CPR lecture.pptx
- Количество слайдов: 135
 Cardiopulmonary Resuscitation Kharkiv National Medical University Department of Anesthesiology, Traumatology and Emergency Medicine, Professor of Anesthesia Olga Khamitovna Fesenko
Cardiopulmonary Resuscitation Kharkiv National Medical University Department of Anesthesiology, Traumatology and Emergency Medicine, Professor of Anesthesia Olga Khamitovna Fesenko
 Cardio-Pulmonary Resuscitation is required in the following cases: n n n Cardiac arrest Respiratory arrest or a combination of the two.
Cardio-Pulmonary Resuscitation is required in the following cases: n n n Cardiac arrest Respiratory arrest or a combination of the two.
 Cardiopulmonary resuscitation (CPR) is required n n when the supply of oxygen to the brain is insufficient to maintain function. Oxygen delivery is dependent upon cardiac output, hemoglobin concentration and saturation of hemoglobin with oxygen; this depends predominantly on respiratory function.
Cardiopulmonary resuscitation (CPR) is required n n when the supply of oxygen to the brain is insufficient to maintain function. Oxygen delivery is dependent upon cardiac output, hemoglobin concentration and saturation of hemoglobin with oxygen; this depends predominantly on respiratory function.
 The effectiveness of CPR (ALS in hospitals) (Rosenberg M. et all. , 1993. The review of results from 14 hospitals) Return of spontaneous circulation took place in 17. 4% – 58% of patients. n 7. 0% – 24. 3% of patients discharged from hospital. n
The effectiveness of CPR (ALS in hospitals) (Rosenberg M. et all. , 1993. The review of results from 14 hospitals) Return of spontaneous circulation took place in 17. 4% – 58% of patients. n 7. 0% – 24. 3% of patients discharged from hospital. n
 The protocols of Cardio. Pulmonary Resuscitation BLS (basic life support) consists of artificial ventilation (with Ambu bag or the rescuer’s expired air) and closed-chest cardiac compressions. n ALS (advanced life support) presupposes a thorough knowledge of basic life support. It requires adjunctive equipment, drugs and specialists. n
The protocols of Cardio. Pulmonary Resuscitation BLS (basic life support) consists of artificial ventilation (with Ambu bag or the rescuer’s expired air) and closed-chest cardiac compressions. n ALS (advanced life support) presupposes a thorough knowledge of basic life support. It requires adjunctive equipment, drugs and specialists. n
 BLS – basic life support n n For optimum effectiveness it should be initiated in a definite sequence and within 4 minutes of the onset of arrest. It should be taught for all populations of people. Everyone might carry out BLS.
BLS – basic life support n n For optimum effectiveness it should be initiated in a definite sequence and within 4 minutes of the onset of arrest. It should be taught for all populations of people. Everyone might carry out BLS.
 ALS-advanced life support includes: n n n the use of adjunctive equipment for the maintenance of ventilation and circulation, electrocardiographic monitoring and arrhythmia recognition, the use of proper drug therapy and defibrillation to establish and maintain an effective cardiac rhythm, establishment of intravenous infusion lines, stabilization of the patient. In order for ALS to be optimally effective, it should be available to the victim within 8 minutes of the time of arrest.
ALS-advanced life support includes: n n n the use of adjunctive equipment for the maintenance of ventilation and circulation, electrocardiographic monitoring and arrhythmia recognition, the use of proper drug therapy and defibrillation to establish and maintain an effective cardiac rhythm, establishment of intravenous infusion lines, stabilization of the patient. In order for ALS to be optimally effective, it should be available to the victim within 8 minutes of the time of arrest.
 Evaluating three systems n n n People fall in different way but they die in the same way. That’s why it’s not worth to waste time for taking correct diagnosis in the first moment (at the beginning). It’s enough to appreciate three main systems for quick understanding situation (to form a correct estimate of situation): 1. nervous system (if the patient is conscious or not) 2. breathing (if the patient is breathing or not) 3. circulation (if the patient’s heart is beating or not).
Evaluating three systems n n n People fall in different way but they die in the same way. That’s why it’s not worth to waste time for taking correct diagnosis in the first moment (at the beginning). It’s enough to appreciate three main systems for quick understanding situation (to form a correct estimate of situation): 1. nervous system (if the patient is conscious or not) 2. breathing (if the patient is breathing or not) 3. circulation (if the patient’s heart is beating or not).
 The A-B-C schedule n In the critical cases there is no time to think it over. That’s why rescuers (911) and boyscouts know the protocols (guidelines) (we call them algorithms) to act in A-B-C schedule
The A-B-C schedule n In the critical cases there is no time to think it over. That’s why rescuers (911) and boyscouts know the protocols (guidelines) (we call them algorithms) to act in A-B-C schedule
 (step-A) : Assessment “Awake or not? ” n n Approach the patient ensuring that there is no danger from the surrounding environment. Assess the level of responsiveness by gently shaking the patient and shouting “Are you all right? ” If the patient is unresponsive then shout for help and commence basic life support immediately. You must ensure the patency of the patient’s airway (A – Airway open!)
(step-A) : Assessment “Awake or not? ” n n Approach the patient ensuring that there is no danger from the surrounding environment. Assess the level of responsiveness by gently shaking the patient and shouting “Are you all right? ” If the patient is unresponsive then shout for help and commence basic life support immediately. You must ensure the patency of the patient’s airway (A – Airway open!)
 (step-B): Breathing. «Breaths or not? » . With the airway held open, check for breathing by: • Looking: to see if the chest wall is moving or if the abdominal wall is indicating an obstructed airway by a seesaw movement. • Listening: over the mouth for sounds of air movement or for added sounds indicating an obstructed airway. • Feeling: over the mouth with the side of the face for signs of air movement indicating effective breathing. n If the patient is not breathing you must begin the artificial respiration with your hands and mouth (“Breath for him!”). n
(step-B): Breathing. «Breaths or not? » . With the airway held open, check for breathing by: • Looking: to see if the chest wall is moving or if the abdominal wall is indicating an obstructed airway by a seesaw movement. • Listening: over the mouth for sounds of air movement or for added sounds indicating an obstructed airway. • Feeling: over the mouth with the side of the face for signs of air movement indicating effective breathing. n If the patient is not breathing you must begin the artificial respiration with your hands and mouth (“Breath for him!”). n
 (step-C): «Circulation» - «Is the blood circulation present or absent or «Is the patient’s heart beating? » . n n Pulse check is carried out by feeling for the carotid pulse on the neck for 10 sec. If there is no pulse or there are no signs of life, start chest compressions immediately.
(step-C): «Circulation» - «Is the blood circulation present or absent or «Is the patient’s heart beating? » . n n Pulse check is carried out by feeling for the carotid pulse on the neck for 10 sec. If there is no pulse or there are no signs of life, start chest compressions immediately.
 Pulse Check in children n If the infant or child is unresponsive and not breathing or only gasping, healthcare providers may take up to 10 seconds to attempt to feel for a pulse (brachial in an infant and carotid or femoral in a child). If, within 10 seconds, you don’t feel a pulse or are not sure if you feel a pulse, begin chest compressions. It can be difficult to determine the presence or absence of a pulse, especially in an emergency, and studies show that both healthcare providers and lay rescuers are unable to reliably detect a pulse.
Pulse Check in children n If the infant or child is unresponsive and not breathing or only gasping, healthcare providers may take up to 10 seconds to attempt to feel for a pulse (brachial in an infant and carotid or femoral in a child). If, within 10 seconds, you don’t feel a pulse or are not sure if you feel a pulse, begin chest compressions. It can be difficult to determine the presence or absence of a pulse, especially in an emergency, and studies show that both healthcare providers and lay rescuers are unable to reliably detect a pulse.
 Airway n n In the unresponsive patient, open the airway by tilting the head back and lifting the jaw forwards. This displaces the tongue, the most common cause of airway obstruction, from the back of the pharynx. In cases of suspected cervical spine injury, the airway should be opened by using the jaw thrust maneuver only, whilst maintaining in-line cervical spine immobilization. Head tilt and neck extension must never be used in this situation.
Airway n n In the unresponsive patient, open the airway by tilting the head back and lifting the jaw forwards. This displaces the tongue, the most common cause of airway obstruction, from the back of the pharynx. In cases of suspected cervical spine injury, the airway should be opened by using the jaw thrust maneuver only, whilst maintaining in-line cervical spine immobilization. Head tilt and neck extension must never be used in this situation.
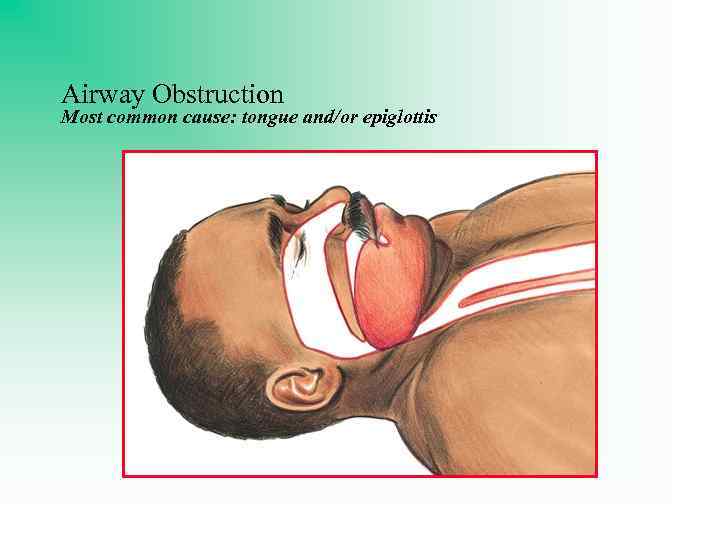 Airway Obstruction Most common cause: tongue and/or epiglottis
Airway Obstruction Most common cause: tongue and/or epiglottis
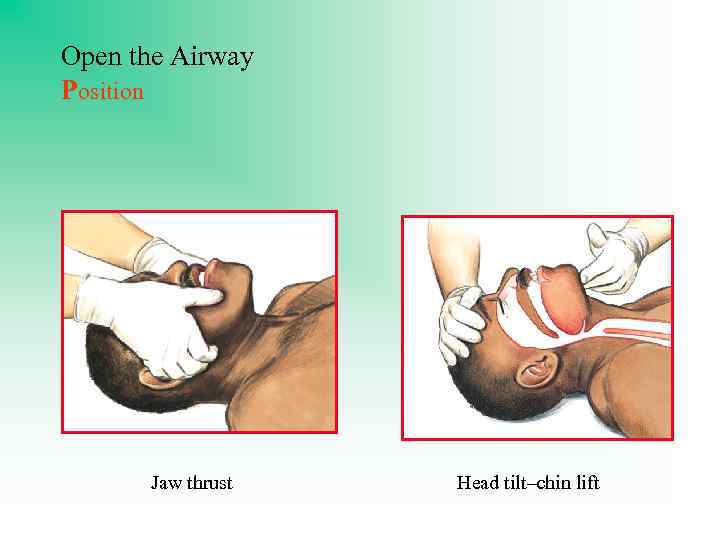 Open the Airway Position Jaw thrust Head tilt–chin lift
Open the Airway Position Jaw thrust Head tilt–chin lift
 Open the Airway Oropharyngeal Airway
Open the Airway Oropharyngeal Airway
 Open the Airway Nasopharyngeal Airway
Open the Airway Nasopharyngeal Airway
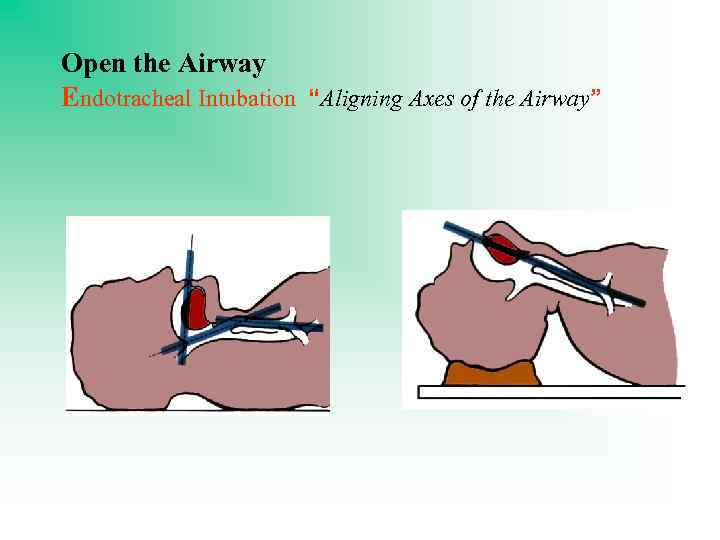 Open the Airway Endotracheal Intubation “Aligning Axes of the Airway”
Open the Airway Endotracheal Intubation “Aligning Axes of the Airway”
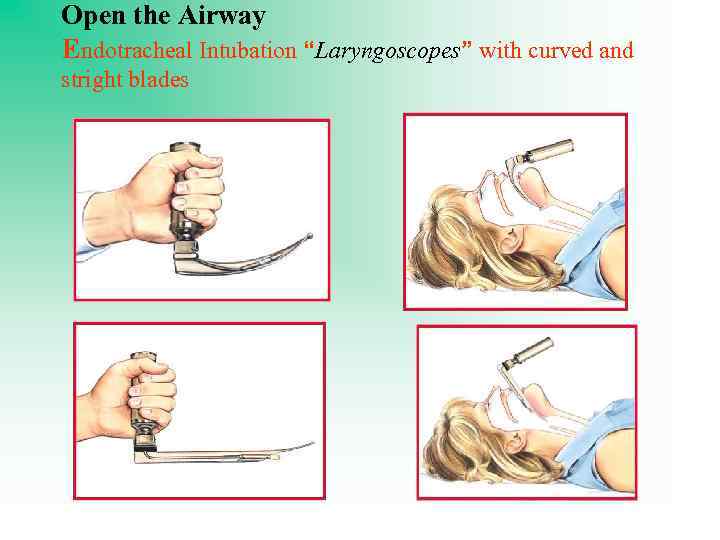 Open the Airway Endotracheal Intubation “Laryngoscopes” with curved and stright blades
Open the Airway Endotracheal Intubation “Laryngoscopes” with curved and stright blades
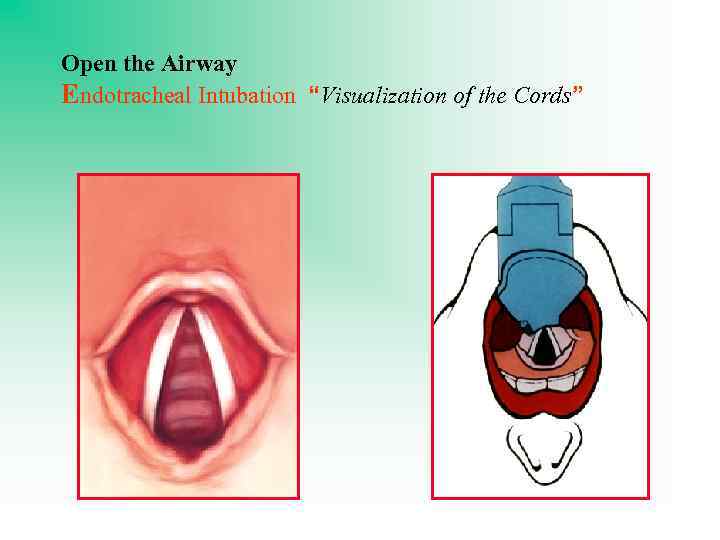 Open the Airway Endotracheal Intubation “Visualization of the Cords”
Open the Airway Endotracheal Intubation “Visualization of the Cords”
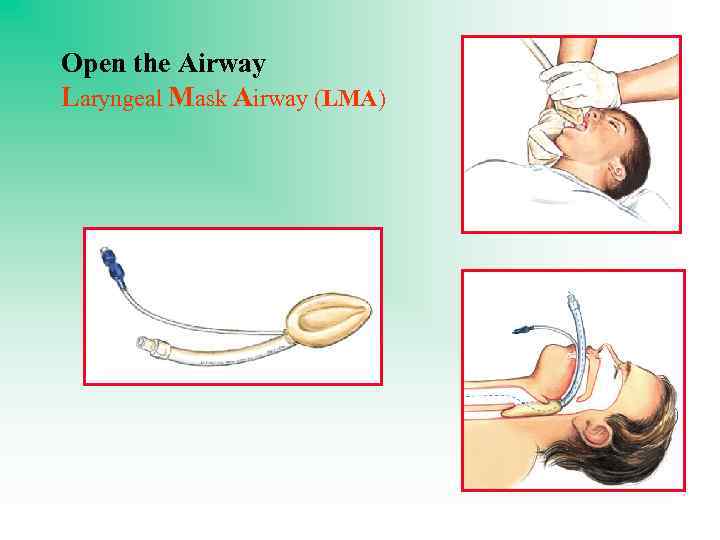 Open the Airway Laryngeal Mask Airway (LMA)
Open the Airway Laryngeal Mask Airway (LMA)
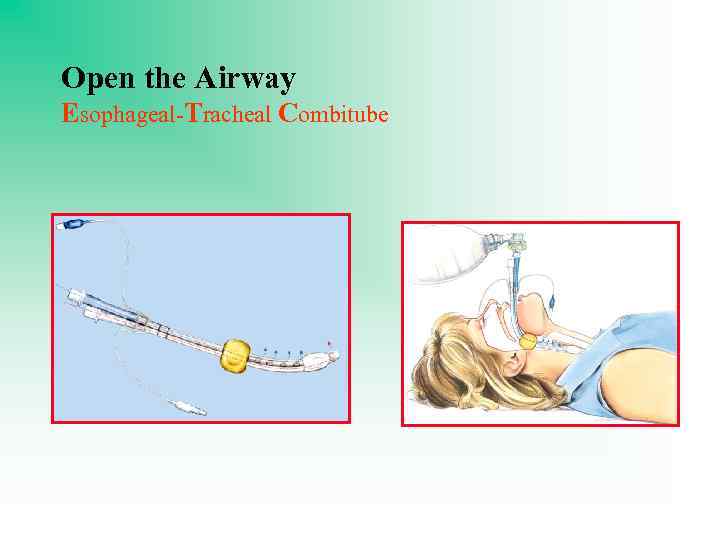 Open the Airway Esophageal-Tracheal Combitube
Open the Airway Esophageal-Tracheal Combitube
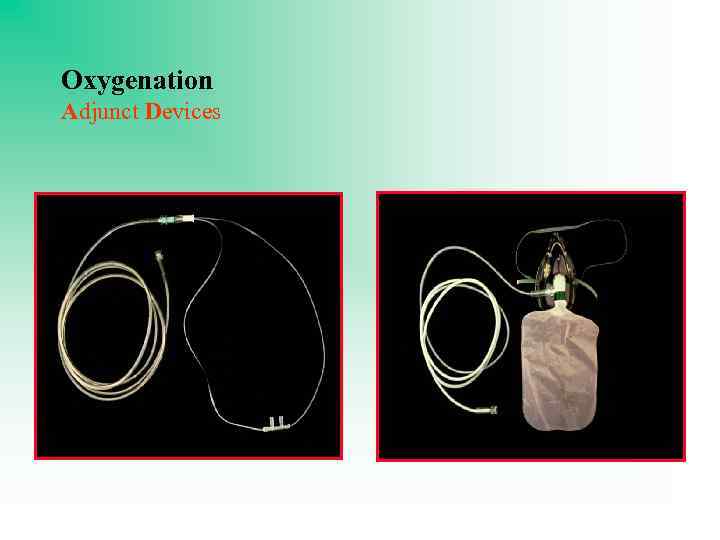 Oxygenation Adjunct Devices
Oxygenation Adjunct Devices
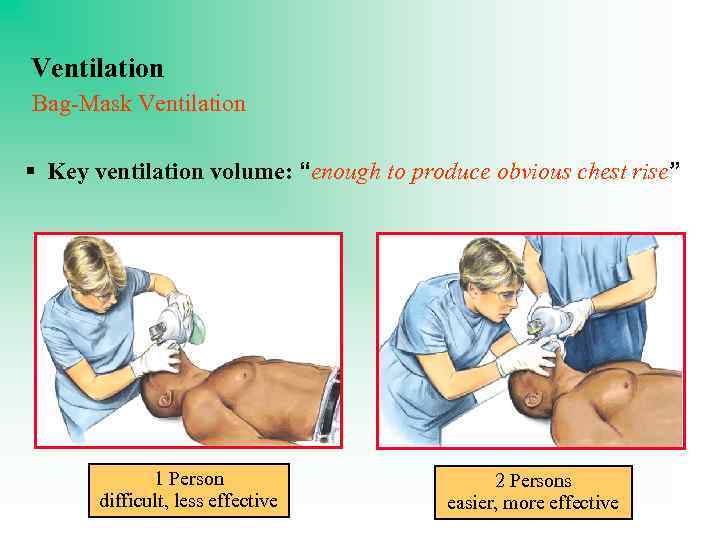 Ventilation Bag-Mask Ventilation § Key ventilation volume: “enough to produce obvious chest rise” 1 Person difficult, less effective 2 Persons easier, more effective
Ventilation Bag-Mask Ventilation § Key ventilation volume: “enough to produce obvious chest rise” 1 Person difficult, less effective 2 Persons easier, more effective
 A precordial thump n n The precordial thump should not be used for unwitnessed out-of-hospital cardiac arrest. The precordial thump may be considered for patients with witnessed, monitored, unstable VT (including pulseless VT) if a defibrillator is not immediately ready for use, but it should not delay CPR and defibrillation.
A precordial thump n n The precordial thump should not be used for unwitnessed out-of-hospital cardiac arrest. The precordial thump may be considered for patients with witnessed, monitored, unstable VT (including pulseless VT) if a defibrillator is not immediately ready for use, but it should not delay CPR and defibrillation.
 Chest compressions n n Chest compressions are performed on the lower third of the sternum, two fingers breadth above the xiphisternum. The overlapping heels of both hands are used to compress the chest by depressing the sternum approximately 5 cm at a rate of 100 compressions per min.
Chest compressions n n Chest compressions are performed on the lower third of the sternum, two fingers breadth above the xiphisternum. The overlapping heels of both hands are used to compress the chest by depressing the sternum approximately 5 cm at a rate of 100 compressions per min.
 Mechanisms of action of chest compressions n The original theory of the action of chest compressions was that the heart was squeezed with each depression of the sternum between the sternum anteriorly and the vertebral column posteriorly. Each compression of the heart pumped blood around the circulation (the heart pump theory).
Mechanisms of action of chest compressions n The original theory of the action of chest compressions was that the heart was squeezed with each depression of the sternum between the sternum anteriorly and the vertebral column posteriorly. Each compression of the heart pumped blood around the circulation (the heart pump theory).
 Mechanisms of action of chest compressions n A later theory, the chest pump theory, uses the concept that each chest compression raises the intrathoracic pressure. This raised pressure is transmitted to the intrathoracic vessels; the arteries, being thick-walled, retain and transmit this pressure, whereas the veins, being thin-walled, collapse. The result is a pressure gradient between the arterial and the venous systems and thus a forward flow of blood around the circulation.
Mechanisms of action of chest compressions n A later theory, the chest pump theory, uses the concept that each chest compression raises the intrathoracic pressure. This raised pressure is transmitted to the intrathoracic vessels; the arteries, being thick-walled, retain and transmit this pressure, whereas the veins, being thin-walled, collapse. The result is a pressure gradient between the arterial and the venous systems and thus a forward flow of blood around the circulation.
 What is new in СPR? n The key issues and changes in the 2010 American Heart Association (AHA) Guidelines for Cardiopulmonary Resuscitation (CPR) and Emergency Cardiovascular Care (ECC)
What is new in СPR? n The key issues and changes in the 2010 American Heart Association (AHA) Guidelines for Cardiopulmonary Resuscitation (CPR) and Emergency Cardiovascular Care (ECC)
 A Change From A-B-C to C-A-B n n For all of us who have learned the “A-B-C” (Airway. Breathing-Circulation), we must all learn the new: “C-A -B” sequence (Circulation-Airway-Breathing). Survival studies in Cardiac Arrest all show the primary importance of good and minimally interrupted chest compressions.
A Change From A-B-C to C-A-B n n For all of us who have learned the “A-B-C” (Airway. Breathing-Circulation), we must all learn the new: “C-A -B” sequence (Circulation-Airway-Breathing). Survival studies in Cardiac Arrest all show the primary importance of good and minimally interrupted chest compressions.
 “Hands-Only” • For untrained public bystanders, the outcome is best if “Hands-Only” Cardiopulmonary Resuscitation (CPR) is used. • This is what we should teach the public and what dispatchers should tell bystanders to perform. • Exceptions would be children or adults in whom the arrest is likely respiratory (drowning, etc. ).
“Hands-Only” • For untrained public bystanders, the outcome is best if “Hands-Only” Cardiopulmonary Resuscitation (CPR) is used. • This is what we should teach the public and what dispatchers should tell bystanders to perform. • Exceptions would be children or adults in whom the arrest is likely respiratory (drowning, etc. ).
 Minimal delay in compressions n n n We should spend no more than 10 seconds trying to find a pulse in an unconscious patient. If a patient has gasping agonal respirations and is unconscious or even had a brief seizure, this likely represents a cardiac arrest and may confuse bystanders… So if patient is unconscious, begin good chest compressions with minimal delay to seek pulse.
Minimal delay in compressions n n n We should spend no more than 10 seconds trying to find a pulse in an unconscious patient. If a patient has gasping agonal respirations and is unconscious or even had a brief seizure, this likely represents a cardiac arrest and may confuse bystanders… So if patient is unconscious, begin good chest compressions with minimal delay to seek pulse.
 Chest compressions are the № 1 PRIORITY! n n The trained personnel should use 30: 2 chest compression to ventilation in adult CPR…. . but, NOT to delay chest compressions more than 10 seconds to seek pulse in a collapsed victim.
Chest compressions are the № 1 PRIORITY! n n The trained personnel should use 30: 2 chest compression to ventilation in adult CPR…. . but, NOT to delay chest compressions more than 10 seconds to seek pulse in a collapsed victim.
 Depth of chest compressions: n n In adults: at least 2 inches (5 cm) with time for full recoil. In children: at least one third of the anteriorposterior diameter of the chest. This corresponds to approximately 1½ inches (about 4 cm) in most infants and about 2 inches (5 cm) in most children.
Depth of chest compressions: n n In adults: at least 2 inches (5 cm) with time for full recoil. In children: at least one third of the anteriorposterior diameter of the chest. This corresponds to approximately 1½ inches (about 4 cm) in most infants and about 2 inches (5 cm) in most children.
 And not just any chest compressions: n Studies show we should relieve each other every 2 minutes if we have personnel, as fatigue increases and chest compressions become less adequate in a short time.
And not just any chest compressions: n Studies show we should relieve each other every 2 minutes if we have personnel, as fatigue increases and chest compressions become less adequate in a short time.
 The rapid assessment of the patient's cardiac rhythm The patient must be connected to a cardiac monitor (or defibrillator) and the cardiac rhythm assessed. n If the electrocardiographic rhythm is compatible with a cardiac output then the pulse must be assessed carefully. n
The rapid assessment of the patient's cardiac rhythm The patient must be connected to a cardiac monitor (or defibrillator) and the cardiac rhythm assessed. n If the electrocardiographic rhythm is compatible with a cardiac output then the pulse must be assessed carefully. n
 ECG rhythms associated with cardiac arrest: n n Ventricular fibrillation (VF) Pulseless ventricular tachycardia (VT) Asystole. This is a flat electrocardiograph trace indicating no ventricular activity. Occasionally, there may be P wave electrical activity only. Electromechanical dissociation (EMD). EMD or pulseless electrical activity (PEA) has the worst prognosis of all rhythms associated with cardiac arrest. ECG shows electrical activity consistent with cardiac activity but there is no palpable peripheral pulse.
ECG rhythms associated with cardiac arrest: n n Ventricular fibrillation (VF) Pulseless ventricular tachycardia (VT) Asystole. This is a flat electrocardiograph trace indicating no ventricular activity. Occasionally, there may be P wave electrical activity only. Electromechanical dissociation (EMD). EMD or pulseless electrical activity (PEA) has the worst prognosis of all rhythms associated with cardiac arrest. ECG shows electrical activity consistent with cardiac activity but there is no palpable peripheral pulse.
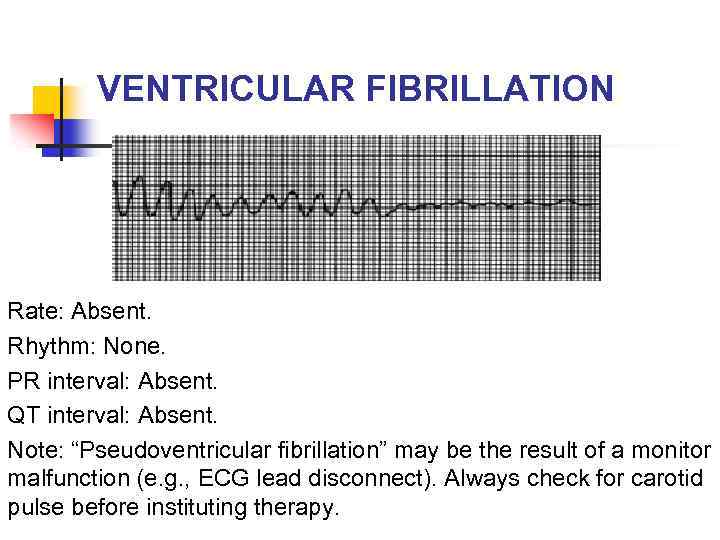 VENTRICULAR FIBRILLATION Rate: Absent. Rhythm: None. PR interval: Absent. QT interval: Absent. Note: “Pseudoventricular fibrillation” may be the result of a monitor malfunction (e. g. , ECG lead disconnect). Always check for carotid pulse before instituting therapy.
VENTRICULAR FIBRILLATION Rate: Absent. Rhythm: None. PR interval: Absent. QT interval: Absent. Note: “Pseudoventricular fibrillation” may be the result of a monitor malfunction (e. g. , ECG lead disconnect). Always check for carotid pulse before instituting therapy.
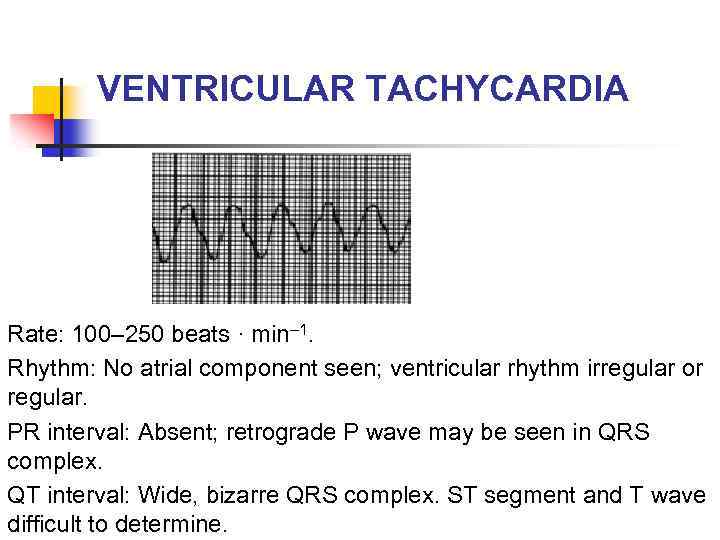 VENTRICULAR TACHYCARDIA Rate: 100– 250 beats · min– 1. Rhythm: No atrial component seen; ventricular rhythm irregular or regular. PR interval: Absent; retrograde P wave may be seen in QRS complex. QT interval: Wide, bizarre QRS complex. ST segment and T wave difficult to determine.
VENTRICULAR TACHYCARDIA Rate: 100– 250 beats · min– 1. Rhythm: No atrial component seen; ventricular rhythm irregular or regular. PR interval: Absent; retrograde P wave may be seen in QRS complex. QT interval: Wide, bizarre QRS complex. ST segment and T wave difficult to determine.
 Causes of cardiac arrest with ventricular fibrillation/pulseless ventricular tachycardia Acute coronary syndrome. n Ischemic heart disease with previous myocardial infarction. n Other structural heart disease (e. g. dilated or hypertrophic cardiomyopathy). n Wolff–Parkinson–White syndrome. n
Causes of cardiac arrest with ventricular fibrillation/pulseless ventricular tachycardia Acute coronary syndrome. n Ischemic heart disease with previous myocardial infarction. n Other structural heart disease (e. g. dilated or hypertrophic cardiomyopathy). n Wolff–Parkinson–White syndrome. n
 Causes of cardiac arrest with pulseless electrical activity (PEA) or asystole Hypovolemia n Hypoxemia n Hypokalemia / hyperkalemia / hypocalcemia n Hypothermia n Toxins (poisoning) n Tamponade: cardiac n Tension pneumothorax n Thromboembolism: pulmonary n
Causes of cardiac arrest with pulseless electrical activity (PEA) or asystole Hypovolemia n Hypoxemia n Hypokalemia / hyperkalemia / hypocalcemia n Hypothermia n Toxins (poisoning) n Tamponade: cardiac n Tension pneumothorax n Thromboembolism: pulmonary n
 Shockable or nonshockable rithms n n Shockable: Ventricular fibrillation (VF) / pulseless ventricular tachycardia (VT) Nonshockable: Asystole, Electromechanical dissociation (EMD) or pulseless electrical activity (PEA)
Shockable or nonshockable rithms n n Shockable: Ventricular fibrillation (VF) / pulseless ventricular tachycardia (VT) Nonshockable: Asystole, Electromechanical dissociation (EMD) or pulseless electrical activity (PEA)
 Defibfillation: electrode placement n n For ease of placement and education, the anterior-lateral pad position is a reasonable default electrode placement: one electrode is applied to the right of the upper sternum below the clavicle and the other is centered over the fifth left intercostal space in the midclavicular line (corresponding to the cardiac apex). Any of 3 alternative pad positions (anterior-posterior, anterior– left infrascapular, and anterior–right infrascapular) may be considered on the basis of individual patient characteristics.
Defibfillation: electrode placement n n For ease of placement and education, the anterior-lateral pad position is a reasonable default electrode placement: one electrode is applied to the right of the upper sternum below the clavicle and the other is centered over the fifth left intercostal space in the midclavicular line (corresponding to the cardiac apex). Any of 3 alternative pad positions (anterior-posterior, anterior– left infrascapular, and anterior–right infrascapular) may be considered on the basis of individual patient characteristics.
 Defibfillation: “stand clear!” n n n Following application of the contact electrodes to the chest, the defibrillator is charged and the operator shouts “stand clear”. Any oxygen source is disconnected from the patient. Following a visual check that no-one is touching the patient, the operator defibrillates the patient.
Defibfillation: “stand clear!” n n n Following application of the contact electrodes to the chest, the defibrillator is charged and the operator shouts “stand clear”. Any oxygen source is disconnected from the patient. Following a visual check that no-one is touching the patient, the operator defibrillates the patient.
 Defibrillation: 3 -shock sequence Defibrillation is delivered as a series of three direct current (DC) shocks at 200, 250 and 360 J. n Subsequent defibrillation attempts are made at 360 J. n
Defibrillation: 3 -shock sequence Defibrillation is delivered as a series of three direct current (DC) shocks at 200, 250 and 360 J. n Subsequent defibrillation attempts are made at 360 J. n
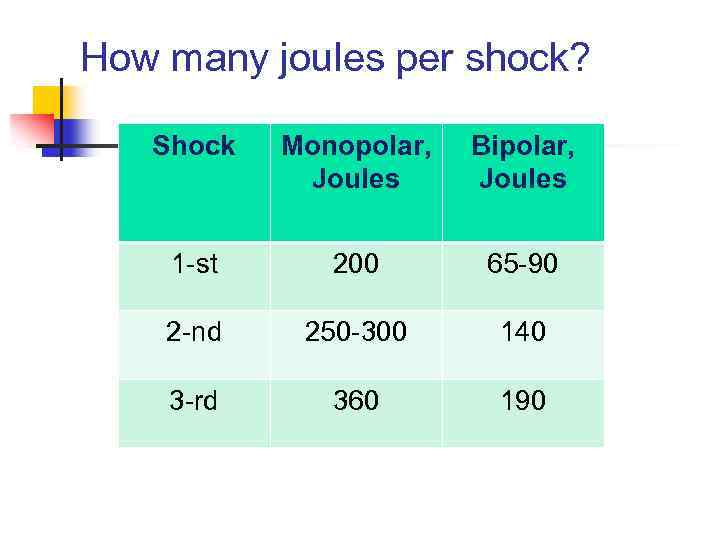 How many joules per shock? Shock Monopolar, Joules Bipolar, Joules 1 -st 200 65 -90 2 -nd 250 -300 140 3 -rd 360 190
How many joules per shock? Shock Monopolar, Joules Bipolar, Joules 1 -st 200 65 -90 2 -nd 250 -300 140 3 -rd 360 190
 1 -Shock sequence n n n Biphasic: Manufacturer recommendation (120200 J); if unknown, use maximum available. Second and subsequent doses should be equivalent, and higher doses may be considered. Monophasic: 360 J.
1 -Shock sequence n n n Biphasic: Manufacturer recommendation (120200 J); if unknown, use maximum available. Second and subsequent doses should be equivalent, and higher doses may be considered. Monophasic: 360 J.
 Pediatric Defibrillation n A dose of 2 to 4 J/kg may be used for the initial defibrillation energy, but for ease of teaching, an initial dose of 2 J/kg may be considered. For subsequent shocks, energy levels should be at least 4 J/kg. Higher energy levels may be considered, not to exceed 10 J/kg or the adult maximum dose.
Pediatric Defibrillation n A dose of 2 to 4 J/kg may be used for the initial defibrillation energy, but for ease of teaching, an initial dose of 2 J/kg may be considered. For subsequent shocks, energy levels should be at least 4 J/kg. Higher energy levels may be considered, not to exceed 10 J/kg or the adult maximum dose.
 1 -Shock Protocol vs 3 -Shock Sequence n n If 1 shock fails to eliminate VF, the incremental benefit of another shock is low, and resumption of CPR is likely to confer a greater value than another immediate shock. Animal studies documenting harmful effects from interruptions to chest compressions and human studies suggesting a survival benefit from a CPR approach that includes a 1 -shock compared with a 3 -shock protocol, supports the recommendation of single shocks followed by immediate CPR rather than stacked shocks for attempted defibrillation.
1 -Shock Protocol vs 3 -Shock Sequence n n If 1 shock fails to eliminate VF, the incremental benefit of another shock is low, and resumption of CPR is likely to confer a greater value than another immediate shock. Animal studies documenting harmful effects from interruptions to chest compressions and human studies suggesting a survival benefit from a CPR approach that includes a 1 -shock compared with a 3 -shock protocol, supports the recommendation of single shocks followed by immediate CPR rather than stacked shocks for attempted defibrillation.
 Automated external defibrillators (AEDs) are now available. n n n These machines voice prompt the operator through a series of actions leading to defibrillation. These sophisticated machines also diagnose ventricular fibrillation or fast ventricular tachycardia, indicate to the operator the need to defibrillate and charge to the appropriate number of joules. The operator then defibrillates the patient by pushing the relevant button and the machine recycles through its program, following the universal ALS algorithm, prompting the operator to the appropriate action.
Automated external defibrillators (AEDs) are now available. n n n These machines voice prompt the operator through a series of actions leading to defibrillation. These sophisticated machines also diagnose ventricular fibrillation or fast ventricular tachycardia, indicate to the operator the need to defibrillate and charge to the appropriate number of joules. The operator then defibrillates the patient by pushing the relevant button and the machine recycles through its program, following the universal ALS algorithm, prompting the operator to the appropriate action.
 Automated external defibrillators (AEDs) are now available. n n The simplicity of the AED belies its sophistication; not only can it diagnose and treat VF/VT faster than manual defibrillation methods, but it can also be used by non-medical operators trained in its use. Some AED models are using a biphasic defibrillation waveform. These biphasic models have been shown to be extremely effective at defibrillation using lower levels of delivered energy.
Automated external defibrillators (AEDs) are now available. n n The simplicity of the AED belies its sophistication; not only can it diagnose and treat VF/VT faster than manual defibrillation methods, but it can also be used by non-medical operators trained in its use. Some AED models are using a biphasic defibrillation waveform. These biphasic models have been shown to be extremely effective at defibrillation using lower levels of delivered energy.
 Early defibrillation n n The key is deep and minimally interrupted chest compressions and getting the AED (automated external defibrillator) or conventional defibrillator used as soon as possible. The 2010 AHA Guidelines recommend the establishment of AED programs in public locations where there is a relatively high likelihood of witnessed cardiac arrest (eg, airports, casinos, sports facilities).
Early defibrillation n n The key is deep and minimally interrupted chest compressions and getting the AED (automated external defibrillator) or conventional defibrillator used as soon as possible. The 2010 AHA Guidelines recommend the establishment of AED programs in public locations where there is a relatively high likelihood of witnessed cardiac arrest (eg, airports, casinos, sports facilities).
 Early defibrillation n Well-done CPR is life-saving, but in America only about 18% of sudden cardiac arrest victims survive after receiving CPR, at best. If effective CPR is not promptly given, the chances for survival decrease by about 10% for every minute of delay until shocked. Studies in America reveal that good chest compressions in terms of depth and rate and uninterrupted are poor even by those trained in CPR.
Early defibrillation n Well-done CPR is life-saving, but in America only about 18% of sudden cardiac arrest victims survive after receiving CPR, at best. If effective CPR is not promptly given, the chances for survival decrease by about 10% for every minute of delay until shocked. Studies in America reveal that good chest compressions in terms of depth and rate and uninterrupted are poor even by those trained in CPR.
 Limit Interruptions in CPR n Chest compressions are crucial n n Oxygen and energy substrate to myocardium Increase chance that rhythm returns Shock may be more effective after CPR A few seconds can increase shock success n n Only stop for breaths, rhythm check, or 1 shock Do not stop for IV access/drug administration/intubation
Limit Interruptions in CPR n Chest compressions are crucial n n Oxygen and energy substrate to myocardium Increase chance that rhythm returns Shock may be more effective after CPR A few seconds can increase shock success n n Only stop for breaths, rhythm check, or 1 shock Do not stop for IV access/drug administration/intubation
 If 1 is good, 2 should be better… n n n Success rate is high for first shock Better defibrillators Minimize CPR interruptions to maintain coronary perfusion pressure
If 1 is good, 2 should be better… n n n Success rate is high for first shock Better defibrillators Minimize CPR interruptions to maintain coronary perfusion pressure
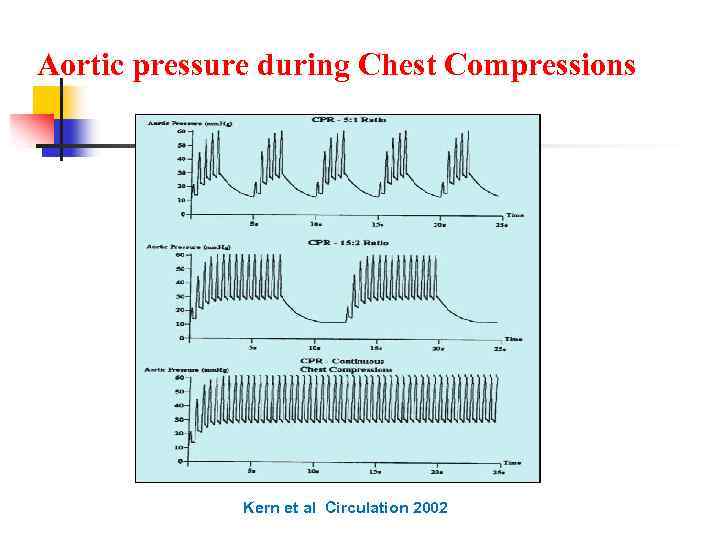 Aortic pressure during Chest Compressions Kern et al Circulation 2002
Aortic pressure during Chest Compressions Kern et al Circulation 2002
 Though the ONLY factors that have a serious impact on chances of survival in the cardiac arrest victim are: Prompt and minimally interrupted “hard, fast, and deep” chest compressions. n Defibrillation as soon as possible. n
Though the ONLY factors that have a serious impact on chances of survival in the cardiac arrest victim are: Prompt and minimally interrupted “hard, fast, and deep” chest compressions. n Defibrillation as soon as possible. n
 §Despite these two most important factors in determining survival, we have almost all been taught the primary importance of Airway and Breathing and IV medications and intubation as soon as possible. §Yet new studies show that pre-Hospital intubation in adult cardiac arrest victims actually results in WORSE outcomes!!!! §Exceptions are newborns and drowning victims or people with known primary airway or respiratory problem.
§Despite these two most important factors in determining survival, we have almost all been taught the primary importance of Airway and Breathing and IV medications and intubation as soon as possible. §Yet new studies show that pre-Hospital intubation in adult cardiac arrest victims actually results in WORSE outcomes!!!! §Exceptions are newborns and drowning victims or people with known primary airway or respiratory problem.
 It is not enough to “do CPR”, but rather to “do CPR right” All the most recent studies reinforce the primary importance of good chest compressions and minimizing delay to defibrillation…. § Airway efforts and rescue breathing should never disrupt good chest compressions unless for only 10 seconds and as seldom as possible.
It is not enough to “do CPR”, but rather to “do CPR right” All the most recent studies reinforce the primary importance of good chest compressions and minimizing delay to defibrillation…. § Airway efforts and rescue breathing should never disrupt good chest compressions unless for only 10 seconds and as seldom as possible.
 Where does all this leave us? 1. Make the FIRST priority prompt “hard, fast and deep” chest compressions that are minimally interrupted. 2. Bystander CPR promptly and “Hands Only” is not only “OK”, it is better until experienced personnel arrive.
Where does all this leave us? 1. Make the FIRST priority prompt “hard, fast and deep” chest compressions that are minimally interrupted. 2. Bystander CPR promptly and “Hands Only” is not only “OK”, it is better until experienced personnel arrive.
 3. Airway devices need to be simplest and easiest, like King Airway, Combitube or LMA, but if good intubator available, do it with less than 10 second interruption in chest compressions. 4. AEDs at all sites of large gatherings, and in more sites in Hospitals, and expand to all/most Police cars as able.
3. Airway devices need to be simplest and easiest, like King Airway, Combitube or LMA, but if good intubator available, do it with less than 10 second interruption in chest compressions. 4. AEDs at all sites of large gatherings, and in more sites in Hospitals, and expand to all/most Police cars as able.
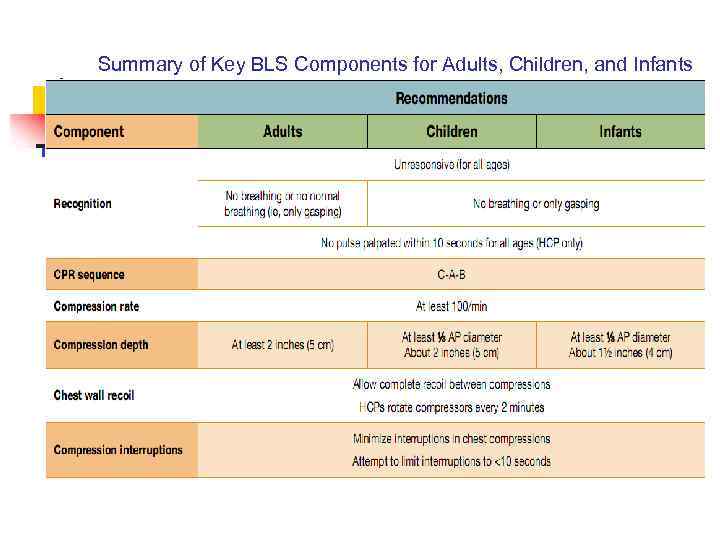 Summary of Key BLS Components for Adults, Children, and Infants
Summary of Key BLS Components for Adults, Children, and Infants
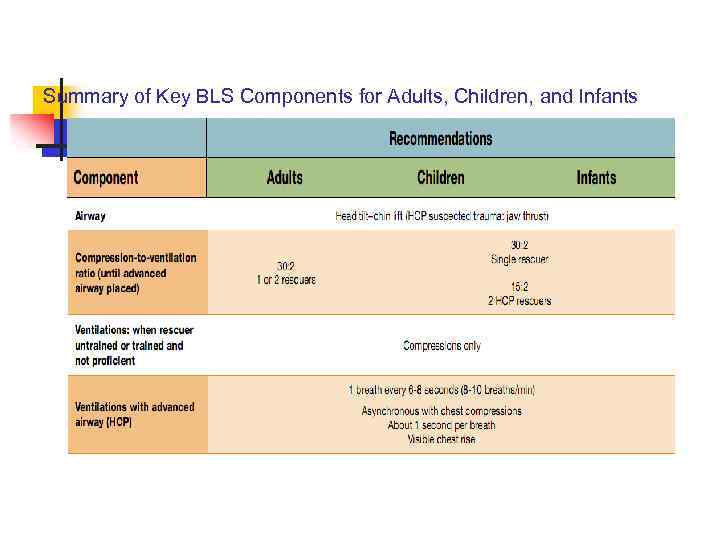 Summary of Key BLS Components for Adults, Children, and Infants
Summary of Key BLS Components for Adults, Children, and Infants
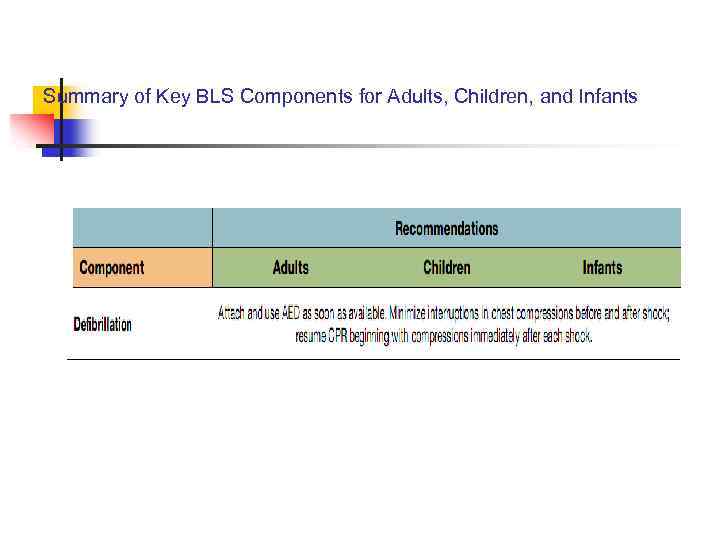 Summary of Key BLS Components for Adults, Children, and Infants
Summary of Key BLS Components for Adults, Children, and Infants
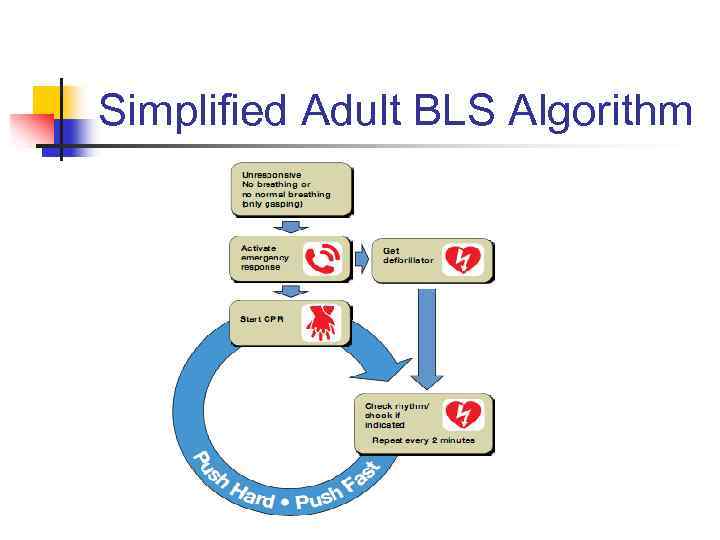 Simplified Adult BLS Algorithm
Simplified Adult BLS Algorithm
 Working in team Basic life support is usually described as a sequence of actions, and this continues to be true for the lone rescuer. n Most healthcare providers (HCP), however, work in teams, and team members typically perform BLS actions simultaneously. n For example, one rescuer immediately initiates chest compressions while another rescuer gets an automated external defibrillator (AED) and calls for help, and a third rescuer opens the airway and provides ventilations. n
Working in team Basic life support is usually described as a sequence of actions, and this continues to be true for the lone rescuer. n Most healthcare providers (HCP), however, work in teams, and team members typically perform BLS actions simultaneously. n For example, one rescuer immediately initiates chest compressions while another rescuer gets an automated external defibrillator (AED) and calls for help, and a third rescuer opens the airway and provides ventilations. n
 Drug Therapy in Cardiac Arrest n n n Epinephrine IV/IO. Dose: 1 mg every 3 -5 minutes. Vasopressin IV/IO. Dose: 40 units can replace first or second dose of epinephrine. Amiodarone IV/IO. Dose: First dose: 300 mg bolus. Second dose: 150 mg.
Drug Therapy in Cardiac Arrest n n n Epinephrine IV/IO. Dose: 1 mg every 3 -5 minutes. Vasopressin IV/IO. Dose: 40 units can replace first or second dose of epinephrine. Amiodarone IV/IO. Dose: First dose: 300 mg bolus. Second dose: 150 mg.
 Epinephrine n n n Epinephrine is used in resuscitation mainly for its αadrenergic receptor stimulant effects. This a-adrenergic action causes peripheral vasoconstriction, raises the systemic vascular resistance, raises the end-diastolic filling pressure and thus improves coronary perfusion. In addition, epinephrine is believed to 'stiffen' the major vessels leading away from the heart, thus aiding in the transmission of the raised intrathoracic pressure and the forward flow of blood (the chest pump theory). Epinephrine also has β-adrenergic receptor activity, stimulating the chronotropic and inotropic receptors of the myocardium.
Epinephrine n n n Epinephrine is used in resuscitation mainly for its αadrenergic receptor stimulant effects. This a-adrenergic action causes peripheral vasoconstriction, raises the systemic vascular resistance, raises the end-diastolic filling pressure and thus improves coronary perfusion. In addition, epinephrine is believed to 'stiffen' the major vessels leading away from the heart, thus aiding in the transmission of the raised intrathoracic pressure and the forward flow of blood (the chest pump theory). Epinephrine also has β-adrenergic receptor activity, stimulating the chronotropic and inotropic receptors of the myocardium.
 Amiodarone n Amiodarone does preventricular arrhythmias and animal studies have demonstrated that it can reduce threshold for defibrillation.
Amiodarone n Amiodarone does preventricular arrhythmias and animal studies have demonstrated that it can reduce threshold for defibrillation.
 Vasopressin n There is little experimental evidence to support the use of other vasopressor drugs, but vasopressin has been shown in clinical trials to significantly raise coronary perfusion pressures and to increase the return of spontaneous circulation rates.
Vasopressin n There is little experimental evidence to support the use of other vasopressor drugs, but vasopressin has been shown in clinical trials to significantly raise coronary perfusion pressures and to increase the return of spontaneous circulation rates.
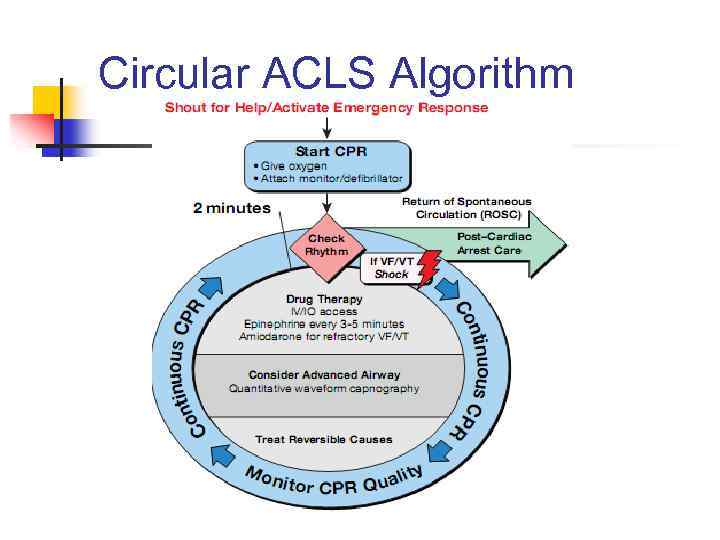 Circular ACLS Algorithm
Circular ACLS Algorithm
![CPR Quality n n n n Push hard (≥ 2 inches [5 cm]) and fast (≥ 100/min) and allow complete chest recoil. Minimize interruptions in compressions. Avoid excessive ventilation. Rotate compressor every 2 minutes. If no advanced airway, CPR Quality n n n n Push hard (≥ 2 inches [5 cm]) and fast (≥ 100/min) and allow complete chest recoil. Minimize interruptions in compressions. Avoid excessive ventilation. Rotate compressor every 2 minutes. If no advanced airway,](https://present5.com/presentation/179166585_148896005/image-73.jpg) CPR Quality n n n n Push hard (≥ 2 inches [5 cm]) and fast (≥ 100/min) and allow complete chest recoil. Minimize interruptions in compressions. Avoid excessive ventilation. Rotate compressor every 2 minutes. If no advanced airway, 30: 2 compression-ventilation ratio. Quantitative waveform capnography: If Pet. CO 2 <10 mm Hg, attempt to improve CPR quality. Intra-arterial pressure: If relaxation phase (diastolic) pressure <20 mm Hg, attempt to improve CPR quality.
CPR Quality n n n n Push hard (≥ 2 inches [5 cm]) and fast (≥ 100/min) and allow complete chest recoil. Minimize interruptions in compressions. Avoid excessive ventilation. Rotate compressor every 2 minutes. If no advanced airway, 30: 2 compression-ventilation ratio. Quantitative waveform capnography: If Pet. CO 2 <10 mm Hg, attempt to improve CPR quality. Intra-arterial pressure: If relaxation phase (diastolic) pressure <20 mm Hg, attempt to improve CPR quality.
 Advanced Airway n n n Supraglottic advanced airway or endotracheal intubation. Waveform capnography to confirm and monitor ET tube placement. 8 -10 breaths per minute with continuous chest compressions.
Advanced Airway n n n Supraglottic advanced airway or endotracheal intubation. Waveform capnography to confirm and monitor ET tube placement. 8 -10 breaths per minute with continuous chest compressions.
 New Medication Protocols n n Atropine is not recommended for routine use in the management of PEA/asystole and has been removed from the ACLS Cardiac Arrest Algorithm. The treatment of PEA/asystole is now consistent in the ACLS and pediatric advanced life support (PALS) recommendations and algorithms.
New Medication Protocols n n Atropine is not recommended for routine use in the management of PEA/asystole and has been removed from the ACLS Cardiac Arrest Algorithm. The treatment of PEA/asystole is now consistent in the ACLS and pediatric advanced life support (PALS) recommendations and algorithms.
 New Medication Protocols n n The algorithm for treatment of tachycardia with pulses has been simplified. Adenosine is recommended in the initial diagnosis and treatment of stable, undifferentiated regular, monomorphic wide-complex tachycardia (this is also consistent in ACLS and PALS recommendations). It is important to note that adenosine should not be used for irregular wide-complex tachycardias because it may cause degeneration of the rhythm to VF.
New Medication Protocols n n The algorithm for treatment of tachycardia with pulses has been simplified. Adenosine is recommended in the initial diagnosis and treatment of stable, undifferentiated regular, monomorphic wide-complex tachycardia (this is also consistent in ACLS and PALS recommendations). It is important to note that adenosine should not be used for irregular wide-complex tachycardias because it may cause degeneration of the rhythm to VF.
 New Medication Protocols n For the treatment of the adult with symptomatic and unstable bradycardia, chronotropic drug infusions are recommended as an alternative to pacing.
New Medication Protocols n For the treatment of the adult with symptomatic and unstable bradycardia, chronotropic drug infusions are recommended as an alternative to pacing.
 Medications During Cardiac Arrest and Shock n The recommendation regarding calcium administration is stronger than in past AHA Guidelines: routine calcium administration is not recommended for pediatric cardiopulmonary arrest in the absence of documented hypocalcemia, calcium channel blocker overdose, hypermagnesemia, or hyperkalemia. Routine calcium administration in cardiac arrest provides no benefit and may be harmful.
Medications During Cardiac Arrest and Shock n The recommendation regarding calcium administration is stronger than in past AHA Guidelines: routine calcium administration is not recommended for pediatric cardiopulmonary arrest in the absence of documented hypocalcemia, calcium channel blocker overdose, hypermagnesemia, or hyperkalemia. Routine calcium administration in cardiac arrest provides no benefit and may be harmful.
 Medications During Cardiac Arrest and Shock n n Etomidate has been shown to facilitate endotracheal intubation in infants and children with minimal hemodynamic effect but is not recommended for routine use in pediatric patients with evidence of septic shock. Etomidate causes adrenal suppression, and the endogenous steroid response may be critically important in patients with septic shock.
Medications During Cardiac Arrest and Shock n n Etomidate has been shown to facilitate endotracheal intubation in infants and children with minimal hemodynamic effect but is not recommended for routine use in pediatric patients with evidence of septic shock. Etomidate causes adrenal suppression, and the endogenous steroid response may be critically important in patients with septic shock.
 ACTIONS TO BE TAKEN DURING CPR n
ACTIONS TO BE TAKEN DURING CPR n
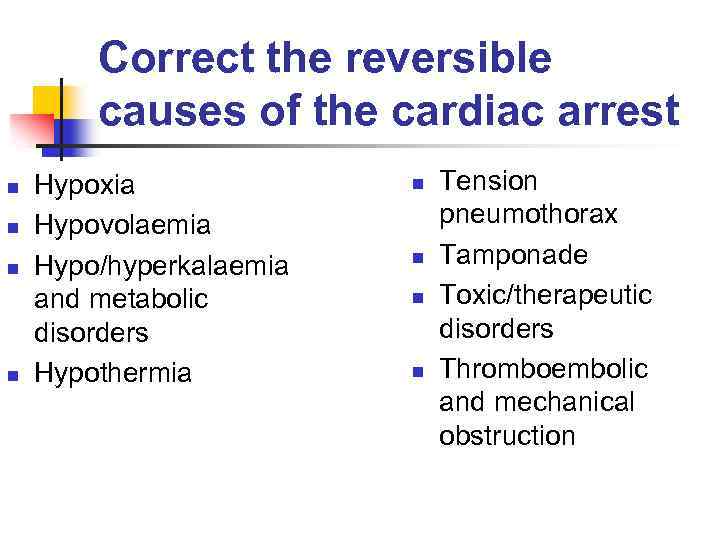 Correct the reversible causes of the cardiac arrest n n Hypoxia Hypovolaemia Hypo/hyperkalaemia and metabolic disorders Hypothermia n n Tension pneumothorax Tamponade Toxic/therapeutic disorders Thromboembolic and mechanical obstruction
Correct the reversible causes of the cardiac arrest n n Hypoxia Hypovolaemia Hypo/hyperkalaemia and metabolic disorders Hypothermia n n Tension pneumothorax Tamponade Toxic/therapeutic disorders Thromboembolic and mechanical obstruction
 Check the electrode/paddle position and contact. n n n Electrocardiographic rhythm assessment is fundamental to the use of the ALS algorithm. Therefore, it is essential to ensure that the electrode/paddles are positioned correctly and have effective contact. Rhythms associated with cardiac arrest can be mimicked by movement artefact, lead disconnection and electrical interference.
Check the electrode/paddle position and contact. n n n Electrocardiographic rhythm assessment is fundamental to the use of the ALS algorithm. Therefore, it is essential to ensure that the electrode/paddles are positioned correctly and have effective contact. Rhythms associated with cardiac arrest can be mimicked by movement artefact, lead disconnection and electrical interference.
 Airway and O 2 n n Securing the airway and ventilation of the lungs with a high concentration of inspired oxygen are of major importance. Ventilation can be carried out using a self-inflating bag, valve and mask. The level of inspired oxygen can be raised to 50% by attaching an oxygen supply at 5 -6 L/min directly to the bag, or to 90% by increasing the oxygen flow rate to 8 -10 L/min and adding an oxygen reservoir bag. An oral or nasal airway may be inserted to improve the efficiency of bag, valve, mask ventilation.
Airway and O 2 n n Securing the airway and ventilation of the lungs with a high concentration of inspired oxygen are of major importance. Ventilation can be carried out using a self-inflating bag, valve and mask. The level of inspired oxygen can be raised to 50% by attaching an oxygen supply at 5 -6 L/min directly to the bag, or to 90% by increasing the oxygen flow rate to 8 -10 L/min and adding an oxygen reservoir bag. An oral or nasal airway may be inserted to improve the efficiency of bag, valve, mask ventilation.
 Tracheal intubation is the method of choice for securing the airway. n n Tracheal intubation ensures that oxygen is delivered directly to the lungs, eliminates leaks and gastric insufflation and protects the airway from the regurgitation of gastric contents. When tracheal intubation has not been achieved, a laryngeal mask airway can be inserted. Paramedics, nurses and doctors not experienced in tracheal intubation can learn the technique of insertion of a laryngeal mask airway in a few hours. Whilst the laryngeal mask does not provide full airway protection, it does provide a more effective airway and ventilation than the bag, valve and mask system.
Tracheal intubation is the method of choice for securing the airway. n n Tracheal intubation ensures that oxygen is delivered directly to the lungs, eliminates leaks and gastric insufflation and protects the airway from the regurgitation of gastric contents. When tracheal intubation has not been achieved, a laryngeal mask airway can be inserted. Paramedics, nurses and doctors not experienced in tracheal intubation can learn the technique of insertion of a laryngeal mask airway in a few hours. Whilst the laryngeal mask does not provide full airway protection, it does provide a more effective airway and ventilation than the bag, valve and mask system.
 Venous access n n n This is required to provide the optimal method of drug delivery. Attempts should be made to cannulate a large peripheral vein with a 14 G or 16 G cannula. Drugs administered via the peripheral route should be flushed with a 20 ml bolus of normal saline (0. 9%). Central venous cannulation requires expertise and training. It does provide significant advantages over peripheral access in terms of the speed of delivery and the pharmacological action of drugs.
Venous access n n n This is required to provide the optimal method of drug delivery. Attempts should be made to cannulate a large peripheral vein with a 14 G or 16 G cannula. Drugs administered via the peripheral route should be flushed with a 20 ml bolus of normal saline (0. 9%). Central venous cannulation requires expertise and training. It does provide significant advantages over peripheral access in terms of the speed of delivery and the pharmacological action of drugs.
 Do I need a central line? n n Not mandatory Do not interrupt CPR Options: PIV/IO/ETT If PIV/IO and still no spontaneous circulation, consider central line
Do I need a central line? n n Not mandatory Do not interrupt CPR Options: PIV/IO/ETT If PIV/IO and still no spontaneous circulation, consider central line
 Antiarrhythmic drugs n The use of antiarrhythmic drugs has been recommended to aid electrical defibrillation, to prevent the reoccurrence of ventricular fibrillation and to terminate serious electrical arrhythmias.
Antiarrhythmic drugs n The use of antiarrhythmic drugs has been recommended to aid electrical defibrillation, to prevent the reoccurrence of ventricular fibrillation and to terminate serious electrical arrhythmias.
 Lidocaine n n n Lidocaine has been used in the treatment of resistant ventricular fibrillation. Clinical trials and animal studies have shown that lidocaine offers no improvement in survival from ventricular fibrillation and may actually raise threshold for defibrillation. Lidocaine is advocated to prevent the reoccurrence of ventricular fibrillation after successful defibrillation.
Lidocaine n n n Lidocaine has been used in the treatment of resistant ventricular fibrillation. Clinical trials and animal studies have shown that lidocaine offers no improvement in survival from ventricular fibrillation and may actually raise threshold for defibrillation. Lidocaine is advocated to prevent the reoccurrence of ventricular fibrillation after successful defibrillation.
 Bretylium n n n Bretylium has been used as a pharmacological defibrillator. It elevates the onset threshold for ventricular fibrillation and may lower the defibrillation threshold. Bretylium has a slow-onset time course and may take up to 20 min to be fully effective. In the post-resuscitation phase, it may cause profound hypotension and EMD. Clinical trials using bretylium have not demonstrated any significant clinical benefit.
Bretylium n n n Bretylium has been used as a pharmacological defibrillator. It elevates the onset threshold for ventricular fibrillation and may lower the defibrillation threshold. Bretylium has a slow-onset time course and may take up to 20 min to be fully effective. In the post-resuscitation phase, it may cause profound hypotension and EMD. Clinical trials using bretylium have not demonstrated any significant clinical benefit.
 Amiodarone n Amiodarone does preventricular arrhythmias and animal studies have demonstrated that it can reduce threshold for defibrillation.
Amiodarone n Amiodarone does preventricular arrhythmias and animal studies have demonstrated that it can reduce threshold for defibrillation.
 Atropine n n Atropine is a parasympathetic nerve blocker and is used to counter increased vagal tone. Its use is well established in peri-arrest arrhythmias, but the evidence for its use in cardiac arrest is equivocal. As atropine is not considered to have any serious adverse effects, it may be given as a single dose of 3 mg intravenously. This dose is sufficient to effectively block vagal activity.
Atropine n n Atropine is a parasympathetic nerve blocker and is used to counter increased vagal tone. Its use is well established in peri-arrest arrhythmias, but the evidence for its use in cardiac arrest is equivocal. As atropine is not considered to have any serious adverse effects, it may be given as a single dose of 3 mg intravenously. This dose is sufficient to effectively block vagal activity.
 Pacing n n Electrical pacing of the heart can be attempted where there is P-wave activity evident. Percutaneous or pervenous pacing can be attempted depending on the local skills and available equipment. Although pacing has been of benefit in the emergency management of severe bradycardias, it has not been shown to be successful in asystole. This may be a failure in technique or, alternatively, it may be that pacing is only considered at too late a stage in the resuscitation sequence, probably when the myocardium is beyond electrical stimulation.
Pacing n n Electrical pacing of the heart can be attempted where there is P-wave activity evident. Percutaneous or pervenous pacing can be attempted depending on the local skills and available equipment. Although pacing has been of benefit in the emergency management of severe bradycardias, it has not been shown to be successful in asystole. This may be a failure in technique or, alternatively, it may be that pacing is only considered at too late a stage in the resuscitation sequence, probably when the myocardium is beyond electrical stimulation.
 Buffers n n n In prolonged resuscitation the patient may become increasingly acidotic. This is especially so when initial basic life support has been delayed, ventilation has not been performed effectively (respiratory acidosis) or chest compressions have not been successful in achieving a satisfactory flow of blood (metabolic acidosis). In most cases, establishing effective basic life support maintains the acid-base status quo without further intervention.
Buffers n n n In prolonged resuscitation the patient may become increasingly acidotic. This is especially so when initial basic life support has been delayed, ventilation has not been performed effectively (respiratory acidosis) or chest compressions have not been successful in achieving a satisfactory flow of blood (metabolic acidosis). In most cases, establishing effective basic life support maintains the acid-base status quo without further intervention.
 Buffers n n n Where basic life support procedures have been established and the patient's lungs have been effectively ventilated, any associated acidosis may be reversed pharmacologically by administration of buffer solution such as sodium bicarbonate solution. There is little evidence to support the routine administration of buffers. A volume of 22. 4 ml of gaseous carbon dioxide is produced for every 1 mmol of carbon dioxide produced by buffering activity. Therefore, if the lungs are not perfused and ventilated effectively, a severe respiratory acidosis occurs.
Buffers n n n Where basic life support procedures have been established and the patient's lungs have been effectively ventilated, any associated acidosis may be reversed pharmacologically by administration of buffer solution such as sodium bicarbonate solution. There is little evidence to support the routine administration of buffers. A volume of 22. 4 ml of gaseous carbon dioxide is produced for every 1 mmol of carbon dioxide produced by buffering activity. Therefore, if the lungs are not perfused and ventilated effectively, a severe respiratory acidosis occurs.
 Buffers n n Furthermore, rapid diffusion of carbon dioxide into cells results in a paradoxical intracellular acidosis. Finally, the hyperosmolarity and high sodium ion concentrations in sodium bicarbonate solution may exacerbate cerebral edema. The recommendation for the use of buffers is therefore limited to severe acidosis, where the p. H is less than 7. 1 and the base excess is greater than -10 mmol/L. Sodium bicarbonate is usually administered as an intravenous 50 ml bolus of an 8. 4% solution (50 mmol of HCO 3 - ion).
Buffers n n Furthermore, rapid diffusion of carbon dioxide into cells results in a paradoxical intracellular acidosis. Finally, the hyperosmolarity and high sodium ion concentrations in sodium bicarbonate solution may exacerbate cerebral edema. The recommendation for the use of buffers is therefore limited to severe acidosis, where the p. H is less than 7. 1 and the base excess is greater than -10 mmol/L. Sodium bicarbonate is usually administered as an intravenous 50 ml bolus of an 8. 4% solution (50 mmol of HCO 3 - ion).
 Buffers n n Following administration of sodium bicarbonate, the intravenous cannula must be flushed carefully, as residual sodium bicarbonate inactivates epinephrine administered subsequently. Sodium bicarbonate is only recommended routinely in patients with pre-existing metabolic acidosis, hyperkalaemia, or tricyclic antidepressant or phenobarbital overdose.
Buffers n n Following administration of sodium bicarbonate, the intravenous cannula must be flushed carefully, as residual sodium bicarbonate inactivates epinephrine administered subsequently. Sodium bicarbonate is only recommended routinely in patients with pre-existing metabolic acidosis, hyperkalaemia, or tricyclic antidepressant or phenobarbital overdose.
 PERI-ARREST ARRHYTHMIAS n n n The guidelines for management of these arrhythmias are presented in three algorithms. These algorithms do not provide a treatment strategy for every known peri-arrest rhythm but merely provide a guide to the initial recognition and management of these arrhythmias. It must be emphasized that where the clinician does not have the required experience or skill, further expert help must be summoned.
PERI-ARREST ARRHYTHMIAS n n n The guidelines for management of these arrhythmias are presented in three algorithms. These algorithms do not provide a treatment strategy for every known peri-arrest rhythm but merely provide a guide to the initial recognition and management of these arrhythmias. It must be emphasized that where the clinician does not have the required experience or skill, further expert help must be summoned.
 Bradycardia n n n A bradycardia is defined as a ventricular rate of below 60 beats/min. If there is a risk of asystole, pace immediately; if there is no perceived risk of asystole but the haemodynamic state of the patient is poor, give atropine and pace only if this is ineffective. If there is no perceived risk of asystole and the patient is not compromised haemodynamically to an important degree then only observation is required.
Bradycardia n n n A bradycardia is defined as a ventricular rate of below 60 beats/min. If there is a risk of asystole, pace immediately; if there is no perceived risk of asystole but the haemodynamic state of the patient is poor, give atropine and pace only if this is ineffective. If there is no perceived risk of asystole and the patient is not compromised haemodynamically to an important degree then only observation is required.
 Broad complex tachycardia n n n A broad complex tachycardia is nearly always ventricular in origin. However, it may be difficult to distinguish a rapid broad complex tachycardia from a supraventricular tachycardia. Little harm results if a supraventricular tachycardia is treated as a ventricular one, whereas the converse may result in very serious consequences.
Broad complex tachycardia n n n A broad complex tachycardia is nearly always ventricular in origin. However, it may be difficult to distinguish a rapid broad complex tachycardia from a supraventricular tachycardia. Little harm results if a supraventricular tachycardia is treated as a ventricular one, whereas the converse may result in very serious consequences.
 Broad complex tachycardia n n n If there is no pulse as a result of the arrhythmia the condition should be treated as cardiac arrest using the ventricular fibrillation/ventricular tachycardia protocol for cardiac arrest. If there is a pulse but inadequate perfusion then cardioversion is required as soon as possible. If there is a broad complex tachycardia without adverse haemodynamic disturbance then routine antiarrhythmic therapy should be used with cardioversion only if this fails.
Broad complex tachycardia n n n If there is no pulse as a result of the arrhythmia the condition should be treated as cardiac arrest using the ventricular fibrillation/ventricular tachycardia protocol for cardiac arrest. If there is a pulse but inadequate perfusion then cardioversion is required as soon as possible. If there is a broad complex tachycardia without adverse haemodynamic disturbance then routine antiarrhythmic therapy should be used with cardioversion only if this fails.
 Narrow complex tachycardia n n n A narrow complex tachycardia is nearly always a supraventricular arrhythmia. Although a narrow complex tachycardia is generally regarded as less hazardous than a broad complex tachycardia, it is a recognized trigger for ventricular fibrillation in susceptible patients. For regular arrhythmic supraventricular tachycardias (that almost always have heart rates faster than 140/min), vagal manoeuvres or adenosine may be tried first, but if these are not successful, in the presence of adverse signs the recommended strategy is cardioversion. Without adverse signs there is a choice of routine antiarrhythmics that include a short acting β-blocker, digoxin, verapamil and amiodarone. Atrial fibrillation is a special case: rigid guidelines cannot be readily applied, and expert help may be prudent when the rate is persistently over 130 beats/min.
Narrow complex tachycardia n n n A narrow complex tachycardia is nearly always a supraventricular arrhythmia. Although a narrow complex tachycardia is generally regarded as less hazardous than a broad complex tachycardia, it is a recognized trigger for ventricular fibrillation in susceptible patients. For regular arrhythmic supraventricular tachycardias (that almost always have heart rates faster than 140/min), vagal manoeuvres or adenosine may be tried first, but if these are not successful, in the presence of adverse signs the recommended strategy is cardioversion. Without adverse signs there is a choice of routine antiarrhythmics that include a short acting β-blocker, digoxin, verapamil and amiodarone. Atrial fibrillation is a special case: rigid guidelines cannot be readily applied, and expert help may be prudent when the rate is persistently over 130 beats/min.
 When to stop? n n CPR should be continued while VF is present on ECG, that keeps a minimal miocardial metabolism and possibility of circulation restoring. In cases of asystole or pulseless electrical activity, if the reversible causes of the cardiac arrest are excluded, CPR should be stopped after 30 min ineffective efforts. More prolonged CPR is required in hypothermic patients, in cases of medicaments' overdosing. The time of stopping CPR should be fixed as the time of patient's death.
When to stop? n n CPR should be continued while VF is present on ECG, that keeps a minimal miocardial metabolism and possibility of circulation restoring. In cases of asystole or pulseless electrical activity, if the reversible causes of the cardiac arrest are excluded, CPR should be stopped after 30 min ineffective efforts. More prolonged CPR is required in hypothermic patients, in cases of medicaments' overdosing. The time of stopping CPR should be fixed as the time of patient's death.
 When to Stop? n You must make a conscientious and competent effort to resuscitate. n Good clinical judgment. n Respect for human dignity.
When to Stop? n You must make a conscientious and competent effort to resuscitate. n Good clinical judgment. n Respect for human dignity.
 Post-arrest condition n n Coma >48 h is the predictor of bad neurologic outcome. If in 72 h after cardiac arrest unconsciousness ≤ 5 by Glasgow scale, absence of motor reaction to pain and photoreaction of pupil's – it is the predictor of persisting vegetable state.
Post-arrest condition n n Coma >48 h is the predictor of bad neurologic outcome. If in 72 h after cardiac arrest unconsciousness ≤ 5 by Glasgow scale, absence of motor reaction to pain and photoreaction of pupil's – it is the predictor of persisting vegetable state.
 Initial and Later Key Objectives of Post–Cardiac Arrest Care n n n Optimize cardiopulmonary function and vital organ perfusion. Transport/transfer to an appropriate hospital or critical care unit with a comprehensive post–cardiac arrest treatment system of care. Identify and treat acute cardiac syndrome (ACS) and other reversible causes. Control temperature to optimize neurologic recovery. Anticipate, treat, and prevent multiple organ dysfunction. This includes avoiding excessive ventilation and hyperoxia.
Initial and Later Key Objectives of Post–Cardiac Arrest Care n n n Optimize cardiopulmonary function and vital organ perfusion. Transport/transfer to an appropriate hospital or critical care unit with a comprehensive post–cardiac arrest treatment system of care. Identify and treat acute cardiac syndrome (ACS) and other reversible causes. Control temperature to optimize neurologic recovery. Anticipate, treat, and prevent multiple organ dysfunction. This includes avoiding excessive ventilation and hyperoxia.
 Post-resuscitation treatment: circulation n Because of brain autoreculation falling the level of cerebral perfusion pressure (CPP) became depended on medial arterial blood pressure (APm): CPP = APm – ICP (intracranial pressure). So it is important to maintain the APm = 70 – 90 mm Hg. CVP (central venous pressure) = 8 – 12 cm H 2 O.
Post-resuscitation treatment: circulation n Because of brain autoreculation falling the level of cerebral perfusion pressure (CPP) became depended on medial arterial blood pressure (APm): CPP = APm – ICP (intracranial pressure). So it is important to maintain the APm = 70 – 90 mm Hg. CVP (central venous pressure) = 8 – 12 cm H 2 O.
 Post-resuscitation treatment: oxygenation n Arterial hyperoxia should be avoided; The level of Fi. O 2 must support Sa. O 2 = 94 -96%; Artificial ventilation with Fi. O 2 = 1, 0 during the first hour of post-resuscitation period is associated with poor neurologic outcome due to oxidative stress in neurons.
Post-resuscitation treatment: oxygenation n Arterial hyperoxia should be avoided; The level of Fi. O 2 must support Sa. O 2 = 94 -96%; Artificial ventilation with Fi. O 2 = 1, 0 during the first hour of post-resuscitation period is associated with poor neurologic outcome due to oxidative stress in neurons.
 Post-resuscitation treatment: normoxemia, normocapnia Maintain normal Pa. O 2 and Pa. CO 2. n The vasoconstriction due to hyperventilation just as intracranial hypertension due to hypoventilation lead to cerebral ischemia aggravation. n
Post-resuscitation treatment: normoxemia, normocapnia Maintain normal Pa. O 2 and Pa. CO 2. n The vasoconstriction due to hyperventilation just as intracranial hypertension due to hypoventilation lead to cerebral ischemia aggravation. n
 Post-resuscitation treatment: hypothermia or normothermia n n n Hypertermia >39⁰С during the first 72 h after cardiac arrest increases the mortality. Hypertermia is associated with poor neurologic outcome. Unconcious patients after CPR need hypotermia at 32 -34 ⁰С during 12 -24 h.
Post-resuscitation treatment: hypothermia or normothermia n n n Hypertermia >39⁰С during the first 72 h after cardiac arrest increases the mortality. Hypertermia is associated with poor neurologic outcome. Unconcious patients after CPR need hypotermia at 32 -34 ⁰С during 12 -24 h.
 Side effects of hypothermia Increasing blood viscosity; n Poliuriae without renal dysfunction; n Pneumonia; n Arrhythmia. n
Side effects of hypothermia Increasing blood viscosity; n Poliuriae without renal dysfunction; n Pneumonia; n Arrhythmia. n
 Contraindications to hypothermia n n n Pregnancy; Cardiogenic shock (systolic AP <90 mm Hg with adrenomimetic infusion); Overdosing of medicaments, especially opioids.
Contraindications to hypothermia n n n Pregnancy; Cardiogenic shock (systolic AP <90 mm Hg with adrenomimetic infusion); Overdosing of medicaments, especially opioids.
 Monitoring during hypothermia n n n Internal (esophageal, tympanic, rectal) and external temperature ; Coagulation parameters; Blood gases; Electrolytes; Glucose and lactate; Hemodynamic parameters.
Monitoring during hypothermia n n n Internal (esophageal, tympanic, rectal) and external temperature ; Coagulation parameters; Blood gases; Electrolytes; Glucose and lactate; Hemodynamic parameters.
 Methods of hypothermia n n n n Duration – 12 -24 h. Internal goal temperature = 32 -34 ⁰С. External hypotherm; IV infusion of 0, 9% Na. Cl or Ringer-Lactate, with t = 4 ⁰С, dose 30 ml/kg in temp 100 ml/min; Artificial ventilation. Preventing of cold trembling – analgosedatics, relaxants, vasodilatators (nitrates). Slow warming – 0, 2 -0, 5 ⁰С/h at the end of hypothermia.
Methods of hypothermia n n n n Duration – 12 -24 h. Internal goal temperature = 32 -34 ⁰С. External hypotherm; IV infusion of 0, 9% Na. Cl or Ringer-Lactate, with t = 4 ⁰С, dose 30 ml/kg in temp 100 ml/min; Artificial ventilation. Preventing of cold trembling – analgosedatics, relaxants, vasodilatators (nitrates). Slow warming – 0, 2 -0, 5 ⁰С/h at the end of hypothermia.
 Post-resuscitation treatment: normoglycemia n n n Hyperglycemia is associated with poor neurologic outcome. Glycemia > 10 mmol/l must be corrected with insulin. Hypoglycemia must be avoided.
Post-resuscitation treatment: normoglycemia n n n Hyperglycemia is associated with poor neurologic outcome. Glycemia > 10 mmol/l must be corrected with insulin. Hypoglycemia must be avoided.
 Post-resuscitation treatment: moderate hemodilution The blood viscosity is increased in post-resuscitation period. n Ht = 30 – 35% will be optimal. n
Post-resuscitation treatment: moderate hemodilution The blood viscosity is increased in post-resuscitation period. n Ht = 30 – 35% will be optimal. n
 Post-resuscitation treatment: seizure control Benzodiazepine, phenytoine, valproate. n In cases of consistent epileptic activity – thiopental. n
Post-resuscitation treatment: seizure control Benzodiazepine, phenytoine, valproate. n In cases of consistent epileptic activity – thiopental. n
 Post-resuscitation treatment: the goal parameters n n n n n APm = 70 – 90 mm Hg. CVP = 8 – 12 cm H 20. Hb > 100 g/l. Lactate < 2, 0 mmol/l. t internal = 32 -34 ⁰С during the first 12 -24 h, then normothermia. Sa. O 2 = 94 -96%. Sv. O 2 = 65 -75%. DO 2 (delivery) = 400 -500 ml/min/m 2. VO 2 (consumption) > 90 ml/min/m 2. Avoid the dependence of VO 2 on DO 2.
Post-resuscitation treatment: the goal parameters n n n n n APm = 70 – 90 mm Hg. CVP = 8 – 12 cm H 20. Hb > 100 g/l. Lactate < 2, 0 mmol/l. t internal = 32 -34 ⁰С during the first 12 -24 h, then normothermia. Sa. O 2 = 94 -96%. Sv. O 2 = 65 -75%. DO 2 (delivery) = 400 -500 ml/min/m 2. VO 2 (consumption) > 90 ml/min/m 2. Avoid the dependence of VO 2 on DO 2.
 Possible tissue and organ donation n Because of the growing need for transplant tissue and organs, all provider teams who treat postarrest patients should implement appropriate procedures for possible tissue and organ donation that are timely, effective, and supportive of the family members’ and patient’s desires.
Possible tissue and organ donation n Because of the growing need for transplant tissue and organs, all provider teams who treat postarrest patients should implement appropriate procedures for possible tissue and organ donation that are timely, effective, and supportive of the family members’ and patient’s desires.
 Return of Spontaneous Circulation (ROSC) n n n Pulse and blood pressure. Abrupt sustained increase in Pet. CO 2 (typically ≥ 40 mm Hg). Spontaneous arterial pressure waves with intra-arterial monitoring.
Return of Spontaneous Circulation (ROSC) n n n Pulse and blood pressure. Abrupt sustained increase in Pet. CO 2 (typically ≥ 40 mm Hg). Spontaneous arterial pressure waves with intra-arterial monitoring.
 NEONATAL RESUSCITATION n Neonatal cardiac arrest is predominantly asphyxial, so the A-B-C resuscitation sequence with a 3: 1 compression-toventilation ratio has been maintained except when the etiology is clearly cardiac.
NEONATAL RESUSCITATION n Neonatal cardiac arrest is predominantly asphyxial, so the A-B-C resuscitation sequence with a 3: 1 compression-toventilation ratio has been maintained except when the etiology is clearly cardiac.
 NEONATAL RESUSCITATION n n Once positive-pressure ventilation or supplementary oxygen administration is begun, assessment should consist of simultaneous evaluation of 3 clinical characteristics: heart rate, respiratory rate, and evaluation of the state of oxygenation. State of oxygenation is optimally determined by a pulse oximeter rather than by simple assessment of color.
NEONATAL RESUSCITATION n n Once positive-pressure ventilation or supplementary oxygen administration is begun, assessment should consist of simultaneous evaluation of 3 clinical characteristics: heart rate, respiratory rate, and evaluation of the state of oxygenation. State of oxygenation is optimally determined by a pulse oximeter rather than by simple assessment of color.
 NEONATAL RESUSCITATION n n n Pulse oxymetry, with the probe attached to the right upper extremity, should be used to assess any need for supplementary oxygen. For babies born at term, it is best to begin resuscitation with air rather than 100% oxygen. Administration of supplementary oxygen should be regulated by blending oxygen and air, and the amount to be delivered should be guided by oxymetry monitored from the right upper extremity (i. e. , usually the wrist or palm).
NEONATAL RESUSCITATION n n n Pulse oxymetry, with the probe attached to the right upper extremity, should be used to assess any need for supplementary oxygen. For babies born at term, it is best to begin resuscitation with air rather than 100% oxygen. Administration of supplementary oxygen should be regulated by blending oxygen and air, and the amount to be delivered should be guided by oxymetry monitored from the right upper extremity (i. e. , usually the wrist or palm).
 NEONATAL RESUSCITATION n n Evidence is now strong that healthy babies born at term start with an arterial oxyhemoglobin saturation of <60% and can require more than 10 minutes to reach saturations of >90%. Hyperoxia can be toxic, particularly to the preterm baby.
NEONATAL RESUSCITATION n n Evidence is now strong that healthy babies born at term start with an arterial oxyhemoglobin saturation of <60% and can require more than 10 minutes to reach saturations of >90%. Hyperoxia can be toxic, particularly to the preterm baby.
 NEONATAL RESUSCITATION n n n Suctioning immediately after birth (including suctioning with a bulb syringe) should be reserved for babies who have an obvious obstruction to spontaneous breathing or require positive-pressure ventilation. There is no evidence that active babies benefit from airway suctioning, even in the presence of meconium, and there is evidence of risk associated with this suctioning. The available evidence does not support or refute the routine endotracheal suctioning of depressed infants born through meconium-stained amniotic fluid.
NEONATAL RESUSCITATION n n n Suctioning immediately after birth (including suctioning with a bulb syringe) should be reserved for babies who have an obvious obstruction to spontaneous breathing or require positive-pressure ventilation. There is no evidence that active babies benefit from airway suctioning, even in the presence of meconium, and there is evidence of risk associated with this suctioning. The available evidence does not support or refute the routine endotracheal suctioning of depressed infants born through meconium-stained amniotic fluid.
 NEONATAL RESUSCITATION: Ventilation Strategies n Use of the laryngeal mask airway should be considered if face-mask ventilation is unsuccessful and tracheal intubation is unsuccessful or not feasible.
NEONATAL RESUSCITATION: Ventilation Strategies n Use of the laryngeal mask airway should be considered if face-mask ventilation is unsuccessful and tracheal intubation is unsuccessful or not feasible.
 NEONATAL RESUSCITATION: Ventilation Strategies n n n Positive-pressure ventilation should be administered with sufficient pressure to increase the heart rate or create chest expansion; excessive pressure can seriously injure the preterm lung. However, the optimum pressure, inflation time, tidal volumes, and amount of positive end-expiratory pressure required to establish an effective functional residual capacity have not been defined. Continuous positive airway pressure may be helpful in the transitioning of the preterm baby.
NEONATAL RESUSCITATION: Ventilation Strategies n n n Positive-pressure ventilation should be administered with sufficient pressure to increase the heart rate or create chest expansion; excessive pressure can seriously injure the preterm lung. However, the optimum pressure, inflation time, tidal volumes, and amount of positive end-expiratory pressure required to establish an effective functional residual capacity have not been defined. Continuous positive airway pressure may be helpful in the transitioning of the preterm baby.
 NEONATAL RESUSCITATION: Compression-to-Ventilation Ratio n n n The optimal compression-to-ventilation ratio remains unknown. The 3: 1 ratio for newborns facilitates provision of adequate minute ventilation, which is considered critical for the vast majority of newborns who have an asphyxial arrest. The consideration of a 15: 2 ratio (for 2 rescuers) recognizes that newborns with a cardiac etiology of arrest may benefit from a higher compression-to-ventilation ratio.
NEONATAL RESUSCITATION: Compression-to-Ventilation Ratio n n n The optimal compression-to-ventilation ratio remains unknown. The 3: 1 ratio for newborns facilitates provision of adequate minute ventilation, which is considered critical for the vast majority of newborns who have an asphyxial arrest. The consideration of a 15: 2 ratio (for 2 rescuers) recognizes that newborns with a cardiac etiology of arrest may benefit from a higher compression-to-ventilation ratio.
 NEONATAL RESUSCITATION: Delayed Cord Clamping n n There is increasing evidence of benefit of delaying cord clamping for at least 1 minute in term and preterm infants not requiring resuscitation. There is insufficient evidence to support or refute a recommendation to delay cord clamping in babies requiring resuscitation.
NEONATAL RESUSCITATION: Delayed Cord Clamping n n There is increasing evidence of benefit of delaying cord clamping for at least 1 minute in term and preterm infants not requiring resuscitation. There is insufficient evidence to support or refute a recommendation to delay cord clamping in babies requiring resuscitation.
 Withholding or Discontinuing Resuscitative Efforts in infants n n In a newly born baby with no detectable heart rate, which remains undetectable for 10 minutes, it is appropriate to consider stopping resuscitation. The decision to continue resuscitation efforts beyond 10 minutes of no heart rate should take into consideration factors such as the presumed etiology of the arrest, the gestation of the baby, the presence or absence of complications, the potential role of therapeutic hypothermia, and the parents’ previously expressed feelings about acceptable risk of morbidity.
Withholding or Discontinuing Resuscitative Efforts in infants n n In a newly born baby with no detectable heart rate, which remains undetectable for 10 minutes, it is appropriate to consider stopping resuscitation. The decision to continue resuscitation efforts beyond 10 minutes of no heart rate should take into consideration factors such as the presumed etiology of the arrest, the gestation of the baby, the presence or absence of complications, the potential role of therapeutic hypothermia, and the parents’ previously expressed feelings about acceptable risk of morbidity.
 Withholding or Discontinuing Resuscitative Efforts in infants n When gestation, birth weight, or congenital anomalies are associated with almost certain early death and an unacceptably high morbidity is likely among the rare survivors, resuscitation is not indicated.
Withholding or Discontinuing Resuscitative Efforts in infants n When gestation, birth weight, or congenital anomalies are associated with almost certain early death and an unacceptably high morbidity is likely among the rare survivors, resuscitation is not indicated.
 Terminating Resuscitative Efforts in Adults With Out-of-Hospital Cardiac Arrest n n For adults experiencing out-of-hospital cardiac arrest who are receiving only BLS, the “BLS termination of resuscitation rule” was established to consider terminating BLS support before ambulance transport if all of the following criteria are met: Arrest not witnessed by EMS provider or first responder; No ROSC (return of spontaneous circulation) after 3 complete rounds of CPR and AED analyses; No AED shocks delivered;
Terminating Resuscitative Efforts in Adults With Out-of-Hospital Cardiac Arrest n n For adults experiencing out-of-hospital cardiac arrest who are receiving only BLS, the “BLS termination of resuscitation rule” was established to consider terminating BLS support before ambulance transport if all of the following criteria are met: Arrest not witnessed by EMS provider or first responder; No ROSC (return of spontaneous circulation) after 3 complete rounds of CPR and AED analyses; No AED shocks delivered;
 Terminating Resuscitative Efforts in Adults With Out-of-Hospital Cardiac Arrest n n n For situations when ALS EMS personnel are present to provide care for an adult with out-of-hospital cardiac arrest, an “ALS termination of resuscitation” rule was established to consider terminating resuscitative efforts before ambulance transport if all of the following criteria are met: Arrest not witnessed (by anyone); No bystander CPR provided; No ROSC after complete ALS care in the field; No shocks delivered.
Terminating Resuscitative Efforts in Adults With Out-of-Hospital Cardiac Arrest n n n For situations when ALS EMS personnel are present to provide care for an adult with out-of-hospital cardiac arrest, an “ALS termination of resuscitation” rule was established to consider terminating resuscitative efforts before ambulance transport if all of the following criteria are met: Arrest not witnessed (by anyone); No bystander CPR provided; No ROSC after complete ALS care in the field; No shocks delivered.
 Terminating Resuscitative Efforts in Adults With Out-of-Hospital Cardiac Arrest n n n Implementation of these rules includes contacting online medical control when the criteria are met. Emergency medical service providers should receive training in sensitive communication with the family about the outcome of the resuscitation. Support for the rules should be sought from collaborating agencies such as hospital EDs, the medical coroner’s office, online medical directors, and the police.
Terminating Resuscitative Efforts in Adults With Out-of-Hospital Cardiac Arrest n n n Implementation of these rules includes contacting online medical control when the criteria are met. Emergency medical service providers should receive training in sensitive communication with the family about the outcome of the resuscitation. Support for the rules should be sought from collaborating agencies such as hospital EDs, the medical coroner’s office, online medical directors, and the police.
 Terminating Resuscitative Efforts in Adults With Out-of-Hospital Cardiac Arrest n n Implementation of these rules can reduce the rate of unnecessary hospital transport by 40% to 60%, thereby decreasing associated road hazards, which place providers and the public at risk, inadvertent exposure of EMS personnel to potential biohazards, and the higher cost of ED pronouncement. Note: No such criteria have been established for pediatric (neonate, infant, or child) out-of-hospital cardiac arrest, because no predictors of resuscitation outcome have been validated for out-of-hospital cardiac arrest in this population.
Terminating Resuscitative Efforts in Adults With Out-of-Hospital Cardiac Arrest n n Implementation of these rules can reduce the rate of unnecessary hospital transport by 40% to 60%, thereby decreasing associated road hazards, which place providers and the public at risk, inadvertent exposure of EMS personnel to potential biohazards, and the higher cost of ED pronouncement. Note: No such criteria have been established for pediatric (neonate, infant, or child) out-of-hospital cardiac arrest, because no predictors of resuscitation outcome have been validated for out-of-hospital cardiac arrest in this population.
 Thank you for your attention!
Thank you for your attention!


