a0485da7abdc743b149d154c5fd67eb2.ppt
- Количество слайдов: 29

CALL ME ANYTIME: BENEFITS OF 911 AND GETTING TO THE RIGHT PLACE MACK HUTCHISON, BS, AS, NREMT-P QUALITY MANAGER
HISTORY OF EMS The good Samaritan rendered aid to a man laying on the side of the road. Napoleon’s chief physician was the first to develop Pre-Hospital care in 1797. The United States first recognized the need for Pre -Hospital care after the first year of the Civil War.
HISTORY OF EMS 1971, the hit television show “Emergency” caught the attention of the public prompting growing concern for their health. 1985, Trauma became a concern for EMS
STROKE FACTS • Every 45 seconds someone in America has a stroke. • About 700, 000 Americans will have a new or recurrent stroke this year and over 163, 000 of them will die (making it the third leading cause of death in the USA). • There approximately 266, 000 stroke survivors with permanent disabilities.
MORE STROKE FACTS • Fewer than one in five Americans can identify even one stroke symptom. • The economic impact of stroke is estimated to cost $40 -$70 billion per year. • A stroke can be devastating, that's why it's so important to minimize your risk. “CALL 911”
CASE PRESENTATION After returning home from the supermarket, a woman finds her 67 -year-old husband in the kitchen with slurred speech and left-sided weakness. He was acting normally when she left the house earlier that evening. She immediately calls her friend across the street to ask for help. The friend arrives a few minutes later only to find that the patient’s symptoms are getting worse. They decide to call 911. EMS personnel arrive within 5 minutes of the call. Paramedics evaluate the patient and are concerned that the patient may be having a stroke. What are the important elements of the pre-hospital management of potential stroke patients?
STROKE PRESENTATION OBJECTIVES: • Describe the importance of rapid detection of CVA/TIA symptoms in the pre-hospital setting • Describe why extensive neurological examinations are inappropriate in the prehospital setting • Differentiate a Primary Stroke Center from a Comprehensive Stroke Center
PRE-HOSPITAL MANAGEMENT OF STROKE • • Detection Dispatch Delivery Door
PRE-HOSPITAL EMERGENCY CARE 1999 • A lack of awareness/understanding of TIAs • A common sentiment that strokes could be managed non-emergently • Less than half of survey participants were aware of the 3 -hour time window for IV t. PA.
TIME OF SYMPTOM ONSET • • • Question multiple sources Actual time of symptoms vs. symptoms noticed How normal were they? Symptom onset: stuttering vs. acute Baseline level of neurological function
PRE-HOSPITAL CARE • • Airway, Breathing, Circulation Assess vital signs Neurologic exam Check serum blood sugar Determine time of onset Oxygen, IV, Monitor Notify the ED quickly
WHAT NOT TO DO • • Do not delay transport. • • • Do not give dextrose (unless hypoglycemic). Do not give large volumes of fluid (unless the patient is in shock). Do not lower blood pressure. Do not forget to determine time of onset.
IDENTIFY TIME “LAST SEEN NORMAL” • • A 75 year old man with HTN and diabetes finishes dinner with a friend at 8 pm. He drives himself the short distance home that night, and a daughter stops by the next morning to find him still in bed and with right side weakness and severe aphasia. When do we assume the stoke occurred? (Answer: ? ? A 35 year old hypertensive man who is known to be non-compliant with meds is found slumped over in his car in a job site parking area at 3 pm. In the ED he was found to have a massive left hemispheric ischemic stroke. His wife said he left for work at 7 am that morning as normal, and she had a clear and normal cell phone conversation with him at 12: 30 pm. At 1 pm a co-worker stated the man said he wasn’t feeling well and was going to his car to rest. At the time the coworker noticed his speech was slurred. What time can we use as the time “last seen normal”? (Answer: ? ? )
CASE OUTCOME When the paramedics arrived, their first action was to evaluate the patient’s airway, breathing, and circulation status. Since these were found to be adequate, the patient’s vital signs were then assessed. The results were as follows: blood pressure = 180/96, heart rate = 106, and respiratory rate = 22. While one paramedic then acquired some history from the patient’s wife, the other paramedic performed a concise physical examination which included a Glasgow Coma Score (GCS) and a pre-hospital stroke scale assessment.
CASE OUTCOME (CONT’D)……. Based upon the wife’s account, her husband was acting normally 45 minutes earlier when she went grocery shopping. He has never had symptoms like this before and is otherwise a very healthy person. She did not know what to do, so she called her friend across the street. By the time she arrived, he was getting worse, so she called 911. By this time, the second paramedic has determined that the patient has a GCS of 13 (E 4 V 3 M 6). The pre-hospital stroke scale reveals the presence of left-sided facial droop, left-sided arm drift, and slurred speech.
CASE OUTCOME (CONT’D)……. . The paramedics then measure the patient’s blood sugar and oxygen saturation. Both are found to be normal. They explain to the patient’s wife that her husband appears to be having a stroke. Time is critical, and they encourage her to come with them since her assistance may be needed. The patient is promptly transferred to the ambulance. While enroute to the hospital, an IV is established, and the patient is placed on a cardiac monitor and low flow oxygen. The receiving hospital is contacted during the patient’s transport. Upon their arrival at the Emergency Department, the staff have already vacated a room and the physician begins evaluating the patient immediately.
WHY YOU SHOULD CALL 911 FOR A STROKE 1. Dispatchers will offer you verbal instructions. 2. Treatment begins when the paramedic arrives. 3. The ambulance is the most appropriate and safest means of transportation. 4. Inbound radio reports allow the hospital to get ready. 5. You are transported to the closest appropriate hospital.
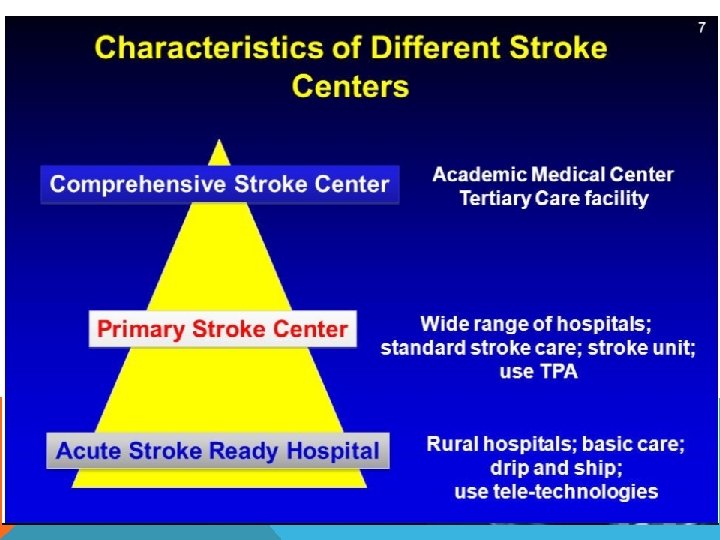
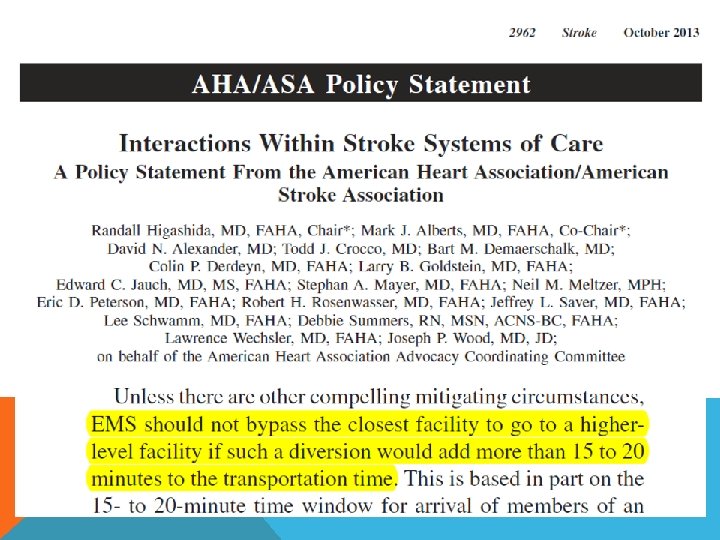
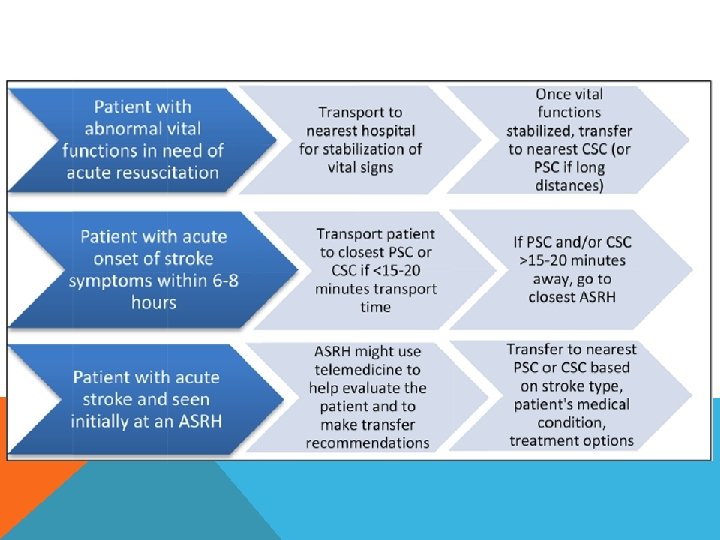
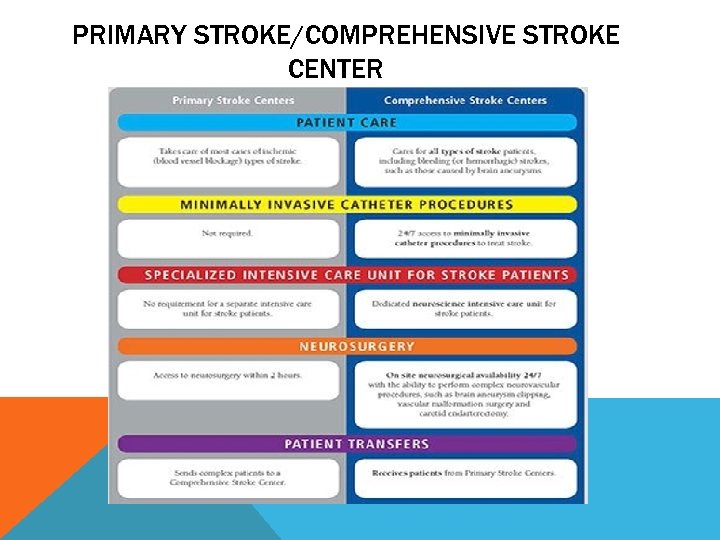
PRIMARY STROKE/COMPREHENSIVE STROKE CENTER
Over triage Patient taken to CSC who doesn’t need it delays t. PA and starves PSC/ASRH - Volume ~ Outcomes Under triage Patient not taken to CSC who needs it delays endovascular care or neurosurgery - Transfer times for STEMI/Trauma
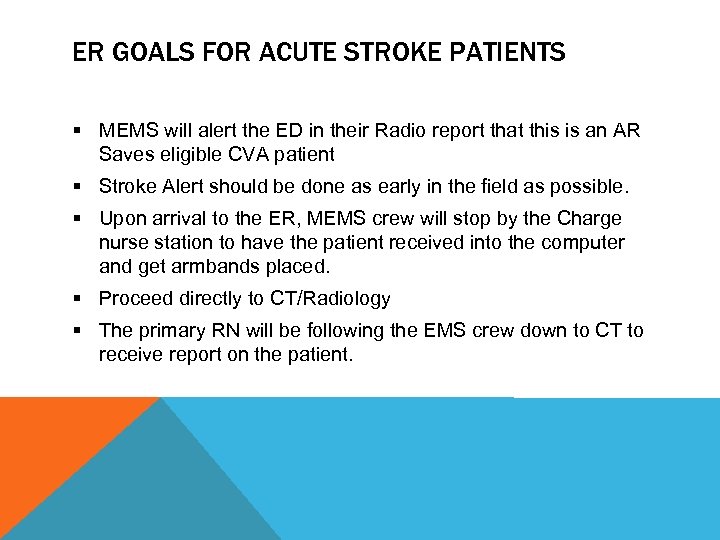
ER GOALS FOR ACUTE STROKE PATIENTS § MEMS will alert the ED in their Radio report that this is an AR Saves eligible CVA patient § Stroke Alert should be done as early in the field as possible. § Upon arrival to the ER, MEMS crew will stop by the Charge nurse station to have the patient received into the computer and get armbands placed. § Proceed directly to CT/Radiology § The primary RN will be following the EMS crew down to CT to receive report on the patient.
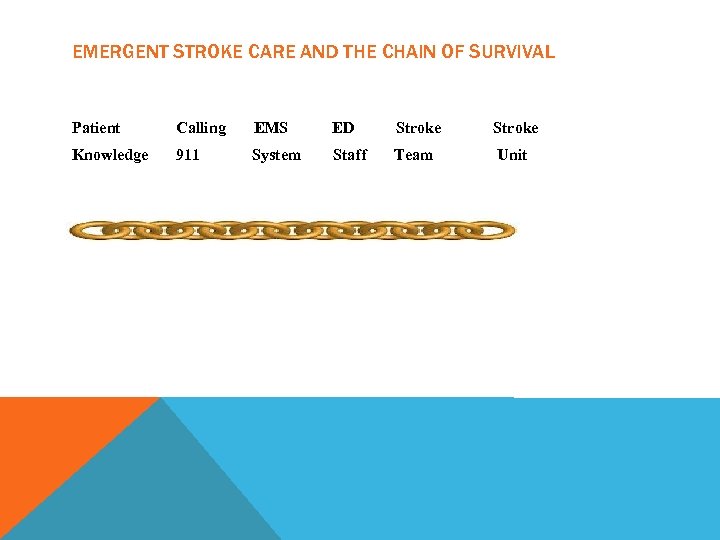
EMERGENT STROKE CARE AND THE CHAIN OF SURVIVAL Patient Calling EMS ED Stroke Knowledge 911 System Staff Team Unit
MYTHS OF EMS *I can get to the hospital before an ambulance arrives! *The ambulance is not going to do anything but take me to the hospital! FACTS OF EMS *Ambulance crews are trained to deal with the medical emergency that you are going to the hospital for. *Ambulances provide some of the same life-saving care that patients in emergency rooms will receive. *If you or your loved one go unconscious enroute to the hospital…. what’s your plan?
SUMMARY: • If you have signs of a stroke, the ambulance is the best option for you. • Treatment starts when you call. • Treatment continues all the way to the hospital. • This sets up the best potential outcome for you!
GOT QUESTIONS? THANKS!. . MACK HUTCHISON – MEMS QA MANAGER
a0485da7abdc743b149d154c5fd67eb2.ppt