073ff8bf446021170969be30afa8d837.ppt
- Количество слайдов: 43

Burden of Disease Research Unit WHO-FIC Collaborating Centre (Under designation) Cause of death statistics from vital registration Debbie Bradshaw
Outline of presentation • Illustrate the public health value of cause of death statistics – City of Cape Town • Process of collecting cause of death statistics • ascertaining the cause of death • underlying cause of death • ICD coding • cause of death statistics • Quality of cause of death certification
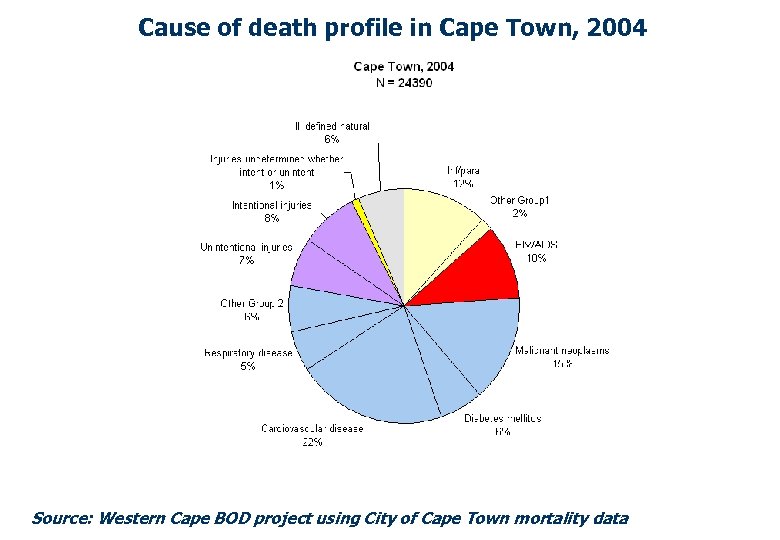
Cause of death profile in Cape Town, 2004 Source: Western Cape BOD project using City of Cape Town mortality data

Age specific HIV death rates, Cape Town 2001 - 2006 Source: Western Cape BOD project using City of Cape Town mortality data
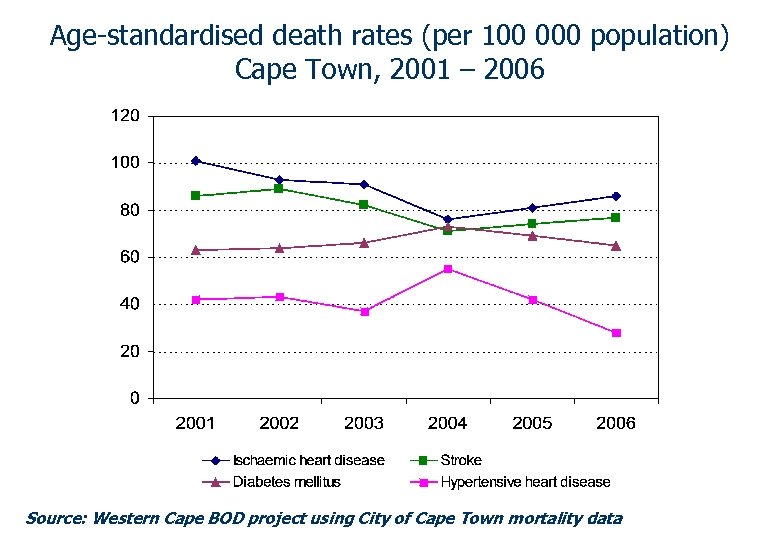
Age-standardised death rates (per 100 000 population) Cape Town, 2001 – 2006 Source: Western Cape BOD project using City of Cape Town mortality data
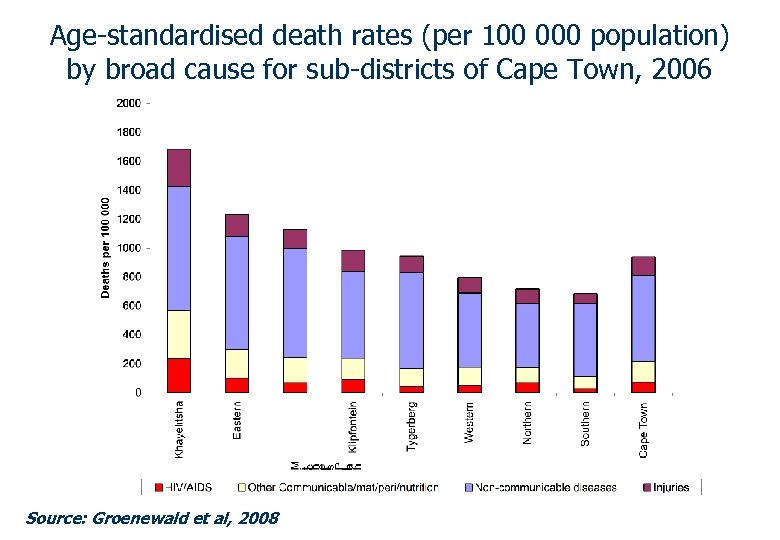
Age-standardised death rates (per 100 000 population) by broad cause for sub-districts of Cape Town, 2006 Source: Groenewald et al, 2008
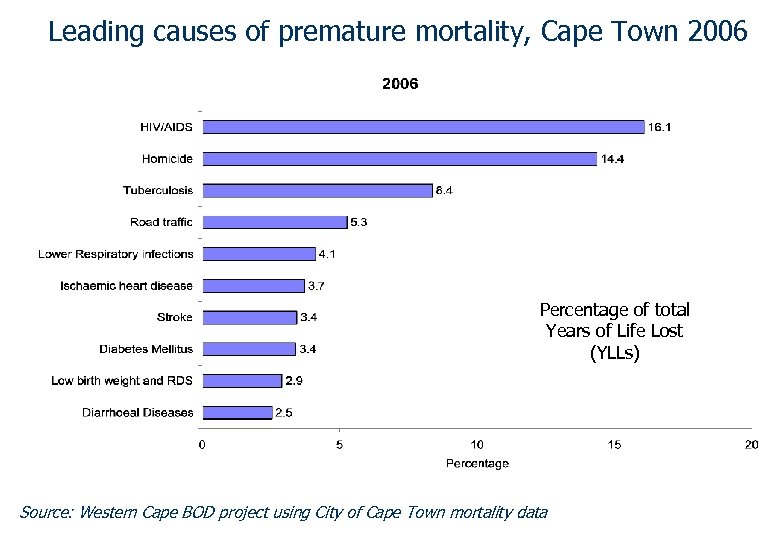
Leading causes of premature mortality, Cape Town 2006 Percentage of total Years of Life Lost (YLLs) Source: Western Cape BOD project using City of Cape Town mortality data
Public health importance of mortality data • Monitor the health of the population – Leading causes of death – Mortality rates (geographic variations) – Trends over time • Inform decisions about health policy and strategy – Prevent premature deaths – Service provision – Health budgets • Evaluate health service outcomes
Main stages in production of cause of death statistics Attending doctor: • Establish diagnosis • Complete death certificate (International form – WHO) Coding by Statistical Office: • Code causes of death (ICD code for each cause listed) • Classify cause of death (select a single underlying cause of death for stats according to ICD selection rules) • Check validity, query Analysis by Statistical Office: • Tabulate and disseminate data Source: Adapted from Johansson LA, 2008

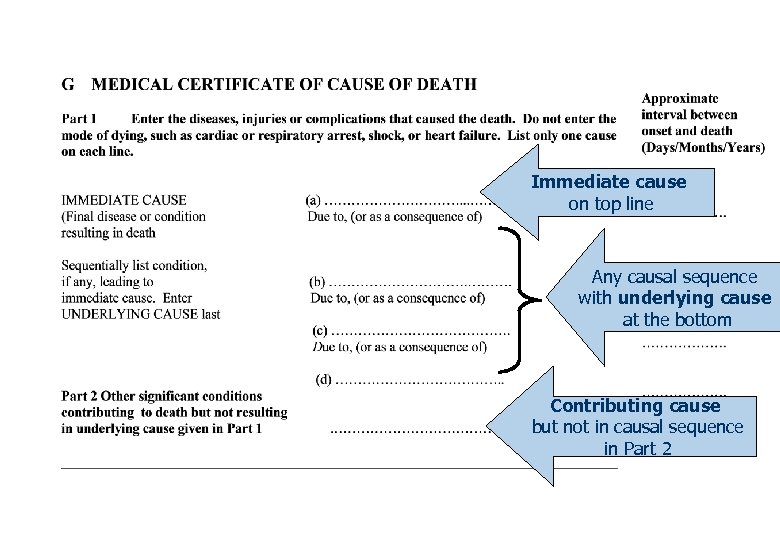
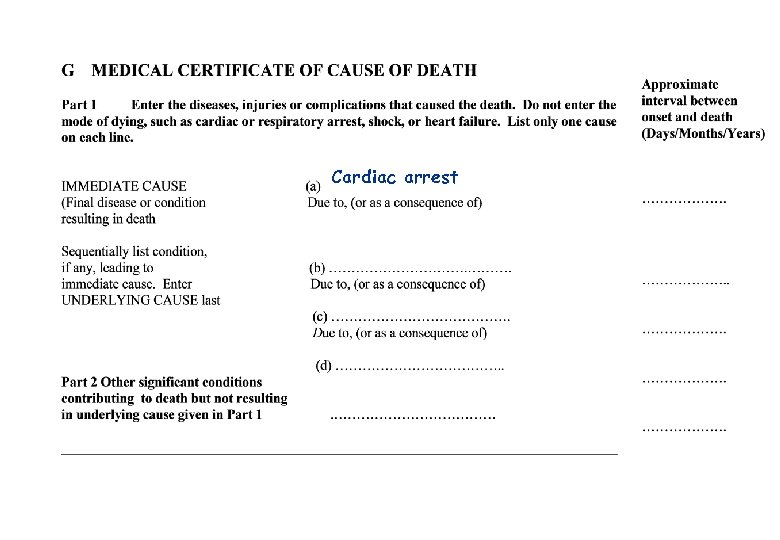
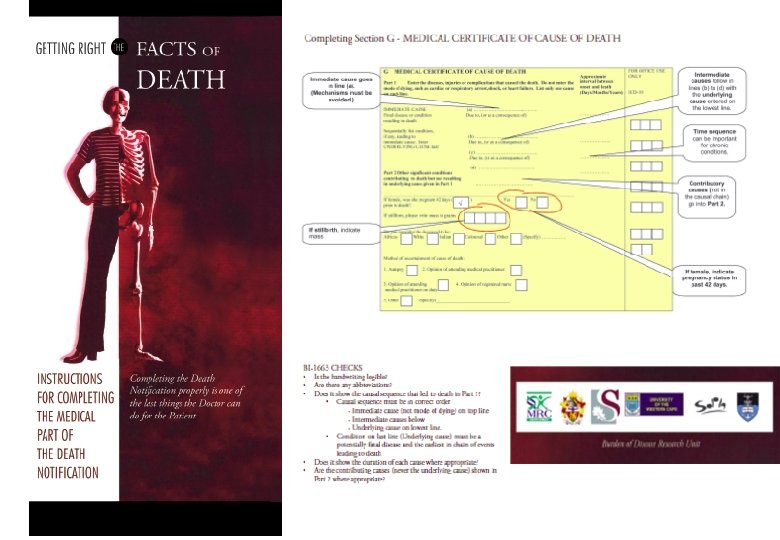
Immediate cause on top line Any causal sequence with underlying cause at the bottom Contributing cause but not in causal sequence in Part 2
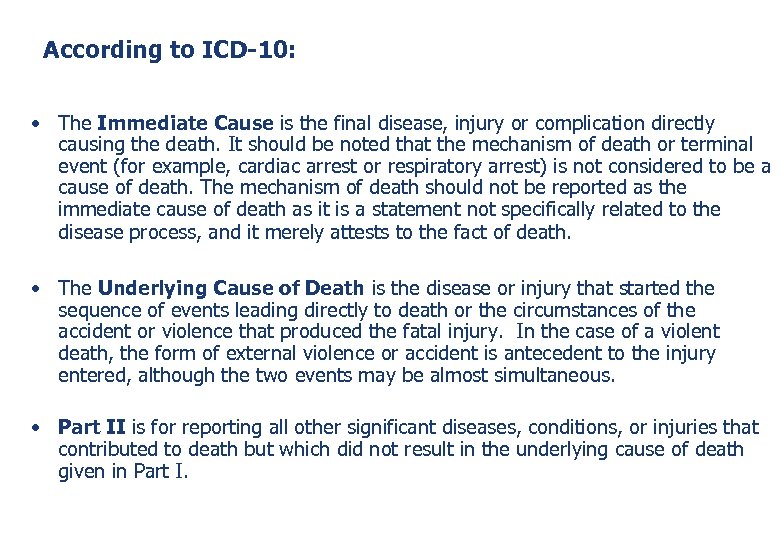
According to ICD-10: • The Immediate Cause is the final disease, injury or complication directly causing the death. It should be noted that the mechanism of death or terminal event (for example, cardiac arrest or respiratory arrest) is not considered to be a cause of death. The mechanism of death should not be reported as the immediate cause of death as it is a statement not specifically related to the disease process, and it merely attests to the fact of death. • The Underlying Cause of Death is the disease or injury that started the sequence of events leading directly to death or the circumstances of the accident or violence that produced the fatal injury. In the case of a violent death, the form of external violence or accident is antecedent to the injury entered, although the two events may be almost simultaneous. • Part II is for reporting all other significant diseases, conditions, or injuries that contributed to death but which did not result in the underlying cause of death given in Part I.
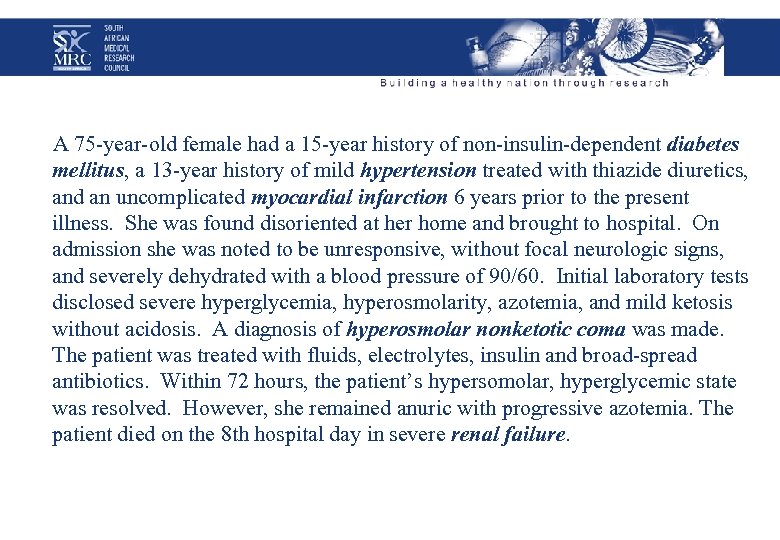
A 75 -year-old female had a 15 -year history of non-insulin-dependent diabetes mellitus, a 13 -year history of mild hypertension treated with thiazide diuretics, and an uncomplicated myocardial infarction 6 years prior to the present illness. She was found disoriented at her home and brought to hospital. On admission she was noted to be unresponsive, without focal neurologic signs, and severely dehydrated with a blood pressure of 90/60. Initial laboratory tests disclosed severe hyperglycemia, hyperosmolarity, azotemia, and mild ketosis without acidosis. A diagnosis of hyperosmolar nonketotic coma was made. The patient was treated with fluids, electrolytes, insulin and broad-spread antibiotics. Within 72 hours, the patient’s hypersomolar, hyperglycemic state was resolved. However, she remained anuric with progressive azotemia. The patient died on the 8 th hospital day in severe renal failure.
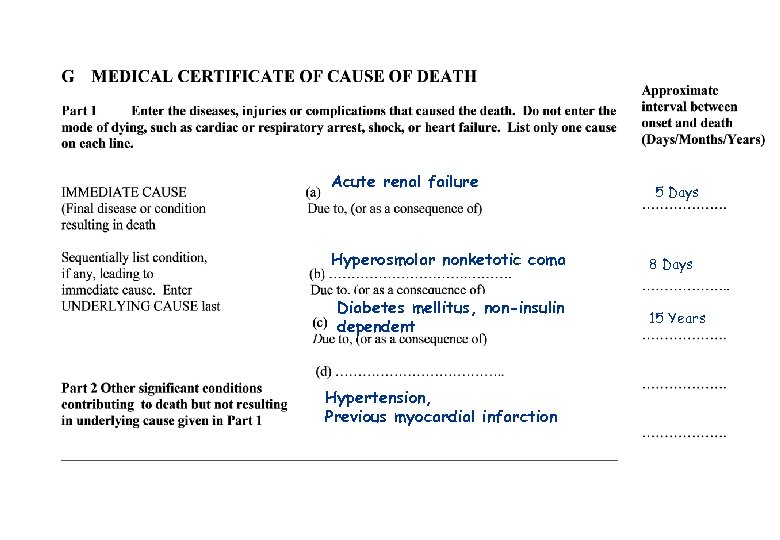
Acute renal failure Hyperosmolar nonketotic coma Diabetes mellitus, non-insulin dependent Hypertension, Previous myocardial infarction 5 Days 8 Days 15 Years
Female aged 77 years, stumbled and fell over while cleaning the house and sustained a fracture of the neck of the left femur. She had an operation for insertion of a pin the following day. Four weeks later her condition deteriorated, she developed hypostatic pneumonia and died two days later.
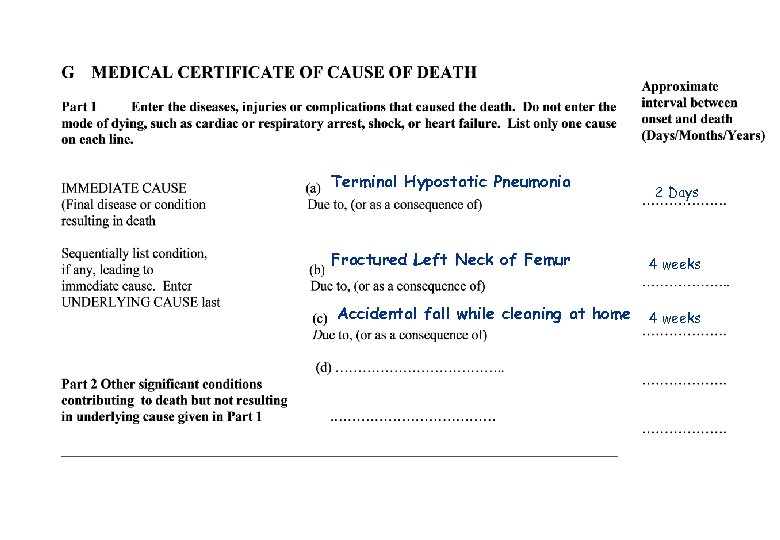
Terminal Hypostatic Pneumonia Fractured Left Neck of Femur Accidental fall while cleaning at home 2 Days 4 weeks
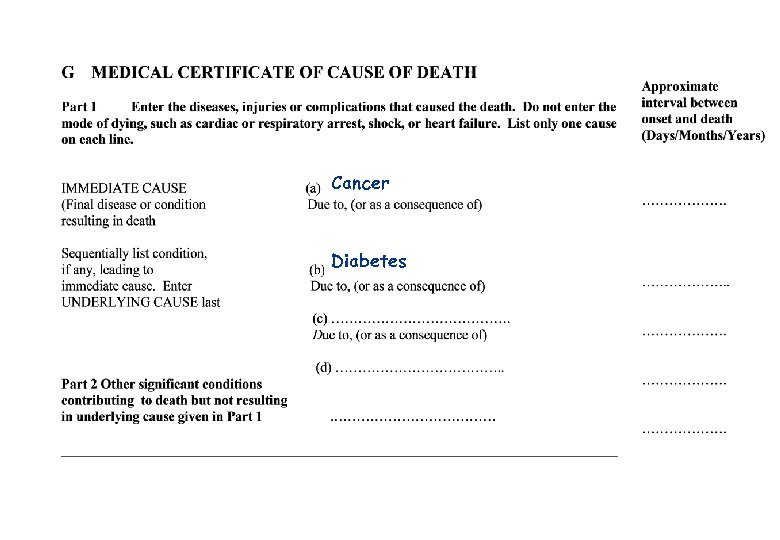
Cancer Diabetes
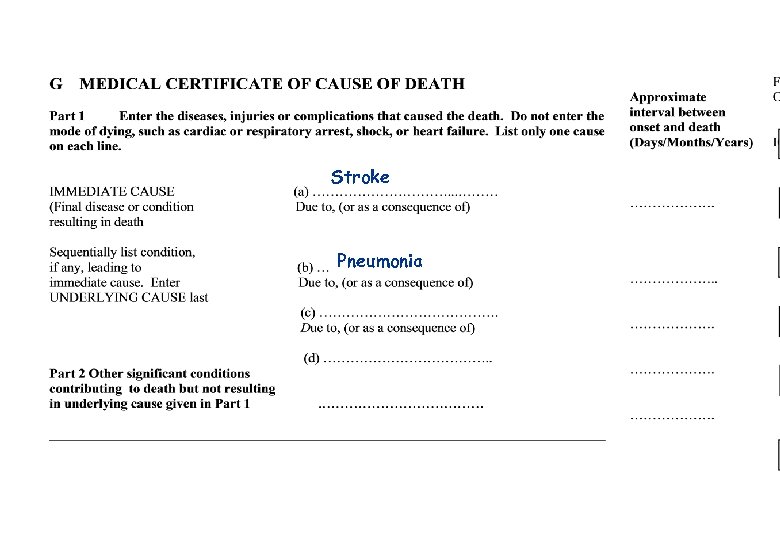
Stroke Pneumonia
Cardiac arrest
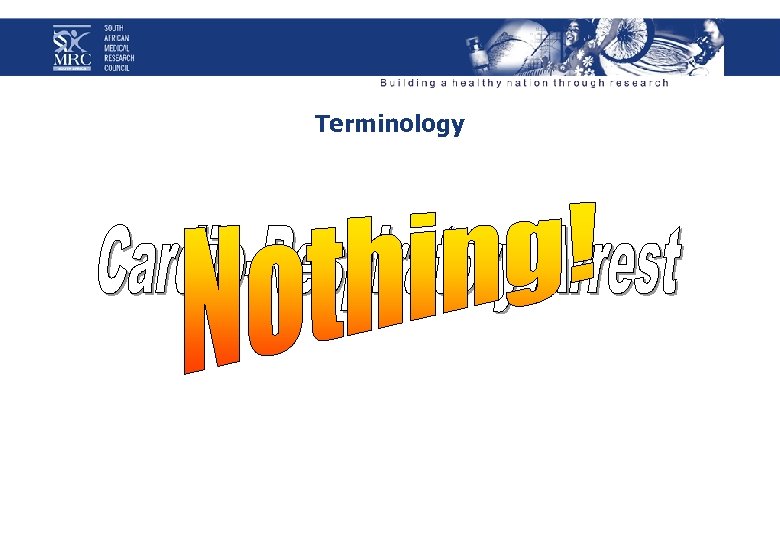
Terminology
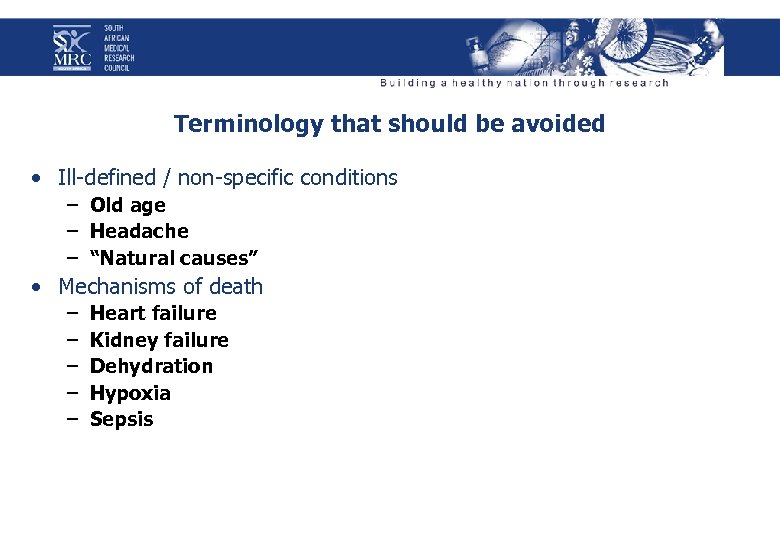
Terminology that should be avoided • Ill-defined / non-specific conditions – Old age – Headache – “Natural causes” • Mechanisms of death – – – Heart failure Kidney failure Dehydration Hypoxia Sepsis
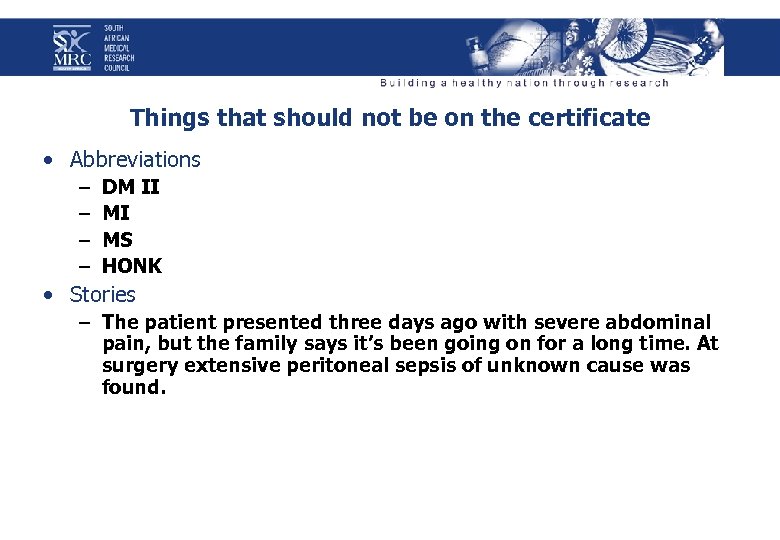
Things that should not be on the certificate • Abbreviations – – DM II MI MS HONK • Stories – The patient presented three days ago with severe abdominal pain, but the family says it’s been going on for a long time. At surgery extensive peritoneal sepsis of unknown cause was found.
Things that should not be on the death certificate
In the case of Human Immunodeficiency Virus – Check hospital notes for HIV-tests or treatment – Underlying COD: Human immunodeficiency virus – Intermediate COD: Acquired Immunodeficiency syndrome – Immediate COD: Tuberculosis / Cryptococcal Meningitis, etc.
Processing information from the medical certificate • Code each cause according to the International Statistical Classification of Diseases and Related Health Problems (ICD -10) • Apply ICD-10 rules to establish the Underlying cause of death • Check the validity of the information – and query or correct • Check consistency of data eg prostate cancer for female
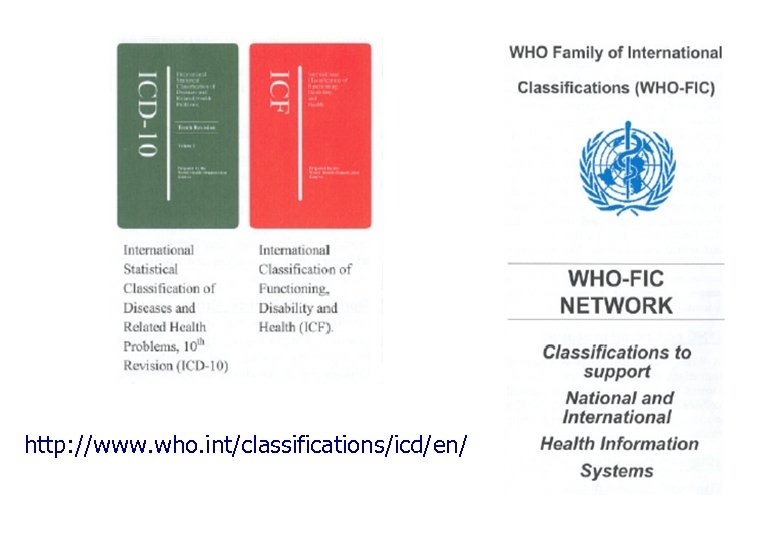
http: //www. who. int/classifications/icd/en/
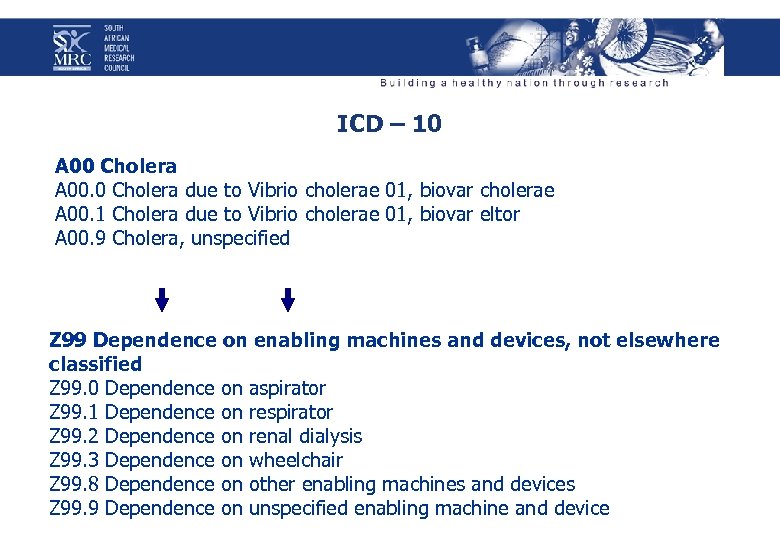
ICD – 10 A 00 Cholera A 00. 0 Cholera due to Vibrio cholerae 01, biovar cholerae A 00. 1 Cholera due to Vibrio cholerae 01, biovar eltor A 00. 9 Cholera, unspecified Z 99 Dependence on enabling machines and devices, not elsewhere classified Z 99. 0 Dependence on aspirator Z 99. 1 Dependence on respirator Z 99. 2 Dependence on renal dialysis Z 99. 3 Dependence on wheelchair Z 99. 8 Dependence on other enabling machines and devices Z 99. 9 Dependence on unspecified enabling machine and device
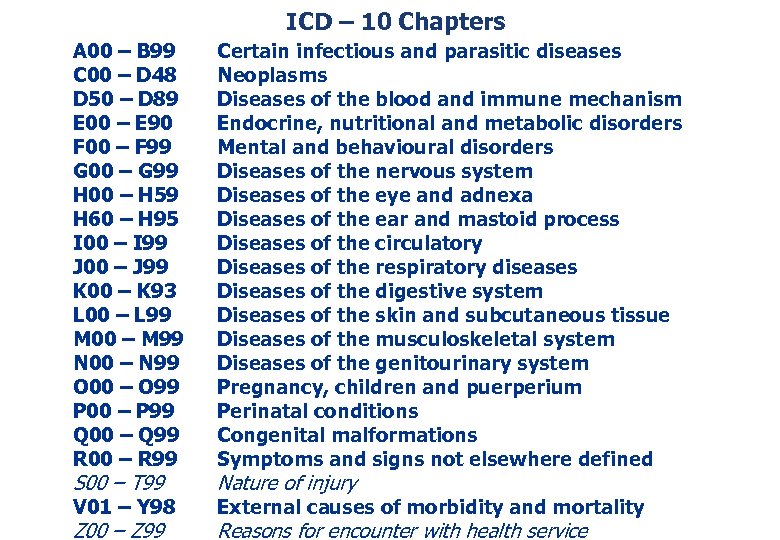
ICD – 10 Chapters A 00 – B 99 C 00 – D 48 D 50 – D 89 E 00 – E 90 F 00 – F 99 G 00 – G 99 H 00 – H 59 H 60 – H 95 I 00 – I 99 J 00 – J 99 K 00 – K 93 L 00 – L 99 M 00 – M 99 N 00 – N 99 O 00 – O 99 P 00 – P 99 Q 00 – Q 99 R 00 – R 99 Certain infectious and parasitic diseases Neoplasms Diseases of the blood and immune mechanism Endocrine, nutritional and metabolic disorders Mental and behavioural disorders Diseases of the nervous system Diseases of the eye and adnexa Diseases of the ear and mastoid process Diseases of the circulatory Diseases of the respiratory diseases Diseases of the digestive system Diseases of the skin and subcutaneous tissue Diseases of the musculoskeletal system Diseases of the genitourinary system Pregnancy, children and puerperium Perinatal conditions Congenital malformations Symptoms and signs not elsewhere defined V 01 – Y 98 External causes of morbidity and mortality S 00 – T 99 Z 00 – Z 99 Nature of injury Reasons for encounter with health service
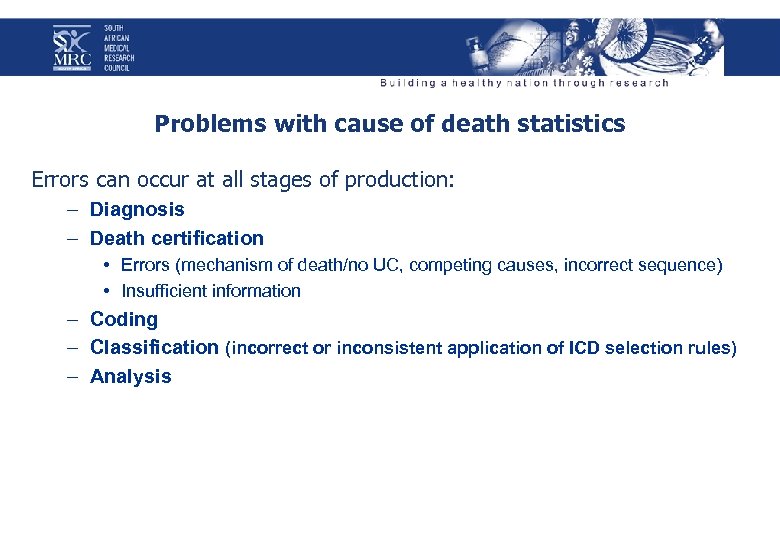
Problems with cause of death statistics Errors can occur at all stages of production: – Diagnosis – Death certification • Errors (mechanism of death/no UC, competing causes, incorrect sequence) • Insufficient information – Coding – Classification (incorrect or inconsistent application of ICD selection rules) – Analysis
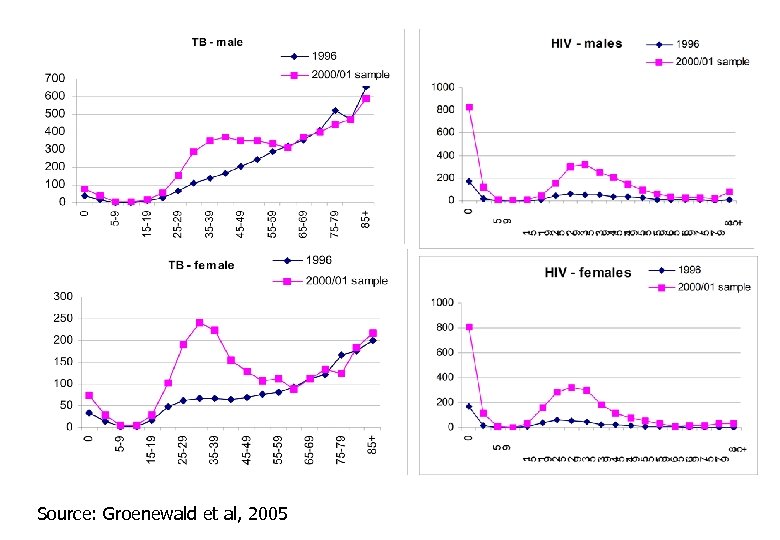
Source: Groenewald et al, 2005
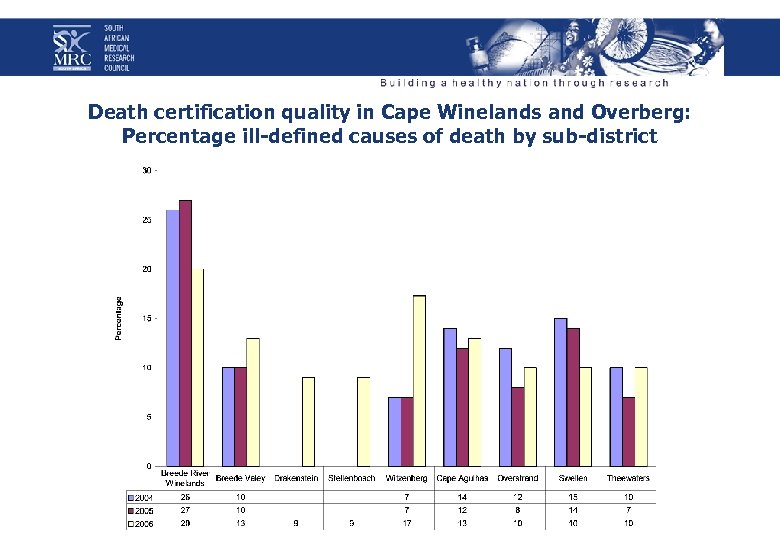
Death certification quality in Cape Winelands and Overberg: Percentage ill-defined causes of death by sub-district
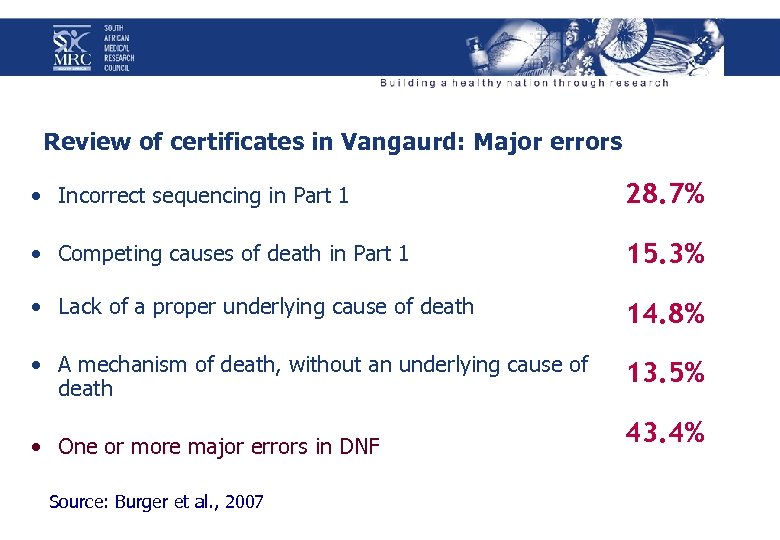
Review of certificates in Vangaurd: Major errors • Incorrect sequencing in Part 1 28. 7% • Competing causes of death in Part 1 15. 3% • Lack of a proper underlying cause of death 14. 8% • A mechanism of death, without an underlying cause of death 13. 5% • One or more major errors in DNF Source: Burger et al. , 2007 43. 4%
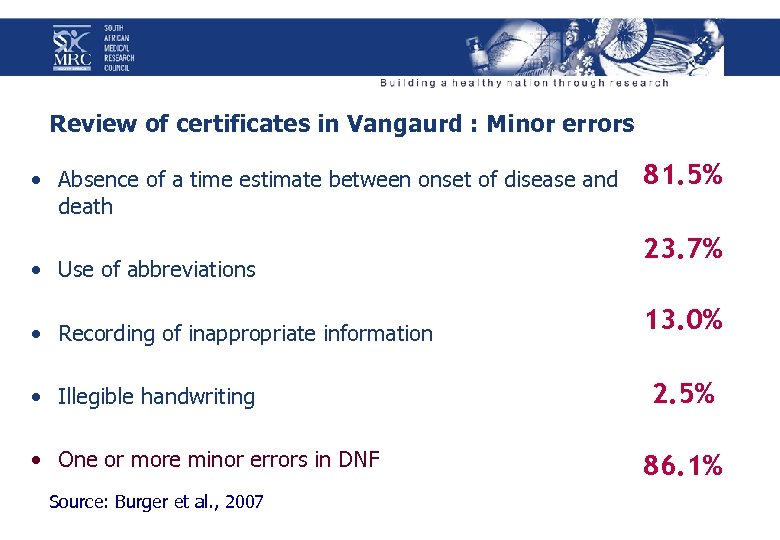
Review of certificates in Vangaurd : Minor errors • Absence of a time estimate between onset of disease and death • Use of abbreviations • Recording of inappropriate information • Illegible handwriting • One or more minor errors in DNF Source: Burger et al. , 2007 81. 5% 23. 7% 13. 0% 2. 5% 86. 1%
In total 91, 7% of cases had at least one error!!
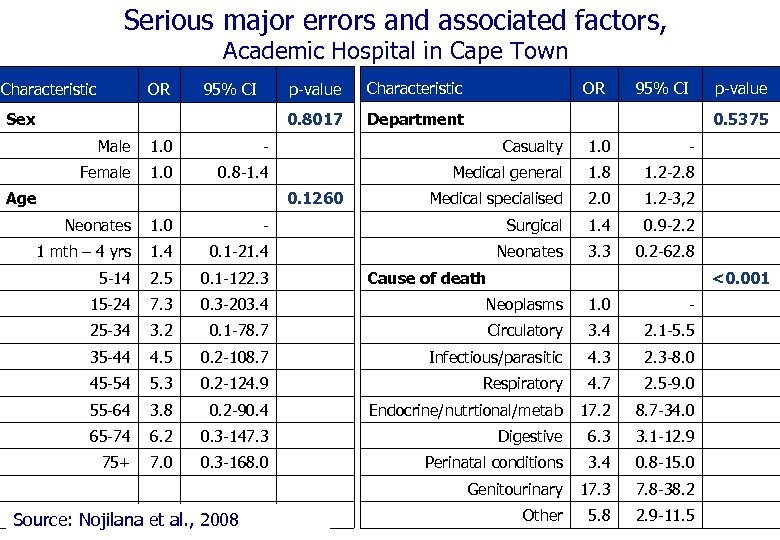
Serious major errors and associated factors, Academic Hospital in Cape Town OR p-value 95% CI Sex Characteristic 0. 8017 Characteristic OR 95% CI Department p-value 0. 5375 Male 1. 0 - Casualty 1. 0 - Female 1. 0 0. 8 -1. 4 Medical general 1. 8 1. 2 -2. 8 Medical specialised 2. 0 1. 2 -3, 2 Age 0. 1260 Neonates 1. 0 - Surgical 1. 4 0. 9 -2. 2 1 mth – 4 yrs 1. 4 0. 1 -21. 4 Neonates 3. 3 0. 2 -62. 8 5 -14 2. 5 0. 1 -122. 3 15 -24 7. 3 0. 3 -203. 4 Neoplasms 1. 0 - 25 -34 3. 2 0. 1 -78. 7 Circulatory 3. 4 2. 1 -5. 5 35 -44 4. 5 0. 2 -108. 7 Infectious/parasitic 4. 3 2. 3 -8. 0 45 -54 5. 3 0. 2 -124. 9 Respiratory 4. 7 2. 5 -9. 0 55 -64 3. 8 0. 2 -90. 4 Endocrine/nutrtional/metab 17. 2 8. 7 -34. 0 65 -74 6. 2 0. 3 -147. 3 Digestive 6. 3 3. 1 -12. 9 75+ 7. 0 0. 3 -168. 0 Perinatal conditions 3. 4 0. 8 -15. 0 Genitourinary 17. 3 7. 8 -38. 2 Other 5. 8 2. 9 -11. 5 Source: Nojilana et al. , 2008 Cause of death <0. 001
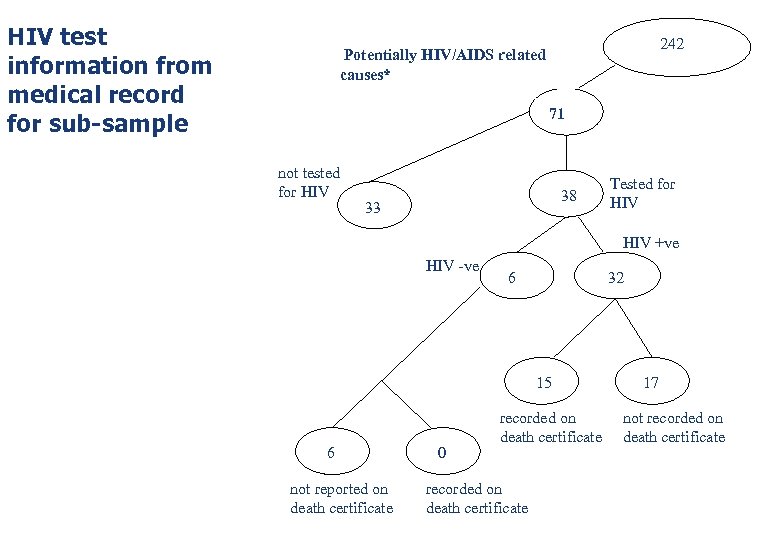
HIV test information from medical record for sub-sample 242 Potentially HIV/AIDS related causes* 71 not tested for HIV 38 33 Tested for HIV +ve HIV -ve 32 6 15 6 not reported on death certificate 0 recorded on death certificate 17 not recorded on death certificate
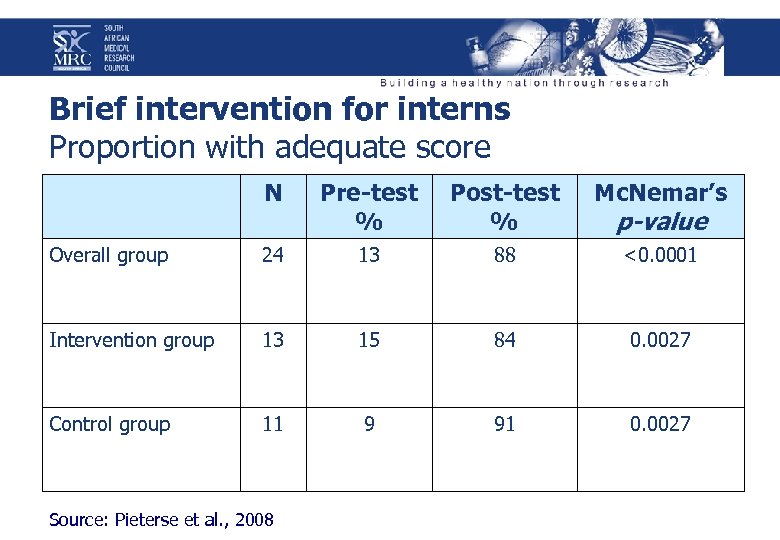
Brief intervention for interns Proportion with adequate score N Pre-test % Post-test % Mc. Nemar’s Overall group 24 13 88 <0. 0001 Intervention group 13 15 84 0. 0027 Control group 11 9 91 0. 0027 Source: Pieterse et al. , 2008 p-value
http: //who. int/bookorders www. healthmetricsnetwork. org healthmetrics@who. int
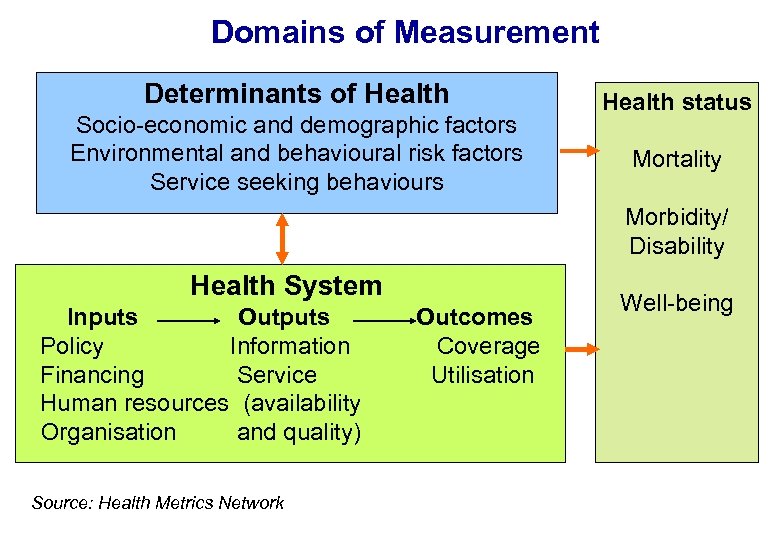
Domains of Measurement Determinants of Health Socio-economic and demographic factors Environmental and behavioural risk factors Service seeking behaviours Health status Mortality Morbidity/ Disability Health System Inputs Outputs Policy Information Financing Service Human resources (availability Organisation and quality) Source: Health Metrics Network Outcomes Coverage Utilisation Well-being
http: //www. who. int/classifications/icd/en/
Acknowledgement BOD Unit and collaborators Dr Pam Groenewald Dr Lene Burger Ms Desiree Pieterse Ms Beatrice Nojilana WHO-FIC Collaborating Centre Ms Lyn Hanmer Dr Pam Groenewald Mr Malute Tshivase Ms Margie Schneider Prof Jenny Jelsma Mr David Bourne Me Sedick Isaacs Local, provincial and national government City of Cape Town Western Cape Department of Health Department of Home Affairs Statistics South Africa
073ff8bf446021170969be30afa8d837.ppt