Acute MI - 9.2017.pptx
- Количество слайдов: 184

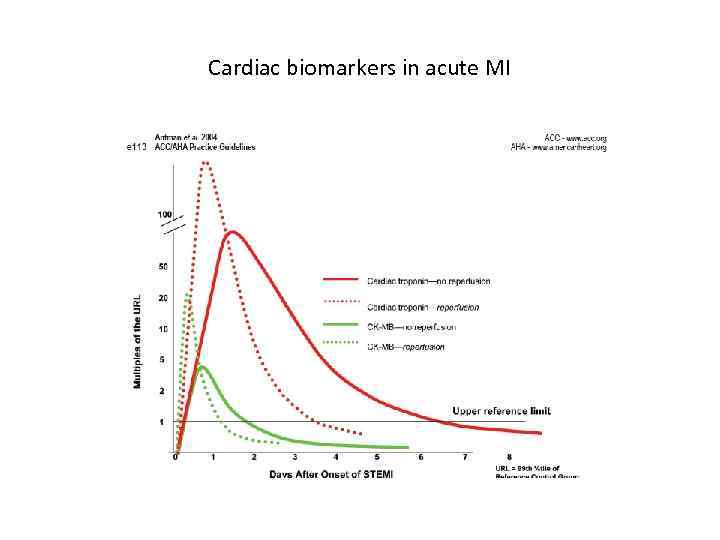
Cardiac biomarkers in acute MI











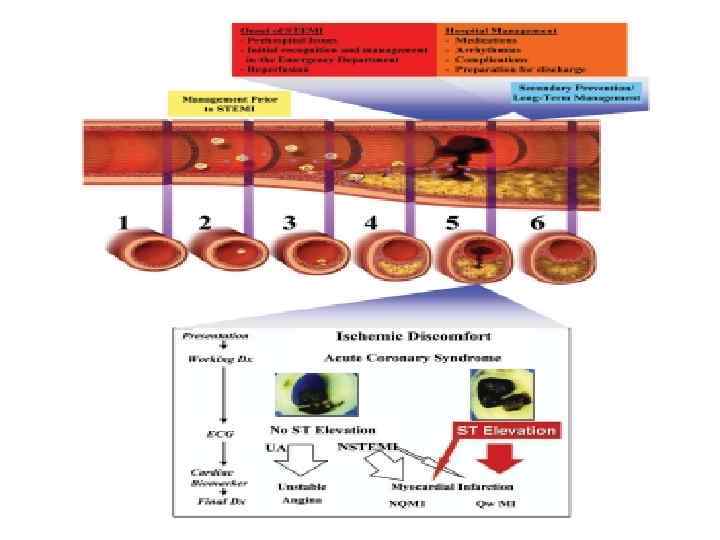
Terms • STEMI - ST segment elevation myocardial infarction previous terms: transmural MI , Q-wave MI • NSTEMI - non-ST elevation myocardial infarction previous terms: subendocardial MI, non-Q-wave MI • Unstable angina and NSTEMI are NSTE acute coronary syndromes (ACS)
Diagnostic methods • • • Complaints & Hx Physical examination ECG Laboratory tests Echo. CG
Clinical presentation: typical anginal pain
Typical chest pain in acute MI • Nature of pain : constricting , crushing, oppressing, compressing, sensation of heavy weight or squeezing of the chest • Location : usually retrosternal, spreading to both sides of anterior chest with predilection for the left side • Irradiation: ulnar aspect of the left arm • Duration : >30 min - hours
Atypical clinical presentations • Heart failure • Classic angina pectoris w/o a particularly severe or prolonged episode • Atypical location of the pain • CNS manifestations resembling those of stroke • Apprehension and nervousness • Sudden mania or psychosis • Syncope • Peripheral embolization
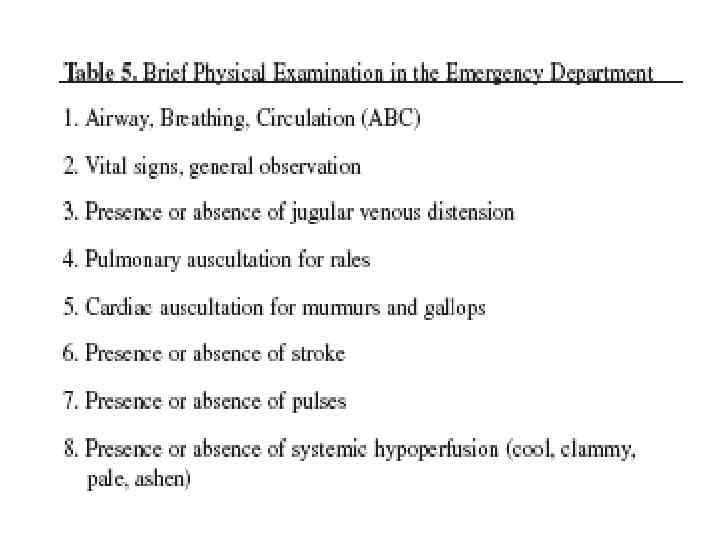
Physical examination • General appearance, consciousness (signs of cerebral hypoperfusion), cognitive status • Body temperature (cool, clammy signs of hypoperfusion due to CS , fever septic shock) • Jugular veins (signs of right heart failure) • Auscultation - lungs (signs of pulmonary edema [left heart failure]) - heart (gallop [left heart failure], murmurs of MR or VSD [MI complications]) • Pulses (entry site for coronary intervention, PVD as a risk factor for adverse outcome)
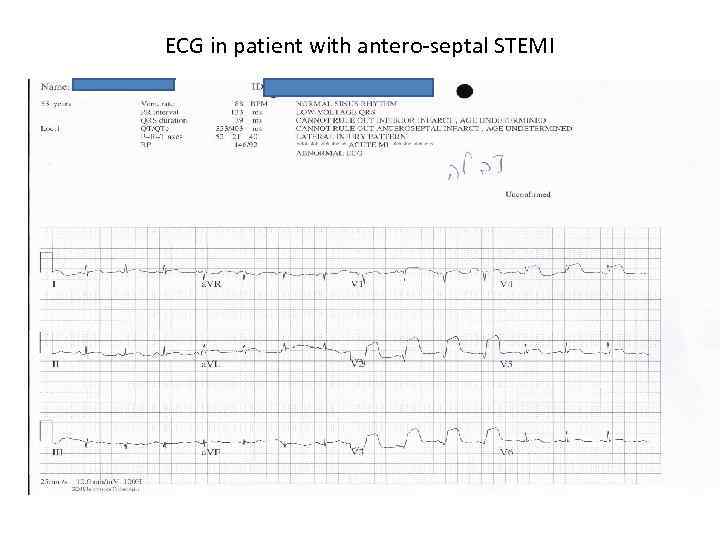
ECG in patient with antero-septal STEMI
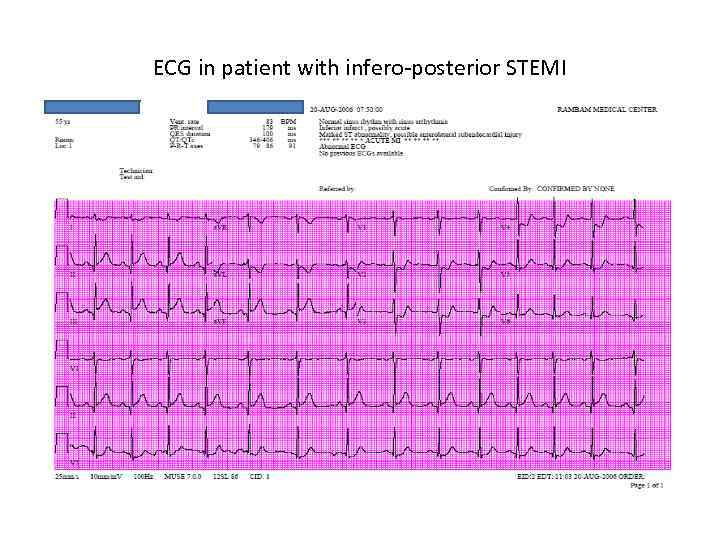
ECG in patient with infero-posterior STEMI
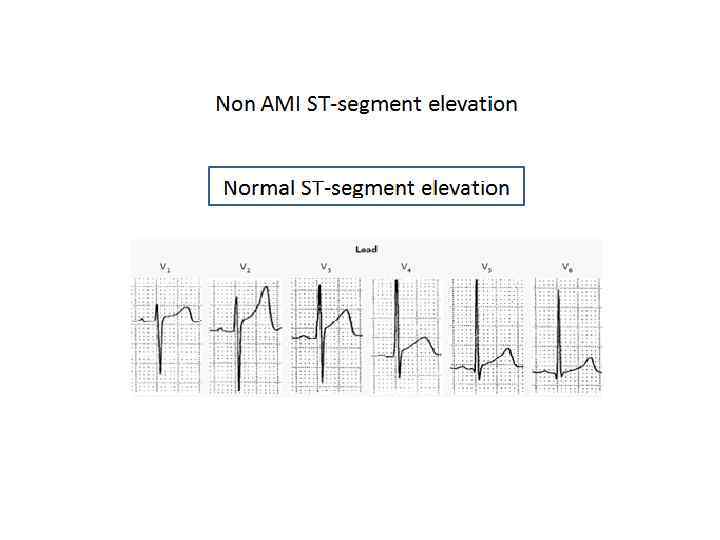
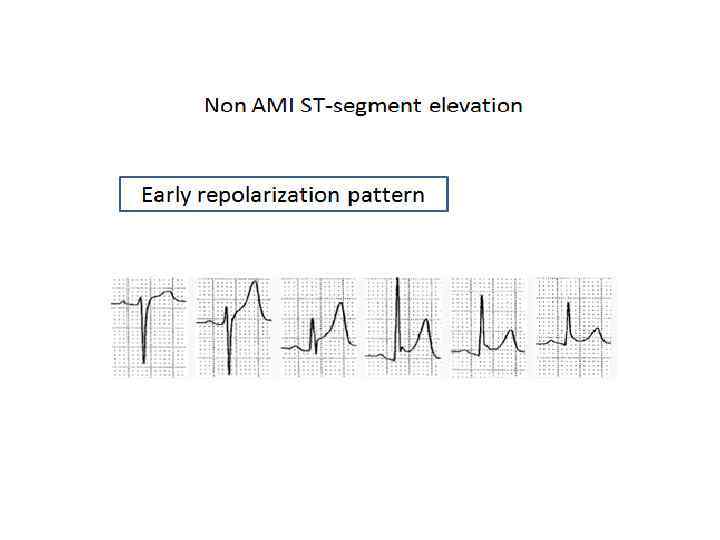
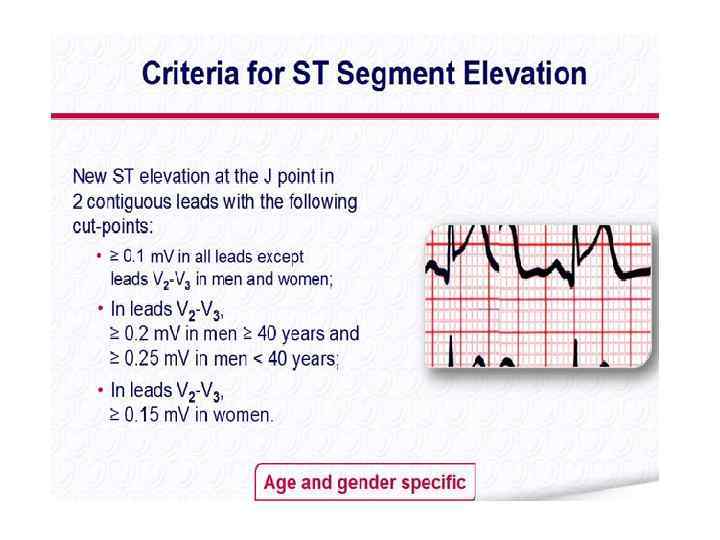
ST-segment elevation in conditions other than acute myocardial infarction • • • Early repolarization Acute pericarditis and perimyocarditis Old MI LBBB Pulmonary embolism Prinzmetal’s angina Hyperkalemia Brugada syndrome and arrhythmogenic RV cardiomyopathy Transthoracic cardioversion Dilated CM Hypertrophic CM / LVH





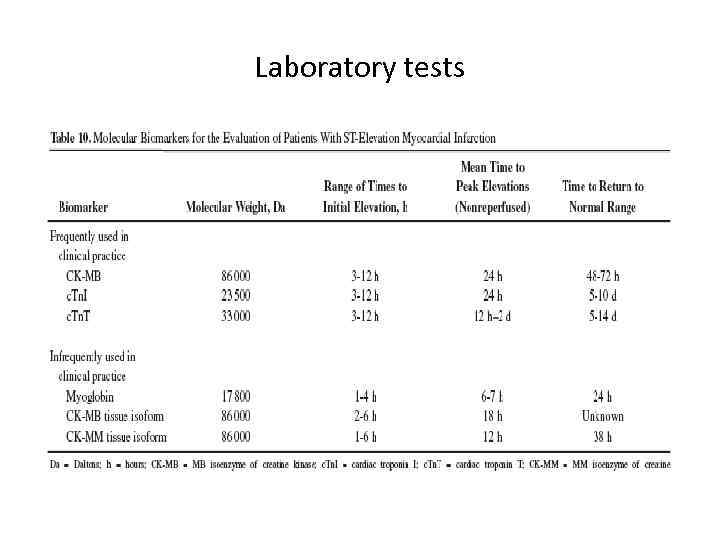
Laboratory tests
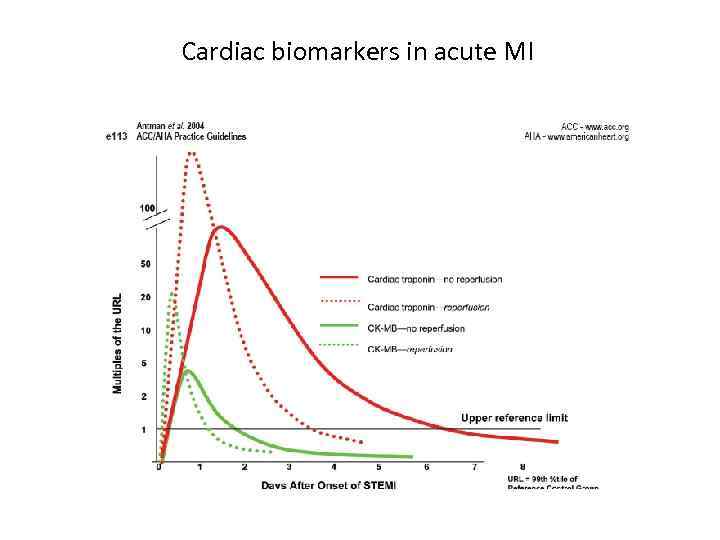
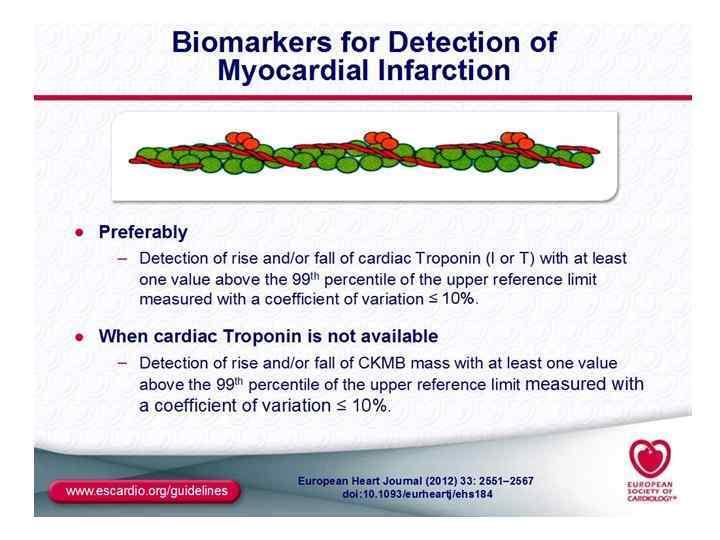
Cardiac biomarkers in acute MI
Elevations of troponin in the absence of overt ischemic heart disease • • • • • Cardiac contusion, or other trauma including surgery, ablation, pacing etc Congestive heart failure – acute on chronic Aortic dissection Aortic valve disease Hypertrophic cardiomyopathy Tachy- or bradyarrythmias, or heart block Apical ballooning syndrome Rhabdomyolysis with cardiac injury Pulmonary embolism, severe pulmonary hypertension Renal failure Acute neurologic disease, including stroke or subarchnoid hemorrhage Infiltrative diseases, e. g. amyloidosis, haemochromatosis, sarcoidosis, and scleroderma Inflammatory diseases, e. g. myocarditis or myocardial extension of endo/pericarditis Drug toxicity or toxins Critically ill patients , especially with respiratory failure or sepsis Burns, especially if affecting > 30% of body surface area Extreme exertion
Differential diagnosis of acute MI
Differential diagnosis of acute MI
Differential diagnosis of acute MI
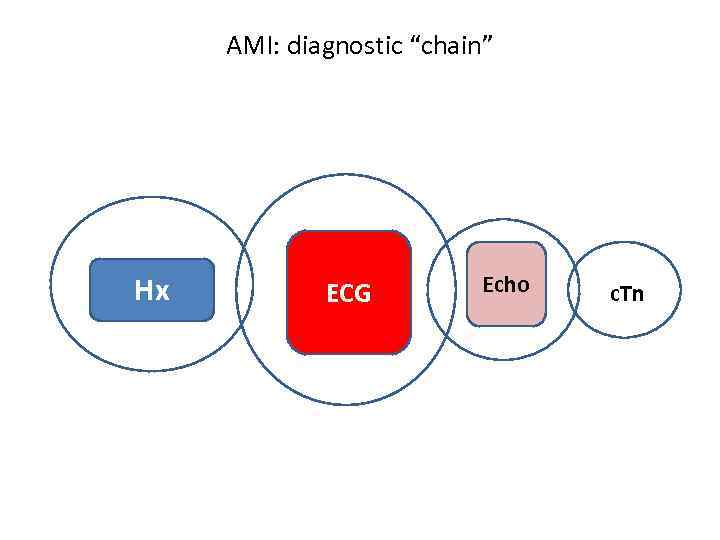
AMI: diagnostic “chain” Hx ECG Echo c. Tn
ST-segment elevation myocardial infarction (STEMI)
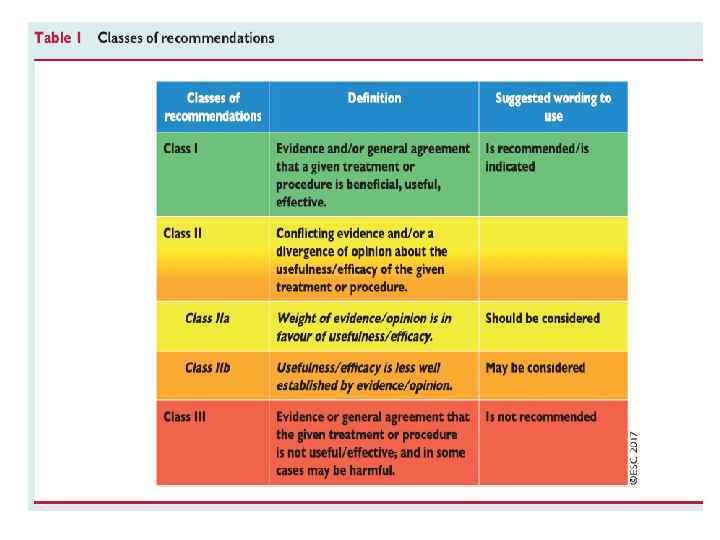

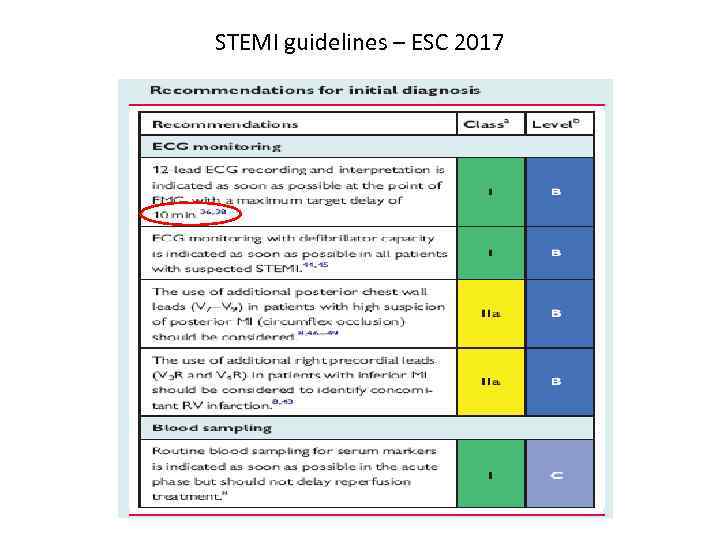
STEMI guidelines – ESC 2017
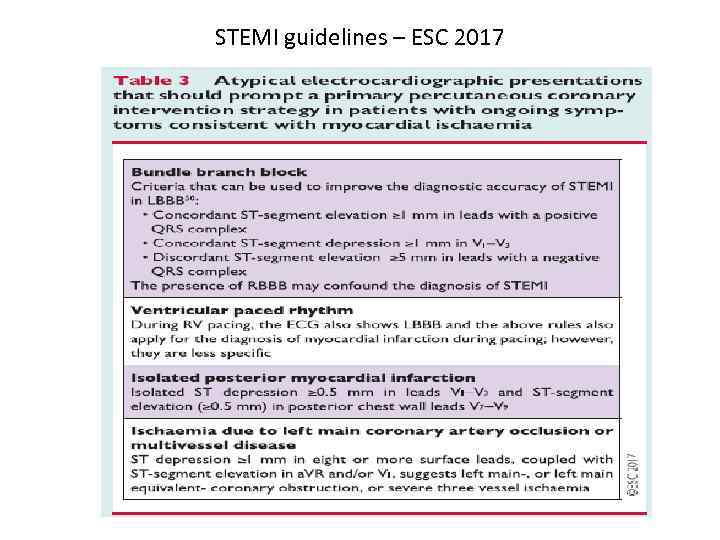
STEMI guidelines – ESC 2017
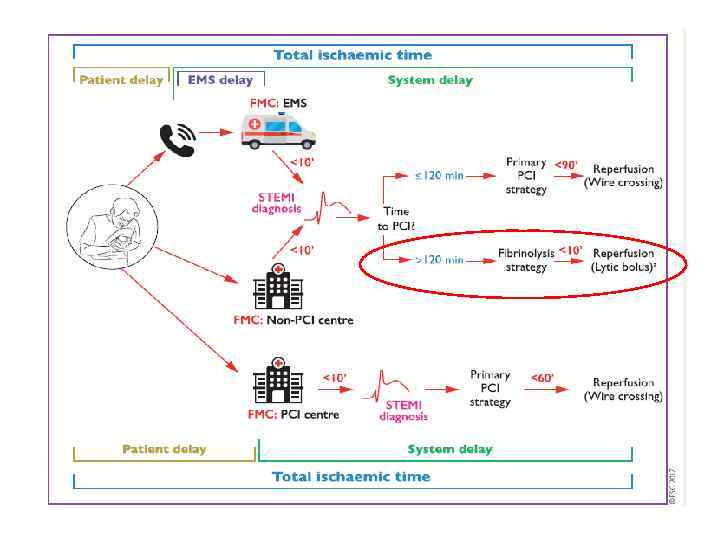
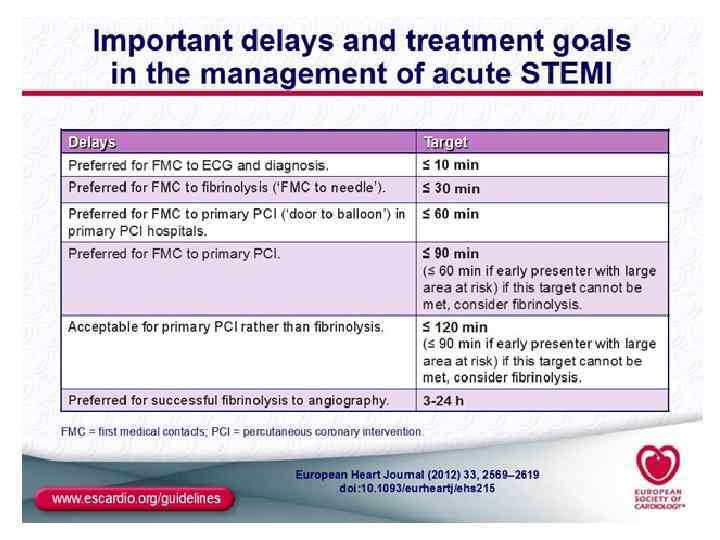
Reperfusion therapy in STEMI • Primary percutaneous coronary intervention (primary PCI) • Thrombolytic (fibrinolytic) therapy ASAP - as soon as possible (!)
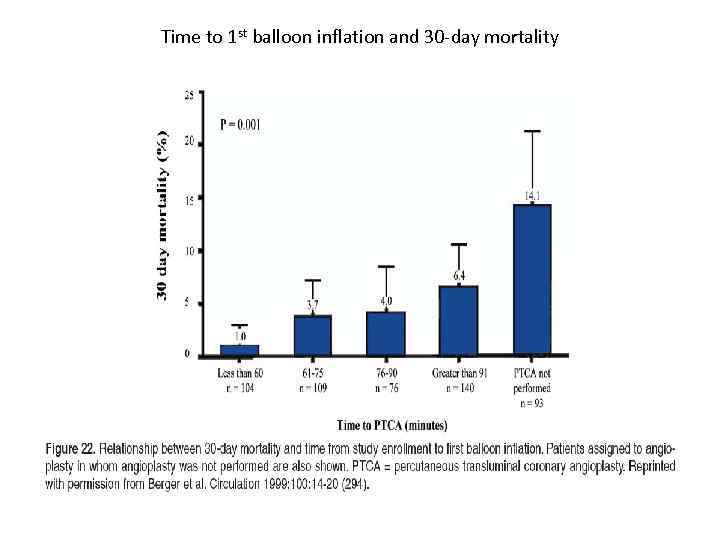
Time to 1 st balloon inflation and 30 -day mortality
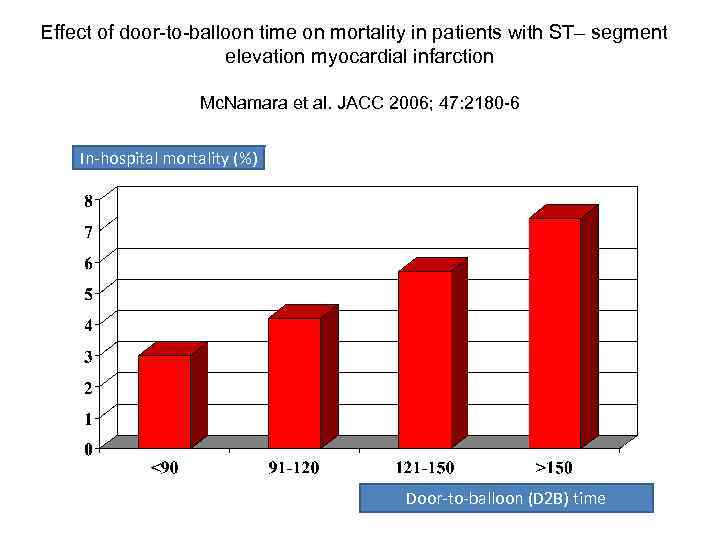
Effect of door-to-balloon time on mortality in patients with ST– segment elevation myocardial infarction Mc. Namara et al. JACC 2006; 47: 2180 -6 In-hospital mortality (%) Door-to-balloon (D 2 B) time
Time is muscle !
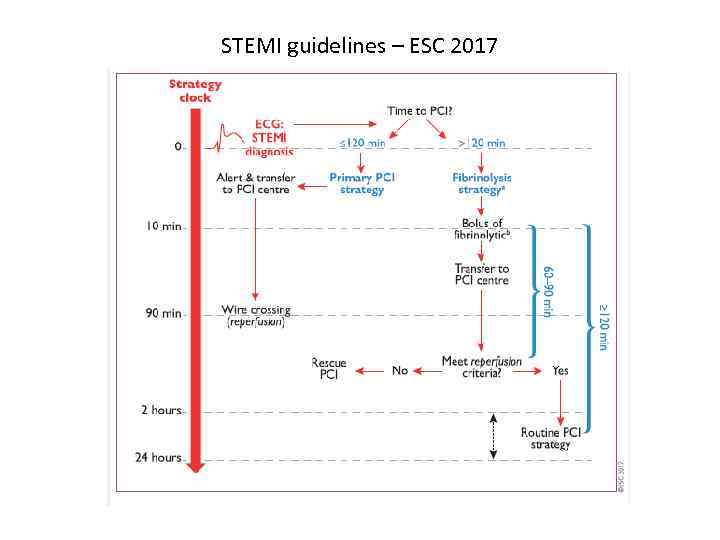
STEMI guidelines – ESC 2017

STEMI guidelines – ESC 2017
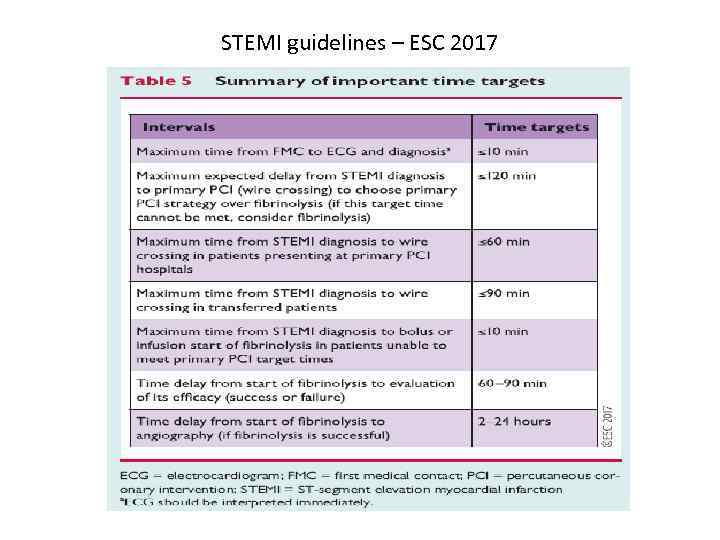
STEMI guidelines – ESC 2017
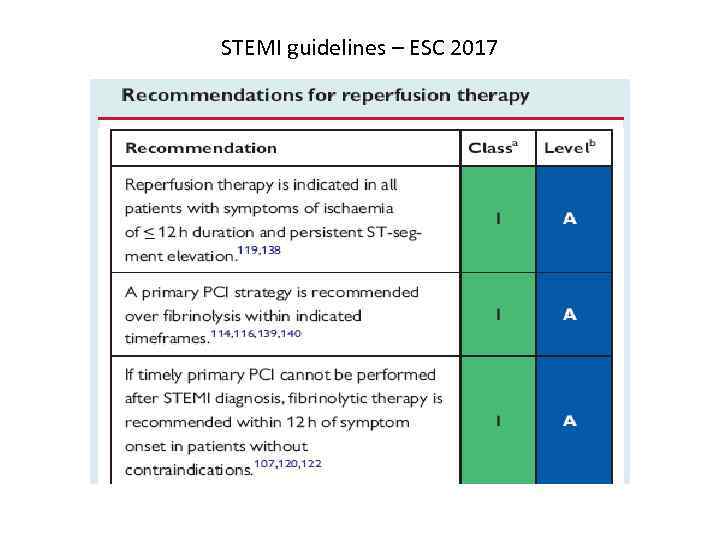
STEMI guidelines – ESC 2017
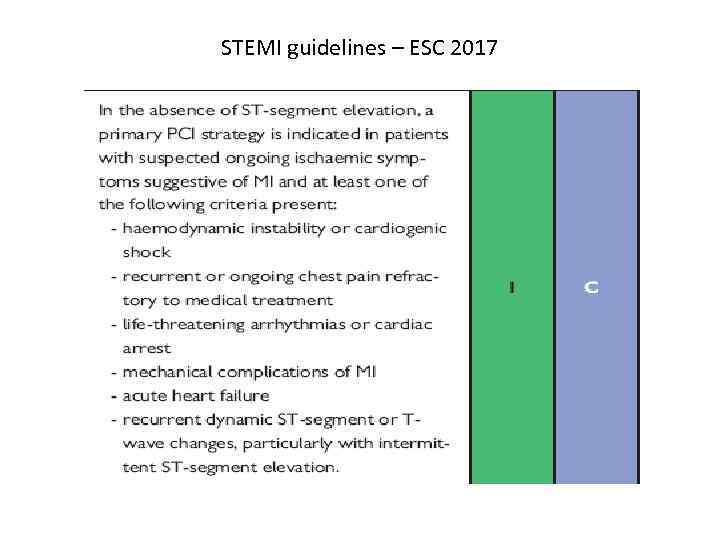
STEMI guidelines – ESC 2017
Primary PCI




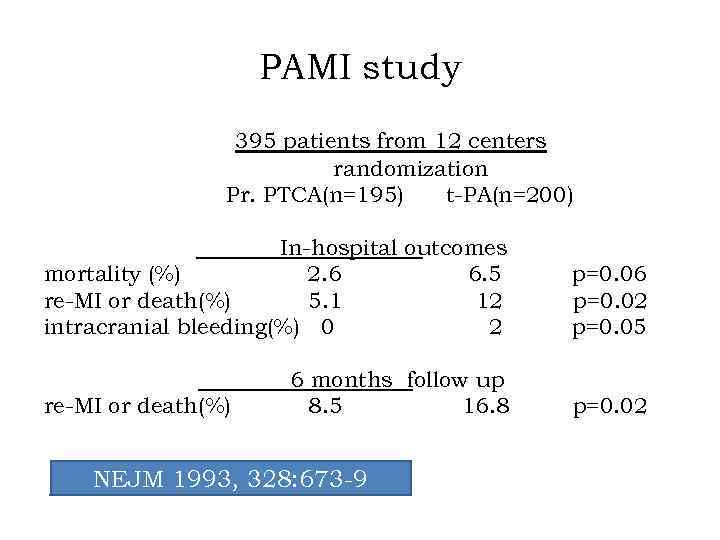
PAMI study 395 patients from 12 centers randomization Pr. PTCA(n=195) t-PA(n=200) In-hospital outcomes mortality (%) 2. 6 6. 5 re-MI or death(%) 5. 1 12 intracranial bleeding(%) 0 2 p=0. 06 p=0. 02 p=0. 05 6 months follow up 8. 5 16. 8 p=0. 02 re-MI or death(%) NEJM 1993, 328: 673 -9
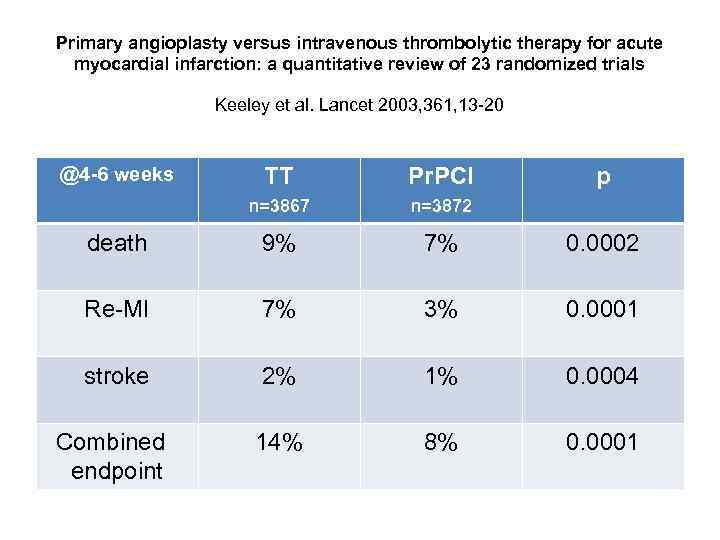
Primary angioplasty versus intravenous thrombolytic therapy for acute myocardial infarction: a quantitative review of 23 randomized trials Keeley et al. Lancet 2003, 361, 13 -20 @4 -6 weeks TT Pr. PCI p n=3867 n=3872 death 9% 7% 0. 0002 Re-MI 7% 3% 0. 0001 stroke 2% 1% 0. 0004 Combined endpoint 14% 8% 0. 0001
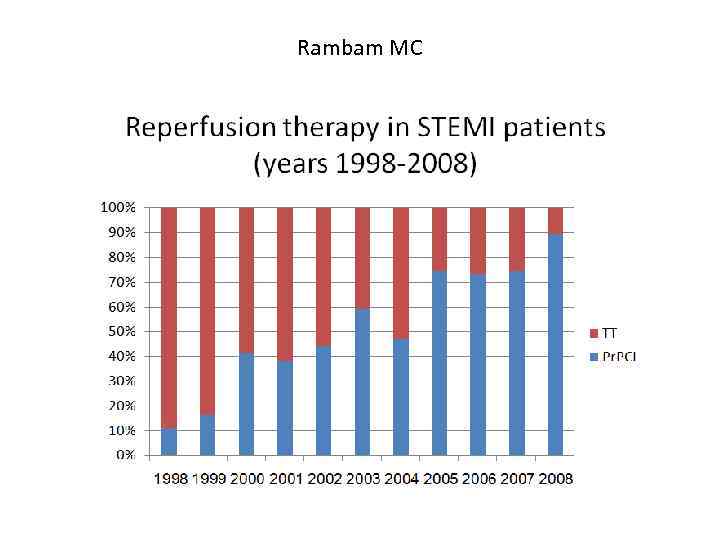
Rambam MC
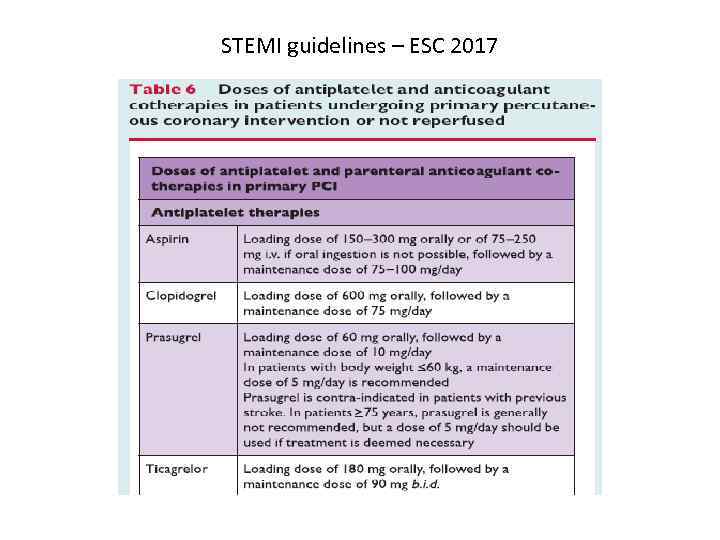
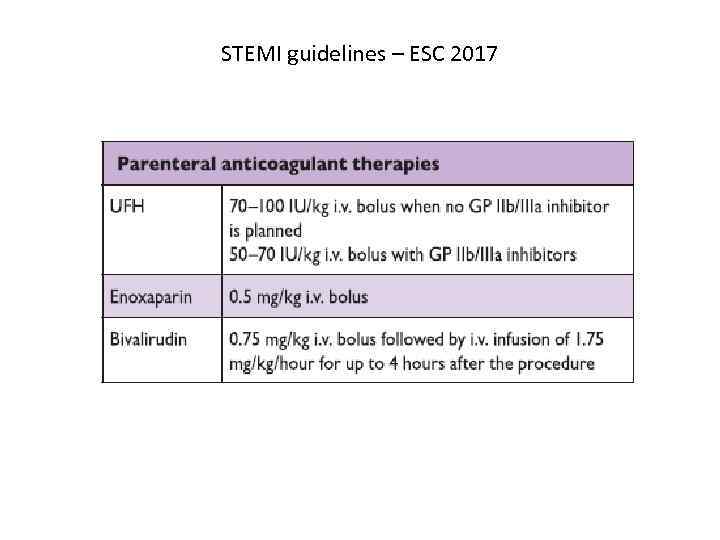
Immediate pharmcologic therapy in patients undergoing primary PCI • Antiplatelet • Anticoagulant
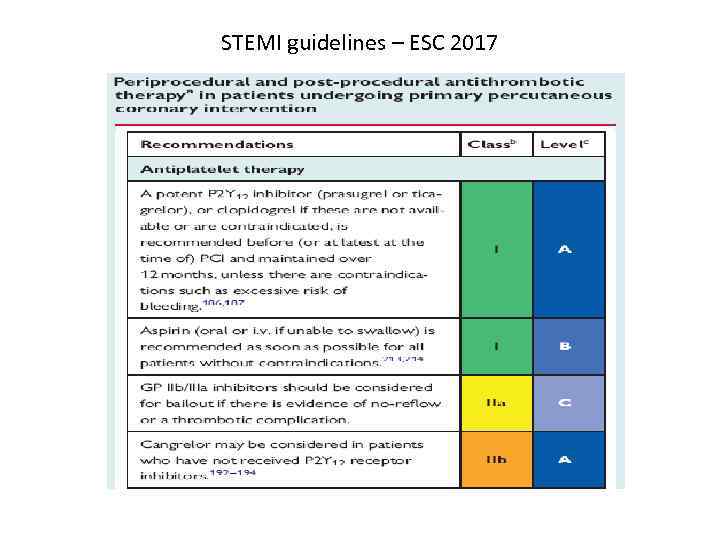
STEMI guidelines – ESC 2017
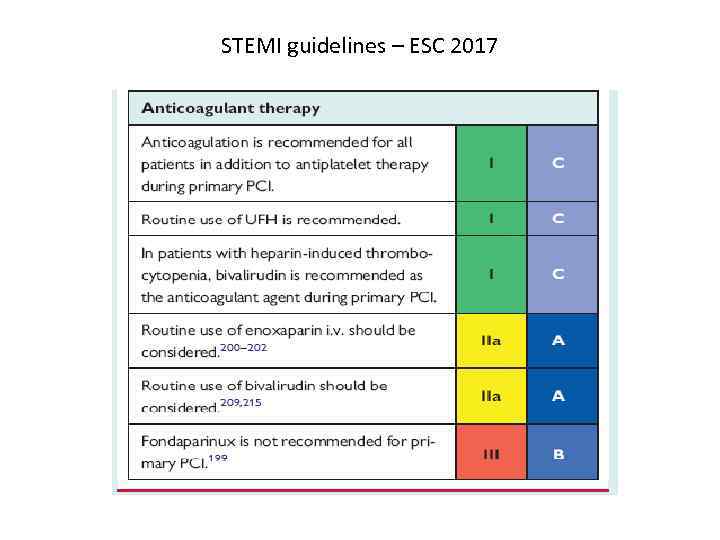
STEMI guidelines – ESC 2017
STEMI guidelines – ESC 2017
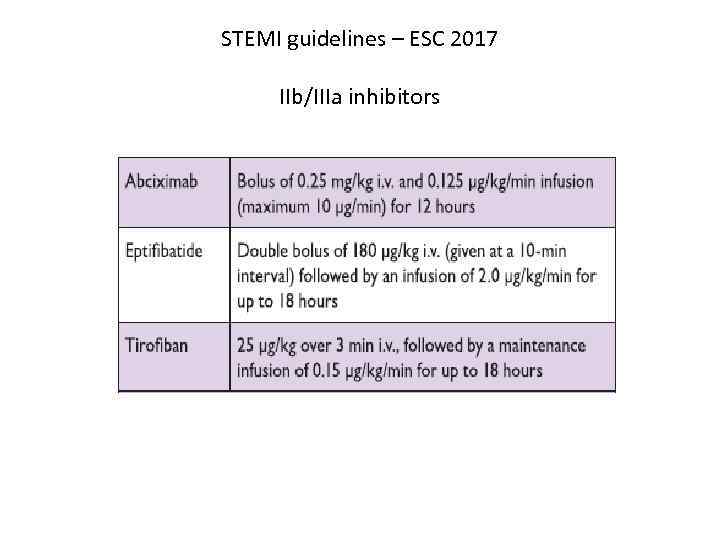
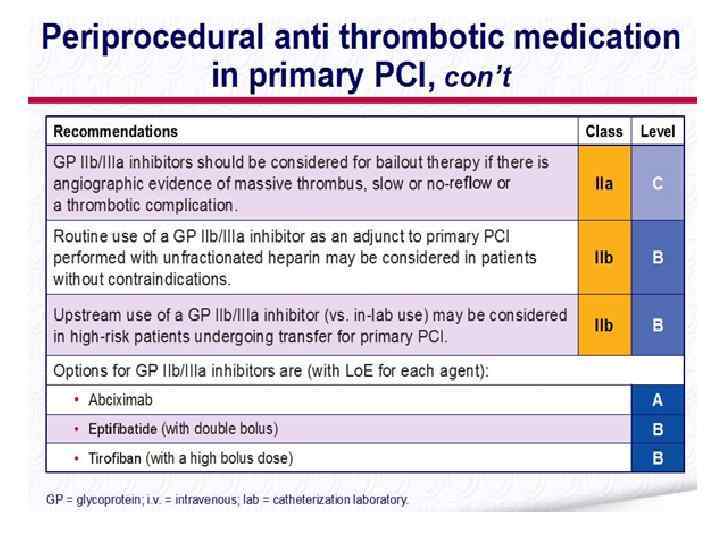
STEMI guidelines – ESC 2017 IIb/IIIa inhibitors
STEMI guidelines – ESC 2017
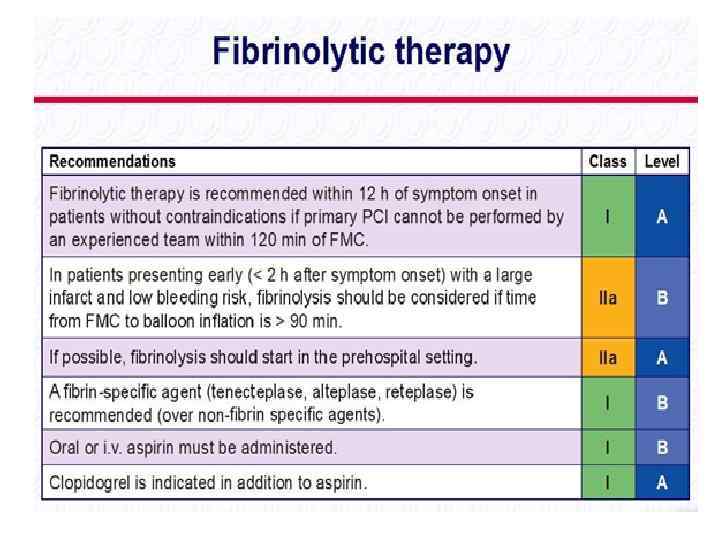
Thrombolytic (fibrinolytic) therapy
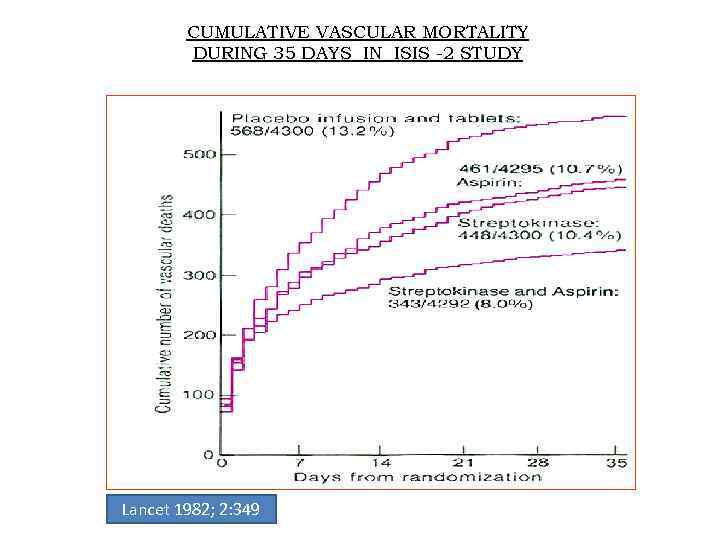
CUMULATIVE VASCULAR MORTALITY DURING 35 DAYS IN ISIS -2 STUDY Lancet 1982; 2: 349
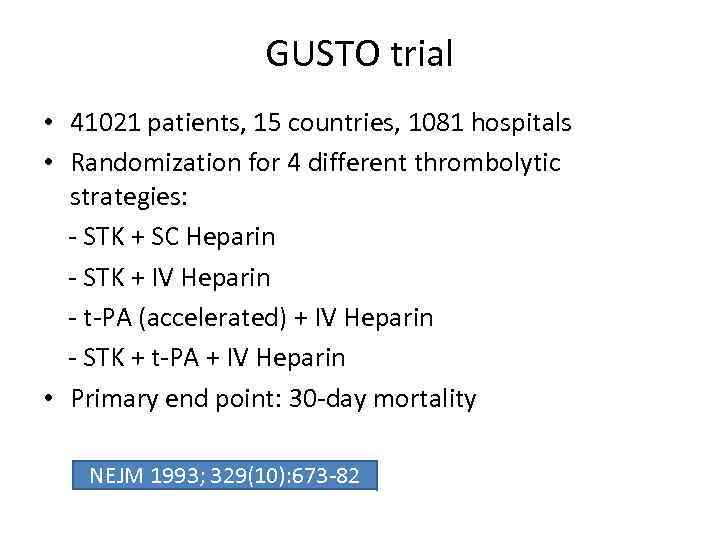
GUSTO trial • 41021 patients, 15 countries, 1081 hospitals • Randomization for 4 different thrombolytic strategies: - STK + SC Heparin - STK + IV Heparin - t-PA (accelerated) + IV Heparin - STK + t-PA + IV Heparin • Primary end point: 30 -day mortality NEJM 1993; 329(10): 673 -82
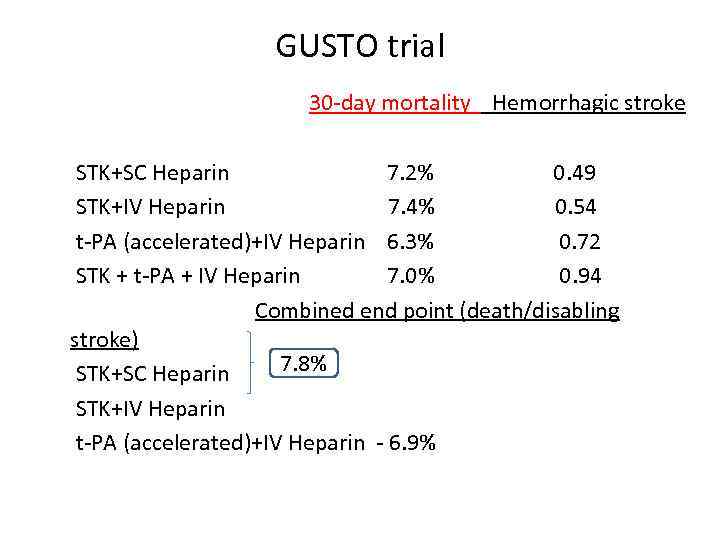
GUSTO trial 30 -day mortality Hemorrhagic stroke STK+SC Heparin 7. 2% 0. 49 STK+IV Heparin 7. 4% 0. 54 t-PA (accelerated)+IV Heparin 6. 3% 0. 72 STK + t-PA + IV Heparin 7. 0% 0. 94 Combined end point (death/disabling stroke) 7. 8% STK+SC Heparin STK+IV Heparin t-PA (accelerated)+IV Heparin - 6. 9%
GUSTO trial Subgroups of patients benefited from t-PA • < 75 years old • anterior location of MI • time to thrombolytic therapy - 0 -4 hrs
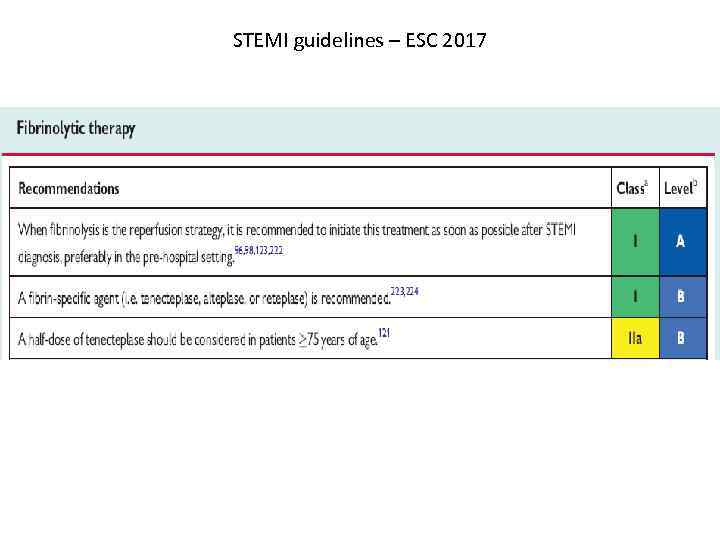
STEMI guidelines – ESC 2017
STEMI guidelines – ESC 2017
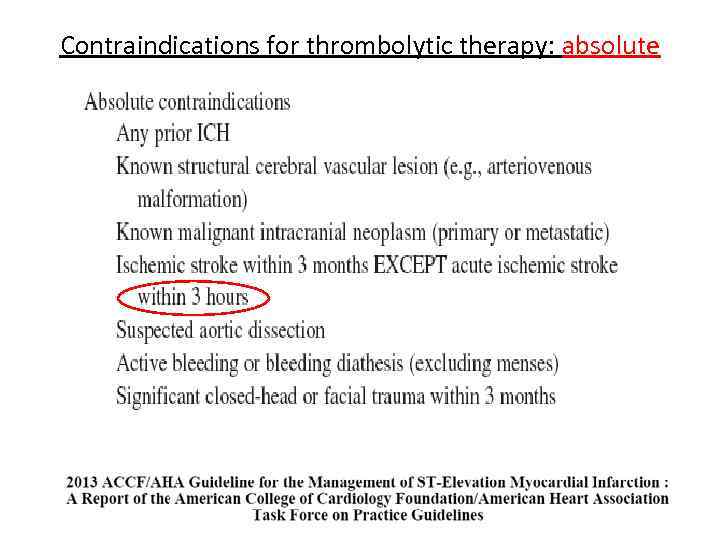
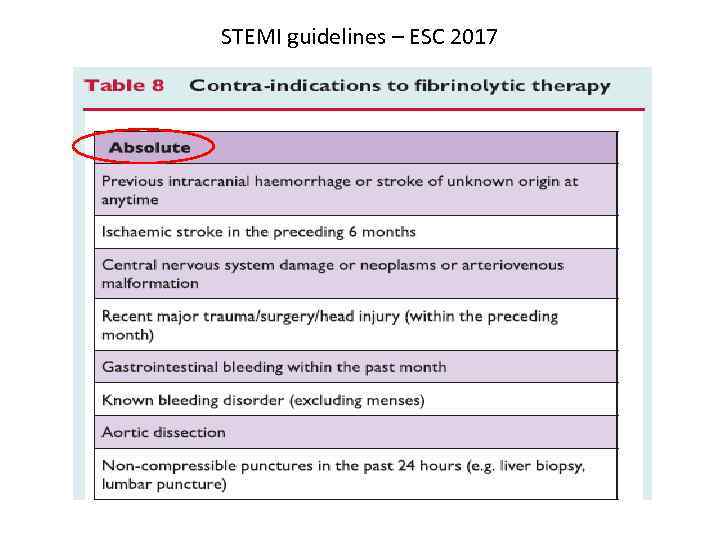
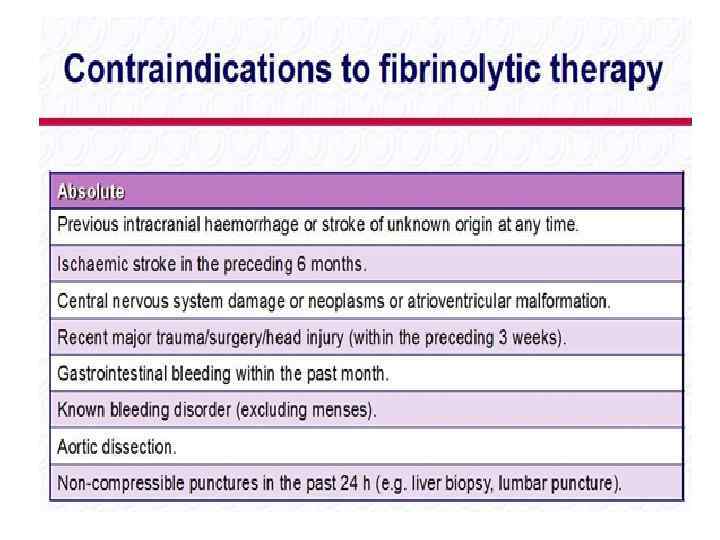
Contraindications for thrombolytic therapy: absolute
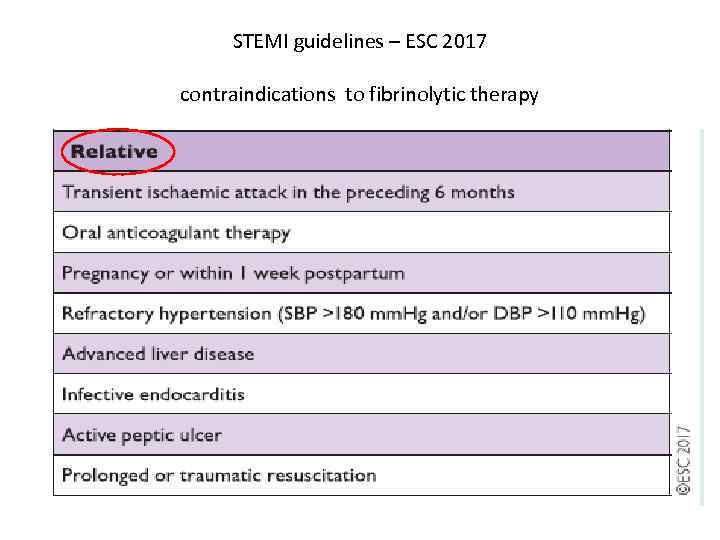
STEMI guidelines – ESC 2017 contraindications to fibrinolytic therapy
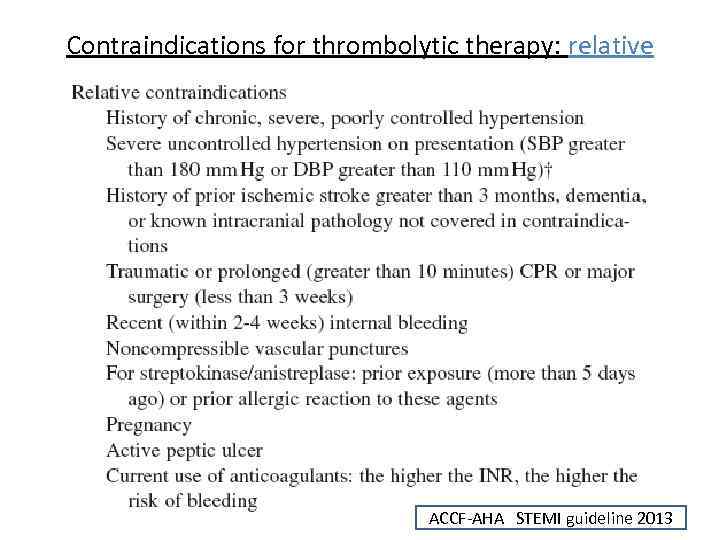
Contraindications for thrombolytic therapy: relative ACCF-AHA STEMI guideline 2013
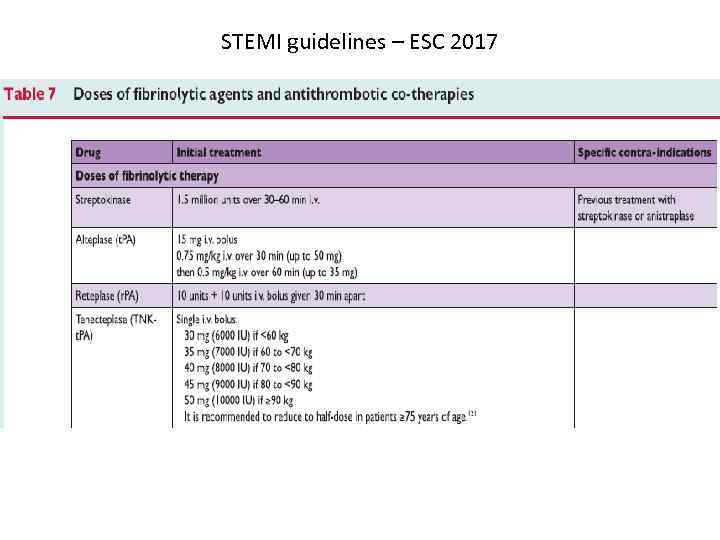
STEMI guidelines – ESC 2017
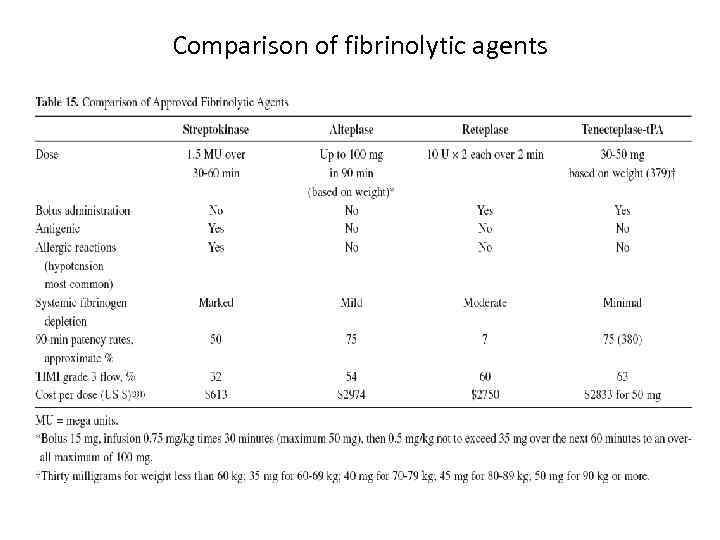
Comparison of fibrinolytic agents
Anticoagulant and antiaggregant therapy in patients treated with fibrinolysis
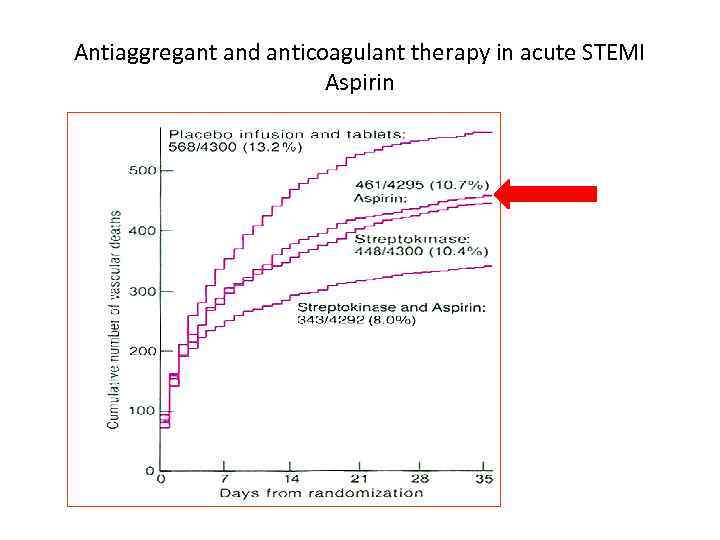
Antiaggregant and anticoagulant therapy in acute STEMI Aspirin
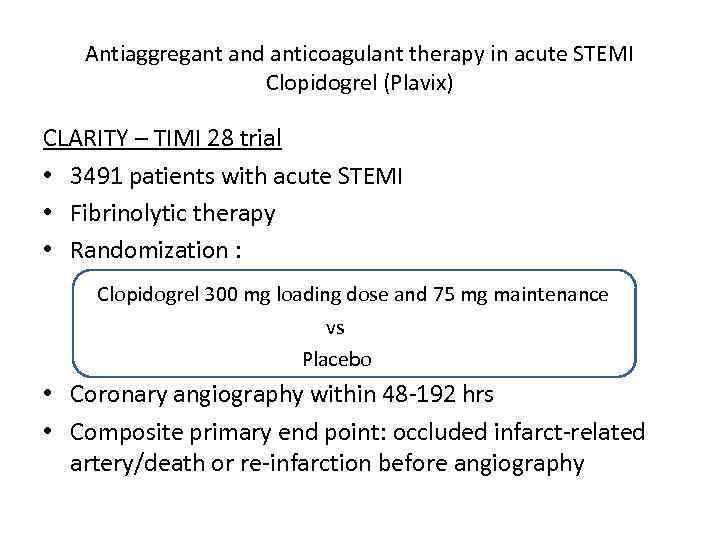
Antiaggregant and anticoagulant therapy in acute STEMI Clopidogrel (Plavix) CLARITY – TIMI 28 trial • 3491 patients with acute STEMI • Fibrinolytic therapy • Randomization : Clopidogrel 300 mg loading dose and 75 mg maintenance vs Placebo • Coronary angiography within 48 -192 hrs • Composite primary end point: occluded infarct-related artery/death or re-infarction before angiography
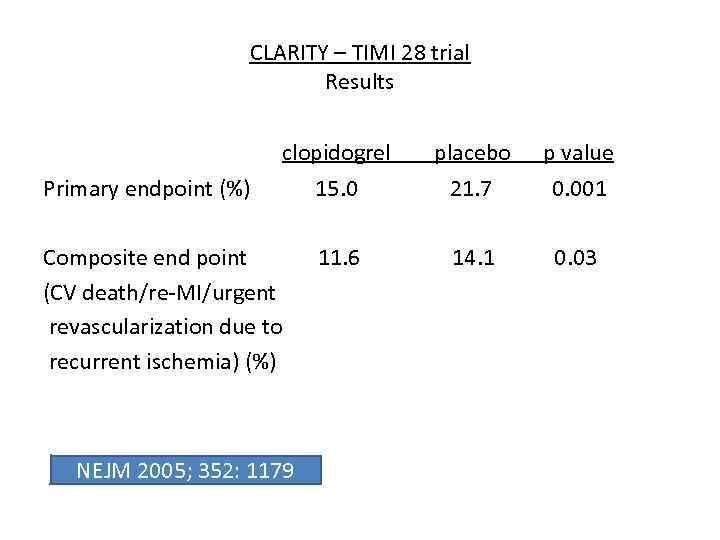
CLARITY – TIMI 28 trial Results clopidogrel placebo p value Primary endpoint (%) 15. 0 21. 7 0. 001 Composite end point (CV death/re-MI/urgent revascularization due to recurrent ischemia) (%) 11. 6 14. 1 0. 03 NEJM 2005; 352: 1179
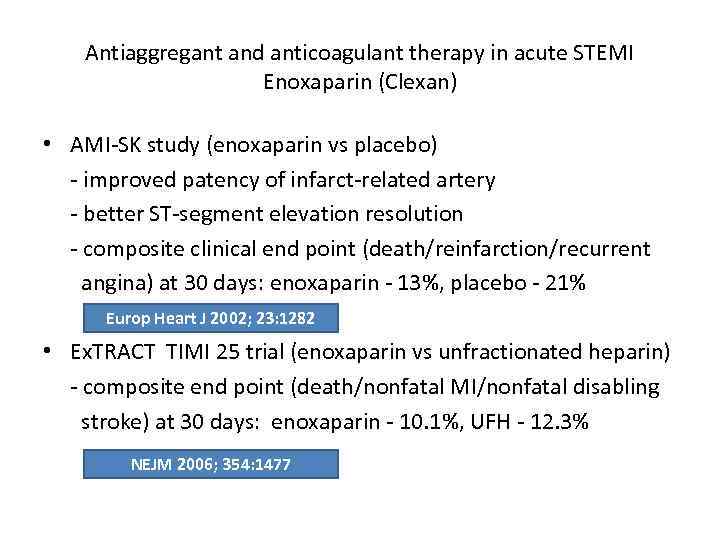
Antiaggregant and anticoagulant therapy in acute STEMI Enoxaparin (Clexan) • AMI-SK study (enoxaparin vs placebo) - improved patency of infarct-related artery - better ST-segment elevation resolution - composite clinical end point (death/reinfarction/recurrent angina) at 30 days: enoxaparin - 13%, placebo - 21% Europ Heart J 2002; 23: 1282 • Ex. TRACT TIMI 25 trial (enoxaparin vs unfractionated heparin) - composite end point (death/nonfatal MI/nonfatal disabling stroke) at 30 days: enoxaparin - 10. 1%, UFH - 12. 3% NEJM 2006; 354: 1477

Antiplatelet and anticoagulant therapy in patients no treated with reperfusion
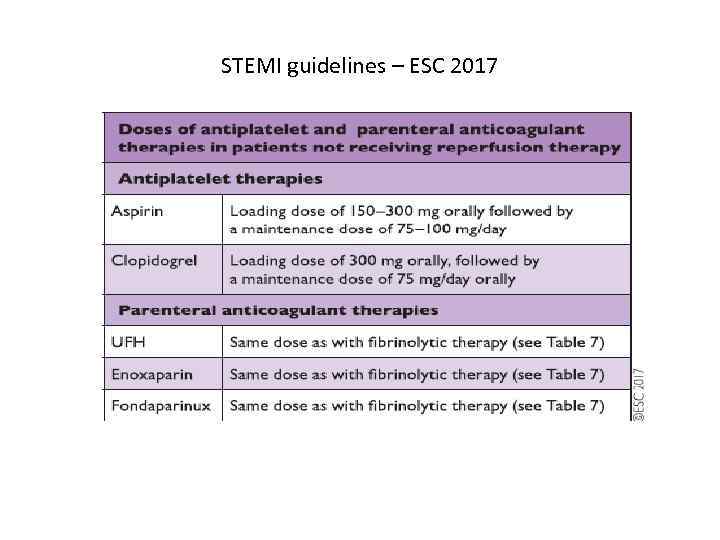
STEMI guidelines – ESC 2017
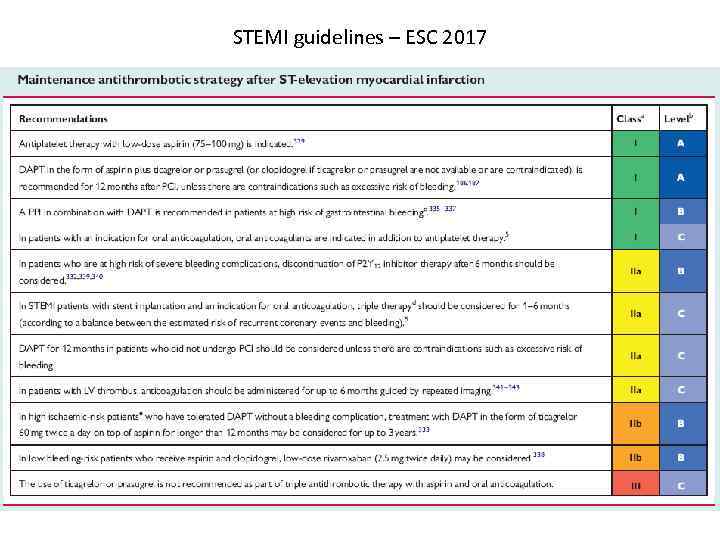
STEMI guidelines – ESC 2017
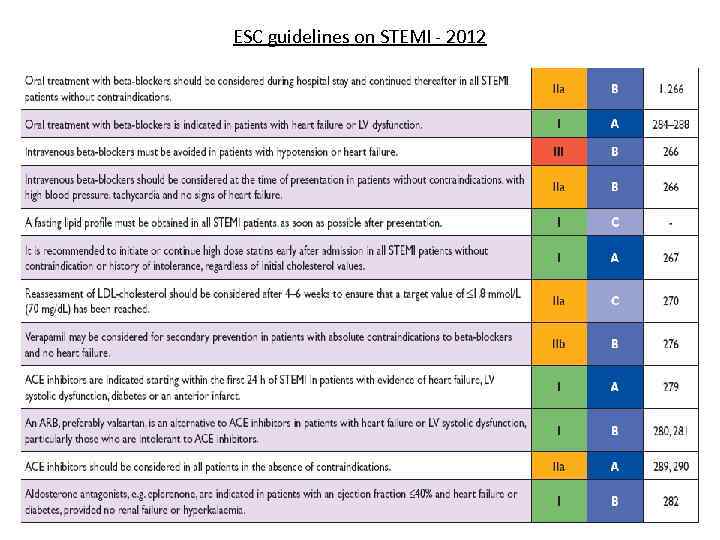
Other important medications • Beta-blockers • ACE inhibitors • Aldosterone antagonists (in patients with reduced LV systolic function and left heart failure) • Statins
Beta-blockers • In patients treated with fibrinolysis IV beta-blokers reduce the incidence of acute malignant arrhythmias, but there is no evidence of long-term clinical benefit • In patients treated with Pr. PCI IV beta-blockers were associated with reduction in infarct size at 5 -7 days and higher EF at 6 months, by CMR in one trial (METOCARD-CNIC) , and showed no benefit in another trial (EARLY-BAMI) • Early IV administration of beta-blocker at the time of presentation followed by oral beta-blocker should be considered in hemodynamically stable patients • Oral long-term beta-blocker therapy was associated with reduced mortality in some but not all studies • Administration of beta-blocker is recommended within first 24 hours if there is no c/i (acute HF, hemodynamic instability, high degree AV block) • Duration of therapy is not known (if there is no specific indication)
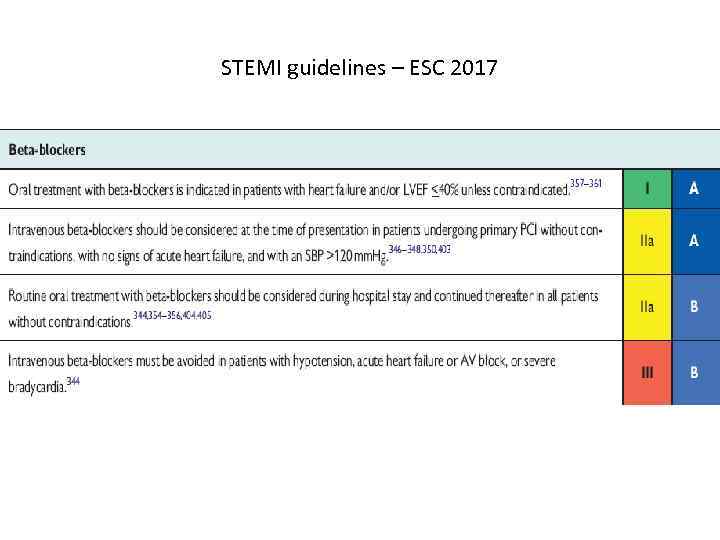
STEMI guidelines – ESC 2017
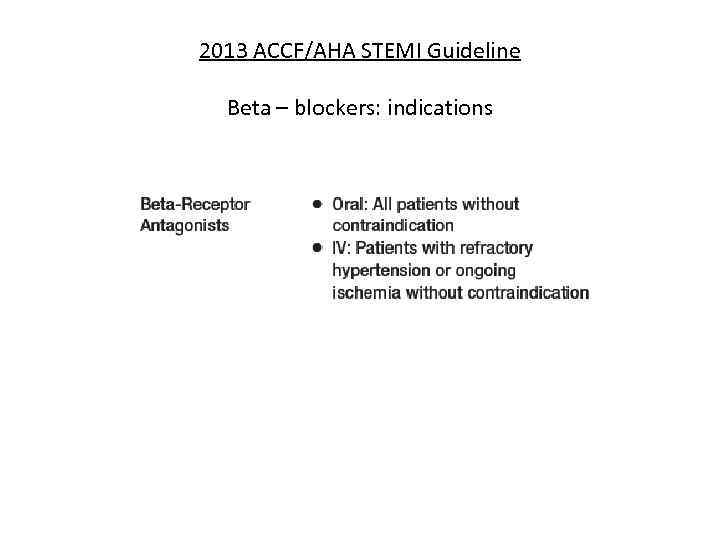
2013 ACCF/AHA STEMI Guideline Beta – blockers: indications
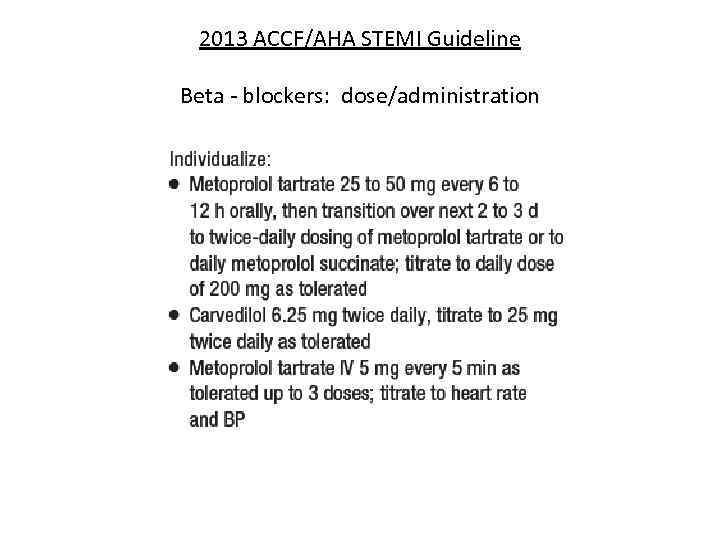
2013 ACCF/AHA STEMI Guideline Beta - blockers: dose/administration
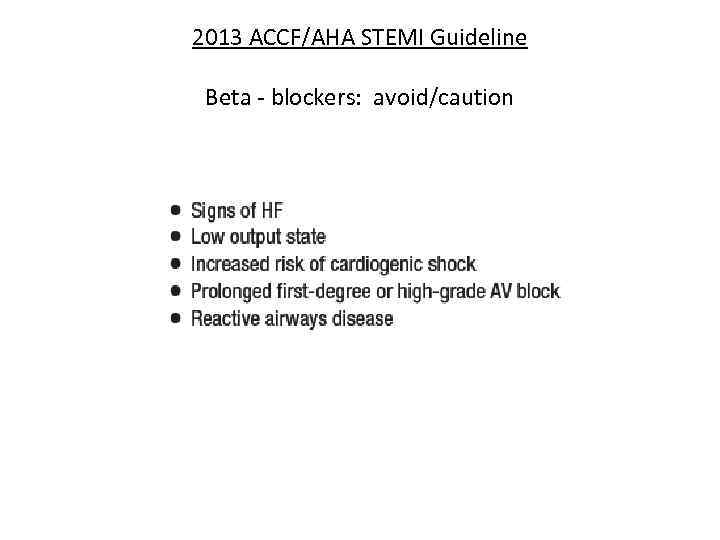
2013 ACCF/AHA STEMI Guideline Beta - blockers: avoid/caution
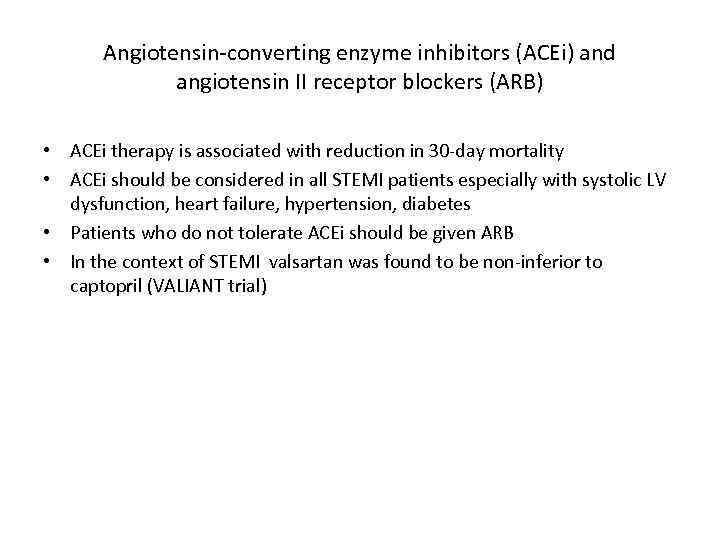
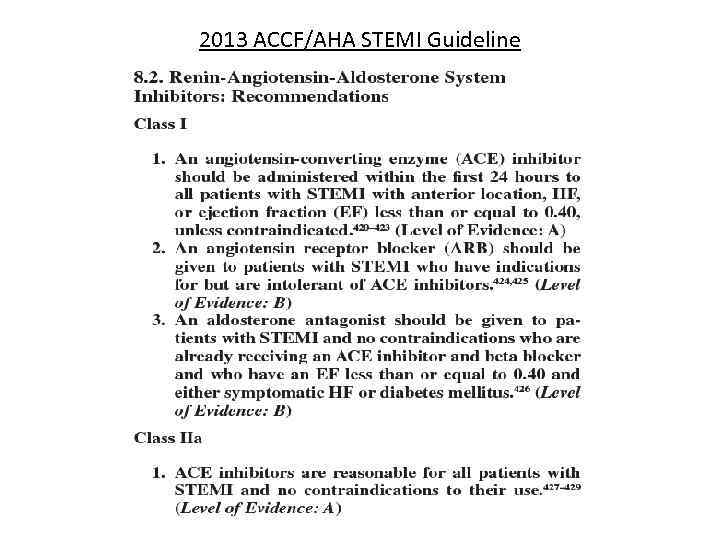
Angiotensin-converting enzyme inhibitors (ACEi) and angiotensin II receptor blockers (ARB) • ACEi therapy is associated with reduction in 30 -day mortality • ACEi should be considered in all STEMI patients especially with systolic LV dysfunction, heart failure, hypertension, diabetes • Patients who do not tolerate ACEi should be given ARB • In the context of STEMI valsartan was found to be non-inferior to captopril (VALIANT trial)
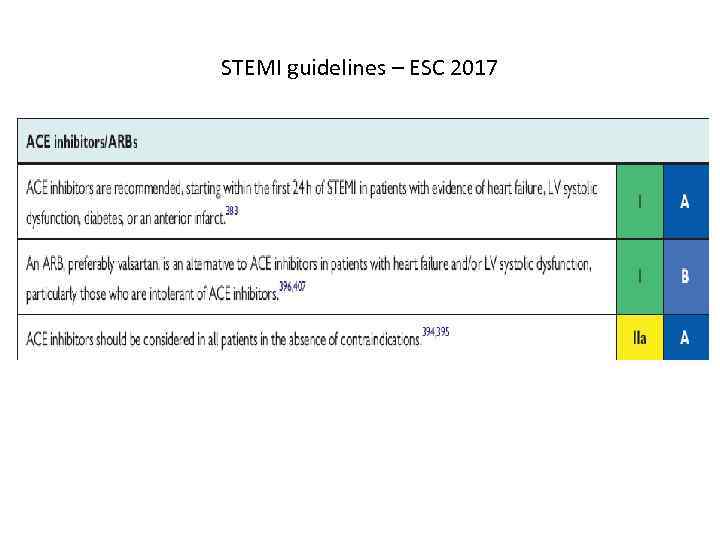
STEMI guidelines – ESC 2017
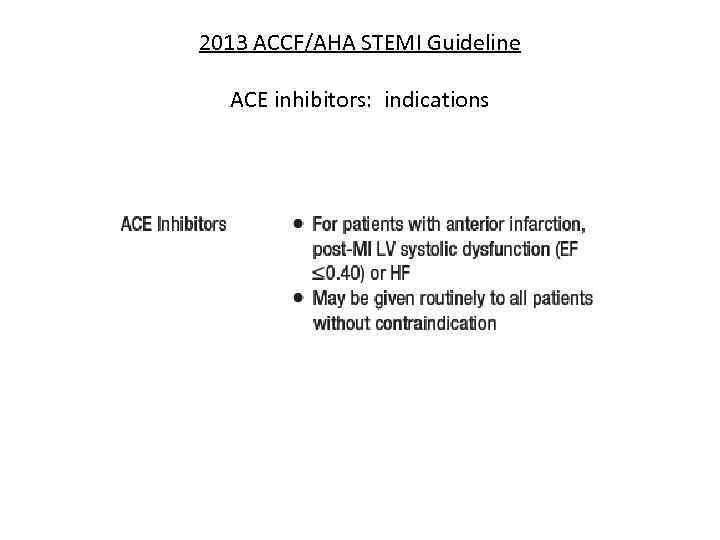
2013 ACCF/AHA STEMI Guideline ACE inhibitors: indications
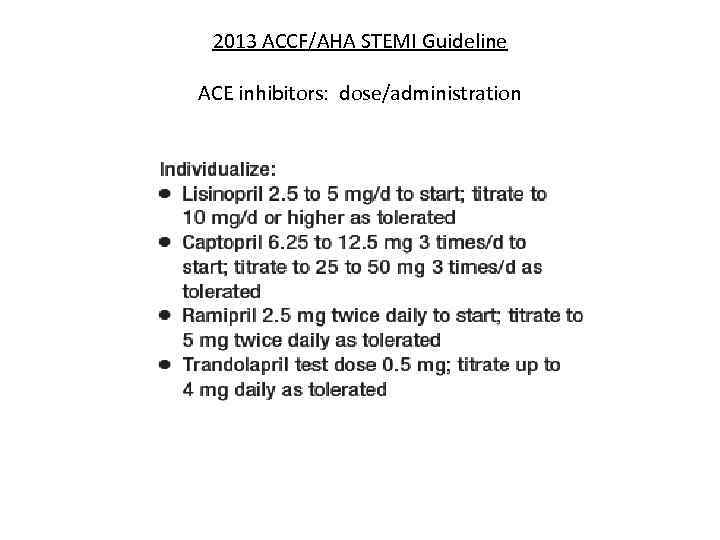
2013 ACCF/AHA STEMI Guideline ACE inhibitors: dose/administration
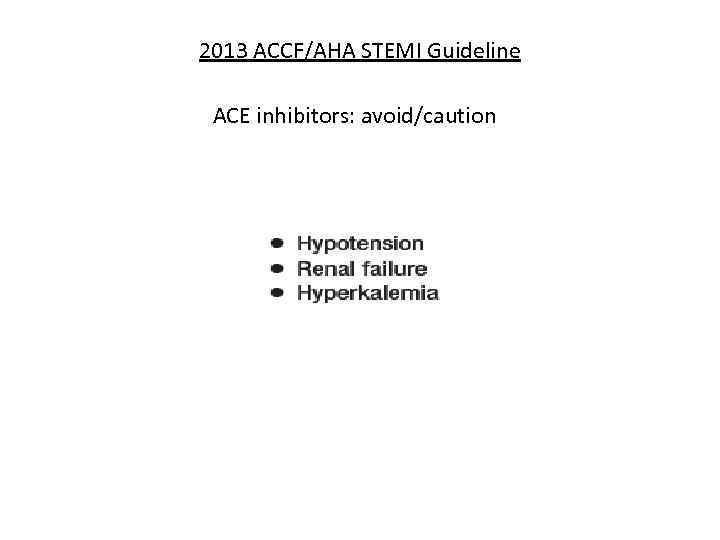
2013 ACCF/AHA STEMI Guideline ACE inhibitors: avoid/caution
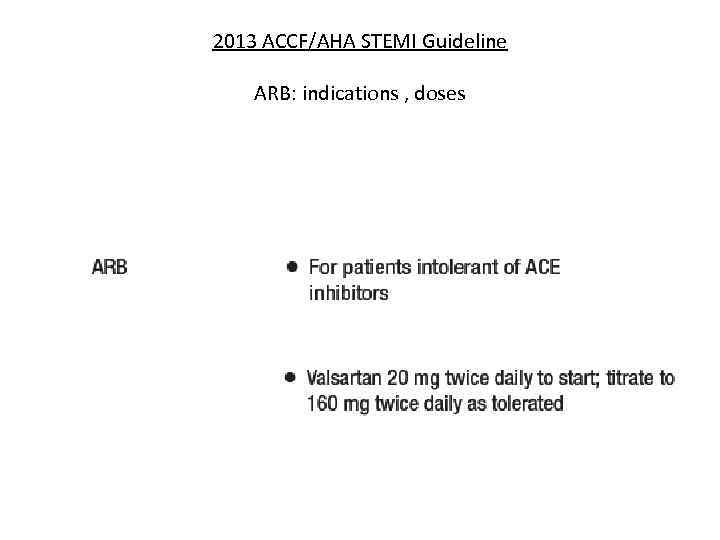
2013 ACCF/AHA STEMI Guideline ARB: indications , doses
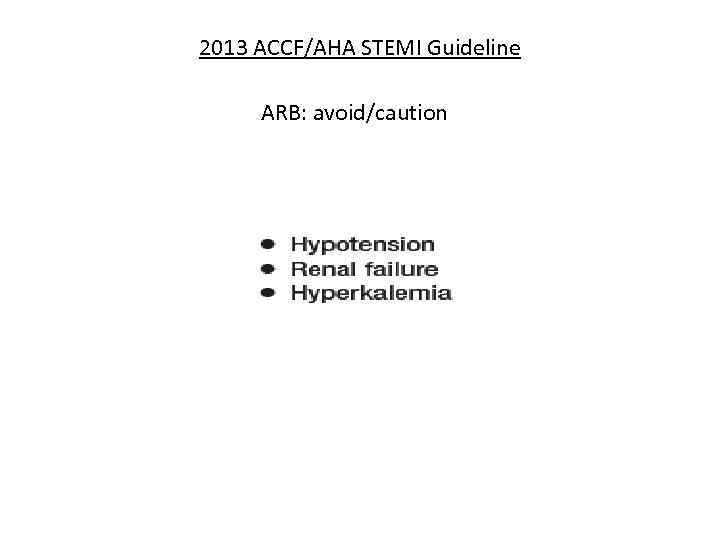
2013 ACCF/AHA STEMI Guideline ARB: avoid/caution
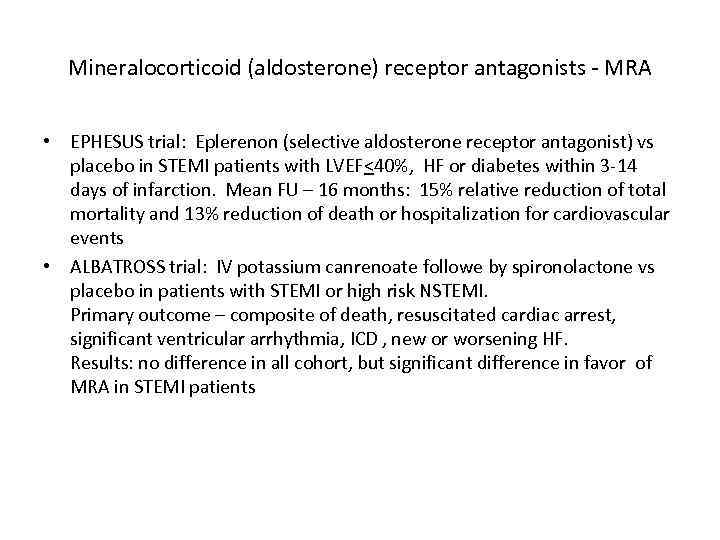
Mineralocorticoid (aldosterone) receptor antagonists - MRA • EPHESUS trial: Eplerenon (selective aldosterone receptor antagonist) vs placebo in STEMI patients with LVEF<40%, HF or diabetes within 3 -14 days of infarction. Mean FU – 16 months: 15% relative reduction of total mortality and 13% reduction of death or hospitalization for cardiovascular events • ALBATROSS trial: IV potassium canrenoate followe by spironolactone vs placebo in patients with STEMI or high risk NSTEMI. Primary outcome – composite of death, resuscitated cardiac arrest, significant ventricular arrhythmia, ICD , new or worsening HF. Results: no difference in all cohort, but significant difference in favor of MRA in STEMI patients
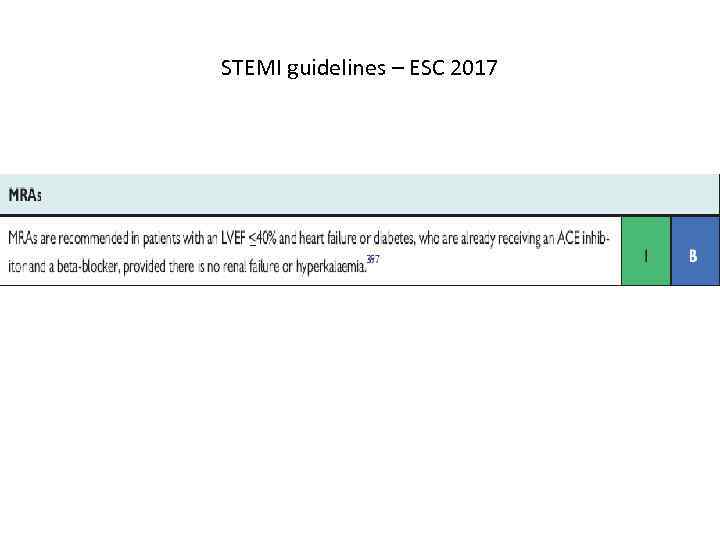
STEMI guidelines – ESC 2017
2013 ACCF/AHA STEMI Guideline
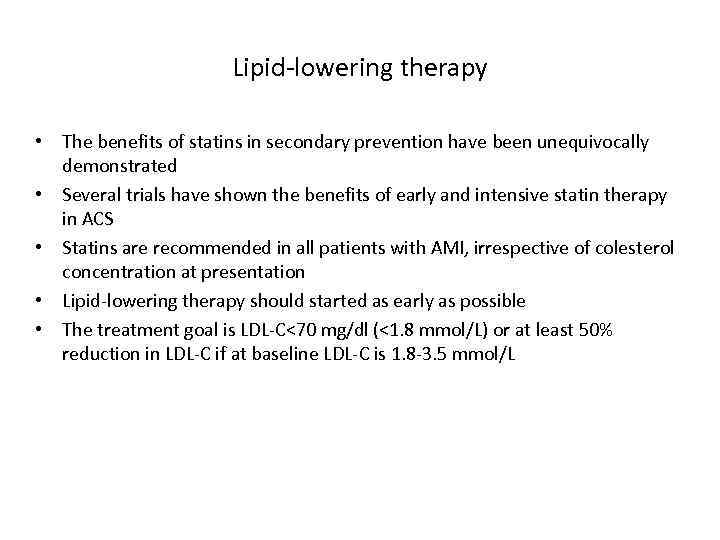
Lipid-lowering therapy • The benefits of statins in secondary prevention have been unequivocally demonstrated • Several trials have shown the benefits of early and intensive statin therapy in ACS • Statins are recommended in all patients with AMI, irrespective of colesterol concentration at presentation • Lipid-lowering therapy should started as early as possible • The treatment goal is LDL-C<70 mg/dl (<1. 8 mmol/L) or at least 50% reduction in LDL-C if at baseline LDL-C is 1. 8 -3. 5 mmol/L
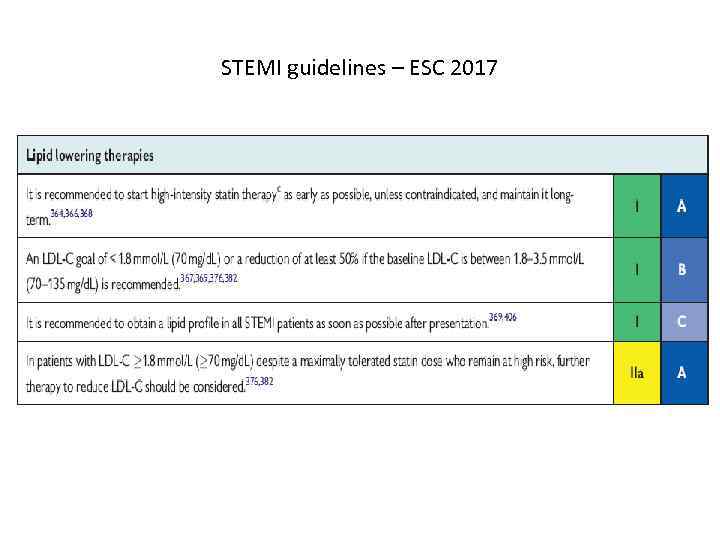
STEMI guidelines – ESC 2017
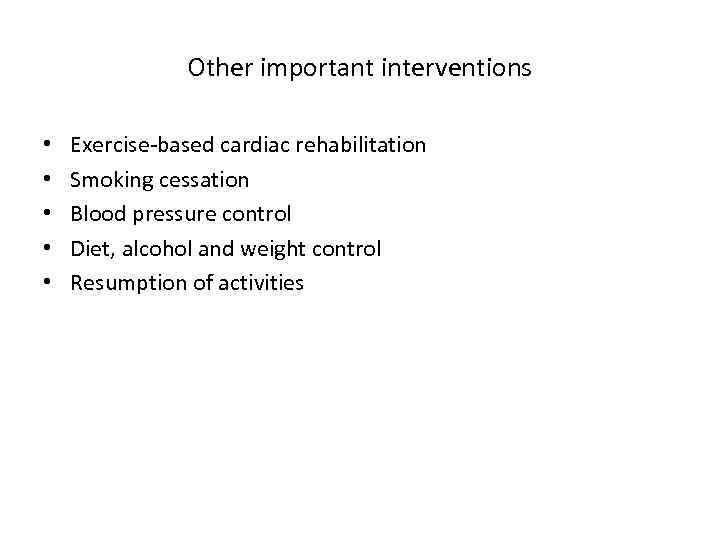
Other important interventions • • • Exercise-based cardiac rehabilitation Smoking cessation Blood pressure control Diet, alcohol and weight control Resumption of activities
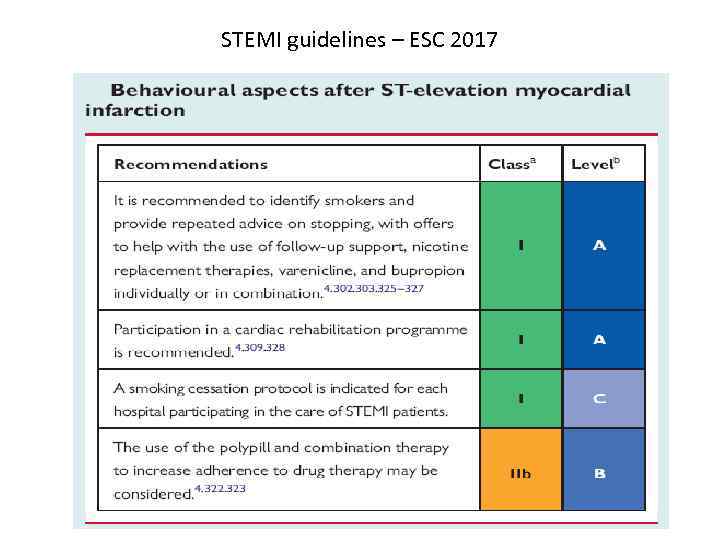
STEMI guidelines – ESC 2017
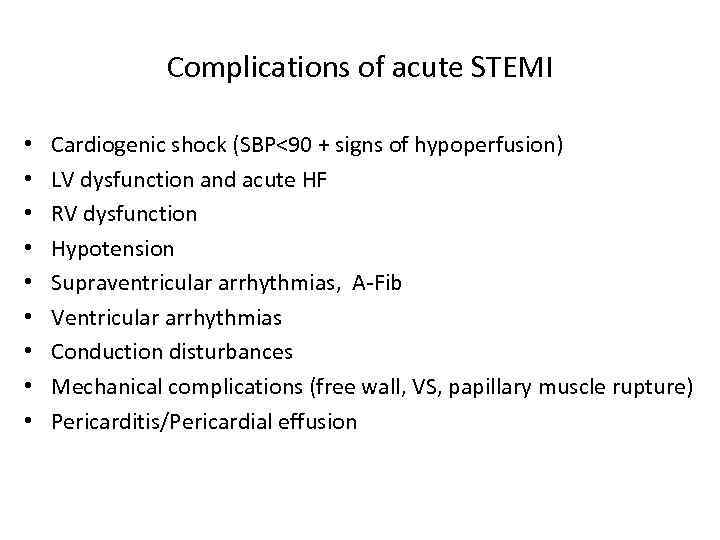
Complications of acute STEMI • • • Cardiogenic shock (SBP<90 + signs of hypoperfusion) LV dysfunction and acute HF RV dysfunction Hypotension Supraventricular arrhythmias, A-Fib Ventricular arrhythmias Conduction disturbances Mechanical complications (free wall, VS, papillary muscle rupture) Pericarditis/Pericardial effusion
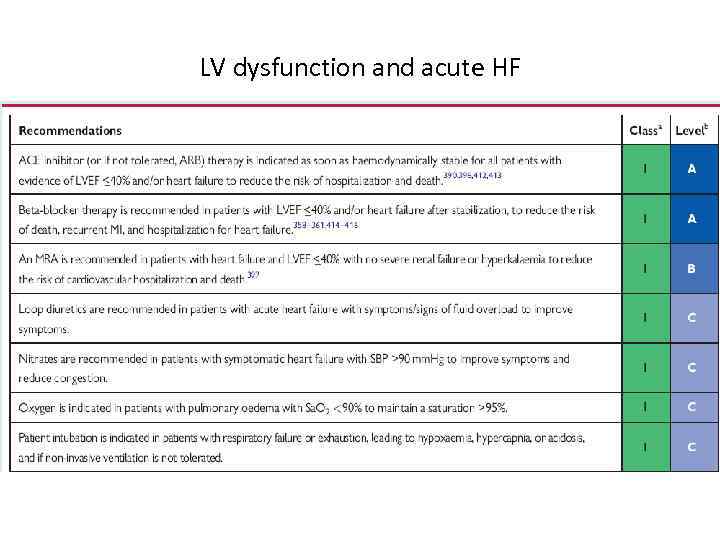
LV dysfunction and acute HF
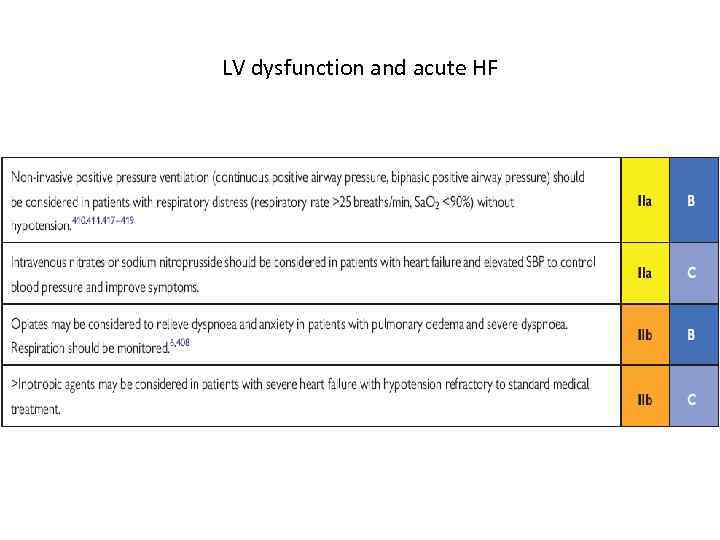
LV dysfunction and acute HF
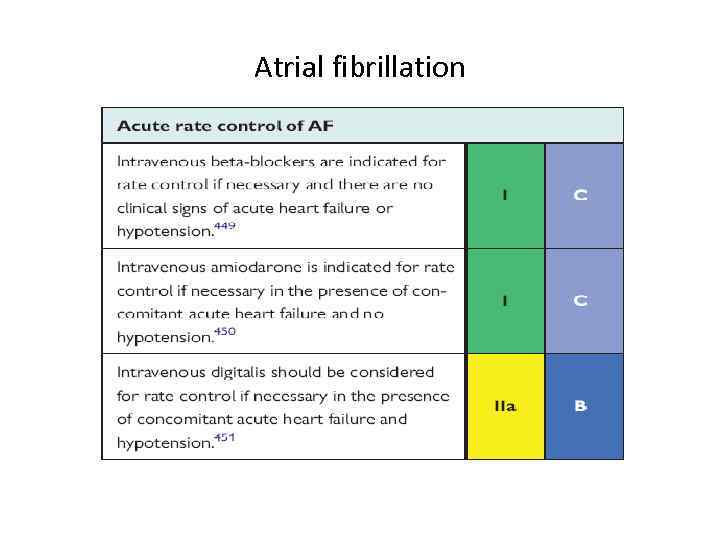
Atrial fibrillation
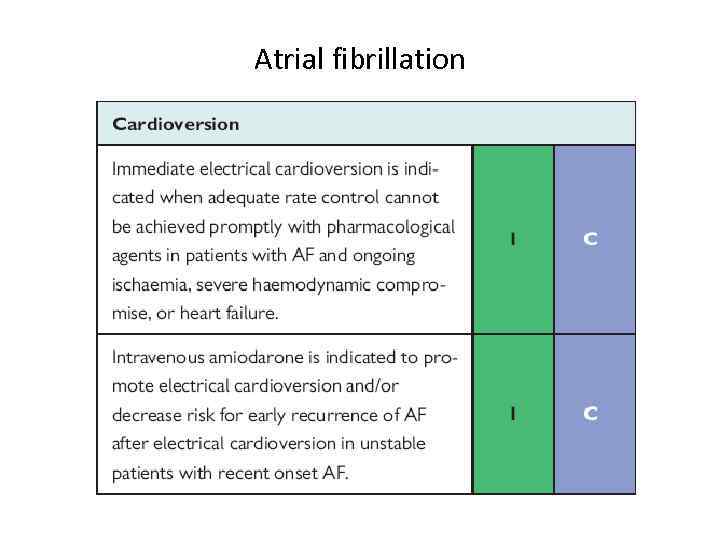
Atrial fibrillation
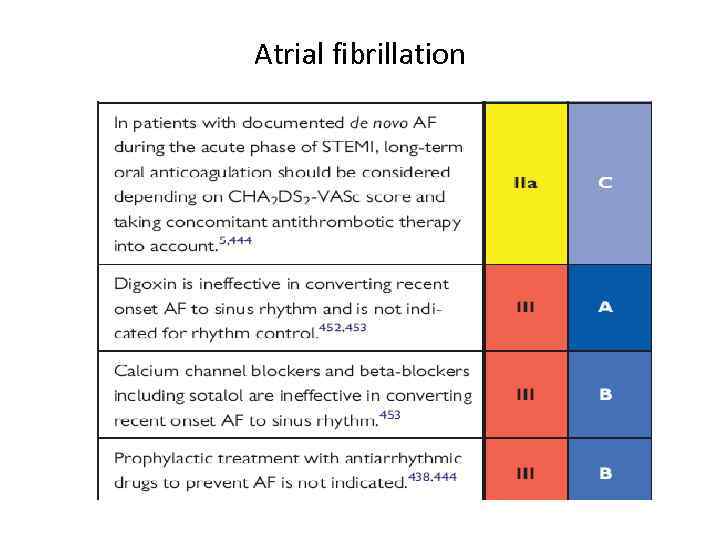
Atrial fibrillation
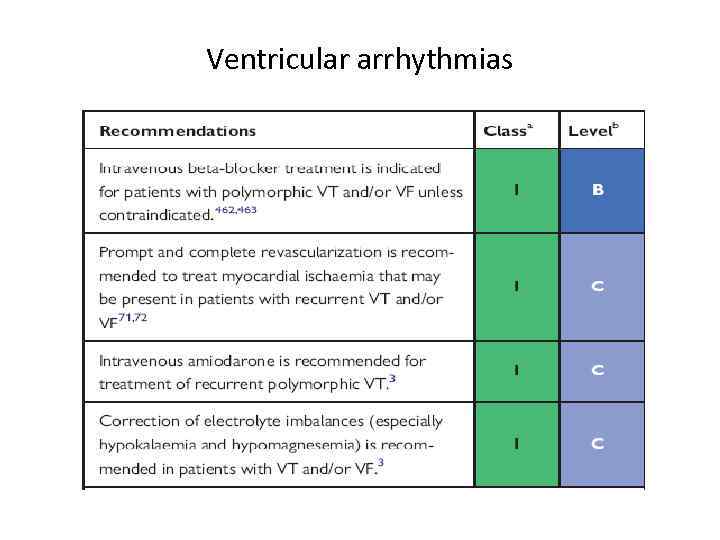
Ventricular arrhythmias
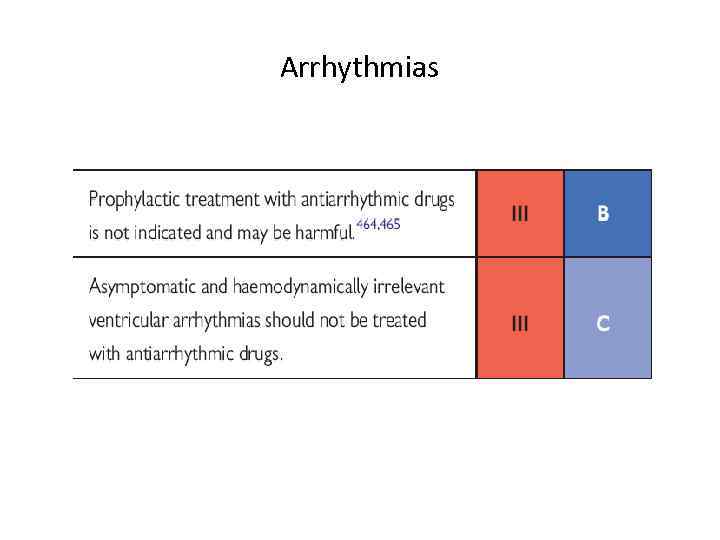
Arrhythmias
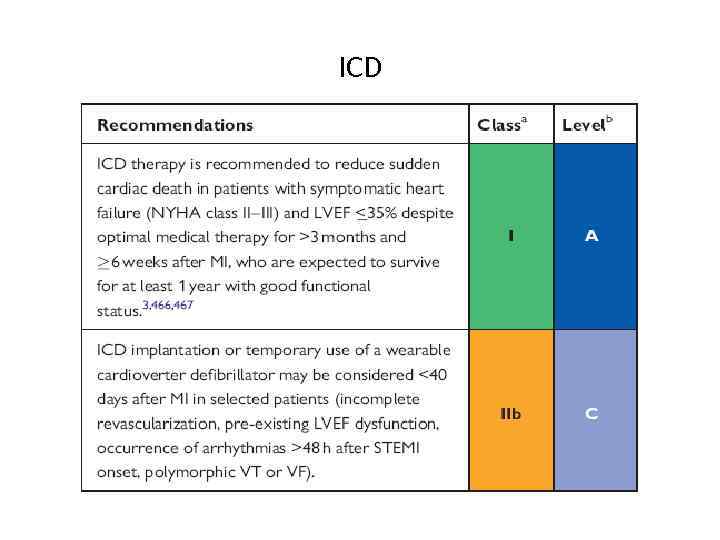
ICD
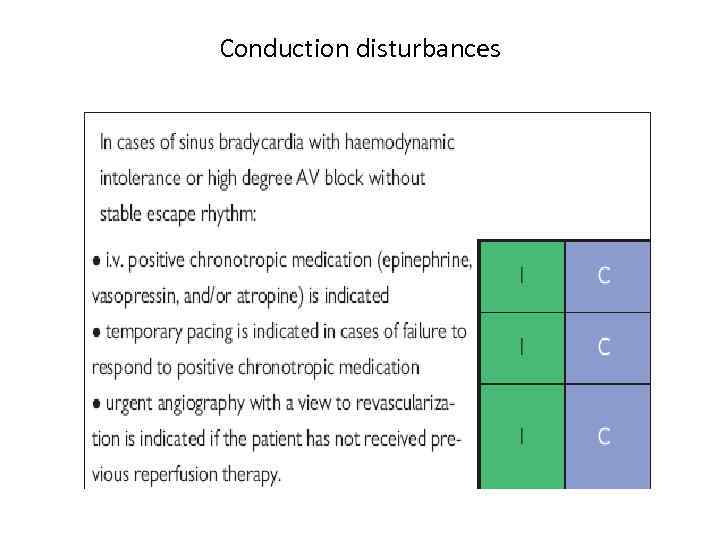
Conduction disturbances
Thank you for attention
Backup slides


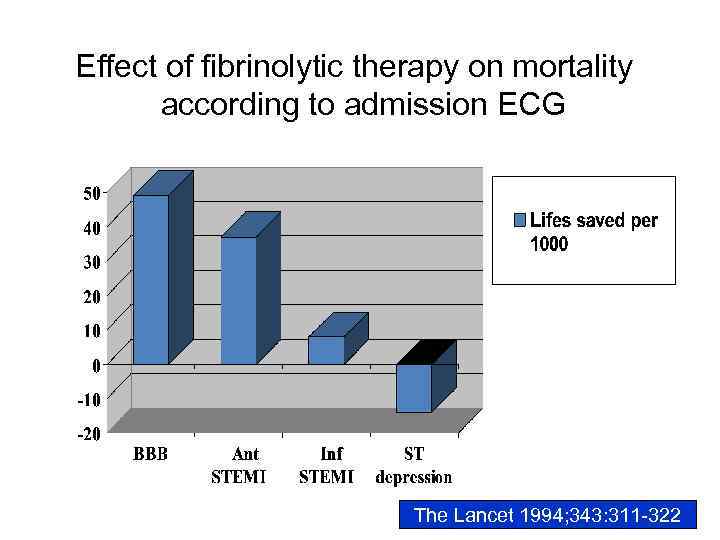
Effect of fibrinolytic therapy on mortality according to admission ECG The Lancet 1994; 343: 311 -322
• Medical Rx: - antiaggregants - anticoagulants - IIb/IIIa inhibitors - beta-blockers - statins
NSTEMI & Unstable angina Early invasive vs selectively invasive strategy
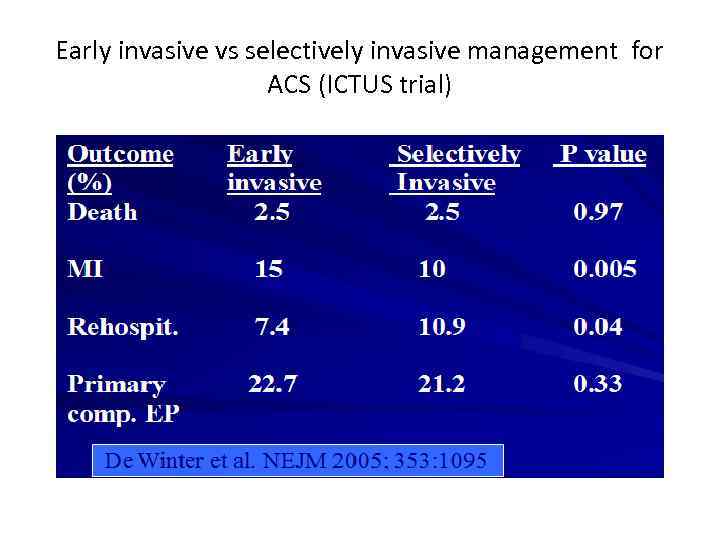
Early invasive vs selectively invasive management for ACS (ICTUS trial)
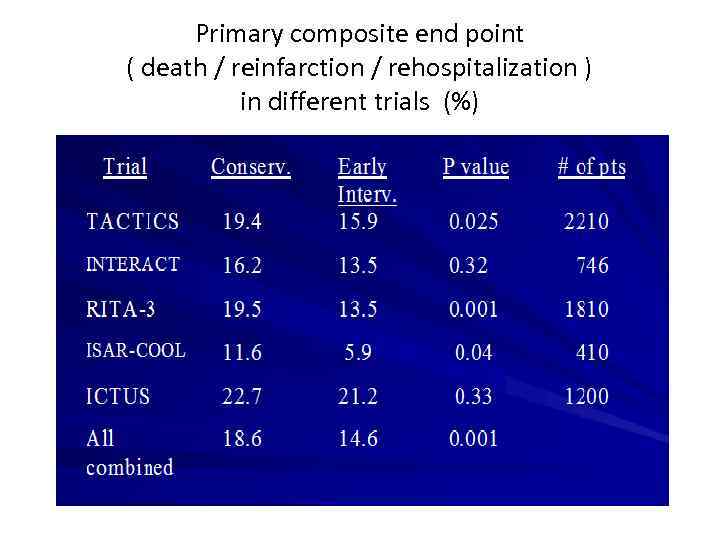
Primary composite end point ( death / reinfarction / rehospitalization ) in different trials (%)

Definition of AMI Universal definition of myocardial infarction Joint ESC/ACCF/AHA/WHF Task Force for the redefinition of myocardial infarction European Heart Journal 2007; 28(20): 2526 -2538
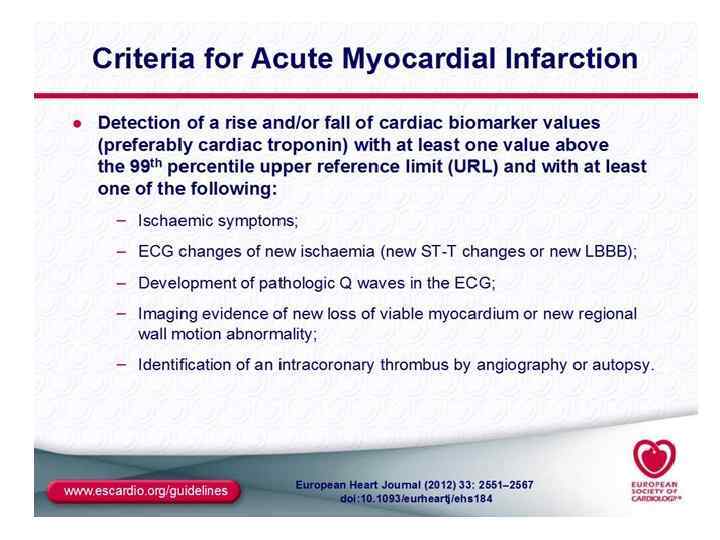
Definition of AMI Criteria for acute myocardial infarction • The term of myocardial infarction should be used when there is evidence of myocardial necrosis in a clinical setting consistent with myocardial ischemia • Under these conditions any one of the following criteria meets the diagnosis for myocardial infarction
Definition of AMI 1. Detection of rise and fall of cardiac biomarkers (preferably troponin) with at least one value above the 99 th percentile of the upper reference limit (URL) together with evidence of myocardial ischemia with at least one of the following: - symptoms of ischemia - ECG changes indicative of new ischemia (new ST-T changes or new LBBB) - development of pathological Q waves in the ECG - imaging evidence of new loss of viable myocardium or new regional wall motion abnormality
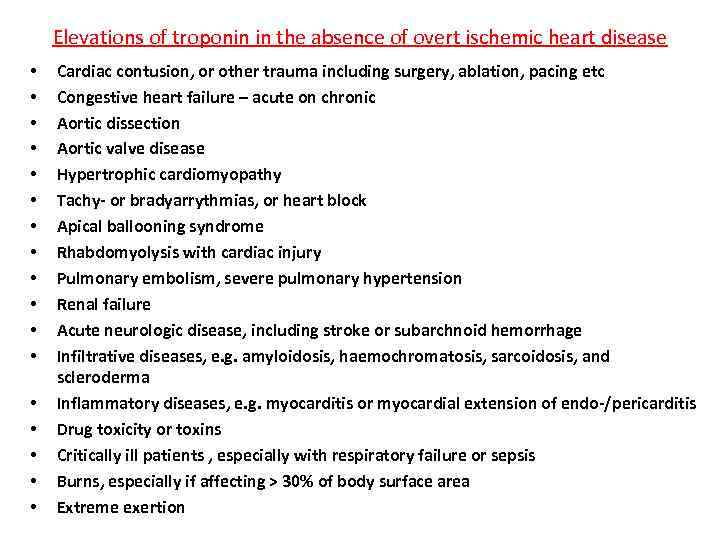
Elevations of troponin in the absence of overt ischemic heart disease • • • • • Cardiac contusion, or other trauma including surgery, ablation, pacing etc Congestive heart failure – acute on chronic Aortic dissection Aortic valve disease Hypertrophic cardiomyopathy Tachy- or bradyarrythmias, or heart block Apical ballooning syndrome Rhabdomyolysis with cardiac injury Pulmonary embolism, severe pulmonary hypertension Renal failure Acute neurologic disease, including stroke or subarchnoid hemorrhage Infiltrative diseases, e. g. amyloidosis, haemochromatosis, sarcoidosis, and scleroderma Inflammatory diseases, e. g. myocarditis or myocardial extension of endo-/pericarditis Drug toxicity or toxins Critically ill patients , especially with respiratory failure or sepsis Burns, especially if affecting > 30% of body surface area Extreme exertion
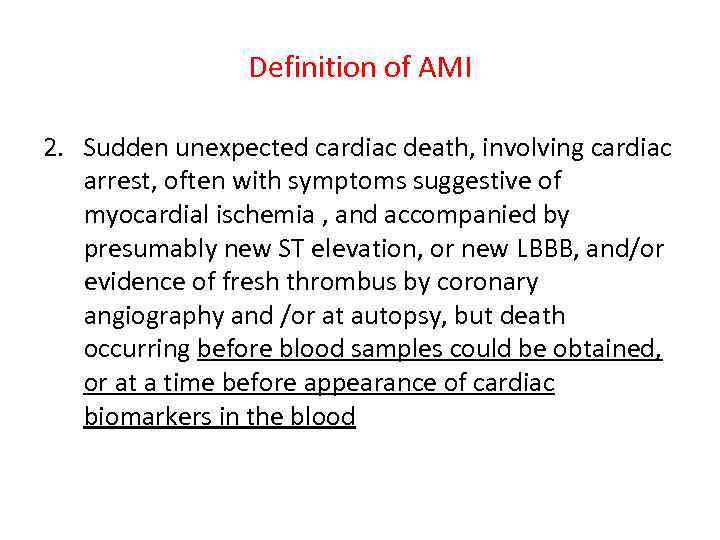
Definition of AMI 2. Sudden unexpected cardiac death, involving cardiac arrest, often with symptoms suggestive of myocardial ischemia , and accompanied by presumably new ST elevation, or new LBBB, and/or evidence of fresh thrombus by coronary angiography and /or at autopsy, but death occurring before blood samples could be obtained, or at a time before appearance of cardiac biomarkers in the blood
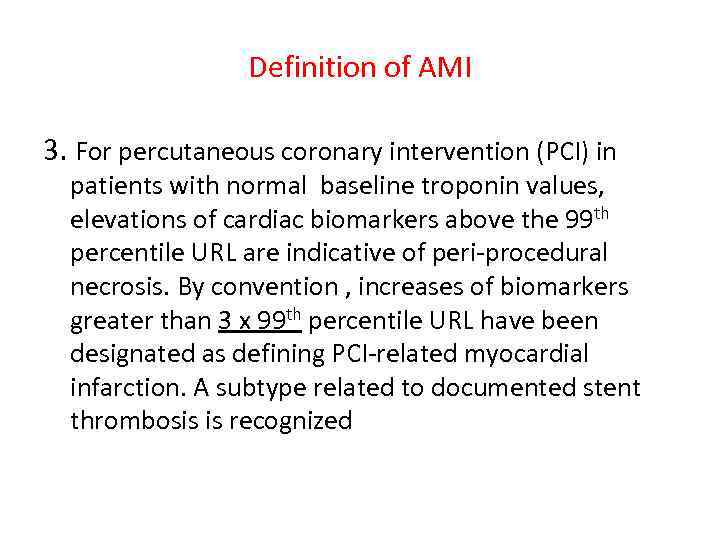
Definition of AMI 3. For percutaneous coronary intervention (PCI) in patients with normal baseline troponin values, elevations of cardiac biomarkers above the 99 th percentile URL are indicative of peri-procedural necrosis. By convention , increases of biomarkers greater than 3 x 99 th percentile URL have been designated as defining PCI-related myocardial infarction. A subtype related to documented stent thrombosis is recognized
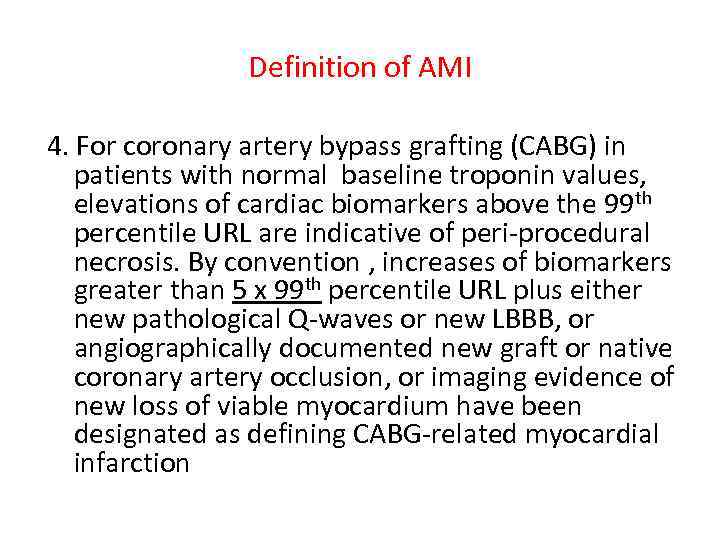
Definition of AMI 4. For coronary artery bypass grafting (CABG) in patients with normal baseline troponin values, elevations of cardiac biomarkers above the 99 th percentile URL are indicative of peri-procedural necrosis. By convention , increases of biomarkers greater than 5 x 99 th percentile URL plus either new pathological Q-waves or new LBBB, or angiographically documented new graft or native coronary artery occlusion, or imaging evidence of new loss of viable myocardium have been designated as defining CABG-related myocardial infarction
Definition of AMI 5. Pathological findings of an acute myocardial infarction
Pathological diagnosis • Evidence of myocardial cell death as a consequence of prolonged ischemia • Characteristic findings: coagulation necrosis, contraction band necrosis, patchy areas of myocytolysis at the periphery of the infarct • During acute phase of MI majority of myocyte loss - via coagulation necrosis, inflammation, phagocytosis of necrotic myocytes and repair by scar formation
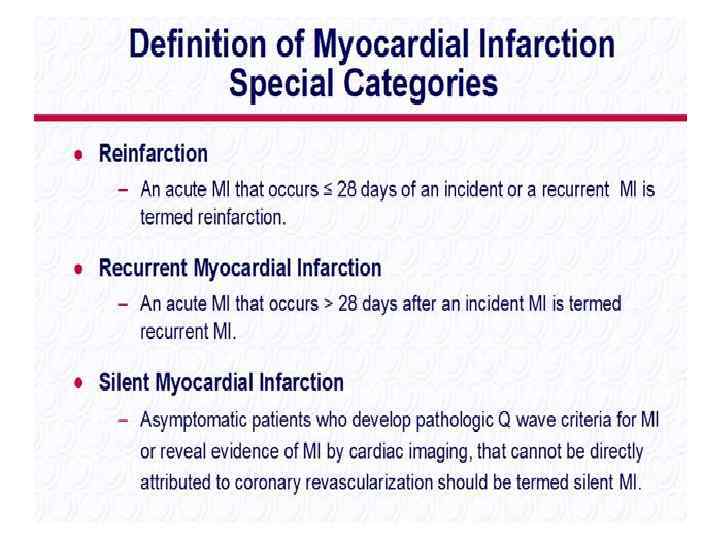
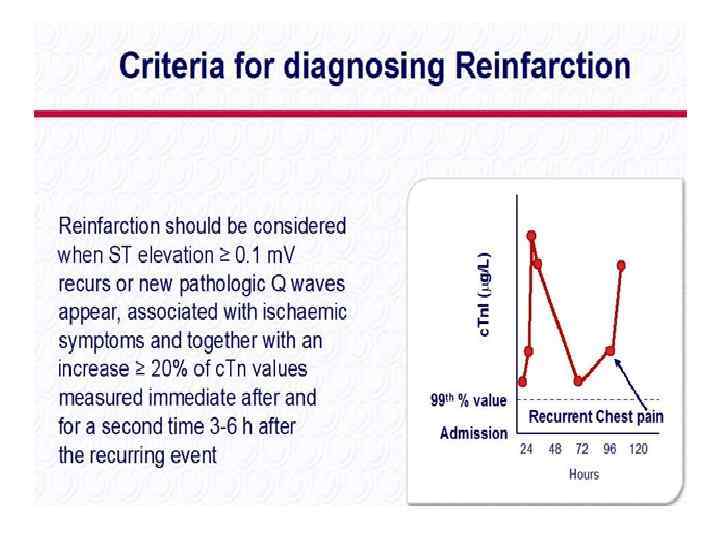
Definition of AMI Criteria for prior myocardial infarction Any of the following criteria meets the diagnosis for prior myocardial infarction: - development of new pathological Q waves with or without symptoms - imaging evidence of a region of loss of viable myocardium that is thinned and fails to contract , in the absence of a nonischemic cause - Pathological signs of healed or healing myocardial infarction
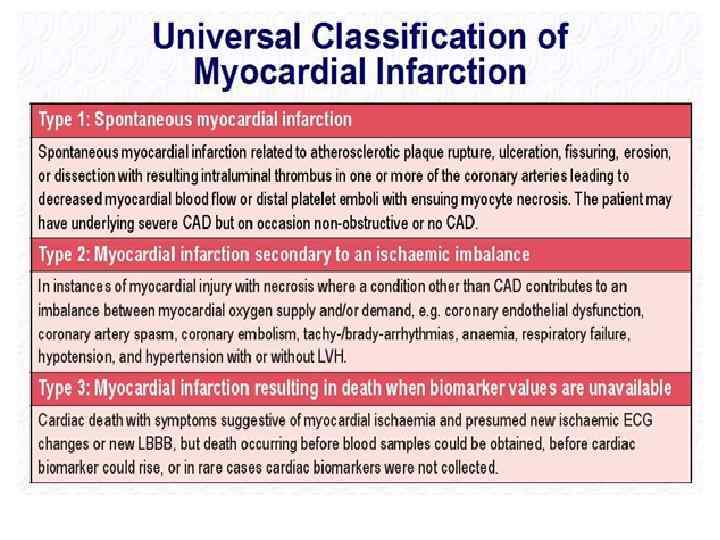
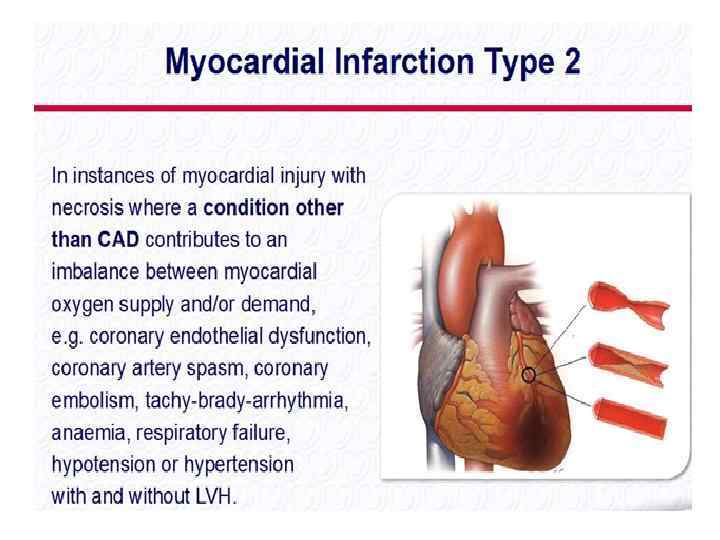
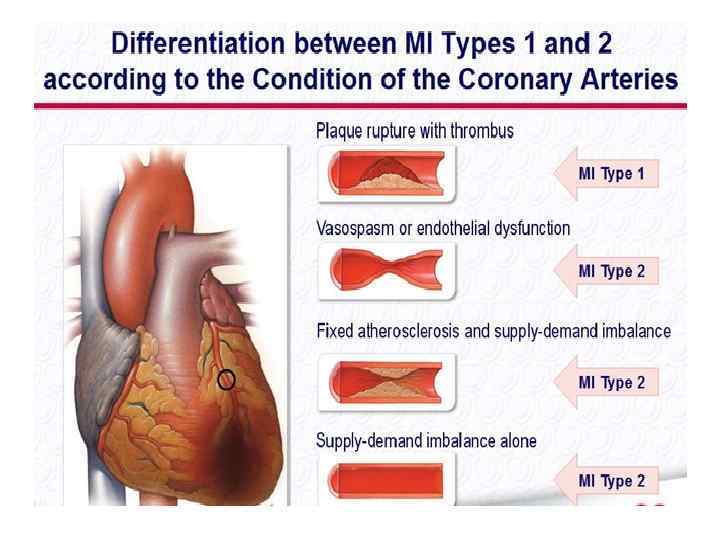
Clinical classification of different types of myocardial infarction Type 1 Spontaneous myocardial infarction related to ischemia due to a primary coronary event such as plaque erosion and /or rupture, fissuring or dissection Type 2 Myocardial infarction secondary to ischemia due to either increased oxygen demand or decreased supply, e. g. coronary artery spasm, coronary embolism, anemia, arrythmias, hypertension or hypotension
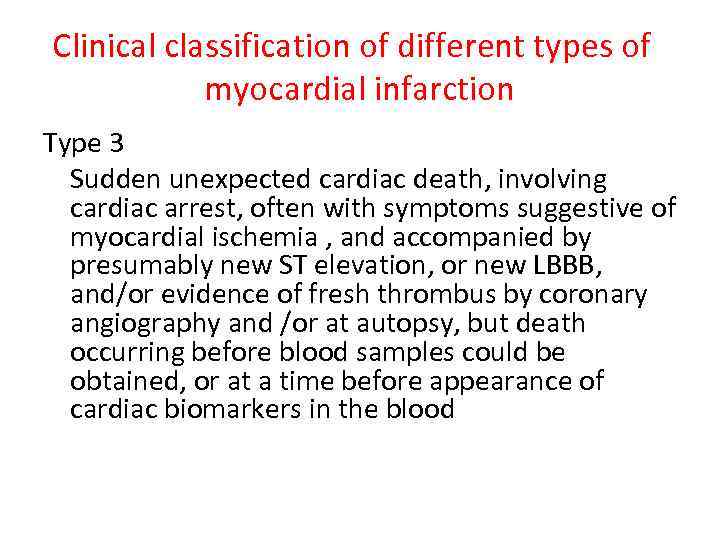
Clinical classification of different types of myocardial infarction Type 3 Sudden unexpected cardiac death, involving cardiac arrest, often with symptoms suggestive of myocardial ischemia , and accompanied by presumably new ST elevation, or new LBBB, and/or evidence of fresh thrombus by coronary angiography and /or at autopsy, but death occurring before blood samples could be obtained, or at a time before appearance of cardiac biomarkers in the blood
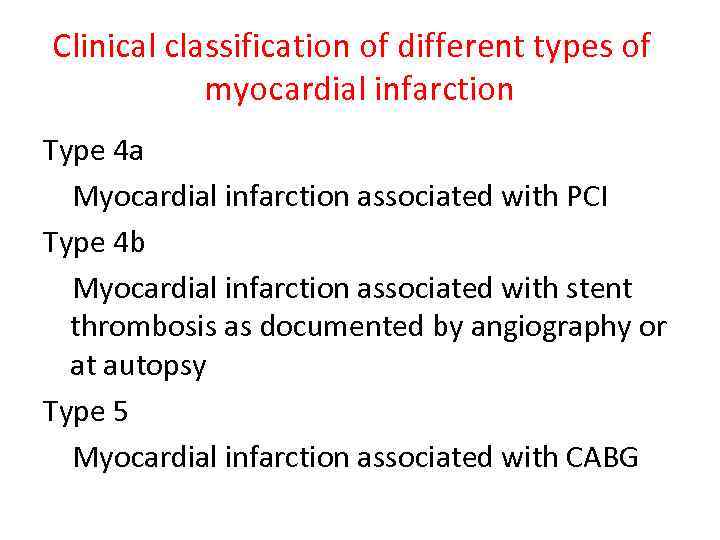
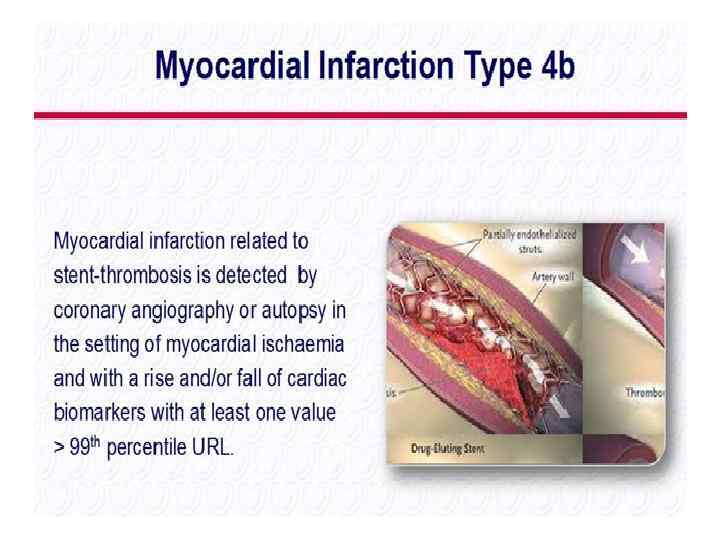
Clinical classification of different types of myocardial infarction Type 4 a Myocardial infarction associated with PCI Type 4 b Myocardial infarction associated with stent thrombosis as documented by angiography or at autopsy Type 5 Myocardial infarction associated with CABG










ESC guidelines on STEMI - 2012
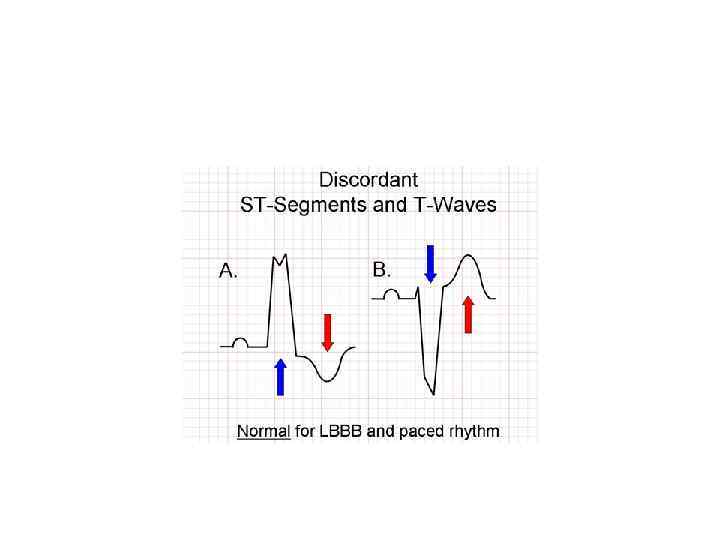

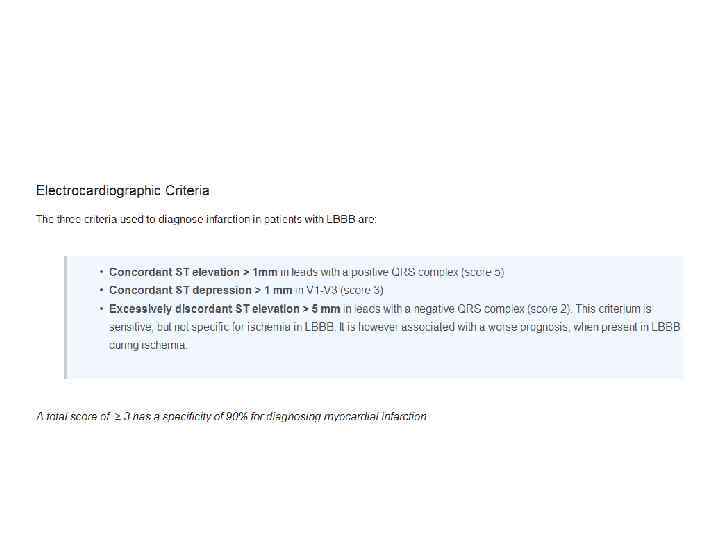
• 7 experienced interventional cardiologists were asked to decide, based on ECG, if they would activate primary PCI protocol • 84 consecutive pts with ECG showing STE (LBBB and ventricular rhythm excluded): 40 pts with STEMI and 44 pts with NISTE • Recommendation to activate Pr. PCI protocol varied from 33% to 75% (!) Am J Cardiol 2011; 108: 1096 -1101
ST-Segment elevation in conditions other than acute myocardial infarction Wang et al. NEJM 2003, 349: 2128 -35
Acute MI - 9.2017.pptx