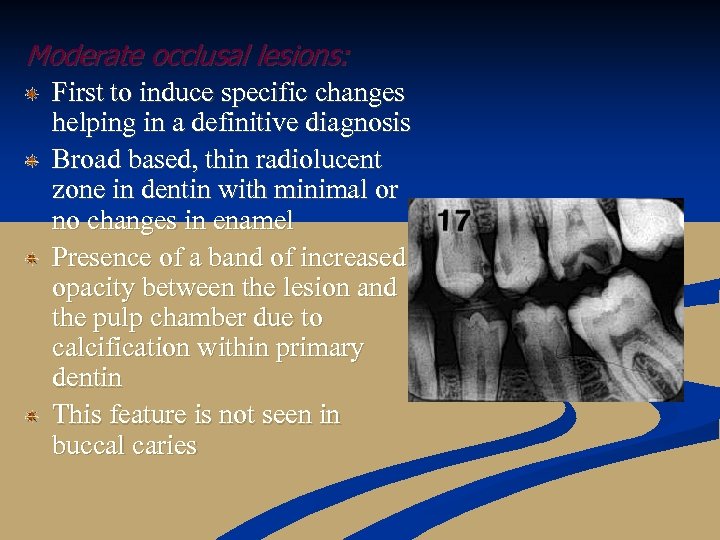 Moderate occlusal lesions: First to induce specific changes helping in a definitive diagnosis Broad based, thin radiolucent zone in dentin with minimal or no changes in enamel Presence of a band of increased opacity between the lesion and the pulp chamber due to calcification within primary dentin This feature is not seen in buccal caries
Moderate occlusal lesions: First to induce specific changes helping in a definitive diagnosis Broad based, thin radiolucent zone in dentin with minimal or no changes in enamel Presence of a band of increased opacity between the lesion and the pulp chamber due to calcification within primary dentin This feature is not seen in buccal caries
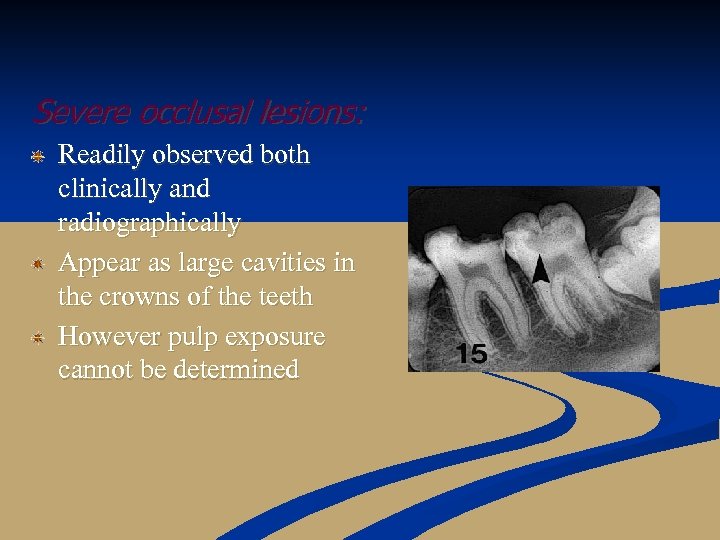 Severe occlusal lesions: Readily observed both clinically and radiographically Appear as large cavities in the crowns of the teeth However pulp exposure cannot be determined
Severe occlusal lesions: Readily observed both clinically and radiographically Appear as large cavities in the crowns of the teeth However pulp exposure cannot be determined
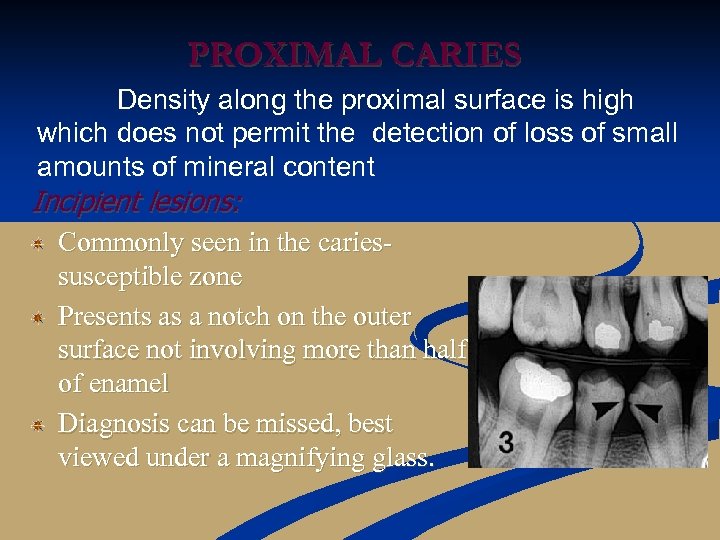 PROXIMAL CARIES Density along the proximal surface is high which does not permit the detection of loss of small amounts of mineral content Incipient lesions: Commonly seen in the cariessusceptible zone Presents as a notch on the outer surface not involving more than half of enamel Diagnosis can be missed, best viewed under a magnifying glass.
PROXIMAL CARIES Density along the proximal surface is high which does not permit the detection of loss of small amounts of mineral content Incipient lesions: Commonly seen in the cariessusceptible zone Presents as a notch on the outer surface not involving more than half of enamel Diagnosis can be missed, best viewed under a magnifying glass.
 Moderate proximal lesions: Involve more than outer half of enamel but do not extend into DEJ May have one of type of appearance: 67% - triangle with broad base towards outer surface 16% - a diffuse radiolucent image 17% - combination of both
Moderate proximal lesions: Involve more than outer half of enamel but do not extend into DEJ May have one of type of appearance: 67% - triangle with broad base towards outer surface 16% - a diffuse radiolucent image 17% - combination of both
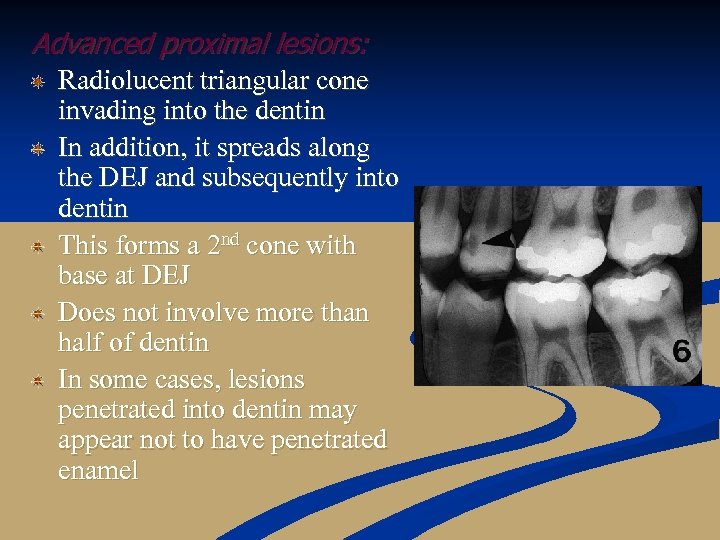 Advanced proximal lesions: Radiolucent triangular cone invading into the dentin In addition, it spreads along the DEJ and subsequently into dentin This forms a 2 nd cone with base at DEJ Does not involve more than half of dentin In some cases, lesions penetrated into dentin may appear not to have penetrated enamel
Advanced proximal lesions: Radiolucent triangular cone invading into the dentin In addition, it spreads along the DEJ and subsequently into dentin This forms a 2 nd cone with base at DEJ Does not involve more than half of dentin In some cases, lesions penetrated into dentin may appear not to have penetrated enamel
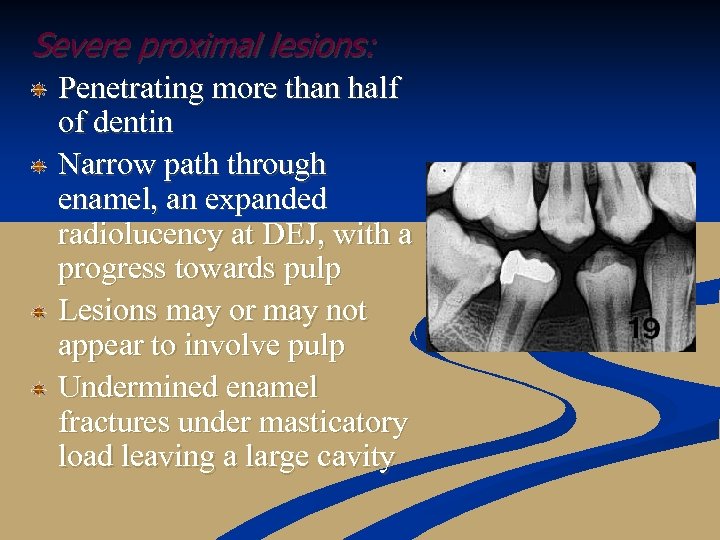 Severe proximal lesions: Penetrating more than half of dentin Narrow path through enamel, an expanded radiolucency at DEJ, with a progress towards pulp Lesions may or may not appear to involve pulp Undermined enamel fractures under masticatory load leaving a large cavity
Severe proximal lesions: Penetrating more than half of dentin Narrow path through enamel, an expanded radiolucency at DEJ, with a progress towards pulp Lesions may or may not appear to involve pulp Undermined enamel fractures under masticatory load leaving a large cavity
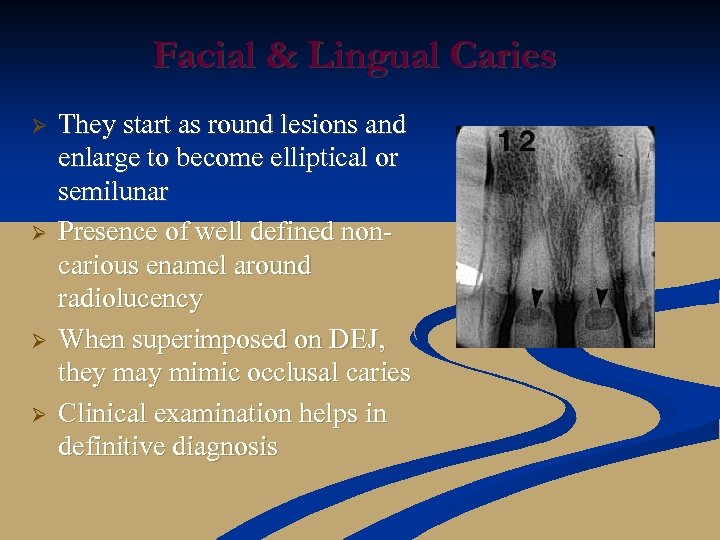 Facial & Lingual Caries Ø Ø They start as round lesions and enlarge to become elliptical or semilunar Presence of well defined noncarious enamel around radiolucency When superimposed on DEJ, they may mimic occlusal caries Clinical examination helps in definitive diagnosis
Facial & Lingual Caries Ø Ø They start as round lesions and enlarge to become elliptical or semilunar Presence of well defined noncarious enamel around radiolucency When superimposed on DEJ, they may mimic occlusal caries Clinical examination helps in definitive diagnosis
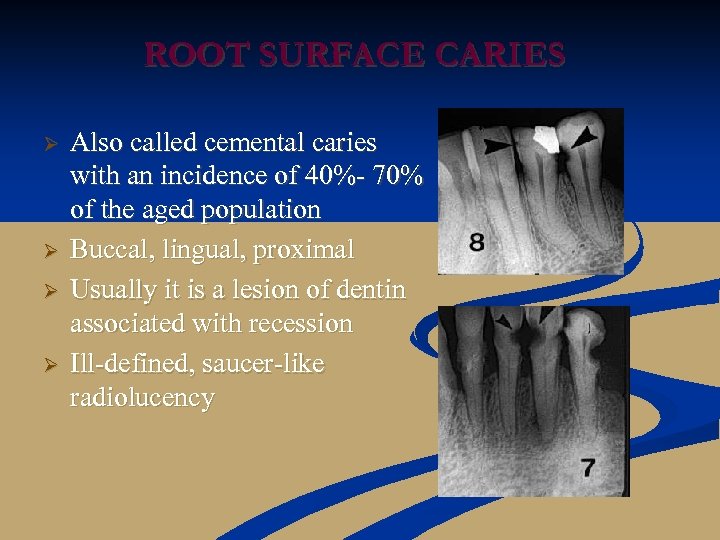 ROOT SURFACE CARIES Ø Ø Also called cemental caries with an incidence of 40%- 70% of the aged population Buccal, lingual, proximal Usually it is a lesion of dentin associated with recession Ill-defined, saucer-like radiolucency
ROOT SURFACE CARIES Ø Ø Also called cemental caries with an incidence of 40%- 70% of the aged population Buccal, lingual, proximal Usually it is a lesion of dentin associated with recession Ill-defined, saucer-like radiolucency
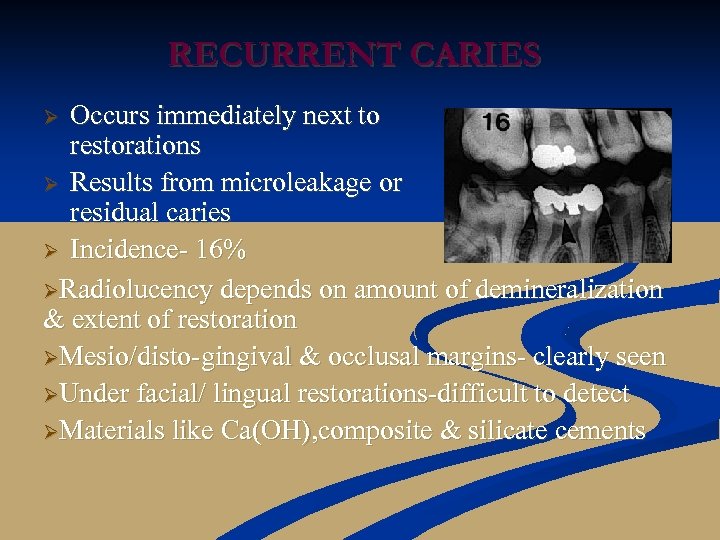 RECURRENT CARIES Occurs immediately next to restorations Ø Results from microleakage or residual caries Ø Incidence- 16% ØRadiolucency depends on amount of demineralization & extent of restoration ØMesio/disto-gingival & occlusal margins- clearly seen ØUnder facial/ lingual restorations-difficult to detect ØMaterials like Ca(OH), composite & silicate cements Ø
RECURRENT CARIES Occurs immediately next to restorations Ø Results from microleakage or residual caries Ø Incidence- 16% ØRadiolucency depends on amount of demineralization & extent of restoration ØMesio/disto-gingival & occlusal margins- clearly seen ØUnder facial/ lingual restorations-difficult to detect ØMaterials like Ca(OH), composite & silicate cements Ø
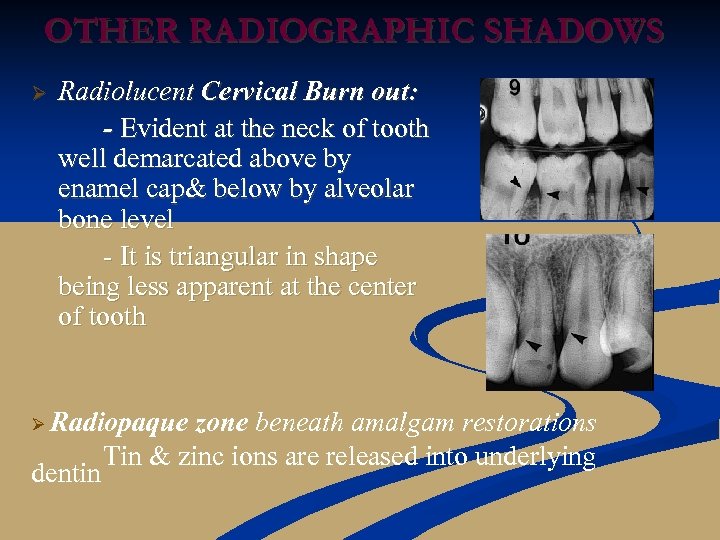 OTHER RADIOGRAPHIC SHADOWS Ø Radiolucent Cervical Burn out: - Evident at the neck of tooth well demarcated above by enamel cap& below by alveolar bone level - It is triangular in shape being less apparent at the center of tooth Ø Radiopaque dentin zone beneath amalgam restorations Tin & zinc ions are released into underlying
OTHER RADIOGRAPHIC SHADOWS Ø Radiolucent Cervical Burn out: - Evident at the neck of tooth well demarcated above by enamel cap& below by alveolar bone level - It is triangular in shape being less apparent at the center of tooth Ø Radiopaque dentin zone beneath amalgam restorations Tin & zinc ions are released into underlying
![Pitfalls Of Radiography 2 dimensional view of 3 dimensional object ] Radiographic depth of Pitfalls Of Radiography 2 dimensional view of 3 dimensional object ] Radiographic depth of](https://present5.com/presentation/bdfad623ee92303f7323b386a9168560/image-42.jpg) Pitfalls Of Radiography 2 dimensional view of 3 dimensional object ] Radiographic depth of a lesion is often less than actual depth ] Overlapping of proximal surfaces on a radiograph ] Occlusal (incipient) caries of enamel difficult to detect ] Dental anomalies like hypoplastic pits mimic proximal caries ] Cervical burnout often confused with root caries ]
Pitfalls Of Radiography 2 dimensional view of 3 dimensional object ] Radiographic depth of a lesion is often less than actual depth ] Overlapping of proximal surfaces on a radiograph ] Occlusal (incipient) caries of enamel difficult to detect ] Dental anomalies like hypoplastic pits mimic proximal caries ] Cervical burnout often confused with root caries ]
![XERORADIOGRAPHY ] ] ] ] It is similar to photocopy machine Consists of Aluminum XERORADIOGRAPHY ] ] ] ] It is similar to photocopy machine Consists of Aluminum](https://present5.com/presentation/bdfad623ee92303f7323b386a9168560/image-43.jpg) XERORADIOGRAPHY ] ] ] ] It is similar to photocopy machine Consists of Aluminum plate coated with selenium which provides a uniform electrostatic charge X- rays selective discharge of particles Latent image Processing unit: Latent image positive image Very good Edge enhancement i. e. , differentiating areas with different densities Twice more sensitive than D speed film, but equivalent to E speed film Disadvantages: Electrostatic charge may cause patient discomfort Processing to be completed by 15 minutes
XERORADIOGRAPHY ] ] ] ] It is similar to photocopy machine Consists of Aluminum plate coated with selenium which provides a uniform electrostatic charge X- rays selective discharge of particles Latent image Processing unit: Latent image positive image Very good Edge enhancement i. e. , differentiating areas with different densities Twice more sensitive than D speed film, but equivalent to E speed film Disadvantages: Electrostatic charge may cause patient discomfort Processing to be completed by 15 minutes
![DIGITAL IMAGING ] ] A digital image is an image formed & represented by DIGITAL IMAGING ] ] A digital image is an image formed & represented by](https://present5.com/presentation/bdfad623ee92303f7323b386a9168560/image-44.jpg) DIGITAL IMAGING ] ] A digital image is an image formed & represented by a spatially distributed set of discrete sensors & pixels 2 types of non- film receptors Direct digital imaging – digital image receptor Indirect digital imaging – video camera forming digital images of a radiograph Two types of detectors are used in Direct digital imaging Photostimulable phosphor ( PSP) –barium fluorohalide Charged couple device (CCD) – silicon Image is stored on a computer
DIGITAL IMAGING ] ] A digital image is an image formed & represented by a spatially distributed set of discrete sensors & pixels 2 types of non- film receptors Direct digital imaging – digital image receptor Indirect digital imaging – video camera forming digital images of a radiograph Two types of detectors are used in Direct digital imaging Photostimulable phosphor ( PSP) –barium fluorohalide Charged couple device (CCD) – silicon Image is stored on a computer
 DIGITAL IMAGING Schick System Digora System Trophy System
DIGITAL IMAGING Schick System Digora System Trophy System
 Manipulation of images 1. Magnification 2. Variable contrast 3. variable density 4. Labeling important information 5. Highlighting and colorization Advantages: 1. Images are available in seconds 2. Exposure is reduced 50 -90% 3. Image size, contrast and density can be manipulated to improve interpretation 4. Record keeping is vastly improved. All films are labeled, filed and retrieved easily. Duplicate hard copies are the same as originals and simple to make 5. Provision of teletransmission
Manipulation of images 1. Magnification 2. Variable contrast 3. variable density 4. Labeling important information 5. Highlighting and colorization Advantages: 1. Images are available in seconds 2. Exposure is reduced 50 -90% 3. Image size, contrast and density can be manipulated to improve interpretation 4. Record keeping is vastly improved. All films are labeled, filed and retrieved easily. Duplicate hard copies are the same as originals and simple to make 5. Provision of teletransmission
 SUBTRACTION RADIOGRAPHY ¯ ¯ ¯ ¯ Structured noise is reduced in order to increase the detectablity of changes in the radiograph Structured noise refers to the information on the radiograph which have not diagnostic value It requires 2 identical images. The subtracted image is a composite these two, representing a difference in their densities Sensitive enough to detect changes of 0. 12 mm 90% accurate in detecting mineral loss of 5% Black end of gray scale suitable for proximal & recurrent caries Contrast can be enhanced with color aid.
SUBTRACTION RADIOGRAPHY ¯ ¯ ¯ ¯ Structured noise is reduced in order to increase the detectablity of changes in the radiograph Structured noise refers to the information on the radiograph which have not diagnostic value It requires 2 identical images. The subtracted image is a composite these two, representing a difference in their densities Sensitive enough to detect changes of 0. 12 mm 90% accurate in detecting mineral loss of 5% Black end of gray scale suitable for proximal & recurrent caries Contrast can be enhanced with color aid.
 COMPUTER IMAGE ANALYSIS ¯ ¯ ¯ Softwares have been developed for automated procedures which are able to overcome the short coming of human eye Software supports an operation whereby a threshold is set up by the examiner which determines the program’s display of lesion probability Tuned Aperture Computed Tomography (TACT) involve the tomosynthesis of structures in 3 D thereby increasing the accurate detection of caries Useful for monitoring carious lesion Increased sensitivity but decreased specificity
COMPUTER IMAGE ANALYSIS ¯ ¯ ¯ Softwares have been developed for automated procedures which are able to overcome the short coming of human eye Software supports an operation whereby a threshold is set up by the examiner which determines the program’s display of lesion probability Tuned Aperture Computed Tomography (TACT) involve the tomosynthesis of structures in 3 D thereby increasing the accurate detection of caries Useful for monitoring carious lesion Increased sensitivity but decreased specificity
 DYES FOR CARIES DETECTION They selectively complex with carious tooth structure which is later disclosed with the help of fluorescence n Aids in both quantitative & qualitative analysis of the lesion DYES FOR ENAMEL CARIES: Procion: N 2 & (OH) groups irreversibly complex with caries Acts as a fixative Calcein: complexes with calcium & remains bound to the tooth Zyglo ZL-22: fluorescent tracer dye, not used in vivo Brilliant blue: 10% aqueous Brilliant Blue, not used in vivo n
DYES FOR CARIES DETECTION They selectively complex with carious tooth structure which is later disclosed with the help of fluorescence n Aids in both quantitative & qualitative analysis of the lesion DYES FOR ENAMEL CARIES: Procion: N 2 & (OH) groups irreversibly complex with caries Acts as a fixative Calcein: complexes with calcium & remains bound to the tooth Zyglo ZL-22: fluorescent tracer dye, not used in vivo Brilliant blue: 10% aqueous Brilliant Blue, not used in vivo n
 DYES FOR DENTIN CARIES: Ø 1% acid red 52 in propylene glycol complexes specifically with denatured collagen, hence used to differentiate infected and affected dentin Ø Iodine penetration method (Pot iodide) for evaluating enamel permeability DISADVANTAGES • Dye staining and bacterial penetration are independent phenomena, hence no actual quantification • They also stain food debris, enamel pellicle, other organic matter • Dye aided carious removal- laborious • Stains DEJ
DYES FOR DENTIN CARIES: Ø 1% acid red 52 in propylene glycol complexes specifically with denatured collagen, hence used to differentiate infected and affected dentin Ø Iodine penetration method (Pot iodide) for evaluating enamel permeability DISADVANTAGES • Dye staining and bacterial penetration are independent phenomena, hence no actual quantification • They also stain food debris, enamel pellicle, other organic matter • Dye aided carious removal- laborious • Stains DEJ
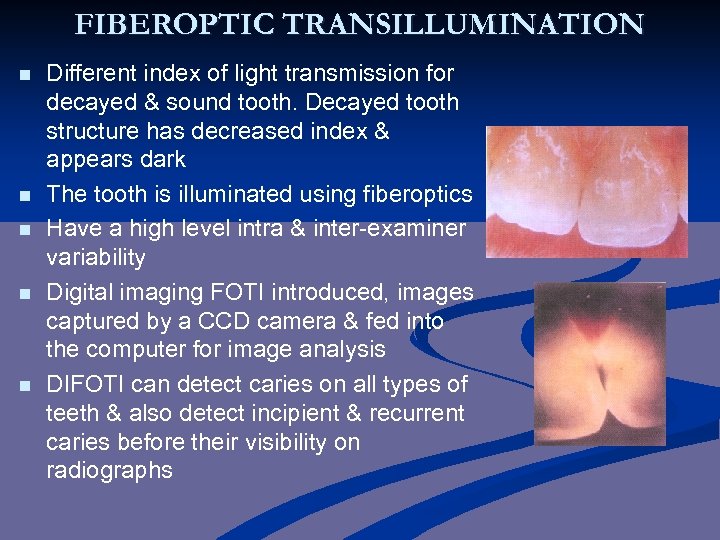 FIBEROPTIC TRANSILLUMINATION n n n Different index of light transmission for decayed & sound tooth. Decayed tooth structure has decreased index & appears dark The tooth is illuminated using fiberoptics Have a high level intra & inter-examiner variability Digital imaging FOTI introduced, images captured by a CCD camera & fed into the computer for image analysis DIFOTI can detect caries on all types of teeth & also detect incipient & recurrent caries before their visibility on radiographs
FIBEROPTIC TRANSILLUMINATION n n n Different index of light transmission for decayed & sound tooth. Decayed tooth structure has decreased index & appears dark The tooth is illuminated using fiberoptics Have a high level intra & inter-examiner variability Digital imaging FOTI introduced, images captured by a CCD camera & fed into the computer for image analysis DIFOTI can detect caries on all types of teeth & also detect incipient & recurrent caries before their visibility on radiographs
 ELECTRIC MEASUREMENTS FOR CARIES n n n First proposed by Magitot in 1878 Tooth demineralization due to caries process causes increased porosity of tooth structure. This porosity contains fluid containing ions. This leads increased electrical conductivity, conversely, leads to decreased electrical resistance or impedance ECM device uses a fixed-frequency (23 Hz)alternating current which measures ‘bulk resistance’ of tooth
ELECTRIC MEASUREMENTS FOR CARIES n n n First proposed by Magitot in 1878 Tooth demineralization due to caries process causes increased porosity of tooth structure. This porosity contains fluid containing ions. This leads increased electrical conductivity, conversely, leads to decreased electrical resistance or impedance ECM device uses a fixed-frequency (23 Hz)alternating current which measures ‘bulk resistance’ of tooth
 n Two systems Vangaurd system – 25 Hz – ordinal scale of 0 – 9 Caries meter L – 400 Hz – 4 colored lights green –no caries yellow – enamel caries orange – dentin caries red –pulp involvement § ECM limited to occlusal sites. ECM to H/P- 97% accuracy Cannot be used where amalgam filling is present Materials have different responses at different frequencies. Electrical Impedance Spectroscopy (EIS) operates over different frequencies & thus determine more accurately these differences. EIS can be used on both occlusal & proximal surfaces § n
n Two systems Vangaurd system – 25 Hz – ordinal scale of 0 – 9 Caries meter L – 400 Hz – 4 colored lights green –no caries yellow – enamel caries orange – dentin caries red –pulp involvement § ECM limited to occlusal sites. ECM to H/P- 97% accuracy Cannot be used where amalgam filling is present Materials have different responses at different frequencies. Electrical Impedance Spectroscopy (EIS) operates over different frequencies & thus determine more accurately these differences. EIS can be used on both occlusal & proximal surfaces § n
 Factors affecting electrical measurements 1. Porosity 2. Surface area 3. Thickness of the tissues 4. Hydration of enamel 5. Temperature 6. Concentrations of ions in the dental tissue fluids
Factors affecting electrical measurements 1. Porosity 2. Surface area 3. Thickness of the tissues 4. Hydration of enamel 5. Temperature 6. Concentrations of ions in the dental tissue fluids
 RECENT ADVANCES IN CARIES DETECTION n n n Research in the past two decades has lead to the development of new technologies that asses changes in fluorescence of enamel & dentin due to loss of mineral Benedict- 1929, normal teeth fluorescence Optical methods used are Quantitative light- induced fluorescence- QLF™ Infrared laser fluorescence - DIAGNOdent
RECENT ADVANCES IN CARIES DETECTION n n n Research in the past two decades has lead to the development of new technologies that asses changes in fluorescence of enamel & dentin due to loss of mineral Benedict- 1929, normal teeth fluorescence Optical methods used are Quantitative light- induced fluorescence- QLF™ Infrared laser fluorescence - DIAGNOdent
 CARIES RISK ASSESSMENT n n Clinical examination neither predicts caries activity nor susceptibility Certain simple reliable lab tests can facilitate this, which is important because; - need & extent of personalized preventive measures - index for therapeutic measures - patient education - manage progress of restorative procedures - identify high risk groups / individuals
CARIES RISK ASSESSMENT n n Clinical examination neither predicts caries activity nor susceptibility Certain simple reliable lab tests can facilitate this, which is important because; - need & extent of personalized preventive measures - index for therapeutic measures - patient education - manage progress of restorative procedures - identify high risk groups / individuals
 Requisites of tests Ø Ø Ø Correlation between predicted & actual caries development Reliability & validity Simple to perform Quick results Measurement of mechanism involved in caries process
Requisites of tests Ø Ø Ø Correlation between predicted & actual caries development Reliability & validity Simple to perform Quick results Measurement of mechanism involved in caries process
 Caries activity Vs Caries susceptibility § § § Caries activity refers to the increment of active lesions Susceptibility refers to inherent propensity of the host & target tissue affected by caries Caries activity tests measure either the quantity of specific bacterial group or their ability to produce acids. Hence this must be coupled with clinical examination prior to treatment planning.
Caries activity Vs Caries susceptibility § § § Caries activity refers to the increment of active lesions Susceptibility refers to inherent propensity of the host & target tissue affected by caries Caries activity tests measure either the quantity of specific bacterial group or their ability to produce acids. Hence this must be coupled with clinical examination prior to treatment planning.
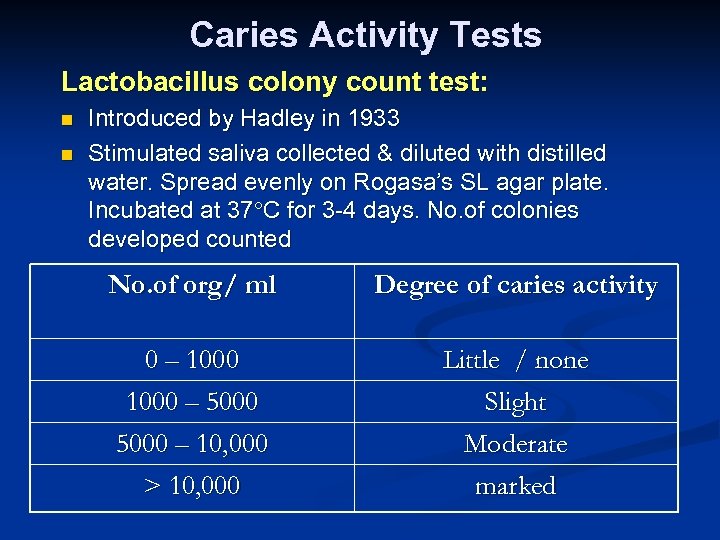 Caries Activity Tests Lactobacillus colony count test: n n Introduced by Hadley in 1933 Stimulated saliva collected & diluted with distilled water. Spread evenly on Rogasa’s SL agar plate. Incubated at 37 C for 3 -4 days. No. of colonies developed counted No. of org/ ml Degree of caries activity 0 – 1000 – 5000 Little / none Slight 5000 – 10, 000 > 10, 000 Moderate marked
Caries Activity Tests Lactobacillus colony count test: n n Introduced by Hadley in 1933 Stimulated saliva collected & diluted with distilled water. Spread evenly on Rogasa’s SL agar plate. Incubated at 37 C for 3 -4 days. No. of colonies developed counted No. of org/ ml Degree of caries activity 0 – 1000 – 5000 Little / none Slight 5000 – 10, 000 > 10, 000 Moderate marked
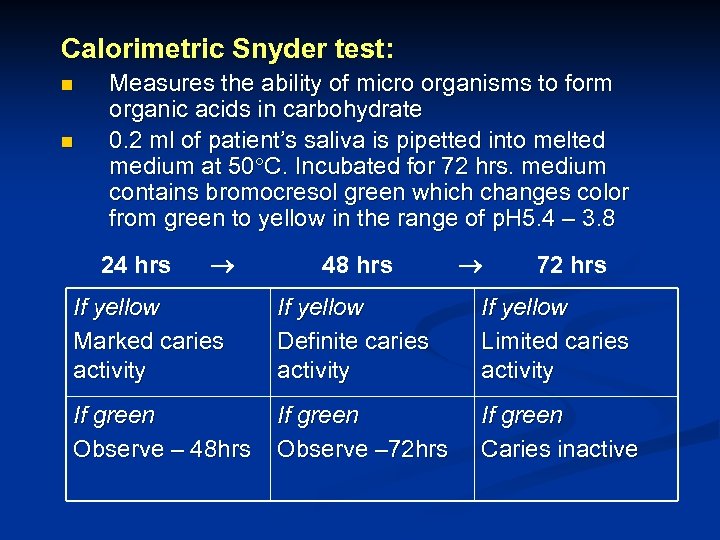 Calorimetric Snyder test: n n Measures the ability of micro organisms to form organic acids in carbohydrate 0. 2 ml of patient’s saliva is pipetted into melted medium at 50 C. Incubated for 72 hrs. medium contains bromocresol green which changes color from green to yellow in the range of p. H 5. 4 – 3. 8 24 hrs 48 hrs 72 hrs If yellow Marked caries activity If yellow Definite caries activity If yellow Limited caries activity If green Observe – 48 hrs If green Observe – 72 hrs If green Caries inactive
Calorimetric Snyder test: n n Measures the ability of micro organisms to form organic acids in carbohydrate 0. 2 ml of patient’s saliva is pipetted into melted medium at 50 C. Incubated for 72 hrs. medium contains bromocresol green which changes color from green to yellow in the range of p. H 5. 4 – 3. 8 24 hrs 48 hrs 72 hrs If yellow Marked caries activity If yellow Definite caries activity If yellow Limited caries activity If green Observe – 48 hrs If green Observe – 72 hrs If green Caries inactive
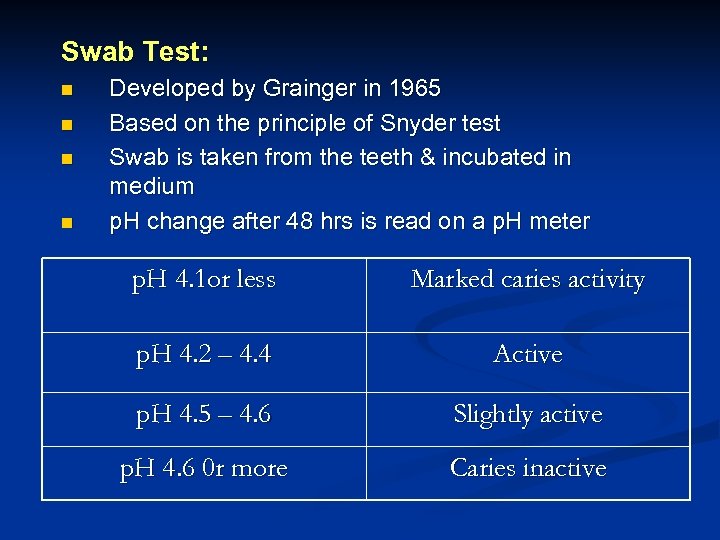 Swab Test: n n Developed by Grainger in 1965 Based on the principle of Snyder test Swab is taken from the teeth & incubated in medium p. H change after 48 hrs is read on a p. H meter p. H 4. 1 or less Marked caries activity p. H 4. 2 – 4. 4 Active p. H 4. 5 – 4. 6 Slightly active p. H 4. 6 0 r more Caries inactive
Swab Test: n n Developed by Grainger in 1965 Based on the principle of Snyder test Swab is taken from the teeth & incubated in medium p. H change after 48 hrs is read on a p. H meter p. H 4. 1 or less Marked caries activity p. H 4. 2 – 4. 4 Active p. H 4. 5 – 4. 6 Slightly active p. H 4. 6 0 r more Caries inactive
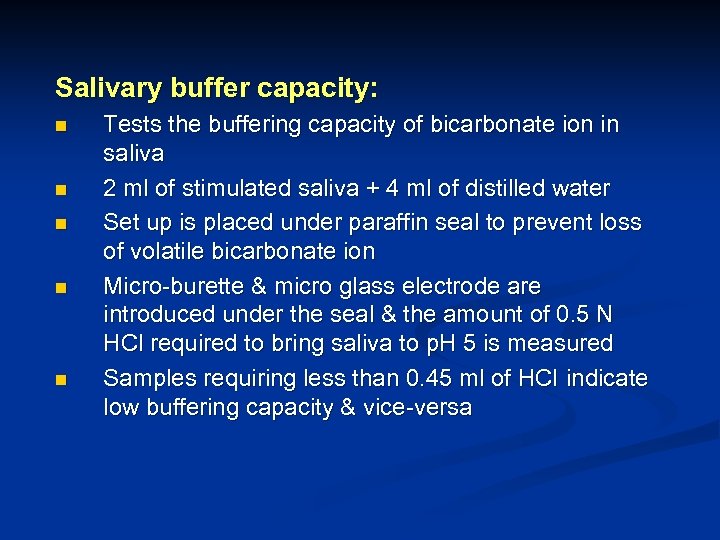 Salivary buffer capacity: n n n Tests the buffering capacity of bicarbonate ion in saliva 2 ml of stimulated saliva + 4 ml of distilled water Set up is placed under paraffin seal to prevent loss of volatile bicarbonate ion Micro-burette & micro glass electrode are introduced under the seal & the amount of 0. 5 N HCl required to bring saliva to p. H 5 is measured Samples requiring less than 0. 45 ml of HCl indicate low buffering capacity & vice-versa
Salivary buffer capacity: n n n Tests the buffering capacity of bicarbonate ion in saliva 2 ml of stimulated saliva + 4 ml of distilled water Set up is placed under paraffin seal to prevent loss of volatile bicarbonate ion Micro-burette & micro glass electrode are introduced under the seal & the amount of 0. 5 N HCl required to bring saliva to p. H 5 is measured Samples requiring less than 0. 45 ml of HCl indicate low buffering capacity & vice-versa
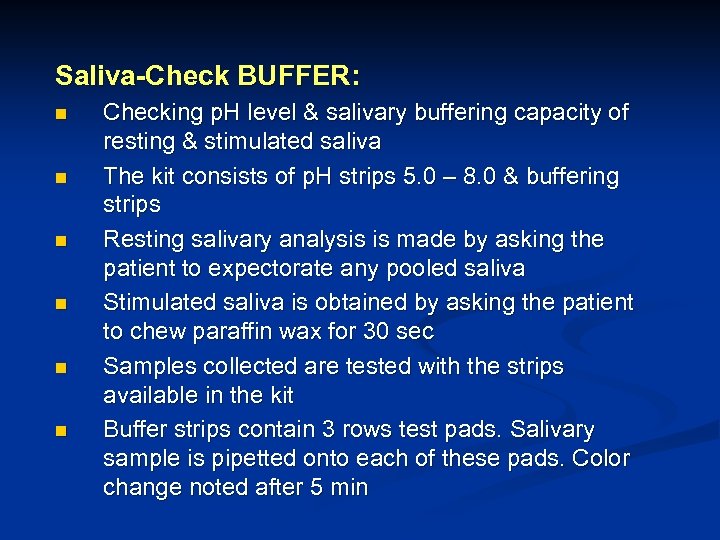 Saliva-Check BUFFER: n n n Checking p. H level & salivary buffering capacity of resting & stimulated saliva The kit consists of p. H strips 5. 0 – 8. 0 & buffering strips Resting salivary analysis is made by asking the patient to expectorate any pooled saliva Stimulated saliva is obtained by asking the patient to chew paraffin wax for 30 sec Samples collected are tested with the strips available in the kit Buffer strips contain 3 rows test pads. Salivary sample is pipetted onto each of these pads. Color change noted after 5 min
Saliva-Check BUFFER: n n n Checking p. H level & salivary buffering capacity of resting & stimulated saliva The kit consists of p. H strips 5. 0 – 8. 0 & buffering strips Resting salivary analysis is made by asking the patient to expectorate any pooled saliva Stimulated saliva is obtained by asking the patient to chew paraffin wax for 30 sec Samples collected are tested with the strips available in the kit Buffer strips contain 3 rows test pads. Salivary sample is pipetted onto each of these pads. Color change noted after 5 min
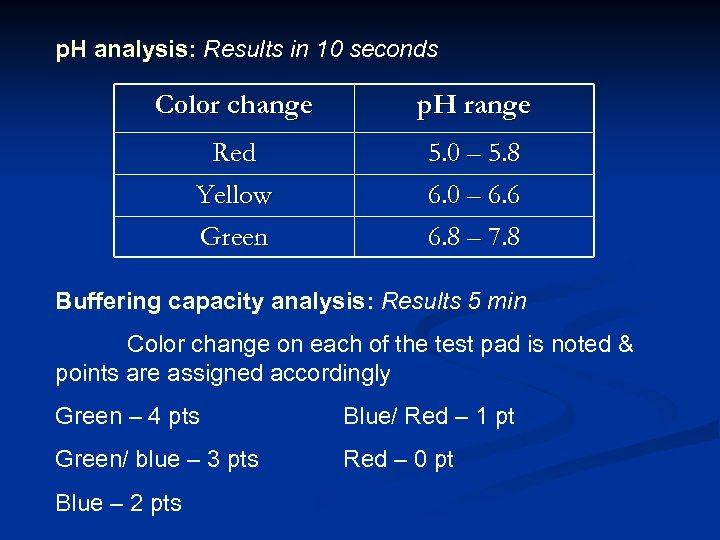 p. H analysis: Results in 10 seconds Color change p. H range Red Yellow Green 5. 0 – 5. 8 6. 0 – 6. 6 6. 8 – 7. 8 Buffering capacity analysis: Results 5 min Color change on each of the test pad is noted & points are assigned accordingly Green – 4 pts Blue/ Red – 1 pt Green/ blue – 3 pts Red – 0 pt Blue – 2 pts
p. H analysis: Results in 10 seconds Color change p. H range Red Yellow Green 5. 0 – 5. 8 6. 0 – 6. 6 6. 8 – 7. 8 Buffering capacity analysis: Results 5 min Color change on each of the test pad is noted & points are assigned accordingly Green – 4 pts Blue/ Red – 1 pt Green/ blue – 3 pts Red – 0 pt Blue – 2 pts
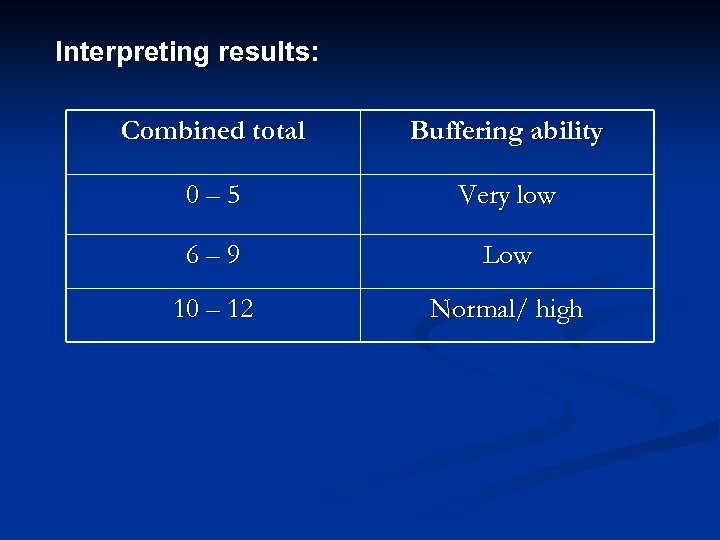 Interpreting results: Combined total Buffering ability 0– 5 Very low 6– 9 Low 10 – 12 Normal/ high
Interpreting results: Combined total Buffering ability 0– 5 Very low 6– 9 Low 10 – 12 Normal/ high
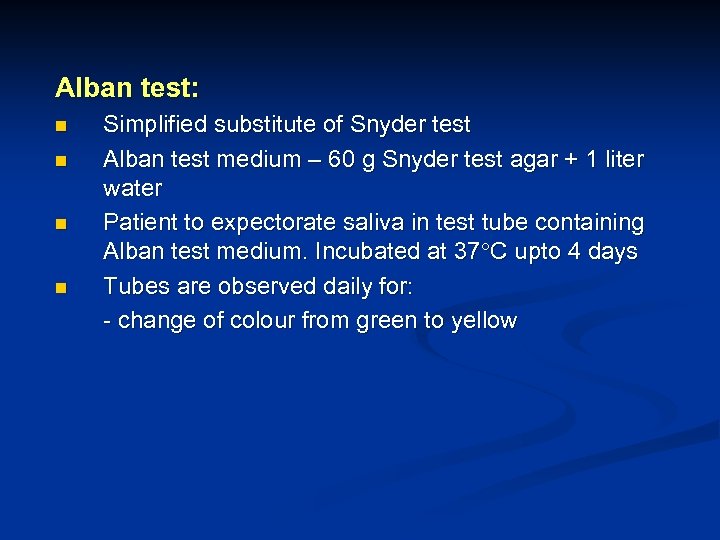 Alban test: n n Simplified substitute of Snyder test Alban test medium – 60 g Snyder test agar + 1 liter water Patient to expectorate saliva in test tube containing Alban test medium. Incubated at 37 C upto 4 days Tubes are observed daily for: - change of colour from green to yellow
Alban test: n n Simplified substitute of Snyder test Alban test medium – 60 g Snyder test agar + 1 liter water Patient to expectorate saliva in test tube containing Alban test medium. Incubated at 37 C upto 4 days Tubes are observed daily for: - change of colour from green to yellow
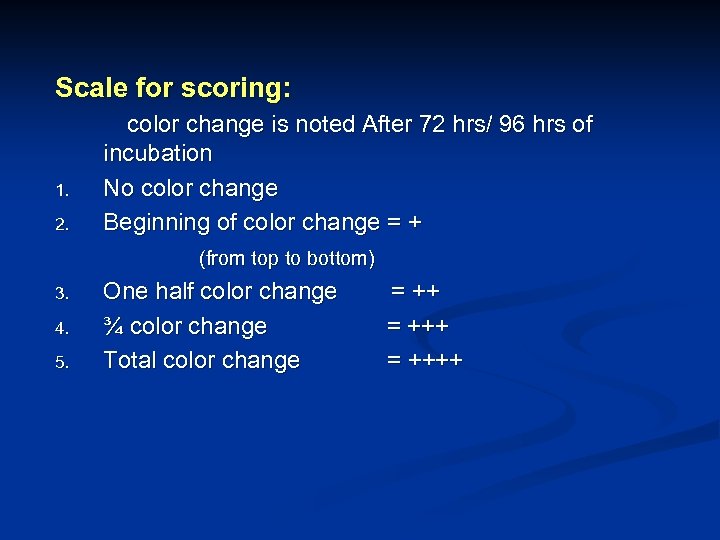 Scale for scoring: 1. 2. color change is noted After 72 hrs/ 96 hrs of incubation No color change Beginning of color change = + (from top to bottom) 3. 4. 5. One half color change ¾ color change Total color change = ++++
Scale for scoring: 1. 2. color change is noted After 72 hrs/ 96 hrs of incubation No color change Beginning of color change = + (from top to bottom) 3. 4. 5. One half color change ¾ color change Total color change = ++++
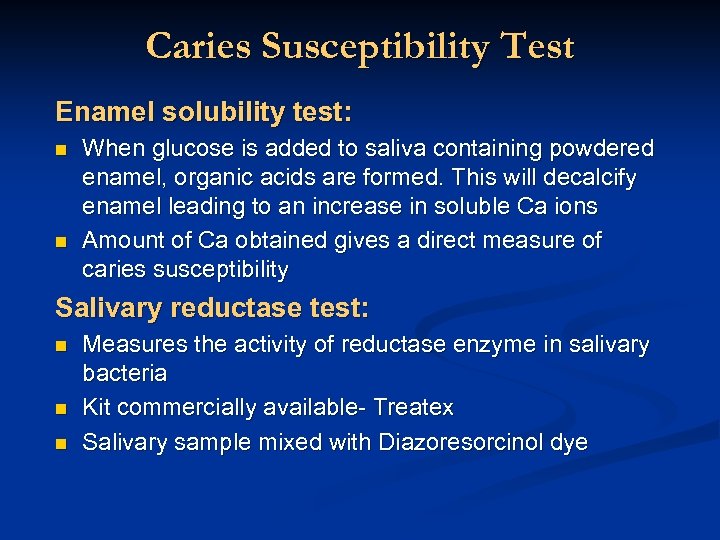 Caries Susceptibility Test Enamel solubility test: n n When glucose is added to saliva containing powdered enamel, organic acids are formed. This will decalcify enamel leading to an increase in soluble Ca ions Amount of Ca obtained gives a direct measure of caries susceptibility Salivary reductase test: n n n Measures the activity of reductase enzyme in salivary bacteria Kit commercially available- Treatex Salivary sample mixed with Diazoresorcinol dye
Caries Susceptibility Test Enamel solubility test: n n When glucose is added to saliva containing powdered enamel, organic acids are formed. This will decalcify enamel leading to an increase in soluble Ca ions Amount of Ca obtained gives a direct measure of caries susceptibility Salivary reductase test: n n n Measures the activity of reductase enzyme in salivary bacteria Kit commercially available- Treatex Salivary sample mixed with Diazoresorcinol dye
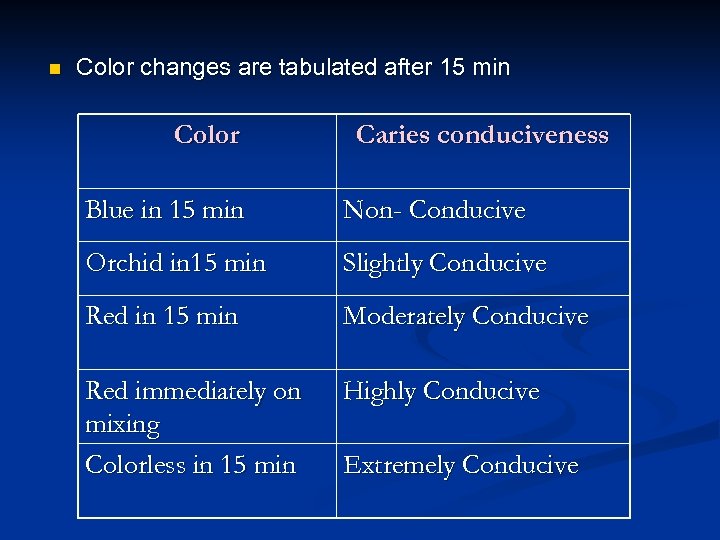 n Color changes are tabulated after 15 min Color Caries conduciveness Blue in 15 min Non- Conducive Orchid in 15 min Slightly Conducive Red in 15 min Moderately Conducive Red immediately on mixing Colorless in 15 min Highly Conducive Extremely Conducive
n Color changes are tabulated after 15 min Color Caries conduciveness Blue in 15 min Non- Conducive Orchid in 15 min Slightly Conducive Red in 15 min Moderately Conducive Red immediately on mixing Colorless in 15 min Highly Conducive Extremely Conducive
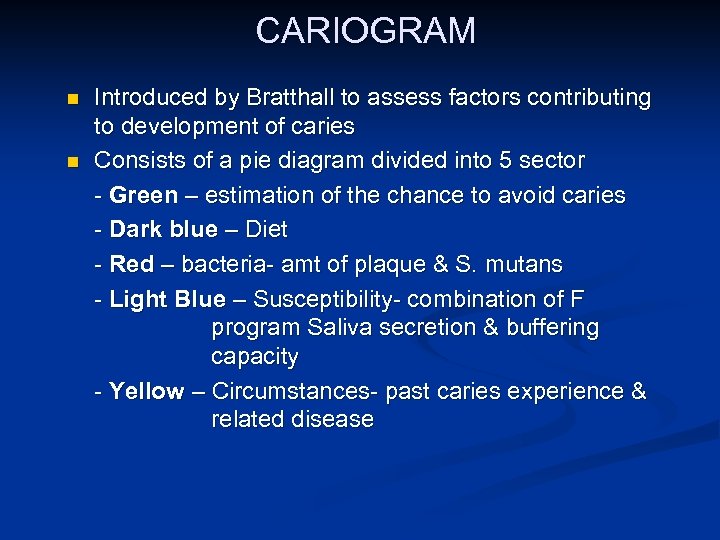 CARIOGRAM n n Introduced by Bratthall to assess factors contributing to development of caries Consists of a pie diagram divided into 5 sector - Green – estimation of the chance to avoid caries - Dark blue – Diet - Red – bacteria- amt of plaque & S. mutans - Light Blue – Susceptibility- combination of F program Saliva secretion & buffering capacity - Yellow – Circumstances- past caries experience & related disease
CARIOGRAM n n Introduced by Bratthall to assess factors contributing to development of caries Consists of a pie diagram divided into 5 sector - Green – estimation of the chance to avoid caries - Dark blue – Diet - Red – bacteria- amt of plaque & S. mutans - Light Blue – Susceptibility- combination of F program Saliva secretion & buffering capacity - Yellow – Circumstances- past caries experience & related disease


