Bronchial Asthma.ppt
- Количество слайдов: 32
Bronchial Asthma Dr. Yousef Al-Noimat Consultant in pulmonary and internal medicine.
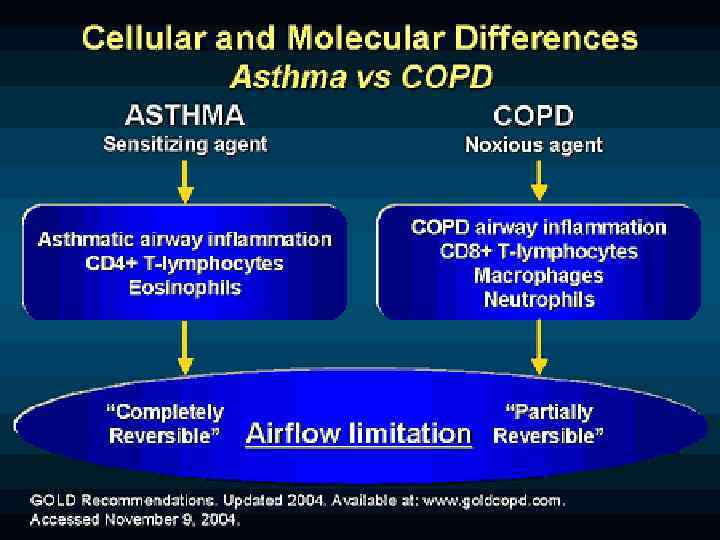
Definition n “A chronic inflammatory disorder of the airways in which many cells play a role, in particular mast cells, eosinophils, and T lymphocytes. In Susceptible individuals this inflammation causes recurrent episodes of wheezing, breathlessness, chest tightness, and cough particularly at night and /or in the early morning.
Definition: cont. n These symptoms are usually associated with widespread but variable airflow limitation that is at least partially reversible either spontaneously or with treatment. The inflammation also causes an associated increase in airway responsiveness to a variety of stimuli. ”
Asthma Prevalence The peak prevalence for asthma is in childhood and is approximately 10% n This declines to about 5 -6% in adolescents n The prevalence rises in adulthood to 7 -9% n Remission in the second decade is common and is as high as 60 -70% n Remission less common in older age groups but may be as high as 20 -30% n
Risk Factors Gender: Childhood: Boys > Girls Age 20 -40: Males=Females Age > 40 : Females > males n Airway hyperresponsiveness n Atopy n Exposure to indoor antigens n Outdoor air pollution n Respiratory infections n
Risk Factors-cont. . Smoking n Passive smoke exposure n Prenatal exposure to maternal smoking n Obesity n Maternal age: younger mothers more risk n Prematurity n
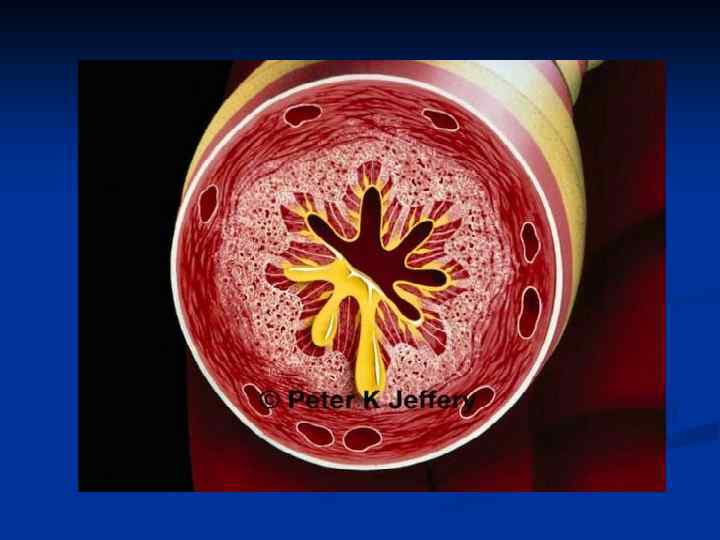
Physiology of Airway obstruction Airway narrowing secondary to 1 -thickening of airway wall 2 -smooth muscle contraction 3 -excessive secretions n Airway narrowing leads to reduced air flow n Air flow obstruction occurs throughout the tracheobronchial tree n
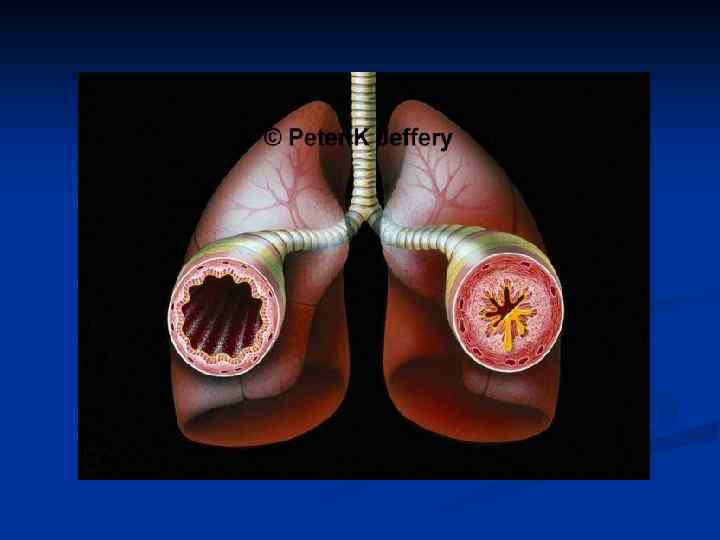
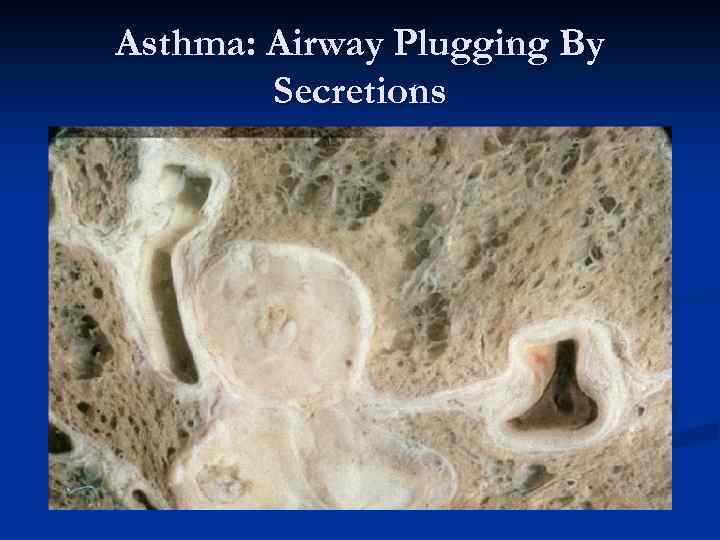
Asthma: Airway Plugging By Secretions
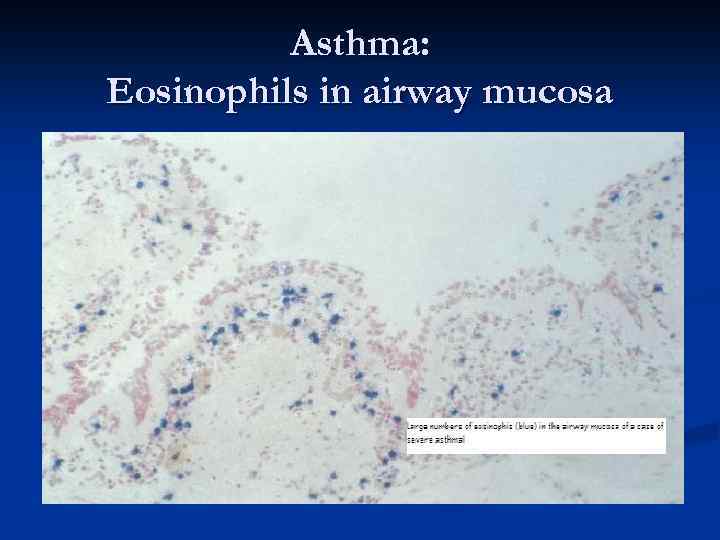
Asthma: Eosinophils in airway mucosa
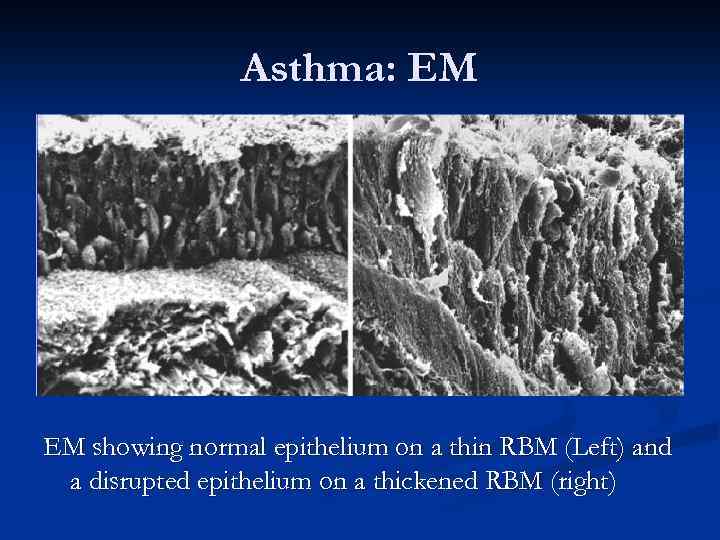
Asthma: EM EM showing normal epithelium on a thin RBM (Left) and a disrupted epithelium on a thickened RBM (right)
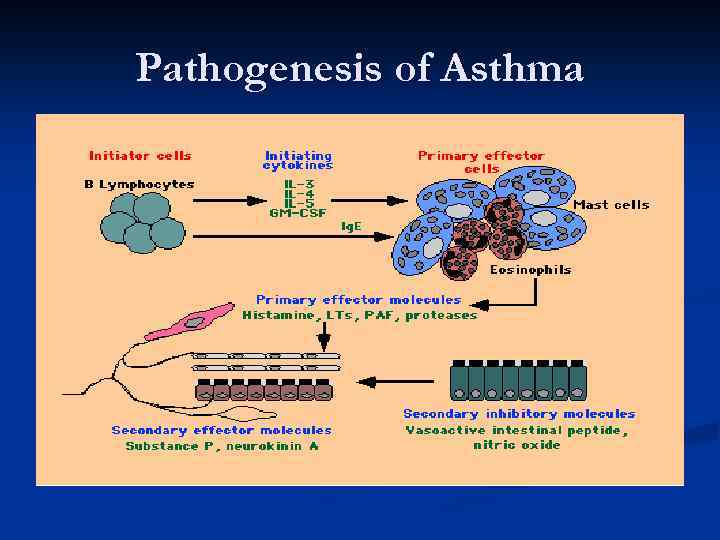
Pathogenesis of Asthma
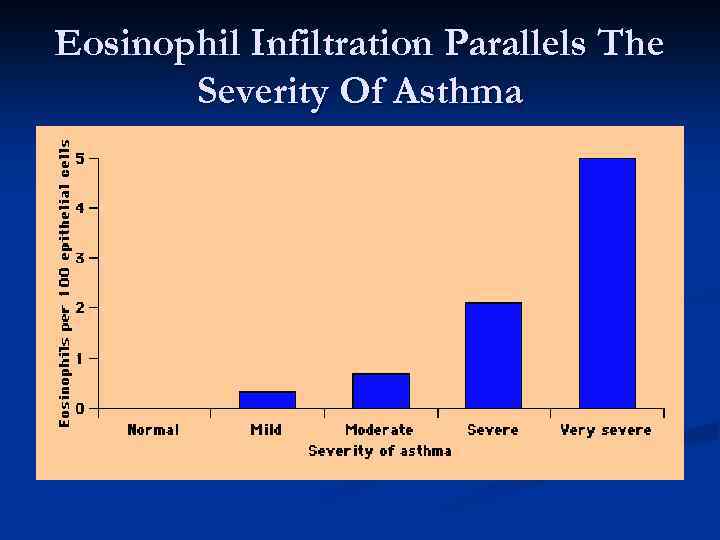
Eosinophil Infiltration Parallels The Severity Of Asthma
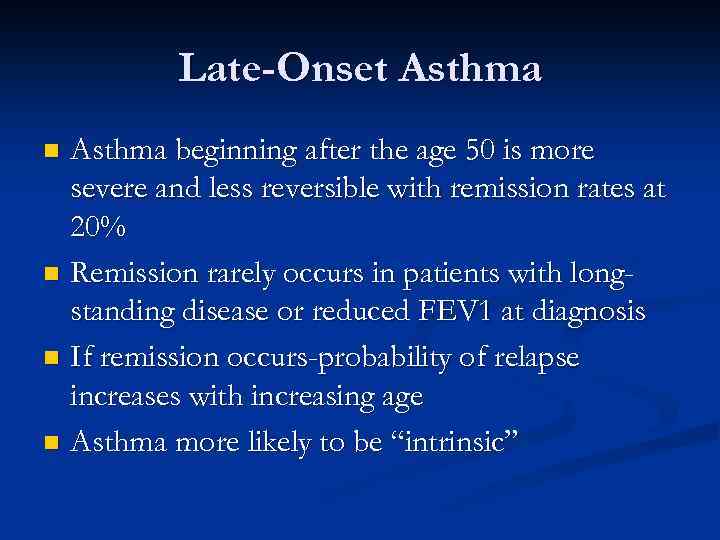
Late-Onset Asthma beginning after the age 50 is more severe and less reversible with remission rates at 20% n Remission rarely occurs in patients with longstanding disease or reduced FEV 1 at diagnosis n If remission occurs-probability of relapse increases with increasing age n Asthma more likely to be “intrinsic” n
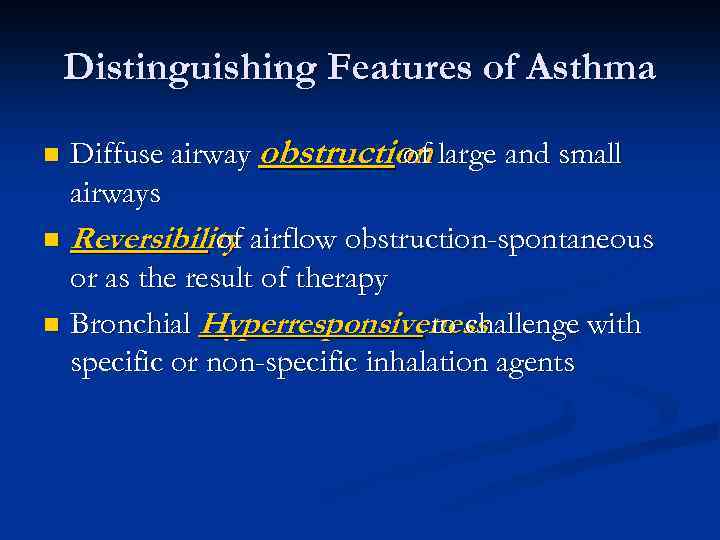
Distinguishing Features of Asthma Diffuse airway obstruction large and small of airways n Reversibility airflow obstruction-spontaneous of or as the result of therapy n Bronchial Hyperresponsiveness to challenge with specific or non-specific inhalation agents n
Clinical Presentation n n n n Persistent wheezing-35% Chronic cough-24% Chronic dyspnea-29% Chest pain or tightness Hyperventilation syndrome Hemoptysis Intermittent seasonal waxing and waning Nocturnal episodes Exacerbation on exposure to stimuli, e. g. exercise, cold air, air pollutants, strong odors and URI
Physical Examination Wheezing: widespread, multiple different pitches n Use of accessory muscles of breathing n Pulsus Paradoxus n Nasal polyposis n Allergic rhinitis, hives, eczema n Exercise limitation n
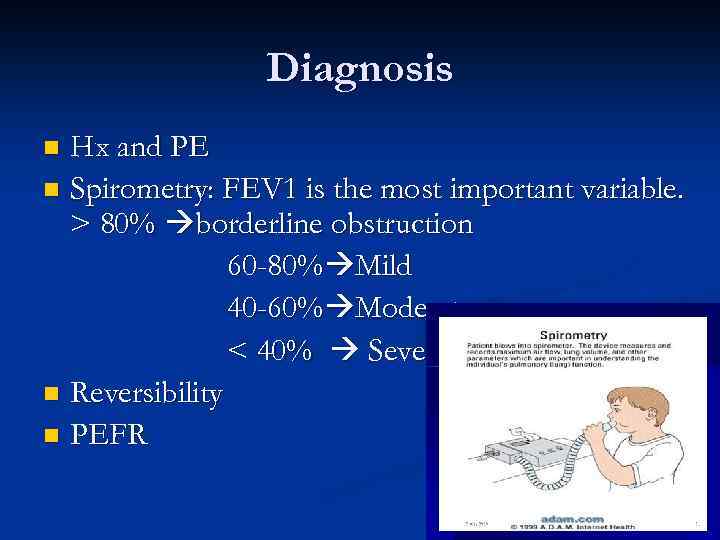
Diagnosis Hx and PE n Spirometry: FEV 1 is the most important variable. > 80% borderline obstruction 60 -80% Mild 40 -60% Moderate < 40% Severe n Reversibility n PEFR n
Reversibility of Airflow Obstruction: n >200 cc and >12% improvement in FEV 1 after short acting bronchodilator; after weeks of corticosteroid therapy or with spontaneous remission n 20% variation in peak flow (PEFR) within 24 hour period
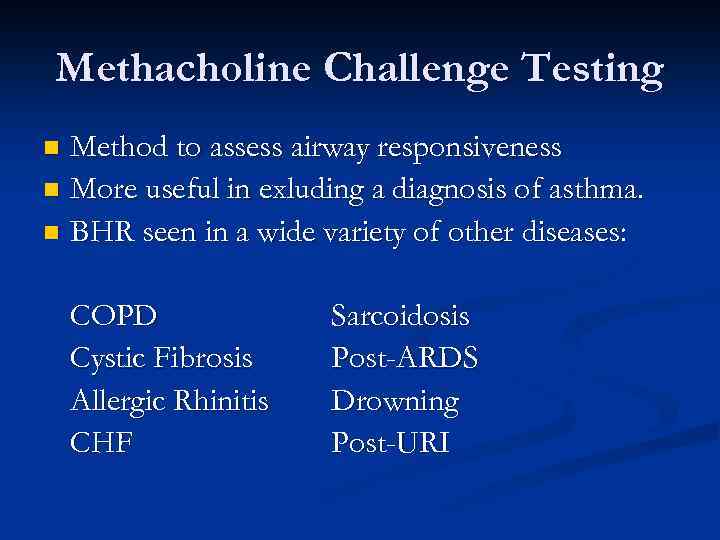
Methacholine Challenge Testing Method to assess airway responsiveness n More useful in exluding a diagnosis of asthma. n BHR seen in a wide variety of other diseases: n COPD Cystic Fibrosis Allergic Rhinitis CHF Sarcoidosis Post-ARDS Drowning Post-URI
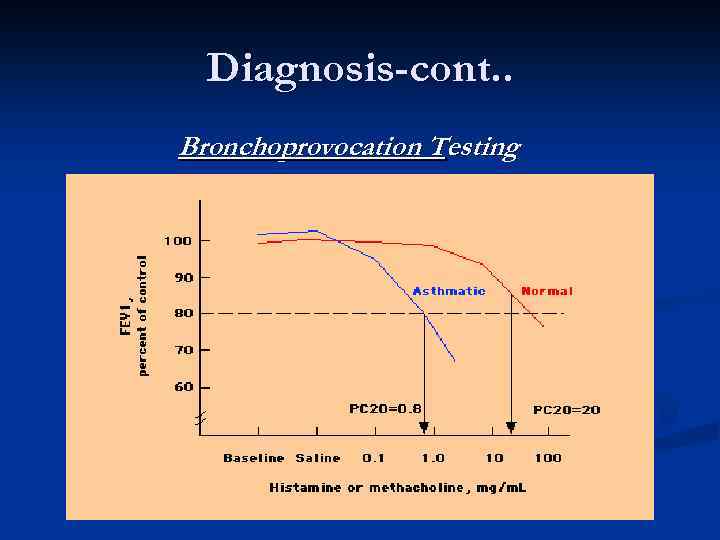
Diagnosis-cont. . Bronchoprovocation Testing
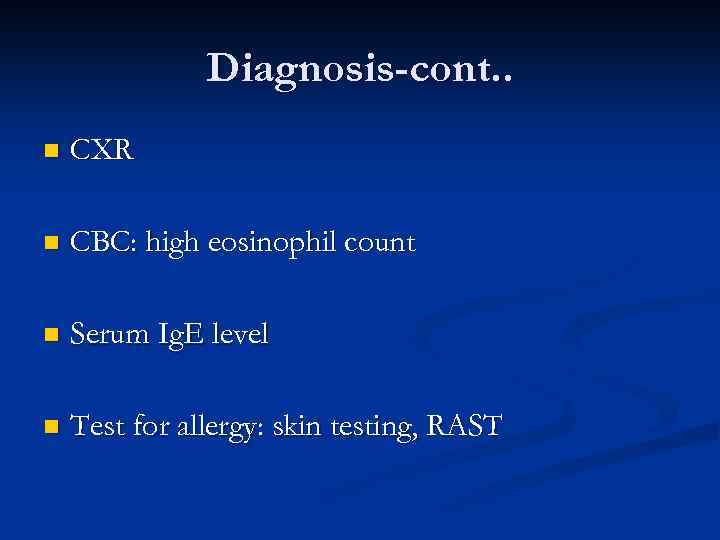
Diagnosis-cont. . n CXR n CBC: high eosinophil count n Serum Ig. E level n Test for allergy: skin testing, RAST
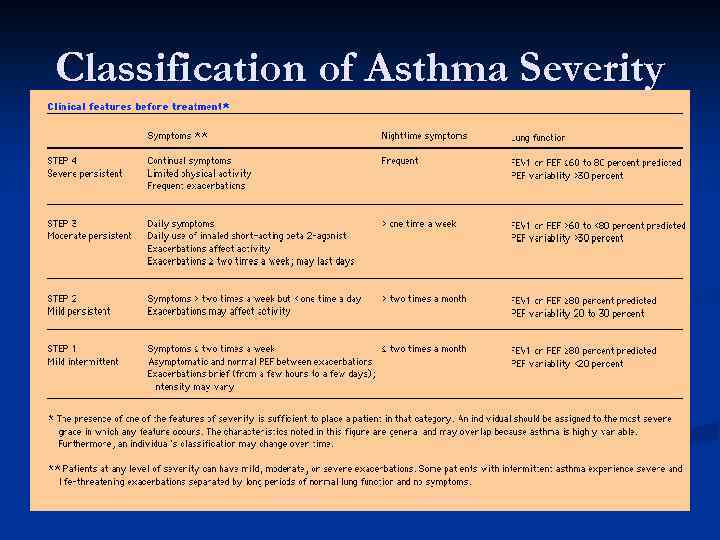
Classification of Asthma Severity
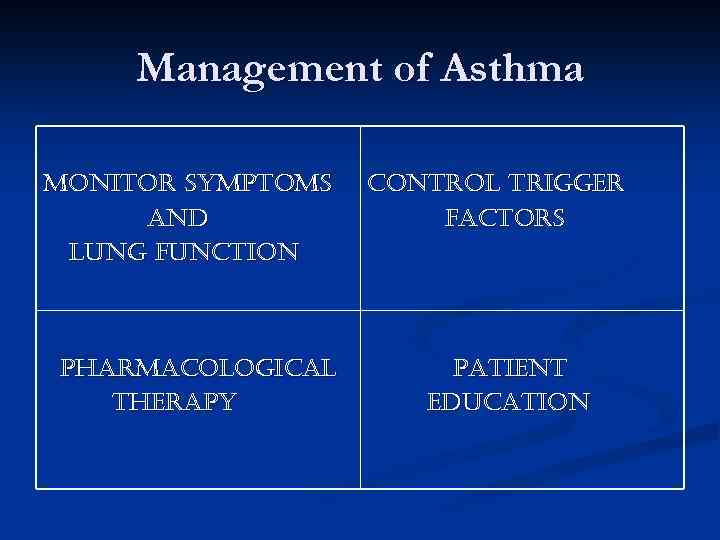
Management of Asthma monitor symptoms and lung function pharmacological therapy control trigger factors patient education
Monitoring of Asthma n PEFR n Sputum eosinophilia n Exhaled nitric oxide analysis
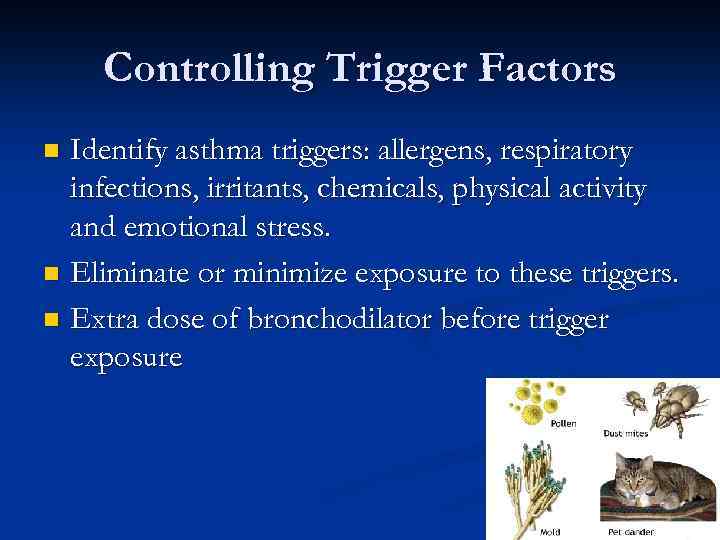
Controlling Trigger Factors Identify asthma triggers: allergens, respiratory infections, irritants, chemicals, physical activity and emotional stress. n Eliminate or minimize exposure to these triggers. n Extra dose of bronchodilator before trigger exposure n

Pharmacological Therapy n Beta- Agonists n Anticholinergics n Cromolyn/Nedocromi n Systemic steroids n Inhaled Steroids n Theophylline n Leukotriene-modifying agents n Others
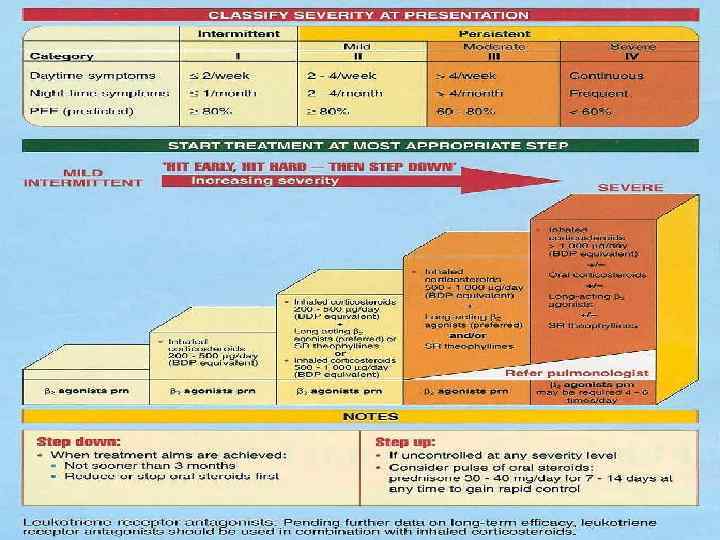
Pharmacological Therapy
Patient Education Understand the triggers of asthma n Learn how to avoid triggers n Understand medicine: when and how to use n Learn how to monitor disease n Understand what to do in emergency n

Thank You
Bronchial Asthma.ppt