7c3afefc968a1bd2e028eaaa8c9e234a.ppt
- Количество слайдов: 75
Bringing Evidence into Dju-Lyn Chng 茹玲 Account Development Manager
What will we cover today? • What is Evidence-Based Medicine? • Why is EBM important? • What is the traditional method of practicing EBM? • How Clinical Evidence fits into the practice of EBM? • Case Scenario
What is evidence based medicine? “Evidence based medicine is the “conscientious, explicit and judicious use of current best evidence in making decisions about individual patients”. Sackett DL et al 1996
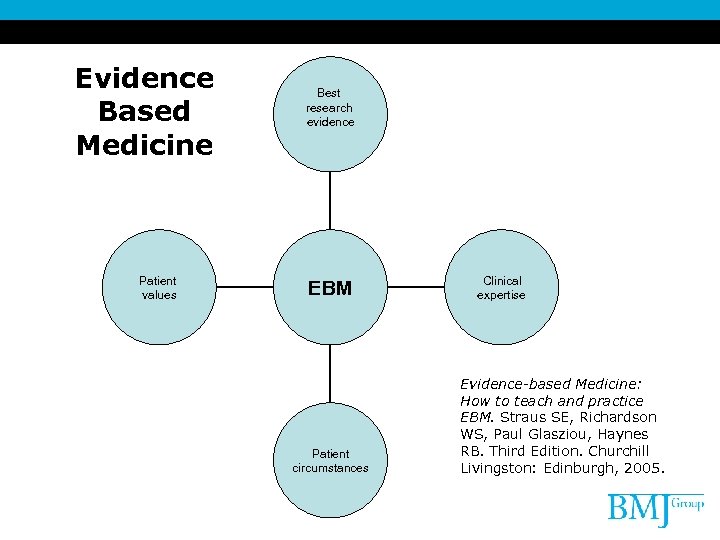
Evidence Based Medicine Patient values Best research evidence EBM Patient circumstances Clinical expertise Evidence-based Medicine: How to teach and practice EBM. Straus SE, Richardson WS, Paul Glasziou, Haynes RB. Third Edition. Churchill Livingston: Edinburgh, 2005.
What is not evidence based medicine? Evidence based medicine does not tell healthcare professionals what to do. Evidence based medicine identifies management options, and how well they are supported by evidence in defined populations.
Why is evidence based medicine important? Evidence based medicine allows healthcare professionals to: • • Identify gaps in knowledge Choose effective treatments Choose between effective treatments Choose cost-effective treatments • Stop using treatments that do not work and / or that harm patients
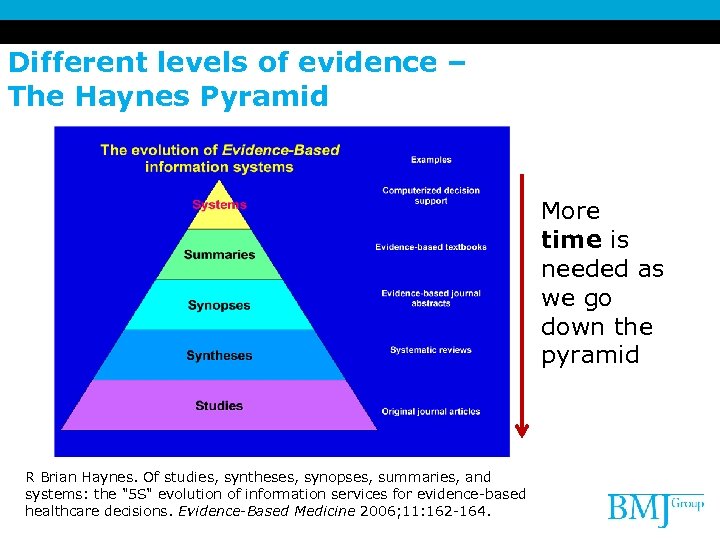
Different levels of evidence – The Haynes Pyramid More time is needed as we go down the pyramid R Brian Haynes. Of studies, syntheses, synopses, summaries, and systems: the "5 S" evolution of information services for evidence-based healthcare decisions. Evidence-Based Medicine 2006; 11: 162 -164.
Pub. Med: Studies: 原始研究文獻
海量的醫學文獻 • 8000 articles published per day • 30 kg of guidelines per family doctor • 25, 000 biomedical journals in print • 1500 medical articles onto Medline per day
Cochrane systematic reviews: Syntheses: 系統性綜述
Evidence based medicine journal: Synopses: 單篇循證文獻摘要性評述
BMJ Clinical Evidence: Summaries: 針對臨床問題結合證據的概述
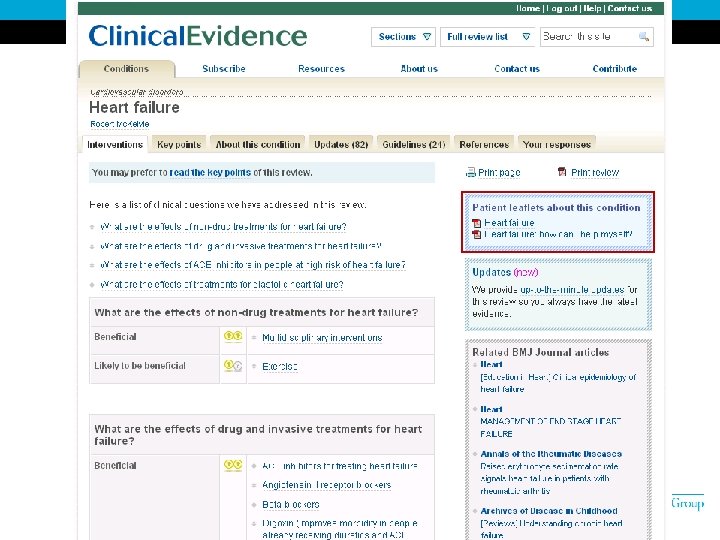
What is BMJ Clinical Evidence? Helping Clinicians Put Evidence Into Practice Features • Provides systematic reviews offering evidence on over 3, 100 interventions in over 650 clinical situations • Includes evidence based research sources from over 10, 000 peer reviewed articles from Cochrane Library, Medline, Embase and evidence based journals • Produced by international panel of clinicians using rigorous searching and evaluation methods • Summary of the best evidence of benefits and harms of interventions • Updated regularly • Links to abstracts on Pub. Med
實證醫學的五個主要步驟 • Assess • Ask clinical question 提出一個可以被回答的問題 • Acquire the evidence 檢索文獻資料 • Appraise the evidence 嚴格評價證據的可信度和相關性 • Apply the evidence 結合實際作出臨床決策
Traditional Steps of Evidence Based Medicine • • • Assess Ask clinical question Acquire the evidence Appraise the evidence Apply the evidence
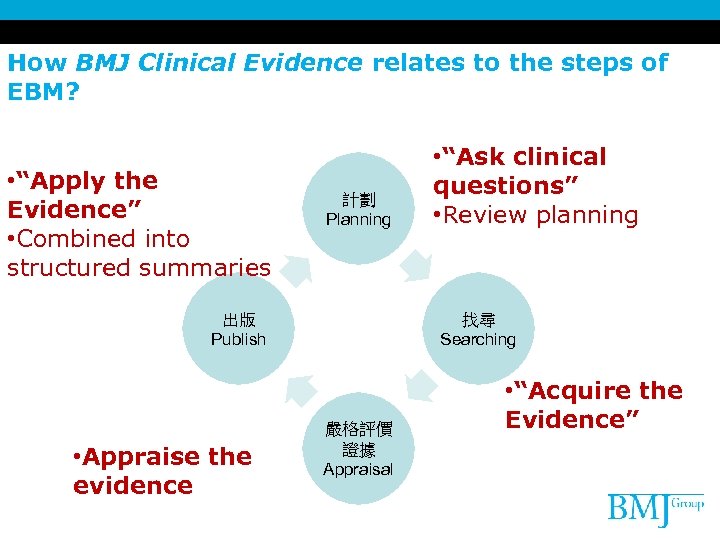
How BMJ Clinical Evidence relates to the steps of EBM? • “Apply the Evidence” • Combined into structured summaries 計劃 Planning 找尋 Searching 出版 Publish • Appraise the evidence • “Ask clinical questions” • Review planning 嚴格評價 證據 Appraisal • “Acquire the Evidence”
Planning – Ask clinical questions. . . • PICOT – – Patient Intervention/Risk factor Comparison Outcome – Type of Study (Systematic reviews? RCTs? ) • Quality parameters – Size of study – Length of follow up – Loss to follow up
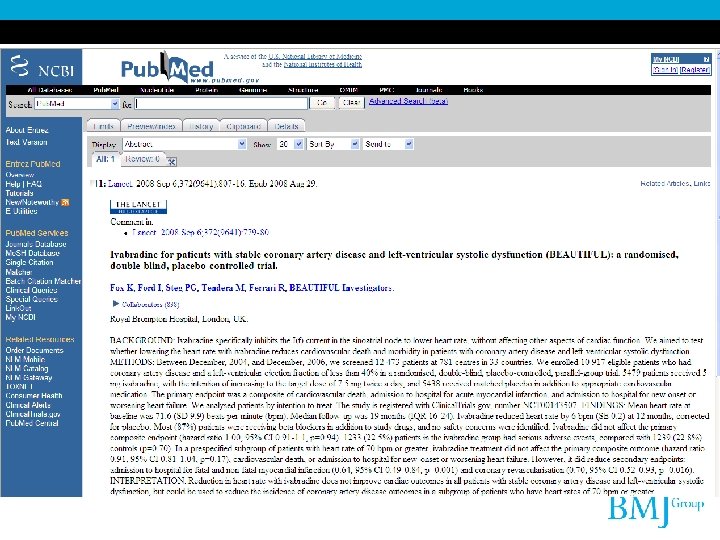
Searching – Acquire the evidence. . . • • • Pub. Medline Cochrane Reviews Embase … and many more
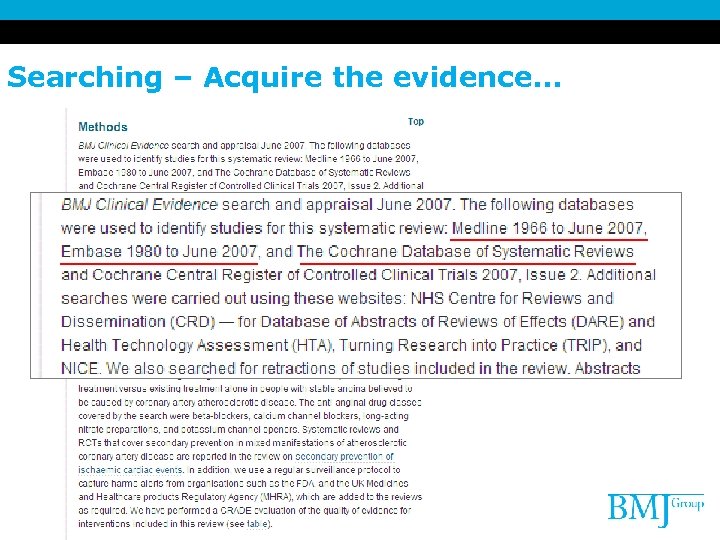
Searching – Acquire the evidence. . .
Searching – Evidence for benefits of a treatment. . . But. . . What about the harms? • Systematic reviews often do not search for adverse effects (Ernst 2001) • RCTs are not big enough or long enough to detect many harms • Published trials including harms data can be difficult to find (Derry 2001) • Many observational studies to appraise
How BMJ Clinical Evidence search for harms • Look for specific adverse effects identified at review planning • Decide which type of evidence will be appropriate • RCTs – for expected and common harms that happen soon after treatment • Unexpected, rare and delayed harms may require case-control/cohort search
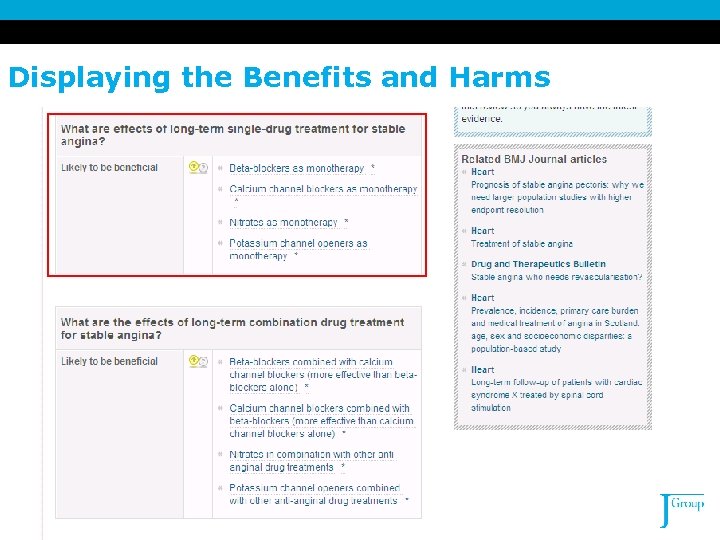
Displaying the Benefits and Harms
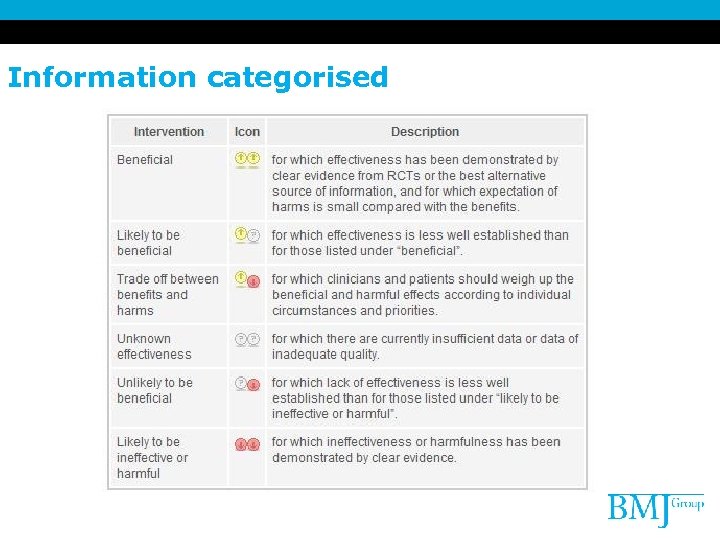
Information categorised
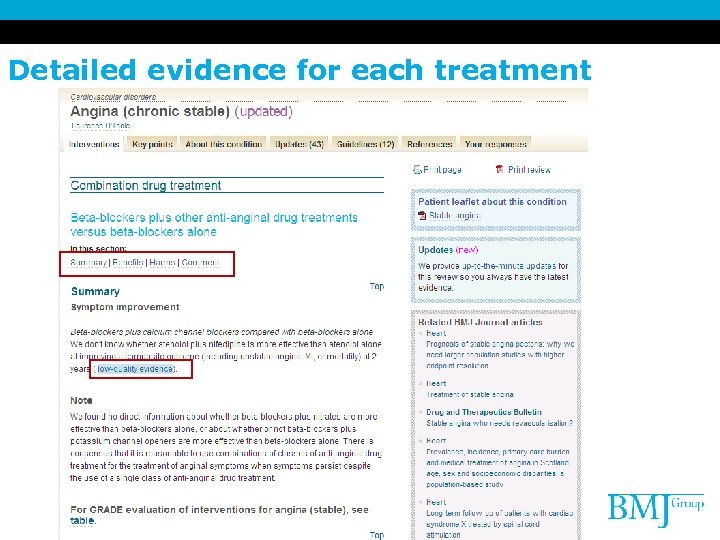
Detailed evidence for each treatment
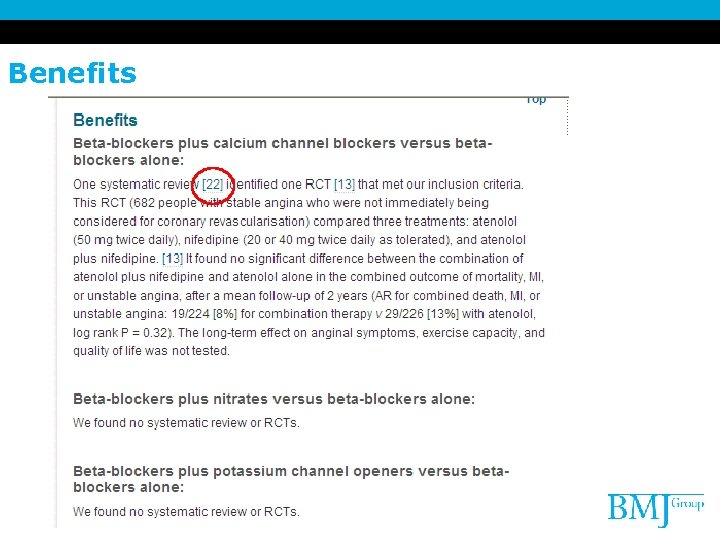
Benefits
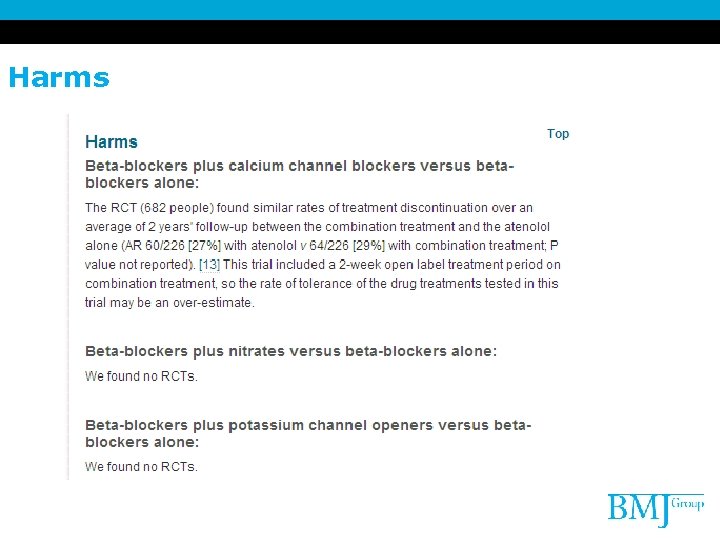
Harms
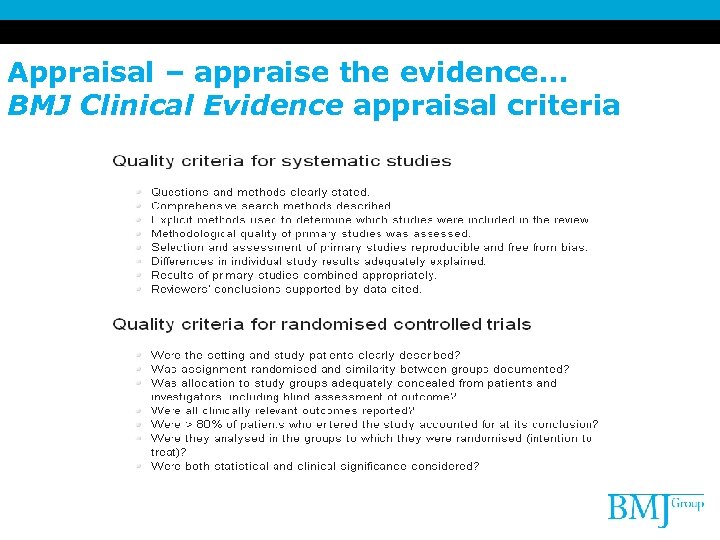
Appraisal – appraise the evidence… BMJ Clinical Evidence appraisal criteria
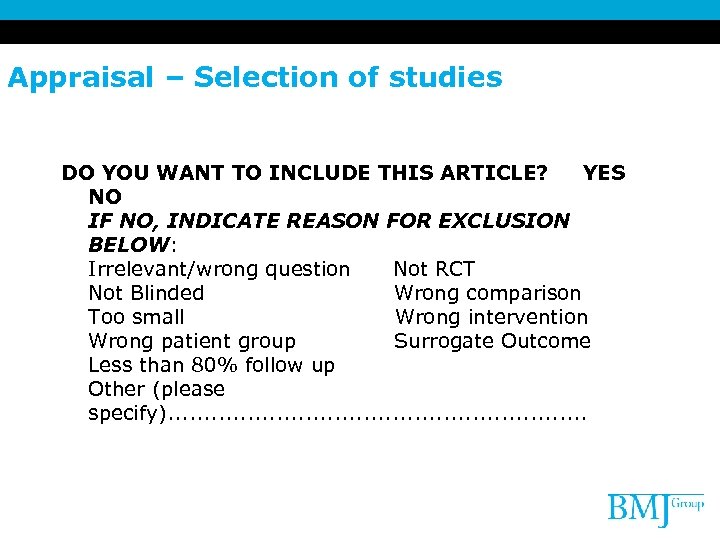
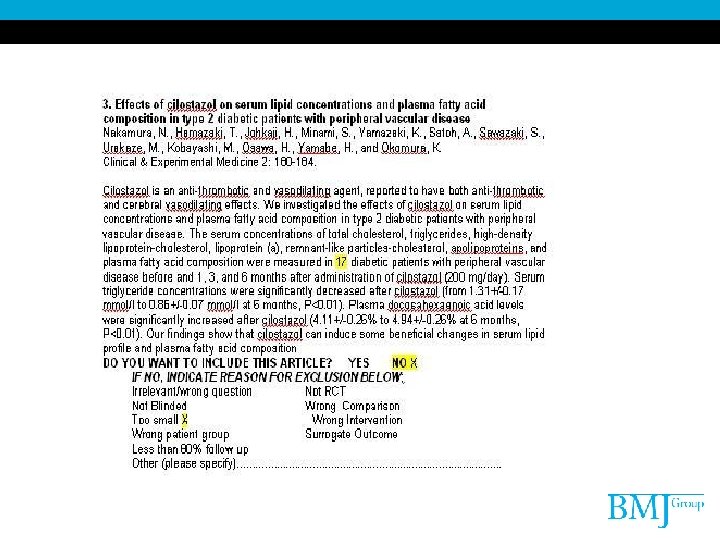
Appraisal – Selection of studies DO YOU WANT TO INCLUDE THIS ARTICLE? YES NO IF NO, INDICATE REASON FOR EXCLUSION BELOW: Irrelevant/wrong question Not RCT Not Blinded Wrong comparison Too small Wrong intervention Wrong patient group Surrogate Outcome Less than 80% follow up Other (please specify). . . .
Appraisal – BMJ Clinical Evidence makes the GRADE
What is GRADE? • Grading of • Recommendations • Assessment, • Development and • Evaluation system for grading evidence
What is GRADE? • Developed by international guideline developers • Explicit evaluation of the importance of outcomes • Explicit, comprehensive criteria for downgrading and upgrading quality of evidence ratings • Clear separation between quality of evidence and strength of recommendations
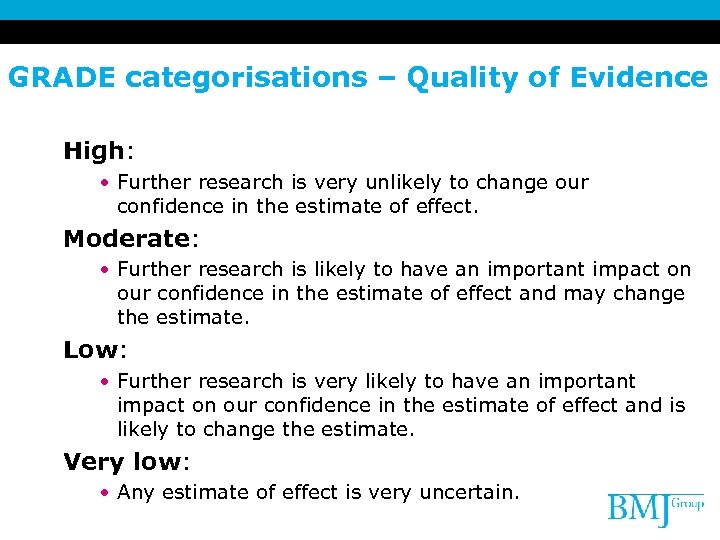
GRADE categorisations – Quality of Evidence High: • Further research is very unlikely to change our confidence in the estimate of effect. Moderate: • Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low: • Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low: • Any estimate of effect is very uncertain.
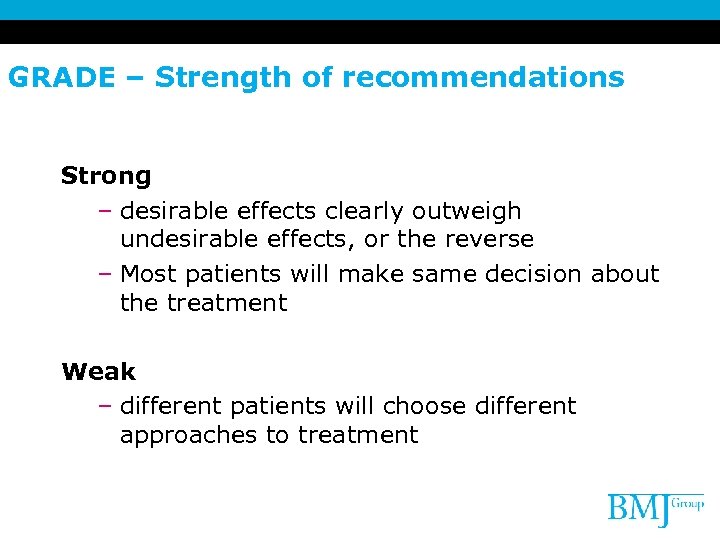
GRADE – Strength of recommendations Strong – desirable effects clearly outweigh undesirable effects, or the reverse – Most patients will make same decision about the treatment Weak – different patients will choose different approaches to treatment
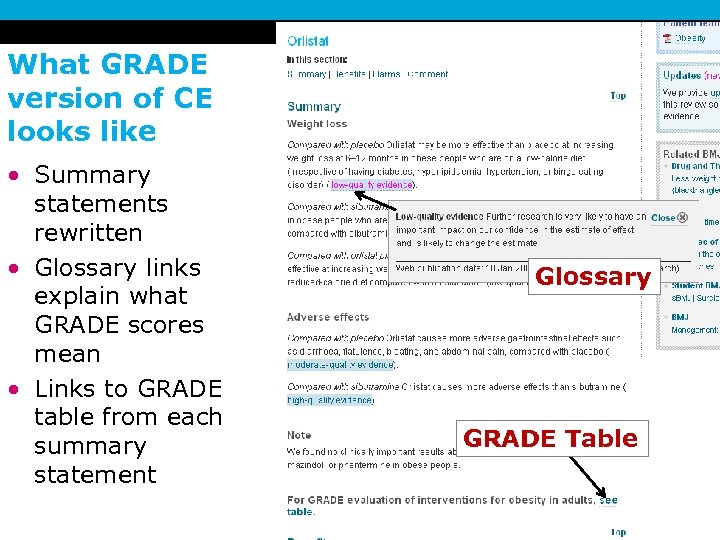
What GRADE version of CE looks like • Summary statements rewritten • Glossary links explain what GRADE scores mean • Links to GRADE table from each summary statement Glossary GRADE Table
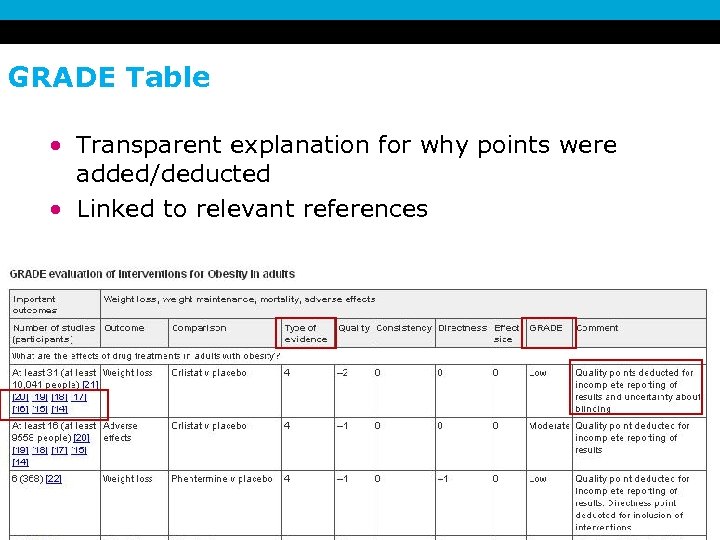
GRADE Table • Transparent explanation for why points were added/deducted • Linked to relevant references
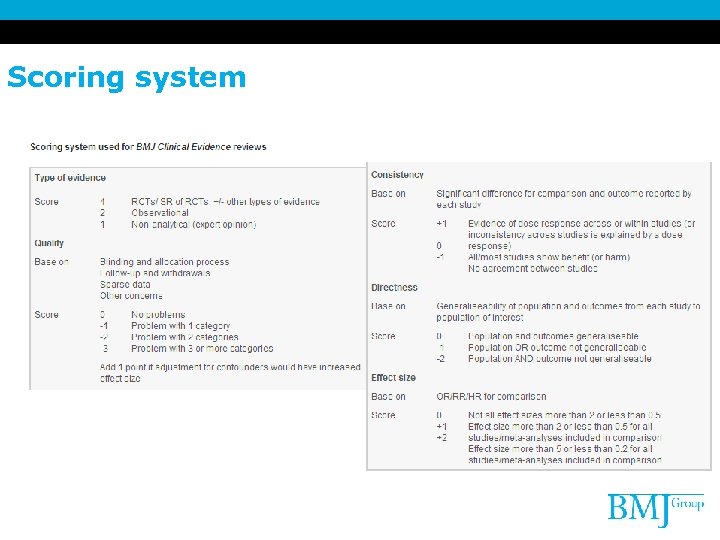
Scoring system
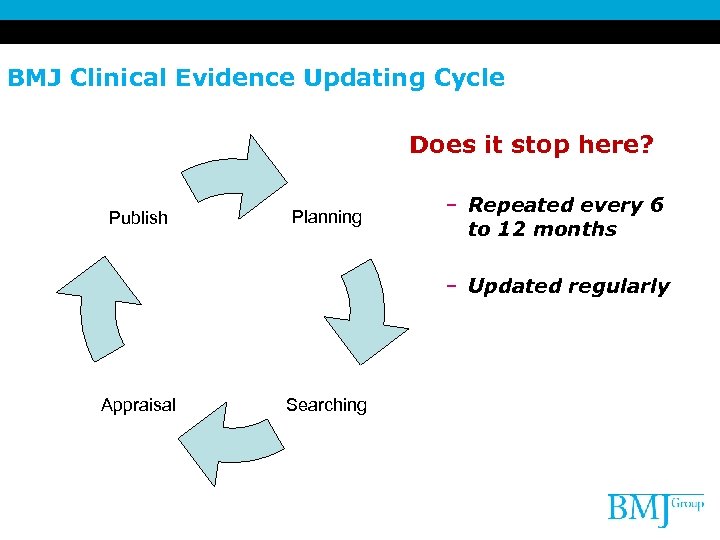
BMJ Clinical Evidence Updating Cycle Does it stop here? Publish Planning – Repeated every 6 to 12 months – Updated regularly Appraisal Searching
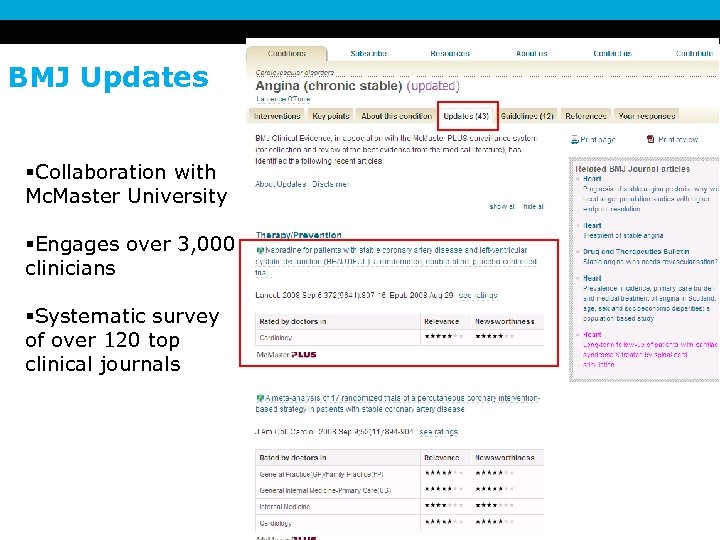
BMJ Updates §Collaboration with Mc. Master University §Engages over 3, 000 clinicians §Systematic survey of over 120 top clinical journals
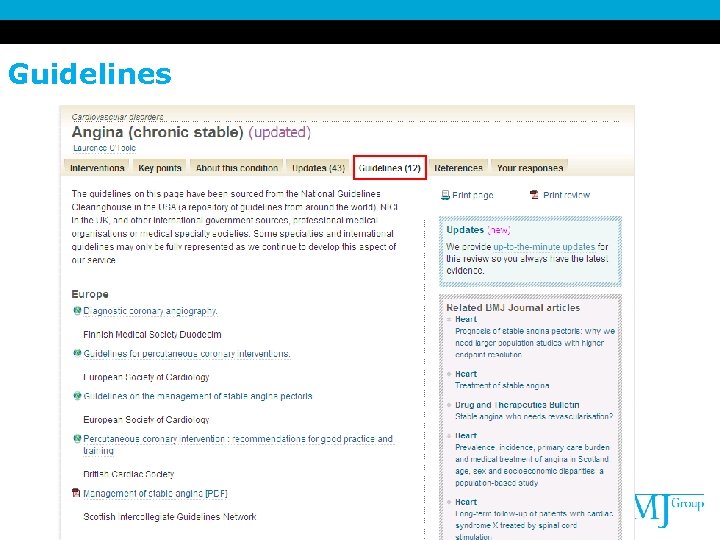
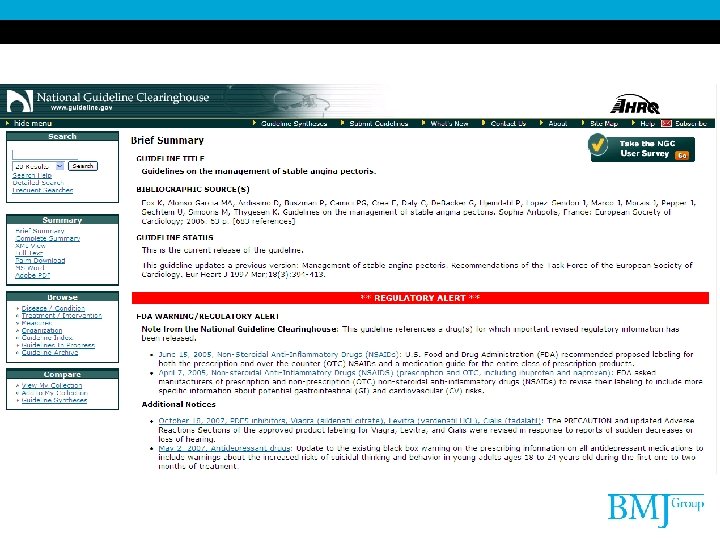
Guidelines
Pop Quiz 1: • What feature in Clinical Evidence will help you determine the quality of an evidence? • Answer: The GRADE Table
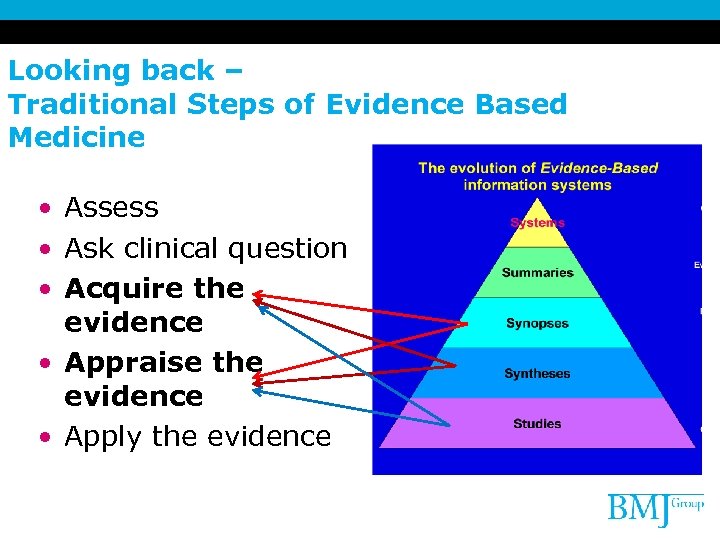
Looking back – Traditional Steps of Evidence Based Medicine • Assess • Ask clinical question • Acquire the evidence • Appraise the evidence • Apply the evidence
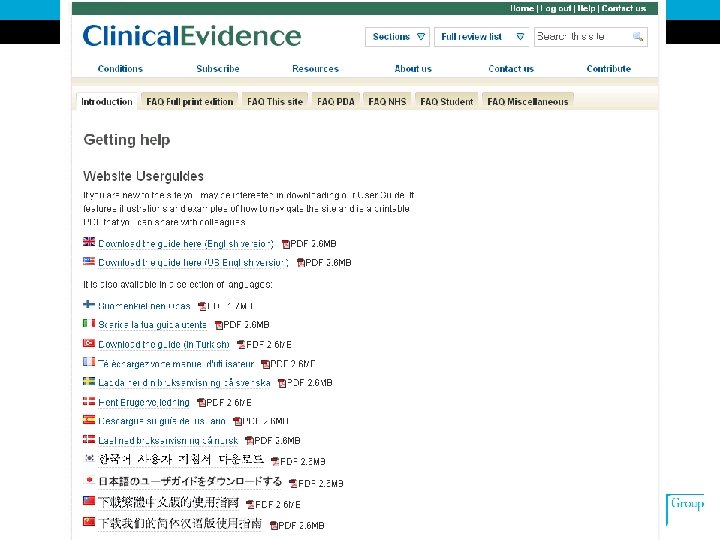
What makes a good EBM Summary Database? • Comprehensive literature search • Pre-appraised – – Appraisal methods Based around clinical questions and patient outcomes Inclusion and Exclusion criteria Preference for systematic reviews over individual studies • Regularly updated • Easy access and use • Links to original paper
Does BMJ Clinical Evidence “fit the bill”? ü Comprehensive literature search ü Pre-appraised ü ü Appraisal methods Based around clinical questions and patient outcomes Inclusion and Exclusion criteria Preference for systematic reviews over individual studies ü Regularly updated ü Links to original paper • Easy access and use
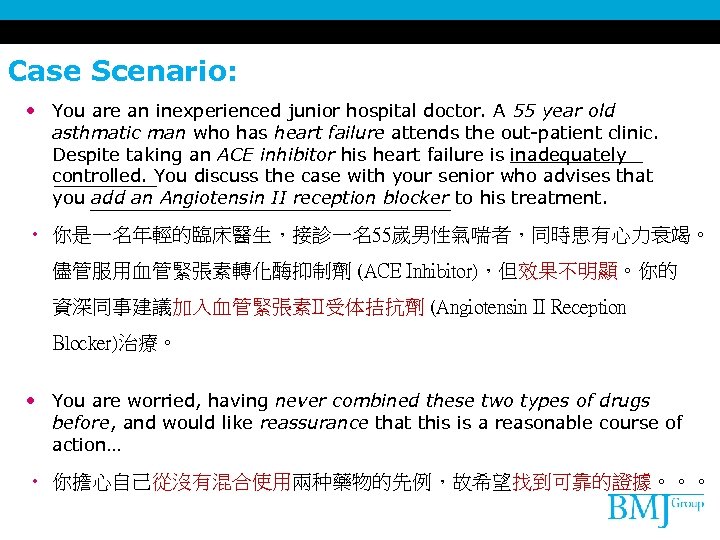
Case Scenario: • You are an inexperienced junior hospital doctor. A 55 year old asthmatic man who has heart failure attends the out-patient clinic. Despite taking an ACE inhibitor his heart failure is inadequately controlled. You discuss the case with your senior who advises that you add an Angiotensin II reception blocker to his treatment. • 你是一名年輕的臨床醫生,接診一名55嵗男性氣喘者,同時患有心力衰竭。 儘管服用血管緊張素轉化酶抑制劑 (ACE Inhibitor),但效果不明顯。你的 資深同事建議加入血管緊張素II受体拮抗劑 (Angiotensin II Reception Blocker)治療。 • You are worried, having never combined these two types of drugs before, and would like reassurance that this is a reasonable course of action… • 你擔心自己從沒有混合使用兩种藥物的先例,故希望找到可靠的證據。。。
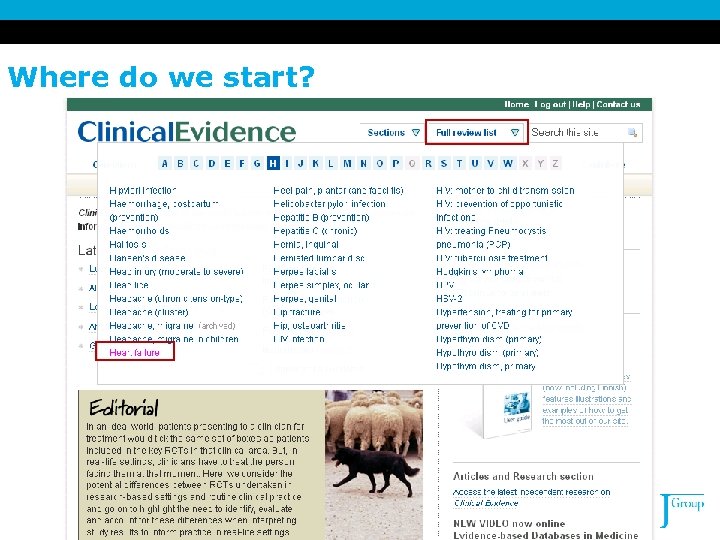
Where do we start?

Does BMJ Clinical Evidence “fit the bill”? ü Comprehensive literature search ü Pre-appraised ü ü Appraisal methods Based around clinical questions and patient outcomes Inclusion and Exclusion criteria Preference for systematic reviews over individual studies ü Regularly updated ü Links to original paper ü Easy access and use
Pop Quiz 2: • Which of the following are features of Clinical Evidence? A. Covers the benefits and harms of each intervention B. Summarises the condition based on key questions asked by clinicians, summary and background of the condition C. Produced by an international panel of clinicians using rigorous searching and evaluation methods D. All of the above
New and Upcoming! - New BMJ Evidence Centre Upcoming BMJ Best Practice
The New BMJ Evidence Centre The new hub of evidence-based medicine… http: //group. bmj. com/products/evidence-centre
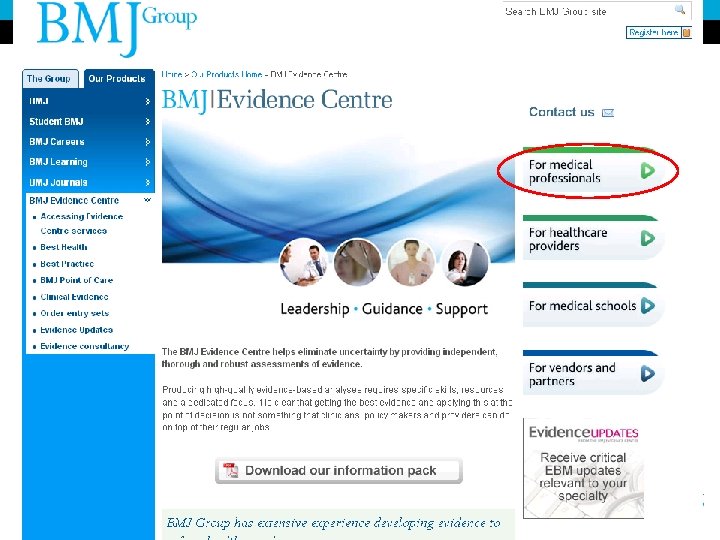


New in January 2009
What is BMJ Best Practice ? • Point of Care tool / Decision Support tool • Combination of Evidence, Expert Opinion and Guidelines • Common conditions primary & secondary care • Structured and set by step approach • Summary, Basic / Background Info, Prevention, Diagnosis, Treatments, Evidence, Drugs, follow up & patient info
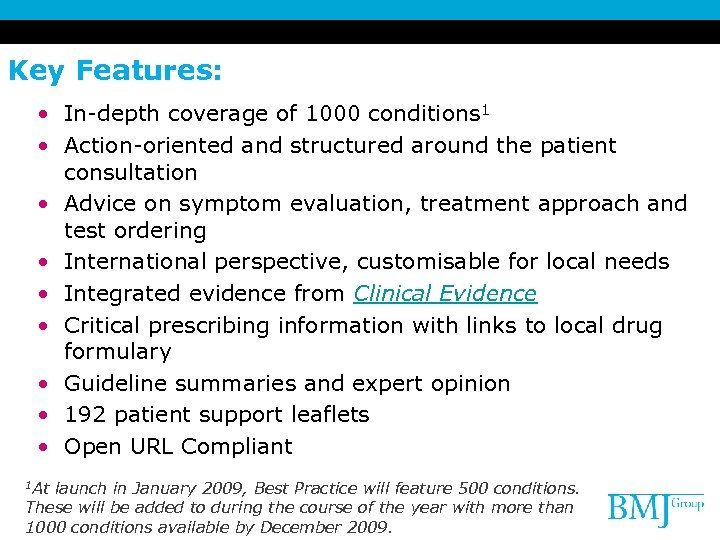
Key Features: • In-depth coverage of 1000 conditions 1 • Action-oriented and structured around the patient consultation • Advice on symptom evaluation, treatment approach and test ordering • International perspective, customisable for local needs • Integrated evidence from Clinical Evidence • Critical prescribing information with links to local drug formulary • Guideline summaries and expert opinion • 192 patient support leaflets • Open URL Compliant 1 At launch in January 2009, Best Practice will feature 500 conditions. These will be added to during the course of the year with more than 1000 conditions available by December 2009.
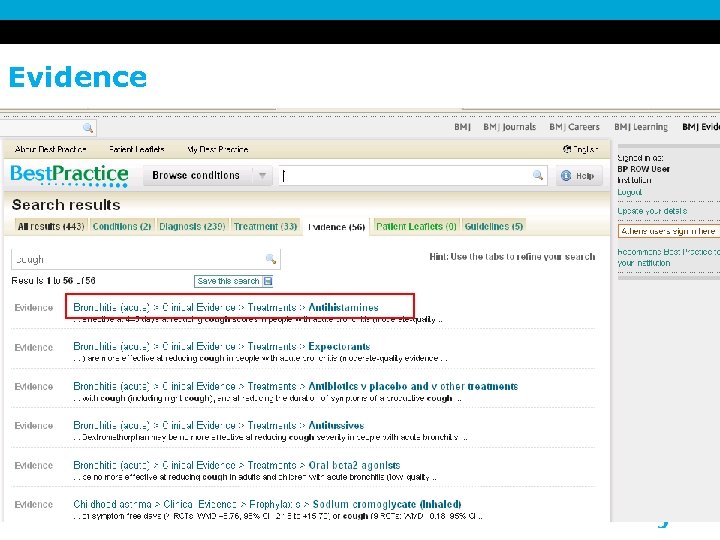
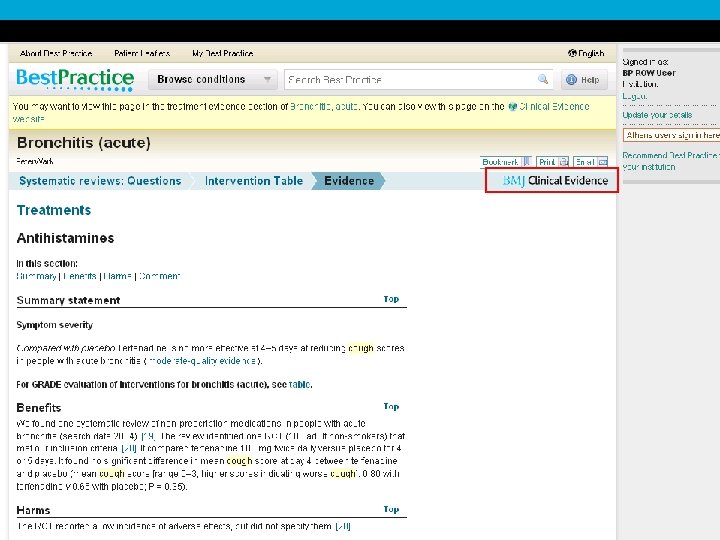
Evidence
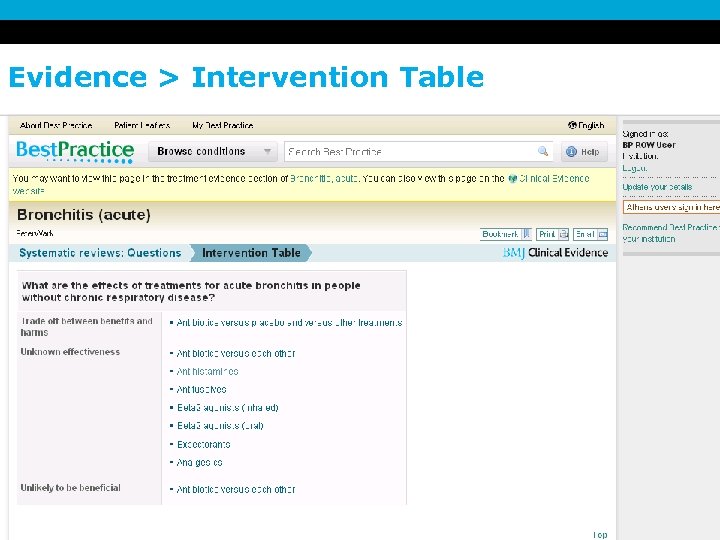
Evidence > Intervention Table
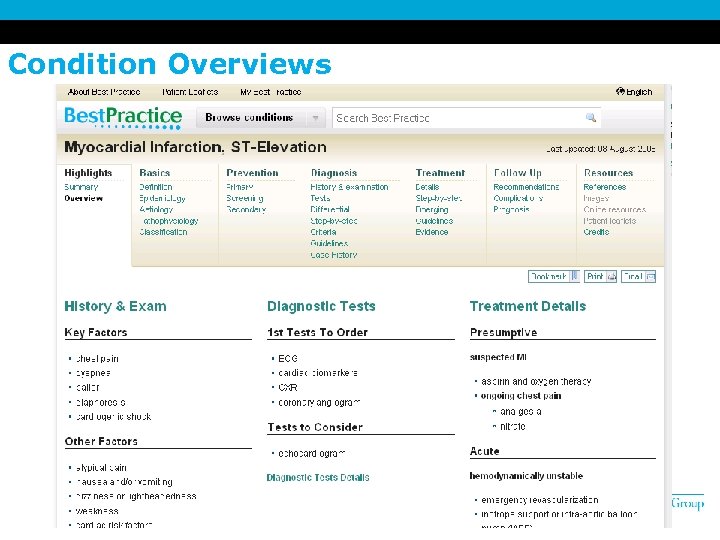
Condition Overviews
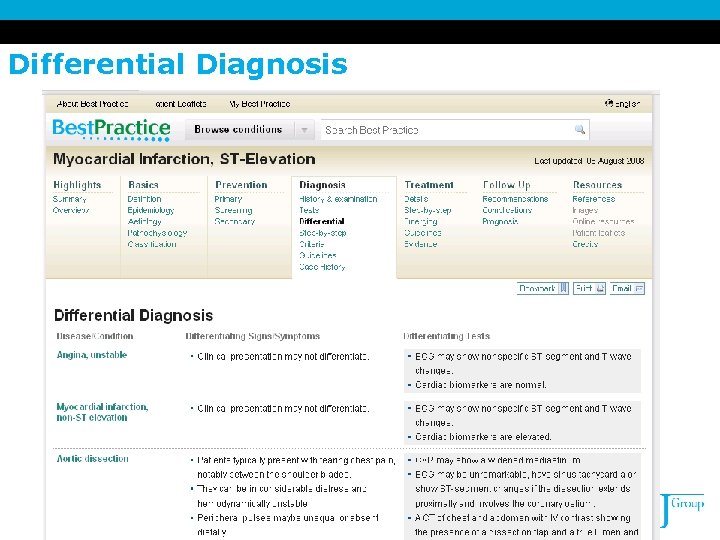
Differential Diagnosis
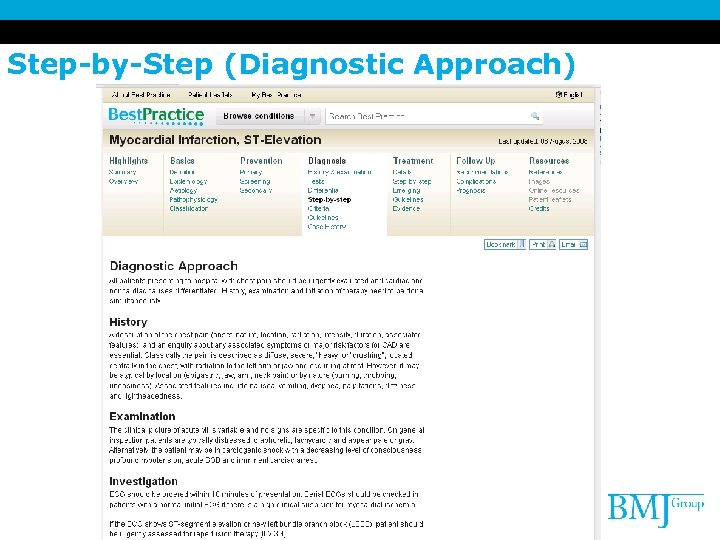
Step-by-Step (Diagnostic Approach)
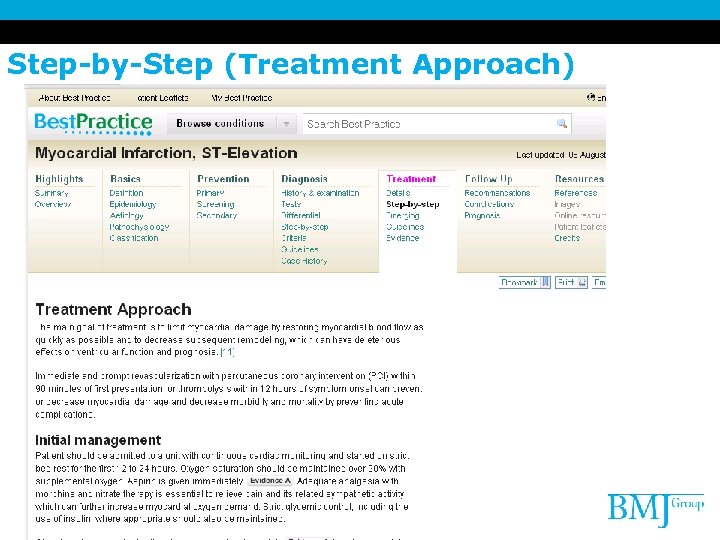
Step-by-Step (Treatment Approach)
Images
My Best Practice
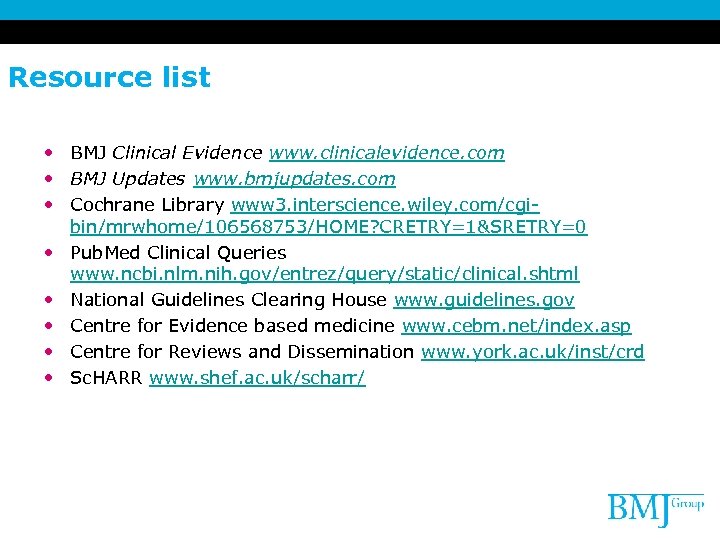
Resource list • BMJ Clinical Evidence www. clinicalevidence. com • BMJ Updates www. bmjupdates. com • Cochrane Library www 3. interscience. wiley. com/cgibin/mrwhome/106568753/HOME? CRETRY=1&SRETRY=0 • Pub. Med Clinical Queries www. ncbi. nlm. nih. gov/entrez/query/static/clinical. shtml • National Guidelines Clearing House www. guidelines. gov • Centre for Evidence based medicine www. cebm. net/index. asp • Centre for Reviews and Dissemination www. york. ac. uk/inst/crd • Sc. HARR www. shef. ac. uk/scharr/

Thank you Dju-Lyn Chng BMJ Group dlchng@bmjgroup. com
7c3afefc968a1bd2e028eaaa8c9e234a.ppt