BRONCHIAL ASTHMA.ppt
- Количество слайдов: 27
BRONCHIAL ASTHMA DR WADAH KHRIESAT KAUH JUST
CASE SCENARIO Khalid 14 years old come to the clinic c/o shortness of breath for one day duration. He is a known asthmatic patient for more than 8 years, he visited A/E frequently. His school performance is below average, with frequent absence from school due to his illness. HOW YOU WILL PROCEED DURING THIS CONSULTATION ?
What are your objectives in caring for bronchial asthma patient ? u u Prevent troublesome symptoms night and day Prevent serious attacks Require little or no reliever medication Have productive, physical, psychological, and social active lives
WHAT IS BRONCHIAL ASTHMA? Asthma is a CHRONIC INFLAMMATORY disorder of the airways. Chronically inflamed airways are hyper responsive; they become obstructed and airflow is limited by bronchoconstriction, mucus plugs, and increased inflammation when airways are exposed to various risk factors.
The prevalence of asthma among school children u Range 4%-23% u Riyadh 10% u Jeddah 12%
What is the Pathophysiology? Trigger Factor u Mast cell u Mediators : histamine, prostaglandin, leukotrienes, as well as cytokines. u Inflammatory cells u Sustained Inflammatory response u Contraction of airway smooth muscles (Bronchoconstriction) u
Pathophysiology (Cont. ) Airway wall swelling (mucosal edema) u Airway hyper responsiveness u Chronic changes u Hypertrophy of the smooth muscles, thickening of the basement membrane u Airway remodeling u There is good evidence that asthma occurs in families. u

What are the Triggering Factors? Domestic dust mites u Air pollution u Tobacco smoke u Occupational irritants u Cockroach u Animal with fur u Pollen u
Triggering Factors ( cont. ) Respiratory (viral) infections u Chemical irritants u Strong emotional expressions u Drugs ( aspirin, beta blockers) u
CASE SCENARIO Ahmed 6 years old come to primary care clinic with his father c/o chronic cough for the last 3 months, mainly at night. How you will approach this patient?
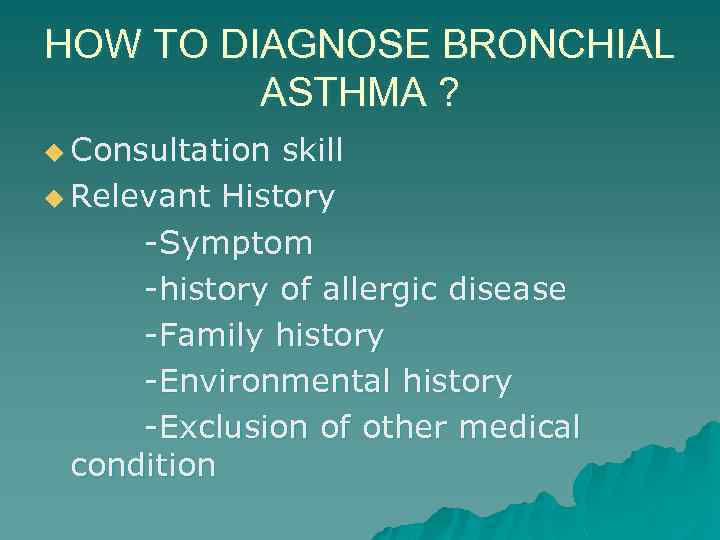
HOW TO DIAGNOSE BRONCHIAL ASTHMA ? u Consultation skill u Relevant History -Symptom -history of allergic disease -Family history -Environmental history -Exclusion of other medical condition
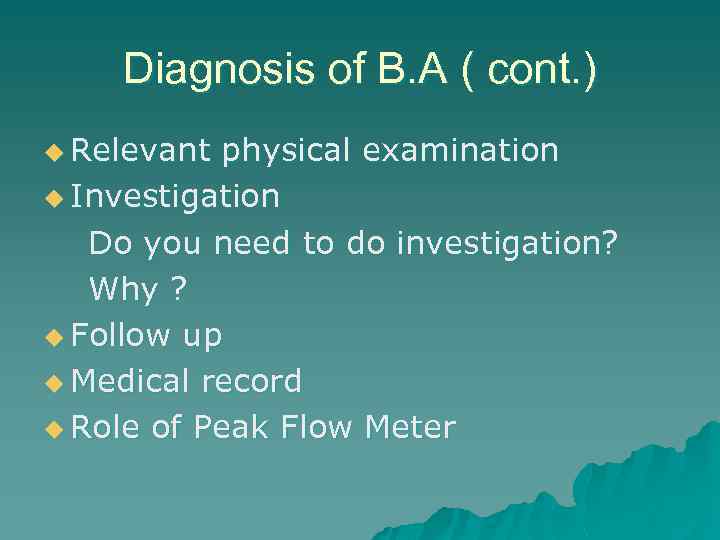
Diagnosis of B. A ( cont. ) u Relevant physical examination u Investigation Do you need to do investigation? Why ? u Follow up u Medical record u Role of Peak Flow Meter
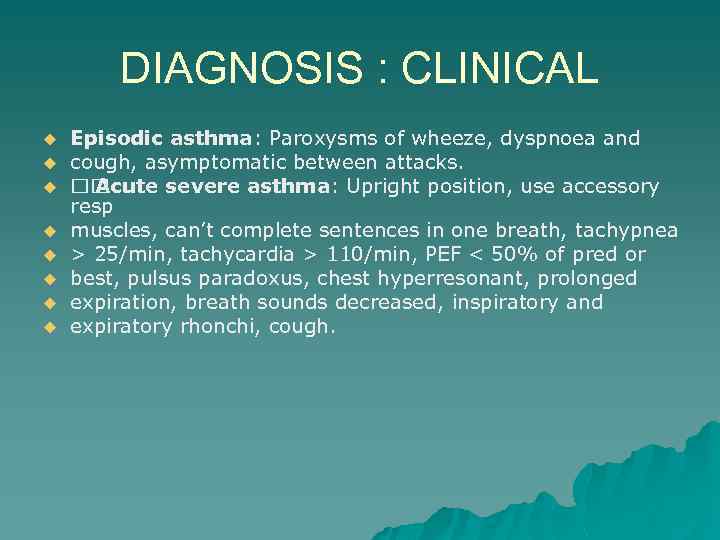
DIAGNOSIS : CLINICAL u u u u Episodic asthma: Paroxysms of wheeze, dyspnoea and cough, asymptomatic between attacks. Acute severe asthma: Upright position, use accessory resp muscles, can’t complete sentences in one breath, tachypnea > 25/min, tachycardia > 110/min, PEF < 50% of pred or best, pulsus paradoxus, chest hyperresonant, prolonged expiration, breath sounds decreased, inspiratory and expiratory rhonchi, cough.
DIAGNOSIS : CLINICAL u u u u u Life-threatening features: PEF < 33% of pred or best, silent chest, cyanosis, bradycardia, hypotension, feeble respiratory effort, exhaustion, confusion, coma, Pa. O 2 < 60, PCO 2 normal or increased, acidosis (low p. H or high [H+]). Chronic asthma: Dyspnea on exertion, wheeze, chest tightness and cough on daily basis, usually at night and early morning; intercurrent acute severe asthma (exacerbations) and productive cough (mucoid sputum), recurrent respiratory infection, expiratory rhonchi throughout and accentuated on forced expiration.
DIAGNOSIS : RADIOLOGY u Chest XR may be normal between attacks. u With attacks hyperinflation may be found. u complicated asthma segmental In lobar collapse (mucous u plugs) and pneumothorax can occur.
DIFFERENTIAL DIAGNOSIS 1. Upper airway obstruction – glottic dysfunction. u 2. Acute LV failure – pulmonary oedema. u 3. Pulmonary embolism. u 4. Endobronchial disease. u 5. Chronic bronchitis. u 6. Eosinophilic pneumonia. u 7. Carsinoid syndrome. u 8. Vasculitis. u
Manifestations of respiratory failure Hypoxemia: cyanosis- very late sign, not u dependable u Hypercapnia: sweating, u tachycardia, widened pulse pressure u Acidosis: tachypnea u Blood gases the only accurate assessment of u ventilatory status u
CLASSIFY ASTHMA SEVERITY u Mild intermittent Asthma (step 1) u Mild persistent Asthma (step 2) u Moderate persistent Asthma (step 3) u Severe persistent Asthma (step 4)
How to manage and control Bronchial Asthma u Educate patients to develop a partnership in asthma care u Assess and monitor asthma severity u Avoid exposure to trigger factors u Establish individual medication plans for long term management in children and adults
How to manage and control Bronchial Asthma ( cont. ) u Establish individual plans to manage asthma attacks u Provide regular follow up care.
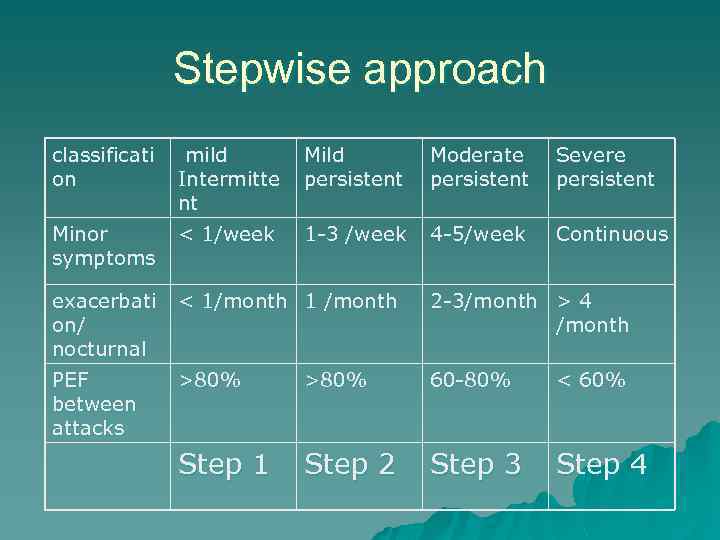
Stepwise approach classificati on mild Intermitte nt Mild persistent Moderate persistent Severe persistent Minor symptoms < 1/week 1 -3 /week 4 -5/week Continuous exacerbati on/ nocturnal < 1/month 1 /month 2 -3/month > 4 /month PEF between attacks >80% 60 -80% < 60% Step 1 Step 2 Step 3 Step 4
MANAGEMENT 1 u u u MANAGEMENT 1 Avoidance of allergen and triggers – may be impractical → adjust Rx. Occasional asthma : Rarely symptomatic → β 2 agonist prn. Mild intermittent asthma )episodic : (β 2 agonist prn +low dose IH corticosteroid. Mild persistent asthma : β 2 agonist prn +high dose IH corticosteroid or long acting β 2 agonist +low dose IH corticosteroid. Moderate persistent asthma : β 2 agonist prn +high dose IH corticosteroid +long acting β 2 agonist or SR theophylline
MANAGEMENT 2 u u u Severe, persistent asthma β 2 agonist prn + high dose IH corticosteroid + long acting β 2 agonist + SR Theophylline + oral corticosteroids. Step up: If uncontrolled at any severity level, oral steroids – Prednisone 30 -40 -mg/day for 7 -14 days. Step down: When stable for at least 3 months – reduce or stop oral steroids first. Leukotriene antagonists: for patients with aspirin/NSAIDS induced asthma. May also be added on for severe persistent asthma or in pts with steroid related side effects such as growth retardation or non-responsiveness to IHS or to allow dose IHS instead of high dose.
MANAGEMENT 3 u u u u u Acute severe asthma: 1. Immediate Rx: O 2 40 -60% via mask or cannula + β 2 agonist (salbutamol 5 mg) via nebulizer + Prednisone tab 30 -60 mg and/or hydrocortisone 200 mg IV. With lifethreatening features add 0. 5 mg ipratropium to nebulized β 2 agonist + Aminophyllin 250 mg IV over 20 min or salbutamol 250 ug over 10 min. 2. Subsequent Rx: Nebulized β 2 agonist 6 hourly + Prednisone 30 -60 mg daily or hydrocortisone 200 mg 6 hourly IV + 40 -60% O 2.
MANAGEMENT 4 u u u u u No improvement after 15 -30 min: Nebulized β 2 agonist every 15 -30 min + Ipratropium. Still no improvement: Aminophyllin infusion 750 mg/24 H (small pt), 1 500 mg/24 H (large pt), or alternatively salbutamol infusion. Monitor Rx: Aminophyllin blood levels + PEF after 15 -30 min + oxymetry (maintain Sa. O 2 > 90) + repeat blood gases after 2 hrs if initial Pa. O 2 < 60, Pa. CO 2 normal or raised and patient deteriorates. Deterioration: ICU, intubate, ventilate + muscle relaxant

QUESTIONS ? ?

THANK YOU WITH MY BEST REGARDS
BRONCHIAL ASTHMA.ppt