breast feeding - Copy.ppt
- Количество слайдов: 64
Breastfeeding and Human Milk Properties AAP Policy Statement: Breastfeeding and the Use of Human Milk. Pediatrics 2005; 115; 496 -506. WHO: Breast Feeding http: //www. who. int/topics/breastfeeding/en/ 1
ﺍﺍﺍ ) ﻻ
Learning Objectives Describe why breast feeding is the best source of nourishment for infants and young children Describe the quantity and quality of components in breast milk Describe the beneficial impact on infant’s health, maternal condition, and socio-environment Describe the few contraindications and common challenges of breast feeding, which could be faced in clinical practice by parents and clinicians 3

Content Breast feeding - definition, goal & rates Human milk ◦ Composition ◦ Functional components ◦ Benefits ◦ Relative contradictions Support system 4

Definition & Goal Exclusive breast feeding is defined as the consumption of human milk with no supplementation of any type except for vitamins and medications Breast feeding is the best nutrition and health protection for the first 6 months of life Breast feeding with complementary foods for at least 12 months is the ideal feeding pattern for infants Exclusive breast feeding rate target in the US: ◦ 75% at initiation ◦ 50% at 6 months ◦ 25% at 12 months Agostoni C, et al. J Pediatr Gastroenterol Nutr 2008; 46: 99 -110. http: //www. healthypeople. gov/document/HTML/Volume 2/16 MICH. htm 5

Breast Feeding Rates From 1970 through 1990 breast feeding dropped ◦ More mothers stepped into the workplace ◦ Easier access to commercial infant formula ◦ Misunderstandings of breast feeding Since 2000: ◦ Recognition of the benefits of breast feeding by the public and by health professionals made breast feeding initiation rates increase gradually 6

Global Breast Feeding Rates At 4 months: At 6 months: 33% in the US Breast feeding rate in Taiwan is unsatisfactory In 2004: ◦ 66% in Norway ◦ 41% in Japan ◦ 28% in Vietnam ◦ Immediately postpartum, 50% of mothers breast fed ◦ At 1 month, 29%-33% exclusively breast fed ◦ At 6 months, 13% exclusively breast fed & 20% supplemented breast feeding with formula feeding WHO Global Data Bank on Breastfeeding and Complementary Feeding http: //apps. who. int/research/iycf/bfcf/ 7
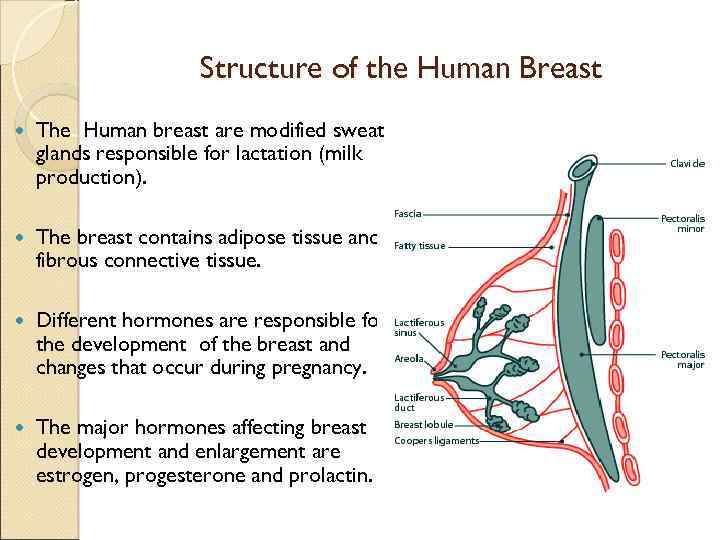
Structure of the Human Breast The Human breast are modified sweat glands responsible for lactation (milk production). The breast contains adipose tissue and fibrous connective tissue. Different hormones are responsible for the development of the breast and changes that occur during pregnancy. The major hormones affecting breast development and enlargement are estrogen, progesterone and prolactin.
Structure of the Human Breast (Cont’d) Each breast contains about 20 lobes, each lobes contains several lobules which at the end have alveolar in which milk is produced. Milk production and secretion are responsive to two major hormones – prolactin and oxytocin; and the sucking reflex. After production of milk in the alveolus, the milk moves through the ducts and are stored in the lactiferous sinus. When the infant latches on the breast, milk is expressed from the sinuses.
Suckling Hormonal Reflex Arc (Cont’d) The sucking reflex arc is a hormonal positive feedback mechanism. The sucking of the breast by the infant stimulates the nipple; this sends messages to the spinal cord and subsequently to the brain. Prolactin is released from the anterior pituitary for milk production and oxytocin from the posterior pituitary for the milk let down. Prolactin receptors are established within the first eight days of delivery. Suckling at breast increases prolactin levels, so at each feeding, levels rise, hence more milk production.
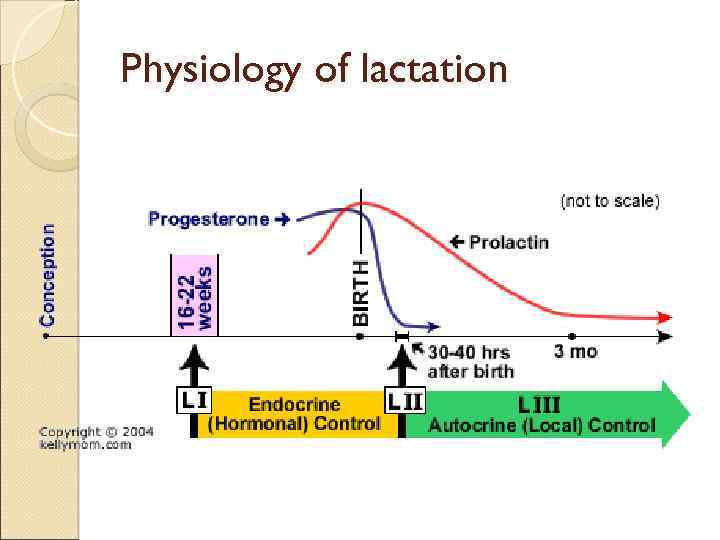
Physiology of lactation Lactation and milk production goes into 3 stages: 1. Lactogenesis I 2. Lactogenesis II 3. Lactogenesis III Lactogenesis ( I & II ) milk supply is hormonally driven endocrine control system. Lactogenesis III switch to the autocrine (or local) control system.
Physiology of lactation
Physiology of lactation The mother will start making colostrum about halfway through pregnancy (Lactogenesis I), but high levels of progesterone inhibit milk secretion. At birth, the delivery of the progesterone/estrogen placenta results in a sudden drop in Prolactine progesterone/estrogen levels. Lactogenesis II
Physiology of lactation After Lactogenesis II, there is a switch to the autocrine (or local) control system (Lactogenesis III ) Maintenance stage of milk production Milk removal is the primary control mechanism for supply. Under normal circumstances, the breasts will continue to make milk indefinitely as long as milk removal continues.
Neonatal feeding reflexes: 1) Rooting reflex: touching the check or circumaural area leads to turning the head to the side of the stimulus leading to opening the mouth seeking for the nipple. 2) Suckling reflex: tactile stimuli of the nipple or aereolar tissue filling the mouth leading to milking action by tongue against hard palate.
3) Swallowing reflex: follows suckling or allows interruption to breathing to prevent choking during swallowing.
Facts about babies and newborns. They are considered as immunocompromised due to there immature immunity. 2. Thy need a high amount of energy for growth and development. 1. 3. There renal solute load is low. 4. There different organs and systems are still not 100% mature. Breast Milk is tailored to help coping with these different immaturity aspects
Composition of breast milk: Colostrum: üSmall amount during days 3 up to 5. üThin yellowish fluid, provide passive immunity to the baby. üHigh in protein, immunoglobulins and minerals. üLow in lactose and fat. Bright lemon yellow ; alkaline ; viscous fluid secreted during first 5 -7 days : compared to mature milk it is : 1) More rich in protein (2. 3 gm/dl) but less CHO or fat.
2) Very rich in immunoglobulin especially Ig. A. 3) rich in cholesterol , Na , K , Cl , Zinc , Copper , leucocytes ( macrophages , lymphocytes ) Antibacterial ( lactofissin , lactofirrin ) more rich in Vit. A than mature milk.
4) Laxative effect by enhancing GIT motility leading to prevention of meconium blood formation which is the most common cause intestinal destruction. 5) reducing enterohepatic circulation and prevent hyperbilirubinaemia.
Milk composition: Transitional milk: ü produced during days 4 to 10 üHigh in fat, lactose üLower in protein and minerals
Milk composition: Mature milk: available by 2 weeks postpartum. üMilk yield: 750 ml/d üProvides 67 kcal/100 ml ü 60 -80% whey protein. ü 7% Lactose provides 40% of caloric need. ü 4% fat Provides 50% of the caloric need üGrowth promoting factors üLow in vitamin D
Breast feeding Nowadays there is a world wide efforts to rise the awareness of the importance of breast feeding for the benefit of the baby, and better health for all humans. WHO strongly recommends exclusive breastfeeding for the first six months of life. Exclusive Breast Feeding Breast milk ONLY, and no other foods or liquids. Not even water !!
Signs of Effective Breastfeeding Frequent feedings 8 -12 times daily. Intermittent episodes of rhythmic sucking with audible swallows should be heard while the infant is nursing. Infant should have about 6 -8 wet diapers in a 24 hour period once breast feeding is established. Infant should have minimum of 3 -4 bowel movements every 24 hours. Stools should be about one tablespoon or larger and should be soft and yellow after day 3. Average daily weight gain of 15 -30 g. Infant has regained birth weight by day 10 of life.
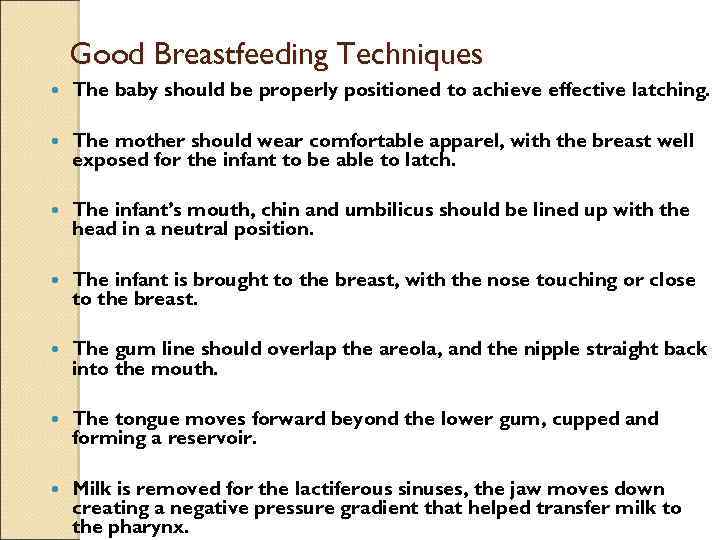
Good Breastfeeding Techniques The baby should be properly positioned to achieve effective latching. The mother should wear comfortable apparel, with the breast well exposed for the infant to be able to latch. The infant’s mouth, chin and umbilicus should be lined up with the head in a neutral position. The infant is brought to the breast, with the nose touching or close to the breast. The gum line should overlap the areola, and the nipple straight back into the mouth. The tongue moves forward beyond the lower gum, cupped and forming a reservoir. Milk is removed for the lactiferous sinuses, the jaw moves down creating a negative pressure gradient that helped transfer milk to the pharynx.
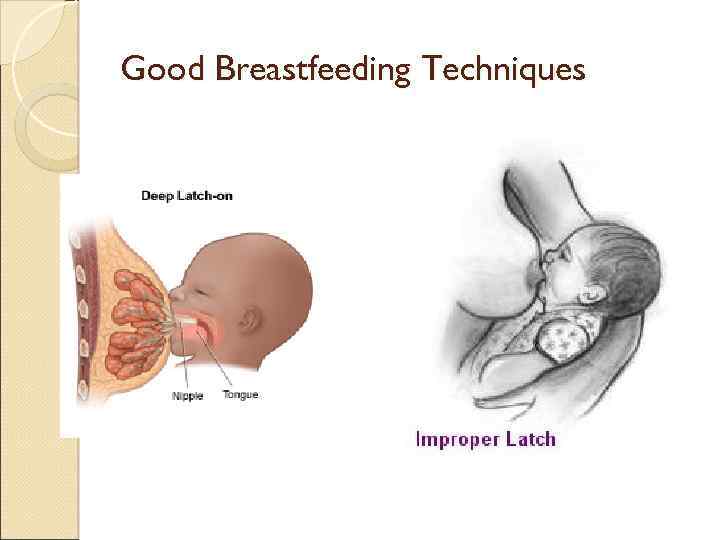
Good Breastfeeding Techniques
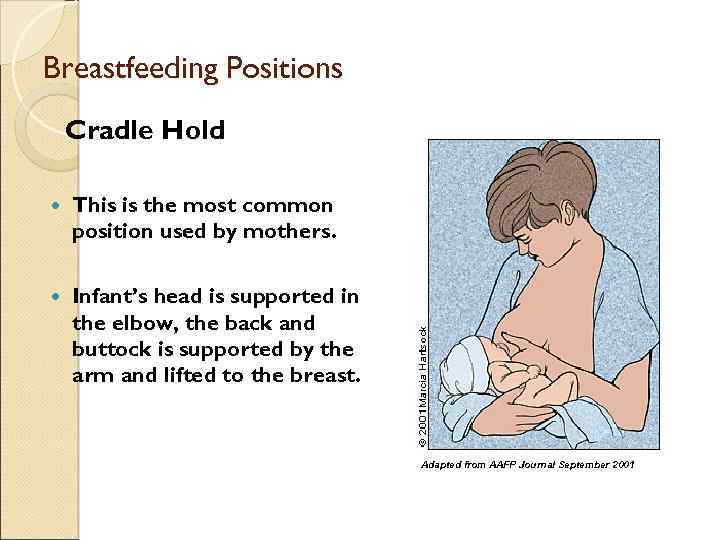
Breastfeeding Positions Cradle Hold This is the most common position used by mothers. Infant’s head is supported in the elbow, the back and buttock is supported by the arm and lifted to the breast. Adapted from AAFP Journal September 2001
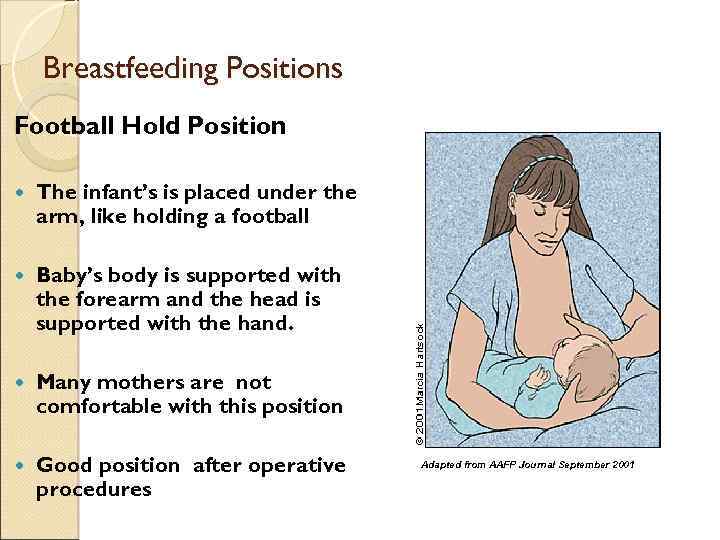
Breastfeeding Positions Football Hold Position The infant’s is placed under the arm, like holding a football Baby’s body is supported with the forearm and the head is supported with the hand. Many mothers are not comfortable with this position Good position after operative procedures Adapted from AAFP Journal September 2001
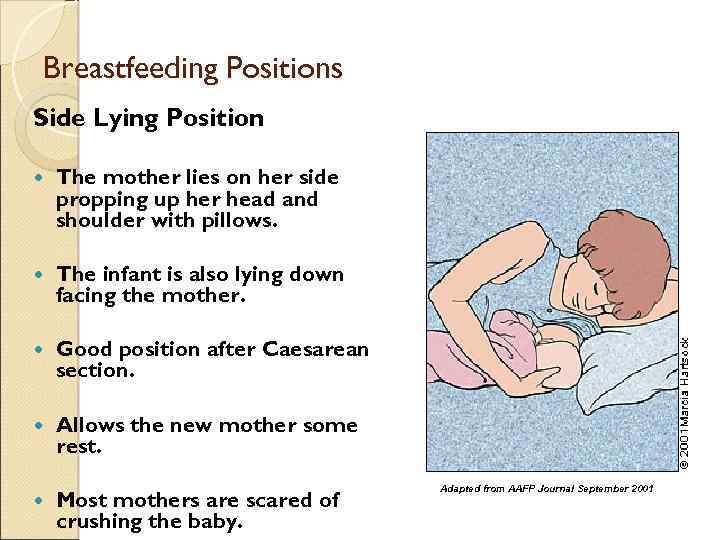
Breastfeeding Positions Side Lying Position The mother lies on her side propping up her head and shoulder with pillows. The infant is also lying down facing the mother. Good position after Caesarean section. Allows the new mother some rest. Most mothers are scared of crushing the baby. Adapted from AAFP Journal September 2001
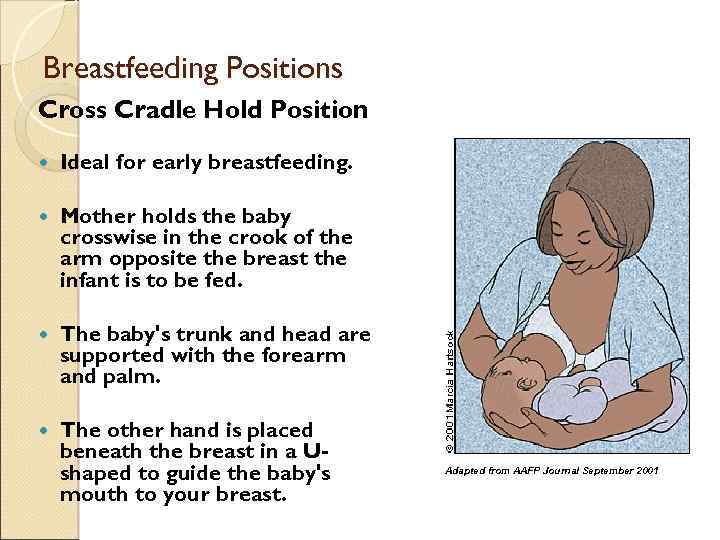
Breastfeeding Positions Cross Cradle Hold Position Ideal for early breastfeeding. Mother holds the baby crosswise in the crook of the arm opposite the breast the infant is to be fed. The baby's trunk and head are supported with the forearm and palm. The other hand is placed beneath the breast in a Ushaped to guide the baby's mouth to your breast. Adapted from AAFP Journal September 2001
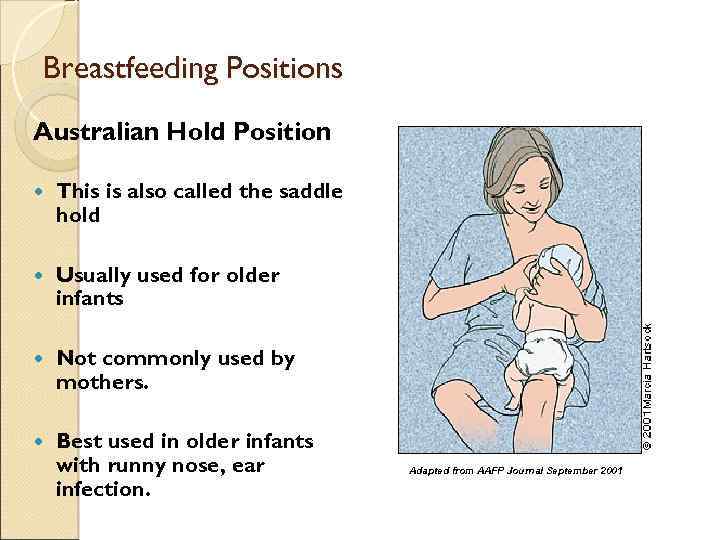
Breastfeeding Positions Australian Hold Position This is also called the saddle hold Usually used for older infants Not commonly used by mothers. Best used in older infants with runny nose, ear infection. Adapted from AAFP Journal September 2001
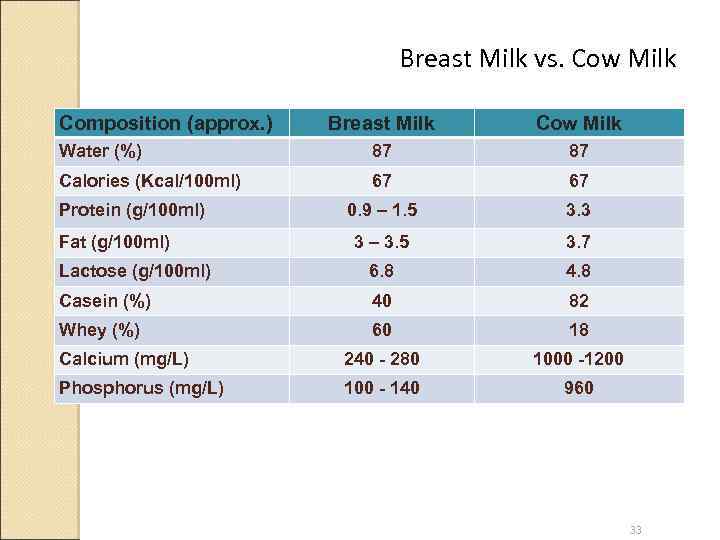
Breast Milk vs. Cow Milk Composition (approx. ) Breast Milk Cow Milk Water (%) 87 87 Calories (Kcal/100 ml) 67 67 0. 9 – 1. 5 3. 3 3 – 3. 5 3. 7 Lactose (g/100 ml) 6. 8 4. 8 Casein (%) 40 82 Whey (%) 60 18 Calcium (mg/L) 240 - 280 1000 -1200 Phosphorus (mg/L) 100 - 140 960 Protein (g/100 ml) Fat (g/100 ml) 33
Breast Milk Contains: Macronutrients ◦ Protein ◦ Fat ◦ Carbohydrate Micronutrients ◦ Minerals ◦ Vitamins Enzymes, hormones, growth factors, immune globulins, trace elements and cells 34
Protein 75% of the nitrogen-containing compounds in breast milk: ◦ Aqueous whey ◦ Micellar casein ◦ Ratio varies considerably during lactation Non-protein nitrogen substances include urea, nucleotides, peptides, free amino acids, and DNA Colostrum: ◦ Protein: 2. 5 gm/dl ◦ Rich in cells ◦ Provides numerous immune factors - secretory Ig. A and lactoferrin ◦ Relatively low fat 35
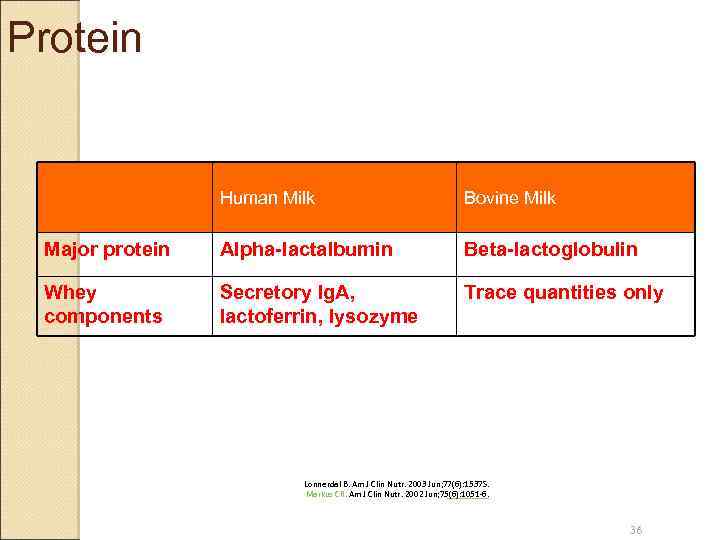
Protein Human Milk Bovine Milk Major protein Alpha-lactalbumin Beta-lactoglobulin Whey components Secretory Ig. A, lactoferrin, lysozyme Trace quantities only Lonnerdal B. Am J Clin Nutr. 2003 Jun; 77(6): 1537 S. Markus CR. Am J Clin Nutr. 2002 Jun; 75(6): 1051 -6. 36
Fat About 50% of kcal More than 98% as triglycerides ◦ Oleic acid (18: 1), palmitic acid (16: 0) are the most abundant fatty acids Human milk: palmitic acid esterified to center or 2 -position of the triglyceride Vegetable oil: palmitic acid esterified mainly at external or 1 - & 3 -positions Human milk has significant beneficial effects on intestinal absorption of fat and calcium in healthy term infants 37
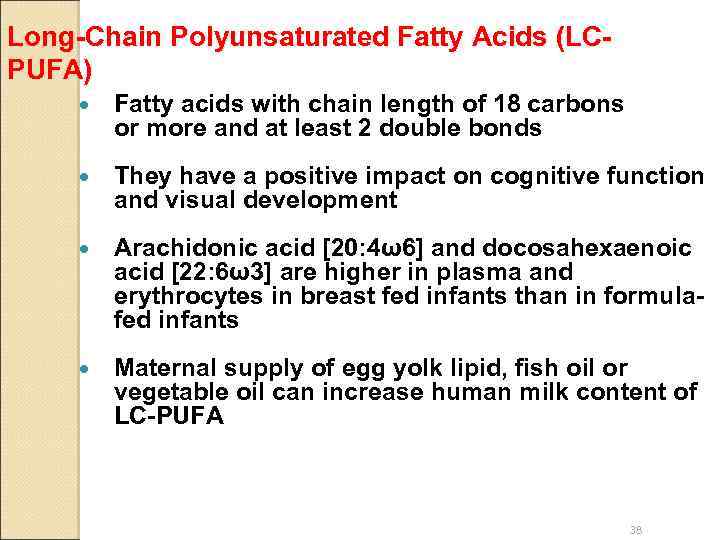
Long-Chain Polyunsaturated Fatty Acids (LCPUFA) Fatty acids with chain length of 18 carbons or more and at least 2 double bonds They have a positive impact on cognitive function and visual development Arachidonic acid [20: 4ω6] and docosahexaenoic acid [22: 6ω3] are higher in plasma and erythrocytes in breast fed infants than in formulafed infants Maternal supply of egg yolk lipid, fish oil or vegetable oil can increase human milk content of LC-PUFA 38
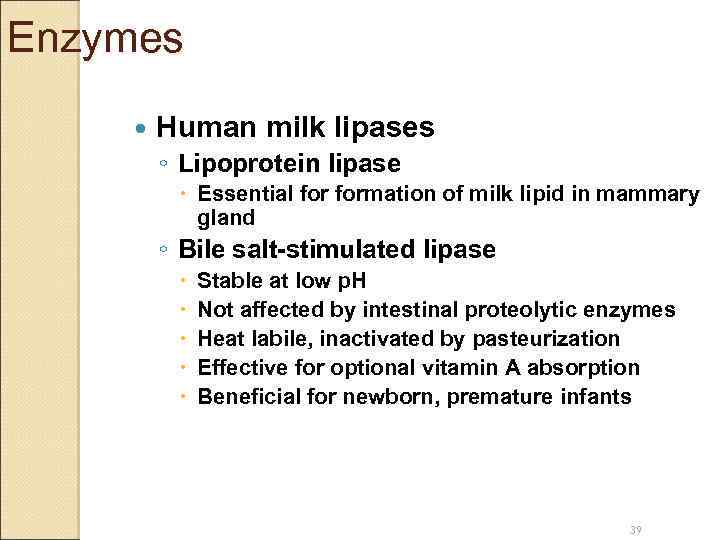
Enzymes Human milk lipases ◦ Lipoprotein lipase Essential formation of milk lipid in mammary gland ◦ Bile salt-stimulated lipase Stable at low p. H Not affected by intestinal proteolytic enzymes Heat labile, inactivated by pasteurization Effective for optional vitamin A absorption Beneficial for newborn, premature infants 39
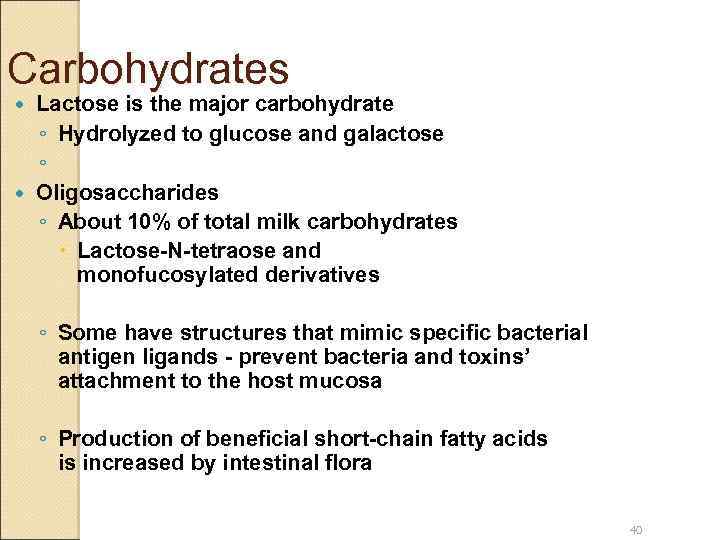
Carbohydrates Lactose is the major carbohydrate ◦ Hydrolyzed to glucose and galactose ◦ Oligosaccharides ◦ About 10% of total milk carbohydrates Lactose-N-tetraose and monofucosylated derivatives ◦ Some have structures that mimic specific bacterial antigen ligands - prevent bacteria and toxins’ attachment to the host mucosa ◦ Production of beneficial short-chain fatty acids is increased by intestinal flora 40
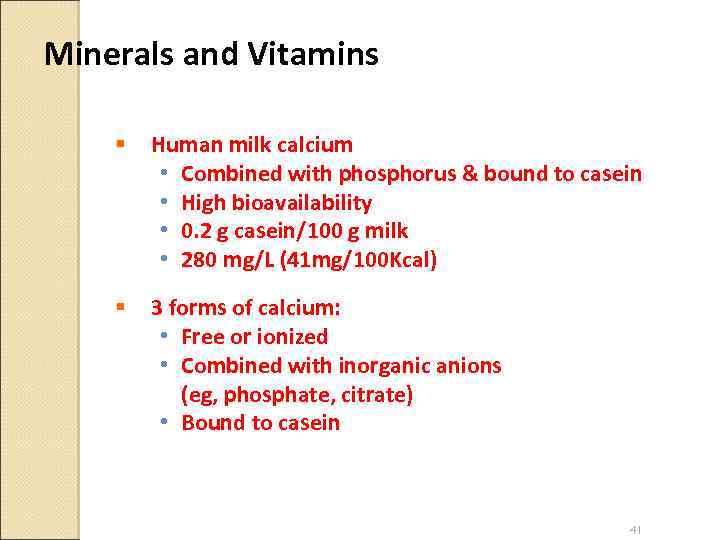
Minerals and Vitamins § Human milk calcium • Combined with phosphorus & bound to casein • High bioavailability • 0. 2 g casein/100 g milk • 280 mg/L (41 mg/100 Kcal) § 3 forms of calcium: • Free or ionized • Combined with inorganic anions (eg, phosphate, citrate) • Bound to casein 41

Iron § Infants born with abundant iron stores • Meet the infant’s requirement until 4 to 6 months • Low birth weight, preterm infants need supplementation § Iron absorption from a variety of foods is about 1% § Iron absorption from human milk is greater than 50% § At 6 months, breast fed infants need 1 mg iron supplementation/kg/day Dee DL, et al. Pediatrics 2008; 122: S 98 -S 104. American Academy of Pediatrics. Pediatric Nutrition Handbook. 6 th ed. Elk Grove Village, IL: American Academy of Pediatrics; 2009. 42
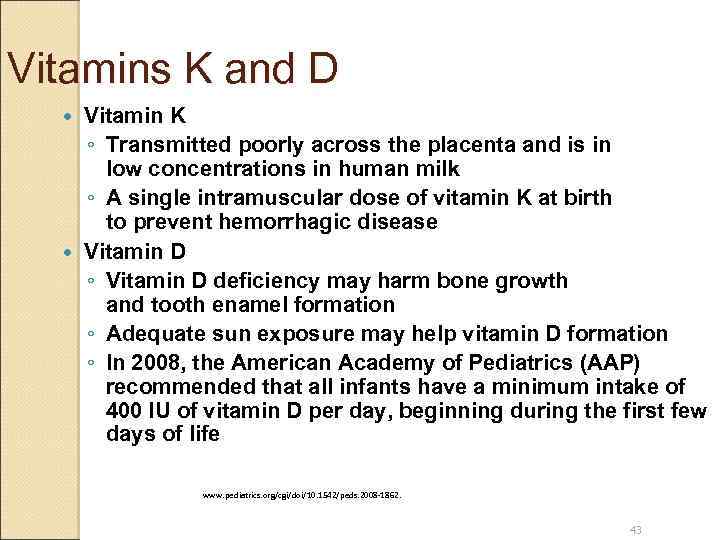
Vitamins K and D Vitamin K ◦ Transmitted poorly across the placenta and is in low concentrations in human milk ◦ A single intramuscular dose of vitamin K at birth to prevent hemorrhagic disease Vitamin D ◦ Vitamin D deficiency may harm bone growth and tooth enamel formation ◦ Adequate sun exposure may help vitamin D formation ◦ In 2008, the American Academy of Pediatrics (AAP) recommended that all infants have a minimum intake of 400 IU of vitamin D per day, beginning during the first few days of life www. pediatrics. org/cgi/doi/10. 1542/peds. 2008 -1862. 43
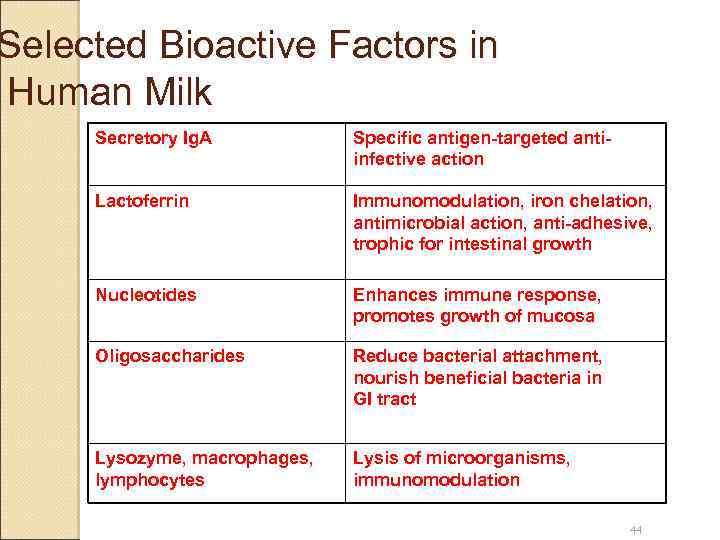
Selected Bioactive Factors in Human Milk Secretory Ig. A Specific antigen-targeted antiinfective action Lactoferrin Immunomodulation, iron chelation, antimicrobial action, anti-adhesive, trophic for intestinal growth Nucleotides Enhances immune response, promotes growth of mucosa Oligosaccharides Reduce bacterial attachment, nourish beneficial bacteria in GI tract Lysozyme, macrophages, lymphocytes Lysis of microorganisms, immunomodulation 44
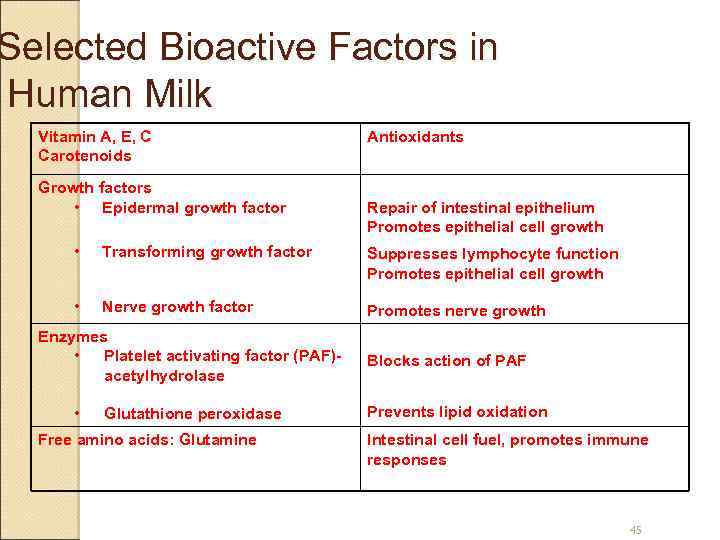
Selected Bioactive Factors in Human Milk Vitamin A, E, C Carotenoids Growth factors • Epidermal growth factor Antioxidants Repair of intestinal epithelium Promotes epithelial cell growth • Transforming growth factor Suppresses lymphocyte function Promotes epithelial cell growth • Nerve growth factor Promotes nerve growth Enzymes • Platelet activating factor (PAF)acetylhydrolase • Glutathione peroxidase Free amino acids: Glutamine Blocks action of PAF Prevents lipid oxidation Intestinal cell fuel, promotes immune responses 45

Breast Feeding: Benefits for Infants Preventing infectious diseases ◦ Bacterial meningitis, bacteremia, diarrhea, respiratory tract infection, necrotizing enterocolitis, otitis media, urinary tract infection, and late-onset sepsis in preterm infants Reduced chronic diseases/conditions ◦ Sudden infant death syndrome, diabetes, lymphoma, leukemia, Hodgkin’s disease, obesity, hypercholesterolemia, atopy, asthma Neurobehavioral aspects ◦ Cognitive development Pediatrics 2005; 115: 496 -506. (http: //aappolicy. aappublications. org/cgi/content/full/pediatrics; 115/2/496). 46
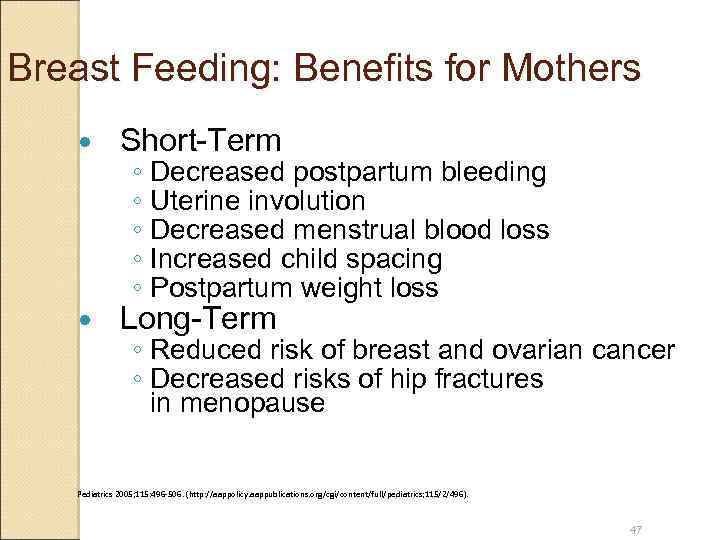
Breast Feeding: Benefits for Mothers Short-Term Long-Term ◦ Decreased postpartum bleeding ◦ Uterine involution ◦ Decreased menstrual blood loss ◦ Increased child spacing ◦ Postpartum weight loss ◦ Reduced risk of breast and ovarian cancer ◦ Decreased risks of hip fractures in menopause Pediatrics 2005; 115: 496 -506. (http: //aappolicy. aappublications. org/cgi/content/full/pediatrics; 115/2/496). 47
Breast Feeding: Benefits for Communities Decreased annual health care costs Decreased public health program costs Decreased absenteeism ◦ Decreased loss of family income More time for siblings and family matters Decreased environmental burdens Pediatrics 2005; 115: 496 -506. (http: //aappolicy. aappublications. org/cgi/content/full/pediatrics; 115/2/496). 48
Breast Feeding: Do NOT recommend when: Infants The baby is diagnosed with galactosemia, or other inborn errors of metabolism Mothers Infected with the human immunodeficiency virus (HIV) Those with human T-cell lymphotropic virus Herpetic lesions localized to the breast Untreated active pulmonary tuberculosis Is taking prescribed cancer chemotherapy agents, such as antimetabolites Is using or dependent upon an illicit drug Is taking antiretroviral medications Is undergoing radiation therapies 49
Breast Feeding: Conditions that are NOT Contraindications Mothers who are infected with hepatitis B or hepatitis C virus Mothers who are seropositive carriers of cytomegalovirus (CMV) Mothers who are febrile unless cause is a contraindication previously outlined Mothers who have been exposed to lowlevel environmental chemical agents Tobacco smoking Breastfeeding mothers who use alcoholic beverages 50
Counseling and FAQ … A mother has mastitis, Does she continue breastfeeding or not ? ! ◦ Breast feeding is NOT contraindicated in mastitis. What about breast abscess ? ! ◦ The mother can nurse form the contralateral breast.
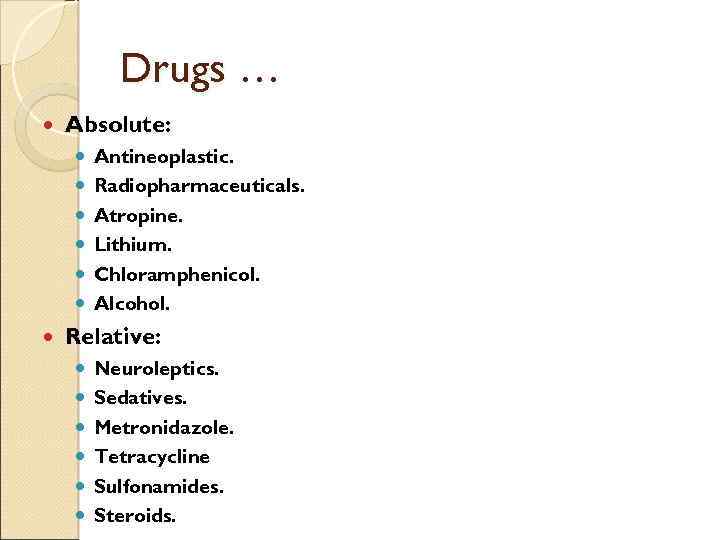
Drugs … Absolute: Antineoplastic. Radiopharmaceuticals. Atropine. Lithium. Chloramphenicol. Alcohol. Relative: Neuroleptics. Sedatives. Metronidazole. Tetracycline Sulfonamides. Steroids.
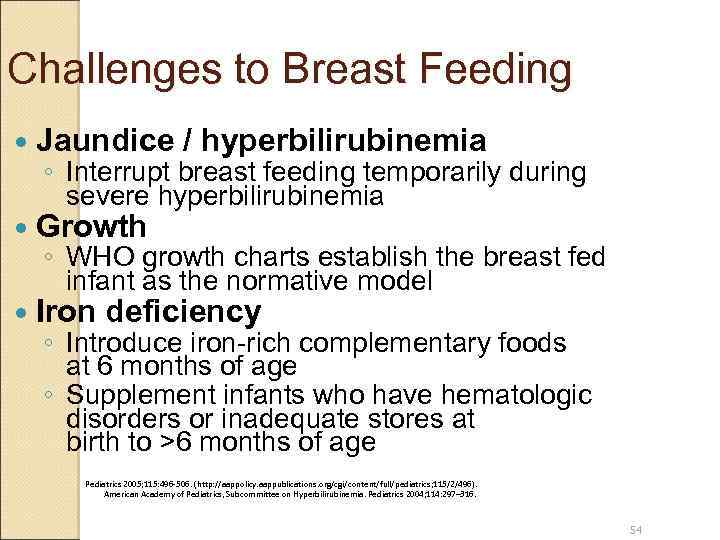
Challenges to Breast Feeding Jaundice / hyperbilirubinemia Growth Iron deficiency ◦ Interrupt breast feeding temporarily during severe hyperbilirubinemia ◦ WHO growth charts establish the breast fed infant as the normative model ◦ Introduce iron-rich complementary foods at 6 months of age ◦ Supplement infants who have hematologic disorders or inadequate stores at birth to >6 months of age Pediatrics 2005; 115: 496 -506. (http: //aappolicy. aappublications. org/cgi/content/full/pediatrics; 115/2/496). American Academy of Pediatrics, Subcommittee on Hyperbilirubinemia. Pediatrics 2004; 114: 297– 316. 54
Obstacles to Breast Feeding Insufficient prenatal education about breast feeding Inappropriate hospital policies and practices Lack postpartum home health visits and routine follow-up care Maternal employment Lack of family and broad societal support Commercial promotion and media portrayal of bottle feeding as normative Lack of guidance and encouragement from health care professionals 55
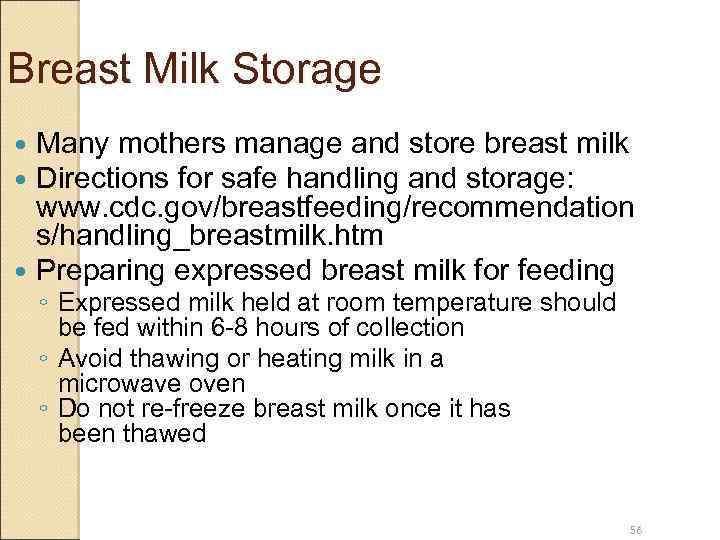
Breast Milk Storage Many mothers manage and store breast milk Directions for safe handling and storage: www. cdc. gov/breastfeeding/recommendation s/handling_breastmilk. htm Preparing expressed breast milk for feeding ◦ Expressed milk held at room temperature should be fed within 6 -8 hours of collection ◦ Avoid thawing or heating milk in a microwave oven ◦ Do not re-freeze breast milk once it has been thawed 56
Support Systems A successful practice of breast feeding requires education and support: ◦ Breastfeeding Helpline: The DHHS Office on Women’s Health http: //www. 4 woman. gov/Breastfeeding/index. cfm? page=ask ◦ Breastfeeding for Parents La Leche League International http: //www. lalecheleague. org/nb. html ◦ One-on-One Consultation The International Lactation Consultant Association http: //www. ilca. org/ ◦ Local communities’ hotline 57
10 Steps to Successful Breast Feeding 1. Have a written breast feeding policy that is routinely communicated to all health care staff 2. Train all health care staff in skills necessary to implement this policy 3. Inform all pregnant women about the benefits and management of breast feeding 4. Help mothers initiate breast feeding within half an hour of birth 5. Show mothers how to breast feed and how to maintain lactation even if they should be separated from their infants http: //www. unicef. org/programme/breastfeeding/baby. htm 58
10 Steps to Successful Breast Feeding 6. Give newborn infants no other foods or drinks besides breast milk, unless medically indicated 7. Practice “rooming-in, ” that is, allow mothers and infants to remain together 24 hours a day 8. Encourage breast feeding on demand 9. Do not give artificial teats or pacifiers (also called dummies or soothers) to breast feeding infants 10. Foster the establishment of breast feeding support groups and refer mothers to them upon discharge from the hospital or clinic http: //www. unicef. org/programme/breastfeeding/baby. htm 59
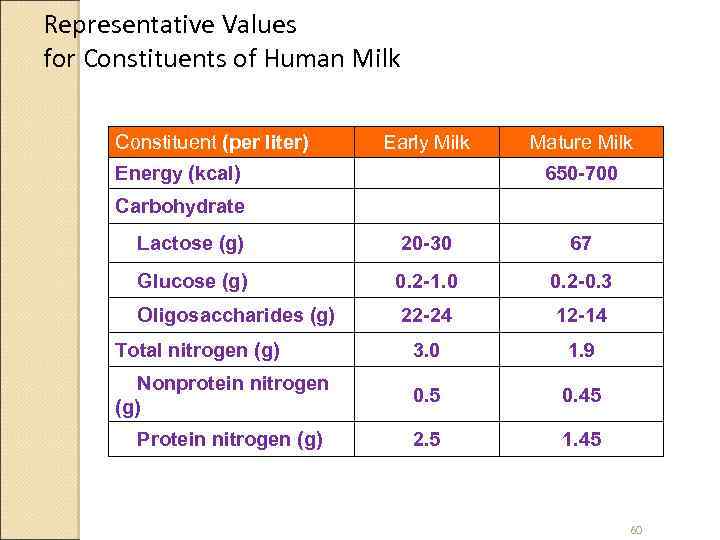
Representative Values for Constituents of Human Milk Constituent (per liter) Early Milk Energy (kcal) Mature Milk 650 -700 Carbohydrate Lactose (g) 20 -30 67 Glucose (g) 0. 2 -1. 0 0. 2 -0. 3 Oligosaccharides (g) 22 -24 12 -14 Total nitrogen (g) 3. 0 1. 9 Nonprotein nitrogen (g) 0. 5 0. 45 2. 5 1. 45 Protein nitrogen (g) 60
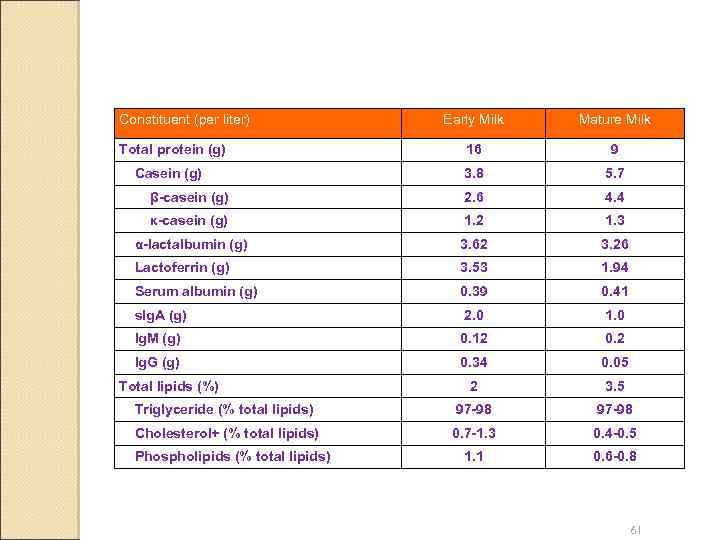
Constituent (per liter) Early Milk Mature Milk Total protein (g) 16 9 Casein (g) 3. 8 5. 7 β-casein (g) 2. 6 4. 4 κ-casein (g) 1. 2 1. 3 α-lactalbumin (g) 3. 62 3. 26 Lactoferrin (g) 3. 53 1. 94 Serum albumin (g) 0. 39 0. 41 s. Ig. A (g) 2. 0 1. 0 Ig. M (g) 0. 12 0. 2 Ig. G (g) 0. 34 0. 05 2 3. 5 Triglyceride (% total lipids) 97 -98 Cholesterol+ (% total lipids) 0. 7 -1. 3 0. 4 -0. 5 1. 1 0. 6 -0. 8 Total lipids (%) Phospholipids (% total lipids) 61
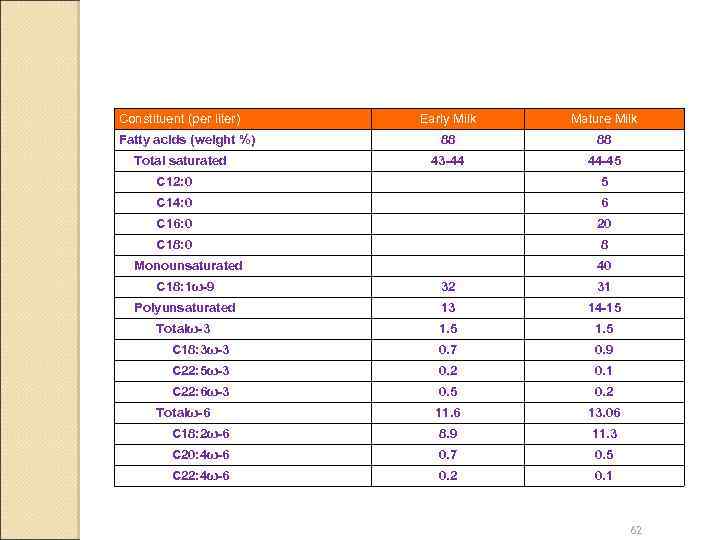
Constituent (per liter) Fatty acids (weight %) Total saturated Early Milk Mature Milk 88 88 43 -44 44 -45 C 12: 0 5 C 14: 0 6 C 16: 0 20 C 18: 0 8 Monounsaturated 40 C 18: 1ω-9 32 31 Polyunsaturated 13 14 -15 Totalω-3 1. 5 C 18: 3ω-3 0. 7 0. 9 C 22: 5ω-3 0. 2 0. 1 C 22: 6ω-3 0. 5 0. 2 11. 6 13. 06 C 18: 2ω-6 8. 9 11. 3 C 20: 4ω-6 0. 7 0. 5 C 22: 4ω-6 0. 2 0. 1 Totalω-6 62
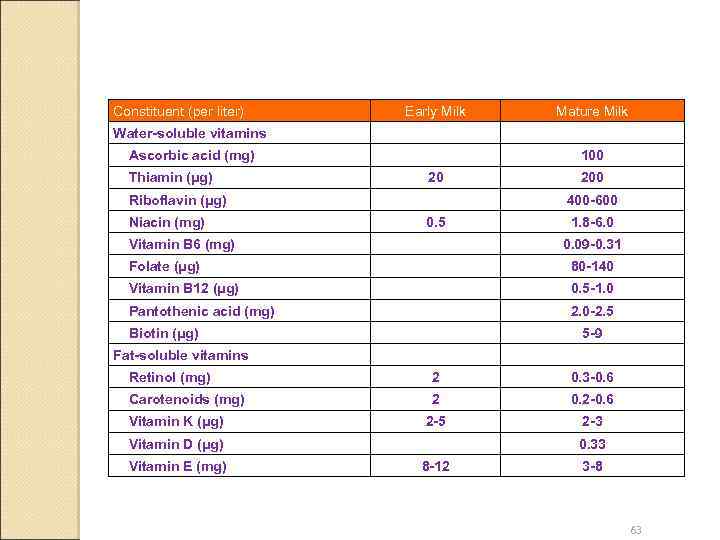
Constituent (per liter) Early Milk Mature Milk Water-soluble vitamins Ascorbic acid (mg) Thiamin (μg) 100 20 Riboflavin (μg) Niacin (mg) 200 400 -600 0. 5 Vitamin B 6 (mg) 1. 8 -6. 0 0. 09 -0. 31 Folate (μg) 80 -140 Vitamin B 12 (μg) 0. 5 -1. 0 Pantothenic acid (mg) 2. 0 -2. 5 Biotin (μg) 5 -9 Fat-soluble vitamins Retinol (mg) 2 0. 3 -0. 6 Carotenoids (mg) 2 0. 2 -0. 6 2 -5 2 -3 Vitamin K (μg) Vitamin D (μg) Vitamin E (mg) 0. 33 8 -12 3 -8 63
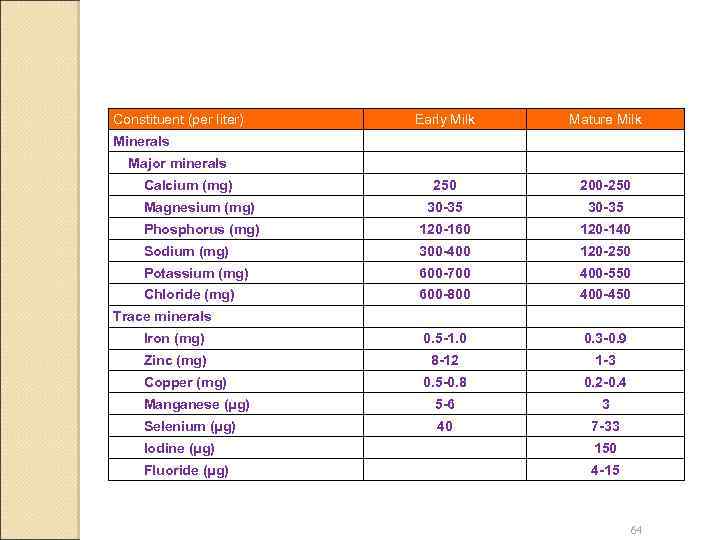
Constituent (per liter) Early Milk Mature Milk 250 200 -250 Magnesium (mg) 30 -35 Phosphorus (mg) 120 -160 120 -140 Sodium (mg) 300 -400 120 -250 Potassium (mg) 600 -700 400 -550 Chloride (mg) 600 -800 400 -450 Iron (mg) 0. 5 -1. 0 0. 3 -0. 9 Zinc (mg) 8 -12 1 -3 0. 5 -0. 8 0. 2 -0. 4 Manganese (μg) 5 -6 3 Selenium (μg) 40 7 -33 Minerals Major minerals Calcium (mg) Trace minerals Copper (mg) Iodine (μg) 150 Fluoride (μg) 4 -15 64
Conclusions Strong evidence continues to demonstrate that human milk is the optimal source of nutrition for the human infant Breast feeding not only decreases the risk of infectious diseases of infants, but also provides benefits for maternal health and for the environment Support for breast feeding from clinicians plays an important role It is predictable that substantial improvements in breast feeding ratio could result in valuable health gains to women and their infants 65

breast feeding - Copy.ppt