bd6532f2ad4aa03b4c55e572271b7088.ppt
- Количество слайдов: 52
 Capnography in the PACU: Theory and Clinical Applications of end tidal C 02 Monitoring Perianesthesia Nurses Association of British Columbia Cathy Hanley, RN, BSN November 6, 2010
Capnography in the PACU: Theory and Clinical Applications of end tidal C 02 Monitoring Perianesthesia Nurses Association of British Columbia Cathy Hanley, RN, BSN November 6, 2010
 Objectives § § § Review of physiology, ventilation vs oxygenation Identify normal and abnormal et. C 02 values and waveforms and appropriate clinical interventions Discuss current applications of capnography in the PACU and beyond Discuss current standards and recommendations Review of capnography case studies
Objectives § § § Review of physiology, ventilation vs oxygenation Identify normal and abnormal et. C 02 values and waveforms and appropriate clinical interventions Discuss current applications of capnography in the PACU and beyond Discuss current standards and recommendations Review of capnography case studies
 Brief History of Capnography Used in anesthesia since the 1970 s § Canadian Anesthesiologists’ Society requires it in the OR § New recommendations and standards expanding utilization §
Brief History of Capnography Used in anesthesia since the 1970 s § Canadian Anesthesiologists’ Society requires it in the OR § New recommendations and standards expanding utilization §
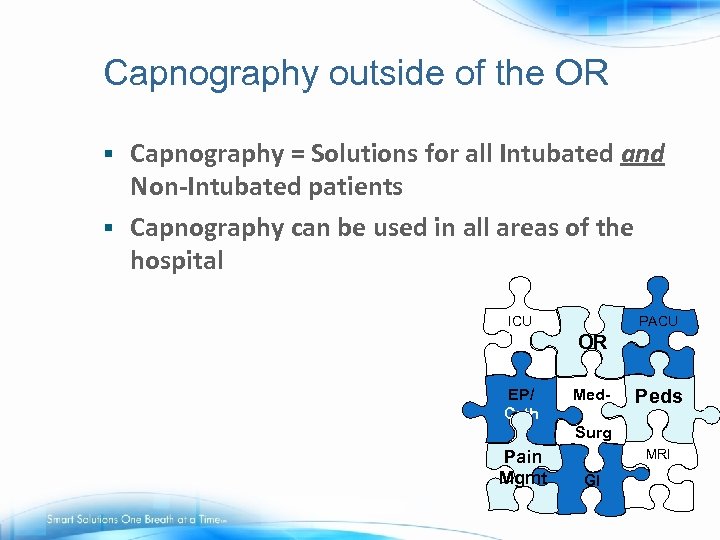 Capnography outside of the OR Capnography = Solutions for all Intubated and Non-Intubated patients § Capnography can be used in all areas of the hospital § PACU ICU OR EP/ Cath Med. Surg Pain Mgmt Peds. MRI GI
Capnography outside of the OR Capnography = Solutions for all Intubated and Non-Intubated patients § Capnography can be used in all areas of the hospital § PACU ICU OR EP/ Cath Med. Surg Pain Mgmt Peds. MRI GI
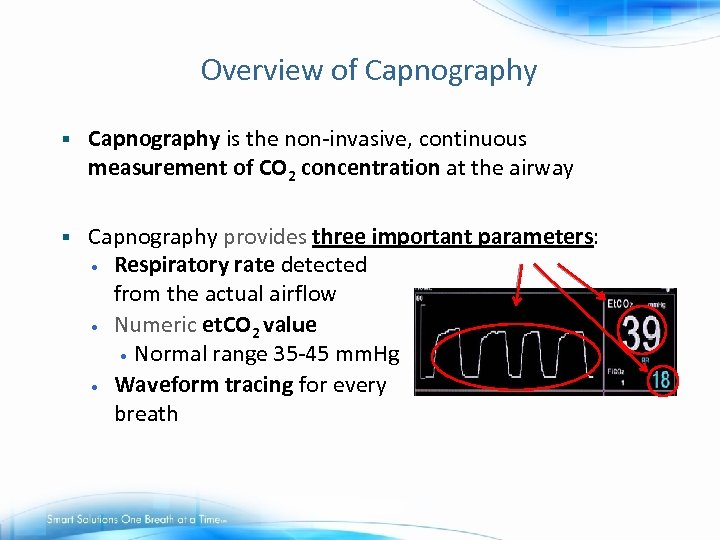 Overview of Capnography § Capnography is the non-invasive, continuous measurement of CO 2 concentration at the airway § Capnography provides three important parameters: • Respiratory rate detected from the actual airflow • Numeric et. CO 2 value • Normal range 35 -45 mm. Hg • Waveform tracing for every breath
Overview of Capnography § Capnography is the non-invasive, continuous measurement of CO 2 concentration at the airway § Capnography provides three important parameters: • Respiratory rate detected from the actual airflow • Numeric et. CO 2 value • Normal range 35 -45 mm. Hg • Waveform tracing for every breath
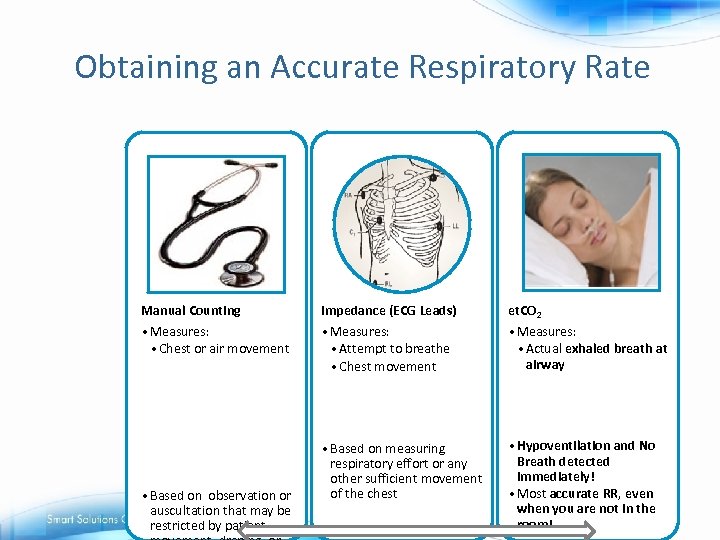 Obtaining an Accurate Respiratory Rate Manual Counting Impedance (ECG Leads) et. CO 2 • Measures: • Chest or air movement • Measures: • Attempt to breathe • Chest movement • Measures: • Actual exhaled breath at airway • Based on measuring respiratory effort or any other sufficient movement of the chest • Hypoventilation and No Breath detected immediately! • Most accurate RR, even when you are not in the room! • Based on observation or auscultation that may be restricted by patient
Obtaining an Accurate Respiratory Rate Manual Counting Impedance (ECG Leads) et. CO 2 • Measures: • Chest or air movement • Measures: • Attempt to breathe • Chest movement • Measures: • Actual exhaled breath at airway • Based on measuring respiratory effort or any other sufficient movement of the chest • Hypoventilation and No Breath detected immediately! • Most accurate RR, even when you are not in the room! • Based on observation or auscultation that may be restricted by patient
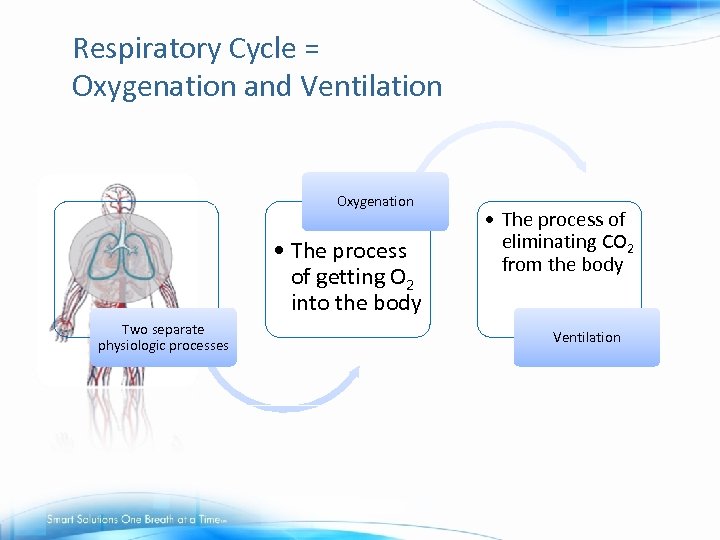 Respiratory Cycle = Oxygenation and Ventilation Oxygenation • The process of getting O 2 into the body Two separate physiologic processes • The process of eliminating CO 2 from the body Ventilation
Respiratory Cycle = Oxygenation and Ventilation Oxygenation • The process of getting O 2 into the body Two separate physiologic processes • The process of eliminating CO 2 from the body Ventilation
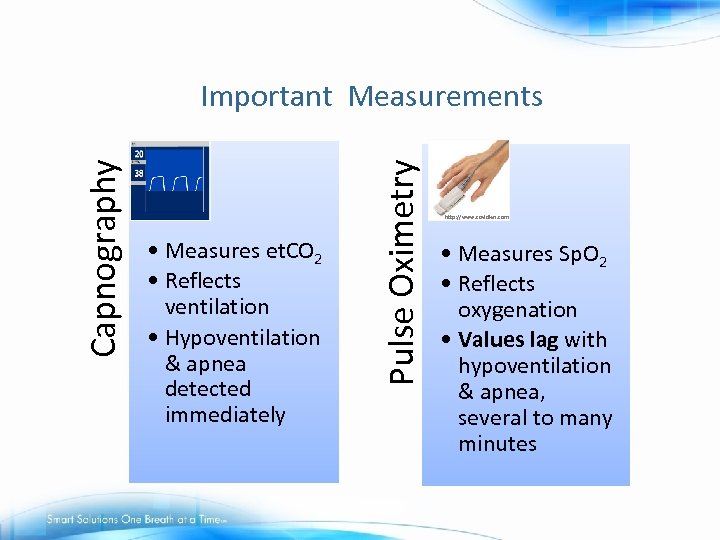 • Measures et. CO 2 • Reflects ventilation • Hypoventilation & apnea detected immediately Pulse Oximetry Capnography Important Measurements http: //www. covidien. com • Measures Sp. O 2 • Reflects oxygenation • Values lag with hypoventilation & apnea, several to many minutes
• Measures et. CO 2 • Reflects ventilation • Hypoventilation & apnea detected immediately Pulse Oximetry Capnography Important Measurements http: //www. covidien. com • Measures Sp. O 2 • Reflects oxygenation • Values lag with hypoventilation & apnea, several to many minutes
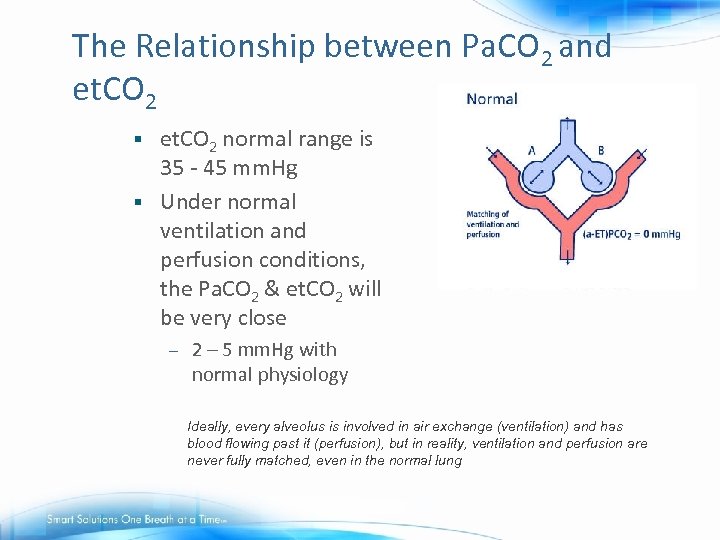 The Relationship between Pa. CO 2 and et. CO 2 normal range is 35 - 45 mm. Hg § Under normal ventilation and perfusion conditions, the Pa. CO 2 & et. CO 2 will be very close § – 2 – 5 mm. Hg with normal physiology Ideally, every alveolus is involved in air exchange (ventilation) and has blood flowing past it (perfusion), but in reality, ventilation and perfusion are never fully matched, even in the normal lung
The Relationship between Pa. CO 2 and et. CO 2 normal range is 35 - 45 mm. Hg § Under normal ventilation and perfusion conditions, the Pa. CO 2 & et. CO 2 will be very close § – 2 – 5 mm. Hg with normal physiology Ideally, every alveolus is involved in air exchange (ventilation) and has blood flowing past it (perfusion), but in reality, ventilation and perfusion are never fully matched, even in the normal lung
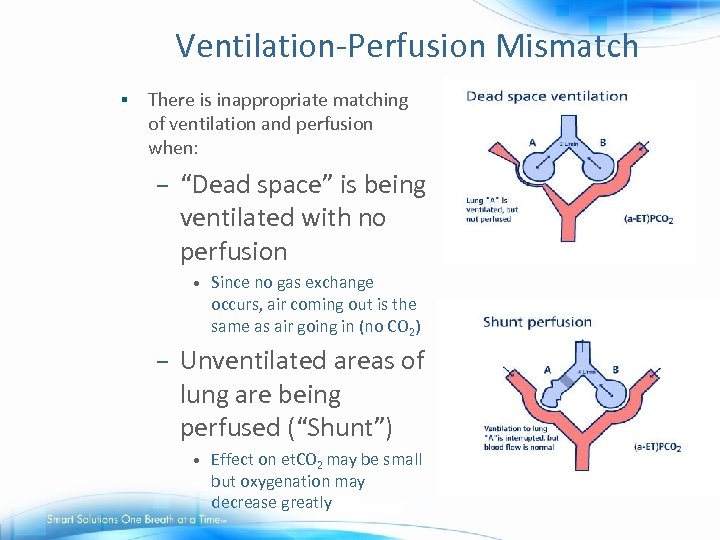 Ventilation-Perfusion Mismatch § There is inappropriate matching of ventilation and perfusion when: – “Dead space” is being ventilated with no perfusion • – Since no gas exchange occurs, air coming out is the same as air going in (no CO 2) Unventilated areas of lung are being perfused (“Shunt”) • Effect on et. CO 2 may be small but oxygenation may decrease greatly
Ventilation-Perfusion Mismatch § There is inappropriate matching of ventilation and perfusion when: – “Dead space” is being ventilated with no perfusion • – Since no gas exchange occurs, air coming out is the same as air going in (no CO 2) Unventilated areas of lung are being perfused (“Shunt”) • Effect on et. CO 2 may be small but oxygenation may decrease greatly
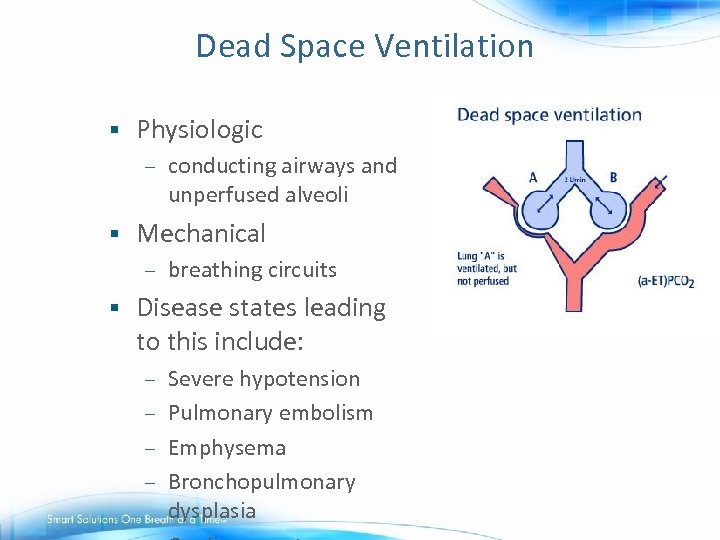 Dead Space Ventilation § Physiologic – § Mechanical – § conducting airways and unperfused alveoli breathing circuits Disease states leading to this include: Severe hypotension – Pulmonary embolism – Emphysema – Bronchopulmonary dysplasia –
Dead Space Ventilation § Physiologic – § Mechanical – § conducting airways and unperfused alveoli breathing circuits Disease states leading to this include: Severe hypotension – Pulmonary embolism – Emphysema – Bronchopulmonary dysplasia –
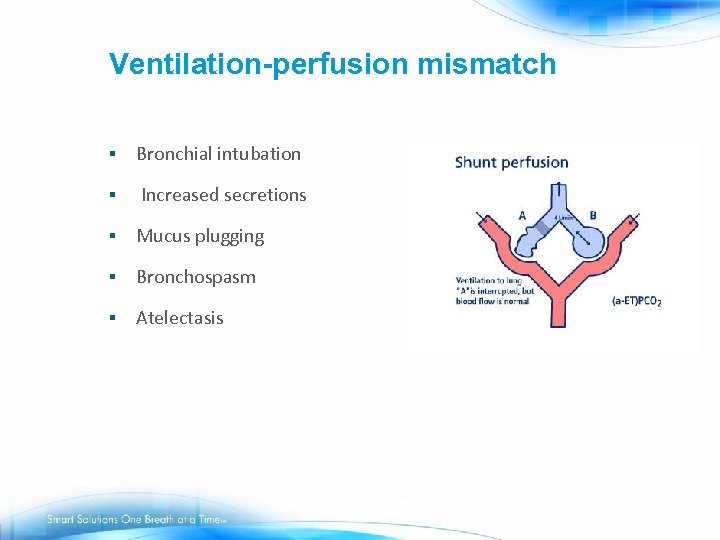 Ventilation-perfusion mismatch § Bronchial intubation § Increased secretions § Mucus plugging § Bronchospasm § Atelectasis
Ventilation-perfusion mismatch § Bronchial intubation § Increased secretions § Mucus plugging § Bronchospasm § Atelectasis
 Summary - Et. CO 2 vs. Pa. CO 2 § End tidal CO 2 (Et. CO 2) = noninvasive measurement of CO 2 at the end of expiration § Et. CO 2 allows trending of Pa. CO 2 - a clinical estimate of the Pa. CO 2, when ventilation and perfusion are appropriately matched § Wide gradient is diagnostic of a ventilation-perfusion mismatch § Et. CO 2 monitoring allows for a breath by breath assessment of ventilation.
Summary - Et. CO 2 vs. Pa. CO 2 § End tidal CO 2 (Et. CO 2) = noninvasive measurement of CO 2 at the end of expiration § Et. CO 2 allows trending of Pa. CO 2 - a clinical estimate of the Pa. CO 2, when ventilation and perfusion are appropriately matched § Wide gradient is diagnostic of a ventilation-perfusion mismatch § Et. CO 2 monitoring allows for a breath by breath assessment of ventilation.
 Why use et. C 02 in the PACU ? § Accurately monitors effective ventilation, giving a true airway respiratory rate • Early warning of : § Hypoventilation § Apnea § Obstruction Provides easy and accurate airway monitoring for intubated or non-intubated patients – Promotes better ventilation assessment resulting in timely interventions – Titrate sedation and pain medication
Why use et. C 02 in the PACU ? § Accurately monitors effective ventilation, giving a true airway respiratory rate • Early warning of : § Hypoventilation § Apnea § Obstruction Provides easy and accurate airway monitoring for intubated or non-intubated patients – Promotes better ventilation assessment resulting in timely interventions – Titrate sedation and pain medication
 Why use et. C 02 in the PACU? § § § Indicator of Malignant Hyperthermia Use with patient with history of respiratory compromise, such as asthma or COPD to monitor trend and need for breathing treatments and response to treatment Endotracheal tube placement Monitoring during weaning Decrease frequency of arterial blood gases Use with non-invasive ventilation (NIV)
Why use et. C 02 in the PACU? § § § Indicator of Malignant Hyperthermia Use with patient with history of respiratory compromise, such as asthma or COPD to monitor trend and need for breathing treatments and response to treatment Endotracheal tube placement Monitoring during weaning Decrease frequency of arterial blood gases Use with non-invasive ventilation (NIV)
 Case Study: Microstream Capnography in the PACU: Submitted by: Larry Myers RRT Cottonwood Hospital Murray, Utah § Profile § A 31 -year-old female s/p abdominal hysterectomy 6 months prior to admission is admitted with right lower quadrant pain. The patient underwent a bilateral salpingooophorectomy and lysis of adhesions on this admission. On post-op day one she became hypotensive and had a substantial decrease in her hematocrit. The patient was returned to the OR for an exploratory laparotomy.
Case Study: Microstream Capnography in the PACU: Submitted by: Larry Myers RRT Cottonwood Hospital Murray, Utah § Profile § A 31 -year-old female s/p abdominal hysterectomy 6 months prior to admission is admitted with right lower quadrant pain. The patient underwent a bilateral salpingooophorectomy and lysis of adhesions on this admission. On post-op day one she became hypotensive and had a substantial decrease in her hematocrit. The patient was returned to the OR for an exploratory laparotomy.
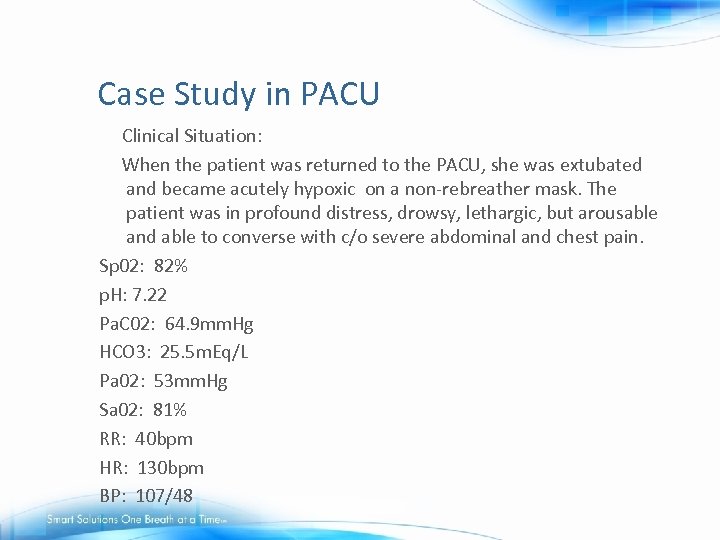 Case Study in PACU Clinical Situation: When the patient was returned to the PACU, she was extubated and became acutely hypoxic on a non-rebreather mask. The patient was in profound distress, drowsy, lethargic, but arousable and able to converse with c/o severe abdominal and chest pain. Sp 02: 82% p. H: 7. 22 Pa. C 02: 64. 9 mm. Hg HCO 3: 25. 5 m. Eq/L Pa 02: 53 mm. Hg Sa 02: 81% RR: 40 bpm HR: 130 bpm BP: 107/48
Case Study in PACU Clinical Situation: When the patient was returned to the PACU, she was extubated and became acutely hypoxic on a non-rebreather mask. The patient was in profound distress, drowsy, lethargic, but arousable and able to converse with c/o severe abdominal and chest pain. Sp 02: 82% p. H: 7. 22 Pa. C 02: 64. 9 mm. Hg HCO 3: 25. 5 m. Eq/L Pa 02: 53 mm. Hg Sa 02: 81% RR: 40 bpm HR: 130 bpm BP: 107/48
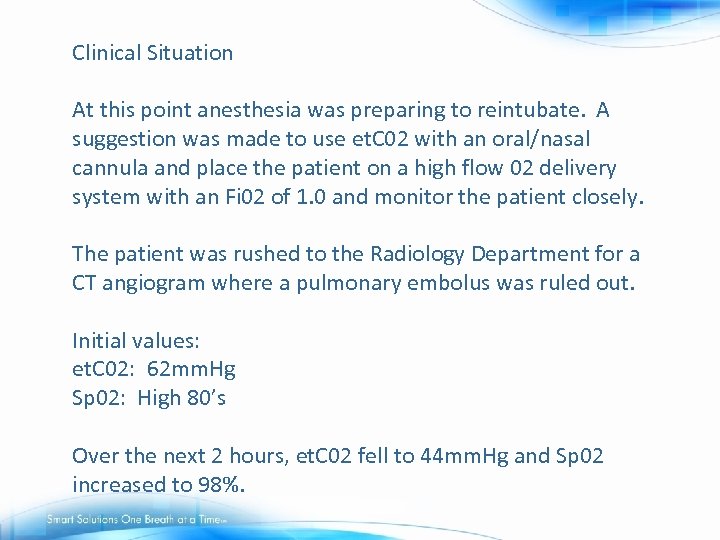 Clinical Situation At this point anesthesia was preparing to reintubate. A suggestion was made to use et. C 02 with an oral/nasal cannula and place the patient on a high flow 02 delivery system with an Fi 02 of 1. 0 and monitor the patient closely. The patient was rushed to the Radiology Department for a CT angiogram where a pulmonary embolus was ruled out. Initial values: et. C 02: 62 mm. Hg Sp 02: High 80’s Over the next 2 hours, et. C 02 fell to 44 mm. Hg and Sp 02 increased to 98%.
Clinical Situation At this point anesthesia was preparing to reintubate. A suggestion was made to use et. C 02 with an oral/nasal cannula and place the patient on a high flow 02 delivery system with an Fi 02 of 1. 0 and monitor the patient closely. The patient was rushed to the Radiology Department for a CT angiogram where a pulmonary embolus was ruled out. Initial values: et. C 02: 62 mm. Hg Sp 02: High 80’s Over the next 2 hours, et. C 02 fell to 44 mm. Hg and Sp 02 increased to 98%.
 Discussion The continuous monitoring of Et. CO 2 and Sp. O 2 when measured in concert but evaluated independently allowed this patient to be safely observed and avoid reintubation and mechanical ventilation. It is also interesting to note, retrospectively, an expensive procedure to rule out PE may have been avoided with a better understanding of the relationship between arterial and end-tidal CO 2. The probability of a PE in this case was low with a measured Et. CO 2 of 62 mm. Hg and a correlating Pa. CO 2 of 64. 9 mm. Hg. One would expect a wider gradient in the presence of significant dead space ventilation.
Discussion The continuous monitoring of Et. CO 2 and Sp. O 2 when measured in concert but evaluated independently allowed this patient to be safely observed and avoid reintubation and mechanical ventilation. It is also interesting to note, retrospectively, an expensive procedure to rule out PE may have been avoided with a better understanding of the relationship between arterial and end-tidal CO 2. The probability of a PE in this case was low with a measured Et. CO 2 of 62 mm. Hg and a correlating Pa. CO 2 of 64. 9 mm. Hg. One would expect a wider gradient in the presence of significant dead space ventilation.
 PACU, Post-op PCA, Med/Surg Floors Post operative patients on Patient Controlled Analgesia (PCA) - often starts in PACU § Bariatric Patients/Obstructive Sleep Apnea(OSA) high risk patients § Awareness building regarding the need for monitoring ventilation/breathing on general floors § Patient sentinel events/deaths – Recent professional statements (APSF, ISMP) – § Great need for more education on Oxygenation vs. Ventilation for nurses in non-acute areas
PACU, Post-op PCA, Med/Surg Floors Post operative patients on Patient Controlled Analgesia (PCA) - often starts in PACU § Bariatric Patients/Obstructive Sleep Apnea(OSA) high risk patients § Awareness building regarding the need for monitoring ventilation/breathing on general floors § Patient sentinel events/deaths – Recent professional statements (APSF, ISMP) – § Great need for more education on Oxygenation vs. Ventilation for nurses in non-acute areas
 Compelling Recent Research “During analgesia and anesthesia, cases of respiratory depression were 28 times as likely to be detected if they were monitored by capnography as those that were not” University of Alabama – Birmingham, Waugh, Epps, Khodneva - meta-analysis presented at the Society of Technology in Anesthesia International Congress, January, 2008
Compelling Recent Research “During analgesia and anesthesia, cases of respiratory depression were 28 times as likely to be detected if they were monitored by capnography as those that were not” University of Alabama – Birmingham, Waugh, Epps, Khodneva - meta-analysis presented at the Society of Technology in Anesthesia International Congress, January, 2008
 Capnography monitoring in patients receiving patient controlled analgesia (PCA)
Capnography monitoring in patients receiving patient controlled analgesia (PCA)
 Patient safety with Patient Controlled Analgesia (PCA) § § Patient Controlled Analgesia (PCA) aids patients in balancing effective pain control with sedation The risk of patient harm due to medication errors with PCA pumps is 3. 5 -times the risk of harm to a patient from any other type of medication administration error § 2004 more deaths with PCA than with all other IV infusions combined § Due to oversedation and respiratory depression with PCA delivery Sullivan M, Phillips MS, Schneider P. Patient-controlled analgesia pumps. USP Quality Review 2004; 81: 1 -3. Available on the web at: http: //www. usp. org/ pdf/patient. Safety/qr 812004 -09 -01. pdf.
Patient safety with Patient Controlled Analgesia (PCA) § § Patient Controlled Analgesia (PCA) aids patients in balancing effective pain control with sedation The risk of patient harm due to medication errors with PCA pumps is 3. 5 -times the risk of harm to a patient from any other type of medication administration error § 2004 more deaths with PCA than with all other IV infusions combined § Due to oversedation and respiratory depression with PCA delivery Sullivan M, Phillips MS, Schneider P. Patient-controlled analgesia pumps. USP Quality Review 2004; 81: 1 -3. Available on the web at: http: //www. usp. org/ pdf/patient. Safety/qr 812004 -09 -01. pdf.
 PCA Issues List § PCA by proxy § Drug product mix-ups § Device design flaws § Inadequate patient/family education § Practice issues including pump misprogramming § Inadequate monitoring ISMP Medication Safety Newsletter, July 10, 2003 Vol 8, no. 14
PCA Issues List § PCA by proxy § Drug product mix-ups § Device design flaws § Inadequate patient/family education § Practice issues including pump misprogramming § Inadequate monitoring ISMP Medication Safety Newsletter, July 10, 2003 Vol 8, no. 14
 Currently, no monitoring during PCA therapy at most hospitals § § § Post operative surgical units where there is no centralized monitoring Large units making proximity to patient impossible Vital signs are typically every 4 hours Sometimes spot checking with pulse oximetry Nurse to patient ratio can be 1: 6 – 1: 10
Currently, no monitoring during PCA therapy at most hospitals § § § Post operative surgical units where there is no centralized monitoring Large units making proximity to patient impossible Vital signs are typically every 4 hours Sometimes spot checking with pulse oximetry Nurse to patient ratio can be 1: 6 – 1: 10
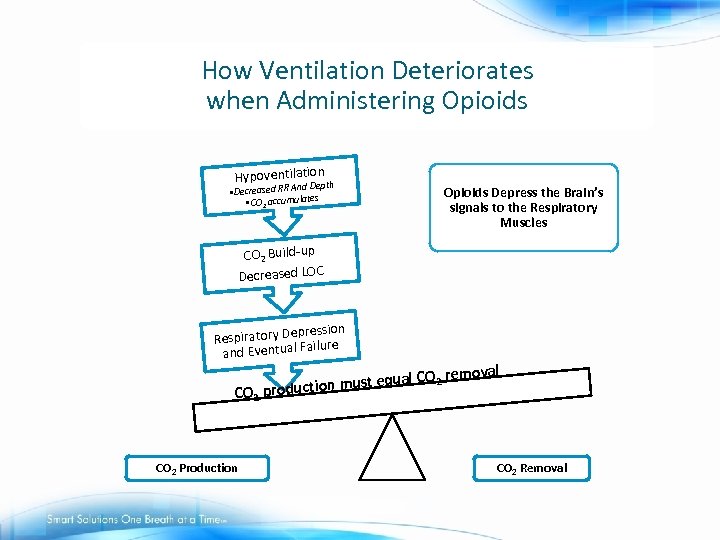 How Ventilation Deteriorates when Administering Opioids Hypoventilation h pt d De • Decreased RR An cumulates • CO 2 ac Opioids Depress the Brain’s signals to the Respiratory Muscles CO 2 Build-up Decreased LOC pression Respiratory De ilure a and Eventual F emoval ust equal CO 2 r n m CO 2 productio CO 2 Production CO 2 Removal
How Ventilation Deteriorates when Administering Opioids Hypoventilation h pt d De • Decreased RR An cumulates • CO 2 ac Opioids Depress the Brain’s signals to the Respiratory Muscles CO 2 Build-up Decreased LOC pression Respiratory De ilure a and Eventual F emoval ust equal CO 2 r n m CO 2 productio CO 2 Production CO 2 Removal
 Case scenario § 16 yr-old Billy falls off his skateboard and sustains a left femur fracture. He is now post-op from ORIF and is in the PACU extubated. He rates his pain at a 10 on 0 -10 scale and has been given multiple doses of IV Morphine and is now on a PCA pump for pain.
Case scenario § 16 yr-old Billy falls off his skateboard and sustains a left femur fracture. He is now post-op from ORIF and is in the PACU extubated. He rates his pain at a 10 on 0 -10 scale and has been given multiple doses of IV Morphine and is now on a PCA pump for pain.
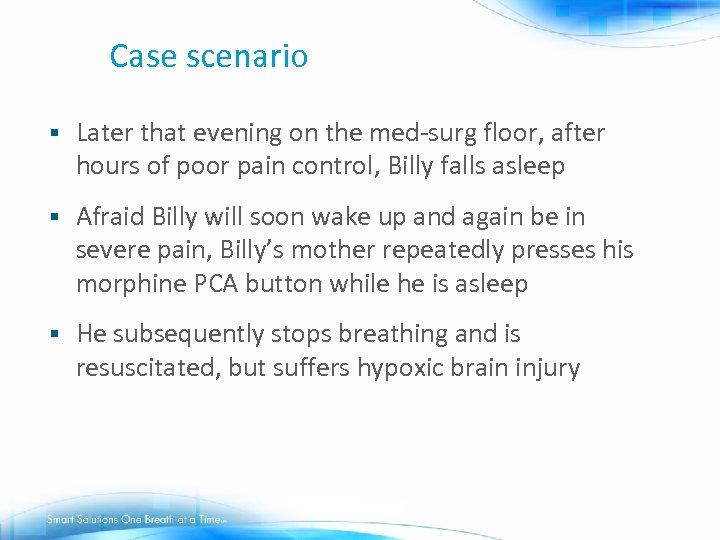 Case scenario § Later that evening on the med-surg floor, after hours of poor pain control, Billy falls asleep § Afraid Billy will soon wake up and again be in severe pain, Billy’s mother repeatedly presses his morphine PCA button while he is asleep § He subsequently stops breathing and is resuscitated, but suffers hypoxic brain injury
Case scenario § Later that evening on the med-surg floor, after hours of poor pain control, Billy falls asleep § Afraid Billy will soon wake up and again be in severe pain, Billy’s mother repeatedly presses his morphine PCA button while he is asleep § He subsequently stops breathing and is resuscitated, but suffers hypoxic brain injury
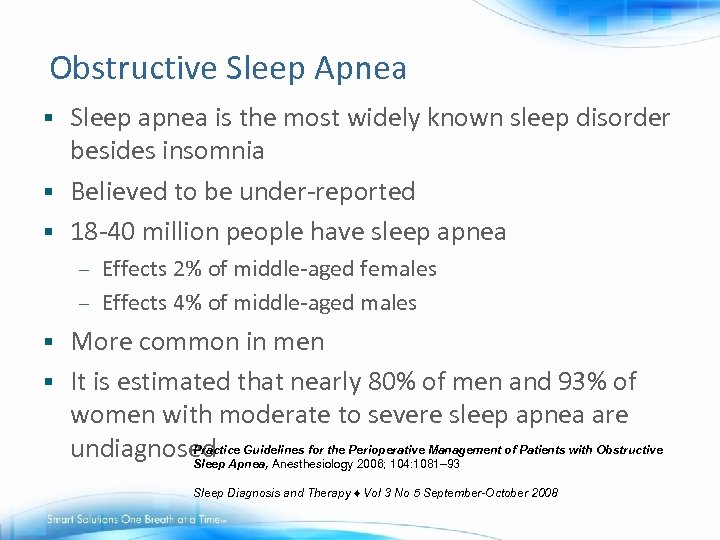 Obstructive Sleep Apnea Sleep apnea is the most widely known sleep disorder besides insomnia § Believed to be under-reported § 18 -40 million people have sleep apnea § Effects 2% of middle-aged females – Effects 4% of middle-aged males – More common in men § It is estimated that nearly 80% of men and 93% of women with moderate to severe sleep apnea are Practice Guidelines for the undiagnosed Apnea, Anesthesiology. Perioperative Management of Patients with Obstructive Sleep 2006; 104: 1081– 93 § Sleep Diagnosis and Therapy ♦ Vol 3 No 5 September-October 2008
Obstructive Sleep Apnea Sleep apnea is the most widely known sleep disorder besides insomnia § Believed to be under-reported § 18 -40 million people have sleep apnea § Effects 2% of middle-aged females – Effects 4% of middle-aged males – More common in men § It is estimated that nearly 80% of men and 93% of women with moderate to severe sleep apnea are Practice Guidelines for the undiagnosed Apnea, Anesthesiology. Perioperative Management of Patients with Obstructive Sleep 2006; 104: 1081– 93 § Sleep Diagnosis and Therapy ♦ Vol 3 No 5 September-October 2008
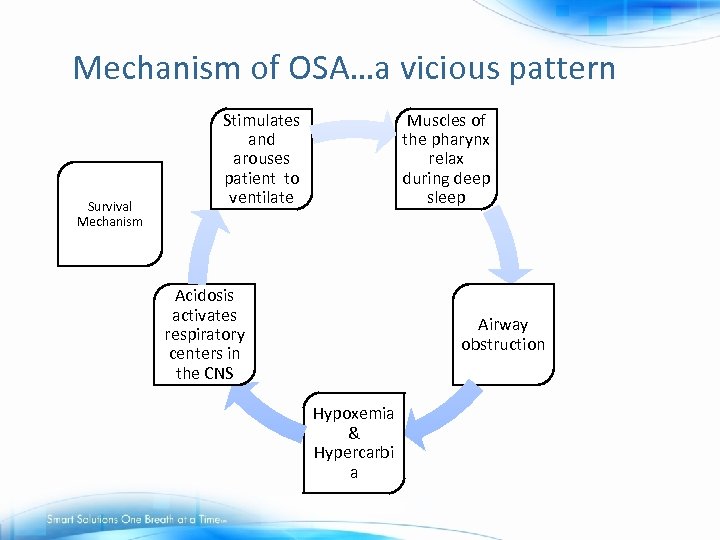 Mechanism of OSA…a vicious pattern Survival Mechanism Stimulates and arouses patient to ventilate Muscles of the pharynx relax during deep sleep Acidosis activates respiratory centers in the CNS Airway obstruction Hypoxemia & Hypercarbi a
Mechanism of OSA…a vicious pattern Survival Mechanism Stimulates and arouses patient to ventilate Muscles of the pharynx relax during deep sleep Acidosis activates respiratory centers in the CNS Airway obstruction Hypoxemia & Hypercarbi a
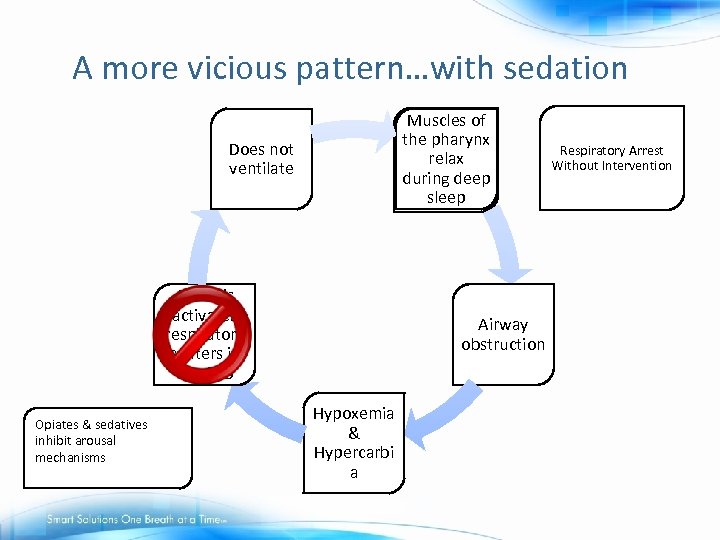 A more vicious pattern…with sedation Muscles of the pharynx relax during deep sleep Does not ventilate Acidosis activates respiratory centers in the CNS Opiates & sedatives inhibit arousal mechanisms Airway obstruction Hypoxemia & Hypercarbi a Respiratory Arrest Without Intervention
A more vicious pattern…with sedation Muscles of the pharynx relax during deep sleep Does not ventilate Acidosis activates respiratory centers in the CNS Opiates & sedatives inhibit arousal mechanisms Airway obstruction Hypoxemia & Hypercarbi a Respiratory Arrest Without Intervention
 PCA Case Scenario #2 60 year old female with morbid obesity and history of intractable low back pain § X-rays demonstrated severe bone-onbone changes in both knee and hip areas § Placed on PCA continuous infusion with PCA demand dose § Placed on continuous Sp. O 2 and Et. CO 2 monitoring §
PCA Case Scenario #2 60 year old female with morbid obesity and history of intractable low back pain § X-rays demonstrated severe bone-onbone changes in both knee and hip areas § Placed on PCA continuous infusion with PCA demand dose § Placed on continuous Sp. O 2 and Et. CO 2 monitoring §
 PCA Case Scenario #2 cont. Soon after starting PCA, patient desaturated to Sp. O 2 = 85% § Patient placed on 60% O 2 aerosol mask and Et. CO 2 monitoring discontinued § PCA continuous discontinued, PCA demand dose continued §
PCA Case Scenario #2 cont. Soon after starting PCA, patient desaturated to Sp. O 2 = 85% § Patient placed on 60% O 2 aerosol mask and Et. CO 2 monitoring discontinued § PCA continuous discontinued, PCA demand dose continued §
 PCA Case Study #2 cont. Following morning, patient appeared very lethargic and difficult to arouse § Sp. O 2 in high 90 s § Et. CO 2 monitor reapplied on patient with readings of 74 mm. Hg* indicating elevated CO 2 level § Patient was transferred to ICU with diagnosis of obstructive sleep apnea complicated by obesity and PCA §
PCA Case Study #2 cont. Following morning, patient appeared very lethargic and difficult to arouse § Sp. O 2 in high 90 s § Et. CO 2 monitor reapplied on patient with readings of 74 mm. Hg* indicating elevated CO 2 level § Patient was transferred to ICU with diagnosis of obstructive sleep apnea complicated by obesity and PCA §
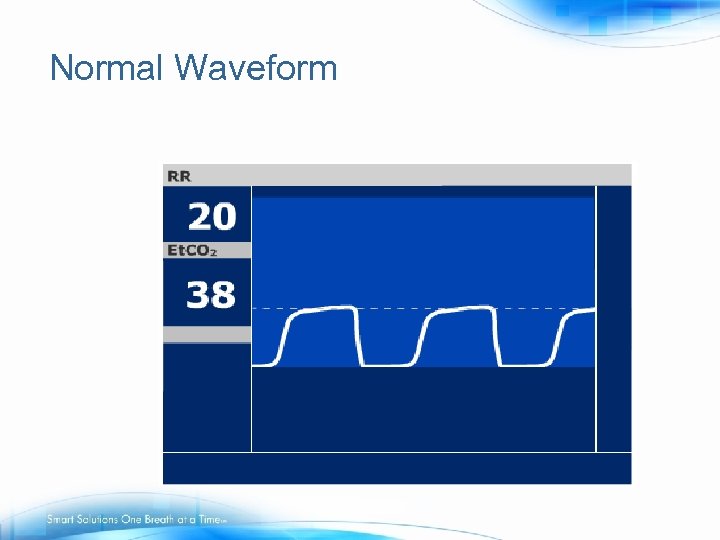 Normal Waveform
Normal Waveform
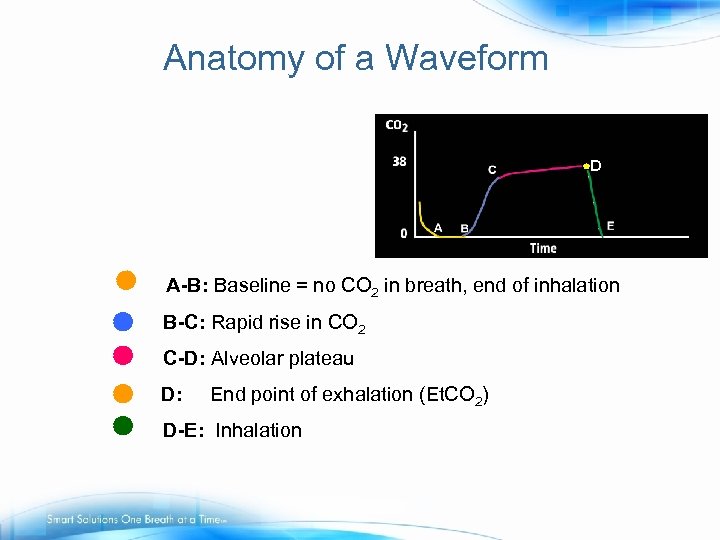 Anatomy of a Waveform D A-B: Baseline = no CO 2 in breath, end of inhalation B-C: Rapid rise in CO 2 C-D: Alveolar plateau D: End point of exhalation (Et. CO 2) D-E: Inhalation
Anatomy of a Waveform D A-B: Baseline = no CO 2 in breath, end of inhalation B-C: Rapid rise in CO 2 C-D: Alveolar plateau D: End point of exhalation (Et. CO 2) D-E: Inhalation
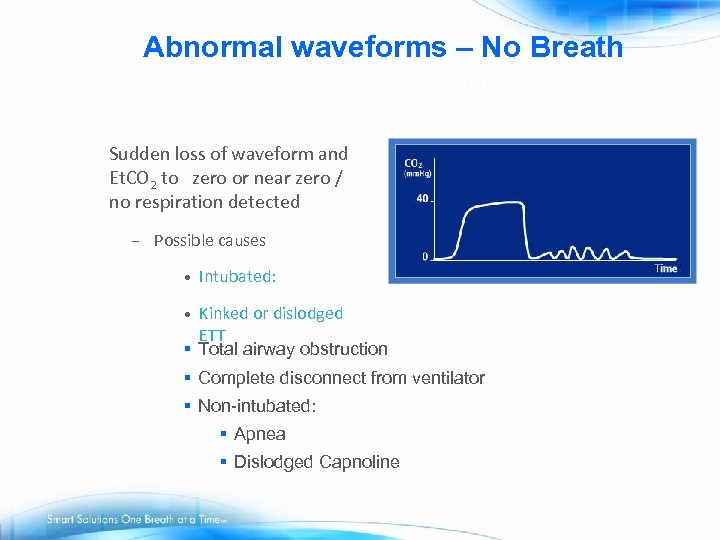 Abnormal waveforms – No Breath loss of waveform Sudden loss of waveform and Et. CO 2 to zero or near zero / no respiration detected – Possible causes • Intubated: Kinked or dislodged ETT § Total airway obstruction • § Complete disconnect from ventilator § Non-intubated: § Apnea § Dislodged Capnoline
Abnormal waveforms – No Breath loss of waveform Sudden loss of waveform and Et. CO 2 to zero or near zero / no respiration detected – Possible causes • Intubated: Kinked or dislodged ETT § Total airway obstruction • § Complete disconnect from ventilator § Non-intubated: § Apnea § Dislodged Capnoline
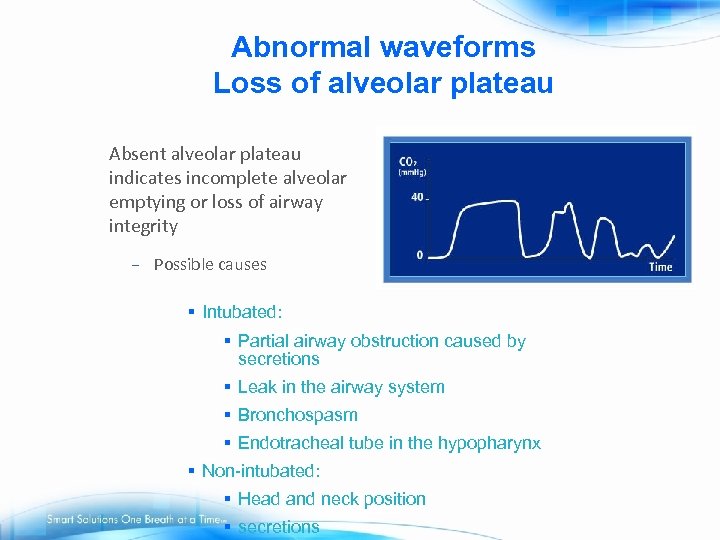 Abnormal waveforms Loss of alveolar plateau Absent alveolar plateau indicates incomplete alveolar emptying or loss of airway integrity – Possible causes § Intubated: § Partial airway obstruction caused by secretions § Leak in the airway system § Bronchospasm § Endotracheal tube in the hypopharynx § Non-intubated: § Head and neck position § secretions
Abnormal waveforms Loss of alveolar plateau Absent alveolar plateau indicates incomplete alveolar emptying or loss of airway integrity – Possible causes § Intubated: § Partial airway obstruction caused by secretions § Leak in the airway system § Bronchospasm § Endotracheal tube in the hypopharynx § Non-intubated: § Head and neck position § secretions
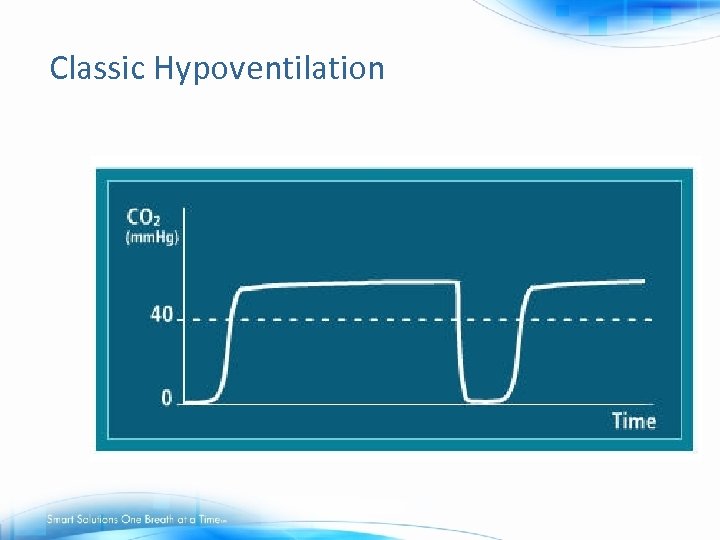 Classic Hypoventilation
Classic Hypoventilation
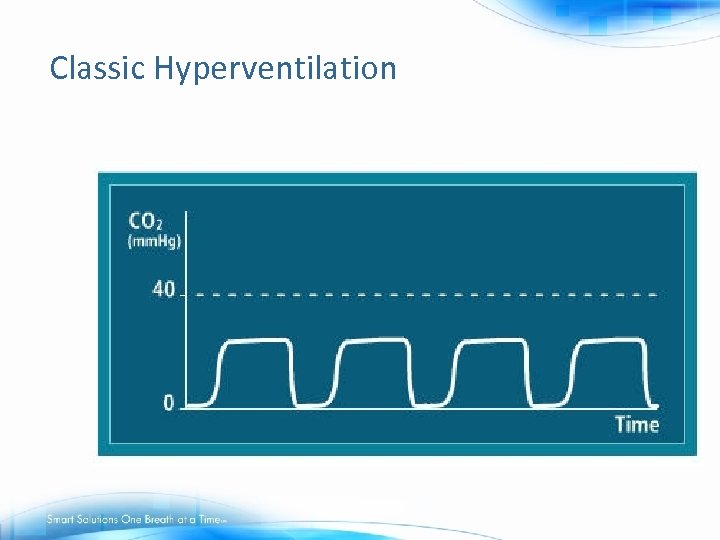 Classic Hyperventilation
Classic Hyperventilation
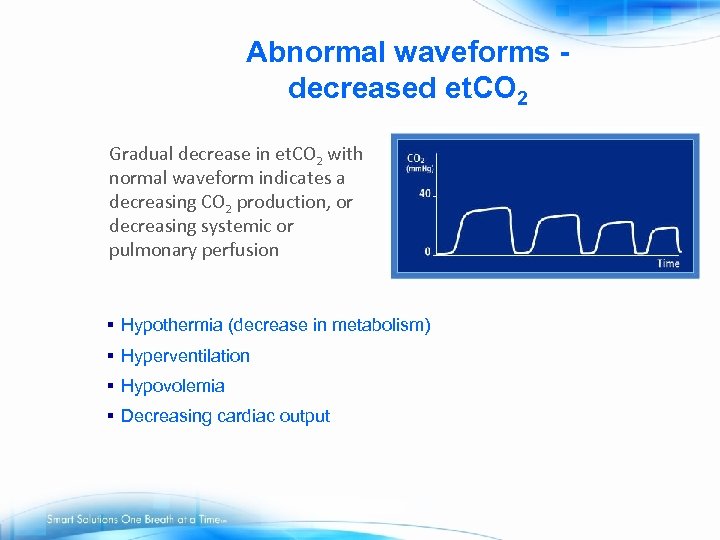 Abnormal waveforms decreased et. CO 2 Gradual decrease in et. CO 2 with normal waveform indicates a decreasing CO 2 production, or decreasing systemic or pulmonary perfusion § Hypothermia (decrease in metabolism) § Hyperventilation § Hypovolemia § Decreasing cardiac output
Abnormal waveforms decreased et. CO 2 Gradual decrease in et. CO 2 with normal waveform indicates a decreasing CO 2 production, or decreasing systemic or pulmonary perfusion § Hypothermia (decrease in metabolism) § Hyperventilation § Hypovolemia § Decreasing cardiac output
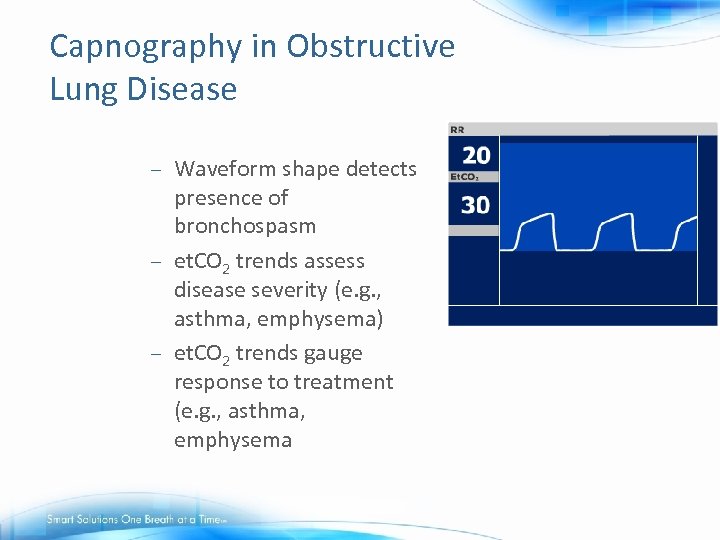 Capnography in Obstructive Lung Disease Waveform shape detects presence of bronchospasm – et. CO 2 trends assess disease severity (e. g. , asthma, emphysema) – et. CO 2 trends gauge response to treatment (e. g. , asthma, emphysema –
Capnography in Obstructive Lung Disease Waveform shape detects presence of bronchospasm – et. CO 2 trends assess disease severity (e. g. , asthma, emphysema) – et. CO 2 trends gauge response to treatment (e. g. , asthma, emphysema –
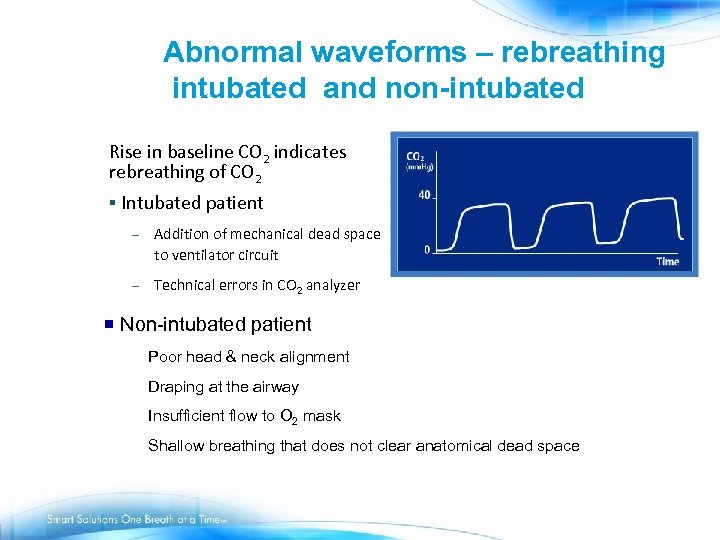 Abnormal waveforms – rebreathing intubated and non-intubated Rise in baseline CO 2 indicates rebreathing of CO 2 § Intubated patient – Addition of mechanical dead space to ventilator circuit – Technical errors in CO 2 analyzer ¡ Non-intubated patient Poor head & neck alignment Draping at the airway Insufficient flow to O 2 mask Shallow breathing that does not clear anatomical dead space
Abnormal waveforms – rebreathing intubated and non-intubated Rise in baseline CO 2 indicates rebreathing of CO 2 § Intubated patient – Addition of mechanical dead space to ventilator circuit – Technical errors in CO 2 analyzer ¡ Non-intubated patient Poor head & neck alignment Draping at the airway Insufficient flow to O 2 mask Shallow breathing that does not clear anatomical dead space
 Abnormal Waveforms – What to do § § § Assess patient Check sample line position – reposition or check ET tube position Check head/neck alignment, and open airway, suction if needed Instruct patient to take a deep breath If patient is not breathing and not
Abnormal Waveforms – What to do § § § Assess patient Check sample line position – reposition or check ET tube position Check head/neck alignment, and open airway, suction if needed Instruct patient to take a deep breath If patient is not breathing and not
 Movers and Shakers / Clinical Compass
Movers and Shakers / Clinical Compass
 ‘The monitoring used in the PACU should be appropriate to the patient’s condition and a full range of monitoring devices should be available’. Canadian Anesthesiologists’ Society, R. Merchant, et al Revised edition 2010
‘The monitoring used in the PACU should be appropriate to the patient’s condition and a full range of monitoring devices should be available’. Canadian Anesthesiologists’ Society, R. Merchant, et al Revised edition 2010
 Institute for Safe Medication Practices (ISMP) § “Do not rely on pulse oximetry readings alone to detect opiate toxicity. Use capnography to detect respiratory changes caused by opiates, especially for patients who are at high risk (e. g. , patients with sleep apnea, obese patients). ” – Establish guidelines for appropriate monitoring of patients who are receiving opiates, including frequent assessment of the quality of respirations (not just respiratory rate) and specific signs of oversedation. ISMP Medication Safety Alert, February 22, 2007, Vol. 12, Issue 4
Institute for Safe Medication Practices (ISMP) § “Do not rely on pulse oximetry readings alone to detect opiate toxicity. Use capnography to detect respiratory changes caused by opiates, especially for patients who are at high risk (e. g. , patients with sleep apnea, obese patients). ” – Establish guidelines for appropriate monitoring of patients who are receiving opiates, including frequent assessment of the quality of respirations (not just respiratory rate) and specific signs of oversedation. ISMP Medication Safety Alert, February 22, 2007, Vol. 12, Issue 4
 ASA (American Society of Anesthesiologists) Practice guidelines for the perioperative management of patients with obstructive sleep apnea CO 2 monitoring should be used during moderate or deep sedation for patients with OSA. If moderate sedation is used, ventilation should be continuously monitored by capnography or another automated method if feasible because of the increased risk of undetected airway obstruction in these patients. Postoperative Management: OSA patients should be monitored for a median of 3 hours longer than the non-OSA counterparts before discharge. Monitoring of OSA patients should continue for a median of 7 hours after the last episode of airway obstruction or hypoxemia. Practice guidelines for the perioperative management of patients with obstructive sleep apnea: a report by the American Society of Anesthesiologists Task Force on Perioperative Management of Patients with Obstructive Sleep Apnea. Anesthesiology 2006 May; 104(5): 1081 -93
ASA (American Society of Anesthesiologists) Practice guidelines for the perioperative management of patients with obstructive sleep apnea CO 2 monitoring should be used during moderate or deep sedation for patients with OSA. If moderate sedation is used, ventilation should be continuously monitored by capnography or another automated method if feasible because of the increased risk of undetected airway obstruction in these patients. Postoperative Management: OSA patients should be monitored for a median of 3 hours longer than the non-OSA counterparts before discharge. Monitoring of OSA patients should continue for a median of 7 hours after the last episode of airway obstruction or hypoxemia. Practice guidelines for the perioperative management of patients with obstructive sleep apnea: a report by the American Society of Anesthesiologists Task Force on Perioperative Management of Patients with Obstructive Sleep Apnea. Anesthesiology 2006 May; 104(5): 1081 -93
 Conclusion § Capnography for sedation/analgesia/postoperative monitoring: – – – Accurately monitors RR Monitors adequate ventilation Monitors hypoventilation due to over-sedation more effectively than pulse oximetry Earliest indicator of apnea and obstruction Adds additional level of safety providing caregiver with objective information to make accurate assessments and timely interventions
Conclusion § Capnography for sedation/analgesia/postoperative monitoring: – – – Accurately monitors RR Monitors adequate ventilation Monitors hypoventilation due to over-sedation more effectively than pulse oximetry Earliest indicator of apnea and obstruction Adds additional level of safety providing caregiver with objective information to make accurate assessments and timely interventions
 Be Prepared. Be Proactive
Be Prepared. Be Proactive
 Continuing Capnography Education § Oridion Knowledge Center: www. capnographyeducation. com § Three capnography courses available: A Guide to Capnography during Procedural Sedation – A Guide to Capnography in the Management of the Critically Ill – A Guide to Monitoring et. CO 2 during Opioid Delivery –
Continuing Capnography Education § Oridion Knowledge Center: www. capnographyeducation. com § Three capnography courses available: A Guide to Capnography during Procedural Sedation – A Guide to Capnography in the Management of the Critically Ill – A Guide to Monitoring et. CO 2 during Opioid Delivery –


