df973cf2a42039cf949bb158b0169bae.ppt
- Количество слайдов: 30
Building Physician Support for Trauma Care Best Practices in Community Hospitals Greg Bishop, President Bishop+ Associates June 2004
Building Physician Support for Trauma Care Best Practices in Community Hospitals n Problems, Factors & Principles n Improving Trauma Medical Staff Value n Cost-Effective Trauma Physician Support n Arriving At Fair Trauma Physician Compensation n Specialty Issues & Market Norms
Problems, Factors & Principles n Problematic Physician Structures n Multiple Contributing Factors n Principles For Proceeding
Problematic Physician Structures n Fragile, Complex Structures n Serious Shortages, Few In Pipeline n Costs, Closures, Weak & Unstable Structures n Balkans of Hospital/Physician Relations
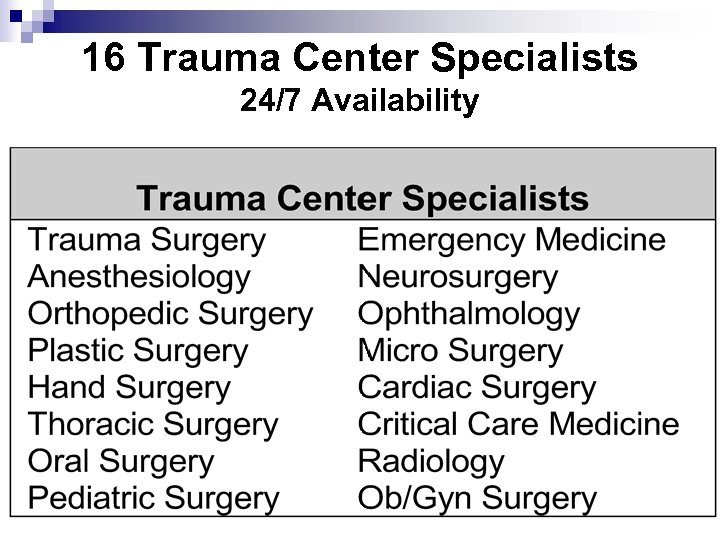
16 Trauma Center Specialists 24/7 Availability
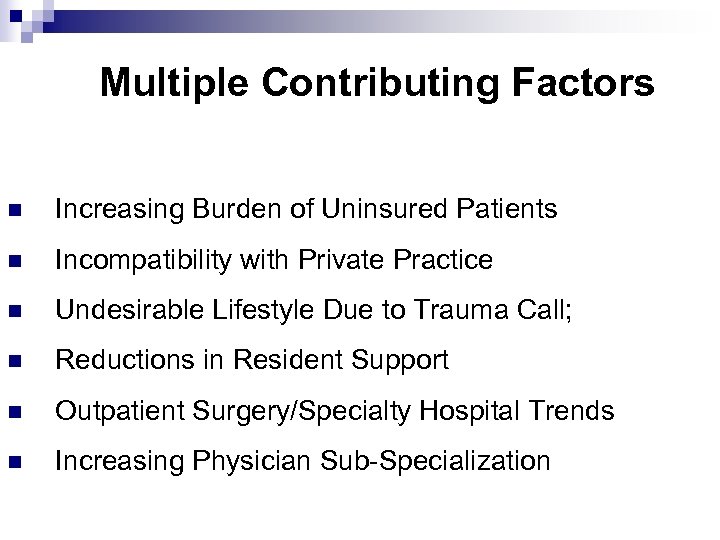
Multiple Contributing Factors n Increasing Burden of Uninsured Patients n Incompatibility with Private Practice n Undesirable Lifestyle Due to Trauma Call; n Reductions in Resident Support n Outpatient Surgery/Specialty Hospital Trends n Increasing Physician Sub-Specialization
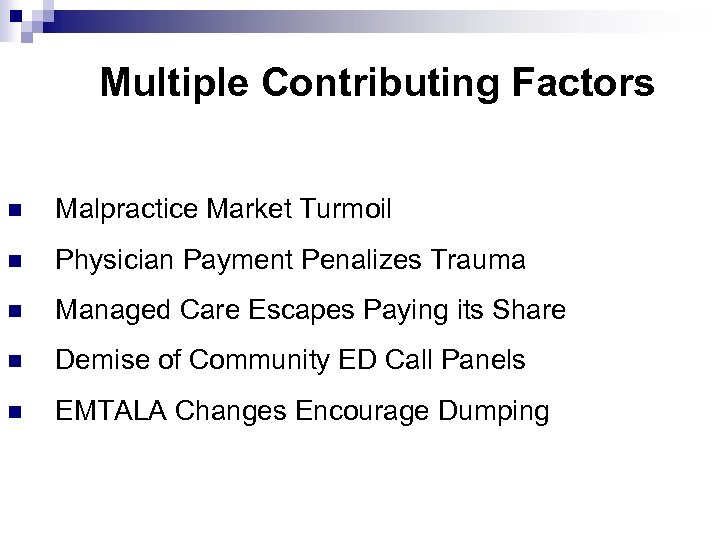
Multiple Contributing Factors n Malpractice Market Turmoil n Physician Payment Penalizes Trauma n Managed Care Escapes Paying its Share n Demise of Community ED Call Panels n EMTALA Changes Encourage Dumping
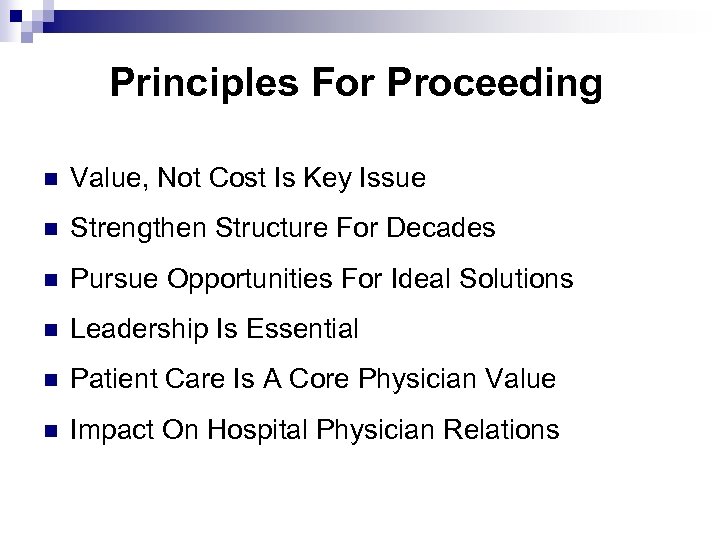
Principles For Proceeding n Value, Not Cost Is Key Issue n Strengthen Structure For Decades n Pursue Opportunities For Ideal Solutions n Leadership Is Essential n Patient Care Is A Core Physician Value n Impact On Hospital Physician Relations
Improving Value In Trauma Care Strengthening Trauma Program n Quality of Care; Responsiveness n Maintaining Verification Status n QA, CME, Protocols n Cost effectiveness; Reduced LOS n Community Outreach & Injury Prevention n Public Advocate for Optimal Trauma Care
Improving Value In Trauma Care Strengthening Hospital n Surgical Critical Care Program n Ortho & Neuro Centers of Excellence n Orthopedic Hospitalist Model n Hospital/Physician Relations n ED/OR/ICU Issues n Trauma Center Halo Effect
Framework For Cost Effective Trauma Physician Support n Effective Structure n Hospital Support n Optimal Franchise n Trauma Physician Compensation n Dealing With Leverage
Effective Structure n Strong Trauma Medical Leadership n Strong Trauma Service n Make Trauma Call Less Burdensome ¨ Only Call in Specialty When Needed ¨ Have Patient Ready When Specialist Arrives ¨ Don’t Make Specialists Wait for Diagnostic Results ¨ Implement Tiered Call System; Facial Fracture Panels
Hospital Support n OR Block Time n ED Throughput n Physician Assistants n Nurse Practitioners n Other
Optimize Franchise n Trauma/SICU/Surgery n Hospital Based Orthopedic Program n Establishment of Centers of Excellence n Halo Effect for both Physicians and Hospital
Trauma Physician Compensation n Trauma Medical Director Compensation n Payment on Uninsured Patients n Call Stipends; In-house call versus on-call n Response Fees/Complex Schemes n Consolidated Trauma Physician Billing Support n Net Annual Hospital Cost (NAHC)
Dealing With Leverage n Balkans Revisited n Stark Provides Constraint n Do Not Form A Cartel n Compliance Is A Serious Issue
Arriving At Fair Compensation n Key Payment Factors n Employment vs. Contracting n Data and Market Norms n Process is Key
Key Payment Factors n Lack of Residency n Volume of Uninsured n Role versus Value Provided n In-House Call versus On-Call n Trauma Volume +/-
Employment vs. Contracting n Contract With Group For Service/Employment Of Trauma Specialist n Hospital Employment of Surgeons n Contract with Individual Surgeons
Data & Market Norms n Data Sources n Comparison to Salary Data n Specialty Outliers n Payment on Uninsured
Dealing With Leverage n Balkans Revisited n Stark Provides Constraint n Do Not Form A Cartel n Compliance Is A Serious Issue
Process Is Key n Do Not Ignore Requests n Effective Hospital Leadership n Benchmark Trauma Financial Performance n Solicit Specialty Input n Address Non-Financial Issues n Define Fair Level of Compensation
Specialty Issues & Market Norms n Trauma Surgery n Neurosurgery n Orthopedic Surgery n Plastic Surgery n Low Volume Specialties n Hospital Based Specialties
Trauma Surgery n Key Issues: ¨ ¨ n Core of Trauma Center Highest impact specialty Frontline and patient care manager roles Franchise Value Market Norms ¨ ¨ ¨ Most Trauma Surgeons within Community Hospitals Receive Hospital Support In-House Call $1000 -$2500 per day On-Call $500 -$1500 per day
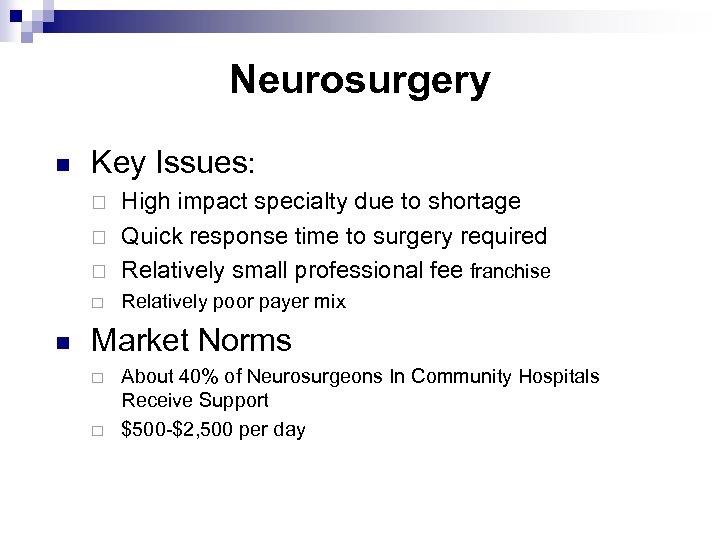
Neurosurgery n Key Issues: ¨ High impact specialty due to shortage Quick response time to surgery required Relatively small professional fee franchise ¨ Relatively poor payer mix ¨ ¨ n Market Norms ¨ ¨ About 40% of Neurosurgeons In Community Hospitals Receive Support $500 -$2, 500 per day
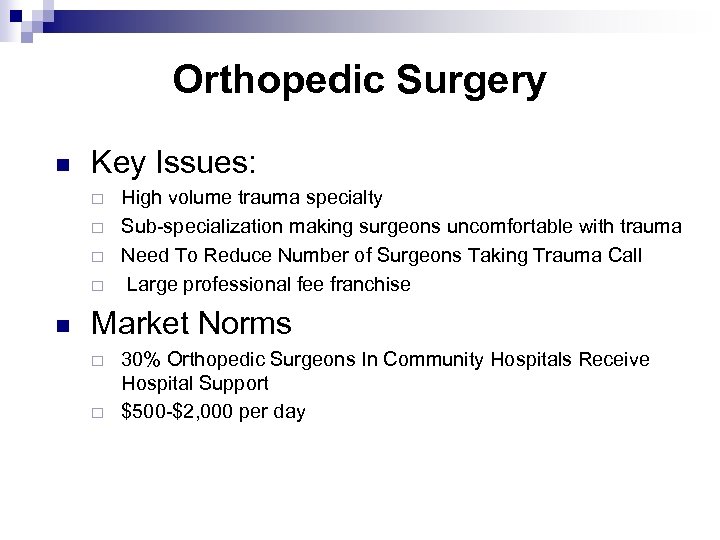
Orthopedic Surgery n Key Issues: ¨ ¨ n High volume trauma specialty Sub-specialization making surgeons uncomfortable with trauma Need To Reduce Number of Surgeons Taking Trauma Call Large professional fee franchise Market Norms ¨ ¨ 30% Orthopedic Surgeons In Community Hospitals Receive Hospital Support $500 -$2, 000 per day
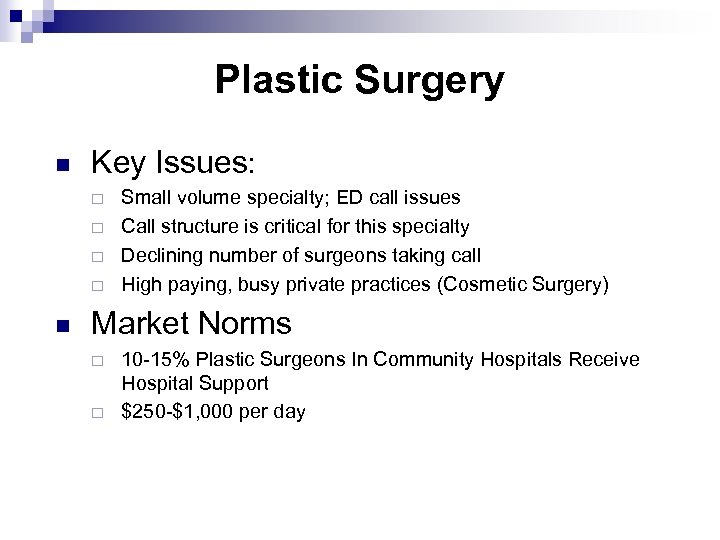
Plastic Surgery n Key Issues: ¨ ¨ n Small volume specialty; ED call issues Call structure is critical for this specialty Declining number of surgeons taking call High paying, busy private practices (Cosmetic Surgery) Market Norms ¨ ¨ 10 -15% Plastic Surgeons In Community Hospitals Receive Hospital Support $250 -$1, 000 per day
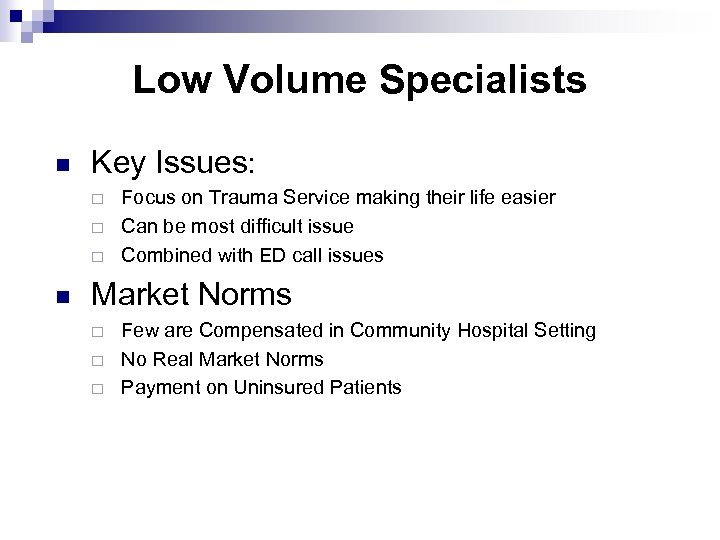
Low Volume Specialists n Key Issues: ¨ ¨ ¨ n Focus on Trauma Service making their life easier Can be most difficult issue Combined with ED call issues Market Norms ¨ ¨ ¨ Few are Compensated in Community Hospital Setting No Real Market Norms Payment on Uninsured Patients
Hospital Based Specialists n Trauma is Part of Their Hospital Franchise n Few Payment Examples n In house Anesthesia is exception
Trauma Center Of The Future n The emerging Hospitalist Model n Carved out Trauma Physician Billing n Trauma Specific CPT Codes and RVU’s n Unfallkrankenhaus Lorenz Bohler
df973cf2a42039cf949bb158b0169bae.ppt