b43d0dca66f765e392468f9845b2b963.ppt
- Количество слайдов: 60
 Cardiac Function Tests n Heart disease üSymptoms of heart disease üCongenital heart disease üCongestive heart failure üAcute coronary syndrome üHypertensive heart disease üInfective heart disease Diagnosis of heart disease §Laboratory diagnosis of AMI § üEnzymes, cardiac proteins. Markers of inflammation and coagulation §Markers of congestive heart failure §Other markers §The role of the lab in monitoring heart disease §
Cardiac Function Tests n Heart disease üSymptoms of heart disease üCongenital heart disease üCongestive heart failure üAcute coronary syndrome üHypertensive heart disease üInfective heart disease Diagnosis of heart disease §Laboratory diagnosis of AMI § üEnzymes, cardiac proteins. Markers of inflammation and coagulation §Markers of congestive heart failure §Other markers §The role of the lab in monitoring heart disease §
 Heart disease is the primary cause of illness and death in the United States n 50 000 patients have hypertension; 7600 000 patients suffer a myocardial infarction each year; 4900 000 patients have been diagnosed with congestive heart failure. n. Patients of heart disease usually asymptomatic until late stage of the disease. n. Improved n. Blood detection of heart disease can save lives tests have been used to detect substances that are present in the blood that indicate either disease or a future risk of the development of a disease n. Blood tests detect substances that normally are not present or measure substances that, when elevated above normal levels, indicate disease n selection of appropriate cardiac markers that provide the most effective and clinically useful indicators of myocardial function is critical
Heart disease is the primary cause of illness and death in the United States n 50 000 patients have hypertension; 7600 000 patients suffer a myocardial infarction each year; 4900 000 patients have been diagnosed with congestive heart failure. n. Patients of heart disease usually asymptomatic until late stage of the disease. n. Improved n. Blood detection of heart disease can save lives tests have been used to detect substances that are present in the blood that indicate either disease or a future risk of the development of a disease n. Blood tests detect substances that normally are not present or measure substances that, when elevated above normal levels, indicate disease n selection of appropriate cardiac markers that provide the most effective and clinically useful indicators of myocardial function is critical
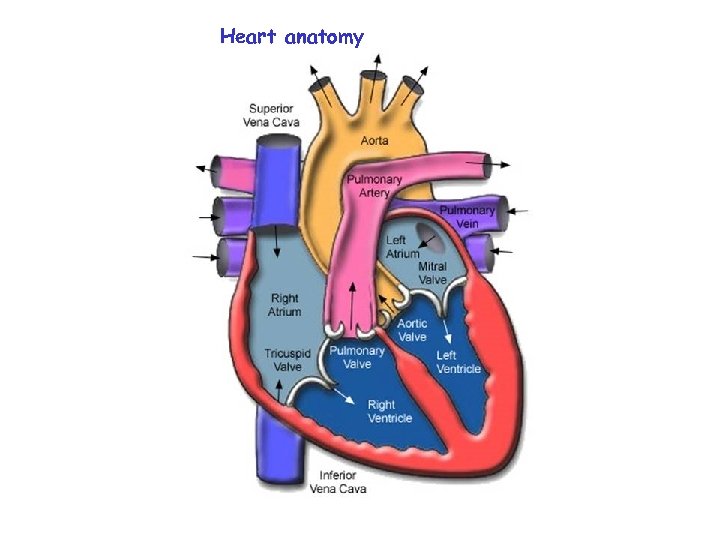 Heart anatomy
Heart anatomy
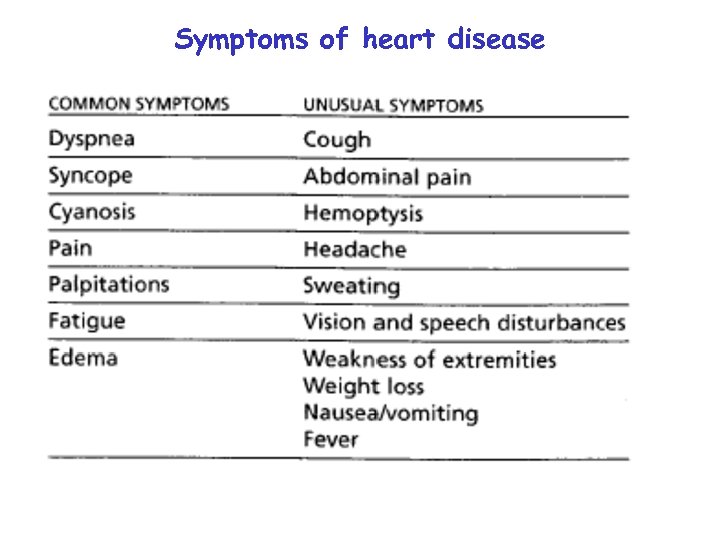 Symptoms of heart disease
Symptoms of heart disease
 Symptoms of heart disease n. Patients with cardiac disease are often asymptomatic until a relatively late stage in their condition. n. The most frequent symptoms manifested in heart disease are dyspnea n. Dyspnea: ü Dyspnea is a difficulty in breathing. ü It can be a result of cardiac or respiratory disease and is a normal response during exercise in healthy individuals. ü Dyspnea as a result of cardiac disease may occur only on exercise or can be present at rest in advanced disease. n. Cyanosis: Ø a bluish discoloration of the skin Ø Result of dyspnea and is caused by an increased amount of nonoxygenated hemoglobin in the blood.
Symptoms of heart disease n. Patients with cardiac disease are often asymptomatic until a relatively late stage in their condition. n. The most frequent symptoms manifested in heart disease are dyspnea n. Dyspnea: ü Dyspnea is a difficulty in breathing. ü It can be a result of cardiac or respiratory disease and is a normal response during exercise in healthy individuals. ü Dyspnea as a result of cardiac disease may occur only on exercise or can be present at rest in advanced disease. n. Cyanosis: Ø a bluish discoloration of the skin Ø Result of dyspnea and is caused by an increased amount of nonoxygenated hemoglobin in the blood.
 Symptoms of heart disease n. Angina pectoris: n is the most common symptom associated with ischemic heart disease. n It is a gripping or crushing, central chest pain that may be felt around or deep within the chest. n The pain may radiate to the neck or jaw, n It is typically worsened by exercise and relieved by rest. n The pain is most often caused by a lack of oxygen to the myocardium as a result of inadequate coronary blood flow n Palpitation: n A palpitation may be an increased awareness of a normal heartbeat or the sensation of a slow, rapid, or irregular heart rate.
Symptoms of heart disease n. Angina pectoris: n is the most common symptom associated with ischemic heart disease. n It is a gripping or crushing, central chest pain that may be felt around or deep within the chest. n The pain may radiate to the neck or jaw, n It is typically worsened by exercise and relieved by rest. n The pain is most often caused by a lack of oxygen to the myocardium as a result of inadequate coronary blood flow n Palpitation: n A palpitation may be an increased awareness of a normal heartbeat or the sensation of a slow, rapid, or irregular heart rate.
 Symptoms of heart disease n. Syncope: Ø Ø Partial or complete loss of consciousness with interruption of awareness of oneself and ones surroundings. It is temporary and there is spontaneous recovery. The most common syncopal attacks are vasovagal in nature (simple faints) and not a result of serious disease. Without warning, the patient falls to the ground with a slow or absent pulse and, after a few seconds, the patient recovers consciousness n. Fatigue: n n is a common, but nonspecific, cardiac symptom. Lethargy (Abnormal drowsiness) is associated with heart failure, persistent cardiac arrhythmia, It may be a result of both poor cerebral and peripheral perfusion and poor oxygenation of blood.
Symptoms of heart disease n. Syncope: Ø Ø Partial or complete loss of consciousness with interruption of awareness of oneself and ones surroundings. It is temporary and there is spontaneous recovery. The most common syncopal attacks are vasovagal in nature (simple faints) and not a result of serious disease. Without warning, the patient falls to the ground with a slow or absent pulse and, after a few seconds, the patient recovers consciousness n. Fatigue: n n is a common, but nonspecific, cardiac symptom. Lethargy (Abnormal drowsiness) is associated with heart failure, persistent cardiac arrhythmia, It may be a result of both poor cerebral and peripheral perfusion and poor oxygenation of blood.
 Symptoms of heart disease n. Edema: n n Retained fluid accumulates in the feet and ankles of patients The edema associated with heart disease is often absent in the morning because the fluid is reabsorbed when lying down, but becomes progressively worse during the day. n. Unusual Ø symptoms A cough may be the primary complaint in some patients with pulmonary congestion. Ø Nocturia (is the need to get up during the night in order to urinate, thus interrupting sleep) is also common in patients with congestive heart failure. Ø Anorexia, abdominal fullness, right upper quadrant tenderness, and weight loss are seen in patients with advanced heart failure but are rare in mild or early heart disease.
Symptoms of heart disease n. Edema: n n Retained fluid accumulates in the feet and ankles of patients The edema associated with heart disease is often absent in the morning because the fluid is reabsorbed when lying down, but becomes progressively worse during the day. n. Unusual Ø symptoms A cough may be the primary complaint in some patients with pulmonary congestion. Ø Nocturia (is the need to get up during the night in order to urinate, thus interrupting sleep) is also common in patients with congestive heart failure. Ø Anorexia, abdominal fullness, right upper quadrant tenderness, and weight loss are seen in patients with advanced heart failure but are rare in mild or early heart disease.
 Congenital Heart disease Congenital heart defects are important cause cardiac disease and occur in about 8% of live births. There is an overall male predominance, although some specific lesions occur more frequently in females, and it is a common cause of death in the first year of life n n Congenital heart disease includes: ü ü ü Valvular defects that interfere with the normal blood flow Septal defects that allow mixing of oxygenated blood from the pulmonary circulation with unoxygenated blood from the systemic circulation, Shunts, abnormalities in position or shape of the aorta or pulmonary arteries, Tetralogy of Fallot or a combination of these conditions. degrees of severity are possible. Many variations and
Congenital Heart disease Congenital heart defects are important cause cardiac disease and occur in about 8% of live births. There is an overall male predominance, although some specific lesions occur more frequently in females, and it is a common cause of death in the first year of life n n Congenital heart disease includes: ü ü ü Valvular defects that interfere with the normal blood flow Septal defects that allow mixing of oxygenated blood from the pulmonary circulation with unoxygenated blood from the systemic circulation, Shunts, abnormalities in position or shape of the aorta or pulmonary arteries, Tetralogy of Fallot or a combination of these conditions. degrees of severity are possible. Many variations and
 The etiology of congenital cardiac disease Ø The etiology of congenital cardiac disease is often unknown Ø However, most defects appear to be multifactorial and reflect a combination of both genetic and environmental influences Ø The rubella virus, the causative agent of German measles, Infection of the mother during the first 3 months of pregnancy is associated with a high incidence of congenital heart disease in the baby. Ø Fetal alcohol syndrome is often associated with heart defects, as alcohol affects the fetal heart by directly interfering with its development. Ø Chromosomal abnormalities are associated with several developmental syndromes, many of which include heart disease, the best-known example is Down syndrome
The etiology of congenital cardiac disease Ø The etiology of congenital cardiac disease is often unknown Ø However, most defects appear to be multifactorial and reflect a combination of both genetic and environmental influences Ø The rubella virus, the causative agent of German measles, Infection of the mother during the first 3 months of pregnancy is associated with a high incidence of congenital heart disease in the baby. Ø Fetal alcohol syndrome is often associated with heart defects, as alcohol affects the fetal heart by directly interfering with its development. Ø Chromosomal abnormalities are associated with several developmental syndromes, many of which include heart disease, the best-known example is Down syndrome
 Congenital Cardiac Disease Ø The symptoms of congenital heart disease may be • Evident at birth or during early infancy, • Or they may not become evident until later in life. Ø Signs and symptoms common to many congenital heart diseases include cyanosis, pulmonary hypertension, clubbing of fingers, embolism or thrombus formation, reduced growth, or syncope
Congenital Cardiac Disease Ø The symptoms of congenital heart disease may be • Evident at birth or during early infancy, • Or they may not become evident until later in life. Ø Signs and symptoms common to many congenital heart diseases include cyanosis, pulmonary hypertension, clubbing of fingers, embolism or thrombus formation, reduced growth, or syncope
 Congenital Cardiac Disease v The most common congenital cardiac lesions are: v Ventricular septal defect (VSD): Ø Commonly known as a hole the heart, is the most common congenital cardiac malformation. ØIn this condition, blood flows through the septal defect from the left ventricle to the right ventricle causing less blood to be pumped from the left ventricle and reducing output to the systemic circulation. ØMore blood enters the pulmonary circulation which overloads and irreversibly damages the pulmonary vessels, causing pulmonary hypertension. ØSome small VSDs will close spontaneously but others should be repaired surgically before the development of sever pulmonary hypertension
Congenital Cardiac Disease v The most common congenital cardiac lesions are: v Ventricular septal defect (VSD): Ø Commonly known as a hole the heart, is the most common congenital cardiac malformation. ØIn this condition, blood flows through the septal defect from the left ventricle to the right ventricle causing less blood to be pumped from the left ventricle and reducing output to the systemic circulation. ØMore blood enters the pulmonary circulation which overloads and irreversibly damages the pulmonary vessels, causing pulmonary hypertension. ØSome small VSDs will close spontaneously but others should be repaired surgically before the development of sever pulmonary hypertension
 Congenital Cardiac Disease The most common congenital cardiac lesions are: v Atrial septal defects (ASD) are often first diagnosed in adulthood. ü This abnormality causes left-to-right shunting of blood between the atria. üPulmonary hypertension and atrial arrhythmia are common when the patient is older than age 30 years, but most children with this condition are asymptomatic. üA significant ASD should be surgically repaired as soon as possible after diagnosis v Coarctation of the aorta: is a narrowing of the aorta v Congenital valve problems may be classified as stenosis (narrowing of a valve that restricts the forward flow of blood) or valvular incompetence (a valve that fails to close completely, allowing blood to leak backward
Congenital Cardiac Disease The most common congenital cardiac lesions are: v Atrial septal defects (ASD) are often first diagnosed in adulthood. ü This abnormality causes left-to-right shunting of blood between the atria. üPulmonary hypertension and atrial arrhythmia are common when the patient is older than age 30 years, but most children with this condition are asymptomatic. üA significant ASD should be surgically repaired as soon as possible after diagnosis v Coarctation of the aorta: is a narrowing of the aorta v Congenital valve problems may be classified as stenosis (narrowing of a valve that restricts the forward flow of blood) or valvular incompetence (a valve that fails to close completely, allowing blood to leak backward
 Tetralogy of Fallot is the most common cyanotic congenital heart abnormality in children. It is a combination of four defects: * Pulmonary valve stenosis is a narrowing of the pulmonary valve and the area below the valve. This slows the flow of blood from the right side of the heart to the lungs. The heart must pump harder to push blood to the lungs where the blood picks up oxygen. *Ventricular septal defect (VSD) is a hole in the wall that separates the lower chambers (ventricles) of the heart. * Overriding aorta is a defect in the position of the large artery (aorta) that takes red (oxygen-rich blood) to the body. In a normal heart the aorta attaches to the left ventricle. In tetralogy of Fallot, the aorta sits between the left and right ventricles, over the VSD. This causes mixing of red and blue (oxygen-poor) blood. * Right ventricular hypertrophy is the thickening of the right lower chamber of the heart (ventricle). Unlike other muscles in your body, when the heart thickens it does not work well. The heart has to pump harder to move blood through the narrowed pulmonary valve and the area below
Tetralogy of Fallot is the most common cyanotic congenital heart abnormality in children. It is a combination of four defects: * Pulmonary valve stenosis is a narrowing of the pulmonary valve and the area below the valve. This slows the flow of blood from the right side of the heart to the lungs. The heart must pump harder to push blood to the lungs where the blood picks up oxygen. *Ventricular septal defect (VSD) is a hole in the wall that separates the lower chambers (ventricles) of the heart. * Overriding aorta is a defect in the position of the large artery (aorta) that takes red (oxygen-rich blood) to the body. In a normal heart the aorta attaches to the left ventricle. In tetralogy of Fallot, the aorta sits between the left and right ventricles, over the VSD. This causes mixing of red and blue (oxygen-poor) blood. * Right ventricular hypertrophy is the thickening of the right lower chamber of the heart (ventricle). Unlike other muscles in your body, when the heart thickens it does not work well. The heart has to pump harder to move blood through the narrowed pulmonary valve and the area below
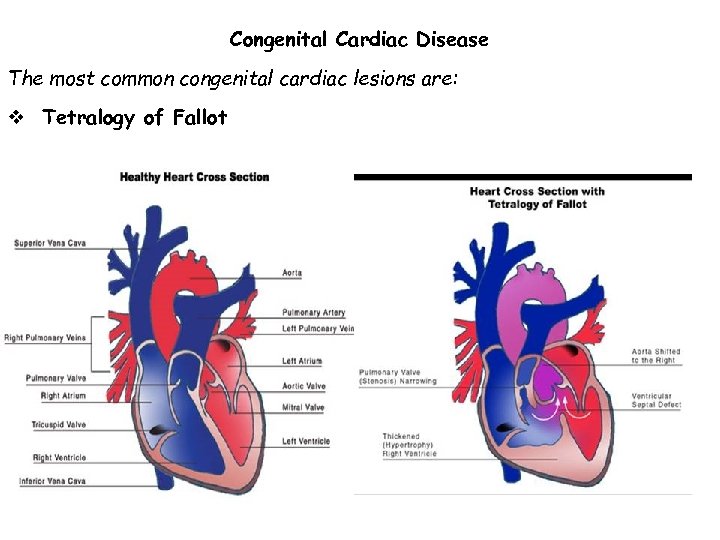 Congenital Cardiac Disease The most common congenital cardiac lesions are: v Tetralogy of Fallot
Congenital Cardiac Disease The most common congenital cardiac lesions are: v Tetralogy of Fallot
 Congestive heart failure results when the heart is unable to pump blood effectively. Ø It is characterized by fluid accumulation, initially in the lungs and subsequently throughout the body. Ø When the heart is unable to pump efficiently, cardiac output decreases. Ø When the left side of the heart fails excess fluid accumulates in the lungs, resulting in pulmonary edema reduced output to the systemic circulation The kidneys respond to this decreased blood flow with excessive fluid retention making the heart failure worse. Ø When the right side of the heart fails excess fluid accumulates in the systemic venous circulatory system and generalized edema results. There is also diminished blood flow to the lungs and to the left side of the heart, resulting in decreased cardiac output to the systemic arterial circulation.
Congestive heart failure results when the heart is unable to pump blood effectively. Ø It is characterized by fluid accumulation, initially in the lungs and subsequently throughout the body. Ø When the heart is unable to pump efficiently, cardiac output decreases. Ø When the left side of the heart fails excess fluid accumulates in the lungs, resulting in pulmonary edema reduced output to the systemic circulation The kidneys respond to this decreased blood flow with excessive fluid retention making the heart failure worse. Ø When the right side of the heart fails excess fluid accumulates in the systemic venous circulatory system and generalized edema results. There is also diminished blood flow to the lungs and to the left side of the heart, resulting in decreased cardiac output to the systemic arterial circulation.
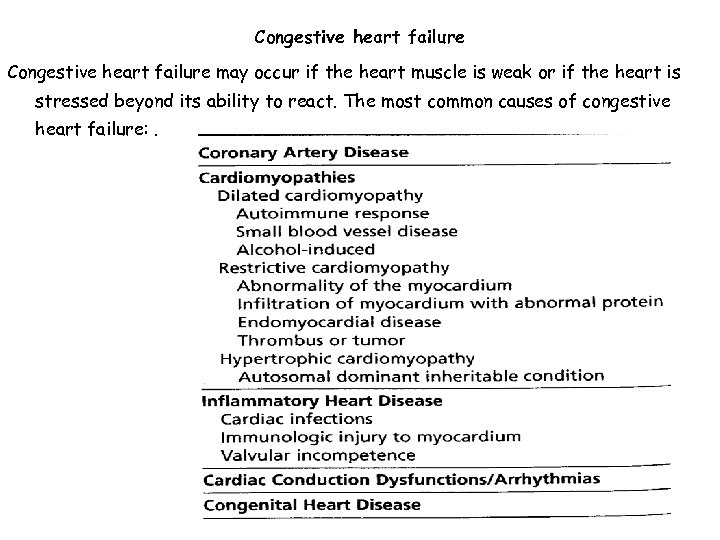 Congestive heart failure may occur if the heart muscle is weak or if the heart is stressed beyond its ability to react. The most common causes of congestive heart failure: .
Congestive heart failure may occur if the heart muscle is weak or if the heart is stressed beyond its ability to react. The most common causes of congestive heart failure: .
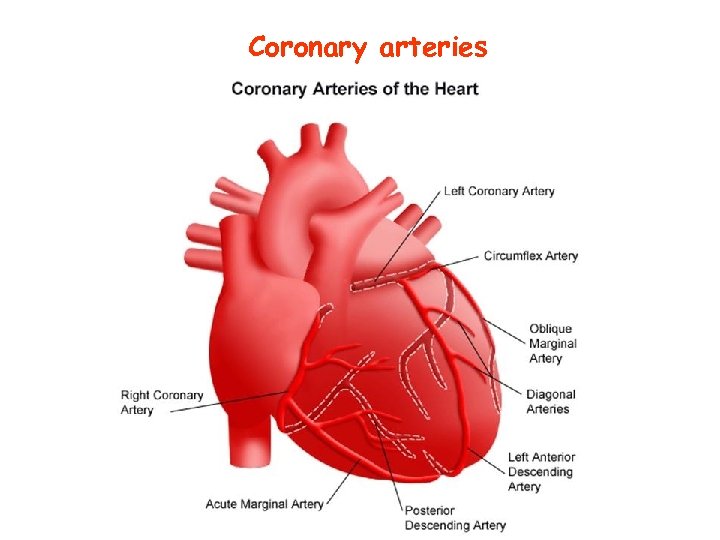 Coronary arteries
Coronary arteries
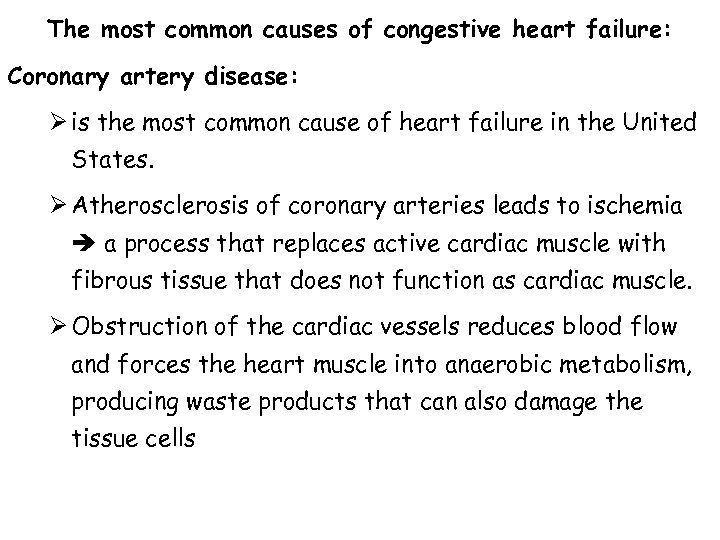 The most common causes of congestive heart failure: Coronary artery disease: Ø is the most common cause of heart failure in the United States. Ø Atherosclerosis of coronary arteries leads to ischemia a process that replaces active cardiac muscle with fibrous tissue that does not function as cardiac muscle. Ø Obstruction of the cardiac vessels reduces blood flow and forces the heart muscle into anaerobic metabolism, producing waste products that can also damage the tissue cells
The most common causes of congestive heart failure: Coronary artery disease: Ø is the most common cause of heart failure in the United States. Ø Atherosclerosis of coronary arteries leads to ischemia a process that replaces active cardiac muscle with fibrous tissue that does not function as cardiac muscle. Ø Obstruction of the cardiac vessels reduces blood flow and forces the heart muscle into anaerobic metabolism, producing waste products that can also damage the tissue cells
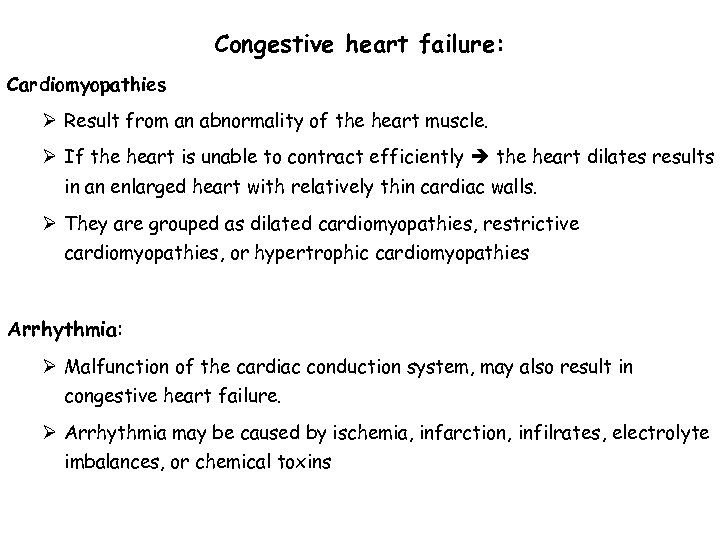 Congestive heart failure: Cardiomyopathies Ø Result from an abnormality of the heart muscle. Ø If the heart is unable to contract efficiently the heart dilates results in an enlarged heart with relatively thin cardiac walls. Ø They are grouped as dilated cardiomyopathies, restrictive cardiomyopathies, or hypertrophic cardiomyopathies Arrhythmia: Ø Malfunction of the cardiac conduction system, may also result in congestive heart failure. Ø Arrhythmia may be caused by ischemia, infarction, infilrates, electrolyte imbalances, or chemical toxins
Congestive heart failure: Cardiomyopathies Ø Result from an abnormality of the heart muscle. Ø If the heart is unable to contract efficiently the heart dilates results in an enlarged heart with relatively thin cardiac walls. Ø They are grouped as dilated cardiomyopathies, restrictive cardiomyopathies, or hypertrophic cardiomyopathies Arrhythmia: Ø Malfunction of the cardiac conduction system, may also result in congestive heart failure. Ø Arrhythmia may be caused by ischemia, infarction, infilrates, electrolyte imbalances, or chemical toxins
 Congestive heart failure: Ø Clinical indications of congestive heart failure range from mild symptoms that appear only on effort to the most advanced conditions in which the heart is unable to function without external support. Ø Congestive heart failure is readily detectable if it involves a patient with myocardial infarction, angina, pulmonary problems, or arrhythmia Ø Congestive heart failure is most commonly investigated because of dyspnea, edema, cough, or angina. Ø Other symptoms, as exercise intolerance, fatigue, and weakness, are common
Congestive heart failure: Ø Clinical indications of congestive heart failure range from mild symptoms that appear only on effort to the most advanced conditions in which the heart is unable to function without external support. Ø Congestive heart failure is readily detectable if it involves a patient with myocardial infarction, angina, pulmonary problems, or arrhythmia Ø Congestive heart failure is most commonly investigated because of dyspnea, edema, cough, or angina. Ø Other symptoms, as exercise intolerance, fatigue, and weakness, are common
 Acute Coronary Syndrome ØCoronary heart disease is caused by a lack of nutrients and oxygen reaching the heart muscle and resulting in myocardial ischemia. ØIschemia is a reduced blood supply to one area of the heart and is often a result of atherosclerosis, thrombosis, spasms, or embolisms but may also be a result of anemia, carboxyhemoglobinemia, or hypotension, which causes reduced blood flow to the heart. Increased demand for oxygen and nutrients as a result of extreme exercise. ØIschemic heart disease involves a progression of pathologic conditions that includes erosion and rupture of coronary artery plaques, activation of platelets, and thrombi. ØThis progression is termed Acute coronary syndrome and ranges from unstable angina to extensive tissue necrosis in acute myocardial infarction.
Acute Coronary Syndrome ØCoronary heart disease is caused by a lack of nutrients and oxygen reaching the heart muscle and resulting in myocardial ischemia. ØIschemia is a reduced blood supply to one area of the heart and is often a result of atherosclerosis, thrombosis, spasms, or embolisms but may also be a result of anemia, carboxyhemoglobinemia, or hypotension, which causes reduced blood flow to the heart. Increased demand for oxygen and nutrients as a result of extreme exercise. ØIschemic heart disease involves a progression of pathologic conditions that includes erosion and rupture of coronary artery plaques, activation of platelets, and thrombi. ØThis progression is termed Acute coronary syndrome and ranges from unstable angina to extensive tissue necrosis in acute myocardial infarction.
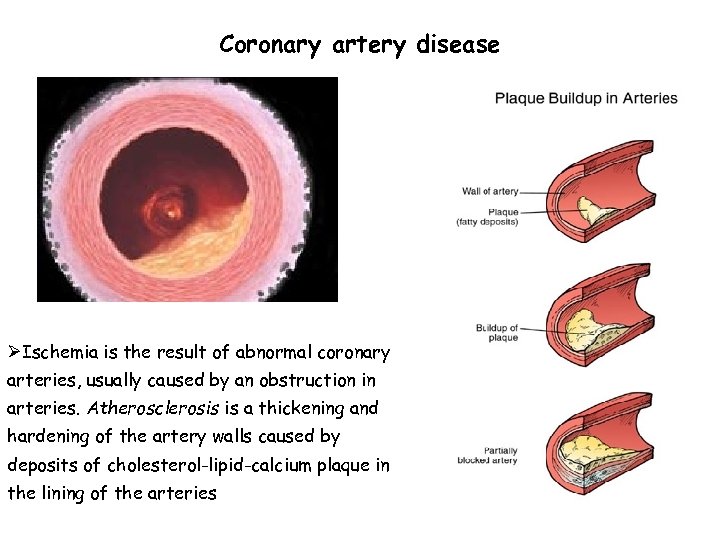 Coronary artery disease ØIschemia is the result of abnormal coronary arteries, usually caused by an obstruction in arteries. Atherosclerosis is a thickening and hardening of the artery walls caused by deposits of cholesterol-lipid-calcium plaque in the lining of the arteries
Coronary artery disease ØIschemia is the result of abnormal coronary arteries, usually caused by an obstruction in arteries. Atherosclerosis is a thickening and hardening of the artery walls caused by deposits of cholesterol-lipid-calcium plaque in the lining of the arteries
 Risk factors for development of arterial plaques: Age: Atherosclerosis may develop in early life but becomes a more significant risk factor with increasing age. Sex: Men tend to be more affected by atherosclerosis than premenopausal women of comparable age. After menopause, the difference tends to disappear. Family history: Atherosclerosis is often found in members of the same family. Some conditions are directly inherited, such as familial hypercholesterolemia and familial combined hyperlipidemia. Hyperlipidemia: An increased serum cholesterol concentration has been shown to have a strong association with atherosclerosis. High level of LDL, low level of HDL increases the risk Smoking: There is a direct relationship between number of cigarettes smoked and the risk of coronary artery disease Hypertension: Both systolic and diastolic hypertensionis associated with increased risk for atherosclerosis Sedentary lifestyle: Regular exercise has shown some protection against the development of heart disease Diabetes mellitus: Because of the strong relationship between diabetes and vascular disease Response to stress. Aggressive, ambitious, compulsive persons have almost twice the risk for coronary disease as persons who do not express these characteristics
Risk factors for development of arterial plaques: Age: Atherosclerosis may develop in early life but becomes a more significant risk factor with increasing age. Sex: Men tend to be more affected by atherosclerosis than premenopausal women of comparable age. After menopause, the difference tends to disappear. Family history: Atherosclerosis is often found in members of the same family. Some conditions are directly inherited, such as familial hypercholesterolemia and familial combined hyperlipidemia. Hyperlipidemia: An increased serum cholesterol concentration has been shown to have a strong association with atherosclerosis. High level of LDL, low level of HDL increases the risk Smoking: There is a direct relationship between number of cigarettes smoked and the risk of coronary artery disease Hypertension: Both systolic and diastolic hypertensionis associated with increased risk for atherosclerosis Sedentary lifestyle: Regular exercise has shown some protection against the development of heart disease Diabetes mellitus: Because of the strong relationship between diabetes and vascular disease Response to stress. Aggressive, ambitious, compulsive persons have almost twice the risk for coronary disease as persons who do not express these characteristics
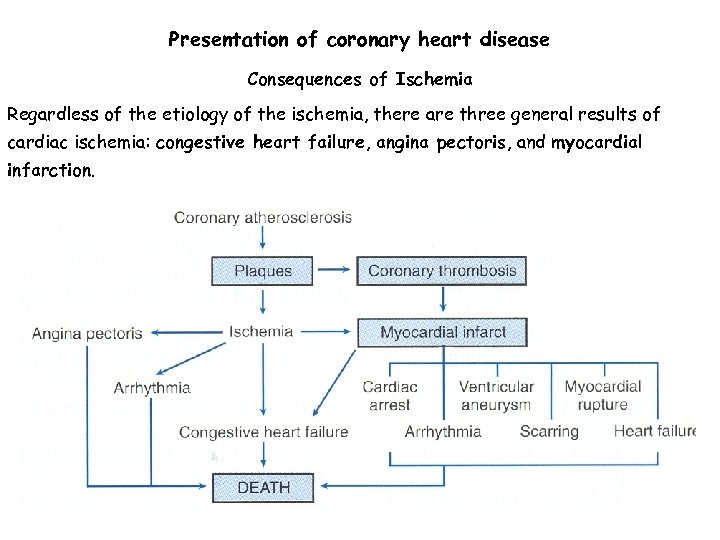 Presentation of coronary heart disease Consequences of Ischemia Regardless of the etiology of the ischemia, there are three general results of cardiac ischemia: congestive heart failure, angina pectoris, and myocardial infarction.
Presentation of coronary heart disease Consequences of Ischemia Regardless of the etiology of the ischemia, there are three general results of cardiac ischemia: congestive heart failure, angina pectoris, and myocardial infarction.
 Consequences of Ischemia Congestive heart failure: Ø Results when there is reduced oxygen supply to the cardiac muscle, causing it to fail to pump the blood efficiently. Angina pectoris: Ø is a symptom of inadequate perfusion of the heart muscle, resulting in chest pain. Ø Typical angina pectoris occurs with increased physical effort or stress and usually rapidly resolves with rest. Ø In patients with coronary artery disease, the narrowed cardiac vessels do not allow for increased blood flow into the cardiac muscle at times of additional physical or emotional stress causing the pain
Consequences of Ischemia Congestive heart failure: Ø Results when there is reduced oxygen supply to the cardiac muscle, causing it to fail to pump the blood efficiently. Angina pectoris: Ø is a symptom of inadequate perfusion of the heart muscle, resulting in chest pain. Ø Typical angina pectoris occurs with increased physical effort or stress and usually rapidly resolves with rest. Ø In patients with coronary artery disease, the narrowed cardiac vessels do not allow for increased blood flow into the cardiac muscle at times of additional physical or emotional stress causing the pain
 Consequences of Ischemia Myocardial infarction, or heart attack, ü Occurs when blood flow to an area of the cardiac muscle is suddenly blocked ü This leads to ischemia and death of myocardial tissue. ü The heart tissue becomes in inflamed and necrotic at the point of obstruction and is followed by the release of cellular enzymes and proteins into the blood. ü The damaged area of the heart quickly loses its ability to contract and conduct electrical impulses and oxygen supplies are depleted. ü This type of damage is irreversible and the area of necrosis is eventually replaced by fibrous scar tissue. ü The severity of damage from a myocardial infarction varies greatly and is primarily related to the size and location of the infarct
Consequences of Ischemia Myocardial infarction, or heart attack, ü Occurs when blood flow to an area of the cardiac muscle is suddenly blocked ü This leads to ischemia and death of myocardial tissue. ü The heart tissue becomes in inflamed and necrotic at the point of obstruction and is followed by the release of cellular enzymes and proteins into the blood. ü The damaged area of the heart quickly loses its ability to contract and conduct electrical impulses and oxygen supplies are depleted. ü This type of damage is irreversible and the area of necrosis is eventually replaced by fibrous scar tissue. ü The severity of damage from a myocardial infarction varies greatly and is primarily related to the size and location of the infarct
 Hypertensive heart disease Ø Hypertension is defined by the World Health Organization as systolic pressure greater than 160 mm Hg and diastolic pressure greater than 95 mm Hg. It is one of the most common cardiovascular diseases, Ø Blood pressure is determined by peripheral resistance if it is increased results in heart disease because it increases the workload of the left ventricle eventually resulting in hypertrophy and dilation. Ø The increase in size of the left ventricle causes the mitral valve to allow circulation of blood into the left atrium that with time, results in dilatation and increased pressure in the left atrium this increased pressure is transferred to the pulmonary circulation and affects the right side of the heart. Ø Another complicating factor in this process is that hypertension is also associated with an increased prevalence of atherosclerosis, further increasing risk for heart disease
Hypertensive heart disease Ø Hypertension is defined by the World Health Organization as systolic pressure greater than 160 mm Hg and diastolic pressure greater than 95 mm Hg. It is one of the most common cardiovascular diseases, Ø Blood pressure is determined by peripheral resistance if it is increased results in heart disease because it increases the workload of the left ventricle eventually resulting in hypertrophy and dilation. Ø The increase in size of the left ventricle causes the mitral valve to allow circulation of blood into the left atrium that with time, results in dilatation and increased pressure in the left atrium this increased pressure is transferred to the pulmonary circulation and affects the right side of the heart. Ø Another complicating factor in this process is that hypertension is also associated with an increased prevalence of atherosclerosis, further increasing risk for heart disease
 Infective heart disease Ø Infectious agents continue to be implicated in a variety of heart diseases Ø The most common infectious diseases involving the heart are rheumatic heart disease, infectious endocarditis, and pericarditis Ø Rheumatic fever is an inflammatory disease of children and young adults that occurs as a result of complications from infection with group A streptococci Ø Rheumatic fever is not caused by a direct infection or toxin but because of the antibodies against the streptococcal antigens cross-react with similar antigens found in the heart and initiate a cell-mediated immune response involving macro phages and lymphocytes.
Infective heart disease Ø Infectious agents continue to be implicated in a variety of heart diseases Ø The most common infectious diseases involving the heart are rheumatic heart disease, infectious endocarditis, and pericarditis Ø Rheumatic fever is an inflammatory disease of children and young adults that occurs as a result of complications from infection with group A streptococci Ø Rheumatic fever is not caused by a direct infection or toxin but because of the antibodies against the streptococcal antigens cross-react with similar antigens found in the heart and initiate a cell-mediated immune response involving macro phages and lymphocytes.
 Diagnosis of heart disease Because of its dangerous consequences great efforts have been made to determine the best tools for the early and accurate diagnosis of acute myocardial infarction (AMI). WHO determined criteria for the diagnosis of AMI üHistory acute, severe and prolonged chest pain üECG üSerum cardiac markers an initial rise and subsequent fall of certain enzymes/proteins serum concentration ØSingle diagnostic laboratory test that quickly and accurately assess cardiac function does not exist A combination of cardiac markers is required. ØResearch is going on to find a cardiac marker that would be useful in evaluating many types of heart conditions.
Diagnosis of heart disease Because of its dangerous consequences great efforts have been made to determine the best tools for the early and accurate diagnosis of acute myocardial infarction (AMI). WHO determined criteria for the diagnosis of AMI üHistory acute, severe and prolonged chest pain üECG üSerum cardiac markers an initial rise and subsequent fall of certain enzymes/proteins serum concentration ØSingle diagnostic laboratory test that quickly and accurately assess cardiac function does not exist A combination of cardiac markers is required. ØResearch is going on to find a cardiac marker that would be useful in evaluating many types of heart conditions.
 Features required for an ideal marker Ø The marker should be absolutely heart specific to allow reliable diagnosis of myocardial damage in the presence of skeletal muscle injury. Ø The marker should be highly sensitive to detect even minor heart damage. Ø The marker should be able to differentiate reversible from irreversible damage. Ø In acute myocardial infarction, the marker should allow monitoring of reperfusion therapy and estimation of infarct size and prognosis. Ø The marker should be stable and the measurement rapid, easy to perform, quantitative, and cost effective. Ø The marker should not be detectable in patients who do not have myocardial damage
Features required for an ideal marker Ø The marker should be absolutely heart specific to allow reliable diagnosis of myocardial damage in the presence of skeletal muscle injury. Ø The marker should be highly sensitive to detect even minor heart damage. Ø The marker should be able to differentiate reversible from irreversible damage. Ø In acute myocardial infarction, the marker should allow monitoring of reperfusion therapy and estimation of infarct size and prognosis. Ø The marker should be stable and the measurement rapid, easy to perform, quantitative, and cost effective. Ø The marker should not be detectable in patients who do not have myocardial damage
 Lab diagnosis of AMI • Enzymes ü AST, LD are no longer used ü Creatinine kinase, CK-MB • Cardiac proteins ü Myoglobin ü Troponin T and troponin I ü Cardiac myosin light chains
Lab diagnosis of AMI • Enzymes ü AST, LD are no longer used ü Creatinine kinase, CK-MB • Cardiac proteins ü Myoglobin ü Troponin T and troponin I ü Cardiac myosin light chains
 Lab diagnosis of AMI Enzymes AST LD Ø These enzymes were used as indicator for MI but they are no longer used in diagnosis because of lack of specificity to cardiac cells Ø Although LD isoenzyme determinations increase specificity for cardiac tissue, with the LDI and LD 2 subfractions being most indicative of cardiac involvement, the National Academy of Clinical Biochemistry recommends that LD and LD isoenzymes no longer have a role in diagnosis of cardiac diseases
Lab diagnosis of AMI Enzymes AST LD Ø These enzymes were used as indicator for MI but they are no longer used in diagnosis because of lack of specificity to cardiac cells Ø Although LD isoenzyme determinations increase specificity for cardiac tissue, with the LDI and LD 2 subfractions being most indicative of cardiac involvement, the National Academy of Clinical Biochemistry recommends that LD and LD isoenzymes no longer have a role in diagnosis of cardiac diseases
 Creatine kinase (CK) Ø Creatine kinase (CK) is a cytosolic enzyme involved in the transfer of energy in muscle metabolism. Ø It is a dimer comprised of two subunits (the B, or brain form, and the M, or muscle form), resulting in three CK isoenzymes. ü The CK-BB (CKl) isoenzyme is of brain origin and only found in the blood if the blood-brain barrier has been breached. ü CK-MM (CK 3) isoenzyme accounts for most of the CK activity in skeletal muscle, ü whereas CK-MB (CK 2) has the most specificity for cardiac muscle, even though it accounts for only 3 -20% of total CK activity in the heart, it can be used as a marker of early AMl
Creatine kinase (CK) Ø Creatine kinase (CK) is a cytosolic enzyme involved in the transfer of energy in muscle metabolism. Ø It is a dimer comprised of two subunits (the B, or brain form, and the M, or muscle form), resulting in three CK isoenzymes. ü The CK-BB (CKl) isoenzyme is of brain origin and only found in the blood if the blood-brain barrier has been breached. ü CK-MM (CK 3) isoenzyme accounts for most of the CK activity in skeletal muscle, ü whereas CK-MB (CK 2) has the most specificity for cardiac muscle, even though it accounts for only 3 -20% of total CK activity in the heart, it can be used as a marker of early AMl
 CK-MB (CK-2) Ø CK-MB is a valuable tool for the diagnosis of AMl because of its relatively high specificity for cardiac injury. Ø Extensive experience with CK-MB has established it as the gold standard for other cardiac markers. Ø It takes at least 4 -6 hours from onset of chest pain before CKMB activities increase to significant levels in the blood. Ø Peak levels occur at 12 -24 hours, and serum activities usually return to baseline levels with 2 -3 days Ø Although the specificity of CK-MB for heart tissue is greater than 85%, it is also found in skeletal muscle and false-positive results may be caused at clinical conditions such as muscle disease and acute or chronic muscle injuries
CK-MB (CK-2) Ø CK-MB is a valuable tool for the diagnosis of AMl because of its relatively high specificity for cardiac injury. Ø Extensive experience with CK-MB has established it as the gold standard for other cardiac markers. Ø It takes at least 4 -6 hours from onset of chest pain before CKMB activities increase to significant levels in the blood. Ø Peak levels occur at 12 -24 hours, and serum activities usually return to baseline levels with 2 -3 days Ø Although the specificity of CK-MB for heart tissue is greater than 85%, it is also found in skeletal muscle and false-positive results may be caused at clinical conditions such as muscle disease and acute or chronic muscle injuries
 CK-MB (CK-2) Ø CK-MB activity assays have been increasingly replaced by CK-MB mass assays that measure the protein concentration of CK-MB rather than its catalytic activity. Ø These laboratory procedures are based on immunoassay techniques using monoclonal antibodies and have fewer interferences and higher analytic sensitivity than activity-based assays. Ø Mass assays can detect an increased concentration of serum CK-MB about 1 hour earlier than activity-based methods Ø To increase specificity of CK-MB for cardiac tissue, it has been proposed that a ratio (relative index) of CK-MB mass/CK activity be calculated If this ratio exceeds 3, it is indicative of AMI rather than skeletal muscle damage Ø CK isoforms may be effectively used as indicators of reperfusion after thrombolytic therapy in patients with confirmed AMI
CK-MB (CK-2) Ø CK-MB activity assays have been increasingly replaced by CK-MB mass assays that measure the protein concentration of CK-MB rather than its catalytic activity. Ø These laboratory procedures are based on immunoassay techniques using monoclonal antibodies and have fewer interferences and higher analytic sensitivity than activity-based assays. Ø Mass assays can detect an increased concentration of serum CK-MB about 1 hour earlier than activity-based methods Ø To increase specificity of CK-MB for cardiac tissue, it has been proposed that a ratio (relative index) of CK-MB mass/CK activity be calculated If this ratio exceeds 3, it is indicative of AMI rather than skeletal muscle damage Ø CK isoforms may be effectively used as indicators of reperfusion after thrombolytic therapy in patients with confirmed AMI
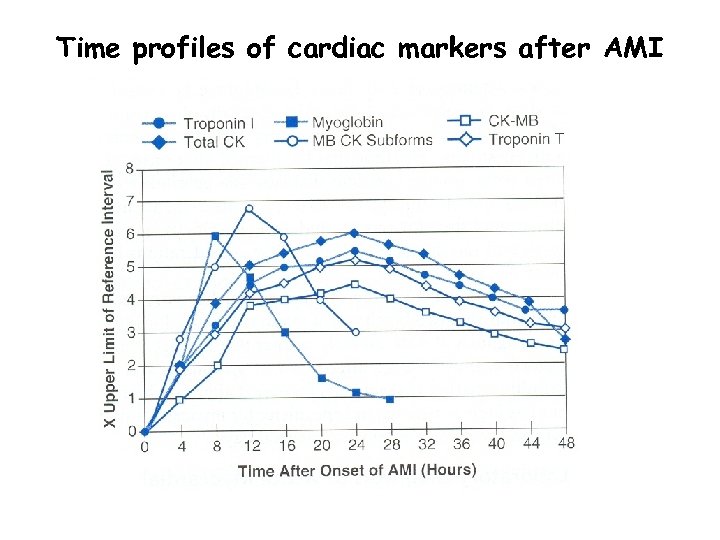 Time profiles of cardiac markers after AMI
Time profiles of cardiac markers after AMI
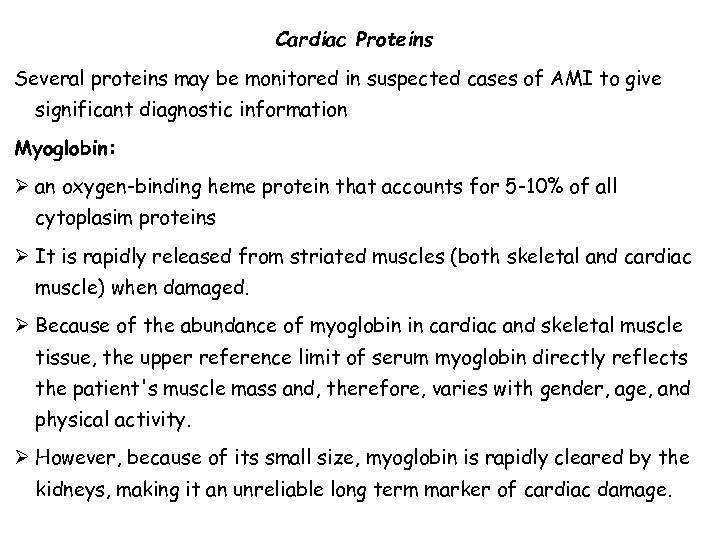 Cardiac Proteins Several proteins may be monitored in suspected cases of AMI to give significant diagnostic information Myoglobin: Ø an oxygen-binding heme protein that accounts for 5 -10% of all cytoplasim proteins Ø It is rapidly released from striated muscles (both skeletal and cardiac muscle) when damaged. Ø Because of the abundance of myoglobin in cardiac and skeletal muscle tissue, the upper reference limit of serum myoglobin directly reflects the patient's muscle mass and, therefore, varies with gender, age, and physical activity. Ø However, because of its small size, myoglobin is rapidly cleared by the kidneys, making it an unreliable long term marker of cardiac damage.
Cardiac Proteins Several proteins may be monitored in suspected cases of AMI to give significant diagnostic information Myoglobin: Ø an oxygen-binding heme protein that accounts for 5 -10% of all cytoplasim proteins Ø It is rapidly released from striated muscles (both skeletal and cardiac muscle) when damaged. Ø Because of the abundance of myoglobin in cardiac and skeletal muscle tissue, the upper reference limit of serum myoglobin directly reflects the patient's muscle mass and, therefore, varies with gender, age, and physical activity. Ø However, because of its small size, myoglobin is rapidly cleared by the kidneys, making it an unreliable long term marker of cardiac damage.
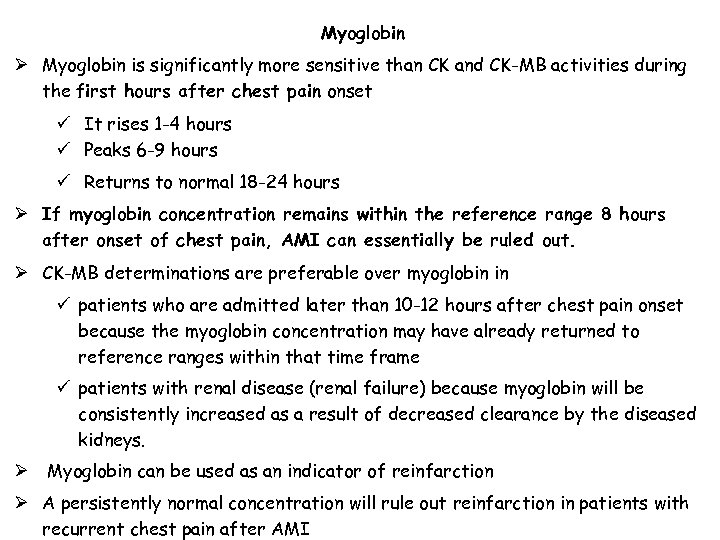 Myoglobin Ø Myoglobin is significantly more sensitive than CK and CK-MB activities during the first hours after chest pain onset ü It rises 1 -4 hours ü Peaks 6 -9 hours ü Returns to normal 18 -24 hours Ø If myoglobin concentration remains within the reference range 8 hours after onset of chest pain, AMI can essentially be ruled out. Ø CK-MB determinations are preferable over myoglobin in ü patients who are admitted later than 10 -12 hours after chest pain onset because the myoglobin concentration may have already returned to reference ranges within that time frame ü patients with renal disease (renal failure) because myoglobin will be consistently increased as a result of decreased clearance by the diseased kidneys. Ø Myoglobin can be used as an indicator of reinfarction Ø A persistently normal concentration will rule out reinfarction in patients with recurrent chest pain after AMI
Myoglobin Ø Myoglobin is significantly more sensitive than CK and CK-MB activities during the first hours after chest pain onset ü It rises 1 -4 hours ü Peaks 6 -9 hours ü Returns to normal 18 -24 hours Ø If myoglobin concentration remains within the reference range 8 hours after onset of chest pain, AMI can essentially be ruled out. Ø CK-MB determinations are preferable over myoglobin in ü patients who are admitted later than 10 -12 hours after chest pain onset because the myoglobin concentration may have already returned to reference ranges within that time frame ü patients with renal disease (renal failure) because myoglobin will be consistently increased as a result of decreased clearance by the diseased kidneys. Ø Myoglobin can be used as an indicator of reinfarction Ø A persistently normal concentration will rule out reinfarction in patients with recurrent chest pain after AMI
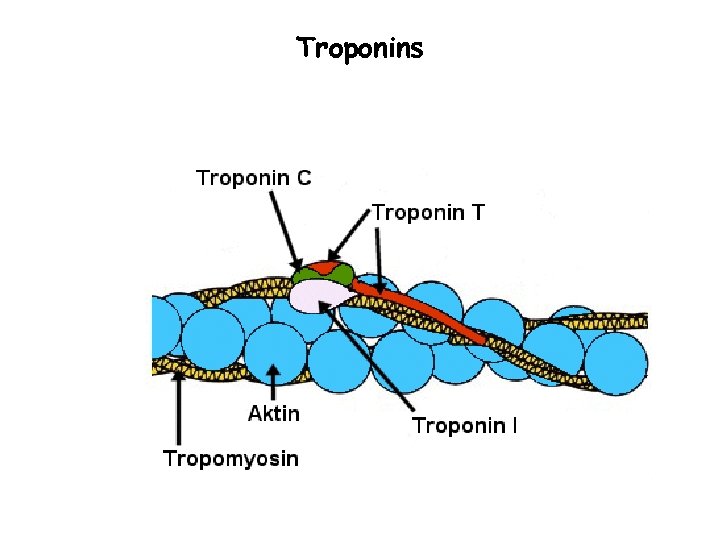
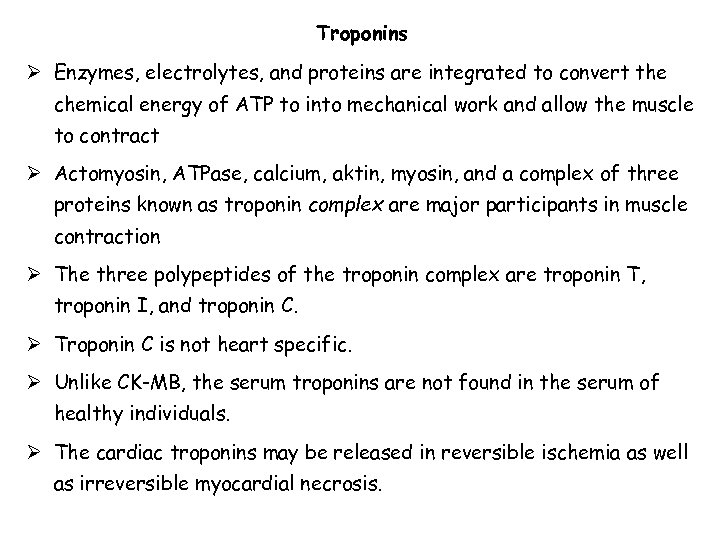 Troponins Ø Enzymes, electrolytes, and proteins are integrated to convert the chemical energy of ATP to into mechanical work and allow the muscle to contract Ø Actomyosin, ATPase, calcium, aktin, myosin, and a complex of three proteins known as troponin complex are major participants in muscle contraction Ø The three polypeptides of the troponin complex are troponin T, troponin I, and troponin C. Ø Troponin C is not heart specific. Ø Unlike CK-MB, the serum troponins are not found in the serum of healthy individuals. Ø The cardiac troponins may be released in reversible ischemia as well as irreversible myocardial necrosis.
Troponins Ø Enzymes, electrolytes, and proteins are integrated to convert the chemical energy of ATP to into mechanical work and allow the muscle to contract Ø Actomyosin, ATPase, calcium, aktin, myosin, and a complex of three proteins known as troponin complex are major participants in muscle contraction Ø The three polypeptides of the troponin complex are troponin T, troponin I, and troponin C. Ø Troponin C is not heart specific. Ø Unlike CK-MB, the serum troponins are not found in the serum of healthy individuals. Ø The cardiac troponins may be released in reversible ischemia as well as irreversible myocardial necrosis.
 Troponins
Troponins
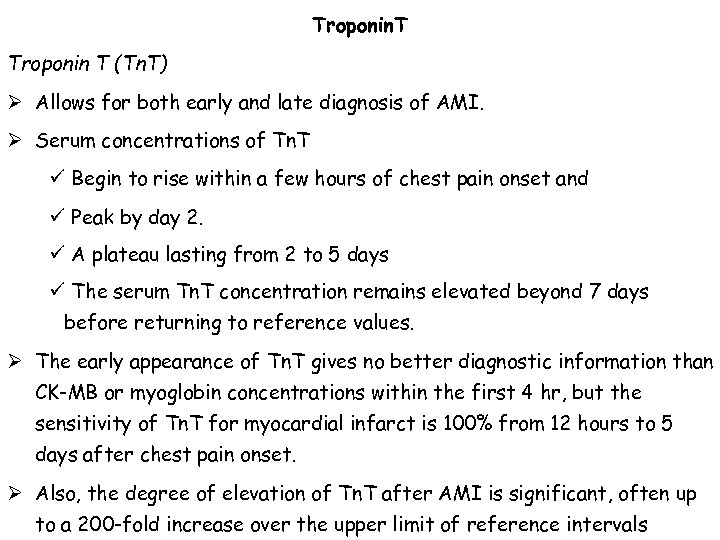 Troponin. T Troponin T (Tn. T) Ø Allows for both early and late diagnosis of AMI. Ø Serum concentrations of Tn. T ü Begin to rise within a few hours of chest pain onset and ü Peak by day 2. ü A plateau lasting from 2 to 5 days ü The serum Tn. T concentration remains elevated beyond 7 days before returning to reference values. Ø The early appearance of Tn. T gives no better diagnostic information than CK-MB or myoglobin concentrations within the first 4 hr, but the sensitivity of Tn. T for myocardial infarct is 100% from 12 hours to 5 days after chest pain onset. Ø Also, the degree of elevation of Tn. T after AMI is significant, often up to a 200 -fold increase over the upper limit of reference intervals
Troponin. T Troponin T (Tn. T) Ø Allows for both early and late diagnosis of AMI. Ø Serum concentrations of Tn. T ü Begin to rise within a few hours of chest pain onset and ü Peak by day 2. ü A plateau lasting from 2 to 5 days ü The serum Tn. T concentration remains elevated beyond 7 days before returning to reference values. Ø The early appearance of Tn. T gives no better diagnostic information than CK-MB or myoglobin concentrations within the first 4 hr, but the sensitivity of Tn. T for myocardial infarct is 100% from 12 hours to 5 days after chest pain onset. Ø Also, the degree of elevation of Tn. T after AMI is significant, often up to a 200 -fold increase over the upper limit of reference intervals
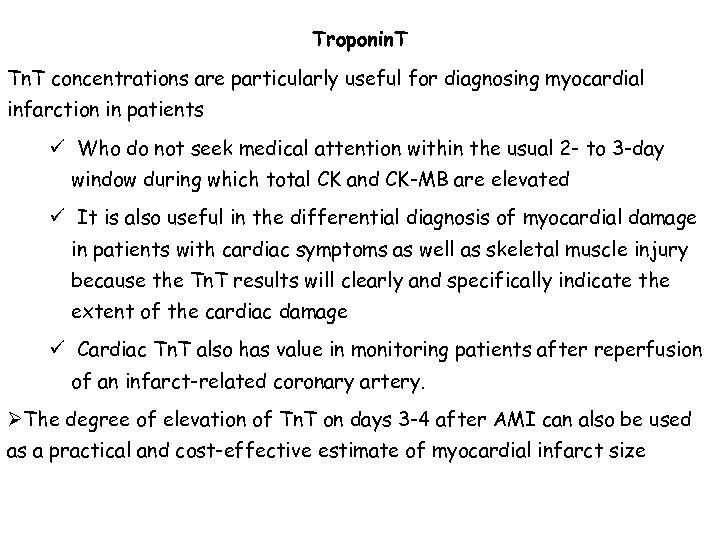 Troponin. T Tn. T concentrations are particularly useful for diagnosing myocardial infarction in patients ü Who do not seek medical attention within the usual 2 - to 3 -day window during which total CK and CK-MB are elevated ü It is also useful in the differential diagnosis of myocardial damage in patients with cardiac symptoms as well as skeletal muscle injury because the Tn. T results will clearly and specifically indicate the extent of the cardiac damage ü Cardiac Tn. T also has value in monitoring patients after reperfusion of an infarct-related coronary artery. ØThe degree of elevation of Tn. T on days 3 -4 after AMI can also be used as a practical and cost-effective estimate of myocardial infarct size
Troponin. T Tn. T concentrations are particularly useful for diagnosing myocardial infarction in patients ü Who do not seek medical attention within the usual 2 - to 3 -day window during which total CK and CK-MB are elevated ü It is also useful in the differential diagnosis of myocardial damage in patients with cardiac symptoms as well as skeletal muscle injury because the Tn. T results will clearly and specifically indicate the extent of the cardiac damage ü Cardiac Tn. T also has value in monitoring patients after reperfusion of an infarct-related coronary artery. ØThe degree of elevation of Tn. T on days 3 -4 after AMI can also be used as a practical and cost-effective estimate of myocardial infarct size
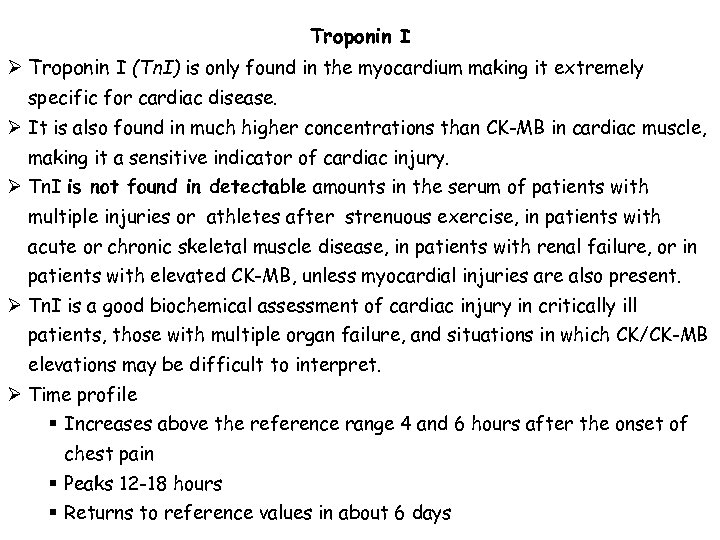 Troponin I Ø Troponin I (Tn. I) is only found in the myocardium making it extremely specific for cardiac disease. Ø It is also found in much higher concentrations than CK-MB in cardiac muscle, making it a sensitive indicator of cardiac injury. Ø Tn. I is not found in detectable amounts in the serum of patients with multiple injuries or athletes after strenuous exercise, in patients with acute or chronic skeletal muscle disease, in patients with renal failure, or in patients with elevated CK-MB, unless myocardial injuries are also present. Ø Tn. I is a good biochemical assessment of cardiac injury in critically ill patients, those with multiple organ failure, and situations in which CK/CK-MB elevations may be difficult to interpret. Ø Time profile § Increases above the reference range 4 and 6 hours after the onset of chest pain § Peaks 12 -18 hours § Returns to reference values in about 6 days
Troponin I Ø Troponin I (Tn. I) is only found in the myocardium making it extremely specific for cardiac disease. Ø It is also found in much higher concentrations than CK-MB in cardiac muscle, making it a sensitive indicator of cardiac injury. Ø Tn. I is not found in detectable amounts in the serum of patients with multiple injuries or athletes after strenuous exercise, in patients with acute or chronic skeletal muscle disease, in patients with renal failure, or in patients with elevated CK-MB, unless myocardial injuries are also present. Ø Tn. I is a good biochemical assessment of cardiac injury in critically ill patients, those with multiple organ failure, and situations in which CK/CK-MB elevations may be difficult to interpret. Ø Time profile § Increases above the reference range 4 and 6 hours after the onset of chest pain § Peaks 12 -18 hours § Returns to reference values in about 6 days
 Markers of inflammation and coagulation disorders Ø Studies have evaluated several acute phase proteins as potential markers for cardiovascular risk assessment, Ø There is evidence that C-reactive protein (CRP) is a reliable predictor of acute coronary syndrome risk Ø CRP is an acute phase reactant produced primarily by the liver. Ø It is stimulated by interleukin-6 and increases rapidly with inflammation. Ø CRP is a sensitive marker for ongoing chronic inflammation that is not affected by ischemic injury. Ø It rises significantly in response to injury, infection, or other inflammatory conditions Ø is not present in appreciable amounts in healthy individuals.
Markers of inflammation and coagulation disorders Ø Studies have evaluated several acute phase proteins as potential markers for cardiovascular risk assessment, Ø There is evidence that C-reactive protein (CRP) is a reliable predictor of acute coronary syndrome risk Ø CRP is an acute phase reactant produced primarily by the liver. Ø It is stimulated by interleukin-6 and increases rapidly with inflammation. Ø CRP is a sensitive marker for ongoing chronic inflammation that is not affected by ischemic injury. Ø It rises significantly in response to injury, infection, or other inflammatory conditions Ø is not present in appreciable amounts in healthy individuals.
 hs-CRP Ø Reliable, automated high sensitivity assays for CRP (hs-CRP) are exist that allow detection of the small increases of CRP often seen in cardiac disease Ø Epidemiologic data document a positive association between hs-CRP and the prevalence of coronary artery disease. Ø Elevated baseline levels of hs-CRP are correlated with higher risk of future cardiovascular morbidity and mortality among those with and without clinical evidence of vascular disease. Ø hs-CRP also demonstrates prognostic capacity in those who do not yet have a diagnosis of vascular disease Ø The level of CRP has been shown to correlate with future risk as follows: üCRP level less than 1 mg/L: lowest risk üCRP levels of 1 to 3 mg/L: intermediate risk üCRP greater than 3 mg/L: highest risk
hs-CRP Ø Reliable, automated high sensitivity assays for CRP (hs-CRP) are exist that allow detection of the small increases of CRP often seen in cardiac disease Ø Epidemiologic data document a positive association between hs-CRP and the prevalence of coronary artery disease. Ø Elevated baseline levels of hs-CRP are correlated with higher risk of future cardiovascular morbidity and mortality among those with and without clinical evidence of vascular disease. Ø hs-CRP also demonstrates prognostic capacity in those who do not yet have a diagnosis of vascular disease Ø The level of CRP has been shown to correlate with future risk as follows: üCRP level less than 1 mg/L: lowest risk üCRP levels of 1 to 3 mg/L: intermediate risk üCRP greater than 3 mg/L: highest risk
 Fibrinogen Ø Fibrinogen is a soluble glycoprotein produced in the liver and involved in platelet aggregation and coagulation. Ø It is also an acute-phase protein produced in response to inflammation. Ø A relationship has been established between elevated levels of fibrinogen and risk of cardiovascular disease and may serve as a marker of long-term prognosis.
Fibrinogen Ø Fibrinogen is a soluble glycoprotein produced in the liver and involved in platelet aggregation and coagulation. Ø It is also an acute-phase protein produced in response to inflammation. Ø A relationship has been established between elevated levels of fibrinogen and risk of cardiovascular disease and may serve as a marker of long-term prognosis.
 D-Dimer Ø D-Dimer is the end product of the ongoing process of thrombus formation and dissolution that occurs at the site of active plaques in acute coronary syndromes. Ø Because this process precedes myocardial cell damage and release of protein contents, it can be used for early detection. Ø It remains elevated for days so it may be an easily detectable physiologic marker of an unstable plaque even when the troponins or CK-MB are not increased, potentially identifying high-risk patients Ø D-Dimer lacks specificity for cardiac damage as it is increased in other conditions that cause thrombosis. Ø Elevations of D-Dimer have been shown to be useful in predicting risk for future cardiac events.
D-Dimer Ø D-Dimer is the end product of the ongoing process of thrombus formation and dissolution that occurs at the site of active plaques in acute coronary syndromes. Ø Because this process precedes myocardial cell damage and release of protein contents, it can be used for early detection. Ø It remains elevated for days so it may be an easily detectable physiologic marker of an unstable plaque even when the troponins or CK-MB are not increased, potentially identifying high-risk patients Ø D-Dimer lacks specificity for cardiac damage as it is increased in other conditions that cause thrombosis. Ø Elevations of D-Dimer have been shown to be useful in predicting risk for future cardiac events.
 Markers of congestive heart failure Ø Brain-type, or B natriuretic peptide (BNP), is a peptide hormone secreted primarily by the cardiac ventricles. Ø It acts on the renal glomerulus to stimulate urinary excretion of sodium and to increase urine flow without affecting the glomerular filtration rate, blood pressure, or renal blood flow Ø Plasma concentrations of BNP are increased in diseases characterized by an expanded fluid volume (renal failure, hepatic cirrhosis with ascites, primary aldosteronism, and congestive heart failure) Ø Diagnosis of congestive heart failure (CHF) is difficult because of its nonspecific symptoms, as well as the lack of a specific biochemical marker üPatients with a BNP < 20 pmol/L are unlikely to have CHF üPatients with BNP > 20 pmol/L have a high probability of CHF Ø BNP may also be clinically relevant in determining the prognosis of patients, especially those with a diagnosis of CHF or those who have experienced a recent AMI
Markers of congestive heart failure Ø Brain-type, or B natriuretic peptide (BNP), is a peptide hormone secreted primarily by the cardiac ventricles. Ø It acts on the renal glomerulus to stimulate urinary excretion of sodium and to increase urine flow without affecting the glomerular filtration rate, blood pressure, or renal blood flow Ø Plasma concentrations of BNP are increased in diseases characterized by an expanded fluid volume (renal failure, hepatic cirrhosis with ascites, primary aldosteronism, and congestive heart failure) Ø Diagnosis of congestive heart failure (CHF) is difficult because of its nonspecific symptoms, as well as the lack of a specific biochemical marker üPatients with a BNP < 20 pmol/L are unlikely to have CHF üPatients with BNP > 20 pmol/L have a high probability of CHF Ø BNP may also be clinically relevant in determining the prognosis of patients, especially those with a diagnosis of CHF or those who have experienced a recent AMI
 Other markers for AMI Ø Glycogen phosphorylase isoenzyme BB (GPBB) üMore sensitive than the other markers during the first 3 -4 hours after onset of chest pain üIt is not specific for cardiac tissue Ø Heart fatty acid-binding protein (H-FABP) ØH-FABP content in skeletal muscle is only 10 -30% of that found in cardiac muscle, it is more sensitive than myoglobin ØIt increases rapidly within 2 -4 hours, peaks within 5 -10 hours and returns to normal within 24 -36 hours ØThe magnitude of the increase in plasma levels has a good correlation with the size of the infarction Ø Carbonic Anhydrase (CA) Isoenzyme III CAIIl is not found in cardiac muscle and, therefore, can be used to differentiate between skeletal muscle and cardiac muscle damage when performed in conjunction with a more heart-specific analyte such as myoglobin.
Other markers for AMI Ø Glycogen phosphorylase isoenzyme BB (GPBB) üMore sensitive than the other markers during the first 3 -4 hours after onset of chest pain üIt is not specific for cardiac tissue Ø Heart fatty acid-binding protein (H-FABP) ØH-FABP content in skeletal muscle is only 10 -30% of that found in cardiac muscle, it is more sensitive than myoglobin ØIt increases rapidly within 2 -4 hours, peaks within 5 -10 hours and returns to normal within 24 -36 hours ØThe magnitude of the increase in plasma levels has a good correlation with the size of the infarction Ø Carbonic Anhydrase (CA) Isoenzyme III CAIIl is not found in cardiac muscle and, therefore, can be used to differentiate between skeletal muscle and cardiac muscle damage when performed in conjunction with a more heart-specific analyte such as myoglobin.
 Other markers Ischemia-modified albumin (IMA) Ø IMA is produced when albumin comes into contact with ischemic tissue, altering it and making it more resistant to binding metals Ø IMA is produced continually during ischemia and rises within 2 -3 hours of an is chemic event Homocysteine Ø Homocysteine is a naturally occurring amino acid found in blood, which is associated with vitamin B 1, B 6, and folic acid deficiency. Ø An elevated homocysteine level is a potential risk factor for coronary heart disease, cerebral vascular disease, carotid artery disease, and peripheral vascular disease by promoting plaque formation.
Other markers Ischemia-modified albumin (IMA) Ø IMA is produced when albumin comes into contact with ischemic tissue, altering it and making it more resistant to binding metals Ø IMA is produced continually during ischemia and rises within 2 -3 hours of an is chemic event Homocysteine Ø Homocysteine is a naturally occurring amino acid found in blood, which is associated with vitamin B 1, B 6, and folic acid deficiency. Ø An elevated homocysteine level is a potential risk factor for coronary heart disease, cerebral vascular disease, carotid artery disease, and peripheral vascular disease by promoting plaque formation.
 Cardiac myosin light chains (MLC) Ø Cardiac myosin light chains (MLC) are also involved with muscle contractions. Ø Recent research has determined that MLC is no more specific for cardiac injury than CK-MB determinations Ø Like the troponins, MLC is released from reversibly ischemic tissue. Ø Although rapid testing of MLC is available, MLC determination does not offer any advantage over cardiac troponin assays. Ø MLC remains of limited clinical significance as a routine cardiac marker
Cardiac myosin light chains (MLC) Ø Cardiac myosin light chains (MLC) are also involved with muscle contractions. Ø Recent research has determined that MLC is no more specific for cardiac injury than CK-MB determinations Ø Like the troponins, MLC is released from reversibly ischemic tissue. Ø Although rapid testing of MLC is available, MLC determination does not offer any advantage over cardiac troponin assays. Ø MLC remains of limited clinical significance as a routine cardiac marker
 lipoprotein phospholipase A 2 (Lp-PLA 2) Ø Lp-PLA 2 generates oxidized molecules within the blood vessel wall that increase the potential of atherosclerosis and irritability of the atherosclerotic plaque Ø Elevations in the levels of Lp-PLA 2 have been shown to indicate greater risk of plaque formation and rupture independent of the levels of either lipids or CRP Ø Patients with elevated levels of Lp-PLA 2 seem to be at a greater risk of cardiac events
lipoprotein phospholipase A 2 (Lp-PLA 2) Ø Lp-PLA 2 generates oxidized molecules within the blood vessel wall that increase the potential of atherosclerosis and irritability of the atherosclerotic plaque Ø Elevations in the levels of Lp-PLA 2 have been shown to indicate greater risk of plaque formation and rupture independent of the levels of either lipids or CRP Ø Patients with elevated levels of Lp-PLA 2 seem to be at a greater risk of cardiac events
 Patient Focused Cardiac Tests ØBecause the situation of patient of serious, special care should be considered ØThe initial patient evaluation be performed within 20 minutes of arrival to the emergency department (ED) ØThe optimum turnaround time from patient arrival to the availability of test results for cardiac markers should be about 30 -60 minute
Patient Focused Cardiac Tests ØBecause the situation of patient of serious, special care should be considered ØThe initial patient evaluation be performed within 20 minutes of arrival to the emergency department (ED) ØThe optimum turnaround time from patient arrival to the availability of test results for cardiac markers should be about 30 -60 minute
 The role of lab in monitoring heart disease The laboratory's role in monitoring heart function primarily involves: Ø Measuring the effects of the heart on other organs, such as the lungs, liver and kidney ü Arterial blood gases measure the patient's acid-base and oxygen status determine the respiratory acidosis and elevated carbon dioxide levels that are often seen in patients with heart disease. ü electrolyte and osmolality : The patient with cardiac disease may develop edema and fluid retention and ionic redistribution. ü Serum electrolyte determinations, including sodium, potassium, chloride, and calcium, are important to monitor diuretic and drug therapy in patients with heart disease ü Elevations of AST, ALT and ALP are often seen in patients with chronic right ventricular failure and GGT value elevated in congestive heart failure, suggesting liver congestion and damage.
The role of lab in monitoring heart disease The laboratory's role in monitoring heart function primarily involves: Ø Measuring the effects of the heart on other organs, such as the lungs, liver and kidney ü Arterial blood gases measure the patient's acid-base and oxygen status determine the respiratory acidosis and elevated carbon dioxide levels that are often seen in patients with heart disease. ü electrolyte and osmolality : The patient with cardiac disease may develop edema and fluid retention and ionic redistribution. ü Serum electrolyte determinations, including sodium, potassium, chloride, and calcium, are important to monitor diuretic and drug therapy in patients with heart disease ü Elevations of AST, ALT and ALP are often seen in patients with chronic right ventricular failure and GGT value elevated in congestive heart failure, suggesting liver congestion and damage.
 The role of lab in monitoring heart disease Ø Lipid evaluation will assess risk for coronary artery disease. ü Maintenance of near normal HDL-cholesterol, LDL cholesterol and , triglyceride levels is highly recommended for cardiac patients. ü Determination of a lipoprotein similar to LDL may also be indicated as it is an independent risk factor associated with development of premature coronary artery and vascular disease. Ø The patient who has secondary heart failure due to thyroid dysfunction can be identified by a highly sensitive thyroid-stimulating hormone assay. Ø The laboratory is also invaluable for monitoring therapeutic drugs following the diagnosis of heart disease. Ø The routine blood count ü Important for detecting anemia and infection Ø Blood cultures ü To identify infections associated with pericarditis, endocarditis and valvular problems
The role of lab in monitoring heart disease Ø Lipid evaluation will assess risk for coronary artery disease. ü Maintenance of near normal HDL-cholesterol, LDL cholesterol and , triglyceride levels is highly recommended for cardiac patients. ü Determination of a lipoprotein similar to LDL may also be indicated as it is an independent risk factor associated with development of premature coronary artery and vascular disease. Ø The patient who has secondary heart failure due to thyroid dysfunction can be identified by a highly sensitive thyroid-stimulating hormone assay. Ø The laboratory is also invaluable for monitoring therapeutic drugs following the diagnosis of heart disease. Ø The routine blood count ü Important for detecting anemia and infection Ø Blood cultures ü To identify infections associated with pericarditis, endocarditis and valvular problems
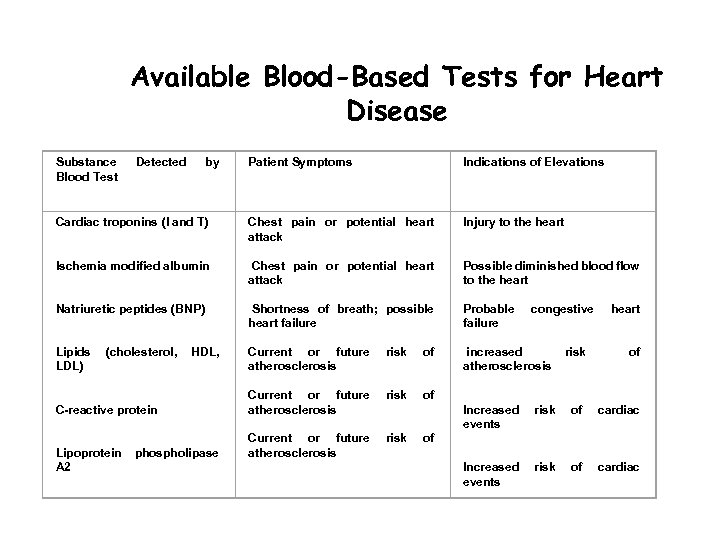 Available Blood-Based Tests for Heart Disease Substance Blood Test Detected by Cardiac troponins (I and T) Ischemia modified albumin Natriuretic peptides (BNP) Lipids (cholesterol, HDL, LDL) C-reactive protein Lipoprotein phospholipase A 2 Patient Symptoms Indications of Elevations Chest pain or potential heart attack Shortness of breath; possible heart failure Current or future risk of atherosclerosis Injury to the heart Possible diminished blood flow to the heart Probable congestive heart failure increased risk of atherosclerosis Increased risk of cardiac events
Available Blood-Based Tests for Heart Disease Substance Blood Test Detected by Cardiac troponins (I and T) Ischemia modified albumin Natriuretic peptides (BNP) Lipids (cholesterol, HDL, LDL) C-reactive protein Lipoprotein phospholipase A 2 Patient Symptoms Indications of Elevations Chest pain or potential heart attack Shortness of breath; possible heart failure Current or future risk of atherosclerosis Injury to the heart Possible diminished blood flow to the heart Probable congestive heart failure increased risk of atherosclerosis Increased risk of cardiac events
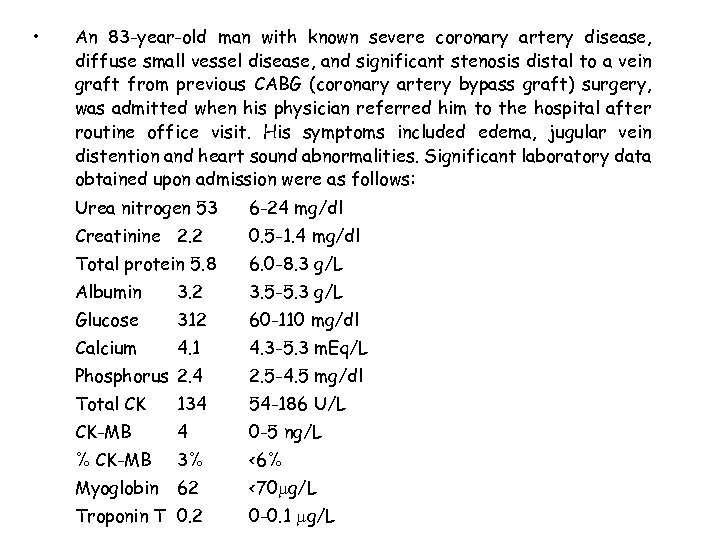 • An 83 -year-old man with known severe coronary artery disease, diffuse small vessel disease, and significant stenosis distal to a vein graft from previous CABG (coronary artery bypass graft) surgery, was admitted when his physician referred him to the hospital after routine office visit. His symptoms included edema, jugular vein distention and heart sound abnormalities. Significant laboratory data obtained upon admission were as follows: Urea nitrogen 53 6 -24 mg/dl Creatinine 2. 2 0. 5 -1. 4 mg/dl Total protein 5. 8 6. 0 -8. 3 g/L Albumin 3. 2 3. 5 -5. 3 g/L Glucose 312 60 -110 mg/dl Calcium 4. 1 4. 3 -5. 3 m. Eq/L Phosphorus 2. 4 2. 5 -4. 5 mg/dl Total CK 134 54 -186 U/L CK-MB 4 0 -5 ng/L % CK-MB 3% <6% Myoglobin 62 <70 g/L Troponin T 0. 2 0 -0. 1 g/L
• An 83 -year-old man with known severe coronary artery disease, diffuse small vessel disease, and significant stenosis distal to a vein graft from previous CABG (coronary artery bypass graft) surgery, was admitted when his physician referred him to the hospital after routine office visit. His symptoms included edema, jugular vein distention and heart sound abnormalities. Significant laboratory data obtained upon admission were as follows: Urea nitrogen 53 6 -24 mg/dl Creatinine 2. 2 0. 5 -1. 4 mg/dl Total protein 5. 8 6. 0 -8. 3 g/L Albumin 3. 2 3. 5 -5. 3 g/L Glucose 312 60 -110 mg/dl Calcium 4. 1 4. 3 -5. 3 m. Eq/L Phosphorus 2. 4 2. 5 -4. 5 mg/dl Total CK 134 54 -186 U/L CK-MB 4 0 -5 ng/L % CK-MB 3% <6% Myoglobin 62 <70 g/L Troponin T 0. 2 0 -0. 1 g/L
 § Questions: 1. Do the symptoms of this patient suggest AMI? 2. Based on lab data, would this diagnosis be AMI? why or why not? 3. Based on the lab data, are there other organ system abnormalities present? 4. What are the indicators of these organ system abnormalities? 5. Is there a specific lab data that might indicate congestive heart failure in this patient?
§ Questions: 1. Do the symptoms of this patient suggest AMI? 2. Based on lab data, would this diagnosis be AMI? why or why not? 3. Based on the lab data, are there other organ system abnormalities present? 4. What are the indicators of these organ system abnormalities? 5. Is there a specific lab data that might indicate congestive heart failure in this patient?
 The End
The End


