1_Auskult_cor_eng.ppt
- Количество слайдов: 43
 Cardiac auscultation. Changes of the heard sounds at norm and pathology. Cardiac murmurs
Cardiac auscultation. Changes of the heard sounds at norm and pathology. Cardiac murmurs
 The purpose of cardiac auscultation To identify the presence and characteristics of normal and abnormal heart sounds.
The purpose of cardiac auscultation To identify the presence and characteristics of normal and abnormal heart sounds.
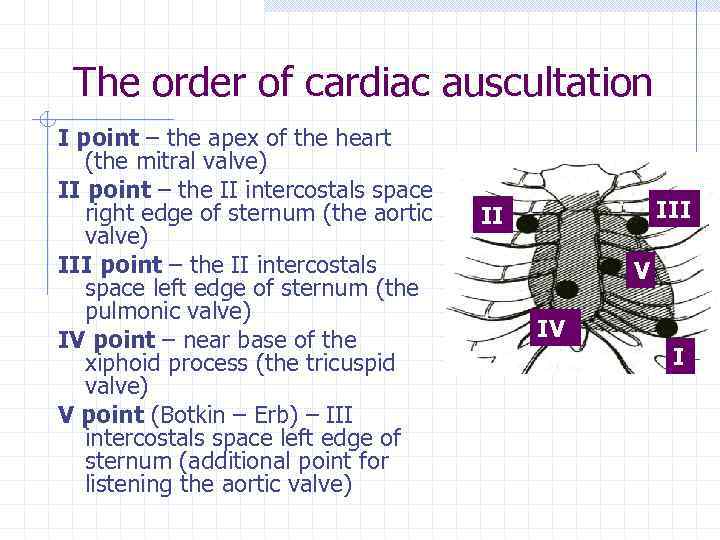 The order of cardiac auscultation І point – the apex of the heart (the mitral valve) ІІ point – the ІІ intercostals space right edge of sternum (the aortic valve) ІІІ point – the ІІ intercostals space left edge of sternum (the pulmonic valve) ІV point – near base of the xiphoid process (the tricuspid valve) V point (Botkin – Erb) – ІІІ intercostals space left edge of sternum (additional point for listening the aortic valve) III II V IV I
The order of cardiac auscultation І point – the apex of the heart (the mitral valve) ІІ point – the ІІ intercostals space right edge of sternum (the aortic valve) ІІІ point – the ІІ intercostals space left edge of sternum (the pulmonic valve) ІV point – near base of the xiphoid process (the tricuspid valve) V point (Botkin – Erb) – ІІІ intercostals space left edge of sternum (additional point for listening the aortic valve) III II V IV I
 Components of the first sound (S 1) 1. Valvate (vibration of atrial-ventricular valve during isometric contraction of the ventricles) 2. Muscular (vibration of the ventricular myocardium during isometric contraction) 3. Vascular (vibration of proximal parts of aorta and pulmonary artery during straining them with blood) 4. Atrial (vibration during contraction of the atria)
Components of the first sound (S 1) 1. Valvate (vibration of atrial-ventricular valve during isometric contraction of the ventricles) 2. Muscular (vibration of the ventricular myocardium during isometric contraction) 3. Vascular (vibration of proximal parts of aorta and pulmonary artery during straining them with blood) 4. Atrial (vibration during contraction of the atria)
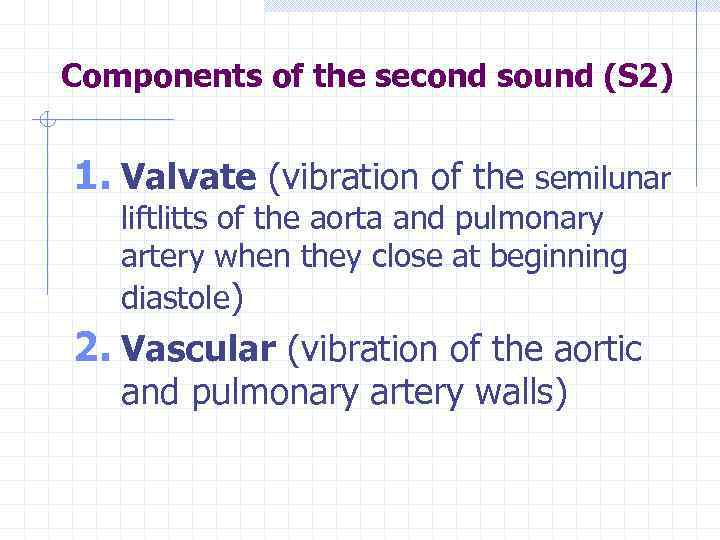 Components of the second sound (S 2) 1. Valvate (vibration of the semilunar liftlitts of the aorta and pulmonary artery when they close at beginning diastole) 2. Vascular (vibration of the aortic and pulmonary artery walls)
Components of the second sound (S 2) 1. Valvate (vibration of the semilunar liftlitts of the aorta and pulmonary artery when they close at beginning diastole) 2. Vascular (vibration of the aortic and pulmonary artery walls)
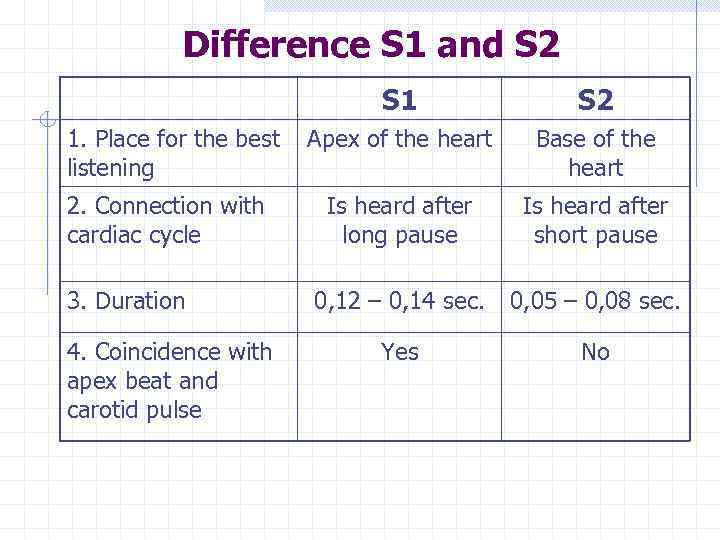 Difference S 1 and S 2 S 1 1. Place for the best listening 2. Connection with cardiac cycle 3. Duration 4. Coincidence with apex beat and carotid pulse S 2 Apex of the heart Base of the heart Is heard after long pause Is heard after short pause 0, 12 – 0, 14 sec. 0, 05 – 0, 08 sec. Yes No
Difference S 1 and S 2 S 1 1. Place for the best listening 2. Connection with cardiac cycle 3. Duration 4. Coincidence with apex beat and carotid pulse S 2 Apex of the heart Base of the heart Is heard after long pause Is heard after short pause 0, 12 – 0, 14 sec. 0, 05 – 0, 08 sec. Yes No
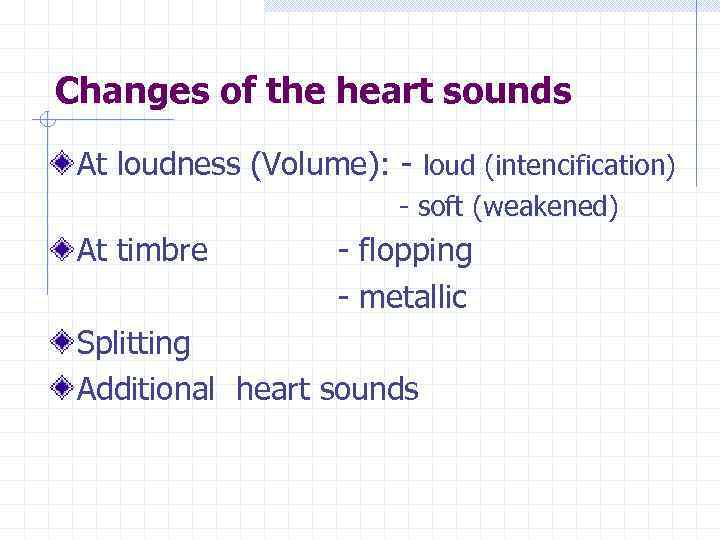 Changes of the heart sounds At loudness (Volume): - loud (intencification) - soft (weakened) At timbre - flopping - metallic Splitting Additional heart sounds
Changes of the heart sounds At loudness (Volume): - loud (intencification) - soft (weakened) At timbre - flopping - metallic Splitting Additional heart sounds
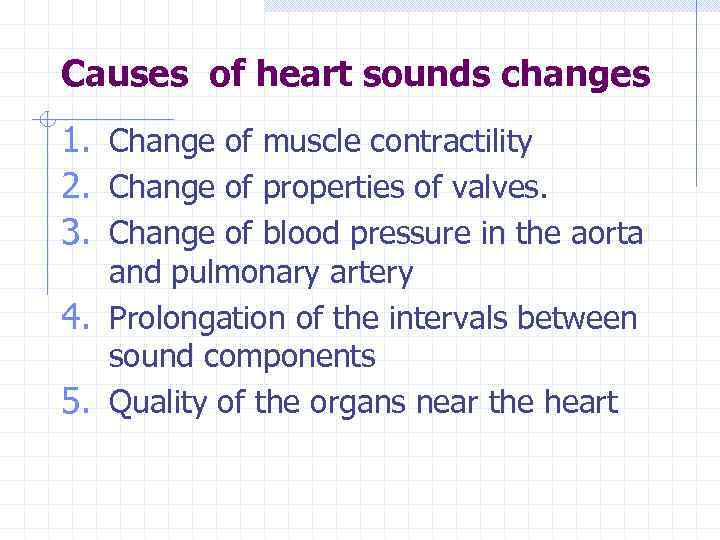 Causes of heart sounds changes 1. Change of muscle contractility 2. Change of properties of valves. 3. Change of blood pressure in the aorta and pulmonary artery 4. Prolongation of the intervals between sound components 5. Quality of the organs near the heart
Causes of heart sounds changes 1. Change of muscle contractility 2. Change of properties of valves. 3. Change of blood pressure in the aorta and pulmonary artery 4. Prolongation of the intervals between sound components 5. Quality of the organs near the heart
 Exrtacardiac causes of diminishing S 1 and S 2: • Thick chest • Edema of the chest • Subcutaneous emphysema near the heart • Lung emphysema • Pleural effusion in the left pleural cavity Cardiac causes of diminishing S 1 and S 2 : • Myocarditis • Myocardial infarction Diminishing contractility • Cardiosclerosis of the cardiac muscle • Cardiomyopathy • Hydropericardium Other causes: massive bleeding, shock, collapse causes
Exrtacardiac causes of diminishing S 1 and S 2: • Thick chest • Edema of the chest • Subcutaneous emphysema near the heart • Lung emphysema • Pleural effusion in the left pleural cavity Cardiac causes of diminishing S 1 and S 2 : • Myocarditis • Myocardial infarction Diminishing contractility • Cardiosclerosis of the cardiac muscle • Cardiomyopathy • Hydropericardium Other causes: massive bleeding, shock, collapse causes
 Exrtacardiac causes of intensification S 1 and S 2 Thin chest Srinkage of the lung edges Consolidation of the lung edges Tumor in the posterior mediastinum High position of the diaphragm Frontal trunk bending Large pulmonary cavity Cardiac causes of intensification S 1 and S 2 Physical exercise Thyrotoxicosis Excitable type of nervous system
Exrtacardiac causes of intensification S 1 and S 2 Thin chest Srinkage of the lung edges Consolidation of the lung edges Tumor in the posterior mediastinum High position of the diaphragm Frontal trunk bending Large pulmonary cavity Cardiac causes of intensification S 1 and S 2 Physical exercise Thyrotoxicosis Excitable type of nervous system
 Causes of diminishing S 1 Mitral regurgitation Aortic regurgitation Tricuspid regurgitation Pulmonary regurgitation Aortic stenosis
Causes of diminishing S 1 Mitral regurgitation Aortic regurgitation Tricuspid regurgitation Pulmonary regurgitation Aortic stenosis
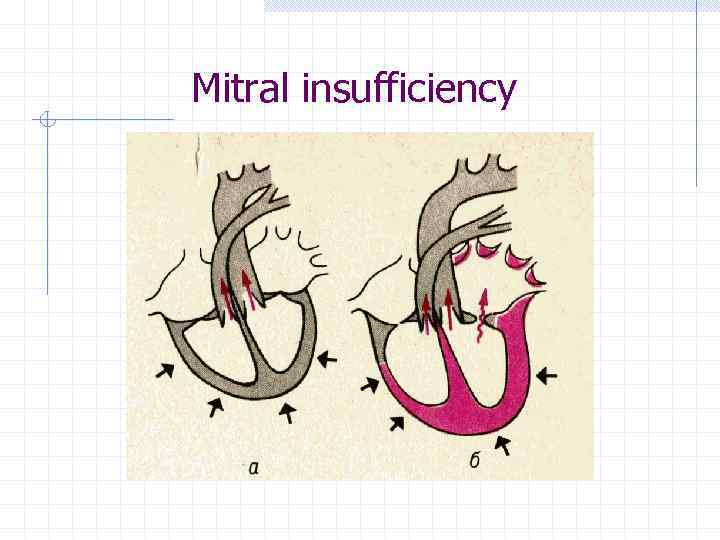 Mitral insufficiency
Mitral insufficiency
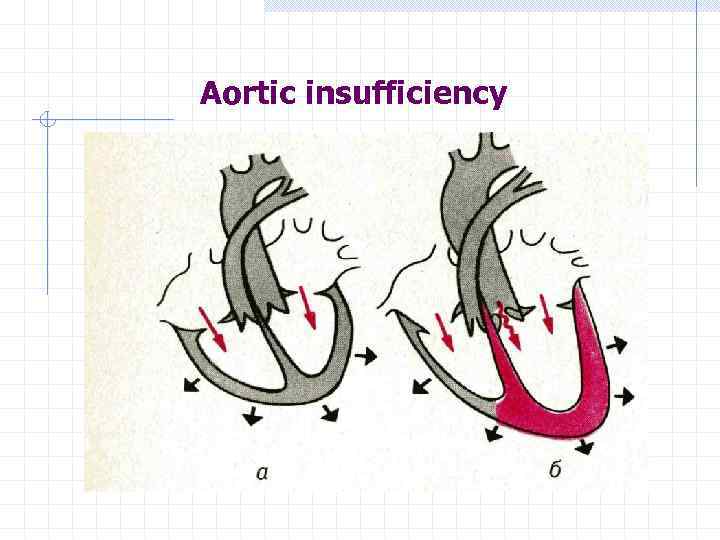 Aortic insufficiency
Aortic insufficiency
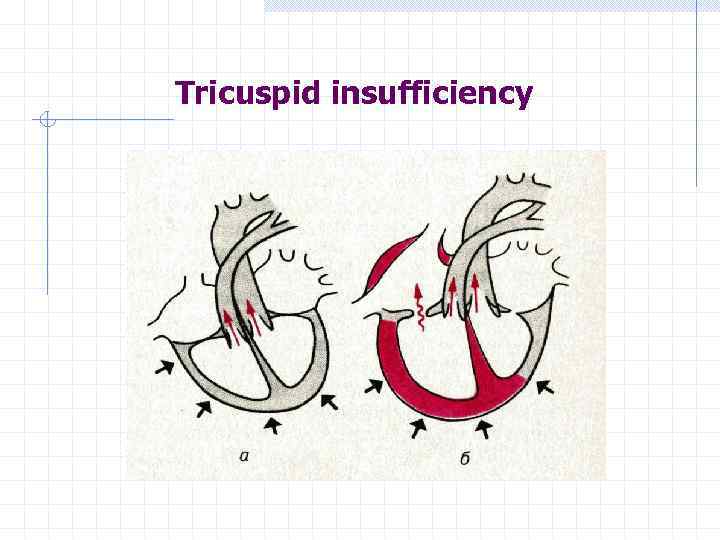 Tricuspid insufficiency
Tricuspid insufficiency
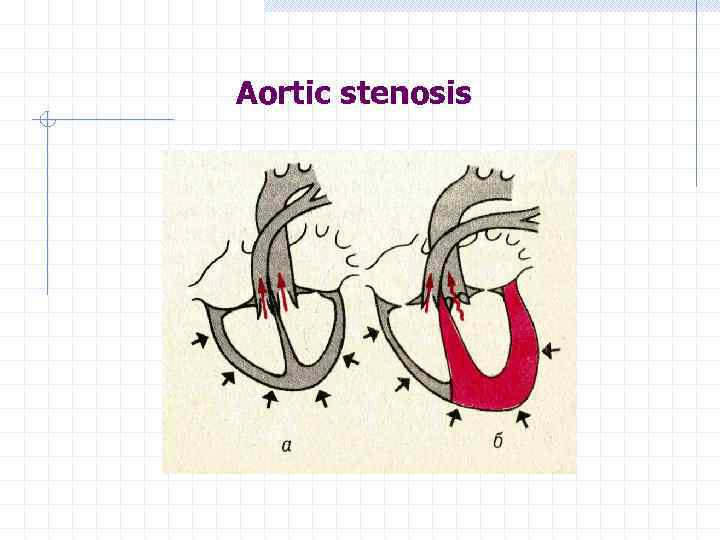 Aortic stenosis
Aortic stenosis
 Causes of intensification of S 1 Mitral stenosis Early ventricular extrasystoles Complete atrial-ventricular block Atrial fibrillation Tachycardia
Causes of intensification of S 1 Mitral stenosis Early ventricular extrasystoles Complete atrial-ventricular block Atrial fibrillation Tachycardia
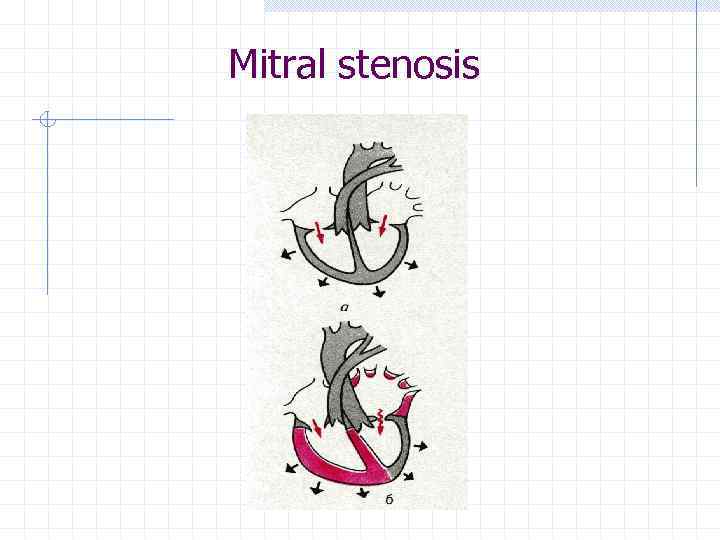 Mitral stenosis
Mitral stenosis
 Causes of diminishing S 2 Over aorta: - aortic regurgitation - aortic stenosis Over pulmonary artery: - pulmonary regurgitation - pulmonic stenosis
Causes of diminishing S 2 Over aorta: - aortic regurgitation - aortic stenosis Over pulmonary artery: - pulmonary regurgitation - pulmonic stenosis
 Causes of intensification of S 2 over aorta Arterial hypertension - essential hypertension, - symptomatic arterial hypertension
Causes of intensification of S 2 over aorta Arterial hypertension - essential hypertension, - symptomatic arterial hypertension
 Causes of intensification of S 2 over pulmonary artery Mitral insufficiency Mitral stenosis pulmonary hypertension primary or secondary (pulmonary embolism, COPD, bronchial asthma and other)
Causes of intensification of S 2 over pulmonary artery Mitral insufficiency Mitral stenosis pulmonary hypertension primary or secondary (pulmonary embolism, COPD, bronchial asthma and other)
 Changes sounds at timbre flopping – S 1 at mitral stenosis metallic – S 2 at aortic stenosis
Changes sounds at timbre flopping – S 1 at mitral stenosis metallic – S 2 at aortic stenosis
 Splitting of heart sounds is phenomenon when two short distinct components is heard instead of one sound. Splitting of heart sounds is stipulated for asynchronous appearance of separate components of heart sounds in the right and left part of the heart: ü non simultaneous closure of the atrialventricular valves causes split S 1, ü non simultaneous closure of the semilunar valves causes split S 2
Splitting of heart sounds is phenomenon when two short distinct components is heard instead of one sound. Splitting of heart sounds is stipulated for asynchronous appearance of separate components of heart sounds in the right and left part of the heart: ü non simultaneous closure of the atrialventricular valves causes split S 1, ü non simultaneous closure of the semilunar valves causes split S 2
 Pathological splitting S 1 occurs when patient has bundle branch block that causes non synchronically right and left ventricles contracting. Pathological splitting S 2 occurs due to ü pulmonary hypertension when closure of the pulmonary valve is delayed because of slow emptying of the right ventricle as a result of high right ventricular afterload (mitral stenosis, emphysema) ü if closure of aortic valve delays at the patients with arterial hypertension.
Pathological splitting S 1 occurs when patient has bundle branch block that causes non synchronically right and left ventricles contracting. Pathological splitting S 2 occurs due to ü pulmonary hypertension when closure of the pulmonary valve is delayed because of slow emptying of the right ventricle as a result of high right ventricular afterload (mitral stenosis, emphysema) ü if closure of aortic valve delays at the patients with arterial hypertension.
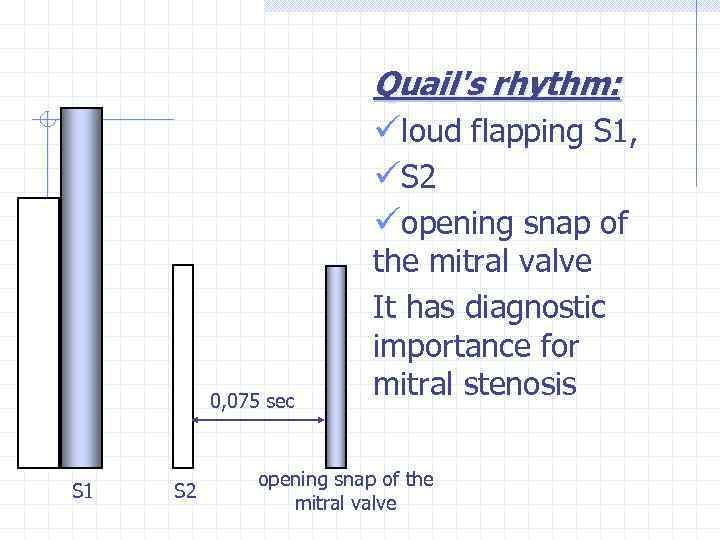 Quail's rhythm: üloud flapping S 1, üS 2 üopening snap of 0, 075 sec S 1 S 2 the mitral valve It has diagnostic importance for mitral stenosis opening snap of the mitral valve
Quail's rhythm: üloud flapping S 1, üS 2 üopening snap of 0, 075 sec S 1 S 2 the mitral valve It has diagnostic importance for mitral stenosis opening snap of the mitral valve
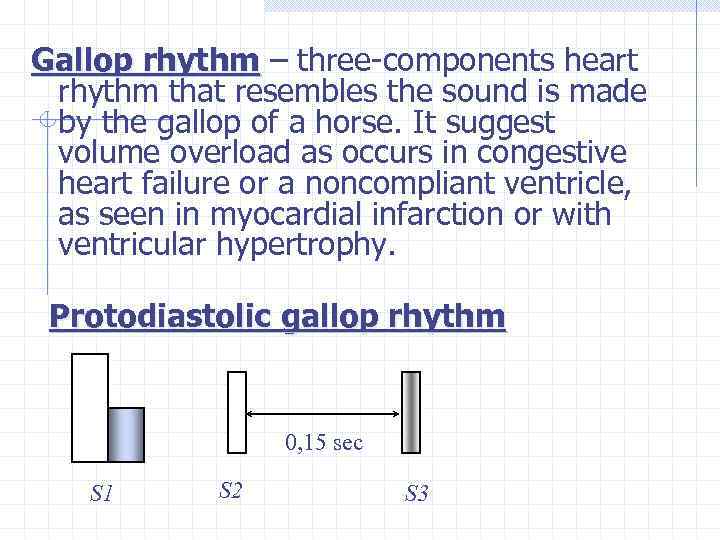 Gallop rhythm – three-components heart rhythm that resembles the sound is made by the gallop of a horse. It suggest volume overload as occurs in congestive heart failure or a noncompliant ventricle, as seen in myocardial infarction or with ventricular hypertrophy. Protodiastolic gallop rhythm 0, 15 sec S 1 S 2 S 3
Gallop rhythm – three-components heart rhythm that resembles the sound is made by the gallop of a horse. It suggest volume overload as occurs in congestive heart failure or a noncompliant ventricle, as seen in myocardial infarction or with ventricular hypertrophy. Protodiastolic gallop rhythm 0, 15 sec S 1 S 2 S 3
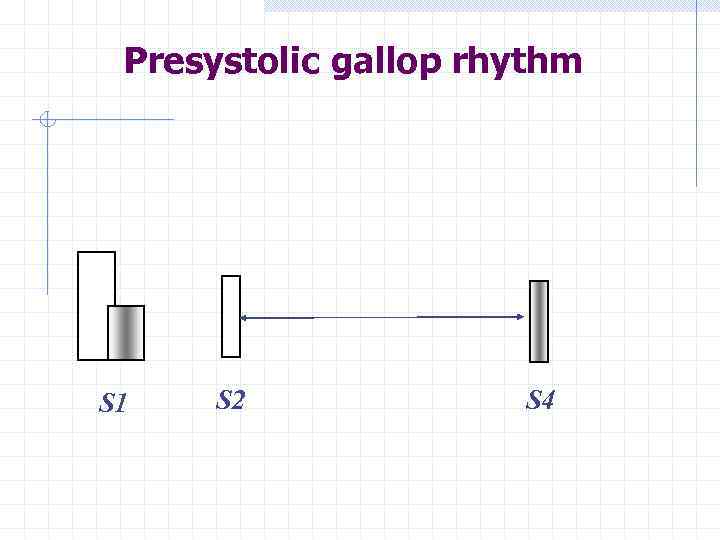 Presystolic gallop rhythm S 1 S 2 S 4
Presystolic gallop rhythm S 1 S 2 S 4
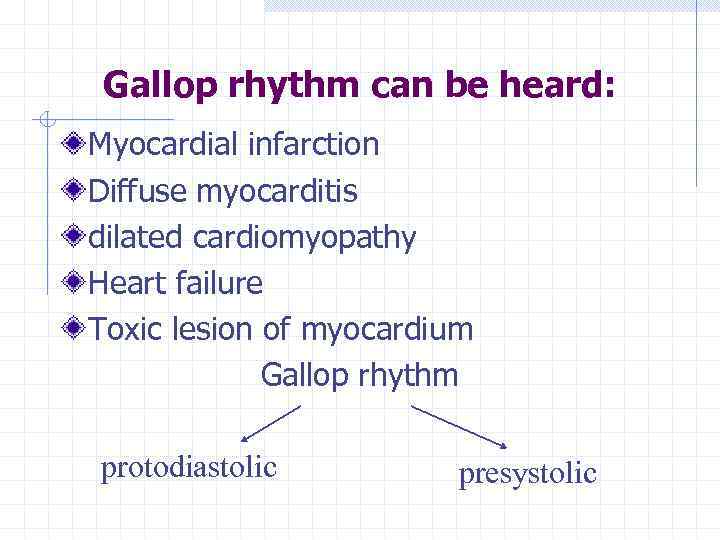 Gallop rhythm can be heard: Myocardial infarction Diffuse myocarditis dilated cardiomyopathy Heart failure Toxic lesion of myocardium Gallop rhythm protodiastolic presystolic
Gallop rhythm can be heard: Myocardial infarction Diffuse myocarditis dilated cardiomyopathy Heart failure Toxic lesion of myocardium Gallop rhythm protodiastolic presystolic
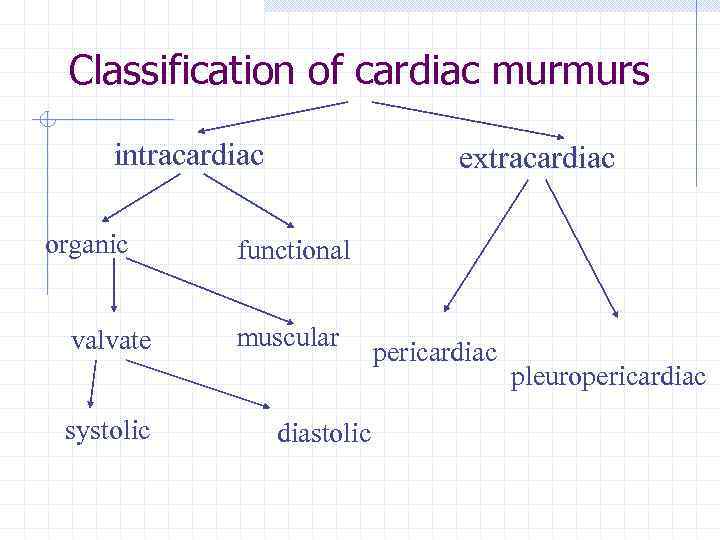 Classification of cardiac murmurs intracardiac organic valvate systolic extracardiac functional muscular diastolic pericardiac pleuropericardiac
Classification of cardiac murmurs intracardiac organic valvate systolic extracardiac functional muscular diastolic pericardiac pleuropericardiac
 Cardiac murmurs is sound phenomena which are heard except heart sounds during cardiac auscultation. Appearance of the intracardiac murmurs can be explained with physical rules of liquid flow through elastic tubes The factors which have importance for appearance of the murmur are: 1. Change of tube lumen – narrowing or widening 2. Change of flow speed 3. Change of properties and contains of liquid The main mechanism of the murmur appearance is turbulent flow of the bloodstream
Cardiac murmurs is sound phenomena which are heard except heart sounds during cardiac auscultation. Appearance of the intracardiac murmurs can be explained with physical rules of liquid flow through elastic tubes The factors which have importance for appearance of the murmur are: 1. Change of tube lumen – narrowing or widening 2. Change of flow speed 3. Change of properties and contains of liquid The main mechanism of the murmur appearance is turbulent flow of the bloodstream
 Systolic murmur 1. It is heard during short pause between S 1 and S 2 2. It coincides with the apex impulse and the carotid pulse 3. Appears in case when during systole blood is going from the ventricle to the atrium (regurgitation murmur) or from the ventricle to the large vessel, meeting the narrow spot on its way
Systolic murmur 1. It is heard during short pause between S 1 and S 2 2. It coincides with the apex impulse and the carotid pulse 3. Appears in case when during systole blood is going from the ventricle to the atrium (regurgitation murmur) or from the ventricle to the large vessel, meeting the narrow spot on its way
 Systolic murmur is heard at the acquired valve diseases: Mitral regurgitation Tricuspid regurgitation Aortic stenosis Pulmonic stenosis
Systolic murmur is heard at the acquired valve diseases: Mitral regurgitation Tricuspid regurgitation Aortic stenosis Pulmonic stenosis
 Diastolic murmur is heard during long pause between S 1 and S 2. There are 4 variants of the diastolic murmur 1. Protodiastolic – after S 2, at the beginning of the diastole 2. Mesodiastolic – at the middle of the diastole 3. Presystolic – at the end of the diastole, before S 1 4. Pandiastolic – continuing all diastole
Diastolic murmur is heard during long pause between S 1 and S 2. There are 4 variants of the diastolic murmur 1. Protodiastolic – after S 2, at the beginning of the diastole 2. Mesodiastolic – at the middle of the diastole 3. Presystolic – at the end of the diastole, before S 1 4. Pandiastolic – continuing all diastole
 Diastolic murmur is heard at the acquired valve diseases: Mitral stenosis Tricuspid stenosis Aortic regurgitation Pulmonic regurgitation
Diastolic murmur is heard at the acquired valve diseases: Mitral stenosis Tricuspid stenosis Aortic regurgitation Pulmonic regurgitation
 There are many cardiac and extracardiac factors influencing on loudness and intensity of the murmurs: murmurs 1. Degree of narrowing or extension of the orifice 2. Bloodstream speed 3. Condition of tissue and vessels around the heart (atherosclerosis, vessel elastics, condition of the lung tissue – emphysema decreases loudness of the murmur and consolidation increases loudness)
There are many cardiac and extracardiac factors influencing on loudness and intensity of the murmurs: murmurs 1. Degree of narrowing or extension of the orifice 2. Bloodstream speed 3. Condition of tissue and vessels around the heart (atherosclerosis, vessel elastics, condition of the lung tissue – emphysema decreases loudness of the murmur and consolidation increases loudness)
 Character of murmur can be: Soft Rough (aortic stenosis) Blowing (mitral regurgitation) Whistling Timing – short and long murmurs
Character of murmur can be: Soft Rough (aortic stenosis) Blowing (mitral regurgitation) Whistling Timing – short and long murmurs
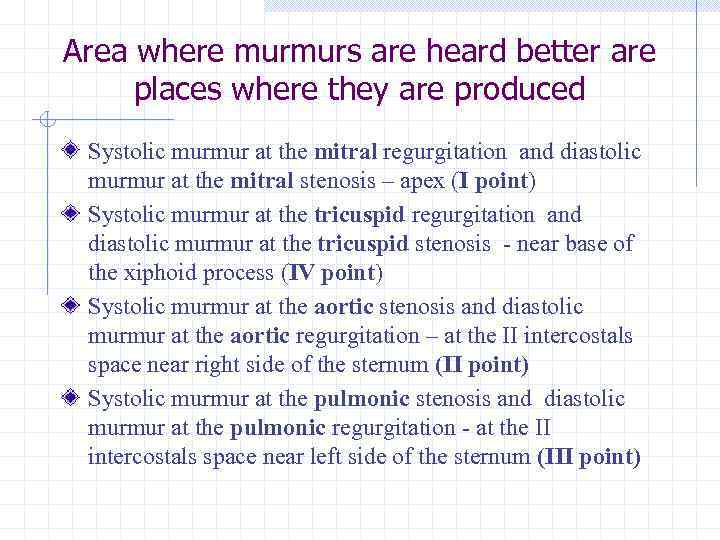 Area where murmurs are heard better are places where they are produced Systolic murmur at the mitral regurgitation and diastolic murmur at the mitral stenosis – apex (І point) Systolic murmur at the tricuspid regurgitation and diastolic murmur at the tricuspid stenosis - near base of the xiphoid process (IV point) Systolic murmur at the aortic stenosis and diastolic murmur at the aortic regurgitation – at the II intercostals space near right side of the sternum (ІІ point) Systolic murmur at the pulmonic stenosis and diastolic murmur at the pulmonic regurgitation - at the II intercostals space near left side of the sternum (ІІI point)
Area where murmurs are heard better are places where they are produced Systolic murmur at the mitral regurgitation and diastolic murmur at the mitral stenosis – apex (І point) Systolic murmur at the tricuspid regurgitation and diastolic murmur at the tricuspid stenosis - near base of the xiphoid process (IV point) Systolic murmur at the aortic stenosis and diastolic murmur at the aortic regurgitation – at the II intercostals space near right side of the sternum (ІІ point) Systolic murmur at the pulmonic stenosis and diastolic murmur at the pulmonic regurgitation - at the II intercostals space near left side of the sternum (ІІI point)
 Radiation of murmur (causes) 1. To the bloodflow (mitral regurgitation – from apex to the II-III intercostals space near left side of the sternum) 2. Through the hypertrophic myocardium (mitral regurgitation – from apex to the axilla) 3. To both sides (front and back) of narrowing (aortic stenosis – from ІІ intercostals space to the apex and carotids)
Radiation of murmur (causes) 1. To the bloodflow (mitral regurgitation – from apex to the II-III intercostals space near left side of the sternum) 2. Through the hypertrophic myocardium (mitral regurgitation – from apex to the axilla) 3. To both sides (front and back) of narrowing (aortic stenosis – from ІІ intercostals space to the apex and carotids)
 Position of the patient for the best listening murmurs Systolic murmurs – horizontal position Diastolic murmurs – vertical position According to intensity murmurs can be: Decrescendo quality Crescendo quality Only presystolic murmur at the mitral stenosis is crescendo, others are decrescendo
Position of the patient for the best listening murmurs Systolic murmurs – horizontal position Diastolic murmurs – vertical position According to intensity murmurs can be: Decrescendo quality Crescendo quality Only presystolic murmur at the mitral stenosis is crescendo, others are decrescendo
 Functional murmur Cardiac murmurs, but it is not connected with valvate lesion Causes of functional murmurs Decreasing blood viscosity Rapid bloodflow
Functional murmur Cardiac murmurs, but it is not connected with valvate lesion Causes of functional murmurs Decreasing blood viscosity Rapid bloodflow
 Properties of functional murmurs 1. Most of all - systolic 2. The best listening over a. pulmonalis, 3. 4. 5. 6. 7. apex Not radiation (!!!) Can change after physical exercise, body position, phase of breathing (not constant) Don’t have other signs of valve heart disease isn’t associated with a thrill Timing- short, character - soft
Properties of functional murmurs 1. Most of all - systolic 2. The best listening over a. pulmonalis, 3. 4. 5. 6. 7. apex Not radiation (!!!) Can change after physical exercise, body position, phase of breathing (not constant) Don’t have other signs of valve heart disease isn’t associated with a thrill Timing- short, character - soft
 Extracardiac murmurs: pleuropericardial friction rub and pericardial friction rub Pericardial friction rub may be heard when the pericardial sac becomes inflamed. The surface of pericardium becomes shaggy due to fibrin over its. Pericardial friction rub is heard: 1. Dry pericarditis 2. At the beginning or at the end of exudative pericarditis 3. Uremia 4. Myocardial infarction (Dressler syndrome) 5. Polyserositis (autoimmunity diseases)
Extracardiac murmurs: pleuropericardial friction rub and pericardial friction rub Pericardial friction rub may be heard when the pericardial sac becomes inflamed. The surface of pericardium becomes shaggy due to fibrin over its. Pericardial friction rub is heard: 1. Dry pericarditis 2. At the beginning or at the end of exudative pericarditis 3. Uremia 4. Myocardial infarction (Dressler syndrome) 5. Polyserositis (autoimmunity diseases)
 Signs of pericardial friction rub Is heard during systole and diastole Character – may be soft or rough, like snow crunches The best place for listening – area of absolute dullness of heart Not radiation Increases if patient band front or if the funeral of the stethoscope is pressed to the chest
Signs of pericardial friction rub Is heard during systole and diastole Character – may be soft or rough, like snow crunches The best place for listening – area of absolute dullness of heart Not radiation Increases if patient band front or if the funeral of the stethoscope is pressed to the chest
 Pleuropericardial friction rub may be heard when the pleura near the heart is inflamed. Signs of the pleuropericardial friction rub: Associated with breathing Increases during deep inspiration The best place for listening is the left edge of the relative cardiac dullness
Pleuropericardial friction rub may be heard when the pleura near the heart is inflamed. Signs of the pleuropericardial friction rub: Associated with breathing Increases during deep inspiration The best place for listening is the left edge of the relative cardiac dullness


