
Brain Attack NR-75 D Diana Diaz RN, MS
Objectives n n n Define “stroke” Discuss incidence & risk factors Review Cerebral flow and factors that affect it Discuss pathophysiology of CVA Correlate clinical manifestations of stroke with the pathophysiology.
History of Stroke n n n Hippocrates-2, 400 yrs ago Names for Stroke Most commonly known today n Brain Attack
Definition n n Ischemia is inadequate blood flow Brain attack (Stroke) occurs when there is ischemia to a part of the brain that results in death of brain cells

Incidence n 3 rd Cause of death in US and Canada n n Statistics 2/3 in people >65 = in men and women Higher incidence and death rates among African-Americans, Hispanics, Native. American, Asian Americans

Risk Factors Non Modifiable n Age n Gender n Race n Heredity

Risk Factors Modifiable n Obesity n HTN n Smoking n Heavy alcohol consumption n Hypercoagulability n Hyperlipidemia n n n Asymptomatic carotid stenosis Diabetes mellitus Heart disease, atrial fibrillation Oral contraceptives Physical inactivity Sickle cell disease
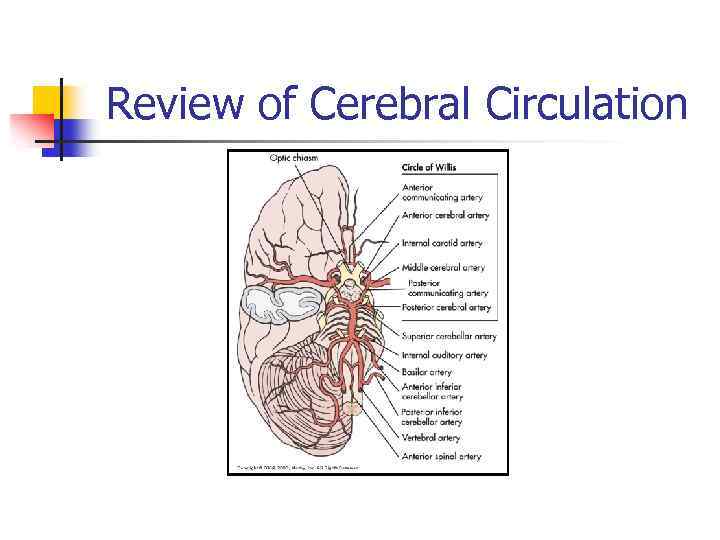
Review of Cerebral Circulation
Blood supply by arteries n Blood is supplied to the brain by two major pairs of arteries n n Internal carotid arteries Vertebral arteries
Blood supply by arteries n Carotid arteries branch to supply most of the n n n Frontal, parietal, and temporal lobes Basal ganglia Part of the diencephalon n n Thalamus Hypothalamus
Blood supply by arteries n Vertebral arteries join to form the basilar artery, which supply the n n n Middle and lower temporal lobes Occipital lobes Cerebellum Brainstem Part of the diencephalon
“Brain Attack” means: Blood flow to the brain is totally interrupted
Etiology n Atherosclerosis – Disease of the arteries; hardening and thickening of the arterial wall because of soft deposits of intraarterial fat and fibrin that harden over time.
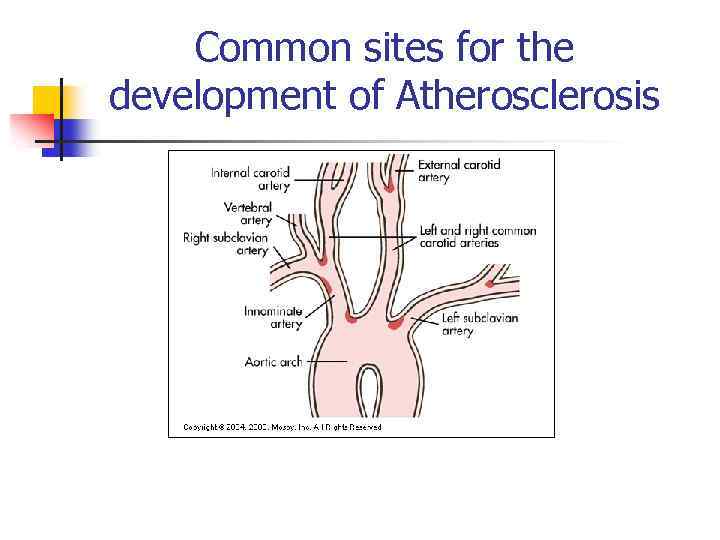
Common sites for the development of Atherosclerosis
Transient Ischemic Attack (TIA) n n n Transient ischemic attack (TIA) is a temporary focal loss of neurologic function caused by ischemia Most TIAs resolve within 3 hours TIAs are a warning sign of progressive cerebrovascular disease
Types of Stroke n Strokes are classified based on the underlying pathophysiologic findings n n Ischemic Hemorrhagic
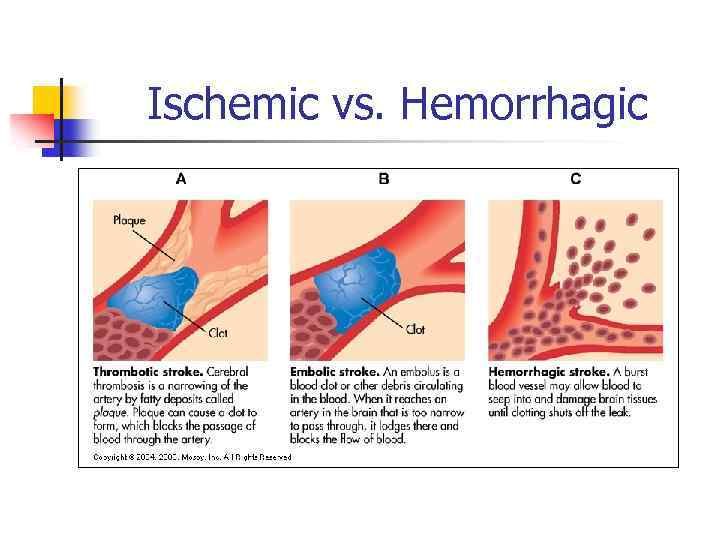
Ischemic vs. Hemorrhagic

Ischemic Stroke n n Ischemic strokes result from inadequate blood flow to the brain from partial or complete occlusion of an artery 85% of all strokes are ischemic strokes
Ischemic Stroke n Thrombotic or Embolic Most patients with ischemic stroke do not have a decreased level of consciousness in the first 24 hours May progress in the first 72 hours
Thrombotic stroke n n n Thrombosis occurs in relation to injury to a blood vessel wall and formation of a blood clot Result of thrombosis or narrowing of the blood vessel Most common cause of stroke
Embolic stroke n n n Occur when an embolus lodges in and occludes a cerebral artery Results in infarction and edema of the area supplied by the involved vessel Second most common cause of stroke

Embolic stroke n n Majority of emboli originate in the inside layer of the heart, with plaque breaking off from the endocardium and entering the circulation Patient with an embolic stroke commonly has a rapid occurrence of severe clinical symptoms

Hemorrhagic Stroke n n Account for approximately 15% of all strokes Result from bleeding into the brain tissue itself or into the subarachnoid space or ventricles
Hemorrhagic Stroke n Intracerebral hemorrhage n n n Bleeding within the brain caused by a rupture of a vessel Hypertension is the most important cause Hemorrhage commonly occurs during periods of activity

Hemorrhagic Stroke n Intracerebral hemorrhage n Manifestations include neurologic deficits, headache, nausea, vomiting, decreased levels of consciousness, and hypertension
Hemorrhagic Stroke n Subarachnoid hemorrhage n n Occurs when there is intracranial bleeding into cerebrospinal fluid-filled space between the arachnoid and pia mater Commonly caused by rupture of a cerebral aneurysm
Clinical Manifestations n Affects many body functions n n n n Motor activity Elimination Intellectual function Spatial-perceptual alterations Personality Affect Sensation Communication
Clinical Manifestations n Brain attack n Term increasingly being used to describe stroke and communicate urgency of recognizing stroke symptoms and treating their onset as a medical emergency

Clinical Manifestations Motor Function n n Most obvious effect of stroke Include impairment of n n n Mobility Respiratory function Swallowing and speech Gag reflex Self-care abilities
Clinical Manifestations Motor Function n n An initial period of flaccidity may last from days to several weeks and is related to nerve damage Spasticity of the muscles follows the flaccid stage and is related to interruption of upper motor neuron influence
Clinical Manifestations Communication n Patient may experience aphasia when a stroke damages the dominant hemisphere of the brain n Aphasia is a total loss of comprehension and use of language
Clinical Manifestations Communication n n Dysphasia refers to difficulty related to the comprehension or use of language and is due to partial disruption or loss Dysphasia can be classified as nonfluent or fluent
Clinical Manifestations Communication n n Dysarthria does not affect the meaning of communication or the comprehension of language It does affect the mechanics of speech
Clinical Manifestations Affect n n Patients who suffer a stroke may have difficulty controlling their emotions Emotional responses may be exaggerated or unpredictable
Clinical Manifestations Intellectual Function n n Both memory and judgment may be impaired as a result of stroke A left-brain stroke is more likely to result in memory problems related to language
Clinical Manifestations Spatial-Perceptual Alterations n n Stroke on the right side of the brain is more likely to cause problems in spatial-perceptual orientation However, this may occur with leftbrain stroke
Clinical Manifestations Spatial-Perceptual Alterations n Spatial-perceptual problems may be divided into four categories 1. 2. Incorrect perception of self and illness Erroneous perception of self in space

Clinical Manifestations Spatial-Perceptual Alterations 3. 4. Inability to recognize an object by sight, touch, or hearing Inability to carry out learned sequential movements on command
Clinical Manifestations Elimination n n Most problems with urinary and bowel elimination occur initially and are temporary When a stroke affects one hemisphere of the brain, the prognosis for normal bladder function is excellent
Diagnostic Studies n When symptoms of a stroke occur, diagnostic studies are done to n n n Confirm that it is a stroke Identify the likely cause of the stroke CT is the primary diagnostic test used after a stroke
Diagnostic Studies n Additional studies n n n Complete blood count Platelets, prothrombin time, activated partial thromboplastin time Electrolytes, blood glucose Renal and hepatic studies Lipid profile
Collaborative Care Prevention n Goals of stroke prevention include n n Health management for the well individual Education and management of modifiable risk factors to prevent a stroke
Collaborative Care Prevention n n Antiplatelet drugs are usually the chosen treatment to prevent further stroke in patients who have had a TIA Aspirin is the most frequently used antiplatelet drug

Collaborative Care Prevention n Surgical interventions for the patient with TIAs from carotid disease include n n Carotid endarterectomy Transluminal angioplasty Stenting Extracranial-intracranial bypass

Collaborative Care Acute Care n Assessment findings n n n n Altered level of consciousness Weakness, numbness, or paralysis Speech or visual disturbances Severe headache ↑ or ↓ heart rate Respiratory distress Unequal pupils
Collaborative Care Acute Care n Interventions – Initial n n n Ensure patient airway Remove dentures Perform pulse oximetry Maintain adequate oxygenation IV access with normal saline Maintain BP according to guidelines

Collaborative Care Acute Care n Interventions – Initial n n n Remove clothing Obtain CT scan immediately Perform baseline laboratory tests Position head midline Elevate head of bed 30 degrees if no symptoms of shock or injury

Collaborative Care Acute Care n Interventions – Ongoing n Monitor vital signs and neurologic status n n n Level of consciousness Motor and sensory function Pupil size and reactivity O 2 saturation Cardiac rhythm
Collaborative Care Acute Care n Recombinant tissue plasminogen activator (t. PA) is used to n Reestablish blood flow through a blocked artery to prevent cell death in patients with acute onset of ischemic stroke symptoms

Collaborative Care Acute Care n Thrombolytic therapy given within 3 hours of the onset of symptoms n n ↓ disability But at the expense of ↑ in deaths within the first 7 to 10 days and ↑ in intracranial hemorrhage
Collaborative Care Acute Care n Surgical interventions for stroke include immediate evacuation of n n Aneurysm-induced hematomas Cerebellar hematomas (>3 cm)
Collaborative Care Rehabilitation Care n n After the stroke has stabilized for 1224 hours, collaborative care shifts from preserving life to lessening disability and attaining optimal functioning Patient may be transferred to a rehabilitation unit
Nursing Management Nursing Implementation n Respiratory System n n Management of the respiratory system is a nursing priority Risk for aspiration pneumonia Risks for airway obstruction May require endotracheal intubation and mechanical ventilation
Nursing Management Nursing Implementation n Neurologic System n Monitor closely to detect changes suggesting n n Extension of the stroke ↑ ICP Vasospasm Recovery from stroke symptoms

Nursing Management Nursing Implementation n Cardiovascular System n n Monitoring vital signs frequently Monitoring cardiac rhythms Calculating intake and output, noting imbalances Regulating IV infusions
Nursing Management Nursing Implementation n Cardiovascular System n n n Adjusting fluid intake to the individual needs of the patient Monitoring lung sounds for crackles and rhonchi (pulmonary congestion) Monitoring heart sounds for murmurs or for S 3 or S 4 heart sounds
Nursing Management Nursing Implementation n Integumentary System n n Skin of the patient is susceptible to breakdown related to loss of sensation, ↓ circulation, and immobility Compounded by patient age, poor nutrition, dehydration, edema, and incontinence

Nursing Management Nursing Implementation n Integumentary System n n n Pressure relief by position changes, special mattresses, or wheelchair cushions Good skin hygiene Emollients applied to dry skin
Nursing Management Nursing Implementation n Integumentary System n n Early mobility Position patient on the weak or paralyzed side for only 30 minutes
Nursing Management Nursing Implementation n Gastrointestinal System n n After careful assessment of swallowing, chewing, gag reflex, oral feedings can be initiated Feedings must be followed by scrupulous oral hygiene

Nursing Management Nursing Implementation n Communication n Nurse’s role in meeting psychologic needs of the patient is primarily supportive Patient is assessed both for the ability to speak and the ability to understand Speak slowly and calmly, using simple words or sentences

Nursing Management Nursing Implementation n Sensory-Perceptual Alterations n n Blindness in the same half of each visual field is a common problem after stroke Other visual problems may include diplopia (double vision), loss of the corneal reflex, and ptosis (drooping eyelid)
Nursing Management Nursing Implementation n Ambulatory and Home Care n The rehabilitation nurse assesses the patient and family with n n Rehabilitation potential of the patient Physical status of all body systems Presence of complications caused by the stroke or other chronic conditions Cognitive status of the patient
Nursing Management Nursing Implementation n Ambulatory and Home Care n The patient is usually discharged from the acute care setting to home, an intermediate or long-term care facility, or a rehabilitation facility
Nursing Management Nursing Implementation n Ambulatory and Home Care n Nurses have an excellent opportunity to prepare the patient and family for discharge through n n Education Demonstration Practice Evaluation of self-care skills