c2bd06c566cffd36c808953ad28c86f4.ppt
- Количество слайдов: 75
 Care of The Post PTCA (Stent) Patient Chris Kolyvas MD
Care of The Post PTCA (Stent) Patient Chris Kolyvas MD
 Disclosures • I have nothing to disclose
Disclosures • I have nothing to disclose
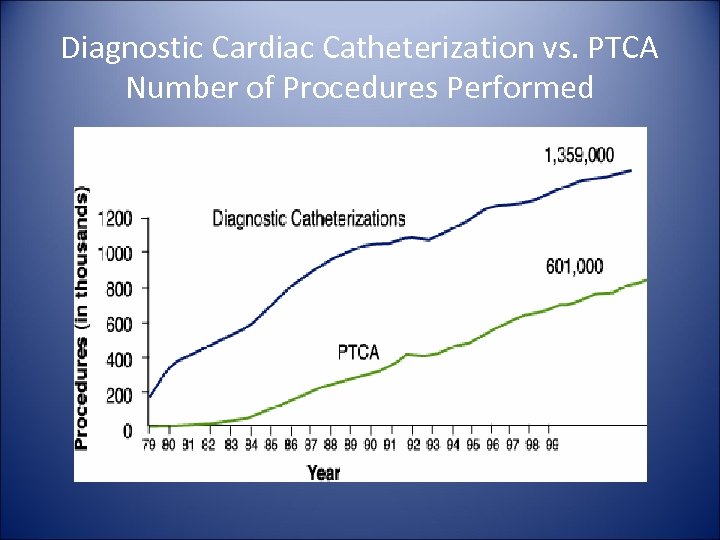 Diagnostic Cardiac Catheterization vs. PTCA Number of Procedures Performed
Diagnostic Cardiac Catheterization vs. PTCA Number of Procedures Performed
 Stents • Bare Metal – – Coil Slotted Tube Open/Closed Cell Covered • Drug Eluting – – Sirolimus (Cypher)-Rapamycin-2003 Everolimus (Endeavor)-2008 Zotarolimus (Promus & Xience)-2008 Paclitaxel (Taxus)-2004
Stents • Bare Metal – – Coil Slotted Tube Open/Closed Cell Covered • Drug Eluting – – Sirolimus (Cypher)-Rapamycin-2003 Everolimus (Endeavor)-2008 Zotarolimus (Promus & Xience)-2008 Paclitaxel (Taxus)-2004
 Why Use Stents? • Nearly Eliminated Abrupt Vessel Closure • Significantly Reduced Restenosis • Reduced Urgent CABG
Why Use Stents? • Nearly Eliminated Abrupt Vessel Closure • Significantly Reduced Restenosis • Reduced Urgent CABG
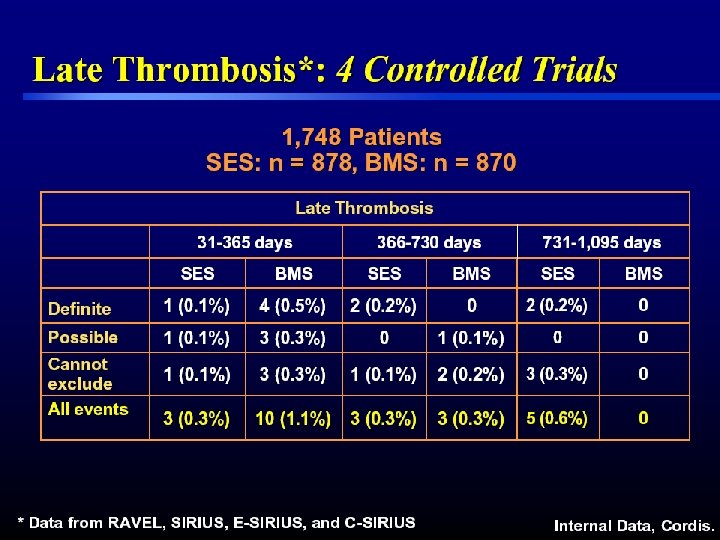
 DES • Reduce Restenosis—TLR~4 -5% a year • More Efficacious in Small Vessels, Long Lesions, Bifurcations, Diabetes • 4 Year Stent Thrombosis – ~1. 2% DES—Metaanalysis Data – 0. 6% BMS—Metaanalysis Data – Sirolimus vs Paclitaxel—Same – Everolimus (? Better)
DES • Reduce Restenosis—TLR~4 -5% a year • More Efficacious in Small Vessels, Long Lesions, Bifurcations, Diabetes • 4 Year Stent Thrombosis – ~1. 2% DES—Metaanalysis Data – 0. 6% BMS—Metaanalysis Data – Sirolimus vs Paclitaxel—Same – Everolimus (? Better)
 DES Use AMI Chronic renal failure Left main Bifurcation Calcification Diffuse disease Multistenting Diabetes “REAL WORLD” Ostium Saphenous graft Multivessel Unstable angina Long lesions Thrombus CTO
DES Use AMI Chronic renal failure Left main Bifurcation Calcification Diffuse disease Multistenting Diabetes “REAL WORLD” Ostium Saphenous graft Multivessel Unstable angina Long lesions Thrombus CTO
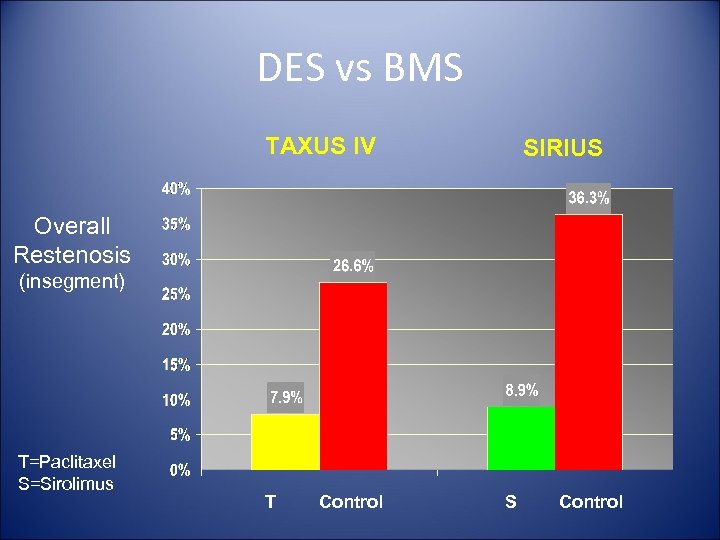 DES vs BMS TAXUS IV SIRIUS Overall Restenosis (insegment) T=Paclitaxel S=Sirolimus T Control S Control
DES vs BMS TAXUS IV SIRIUS Overall Restenosis (insegment) T=Paclitaxel S=Sirolimus T Control S Control
 Initial Evaluation of PCI Patient in Office • Check for Vascular Complications – Hematoma – Retroperitoneal Bleed – Pseudoaneurysm
Initial Evaluation of PCI Patient in Office • Check for Vascular Complications – Hematoma – Retroperitoneal Bleed – Pseudoaneurysm
 Vascular Complications • Insertion of vascular sheaths may produce groin or retroperitoneal hematomas • Groin hematoma presents with localized pain; lower extremity neurological symptoms are due to compression of the femoral nerve • Palpation of localized swelling or tenderness in the area, or loss of sensory or motor function is highly suggestive of a hematoma • Rates of major bleeding are decreasing (0. 7% to 1. 7%)
Vascular Complications • Insertion of vascular sheaths may produce groin or retroperitoneal hematomas • Groin hematoma presents with localized pain; lower extremity neurological symptoms are due to compression of the femoral nerve • Palpation of localized swelling or tenderness in the area, or loss of sensory or motor function is highly suggestive of a hematoma • Rates of major bleeding are decreasing (0. 7% to 1. 7%)
 Retroperitoneal Hematoma • Low incidence (0. 15% to 0. 44%) • Should be suspected in patients with unexplained hypotension and/or marked decrease in Hct • Pts may experience flank, abdominal or back pain– Note: absence of these symptoms does not exclude this condition
Retroperitoneal Hematoma • Low incidence (0. 15% to 0. 44%) • Should be suspected in patients with unexplained hypotension and/or marked decrease in Hct • Pts may experience flank, abdominal or back pain– Note: absence of these symptoms does not exclude this condition
 Retroperitoneal Hematoma • Diagnosis established by CT • Most treated conservatively; only 16% require surgery Kent, J Vasc Surg 1994; 20: 905 -10
Retroperitoneal Hematoma • Diagnosis established by CT • Most treated conservatively; only 16% require surgery Kent, J Vasc Surg 1994; 20: 905 -10
 Pseudoaneurysm (PSA) • Communication between femoral artery and overlying fibromuscular tissue, resulting in a blood filled cavity • Incidence ranges between 0. 5% to 6. 3% • Groin tenderness, a palpable pulsatile mass and/or new bruit in groin should prompt examination by Doppler flow imaging • Most large PSA can be treated by US guided compression, US guided thrombin injection, or surgical repair • New technology to treat PSA is percutaneous PTFE covered stent graft
Pseudoaneurysm (PSA) • Communication between femoral artery and overlying fibromuscular tissue, resulting in a blood filled cavity • Incidence ranges between 0. 5% to 6. 3% • Groin tenderness, a palpable pulsatile mass and/or new bruit in groin should prompt examination by Doppler flow imaging • Most large PSA can be treated by US guided compression, US guided thrombin injection, or surgical repair • New technology to treat PSA is percutaneous PTFE covered stent graft
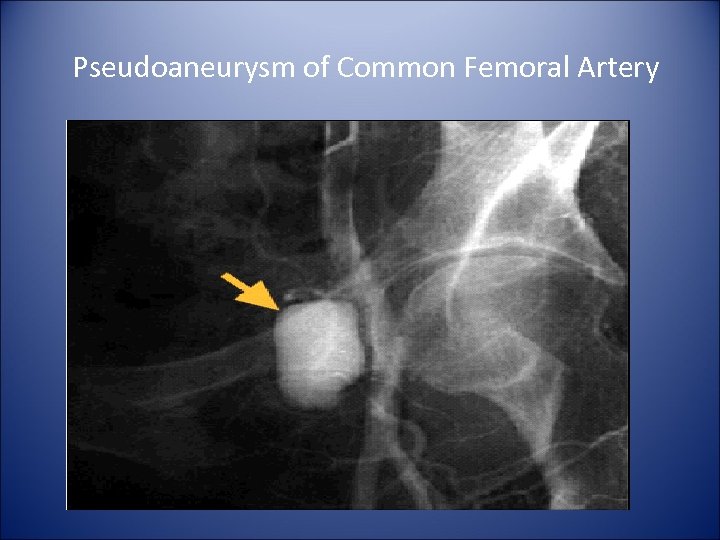 Pseudoaneurysm of Common Femoral Artery
Pseudoaneurysm of Common Femoral Artery
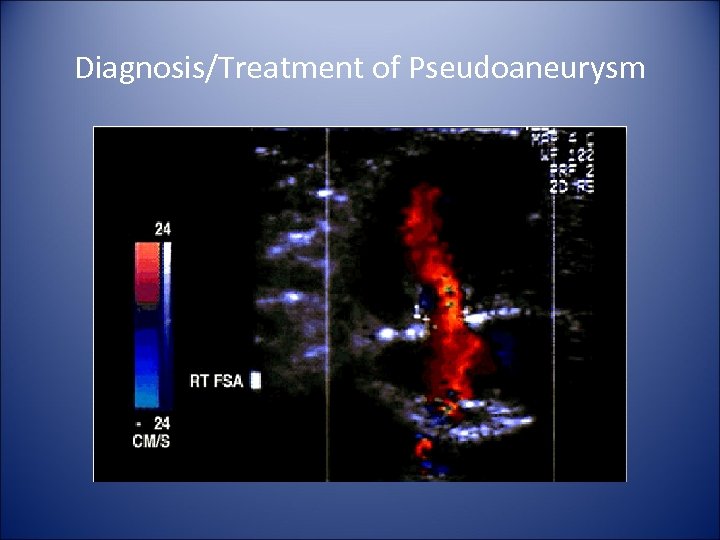 Diagnosis/Treatment of Pseudoaneurysm
Diagnosis/Treatment of Pseudoaneurysm
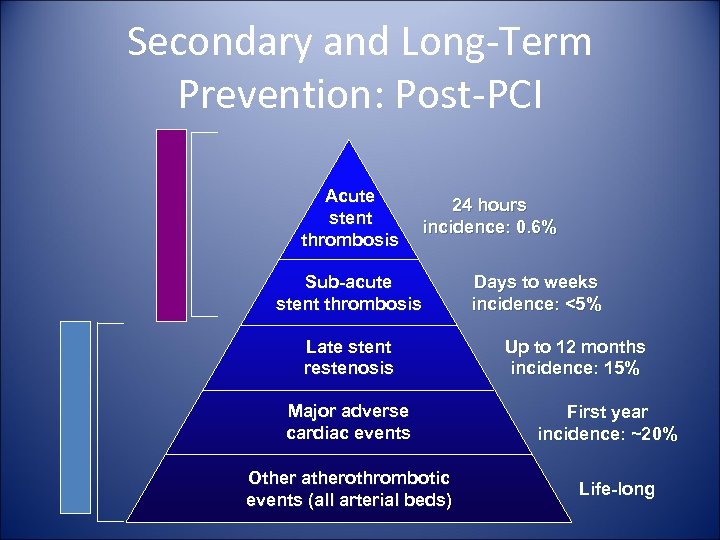 Long-term Prevention Short-term Prevention Secondary and Long-Term Prevention: Post-PCI Acute stent thrombosis 24 hours incidence: 0. 6% Sub-acute stent thrombosis Late stent restenosis Major adverse cardiac events Other atherothrombotic events (all arterial beds) Days to weeks incidence: <5% Up to 12 months incidence: 15% First year incidence: ~20% Life-long
Long-term Prevention Short-term Prevention Secondary and Long-Term Prevention: Post-PCI Acute stent thrombosis 24 hours incidence: 0. 6% Sub-acute stent thrombosis Late stent restenosis Major adverse cardiac events Other atherothrombotic events (all arterial beds) Days to weeks incidence: <5% Up to 12 months incidence: 15% First year incidence: ~20% Life-long
 STENT THROMBOSIS
STENT THROMBOSIS
 Stent Thrombosis is a Major Concern With BMS and DES • • Acute 24 Hours Subacute-1 -30 Days Late-30 -365 Days Very Late->365 Days
Stent Thrombosis is a Major Concern With BMS and DES • • Acute 24 Hours Subacute-1 -30 Days Late-30 -365 Days Very Late->365 Days
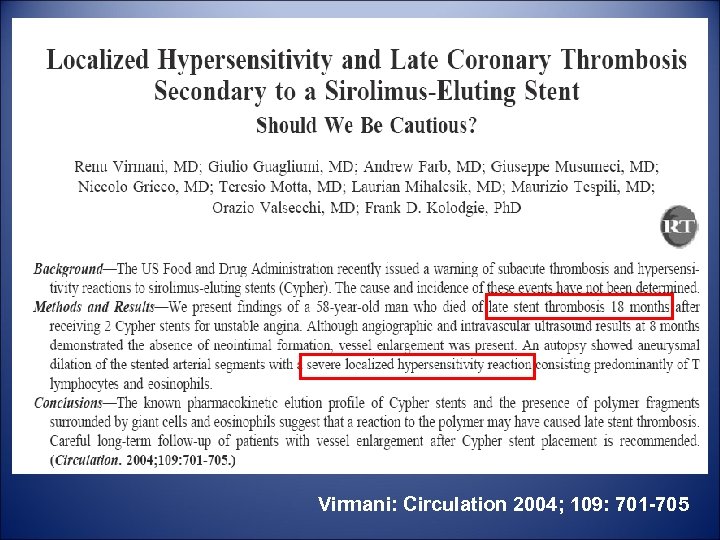 Virmani: Circulation 2004; 109: 701 -705
Virmani: Circulation 2004; 109: 701 -705
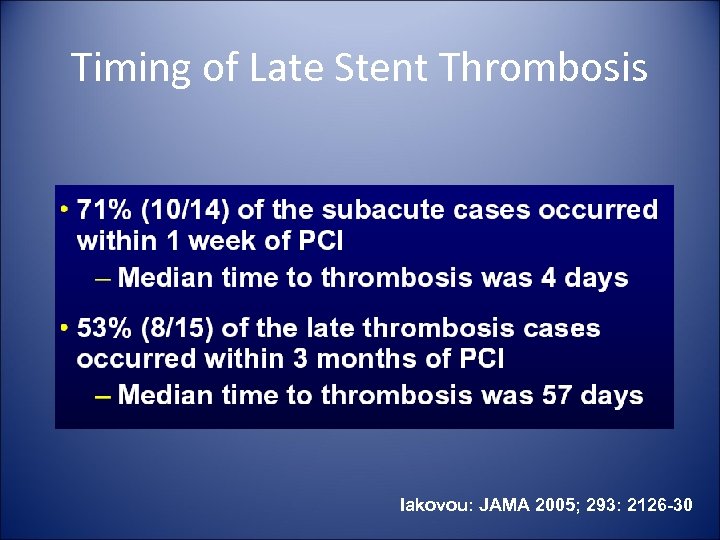 Timing of Late Stent Thrombosis Iakovou: JAMA 2005; 293: 2126 -30
Timing of Late Stent Thrombosis Iakovou: JAMA 2005; 293: 2126 -30
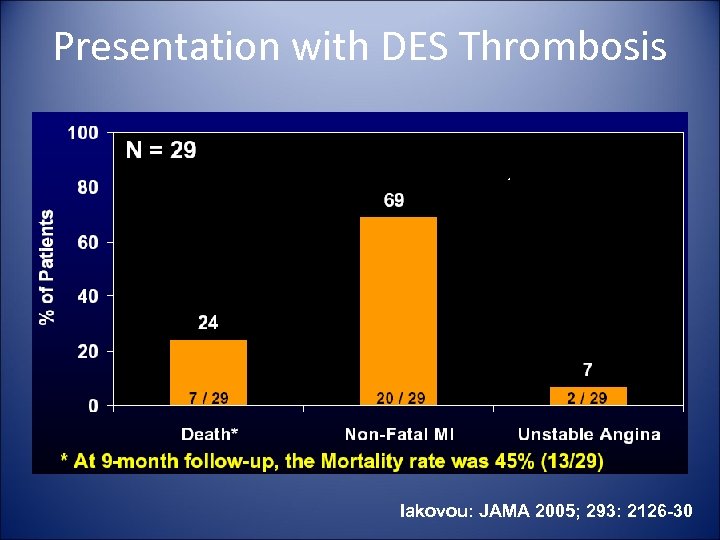 Presentation with DES Thrombosis Iakovou: JAMA 2005; 293: 2126 -30
Presentation with DES Thrombosis Iakovou: JAMA 2005; 293: 2126 -30
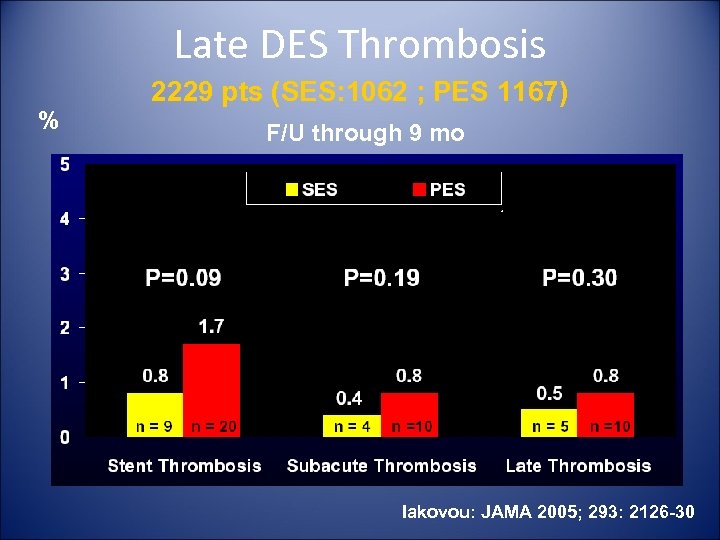 Late DES Thrombosis % 2229 pts (SES: 1062 ; PES 1167) F/U through 9 mo Iakovou: JAMA 2005; 293: 2126 -30
Late DES Thrombosis % 2229 pts (SES: 1062 ; PES 1167) F/U through 9 mo Iakovou: JAMA 2005; 293: 2126 -30
 Predictors of Late Stent Thrombosis • • Thienopyridine Discontinuation <6 months Insulin Treated Diabetes Lest Main Stenting Smoking Lesion Length >28 mm Multiple Stents Moderate to Severe Lesion Calcification
Predictors of Late Stent Thrombosis • • Thienopyridine Discontinuation <6 months Insulin Treated Diabetes Lest Main Stenting Smoking Lesion Length >28 mm Multiple Stents Moderate to Severe Lesion Calcification
 Predictors of Late Stent Thrombosis (cont) • • Reference Vessel Diameter <3 mm Ostial lesions Bifurcations Low EF Renal Failure Suboptimal Stent Result Platelet Nonresponsiveness
Predictors of Late Stent Thrombosis (cont) • • Reference Vessel Diameter <3 mm Ostial lesions Bifurcations Low EF Renal Failure Suboptimal Stent Result Platelet Nonresponsiveness
 Reasons for Discontinuation • • • Cost Lack of Education and F/U Older Age Bleeding/Bruising Clopidogrel has Lower Risk of Bleeding than ASA
Reasons for Discontinuation • • • Cost Lack of Education and F/U Older Age Bleeding/Bruising Clopidogrel has Lower Risk of Bleeding than ASA
 Methods to Prevent Premature Discontinuation • Discuss with Patient BEFORE Stenting • If Procedure Needed in Next 12 months, Consider BMS or Balloon PTCA • Educate Patients Post-Procedure • Instruct Patients to Contact their Physician Prior to Discontinue any Medication • Defer Elective Procedures if Possible
Methods to Prevent Premature Discontinuation • Discuss with Patient BEFORE Stenting • If Procedure Needed in Next 12 months, Consider BMS or Balloon PTCA • Educate Patients Post-Procedure • Instruct Patients to Contact their Physician Prior to Discontinue any Medication • Defer Elective Procedures if Possible
 Oral Antiplatelet Agents Post PCI (Stenting) • Aspirin • Thienopyridines – Ticlopidine – Clopidogrel – Prasugrel
Oral Antiplatelet Agents Post PCI (Stenting) • Aspirin • Thienopyridines – Ticlopidine – Clopidogrel – Prasugrel

 Ticlopidine • • • Initial Oral Thienopyridine 1% Risk of Severe Neutropenia Need CBC Monitoring Rare TTP Use in Patients Unable to Take Clopidogrel Full Antiplatelet Action Takes Several Days
Ticlopidine • • • Initial Oral Thienopyridine 1% Risk of Severe Neutropenia Need CBC Monitoring Rare TTP Use in Patients Unable to Take Clopidogrel Full Antiplatelet Action Takes Several Days
 Clopidogrel • Most Commonly Used Thienopyridine in U. S. • Onset of Full Effect within Hours of a Loading Dose • Indicated in Patients After NSTEMI, U. A. , STEMI
Clopidogrel • Most Commonly Used Thienopyridine in U. S. • Onset of Full Effect within Hours of a Loading Dose • Indicated in Patients After NSTEMI, U. A. , STEMI
 Prasugrel • Newest Thienopyridine • Triton TIMI-38 Trial—PCI – 13, 680 Patients Randomized to Clopidogrel vs. Prasugrel • CV Death, MI, Stroke were Significantly Reduced in Prasugrel Group (9. 9% vs. 12. 1%) • Reduced Stent Thrombosis (2. 4% vs. 1. 1%) • Major & Minor Bleeding was Significantly Increased in Prasugrel Group • Not FDA Approved yet
Prasugrel • Newest Thienopyridine • Triton TIMI-38 Trial—PCI – 13, 680 Patients Randomized to Clopidogrel vs. Prasugrel • CV Death, MI, Stroke were Significantly Reduced in Prasugrel Group (9. 9% vs. 12. 1%) • Reduced Stent Thrombosis (2. 4% vs. 1. 1%) • Major & Minor Bleeding was Significantly Increased in Prasugrel Group • Not FDA Approved yet
 Duration of Therapy Post PCI • Initially 2 -4 weeks • PCI Cure Trial changed that – 31% Decreased Risk of CV Death, MI or Stroke with long term Clopidogrel – No Increase in Major Bleeding – Increase in Minor Bleeding • Credo Trial Found Similar Long Term Benefit Post— PCI • Based on these trials it is rec. ASA & Clopidogrel Post Stenting & PCI go to at least 1 year
Duration of Therapy Post PCI • Initially 2 -4 weeks • PCI Cure Trial changed that – 31% Decreased Risk of CV Death, MI or Stroke with long term Clopidogrel – No Increase in Major Bleeding – Increase in Minor Bleeding • Credo Trial Found Similar Long Term Benefit Post— PCI • Based on these trials it is rec. ASA & Clopidogrel Post Stenting & PCI go to at least 1 year
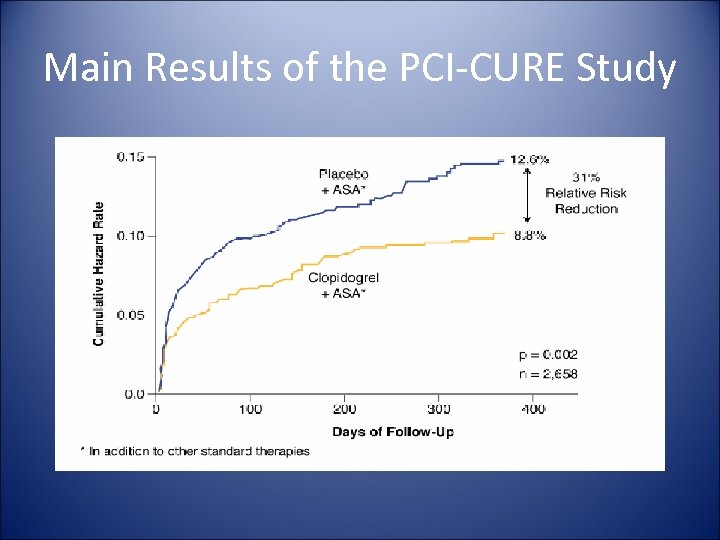 Main Results of the PCI-CURE Study
Main Results of the PCI-CURE Study
 Should Clopidogrel be used > 1 year in DES Patients? • Rationale is a small but increased risk of Late Stent Thrombosis in some DES Trials and Registries
Should Clopidogrel be used > 1 year in DES Patients? • Rationale is a small but increased risk of Late Stent Thrombosis in some DES Trials and Registries
 Nonresponsiveness to ASA/Clopidogrel • • • 746 Patients Complete platelet function Analysis Nonresponsive to ASA = 11. 5% Clopidogrel Nonresponse = 6% Both nonresponse= 6% Responsive to Both = 0%
Nonresponsiveness to ASA/Clopidogrel • • • 746 Patients Complete platelet function Analysis Nonresponsive to ASA = 11. 5% Clopidogrel Nonresponse = 6% Both nonresponse= 6% Responsive to Both = 0%
 Noncardiac Surgery Post PCI • Defer Elective Surgery for 1 Year • If Surgery Needed After 3 -6 months continue Low Dose Aspirin Periop. And Resume Clopidogrel Postop
Noncardiac Surgery Post PCI • Defer Elective Surgery for 1 Year • If Surgery Needed After 3 -6 months continue Low Dose Aspirin Periop. And Resume Clopidogrel Postop
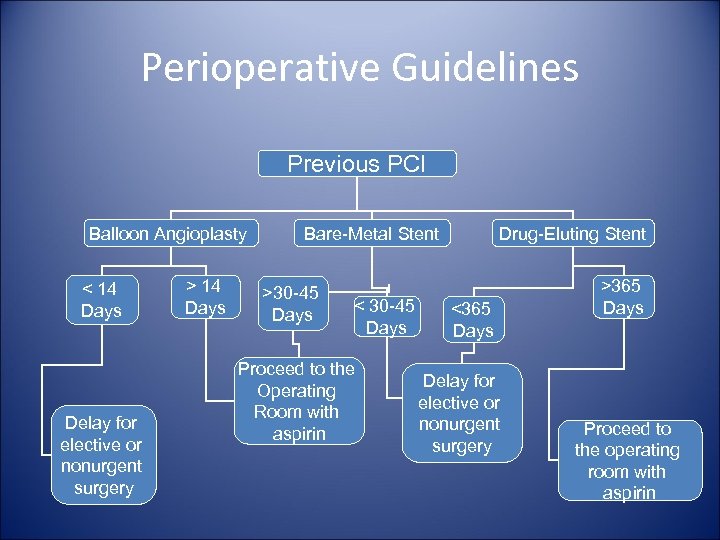 Perioperative Guidelines Previous PCI Balloon Angioplasty < 14 Days Delay for elective or nonurgent surgery > 14 Days Bare-Metal Stent >30 -45 Days < 30 -45 Days Proceed to the Operating Room with aspirin Drug-Eluting Stent <365 Days Delay for elective or nonurgent surgery >365 Days Proceed to the operating room with aspirin
Perioperative Guidelines Previous PCI Balloon Angioplasty < 14 Days Delay for elective or nonurgent surgery > 14 Days Bare-Metal Stent >30 -45 Days < 30 -45 Days Proceed to the Operating Room with aspirin Drug-Eluting Stent <365 Days Delay for elective or nonurgent surgery >365 Days Proceed to the operating room with aspirin
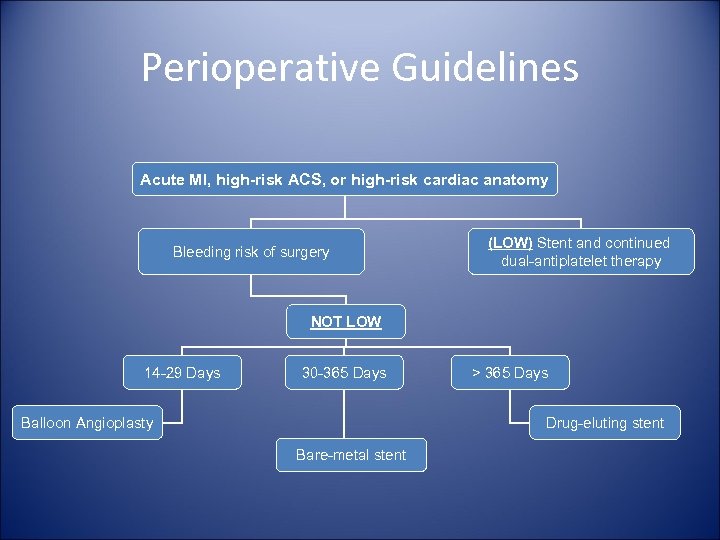 Perioperative Guidelines Acute MI, high-risk ACS, or high-risk cardiac anatomy Bleeding risk of surgery (LOW) Stent and continued dual-antiplatelet therapy NOT LOW 14 -29 Days 30 -365 Days Balloon Angioplasty > 365 Days Drug-eluting stent Bare-metal stent
Perioperative Guidelines Acute MI, high-risk ACS, or high-risk cardiac anatomy Bleeding risk of surgery (LOW) Stent and continued dual-antiplatelet therapy NOT LOW 14 -29 Days 30 -365 Days Balloon Angioplasty > 365 Days Drug-eluting stent Bare-metal stent
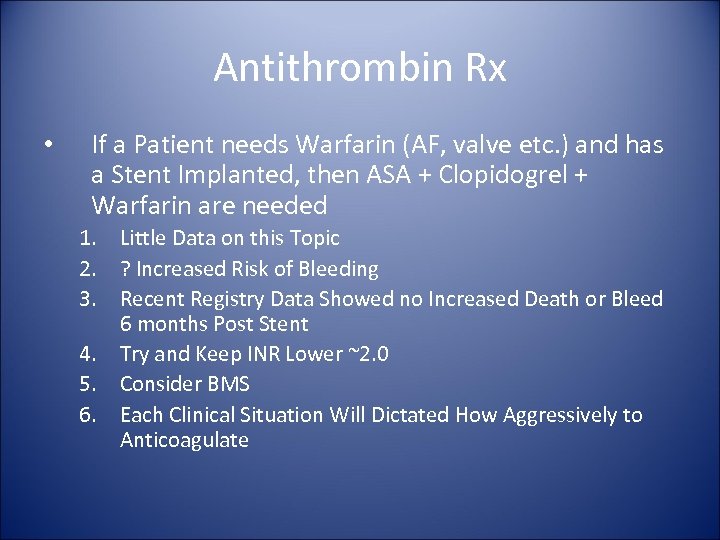 Antithrombin Rx • If a Patient needs Warfarin (AF, valve etc. ) and has a Stent Implanted, then ASA + Clopidogrel + Warfarin are needed 1. Little Data on this Topic 2. ? Increased Risk of Bleeding 3. Recent Registry Data Showed no Increased Death or Bleed 6 months Post Stent 4. Try and Keep INR Lower ~2. 0 5. Consider BMS 6. Each Clinical Situation Will Dictated How Aggressively to Anticoagulate
Antithrombin Rx • If a Patient needs Warfarin (AF, valve etc. ) and has a Stent Implanted, then ASA + Clopidogrel + Warfarin are needed 1. Little Data on this Topic 2. ? Increased Risk of Bleeding 3. Recent Registry Data Showed no Increased Death or Bleed 6 months Post Stent 4. Try and Keep INR Lower ~2. 0 5. Consider BMS 6. Each Clinical Situation Will Dictated How Aggressively to Anticoagulate
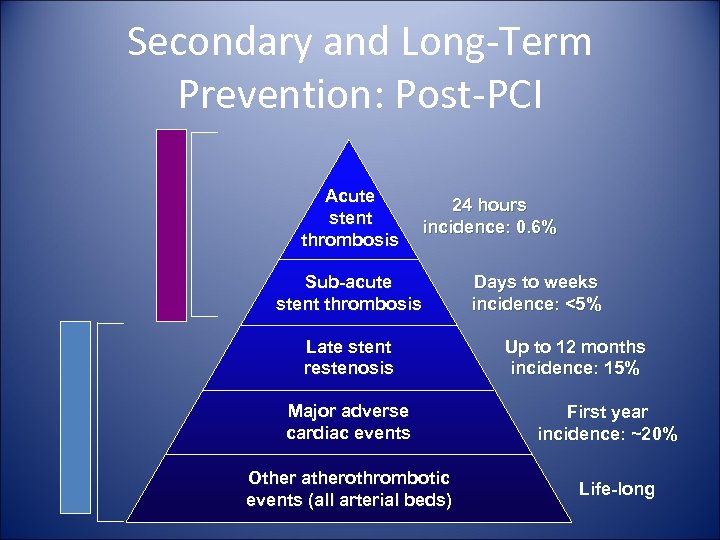 Long-term Prevention Short-term Prevention Secondary and Long-Term Prevention: Post-PCI Acute stent thrombosis 24 hours incidence: 0. 6% Sub-acute stent thrombosis Late stent restenosis Major adverse cardiac events Other atherothrombotic events (all arterial beds) Days to weeks incidence: <5% Up to 12 months incidence: 15% First year incidence: ~20% Life-long
Long-term Prevention Short-term Prevention Secondary and Long-Term Prevention: Post-PCI Acute stent thrombosis 24 hours incidence: 0. 6% Sub-acute stent thrombosis Late stent restenosis Major adverse cardiac events Other atherothrombotic events (all arterial beds) Days to weeks incidence: <5% Up to 12 months incidence: 15% First year incidence: ~20% Life-long
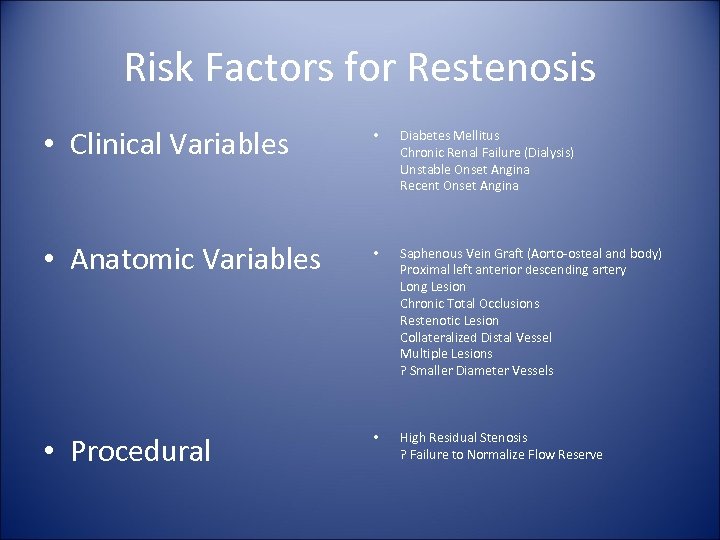 Risk Factors for Restenosis • Clinical Variables • Diabetes Mellitus Chronic Renal Failure (Dialysis) Unstable Onset Angina Recent Onset Angina • Anatomic Variables • Saphenous Vein Graft (Aorto-osteal and body) Proximal left anterior descending artery Long Lesion Chronic Total Occlusions Restenotic Lesion Collateralized Distal Vessel Multiple Lesions ? Smaller Diameter Vessels • Procedural • High Residual Stenosis ? Failure to Normalize Flow Reserve
Risk Factors for Restenosis • Clinical Variables • Diabetes Mellitus Chronic Renal Failure (Dialysis) Unstable Onset Angina Recent Onset Angina • Anatomic Variables • Saphenous Vein Graft (Aorto-osteal and body) Proximal left anterior descending artery Long Lesion Chronic Total Occlusions Restenotic Lesion Collateralized Distal Vessel Multiple Lesions ? Smaller Diameter Vessels • Procedural • High Residual Stenosis ? Failure to Normalize Flow Reserve
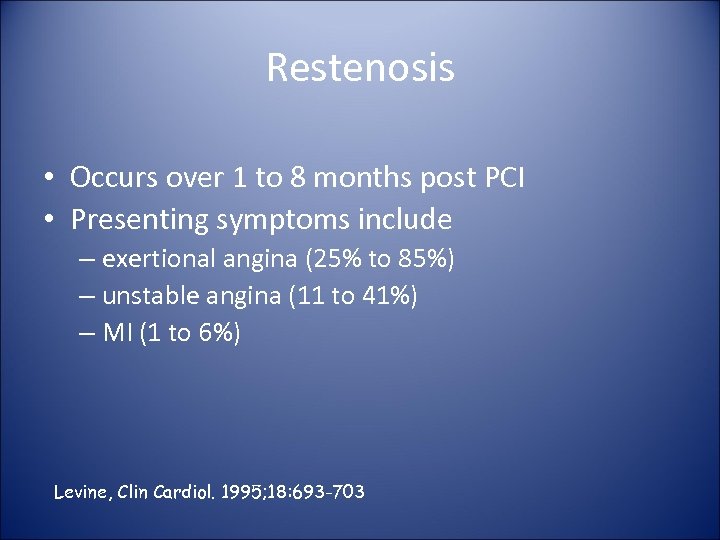 Restenosis • Occurs over 1 to 8 months post PCI • Presenting symptoms include – exertional angina (25% to 85%) – unstable angina (11 to 41%) – MI (1 to 6%) Levine, Clin Cardiol. 1995; 18: 693 -703
Restenosis • Occurs over 1 to 8 months post PCI • Presenting symptoms include – exertional angina (25% to 85%) – unstable angina (11 to 41%) – MI (1 to 6%) Levine, Clin Cardiol. 1995; 18: 693 -703
 Evaluation for Restenosis • Prognosis for asymptomatic or “silent restenosis” is generally favorable • Routine periodic monitoring is not beneficial, indicated or recommended* • Hi risk pts should be followed: ↓ LVEF, multivessel CPD, PLAD lesion, hx of sudden death, DM and hazardous occupation Ritchie, J. Am Coll Cardiol. 1995; 25” 521 -47
Evaluation for Restenosis • Prognosis for asymptomatic or “silent restenosis” is generally favorable • Routine periodic monitoring is not beneficial, indicated or recommended* • Hi risk pts should be followed: ↓ LVEF, multivessel CPD, PLAD lesion, hx of sudden death, DM and hazardous occupation Ritchie, J. Am Coll Cardiol. 1995; 25” 521 -47
 Risk Factor Modification • • • Smoking Cessation Cardiac Rehab & Exercise Lipid Lowering HTN Treatment Weight Management
Risk Factor Modification • • • Smoking Cessation Cardiac Rehab & Exercise Lipid Lowering HTN Treatment Weight Management
 Smoking Independent Risk Factor for CAD 60% of Smokers Do Not Believe this Incidence of MI is 3 -6 x increased Patients with prior CAS have Increased risk of Death, Sudden Death, and Reinfarction • Pathogenesis— LDL + TG + HDL • • – Impaired Endothelial Function—Dose Related – Enhanced Prothrombotic State
Smoking Independent Risk Factor for CAD 60% of Smokers Do Not Believe this Incidence of MI is 3 -6 x increased Patients with prior CAS have Increased risk of Death, Sudden Death, and Reinfarction • Pathogenesis— LDL + TG + HDL • • – Impaired Endothelial Function—Dose Related – Enhanced Prothrombotic State
 Mediators • Nicotine—Sympathetic Neural Stimulation ( BP + HR + O 2 Demand increases ischemia) • CO—binds to Hb and Increases Ischemia, Ventricular Dysfunction • Oxygen Free Radicals—Atherosclerosis development
Mediators • Nicotine—Sympathetic Neural Stimulation ( BP + HR + O 2 Demand increases ischemia) • CO—binds to Hb and Increases Ischemia, Ventricular Dysfunction • Oxygen Free Radicals—Atherosclerosis development
 Post-PCI—Smoking • Death— 1. 75 x • Q wave MI— 2 x • 50% Decreased Reinfarction, Sudden Death & Mortality if Patients Quit
Post-PCI—Smoking • Death— 1. 75 x • Q wave MI— 2 x • 50% Decreased Reinfarction, Sudden Death & Mortality if Patients Quit
 Cigarette Smoking Recommendations Goal: Complete Cessation and No Exposure to Environmental Tobacco Smoke • Ask about tobacco use status at every visit. • Advise every tobacco user to quit. • Assess the tobacco user’s willingness to quit. • Assist by counseling and developing a plan for quitting. • Arrange follow-up, referral to special programs, or pharmacotherapy (including nicotine replacement and bupropion. • Urge avoidance of exposure to environmental tobacco smoke at work and home.
Cigarette Smoking Recommendations Goal: Complete Cessation and No Exposure to Environmental Tobacco Smoke • Ask about tobacco use status at every visit. • Advise every tobacco user to quit. • Assess the tobacco user’s willingness to quit. • Assist by counseling and developing a plan for quitting. • Arrange follow-up, referral to special programs, or pharmacotherapy (including nicotine replacement and bupropion. • Urge avoidance of exposure to environmental tobacco smoke at work and home.
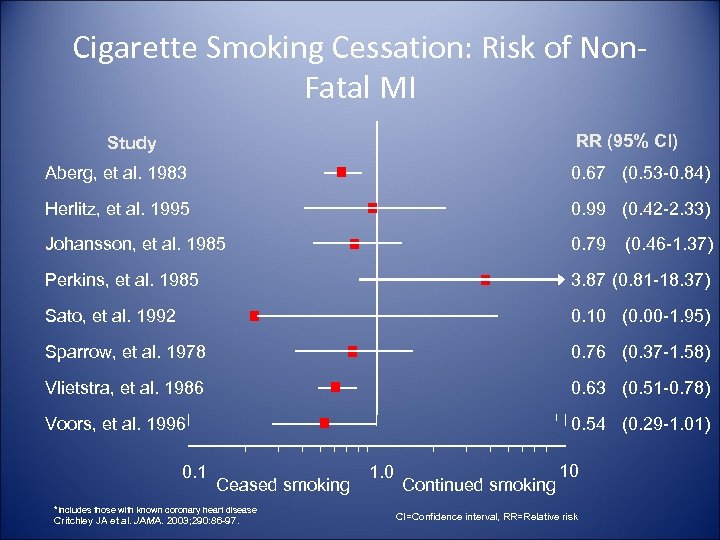 Cigarette Smoking Cessation: Risk of Non. Fatal MI RR (95% Cl) Study Aberg, et al. 1983 0. 67 (0. 53 -0. 84) Herlitz, et al. 1995 0. 99 (0. 42 -2. 33) Johansson, et al. 1985 0. 79 Perkins, et al. 1985 3. 87 (0. 81 -18. 37) Sato, et al. 1992 0. 10 (0. 00 -1. 95) Sparrow, et al. 1978 0. 76 (0. 37 -1. 58) Vlietstra, et al. 1986 0. 63 (0. 51 -0. 78) Voors, et al. 1996 0. 54 (0. 29 -1. 01) 0. 1 Ceased smoking *Includes those with known coronary heart disease Critchley JA et al. JAMA. 2003; 290: 86 -97. 1. 0 Continued smoking 10 CI=Confidence interval, RR=Relative risk (0. 46 -1. 37)
Cigarette Smoking Cessation: Risk of Non. Fatal MI RR (95% Cl) Study Aberg, et al. 1983 0. 67 (0. 53 -0. 84) Herlitz, et al. 1995 0. 99 (0. 42 -2. 33) Johansson, et al. 1985 0. 79 Perkins, et al. 1985 3. 87 (0. 81 -18. 37) Sato, et al. 1992 0. 10 (0. 00 -1. 95) Sparrow, et al. 1978 0. 76 (0. 37 -1. 58) Vlietstra, et al. 1986 0. 63 (0. 51 -0. 78) Voors, et al. 1996 0. 54 (0. 29 -1. 01) 0. 1 Ceased smoking *Includes those with known coronary heart disease Critchley JA et al. JAMA. 2003; 290: 86 -97. 1. 0 Continued smoking 10 CI=Confidence interval, RR=Relative risk (0. 46 -1. 37)
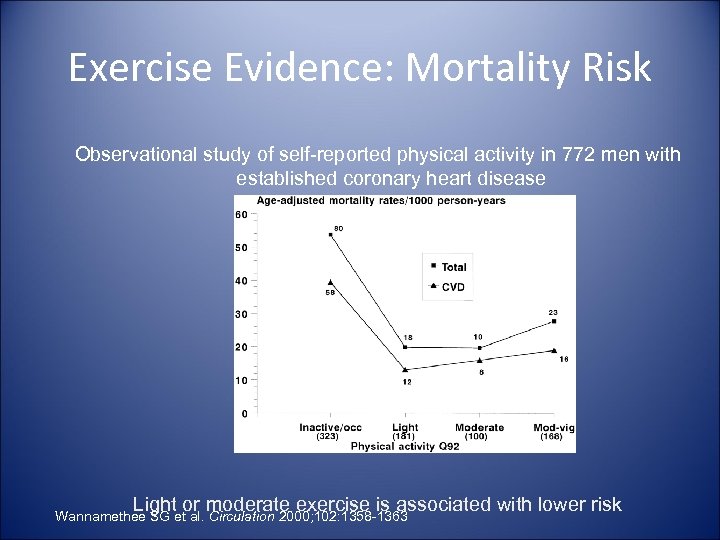 Exercise Evidence: Mortality Risk Observational study of self-reported physical activity in 772 men with established coronary heart disease Light or moderate exercise is associated with lower risk Wannamethee SG et al. Circulation 2000; 102: 1358 -1363
Exercise Evidence: Mortality Risk Observational study of self-reported physical activity in 772 men with established coronary heart disease Light or moderate exercise is associated with lower risk Wannamethee SG et al. Circulation 2000; 102: 1358 -1363
 Cardiac Rehab • Indications – Chronic Angina – Recent MI – Post PCI – Post Surgery • ACC/AHA Recommends a Symptom Limited Exercise Stress Test • Exercise 3 -5 x/week for 30 -60 mins • Target HR = 85% (220 -age)
Cardiac Rehab • Indications – Chronic Angina – Recent MI – Post PCI – Post Surgery • ACC/AHA Recommends a Symptom Limited Exercise Stress Test • Exercise 3 -5 x/week for 30 -60 mins • Target HR = 85% (220 -age)
 Blood Pressure Control Recommendations Goal: <140/90 mm Hg or <130/80 if diabetes or chronic kidney disease Blood pressure 120/80 mm Hg or greater: · Initiate or maintain lifestyle modification: weight control, increased physical activity, alcohol moderation, sodium reduction, and increased consumption of fresh fruits vegetables and low fat dairy products Blood pressure 140/90 mm Hg or greater (or 130/80 or greater for chronic kidney disease or diabetes) · As tolerated, add blood pressure medication, treating initially with beta blockers and/or ACE inhibitors with addition of other drugs such as thiazides as needed to achieve goal blood pressure
Blood Pressure Control Recommendations Goal: <140/90 mm Hg or <130/80 if diabetes or chronic kidney disease Blood pressure 120/80 mm Hg or greater: · Initiate or maintain lifestyle modification: weight control, increased physical activity, alcohol moderation, sodium reduction, and increased consumption of fresh fruits vegetables and low fat dairy products Blood pressure 140/90 mm Hg or greater (or 130/80 or greater for chronic kidney disease or diabetes) · As tolerated, add blood pressure medication, treating initially with beta blockers and/or ACE inhibitors with addition of other drugs such as thiazides as needed to achieve goal blood pressure
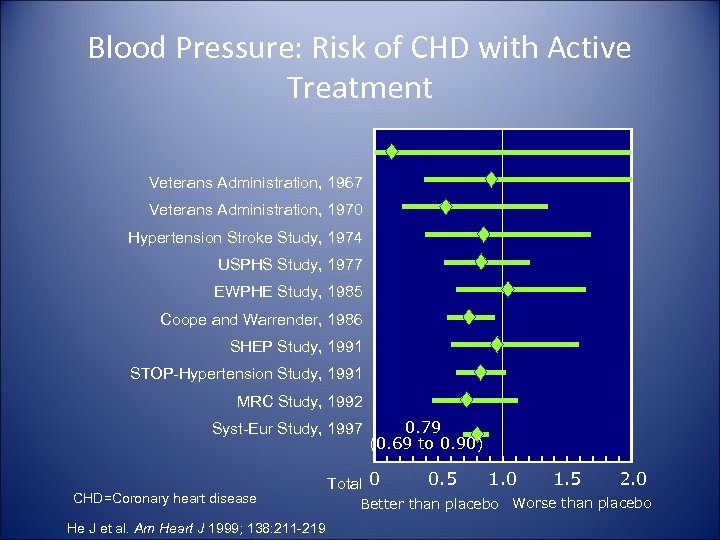 Blood Pressure: Risk of CHD with Active Treatment Veterans Administration, 1967 Veterans Administration, 1970 Hypertension Stroke Study, 1974 USPHS Study, 1977 EWPHE Study, 1985 Coope and Warrender, 1986 SHEP Study, 1991 STOP-Hypertension Study, 1991 MRC Study, 1992 Syst-Eur Study, 1997 CHD=Coronary heart disease He J et al. Am Heart J 1999; 138: 211 -219 0. 79 (0. 69 to 0. 90) Total 0 0. 5 1. 0 1. 5 2. 0 Better than placebo Worse than placebo
Blood Pressure: Risk of CHD with Active Treatment Veterans Administration, 1967 Veterans Administration, 1970 Hypertension Stroke Study, 1974 USPHS Study, 1977 EWPHE Study, 1985 Coope and Warrender, 1986 SHEP Study, 1991 STOP-Hypertension Study, 1991 MRC Study, 1992 Syst-Eur Study, 1997 CHD=Coronary heart disease He J et al. Am Heart J 1999; 138: 211 -219 0. 79 (0. 69 to 0. 90) Total 0 0. 5 1. 0 1. 5 2. 0 Better than placebo Worse than placebo
 Lipid Lowering • For every 1% Reduction in Total Cholesterol there is 1% decreased total Mortality and 1. 5% decreased CV Mortality • 1% CV Events for every 1 -mg/dl in LDL-C
Lipid Lowering • For every 1% Reduction in Total Cholesterol there is 1% decreased total Mortality and 1. 5% decreased CV Mortality • 1% CV Events for every 1 -mg/dl in LDL-C
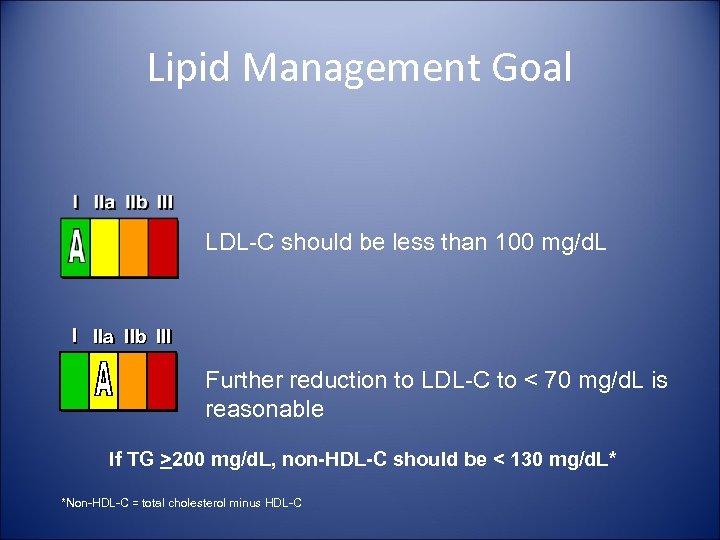 Lipid Management Goal LDL-C should be less than 100 mg/d. L I IIa IIb III Further reduction to LDL-C to < 70 mg/d. L is reasonable If TG >200 mg/d. L, non-HDL-C should be < 130 mg/d. L* *Non-HDL-C = total cholesterol minus HDL-C
Lipid Management Goal LDL-C should be less than 100 mg/d. L I IIa IIb III Further reduction to LDL-C to < 70 mg/d. L is reasonable If TG >200 mg/d. L, non-HDL-C should be < 130 mg/d. L* *Non-HDL-C = total cholesterol minus HDL-C
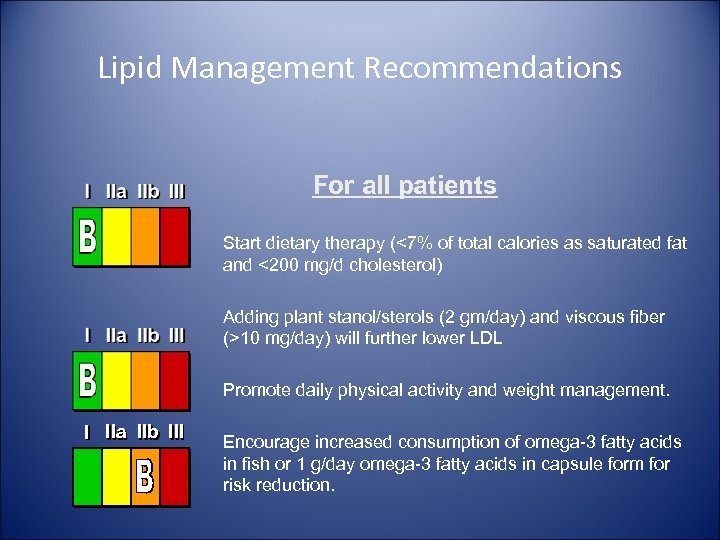 Lipid Management Recommendations For all patients Start dietary therapy (<7% of total calories as saturated fat and <200 mg/d cholesterol) Adding plant stanol/sterols (2 gm/day) and viscous fiber (>10 mg/day) will further lower LDL Promote daily physical activity and weight management. I IIa IIb III Encourage increased consumption of omega-3 fatty acids in fish or 1 g/day omega-3 fatty acids in capsule form for risk reduction.
Lipid Management Recommendations For all patients Start dietary therapy (<7% of total calories as saturated fat and <200 mg/d cholesterol) Adding plant stanol/sterols (2 gm/day) and viscous fiber (>10 mg/day) will further lower LDL Promote daily physical activity and weight management. I IIa IIb III Encourage increased consumption of omega-3 fatty acids in fish or 1 g/day omega-3 fatty acids in capsule form for risk reduction.
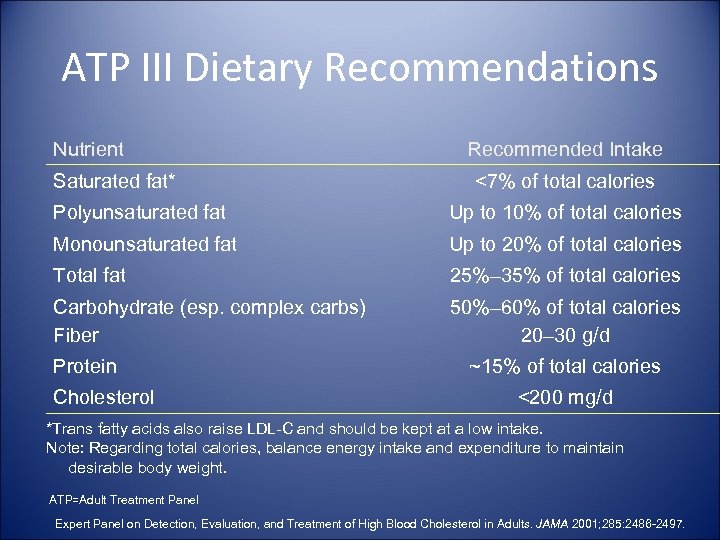 ATP III Dietary Recommendations Nutrient Saturated fat* Recommended Intake <7% of total calories Polyunsaturated fat Up to 10% of total calories Monounsaturated fat Up to 20% of total calories Total fat 25%– 35% of total calories Carbohydrate (esp. complex carbs) Fiber 50%– 60% of total calories 20– 30 g/d Protein Cholesterol ~15% of total calories <200 mg/d *Trans fatty acids also raise LDL-C and should be kept at a low intake. Note: Regarding total calories, balance energy intake and expenditure to maintain desirable body weight. ATP=Adult Treatment Panel Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. JAMA 2001; 285: 2486 -2497.
ATP III Dietary Recommendations Nutrient Saturated fat* Recommended Intake <7% of total calories Polyunsaturated fat Up to 10% of total calories Monounsaturated fat Up to 20% of total calories Total fat 25%– 35% of total calories Carbohydrate (esp. complex carbs) Fiber 50%– 60% of total calories 20– 30 g/d Protein Cholesterol ~15% of total calories <200 mg/d *Trans fatty acids also raise LDL-C and should be kept at a low intake. Note: Regarding total calories, balance energy intake and expenditure to maintain desirable body weight. ATP=Adult Treatment Panel Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. JAMA 2001; 285: 2486 -2497.
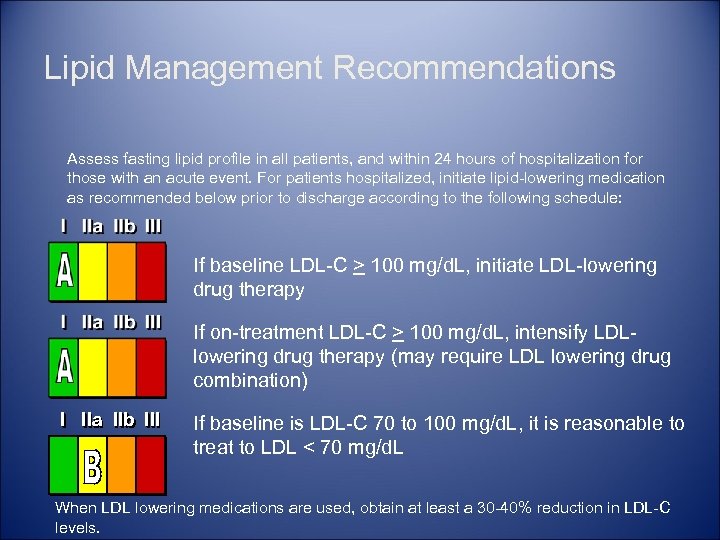 Lipid Management Recommendations Assess fasting lipid profile in all patients, and within 24 hours of hospitalization for those with an acute event. For patients hospitalized, initiate lipid-lowering medication as recommended below prior to discharge according to the following schedule: If baseline LDL-C > 100 mg/d. L, initiate LDL-lowering drug therapy If on-treatment LDL-C > 100 mg/d. L, intensify LDLlowering drug therapy (may require LDL lowering drug combination) I IIa IIb III If baseline is LDL-C 70 to 100 mg/d. L, it is reasonable to treat to LDL < 70 mg/d. L When LDL lowering medications are used, obtain at least a 30 -40% reduction in LDL-C levels.
Lipid Management Recommendations Assess fasting lipid profile in all patients, and within 24 hours of hospitalization for those with an acute event. For patients hospitalized, initiate lipid-lowering medication as recommended below prior to discharge according to the following schedule: If baseline LDL-C > 100 mg/d. L, initiate LDL-lowering drug therapy If on-treatment LDL-C > 100 mg/d. L, intensify LDLlowering drug therapy (may require LDL lowering drug combination) I IIa IIb III If baseline is LDL-C 70 to 100 mg/d. L, it is reasonable to treat to LDL < 70 mg/d. L When LDL lowering medications are used, obtain at least a 30 -40% reduction in LDL-C levels.
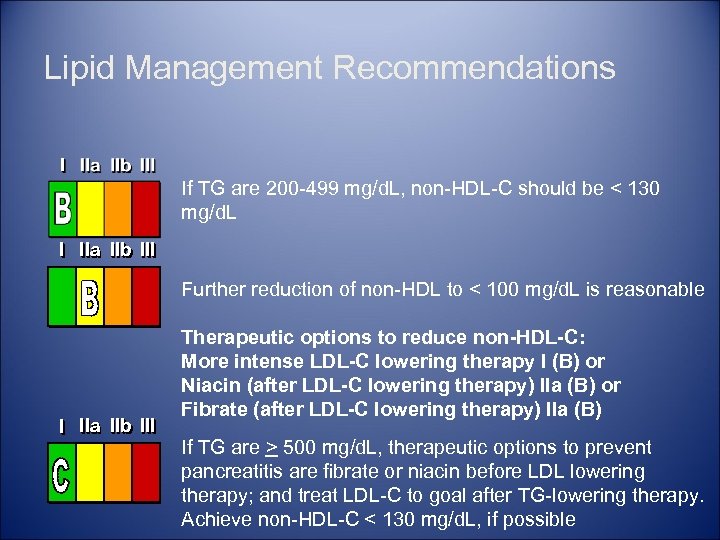 Lipid Management Recommendations If TG are 200 -499 mg/d. L, non-HDL-C should be < 130 mg/d. L I IIa IIb III Further reduction of non-HDL to < 100 mg/d. L is reasonable I IIa IIb III Therapeutic options to reduce non-HDL-C: More intense LDL-C lowering therapy I (B) or Niacin (after LDL-C lowering therapy) IIa (B) or Fibrate (after LDL-C lowering therapy) IIa (B) If TG are > 500 mg/d. L, therapeutic options to prevent pancreatitis are fibrate or niacin before LDL lowering therapy; and treat LDL-C to goal after TG-lowering therapy. Achieve non-HDL-C < 130 mg/d. L, if possible
Lipid Management Recommendations If TG are 200 -499 mg/d. L, non-HDL-C should be < 130 mg/d. L I IIa IIb III Further reduction of non-HDL to < 100 mg/d. L is reasonable I IIa IIb III Therapeutic options to reduce non-HDL-C: More intense LDL-C lowering therapy I (B) or Niacin (after LDL-C lowering therapy) IIa (B) or Fibrate (after LDL-C lowering therapy) IIa (B) If TG are > 500 mg/d. L, therapeutic options to prevent pancreatitis are fibrate or niacin before LDL lowering therapy; and treat LDL-C to goal after TG-lowering therapy. Achieve non-HDL-C < 130 mg/d. L, if possible
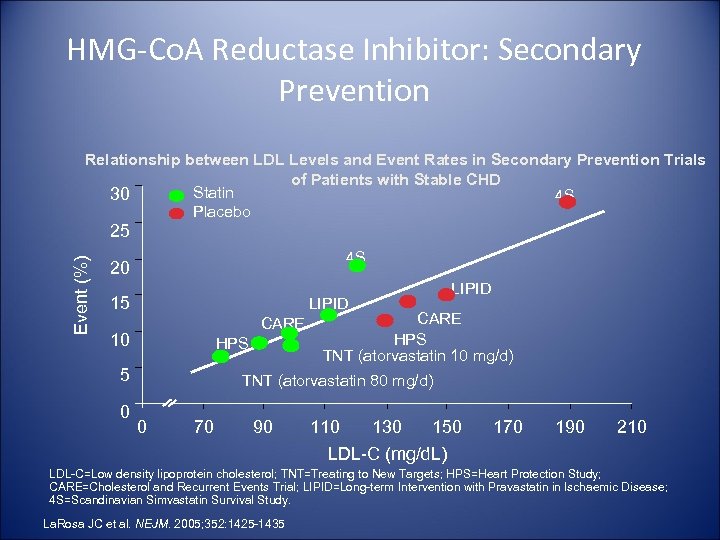 HMG-Co. A Reductase Inhibitor: Secondary Prevention Relationship between LDL Levels and Event Rates in Secondary Prevention Trials of Patients with Stable CHD Statin 30 4 S Placebo Event (%) 25 4 S 20 15 LIPID CARE 10 HPS 5 0 LIPID CARE HPS TNT (atorvastatin 10 mg/d) TNT (atorvastatin 80 mg/d) 0 70 90 110 130 150 LDL-C (mg/d. L) 170 190 210 LDL-C=Low density lipoprotein cholesterol; TNT=Treating to New Targets; HPS=Heart Protection Study; CARE=Cholesterol and Recurrent Events Trial; LIPID=Long-term Intervention with Pravastatin in Ischaemic Disease; 4 S=Scandinavian Simvastatin Survival Study. La. Rosa JC et al. NEJM. 2005; 352: 1425 -1435
HMG-Co. A Reductase Inhibitor: Secondary Prevention Relationship between LDL Levels and Event Rates in Secondary Prevention Trials of Patients with Stable CHD Statin 30 4 S Placebo Event (%) 25 4 S 20 15 LIPID CARE 10 HPS 5 0 LIPID CARE HPS TNT (atorvastatin 10 mg/d) TNT (atorvastatin 80 mg/d) 0 70 90 110 130 150 LDL-C (mg/d. L) 170 190 210 LDL-C=Low density lipoprotein cholesterol; TNT=Treating to New Targets; HPS=Heart Protection Study; CARE=Cholesterol and Recurrent Events Trial; LIPID=Long-term Intervention with Pravastatin in Ischaemic Disease; 4 S=Scandinavian Simvastatin Survival Study. La. Rosa JC et al. NEJM. 2005; 352: 1425 -1435
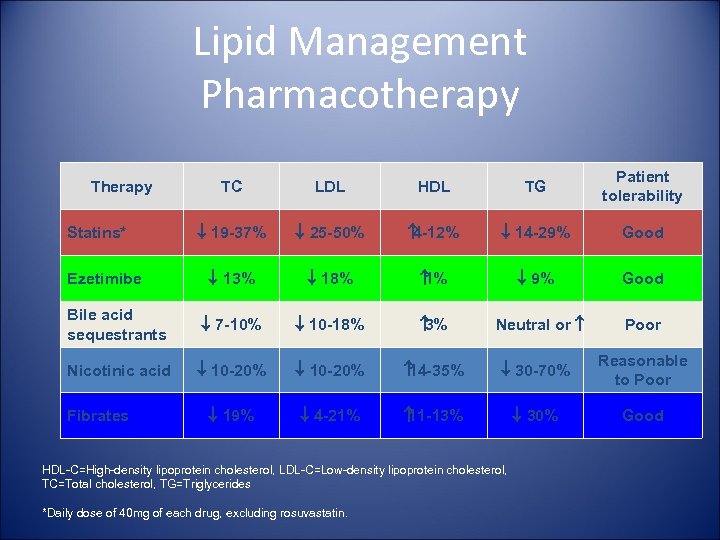 Lipid Management Pharmacotherapy TC LDL HDL TG Patient tolerability ¯ 19 -37% ¯ 25 -50% 4 -12% ¯ 14 -29% Good ¯ 13% ¯ 18% 1% ¯ 9% Good Bile acid sequestrants ¯ 7 -10% ¯ 10 -18% 3% Nicotinic acid ¯ 10 -20% 14 -35% ¯ 30 -70% Reasonable to Poor ¯ 19% ¯ 4 -21% 11 -13% ¯ 30% Good Therapy Statins* Ezetimibe Fibrates Neutral or HDL-C=High-density lipoprotein cholesterol, LDL-C=Low-density lipoprotein cholesterol, TC=Total cholesterol, TG=Triglycerides *Daily dose of 40 mg of each drug, excluding rosuvastatin. Poor
Lipid Management Pharmacotherapy TC LDL HDL TG Patient tolerability ¯ 19 -37% ¯ 25 -50% 4 -12% ¯ 14 -29% Good ¯ 13% ¯ 18% 1% ¯ 9% Good Bile acid sequestrants ¯ 7 -10% ¯ 10 -18% 3% Nicotinic acid ¯ 10 -20% 14 -35% ¯ 30 -70% Reasonable to Poor ¯ 19% ¯ 4 -21% 11 -13% ¯ 30% Good Therapy Statins* Ezetimibe Fibrates Neutral or HDL-C=High-density lipoprotein cholesterol, LDL-C=Low-density lipoprotein cholesterol, TC=Total cholesterol, TG=Triglycerides *Daily dose of 40 mg of each drug, excluding rosuvastatin. Poor
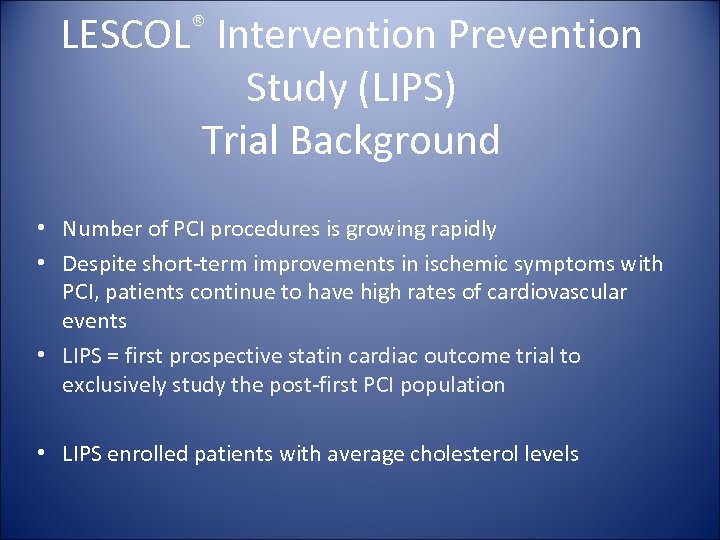 ® LESCOL Intervention Prevention Study (LIPS) Trial Background • Number of PCI procedures is growing rapidly • Despite short-term improvements in ischemic symptoms with PCI, patients continue to have high rates of cardiovascular events • LIPS = first prospective statin cardiac outcome trial to exclusively study the post-first PCI population • LIPS enrolled patients with average cholesterol levels
® LESCOL Intervention Prevention Study (LIPS) Trial Background • Number of PCI procedures is growing rapidly • Despite short-term improvements in ischemic symptoms with PCI, patients continue to have high rates of cardiovascular events • LIPS = first prospective statin cardiac outcome trial to exclusively study the post-first PCI population • LIPS enrolled patients with average cholesterol levels
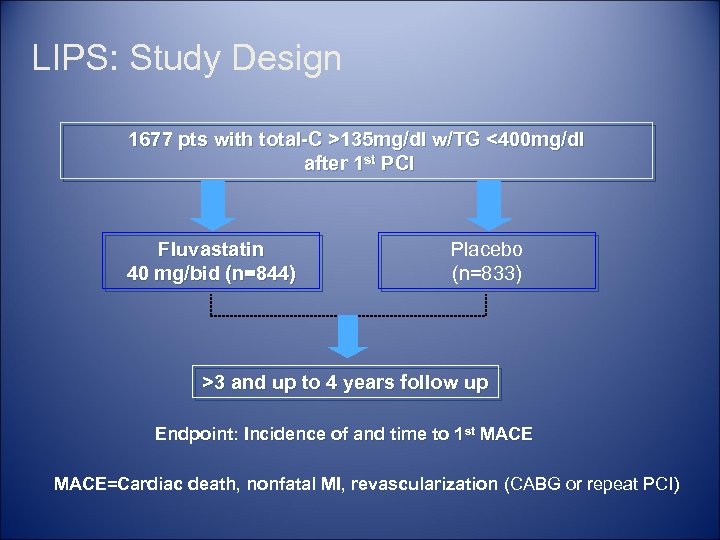 LIPS: Study Design 1677 pts with total-C >135 mg/dl w/TG <400 mg/dl after 1 st PCI Fluvastatin 40 mg/bid (n=844) Placebo (n=833) >3 and up to 4 years follow up Endpoint: Incidence of and time to 1 st MACE=Cardiac death, nonfatal MI, revascularization (CABG or repeat PCI)
LIPS: Study Design 1677 pts with total-C >135 mg/dl w/TG <400 mg/dl after 1 st PCI Fluvastatin 40 mg/bid (n=844) Placebo (n=833) >3 and up to 4 years follow up Endpoint: Incidence of and time to 1 st MACE=Cardiac death, nonfatal MI, revascularization (CABG or repeat PCI)
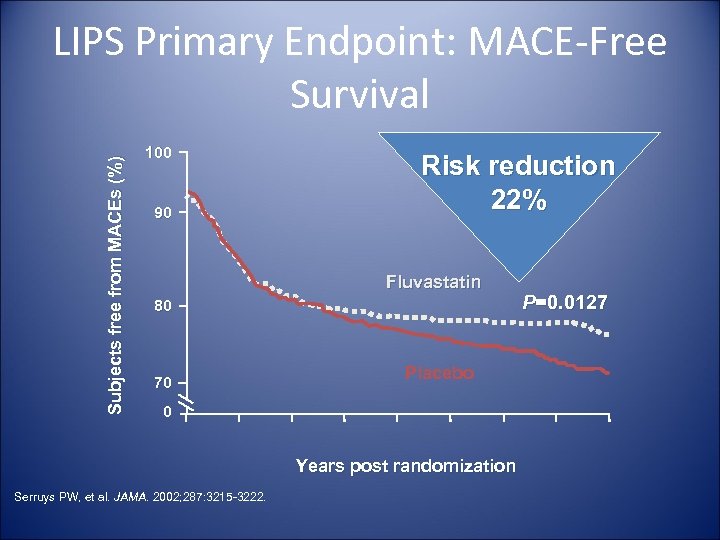 Subjects free from MACEs (%) LIPS Primary Endpoint: MACE-Free Survival 100 90 Risk reduction 22% Fluvastatin 80 70 Placebo 0 Years post randomization Serruys PW, et al. JAMA. 2002; 287: 3215 -3222. P=0. 0127
Subjects free from MACEs (%) LIPS Primary Endpoint: MACE-Free Survival 100 90 Risk reduction 22% Fluvastatin 80 70 Placebo 0 Years post randomization Serruys PW, et al. JAMA. 2002; 287: 3215 -3222. P=0. 0127
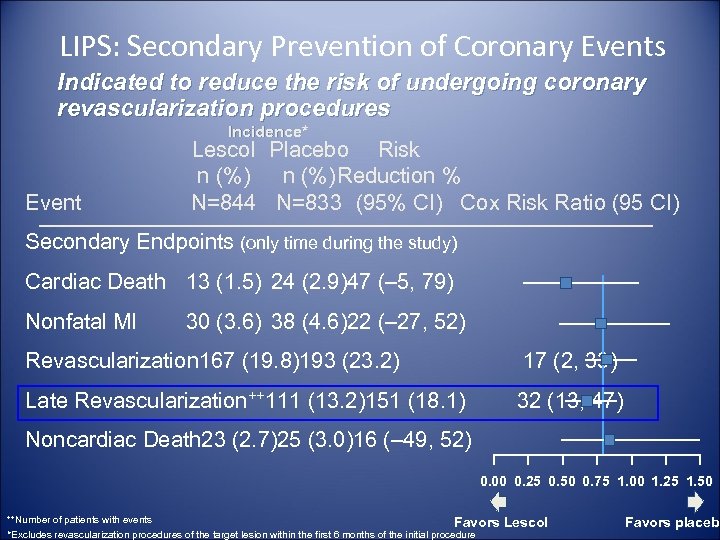 LIPS: Secondary Prevention of Coronary Events Indicated to reduce the risk of undergoing coronary revascularization procedures Incidence* Event Lescol Placebo Risk n (%)Reduction % N=844 N=833 (95% CI) Cox Risk Ratio (95 CI) Secondary Endpoints (only time during the study) Cardiac Death 13 (1. 5) 24 (2. 9)47 (– 5, 79) Nonfatal MI 30 (3. 6) 38 (4. 6)22 (– 27, 52) Revascularization 167 (19. 8)193 (23. 2) 17 (2, 33) Late Revascularization++111 (13. 2)151 (18. 1) 32 (13, 47) Noncardiac Death 23 (2. 7)25 (3. 0)16 (– 49, 52) 0. 00 0. 25 0. 50 0. 75 1. 00 1. 25 1. 50 ++Number of patients with events Favors *Excludes revascularization procedures of the target lesion within the first 6 months of the initial procedure Lescol Favors placebo
LIPS: Secondary Prevention of Coronary Events Indicated to reduce the risk of undergoing coronary revascularization procedures Incidence* Event Lescol Placebo Risk n (%)Reduction % N=844 N=833 (95% CI) Cox Risk Ratio (95 CI) Secondary Endpoints (only time during the study) Cardiac Death 13 (1. 5) 24 (2. 9)47 (– 5, 79) Nonfatal MI 30 (3. 6) 38 (4. 6)22 (– 27, 52) Revascularization 167 (19. 8)193 (23. 2) 17 (2, 33) Late Revascularization++111 (13. 2)151 (18. 1) 32 (13, 47) Noncardiac Death 23 (2. 7)25 (3. 0)16 (– 49, 52) 0. 00 0. 25 0. 50 0. 75 1. 00 1. 25 1. 50 ++Number of patients with events Favors *Excludes revascularization procedures of the target lesion within the first 6 months of the initial procedure Lescol Favors placebo
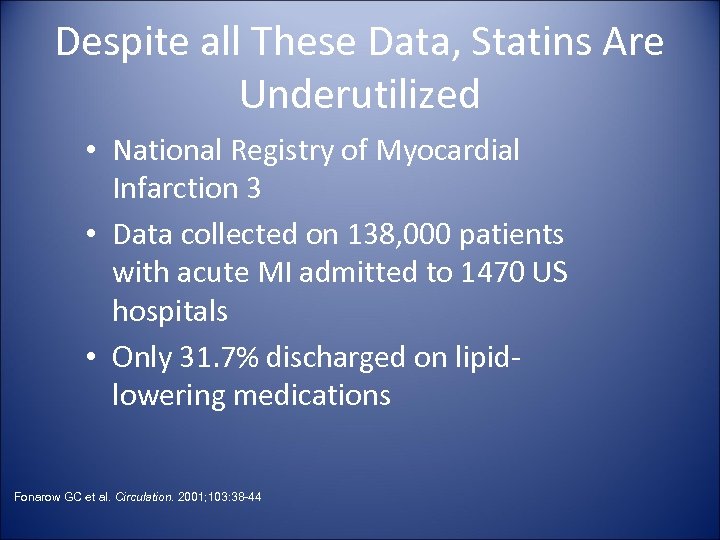 Despite all These Data, Statins Are Underutilized • National Registry of Myocardial Infarction 3 • Data collected on 138, 000 patients with acute MI admitted to 1470 US hospitals • Only 31. 7% discharged on lipidlowering medications Fonarow GC et al. Circulation. 2001; 103: 38 -44
Despite all These Data, Statins Are Underutilized • National Registry of Myocardial Infarction 3 • Data collected on 138, 000 patients with acute MI admitted to 1470 US hospitals • Only 31. 7% discharged on lipidlowering medications Fonarow GC et al. Circulation. 2001; 103: 38 -44
 Conclusions • Statins play a key role in secondary prevention of CHD • The LIPS study showed that statins such as fluvastatin are effective at preventing CHD events after PCI • Choice of statins is based on considerations of – – Efficacy Safety (low propensity for drug interactions, low myopathy rate) Effective use in combination Ease of use
Conclusions • Statins play a key role in secondary prevention of CHD • The LIPS study showed that statins such as fluvastatin are effective at preventing CHD events after PCI • Choice of statins is based on considerations of – – Efficacy Safety (low propensity for drug interactions, low myopathy rate) Effective use in combination Ease of use
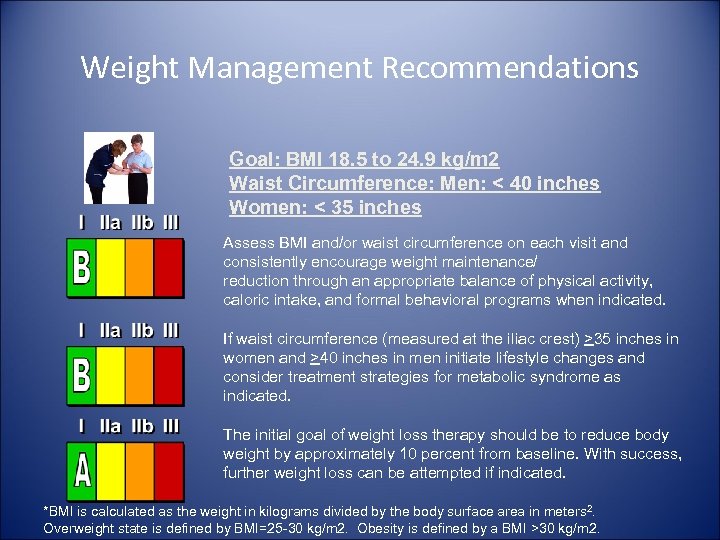 Weight Management Recommendations Goal: BMI 18. 5 to 24. 9 kg/m 2 Waist Circumference: Men: < 40 inches Women: < 35 inches Assess BMI and/or waist circumference on each visit and consistently encourage weight maintenance/ reduction through an appropriate balance of physical activity, caloric intake, and formal behavioral programs when indicated. If waist circumference (measured at the iliac crest) >35 inches in women and >40 inches in men initiate lifestyle changes and consider treatment strategies for metabolic syndrome as indicated. The initial goal of weight loss therapy should be to reduce body weight by approximately 10 percent from baseline. With success, further weight loss can be attempted if indicated. *BMI is calculated as the weight in kilograms divided by the body surface area in meters 2. Overweight state is defined by BMI=25 -30 kg/m 2. Obesity is defined by a BMI >30 kg/m 2.
Weight Management Recommendations Goal: BMI 18. 5 to 24. 9 kg/m 2 Waist Circumference: Men: < 40 inches Women: < 35 inches Assess BMI and/or waist circumference on each visit and consistently encourage weight maintenance/ reduction through an appropriate balance of physical activity, caloric intake, and formal behavioral programs when indicated. If waist circumference (measured at the iliac crest) >35 inches in women and >40 inches in men initiate lifestyle changes and consider treatment strategies for metabolic syndrome as indicated. The initial goal of weight loss therapy should be to reduce body weight by approximately 10 percent from baseline. With success, further weight loss can be attempted if indicated. *BMI is calculated as the weight in kilograms divided by the body surface area in meters 2. Overweight state is defined by BMI=25 -30 kg/m 2. Obesity is defined by a BMI >30 kg/m 2.
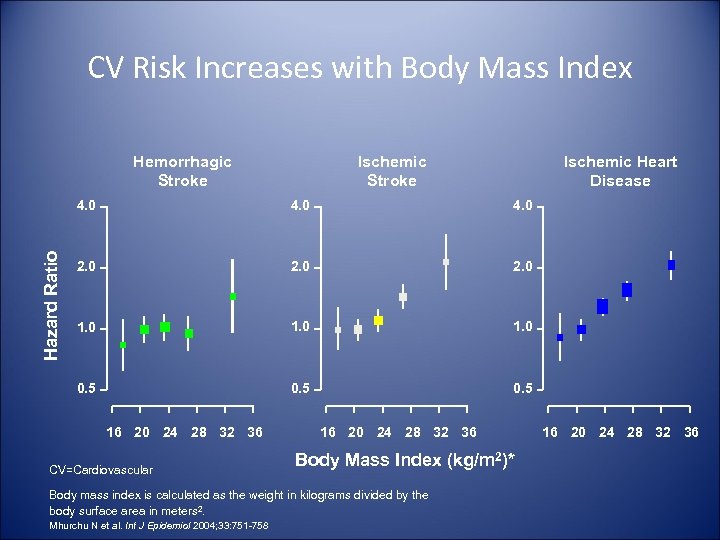 CV Risk Increases with Body Mass Index Hemorrhagic Stroke Ischemic Heart Disease 4. 0 2. 0 1. 0 0. 5 Hazard Ratio 4. 0 0. 5 16 20 24 28 32 36 CV=Cardiovascular 16 20 24 28 32 36 Body Mass Index (kg/m 2)* Body mass index is calculated as the weight in kilograms divided by the body surface area in meters 2. Mhurchu N et al. Int J Epidemiol 2004; 33: 751 -758 16 20 24 28 32 36
CV Risk Increases with Body Mass Index Hemorrhagic Stroke Ischemic Heart Disease 4. 0 2. 0 1. 0 0. 5 Hazard Ratio 4. 0 0. 5 16 20 24 28 32 36 CV=Cardiovascular 16 20 24 28 32 36 Body Mass Index (kg/m 2)* Body mass index is calculated as the weight in kilograms divided by the body surface area in meters 2. Mhurchu N et al. Int J Epidemiol 2004; 33: 751 -758 16 20 24 28 32 36
 Other Issues Related to Stents • Only 4 reported cases of infected stent • Presence of coronary stent is not an indication for SBE • Most coronary stents in use are either nonferromagnetic or weakly ferromagnetic • Presence of stent should not preclude MRI Dieter, Clin Cardiol. 2003; 23: 808 -10
Other Issues Related to Stents • Only 4 reported cases of infected stent • Presence of coronary stent is not an indication for SBE • Most coronary stents in use are either nonferromagnetic or weakly ferromagnetic • Presence of stent should not preclude MRI Dieter, Clin Cardiol. 2003; 23: 808 -10
 Future • • • New Antiplatelet Agents Oral Thrombin Inhibitors New Studies on Optimum Anticoagulation Strategies New Short Acting Thienopyridine Advances in Stent Technology – Bioabsorbable Stents • Better Technique in Stent Deployment – IVUS Guided
Future • • • New Antiplatelet Agents Oral Thrombin Inhibitors New Studies on Optimum Anticoagulation Strategies New Short Acting Thienopyridine Advances in Stent Technology – Bioabsorbable Stents • Better Technique in Stent Deployment – IVUS Guided
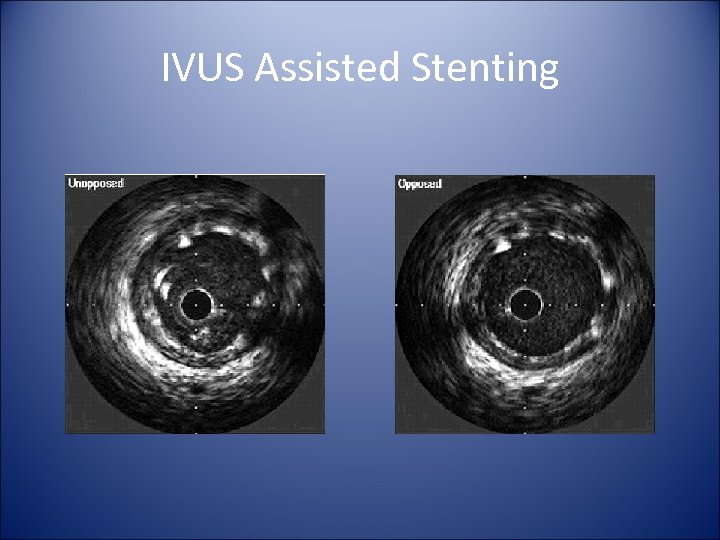 IVUS Assisted Stenting
IVUS Assisted Stenting
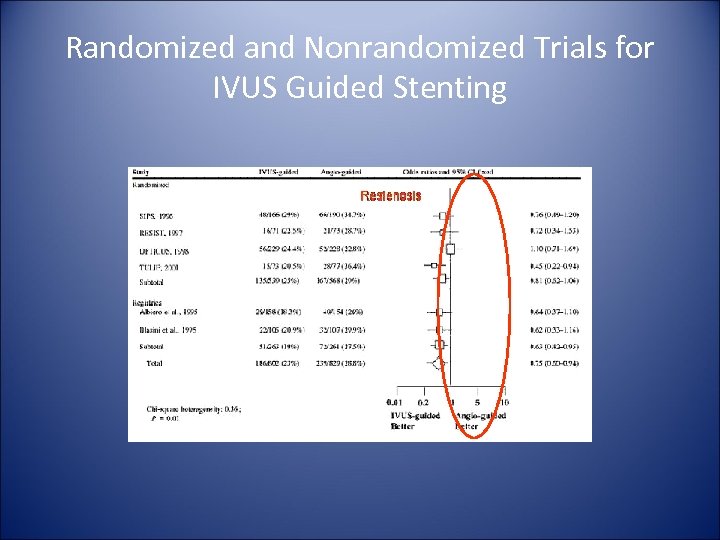 Randomized and Nonrandomized Trials for IVUS Guided Stenting
Randomized and Nonrandomized Trials for IVUS Guided Stenting
 Who should not receive a drug eluting stent? Osama Bin Laden Sadam Hussein Trial Lawyers
Who should not receive a drug eluting stent? Osama Bin Laden Sadam Hussein Trial Lawyers


