02f64e711c090dd83632f0b7bdb8c955.ppt
- Количество слайдов: 79
CARDIAC ARREST AND RESUSCITATION SCIENCE; USING GLOBAL KNOWLEDGE & EXPERIENCE TO STRENGTHEN OUR PRACTICE DR. SOLOMON WAI-CHU WAI Training Coordinator COLLEGE OF EMERGENCY AND PARAMEDIC STUDIES, PORT HARCOURT
OUTLINE INTRODUCTION: What is Cardiac Arrest? EPIDEMIOLOGY and CHAIN OF SURVIVAL: Incidence in Nigeria and Globally CARDIAC ARREST AS A DISEASE: the three-phasemodel of Cardiac Arrest WHAT IS THE DEVELOPED WORLD DOING? Current trends in Management WHICH WAY NIGERIA? How do we improve outcome in Nigeria? THE FUTURE: New Treatments of Cardiac Arrest CONCLUSION: What is Death? When do we pronounce a patient dead?
“The saddest aspect of life right now is that science gathers knowledge faster than society gathers wisdom” ~Isaac Asimov
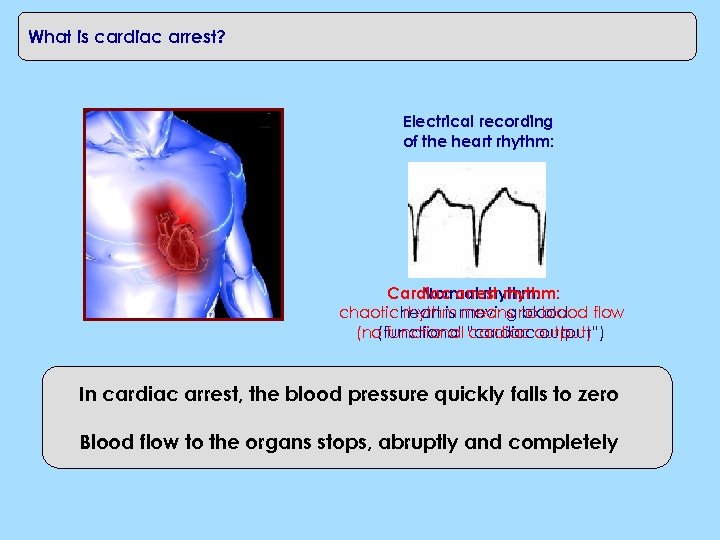
What is cardiac arrest? Electrical recording of the heart rhythm: Cardiac arrest rhythm: Normal rhythm: chaotic heart is moving no blood flow rhythm means blood (no functional “cardiacoutput) (functional cardiac output”) In cardiac arrest, the blood pressure quickly falls to zero Blood flow to the organs stops, abruptly and completely
EPIDEMIOLOGY: Cardiac arrest is a massive public health problem Cardiac arrest is a leading cause of death in the developed world Ø No cohesive data in Nigeria Ø Over 300, 000 people in the U. S. suffer OH cardiac plus over 200, 000 IHCA each year Ø 95 persons per 100, 000 worldwide per annum Ø Most victims die before hospital arrival Ø Less than 10% leave the hospital alive, but… Cardiac arrest commonly strikes people in their 50 s and 60 s – often active, generally healthy people – and strikes with few warning signs or symptoms
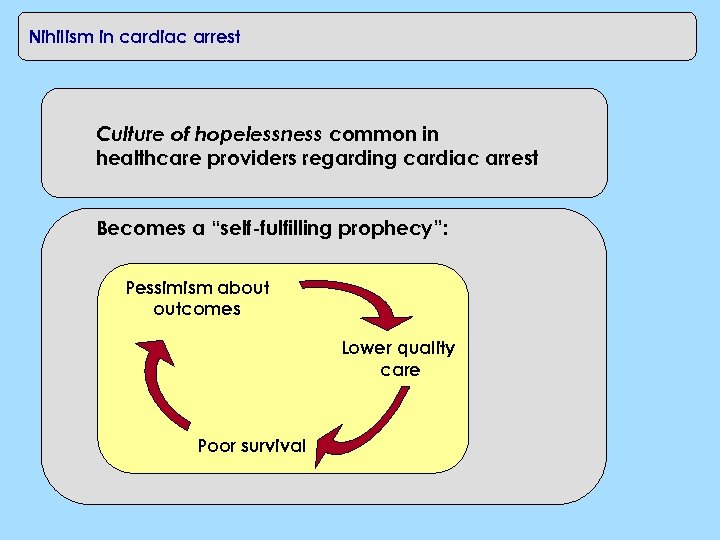
Nihilism in cardiac arrest Culture of hopelessness common in healthcare providers regarding cardiac arrest Becomes a “self-fulfilling prophecy”: Pessimism about outcomes Lower quality care Poor survival
CHAIN OF SURVIVAL: Why is cardiac arrest survival so variable? Cardiac arrest survival depends on the successful performance of the “chain of survival” Not all communities have the same strengths in this chain
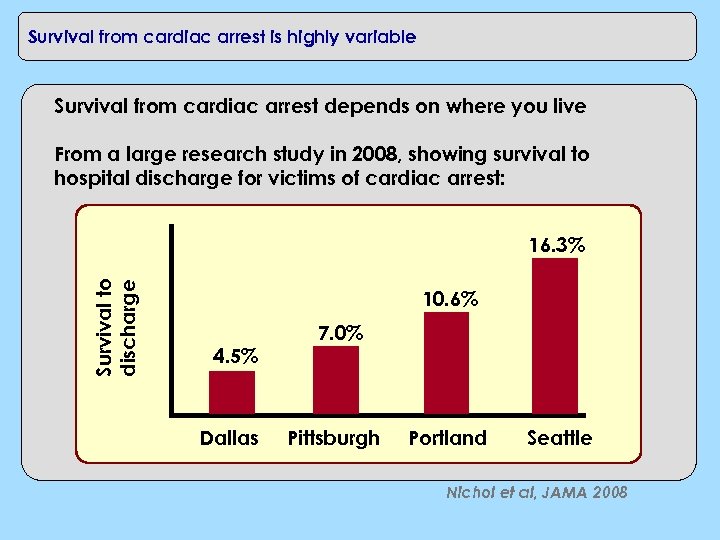
Survival from cardiac arrest is highly variable Survival from cardiac arrest depends on where you live From a large research study in 2008, showing survival to hospital discharge for victims of cardiac arrest: Survival to discharge 16. 3% 10. 6% 4. 5% Dallas 7. 0% Pittsburgh Portland Seattle Nichol et al, JAMA 2008
Survival variability is from multiple factors Public knowledge about CPR, willingness to perform CPR varies from community to community Availability of automated external defibrillators (AEDs) differs widely as well Quality of Emergency Medical Services (EMS) response widely variable
Example: variable public knowledge of AEDs A survey study conducted in a major European train station in 2011 queried members of the public about AEDs Findings from laypersons surveyed: • Only 38% could identify an AED • Only 46% could describe purpose of AED • Only 36% knew AEDs could be used by public If someone collapsed from cardiac arrest at your local bus station or airport, would people know to grab an AED and use it? Is one available? Schober et al, Ann Emerg Med 2011
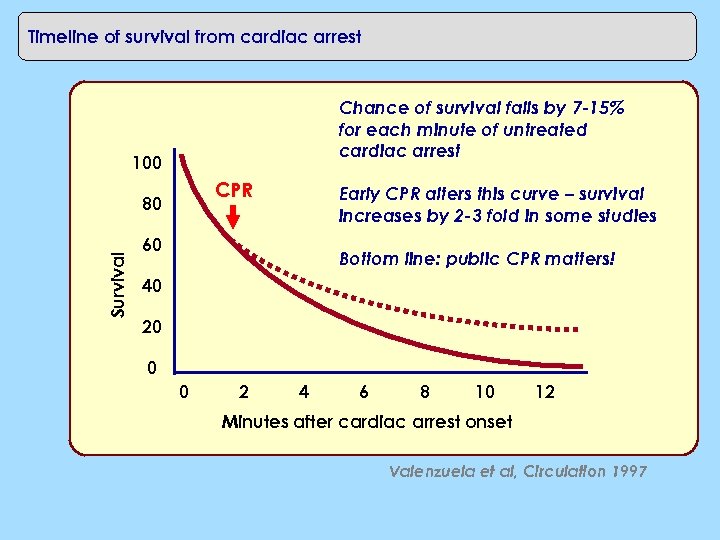
Timeline of survival from cardiac arrest Chance of survival falls by 7 -15% for each minute of untreated cardiac arrest 100 CPR Survival 80 Early CPR alters this curve – survival increases by 2 -3 fold in some studies 60 Bottom line: public CPR matters! 40 20 0 0 2 4 6 8 10 12 Minutes after cardiac arrest onset Valenzuela et al, Circulation 1997
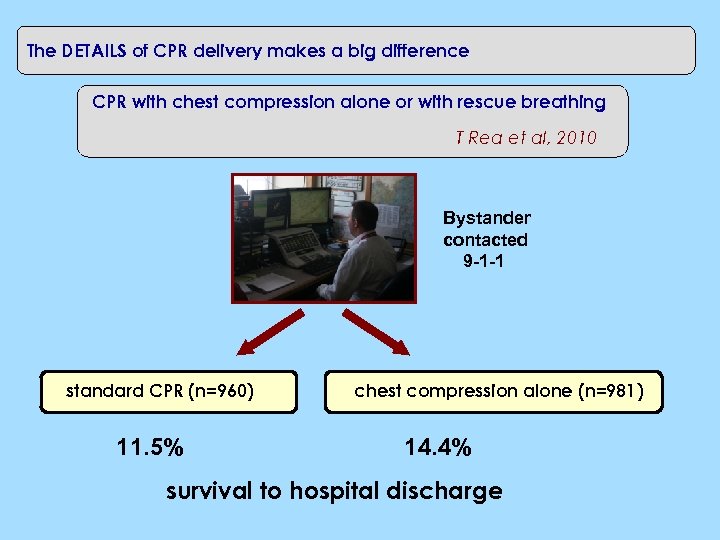
The DETAILS of CPR delivery makes a big difference CPR with chest compression alone or with rescue breathing T Rea et al, 2010 Bystander contacted 9 -1 -1 standard CPR (n=960) 11. 5% chest compression alone (n=981) 14. 4% survival to hospital discharge
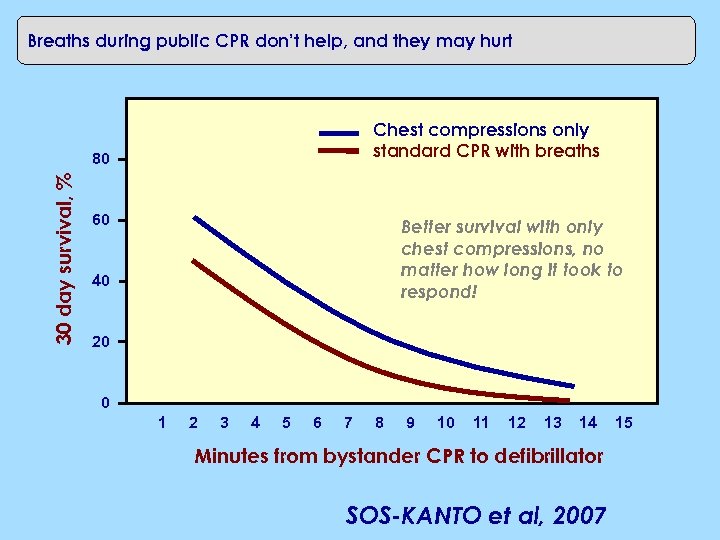
Breaths during public CPR don’t help, and they may hurt Chest compressions only standard CPR with breaths 30 day survival, % 80 60 Better survival with only chest compressions, no matter how long it took to respond! 40 20 0 1 2 3 4 5 6 7 8 9 10 11 12 13 14 Minutes from bystander CPR to defibrillator SOS-KANTO et al, 2007 15
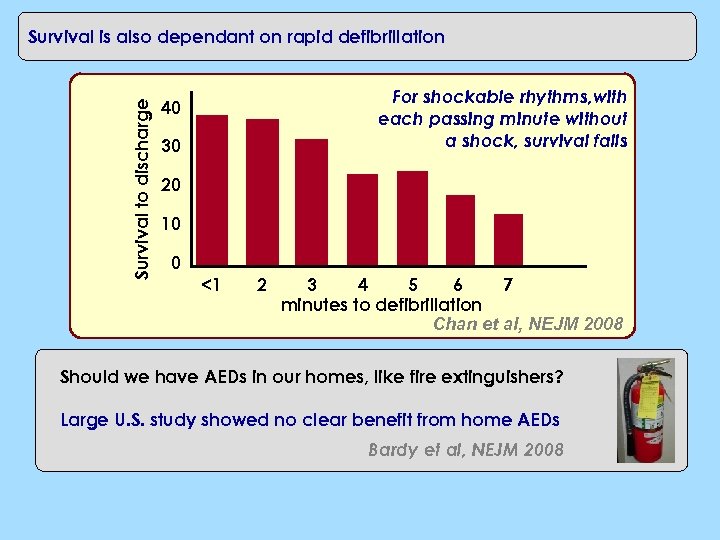
Survival to discharge Survival is also dependant on rapid defibrillation For shockable rhythms, with each passing minute without a shock, survival falls 40 30 20 10 0 <1 2 3 4 5 6 7 minutes to defibrillation Chan et al, NEJM 2008 Should we have AEDs in our homes, like fire extinguishers? Large U. S. study showed no clear benefit from home AEDs Bardy et al, NEJM 2008
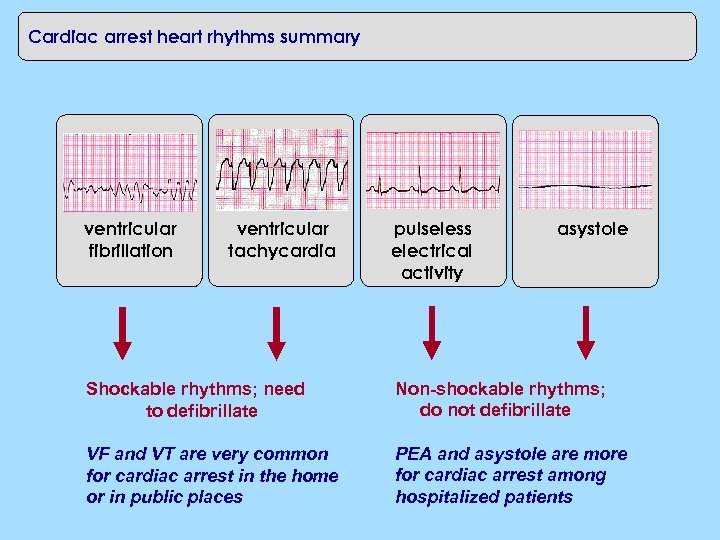
Cardiac arrest heart rhythms summary ventricular fibrillation ventricular tachycardia pulseless electrical activity asystole Shockable rhythms; need to defibrillate Non-shockable rhythms; do not defibrillate VF and VT are very common for cardiac arrest in the home or in public places PEA and asystole are more for cardiac arrest among hospitalized patients
CPR in the workplace Resuscitation in the media February 25, 1990 Terri Schiavo had cardiac arrest at home Was successfully revived by EMS team Suffered severe brain injury from the cardiac arrest event; after protracted legal battle, feeding tube was removed and she died on March 31, 2005
CPR in the home Resuscitation in the media Friday, June 25, 2009 Michael Jackson had cardiac arrest at his home; physician performed CPR Presumed respiratory arrest from drug overdose Attempted resuscitation (CPR and defibrillation) failed CPR performed in the bed – not a hard surface
CPR in the workplace Resuscitation in the media March 17, 2012 Fabrice Muamba had cardiac arrest while on English football field Was successfully revived after prolonged resuscitation efforts Brain injury was largely spared by the use of new treatment option known as “therapeutic hypothermia”
CPR in the workplace Resuscitation in the media June 08, 2016 Stephen Keshi, a former Coach of Nigeria’s Super Eagles died of possible Cardiac Arrest. According to family sources, Keshi complained of being unwell just before midnight on Tuesday, June 7, and he was found to be gasping for breath very close to mid-night. He was rushed to Faith Hospital in the Benin Government Reservation Area, where he died around 00. 30 in the morning of June 8. Not known if resuscitation efforts were made
CPR in the workplace Resuscitation in the media June 12, 2016 Amodu Shuaibu, also a former Coach of Nigeria’s Super Eagles died of possible Cardiac Arrest in his sleep after complaining of chest pains before retiring to bed. Resuscitation attempts were not made
The Three-Phase Model of the Disease, Cardiac Arrest And Reperfusion Injury
Reperfusion injury: clues from the laboratory Heart cells (myocytes) – grown in a petri dish Can simulate cardiac arrest and resuscitation: Bathe them in fluid without oxygen (cardiac arrest) Restore fluid with oxygen (resuscitation)
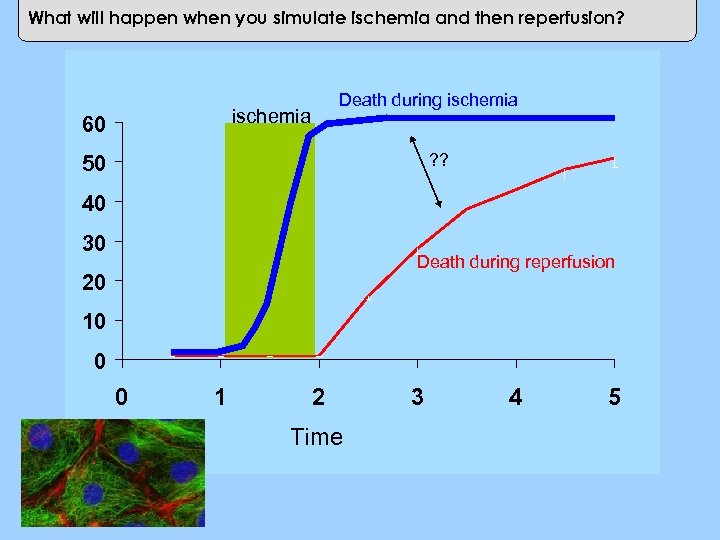
What will happen when you simulate ischemia and then reperfusion? ischemia 60 Cell Death (%) Death during ischemia ? ? 50 40 30 Death during reperfusion 20 10 0 0 1 2 Time 3 4 5
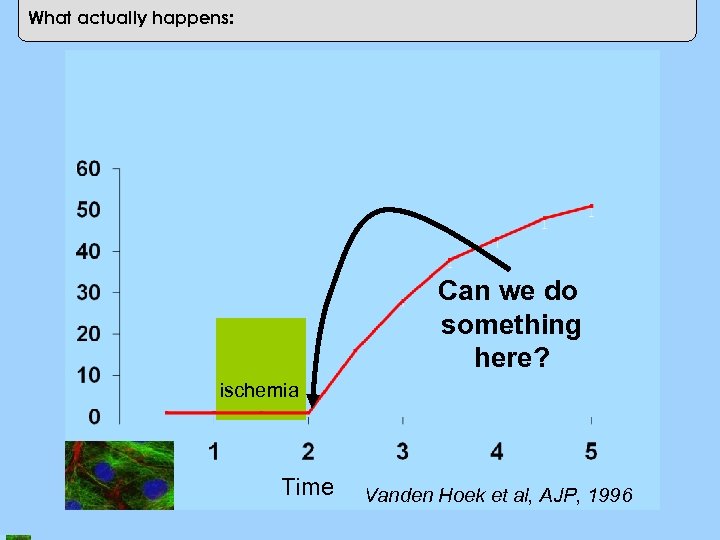
Cell Death (%) What actually happens: Can we do something here? ischemia Time Vanden Hoek et al, AJP, 1996
What this means: imagine the following situation Would you buy this car for $75, 000 ? One quirk: if you run out of gas, And you then put gas in the car…
What this means: imagine the following situation KAH BOOM
‘The most exciting phrase to hear in science, the one that heralds new discoveries, is not 'Eureka!' but 'That's funny. . . ’ Isaac Asimov
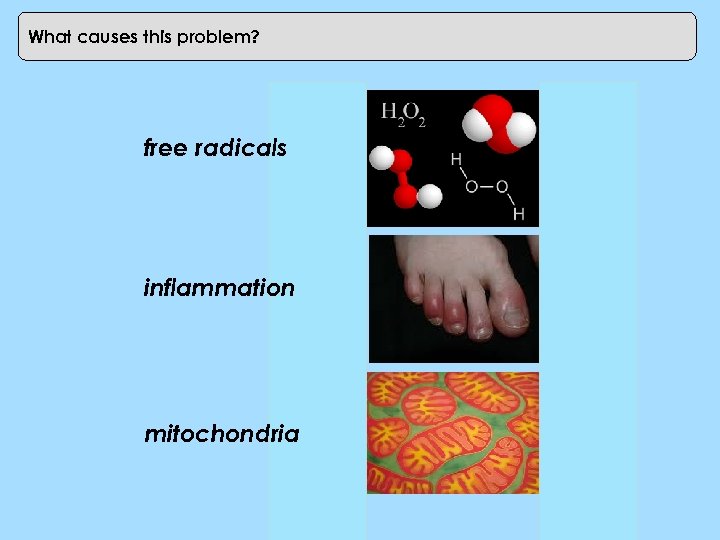
What causes this problem? free radicals inflammation mitochondria
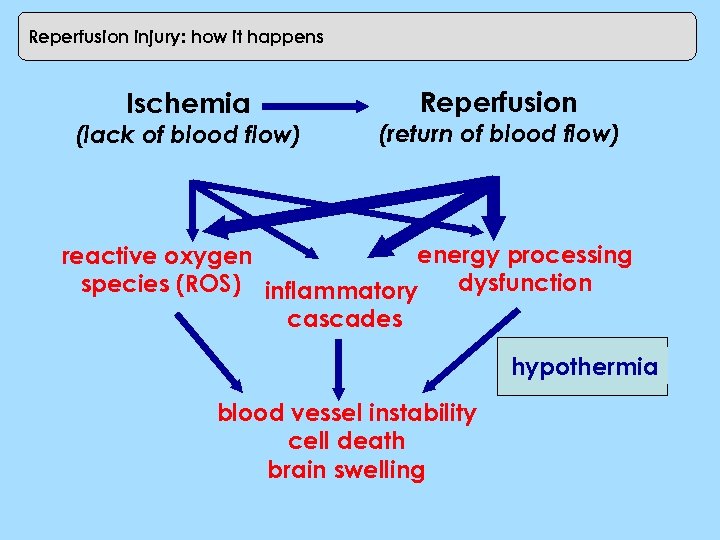
Reperfusion injury: how it happens Ischemia (lack of blood flow) Reperfusion (return of blood flow) energy processing reactive oxygen dysfunction species (ROS) inflammatory cascades hypothermia blood vessel instability cell death brain swelling
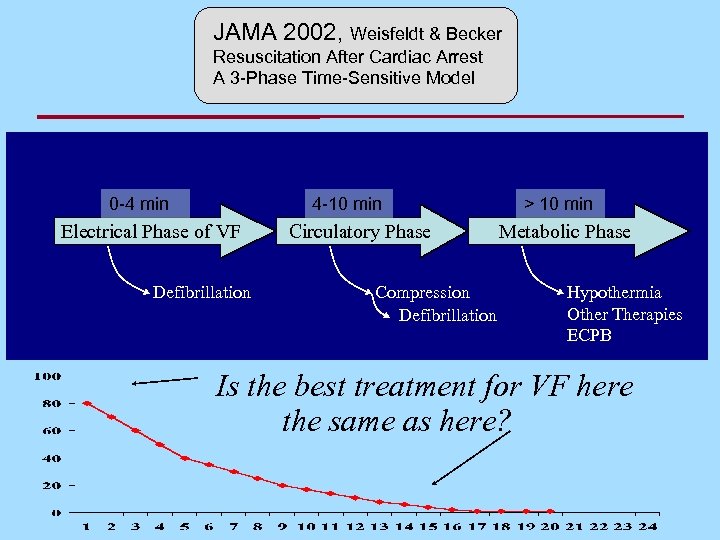
JAMA 2002, Weisfeldt & Becker Resuscitation After Cardiac Arrest A 3 -Phase Time-Sensitive Model 4 -10 min 0 -4 min Electrical Phase of VF Defibrillation Circulatory Phase Compression Defibrillation > 10 min Metabolic Phase Hypothermia Other Therapies ECPB Is the best treatment for VF here the same as here?
Electrical Phase
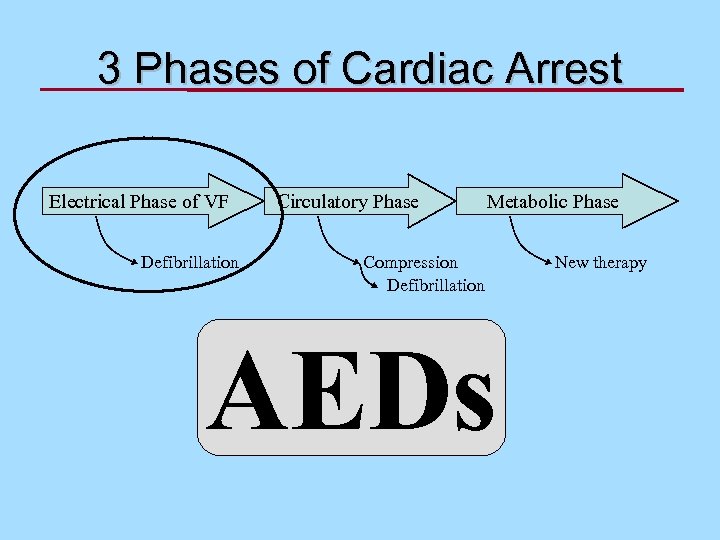
3 Phases of Cardiac Arrest Electrical Phase of VF Defibrillation Circulatory Phase Metabolic Phase Compression Defibrillation AEDs New therapy
Casino Study: Survival--Time is of the Essence • • Trained Security Officers in AEDs 105 patients, VF arrest 92 witnessed arrests Average time, collapse to shock: 4. 4 minutes Valenzuela et al. NEJM, 2000
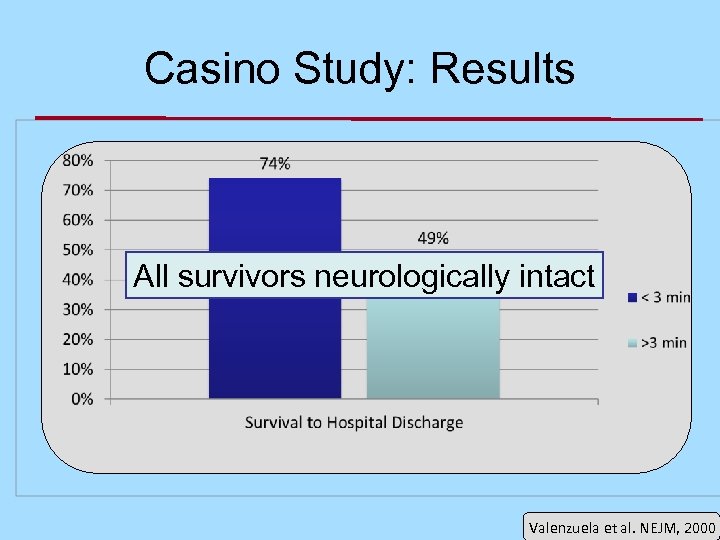
Casino Study: Results All survivors neurologically intact Valenzuela et al. NEJM, 2000
Circulatory Phase
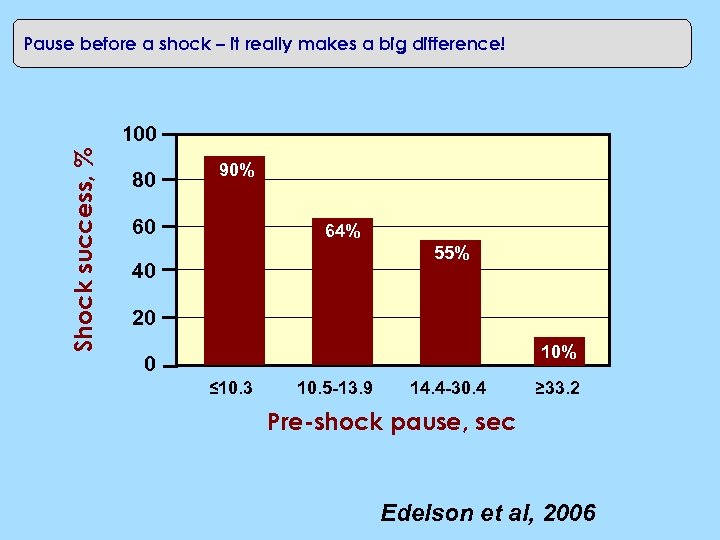
Pause before a shock – it really makes a big difference! Shock success, % 100 80 90% 60 64% 55% 40 20 10% 0 ≤ 10. 3 10. 5 -13. 9 14. 4 -30. 4 ≥ 33. 2 Pre-shock pause, sec Edelson et al, 2006
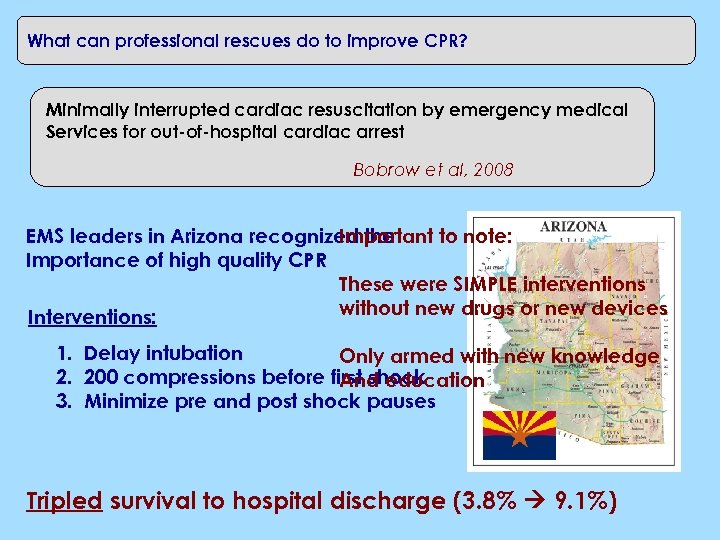
What can professional rescues do to improve CPR? Minimally interrupted cardiac resuscitation by emergency medical Services for out-of-hospital cardiac arrest Bobrow et al, 2008 Important to note: EMS leaders in Arizona recognized the Importance of high quality CPR These were SIMPLE interventions without new drugs or new devices Interventions: 1. Delay intubation Only armed with new knowledge 2. 200 compressions before first shock And education 3. Minimize pre and post shock pauses Tripled survival to hospital discharge (3. 8% 9. 1%)
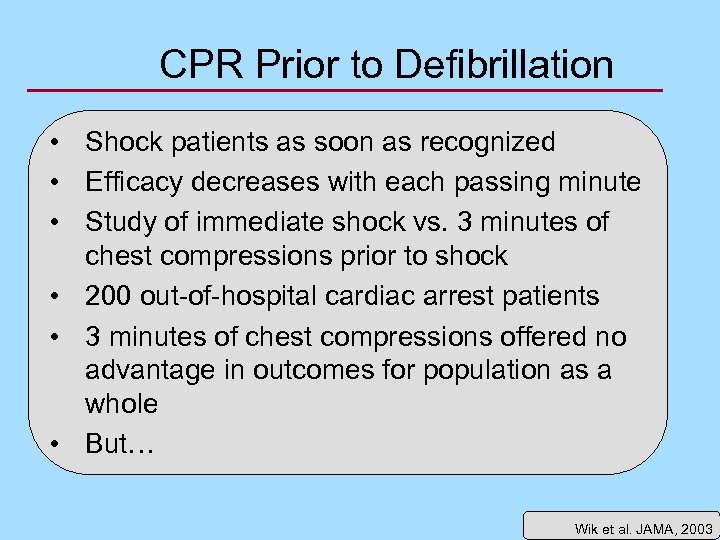
CPR Prior to Defibrillation • Shock patients as soon as recognized • Efficacy decreases with each passing minute • Study of immediate shock vs. 3 minutes of chest compressions prior to shock • 200 out-of-hospital cardiac arrest patients • 3 minutes of chest compressions offered no advantage in outcomes for population as a whole • But… Wik et al. JAMA, 2003
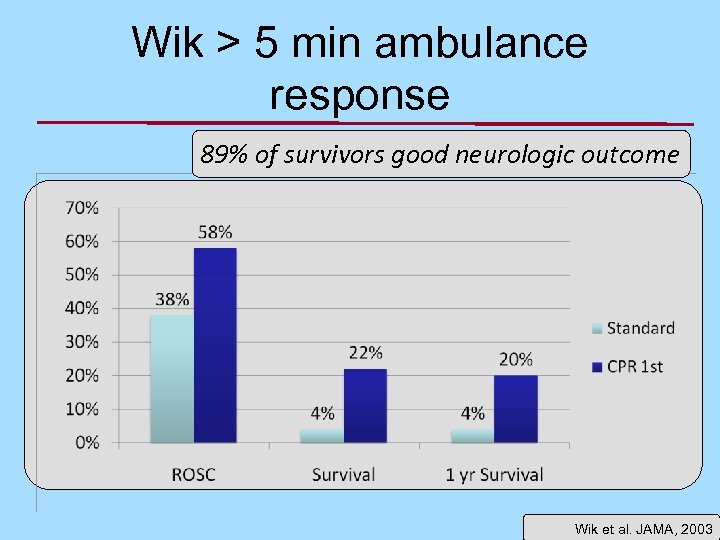
Wik > 5 min ambulance response 89% of survivors good neurologic outcome Wik et al. JAMA, 2003
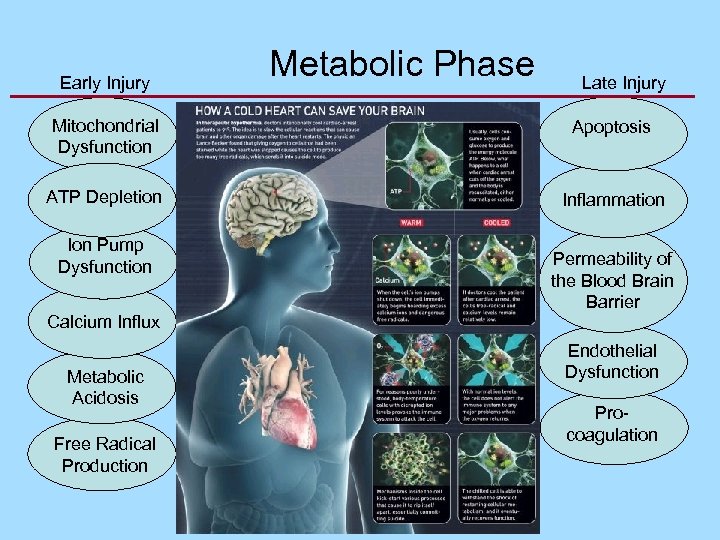
Early Injury Metabolic Phase Late Injury Mitochondrial Dysfunction Apoptosis ATP Depletion Inflammation Ion Pump Dysfunction Calcium Influx Metabolic Acidosis Free Radical Production Permeability of the Blood Brain Barrier Endothelial Dysfunction Procoagulation
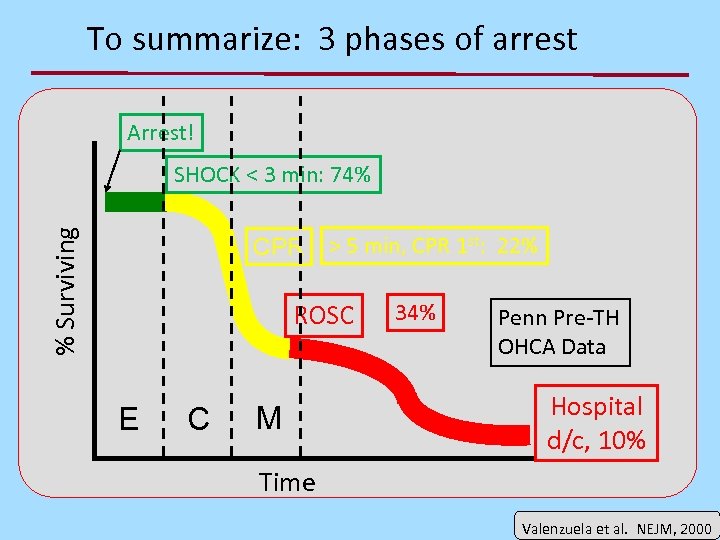
To summarize: 3 phases of arrest Arrest! % Surviving SHOCK < 3 min: 74% CPR > 5 min, CPR 1 st: 22% ROSC E C M 34% Penn Pre-TH OHCA Data Hospital d/c, 10% Time Valenzuela et al. NEJM, 2000
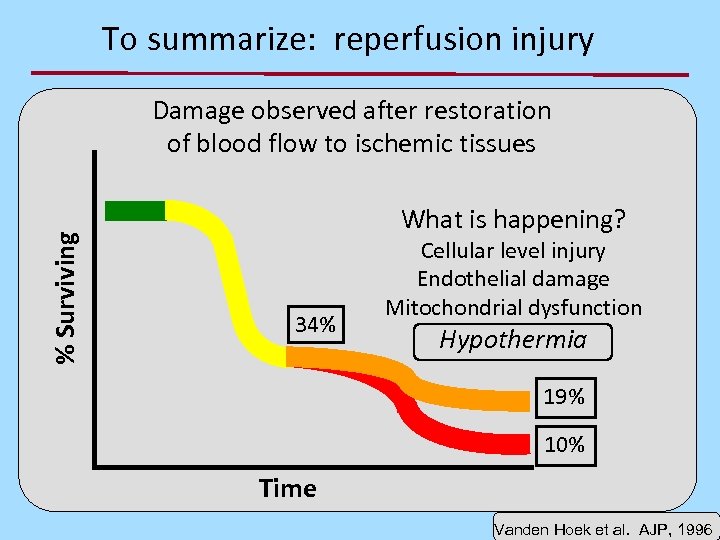
To summarize: reperfusion injury % Surviving Damage observed after restoration of blood flow to ischemic tissues What is happening? 34% Cellular level injury Endothelial damage Mitochondrial dysfunction Hypothermia 19% 10% Time Vanden Hoek et al. AJP, 1996
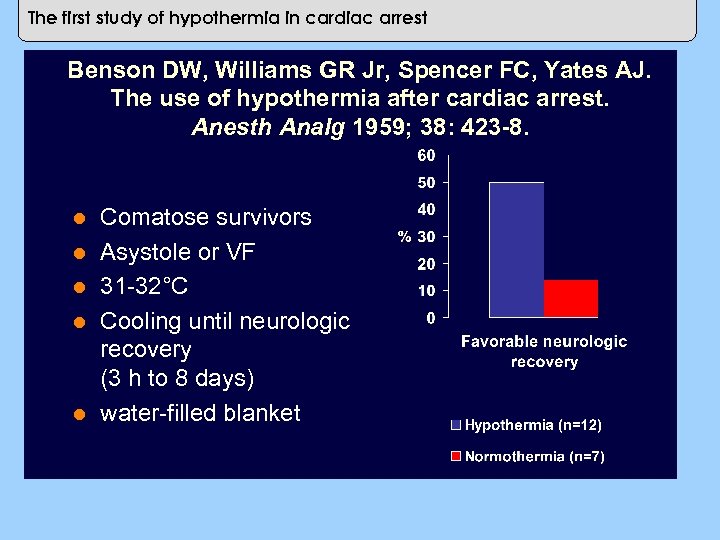
The first study of hypothermia in cardiac arrest Benson DW, Williams GR Jr, Spencer FC, Yates AJ. The use of hypothermia after cardiac arrest. Anesth Analg 1959; 38: 423 -8. l l l Comatose survivors Asystole or VF 31 -32°C Cooling until neurologic recovery (3 h to 8 days) water-filled blanket
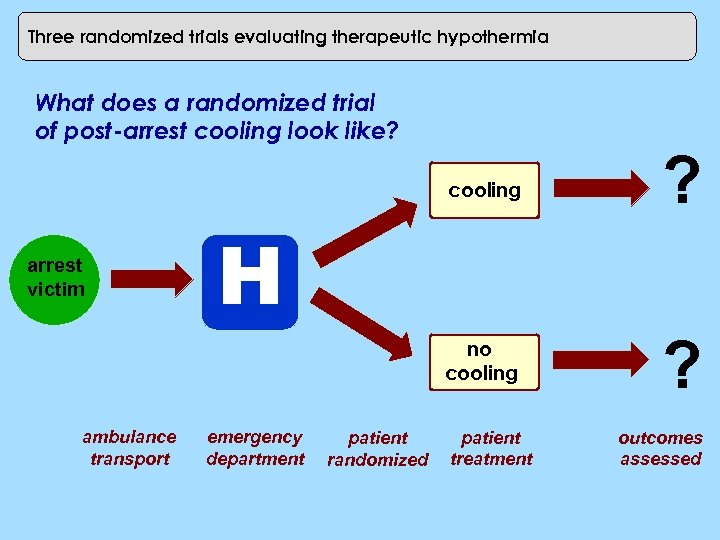
Three randomized trials evaluating therapeutic hypothermia What does a randomized trial of post-arrest cooling look like? cooling no cooling arrest victim ambulance transport ? ? H emergency department patient randomized patient treatment outcomes assessed
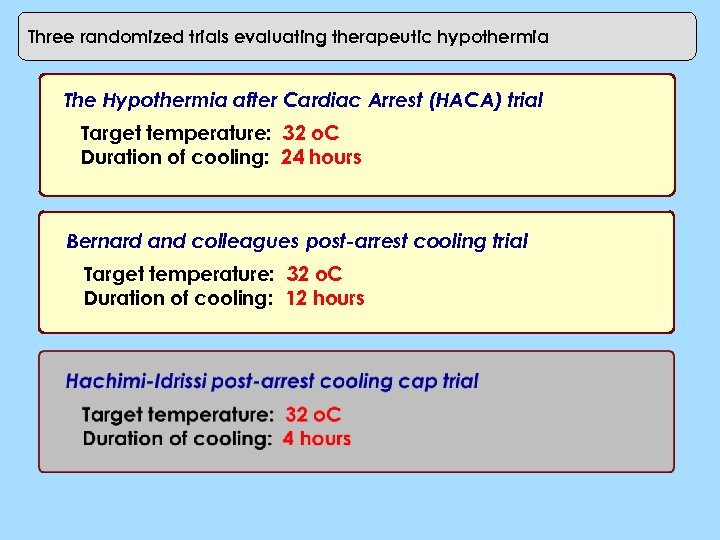
Three randomized trials evaluating therapeutic hypothermia The Hypothermia after Cardiac Arrest (HACA) trial Target temperature: 32 o. C Duration of cooling: 24 hours Bernard and colleagues post-arrest cooling trial Target temperature: 32 o. C Duration of cooling: 12 hours
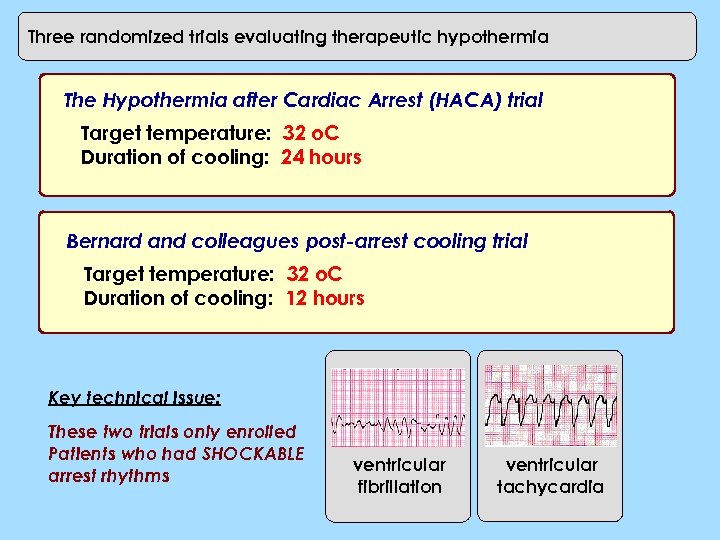
Three randomized trials evaluating therapeutic hypothermia The Hypothermia after Cardiac Arrest (HACA) trial Target temperature: 32 o. C Duration of cooling: 24 hours Bernard and colleagues post-arrest cooling trial Target temperature: 32 o. C Duration of cooling: 12 hours Key technical issue: These two trials only enrolled Patients who had SHOCKABLE arrest rhythms ventricular fibrillation ventricular tachycardia
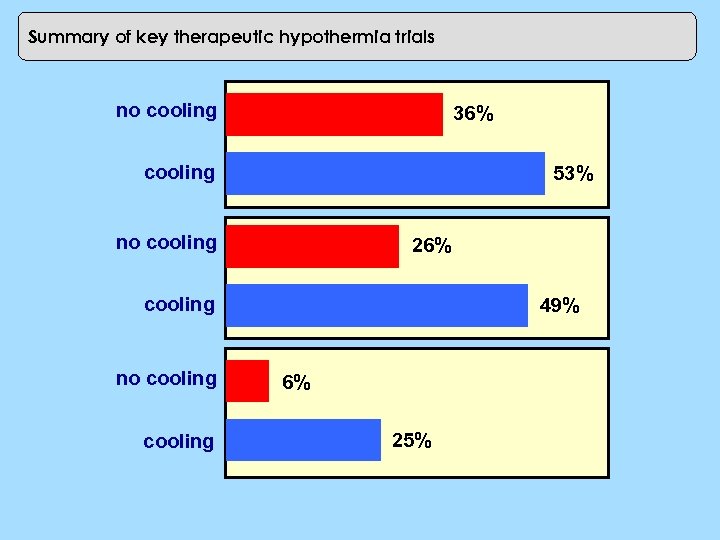
Hypothermia trials: outcomes Summary of key therapeutic hypothermia trials no cooling 36% cooling no cooling 53% 0 10 20 30 40 26% cooling no cooling 50 60 49% 6% 25%
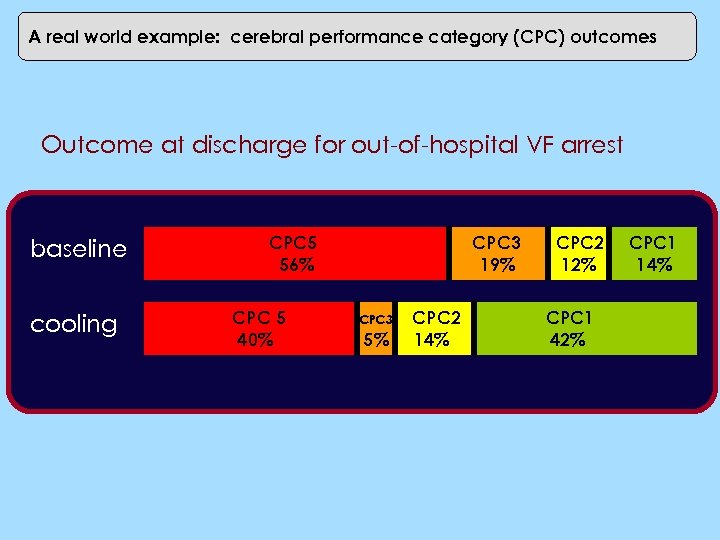
Real world usage: Switzerland A real world example: cerebral performance category (CPC) outcomes Outcome at discharge for out-of-hospital VF arrest baseline cooling CPC 5 56% CPC 5 40% CPC 3 19%. CPC 3 5% CPC 2 14% CPC 2 12% CPC 1 42% CPC 1 14%
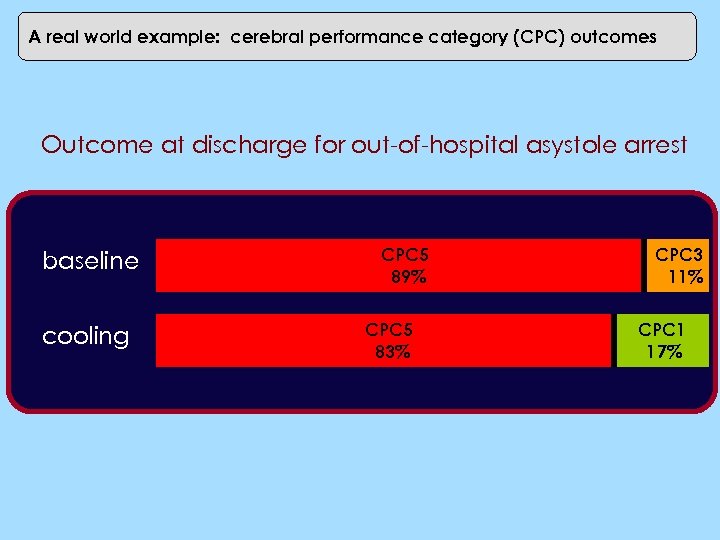
A real world example: cerebral performance category (CPC) Real world usage: Switzerland outcomes Outcome at discharge for out-of-hospital asystole arrest baseline cooling CPC 5 89% CPC 5 83% CPC 3 11% CPC 1 17%
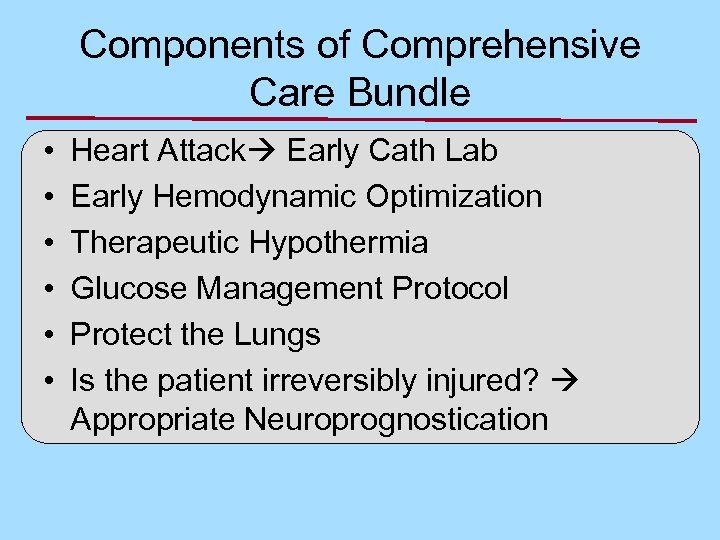
Components of Comprehensive Care Bundle • • • Heart Attack Early Cath Lab Early Hemodynamic Optimization Therapeutic Hypothermia Glucose Management Protocol Protect the Lungs Is the patient irreversibly injured? Appropriate Neuroprognostication
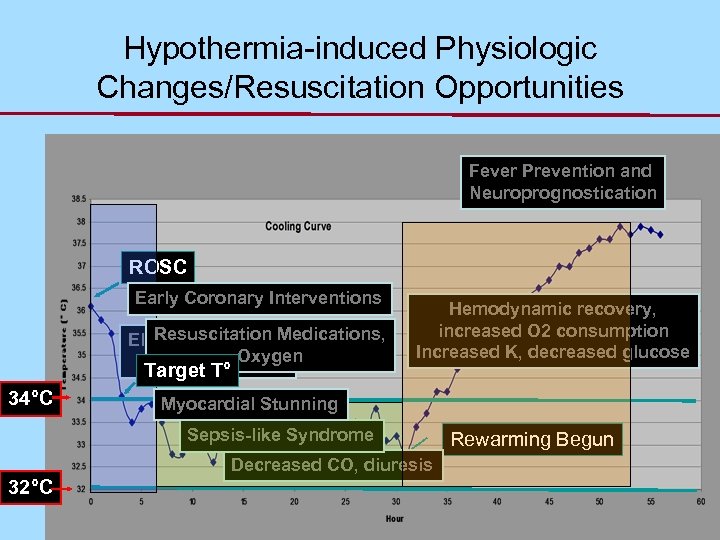
Hypothermia-induced Physiologic Changes/Resuscitation Opportunities Fever Prevention and Neuroprognostication ROSC Early Coronary Interventions Shivering Resuscitation Medications, Electrolyte Losses Oxygen Hyperglycemia Target T° 34°C Hemodynamic recovery, increased O 2 consumption Increased K, decreased glucose Myocardial Stunning Decreased HR, VO 2 Sepsis-like Syndrome Decreased CO, diuresis 32°C Rewarming Begun
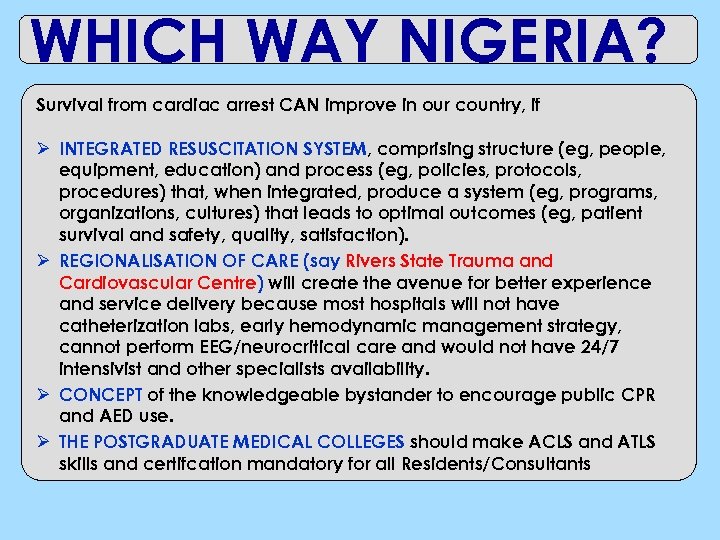
WHICH WAY NIGERIA? Survival from cardiac arrest CAN improve in our country, if Ø INTEGRATED RESUSCITATION SYSTEM, comprising structure (eg, people, equipment, education) and process (eg, policies, protocols, procedures) that, when integrated, produce a system (eg, programs, organizations, cultures) that leads to optimal outcomes (eg, patient survival and safety, quality, satisfaction). Ø REGIONALISATION OF CARE (say Rivers State Trauma and Cardiovascular Centre) will create the avenue for better experience and service delivery because most hospitals will not have catheterization labs, early hemodynamic management strategy, cannot perform EEG/neurocritical care and would not have 24/7 intensivist and other specialists availability. Ø CONCEPT of the knowledgeable bystander to encourage public CPR and AED use. Ø THE POSTGRADUATE MEDICAL COLLEGES should make ACLS and ATLS skills and certifcation mandatory for all Residents/Consultants
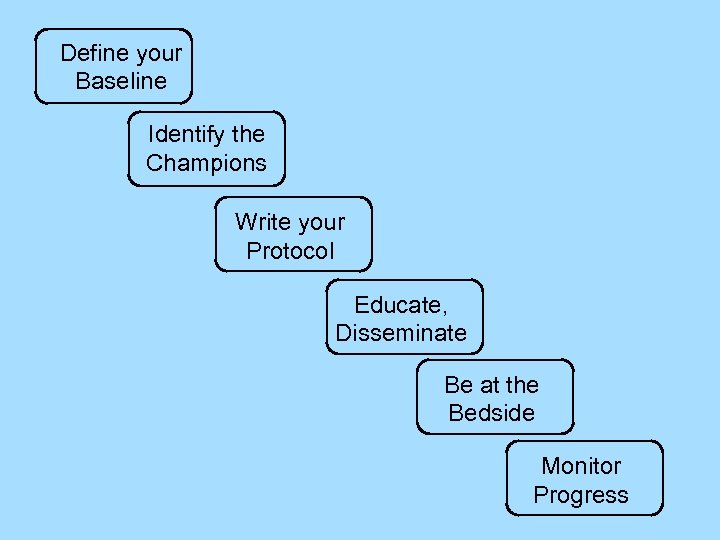
Define your Baseline Identify the Champions Write your Protocol Educate, Disseminate Be at the Bedside Monitor Progress
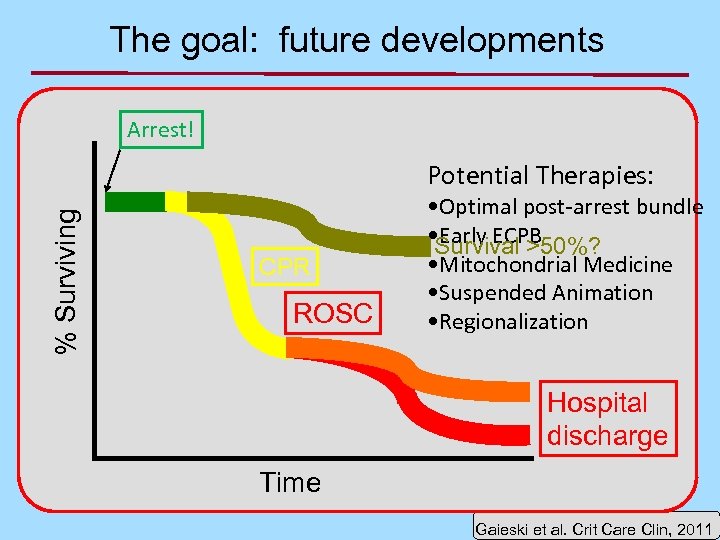
The goal: future developments Arrest! % Surviving Potential Therapies: CPR ROSC • Optimal post-arrest bundle • Early ECPB Survival >50%? • Mitochondrial Medicine • Suspended Animation • Regionalization Hospital discharge Time Gaieski et al. Crit Care Clin, 2011
ECPB Emergency Cardio-Pulmonary Bypass
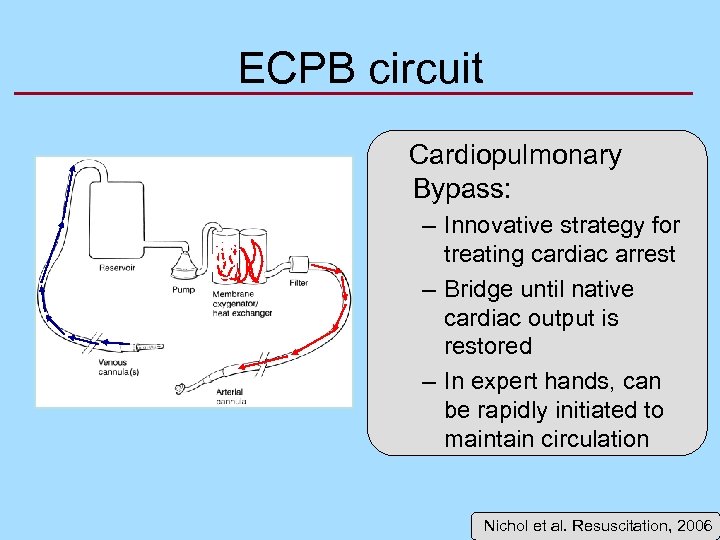
ECPB circuit Cardiopulmonary Bypass: – Innovative strategy for treating cardiac arrest – Bridge until native cardiac output is restored – In expert hands, can be rapidly initiated to maintain circulation Nichol et al. Resuscitation, 2006
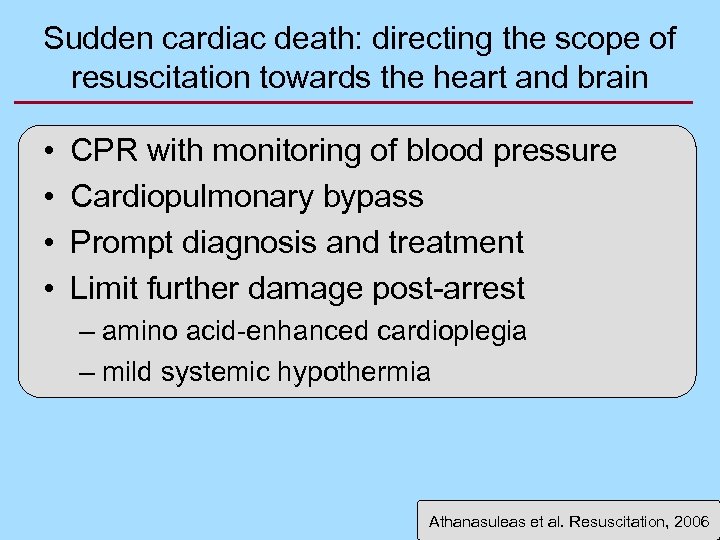
Sudden cardiac death: directing the scope of resuscitation towards the heart and brain • • CPR with monitoring of blood pressure Cardiopulmonary bypass Prompt diagnosis and treatment Limit further damage post-arrest – amino acid-enhanced cardioplegia – mild systemic hypothermia Athanasuleas et al. Resuscitation, 2006
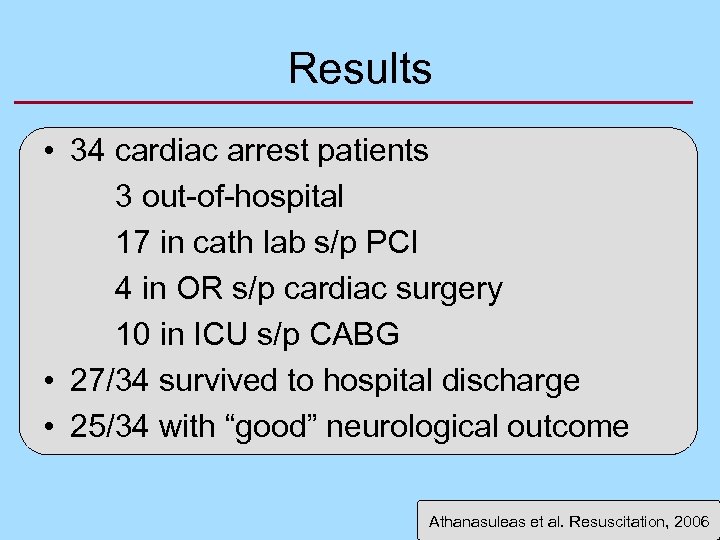
Results • 34 cardiac arrest patients 3 out-of-hospital 17 in cath lab s/p PCI 4 in OR s/p cardiac surgery 10 in ICU s/p CABG • 27/34 survived to hospital discharge • 25/34 with “good” neurological outcome Athanasuleas et al. Resuscitation, 2006
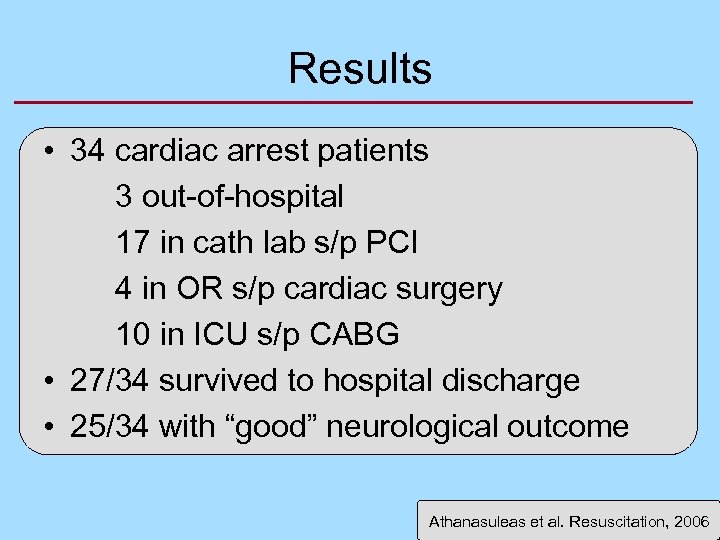
Results • 34 cardiac arrest patients 3 out-of-hospital 17 in cath lab s/p PCI 4 in OR s/p cardiac surgery 10 in ICU s/p CABG • 27/34 survived to hospital discharge • 25/34 with “good” neurological outcome Athanasuleas et al. Resuscitation, 2006
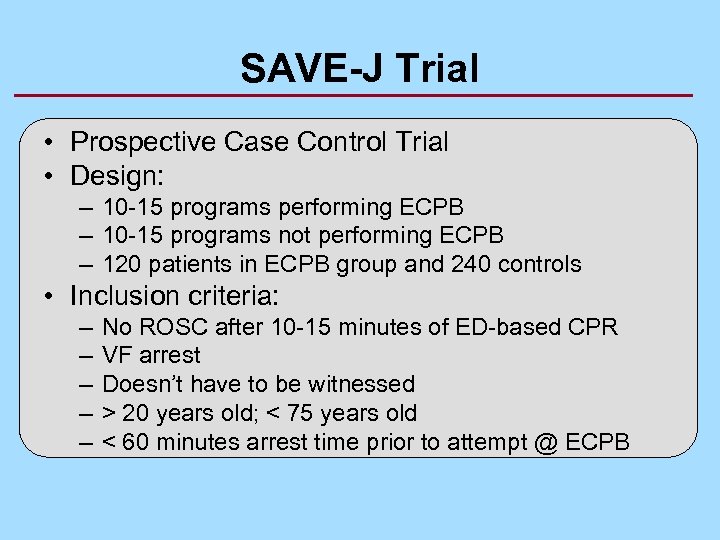
SAVE-J Trial • Prospective Case Control Trial • Design: – 10 -15 programs performing ECPB – 10 -15 programs not performing ECPB – 120 patients in ECPB group and 240 controls • Inclusion criteria: – – – No ROSC after 10 -15 minutes of ED-based CPR VF arrest Doesn’t have to be witnessed > 20 years old; < 75 years old < 60 minutes arrest time prior to attempt @ ECPB
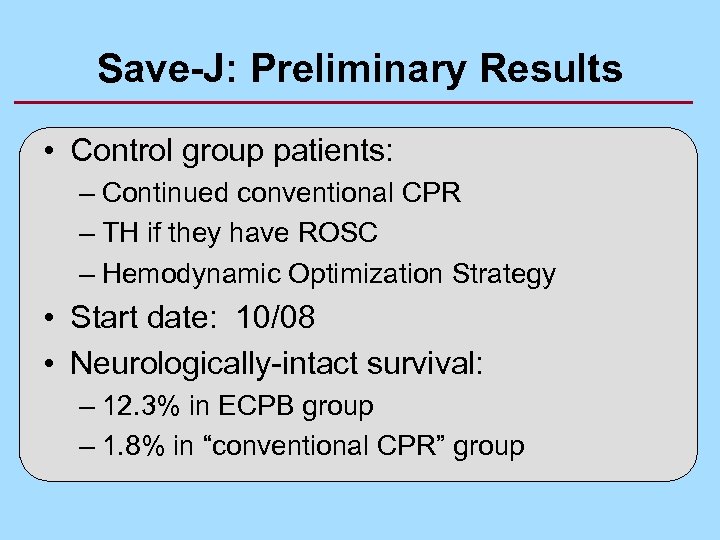
Save-J: Preliminary Results • Control group patients: – Continued conventional CPR – TH if they have ROSC – Hemodynamic Optimization Strategy • Start date: 10/08 • Neurologically-intact survival: – 12. 3% in ECPB group – 1. 8% in “conventional CPR” group
Suspended Animation = Emergency Preservation and Recovery
Hypovolemic Cardiac Arrest • Trauma hypovolemia cardiac arrest • 1984: Safar and Bellamy: – “Suspended animation: rapid preservation of viability of the organism in temporarily unresuscitable cardiac arrest…” – Immediate deep to profound hypothermia – Pharmacology – Surgical repair • 1988: Tisherman dog model of EPR Safer Center for Resuscitation Research. http: //www. safar. pitt. edu/content/programs/safar/
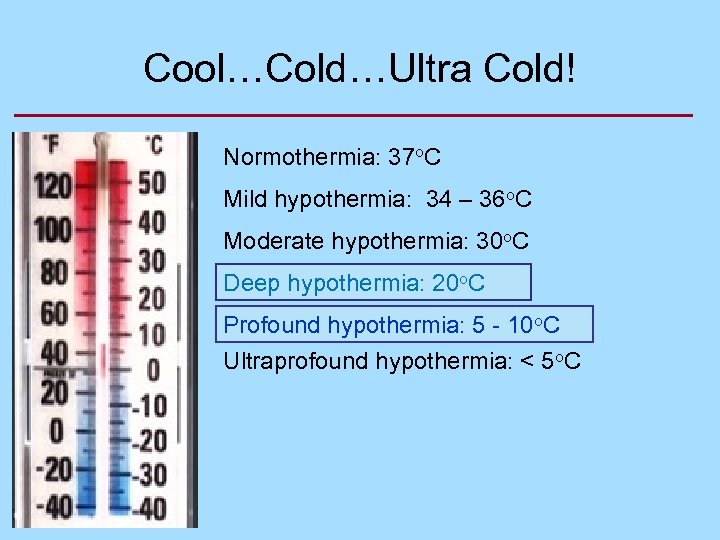
Cool…Cold…Ultra Cold! Normothermia: 37 o. C Mild hypothermia: 34 – 36 o. C Moderate hypothermia: 30 o. C Deep hypothermia: 20 o. C Profound hypothermia: 5 - 10 o. C Ultraprofound hypothermia: < 5 o. C
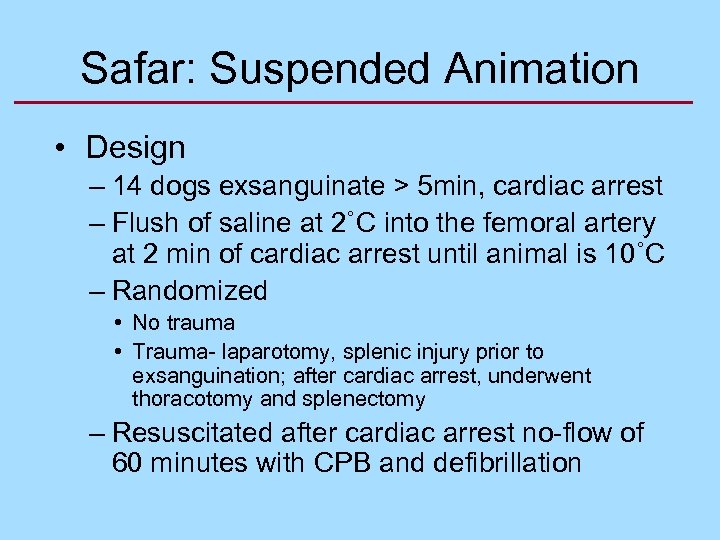
Safar: Suspended Animation • Design – 14 dogs exsanguinate > 5 min, cardiac arrest – Flush of saline at 2˚C into the femoral artery at 2 min of cardiac arrest until animal is 10˚C – Randomized • No trauma • Trauma- laparotomy, splenic injury prior to exsanguination; after cardiac arrest, underwent thoracotomy and splenectomy – Resuscitated after cardiac arrest no-flow of 60 minutes with CPB and defibrillation
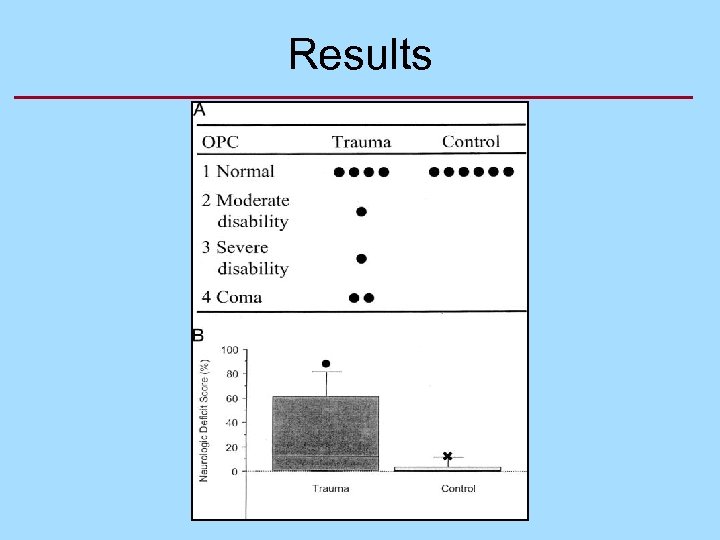
Results

Mitochondrial Medicine
ATP Death Intentional Death
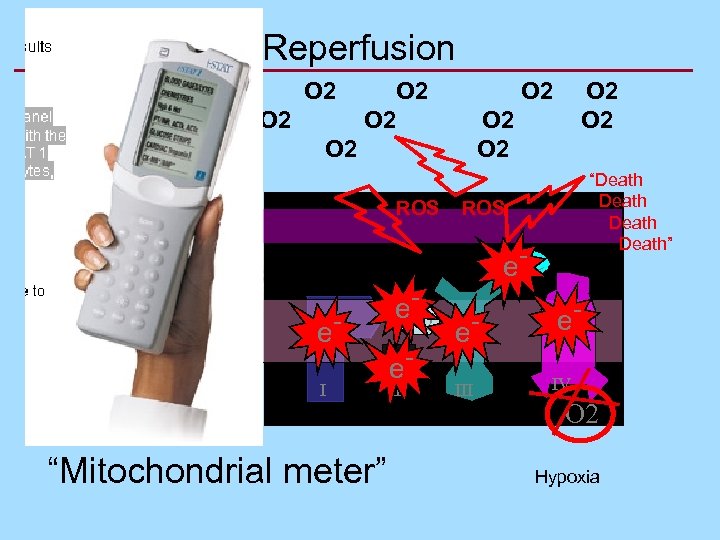
Reperfusion O 2 O 2 O 2 • Cocktail ATP • Antioxidants • Inhibit signaling • Cooling • Turn it OFF! Death • Mito inhibitors • HS, CO, CN O 2 ROS “Death Death” ROS Cyt C e- e. I “Mitochondrial meter” e. UQ e. III e. IV O 2 Hypoxia
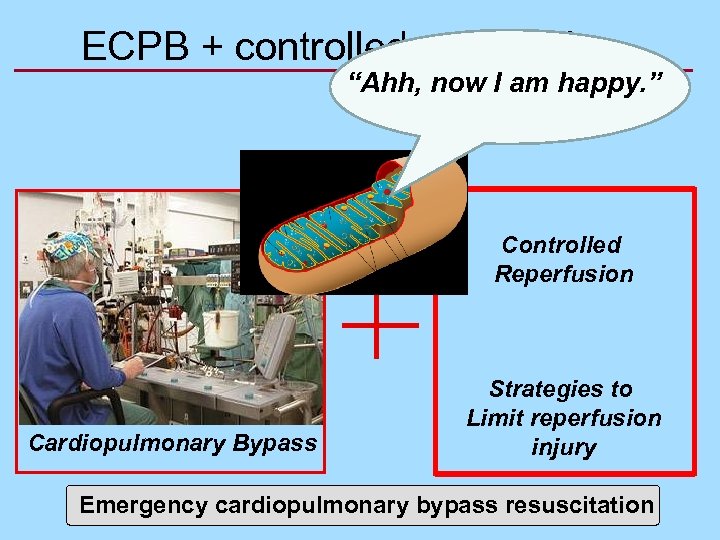
ECPB + controlled reperfusion “Ahh, now I am happy. ” Controlled Reperfusion Cardiopulmonary Bypass Strategies to Limit reperfusion injury Emergency cardiopulmonary bypass resuscitation
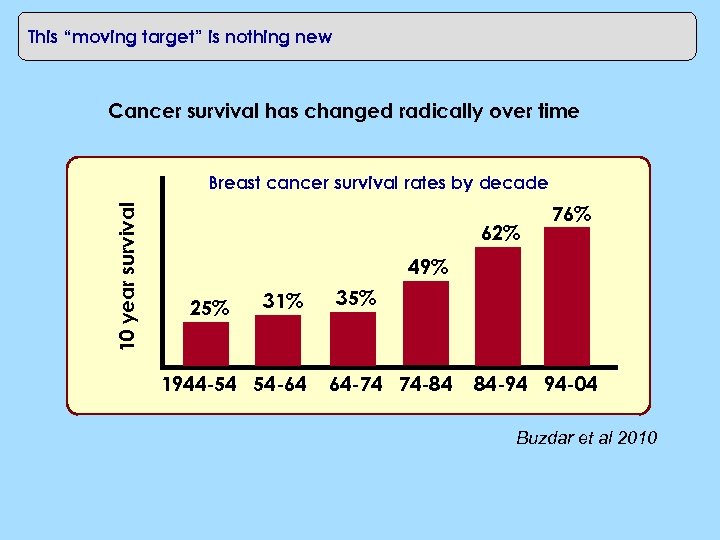
This “moving target” is nothing new Cancer survival has changed radically over time 10 year survival Breast cancer survival rates by decade 62% 76% 49% 25% 31% 1944 -54 54 -64 35% 64 -74 74 -84 84 -94 94 -04 Buzdar et al 2010
CONCLUSION WHEN DO WE SAY SOMEONE IS DEAD?
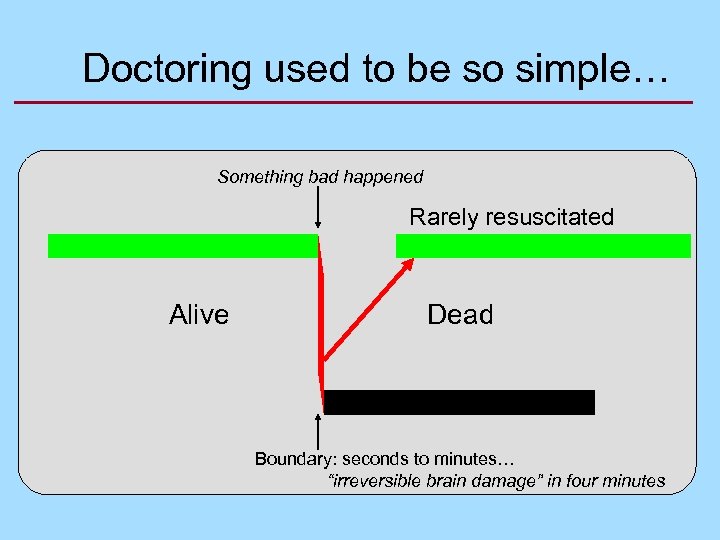
Doctoring used to be so simple… Something bad happened Rarely resuscitated Alive Dead Boundary: seconds to minutes… “irreversible brain damage” in four minutes
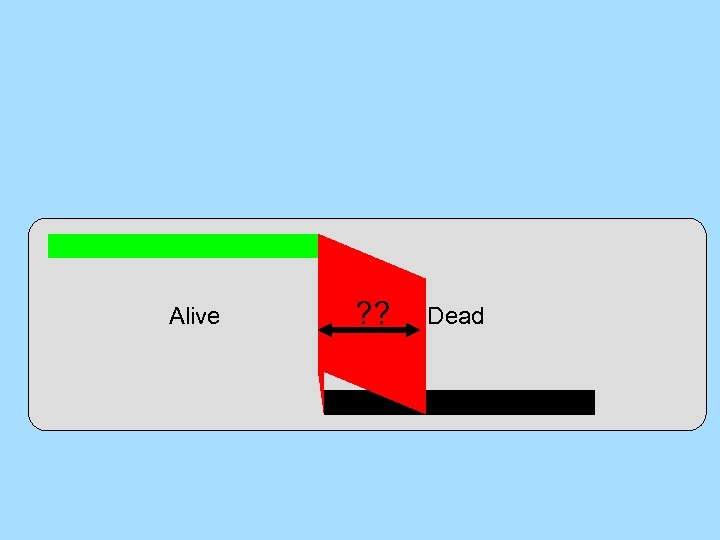
Alive ? ? Dead
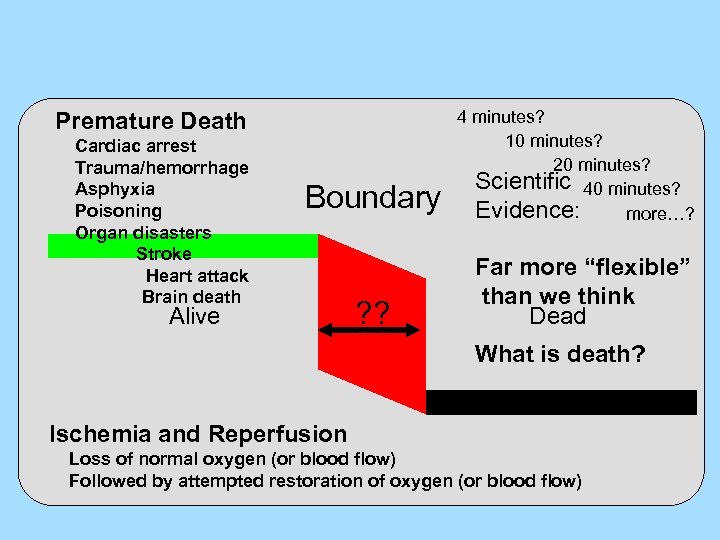
Premature Death Cardiac arrest Trauma/hemorrhage Asphyxia Poisoning Organ disasters Stroke Heart attack Brain death Boundary Alive ? ? 4 minutes? 10 minutes? 20 minutes? Scientific 40 minutes? Evidence: more…? Far more “flexible” than we think Dead What is death? Ischemia and Reperfusion Loss of normal oxygen (or blood flow) Followed by attempted restoration of oxygen (or blood flow)
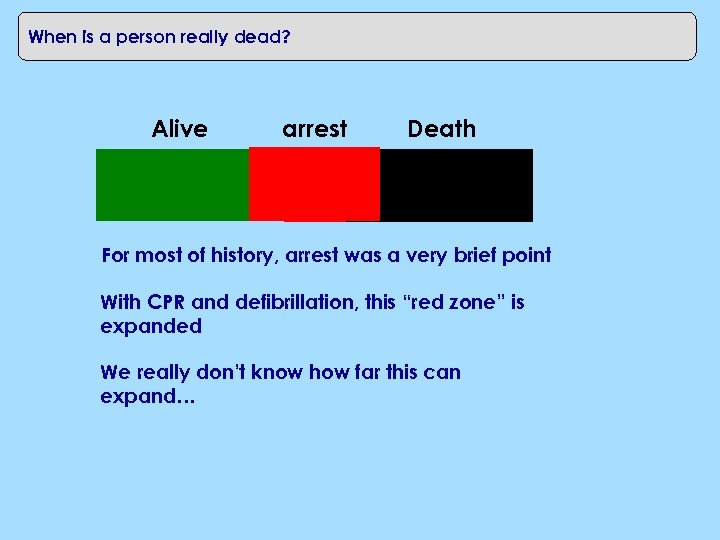
When is a person really dead? Alive arrest Death For most of history, arrest was a very brief point With CPR and defibrillation, this “red zone” is expanded We really don’t know how far this can expand…
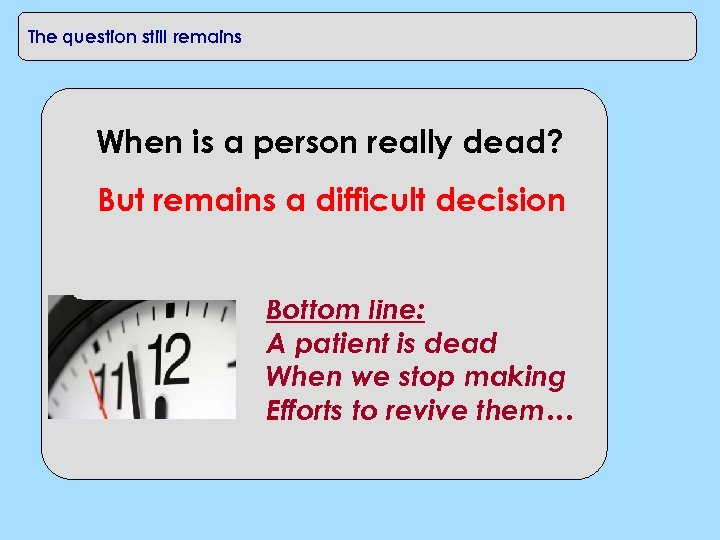
The question still remains When is a person really dead? But remains a difficult decision Health care providers must “call the code”: Very difficult to know when is the right time Body of work exists around termination rules, Bottom line: A patient is dead When we stop making Efforts to revive them…
“Life is pleasant. Death is peaceful. It's the transition that's troublesome. ” ~Isaac Asimov

THANK YOU
02f64e711c090dd83632f0b7bdb8c955.ppt