Bone Tissue Ch. 6
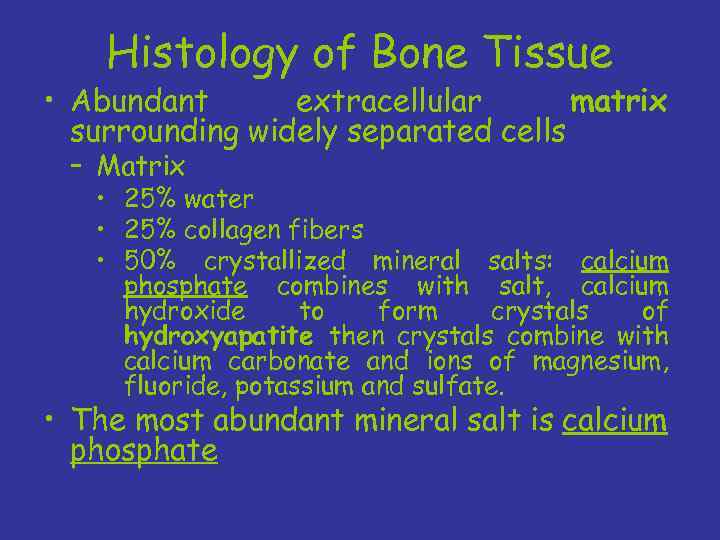
Histology of Bone Tissue • Abundant extracellular matrix surrounding widely separated cells – Matrix • 25% water • 25% collagen fibers • 50% crystallized mineral salts: calcium phosphate combines with salt, calcium hydroxide to form crystals of hydroxyapatite then crystals combine with calcium carbonate and ions of magnesium, fluoride, potassium and sulfate. • The most abundant mineral salt is calcium phosphate
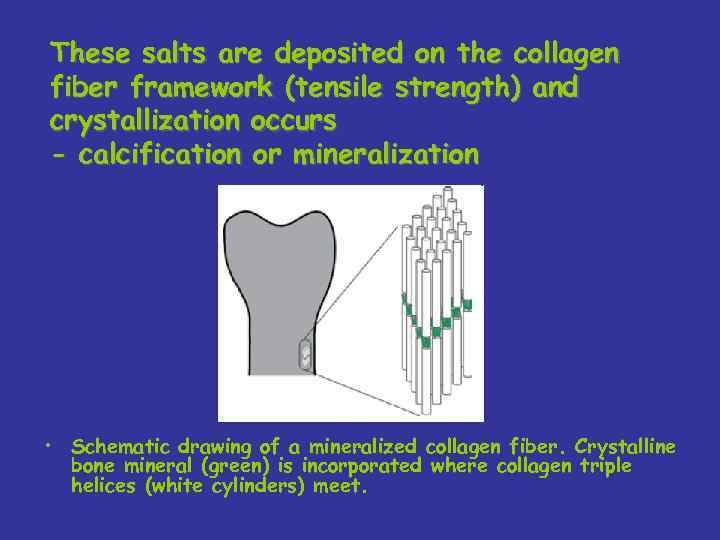
These salts are deposited on the collagen fiber framework (tensile strength) and crystallization occurs - calcification or mineralization • Schematic drawing of a mineralized collagen fiber. Crystalline bone mineral (green) is incorporated where collagen triple helices (white cylinders) meet.
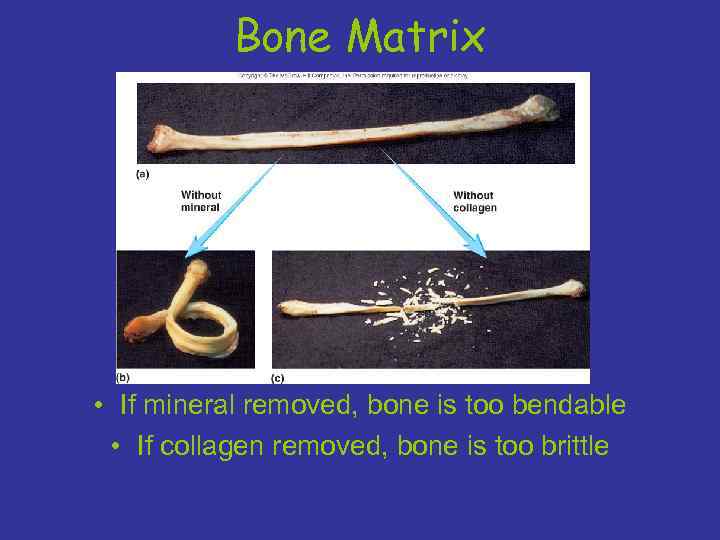
Bone Matrix • If mineral removed, bone is too bendable • If collagen removed, bone is too brittle
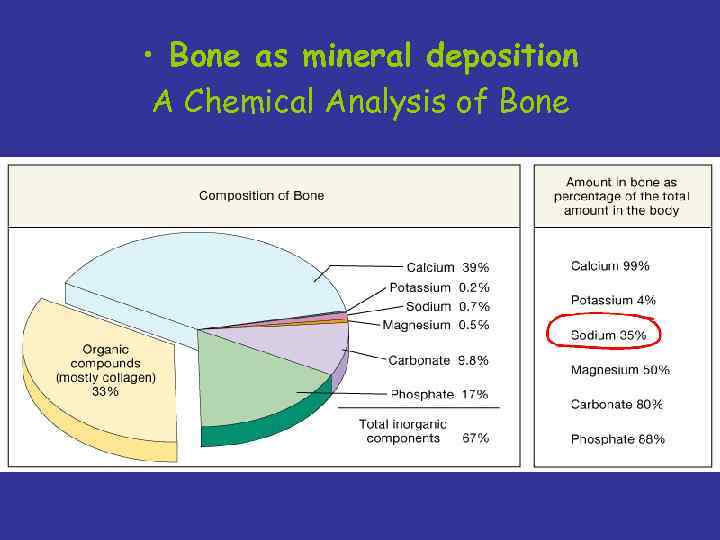
• Bone as mineral deposition A Chemical Analysis of Bone
• Only later did a bony endoskeleton develop presumably under selection for increased mechanical support. • The hard inorganic component of bone is calcium phosphate (in the form of hydroxyapatite) rather than the calcium carbonate found in invertebrates.
• This difference in the form of calcium used is believed to be due to the fact that vertebrates have always engaged in intense bursts of anaerobic activity. • Anaerobic metabolism produces lactic acid which lowers blood p. H. Under acid conditions calcium carbonate dissolves, which is not a desirable trait for a skeleton.
Cells in bone: • Osteocytes = mature bone cells – metabolism • Osteoblasts synthesize new matrix – Osteogenesis • Osteoclasts dissolve bone matrix – Osteolysis • Osteoprogenitor cells differentiate into osteoblasts
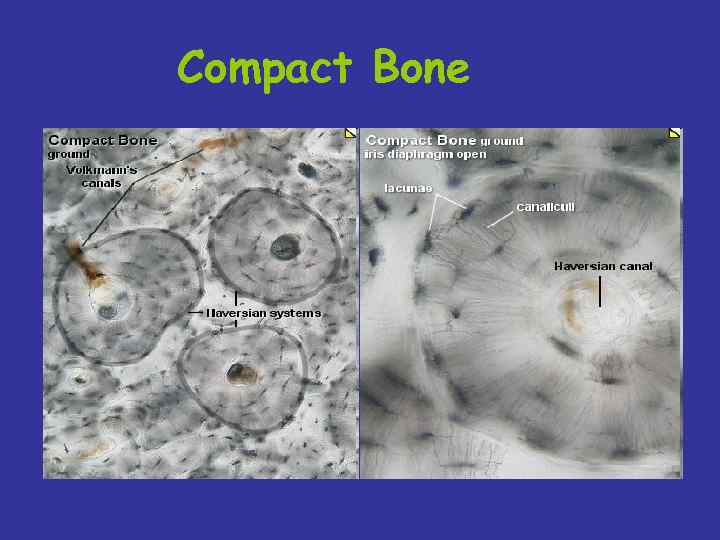
Compact Bone
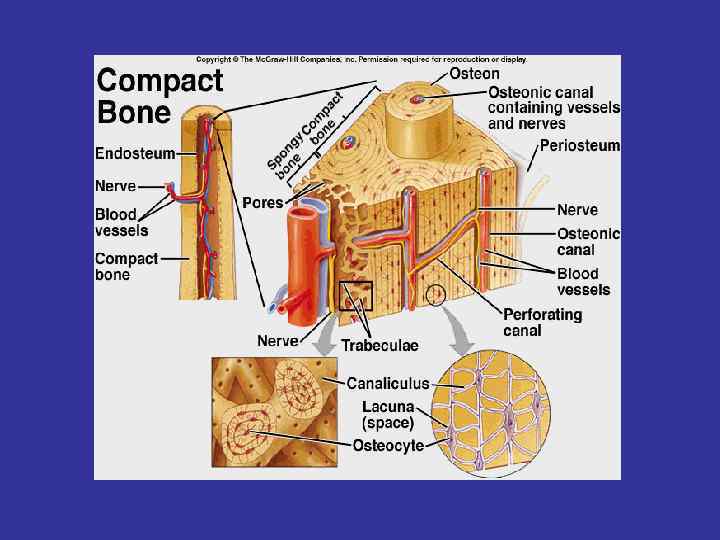
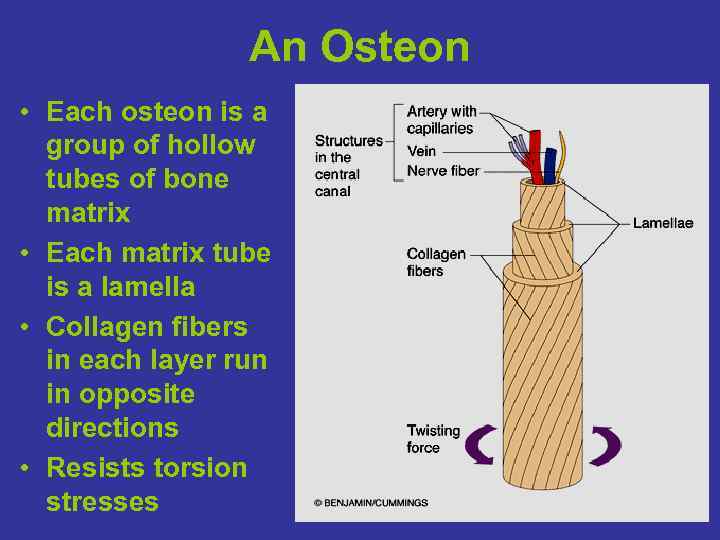
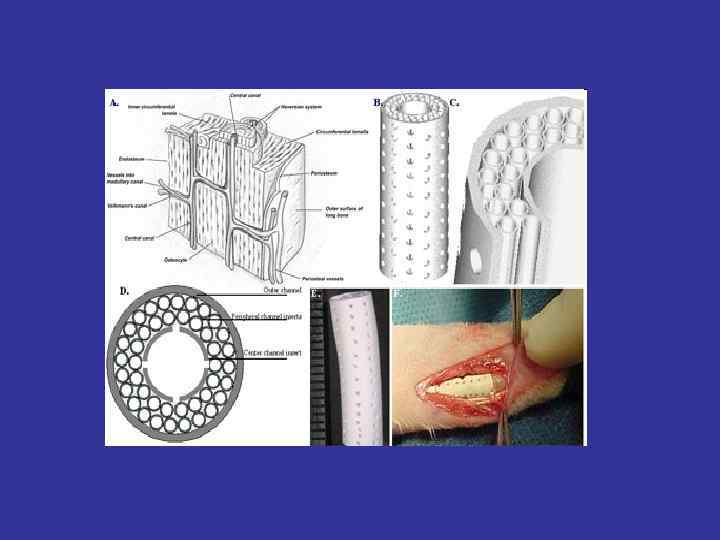
An Osteon • Each osteon is a group of hollow tubes of bone matrix • Each matrix tube is a lamella • Collagen fibers in each layer run in opposite directions • Resists torsion stresses
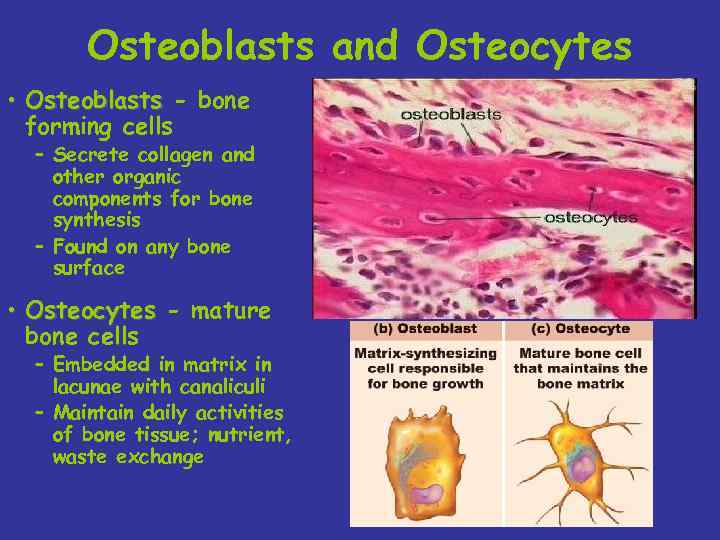
Osteoblasts and Osteocytes • Osteoblasts - bone forming cells – Secrete collagen and other organic components for bone synthesis – Found on any bone surface • Osteocytes - mature bone cells – Embedded in matrix in lacunae with canaliculi – Maintain daily activities of bone tissue; nutrient, waste exchange
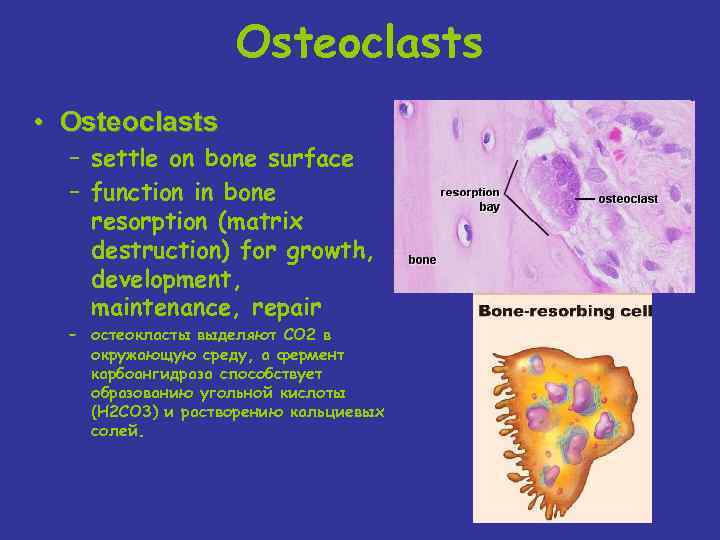
Osteoclasts • Osteoclasts – settle on bone surface – function in bone resorption (matrix destruction) for growth, development, maintenance, repair – остеокласты выделяют СО 2 в окружающую среду, а фермент карбоангидраза способствует образованию угольной кислоты (Н 2 СО 3) и растворению кальциевых солей.
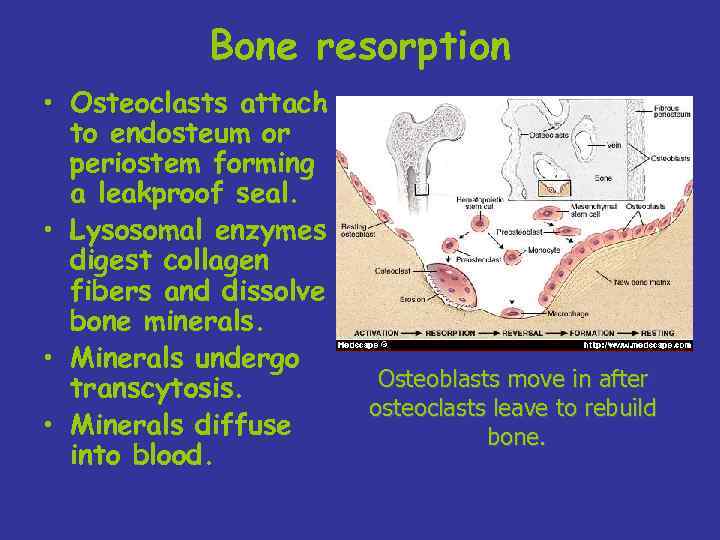
Bone resorption • Osteoclasts attach to endosteum or periostem forming a leakproof seal. • Lysosomal enzymes digest collagen fibers and dissolve bone minerals. • Minerals undergo transcytosis. • Minerals diffuse into blood. Osteoblasts move in after osteoclasts leave to rebuild bone.

Надкостница • Osteoprogenitor cells: - derived from mesenchyme - unspecialized stem cells - undergo mitosis and develop into osteoblasts - found on inner surface of periosteum and endosteum.
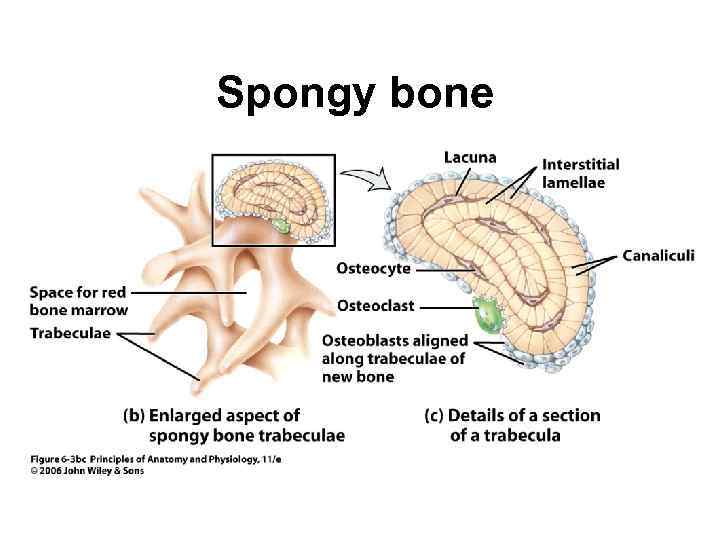
Spongy bone
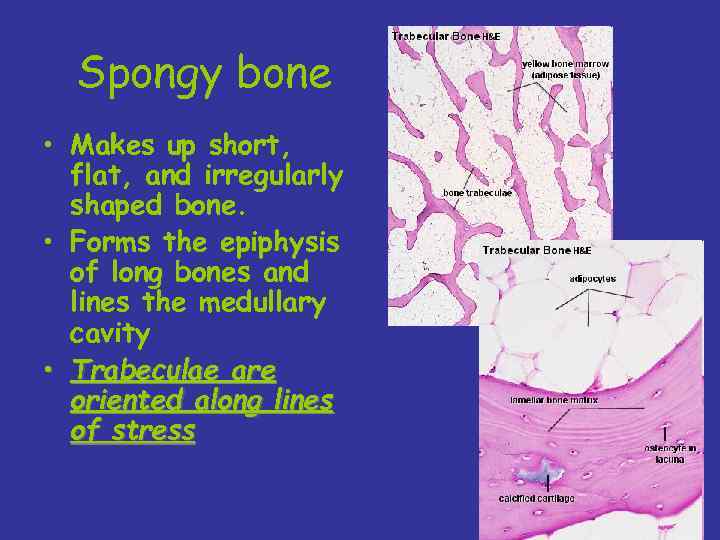
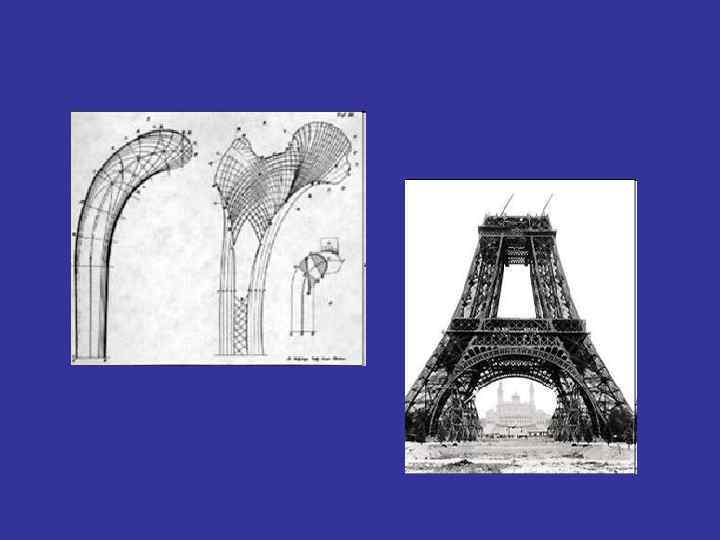
Spongy bone • Makes up short, flat, and irregularly shaped bone. • Forms the epiphysis of long bones and lines the medullary cavity • Trabeculae are oriented along lines of stress
Spongy vs Compact bone • Spongy bone is lighter, which reduces the muscle force needed for movement. • Spongy bone supports and protects the red bone marrow, where hemopoiesis occurs.
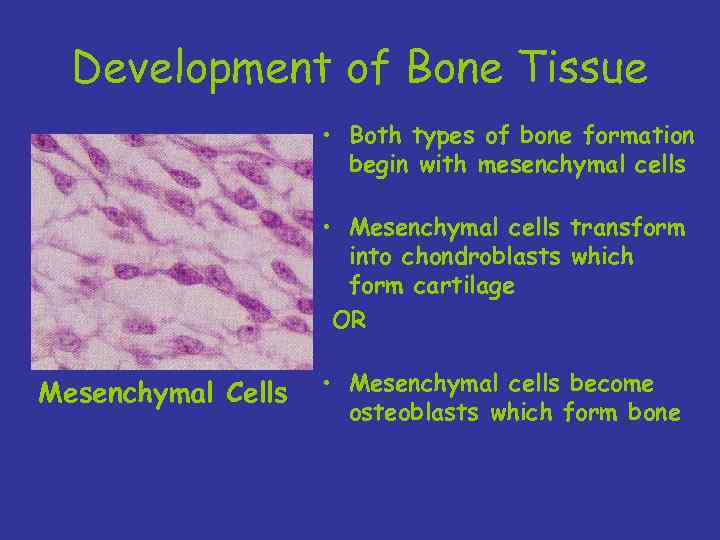
Development of Bone Tissue • Both types of bone formation begin with mesenchymal cells • Mesenchymal cells transform into chondroblasts which form cartilage OR Mesenchymal Cells • Mesenchymal cells become osteoblasts which form bone
Intramembranous bone development (Intramembranous ossification) Many bones are formed directly from mesenchyme (a tissue which consists of loosely organized cells derived from the mesoderm). Begins at 8 weeks of development
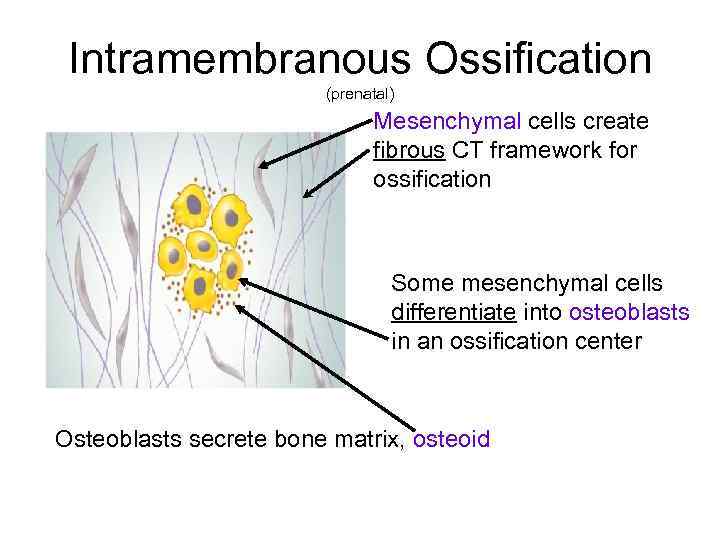
Intramembranous Ossification (prenatal) Mesenchymal cells create fibrous CT framework for ossification Some mesenchymal cells differentiate into osteoblasts in an ossification center Osteoblasts secrete bone matrix, osteoid
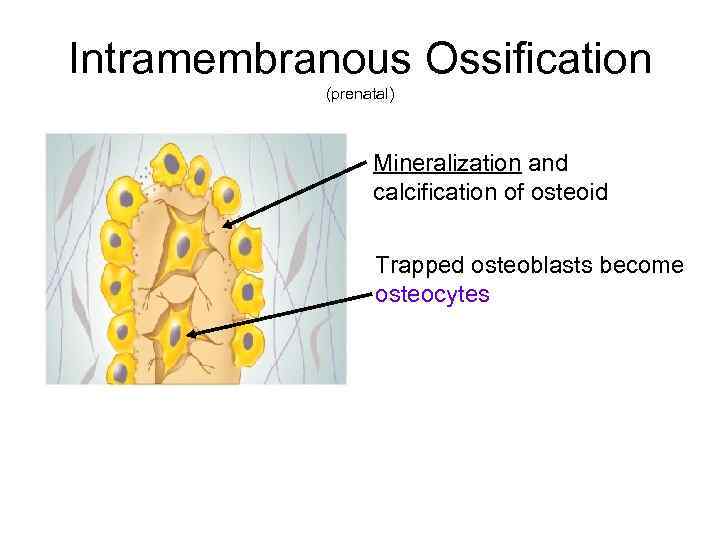
Intramembranous Ossification (prenatal) Mineralization and calcification of osteoid Trapped osteoblasts become osteocytes
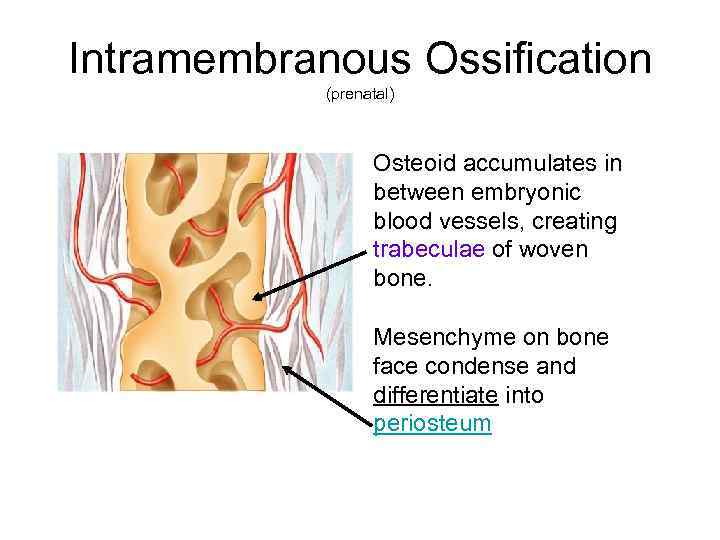
Intramembranous Ossification (prenatal) Osteoid accumulates in between embryonic blood vessels, creating trabeculae of woven bone. Mesenchyme on bone face condense and differentiate into periosteum
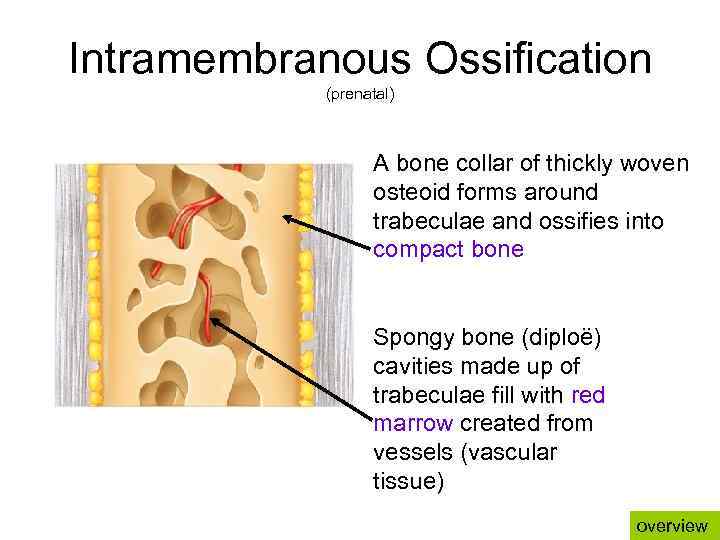
Intramembranous Ossification (prenatal) A bone collar of thickly woven osteoid forms around trabeculae and ossifies into compact bone Spongy bone (diploë) cavities made up of trabeculae fill with red marrow created from vessels (vascular tissue) overview
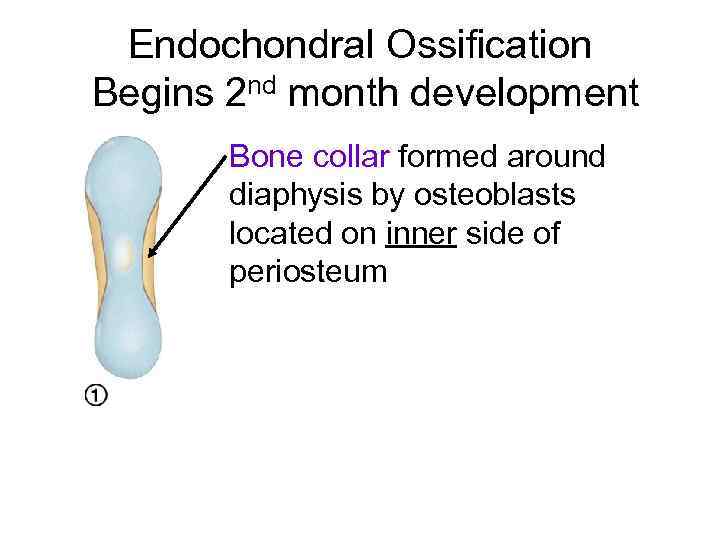
Endochondral Ossification Begins 2 nd month development Bone collar formed around diaphysis by osteoblasts located on inner side of periosteum
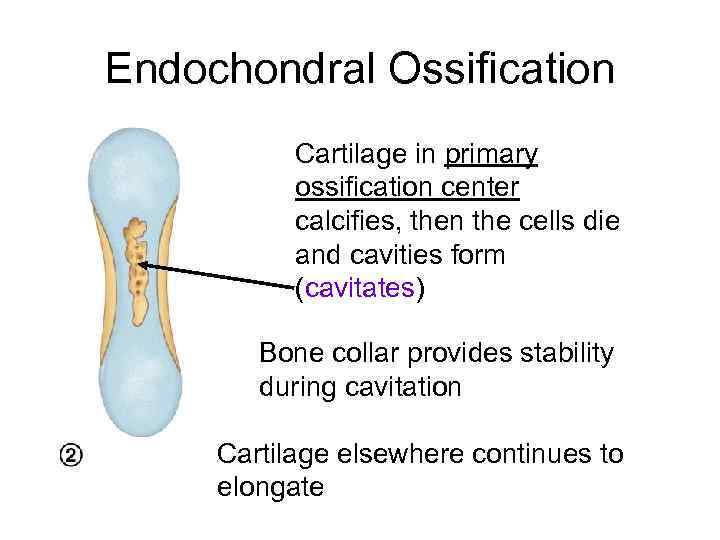
Endochondral Ossification Cartilage in primary ossification center calcifies, then the cells die and cavities form (cavitates) Bone collar provides stability during cavitation Cartilage elsewhere continues to elongate
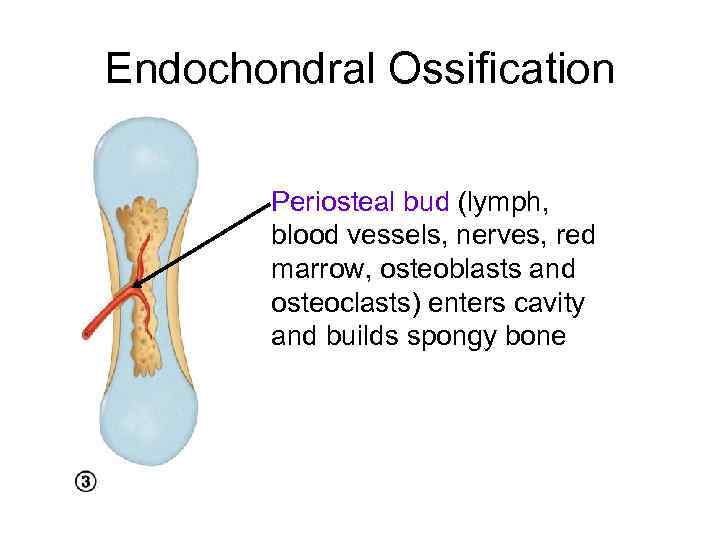
Endochondral Ossification Periosteal bud (lymph, blood vessels, nerves, red marrow, osteoblasts and osteoclasts) enters cavity and builds spongy bone
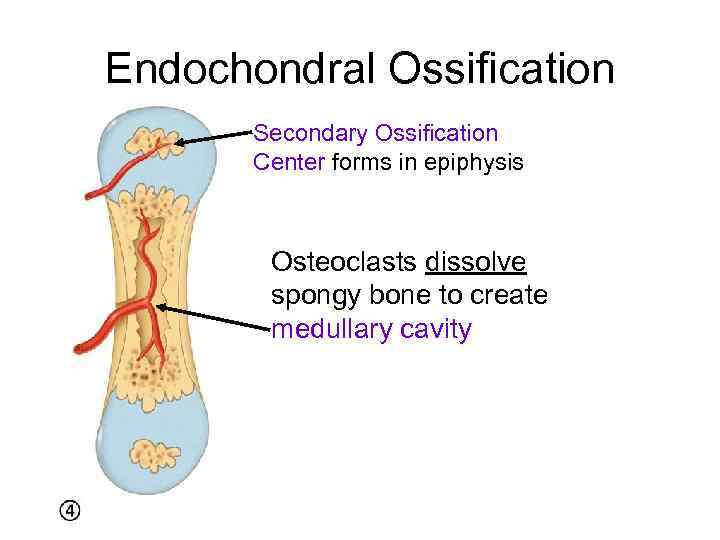
Endochondral Ossification Secondary Ossification Center forms in epiphysis Osteoclasts dissolve spongy bone to create medullary cavity
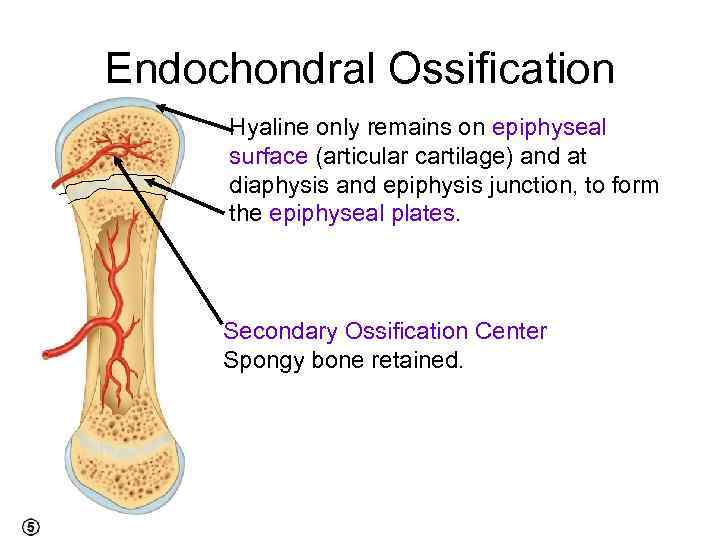
Endochondral Ossification Hyaline only remains on epiphyseal surface (articular cartilage) and at diaphysis and epiphysis junction, to form the epiphyseal plates. Secondary Ossification Center Spongy bone retained.
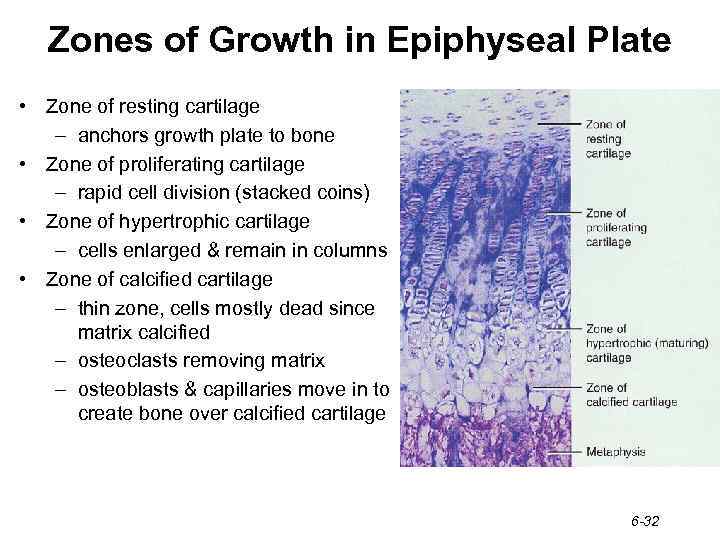
Zones of Growth in Epiphyseal Plate • Zone of resting cartilage – anchors growth plate to bone • Zone of proliferating cartilage – rapid cell division (stacked coins) • Zone of hypertrophic cartilage – cells enlarged & remain in columns • Zone of calcified cartilage – thin zone, cells mostly dead since matrix calcified – osteoclasts removing matrix – osteoblasts & capillaries move in to create bone over calcified cartilage 6 -32
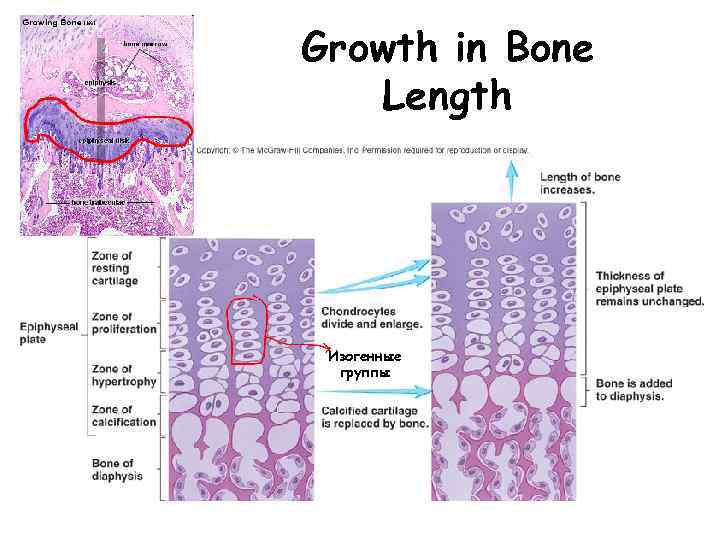
Growth in Bone Length Изогенные группы
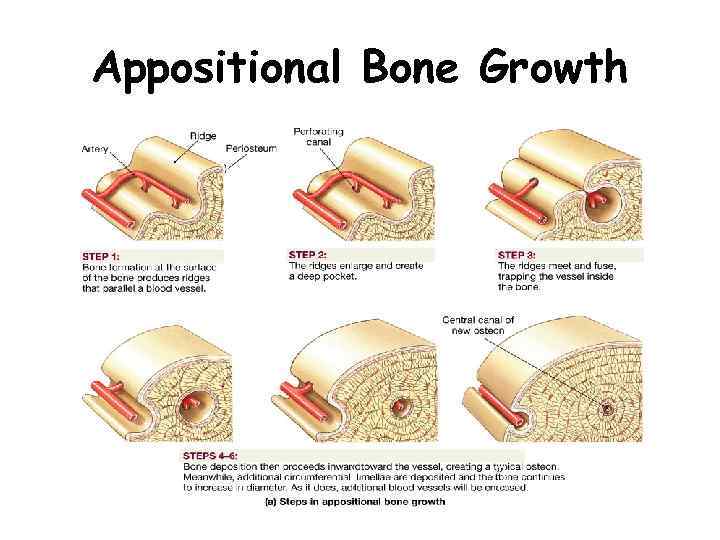
Appositional Bone Growth
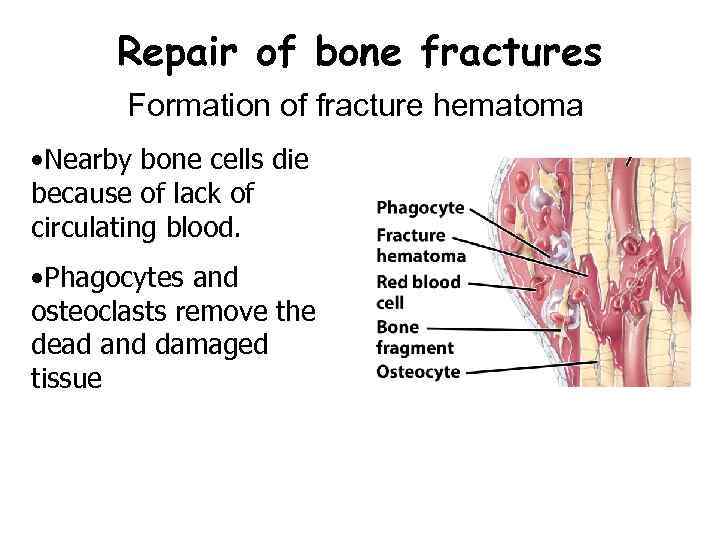
Repair of bone fractures Formation of fracture hematoma • Nearby bone cells die because of lack of circulating blood. • Phagocytes and osteoclasts remove the dead and damaged tissue
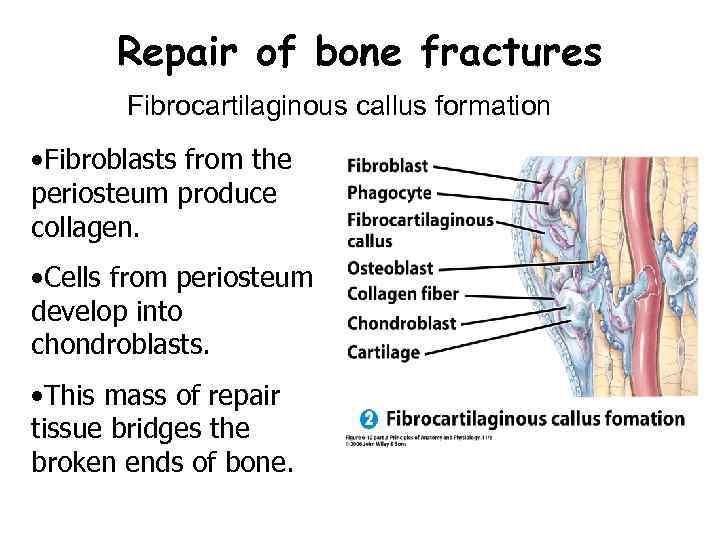
Repair of bone fractures Fibrocartilaginous callus formation • Fibroblasts from the periosteum produce collagen. • Cells from periosteum develop into chondroblasts. • This mass of repair tissue bridges the broken ends of bone.
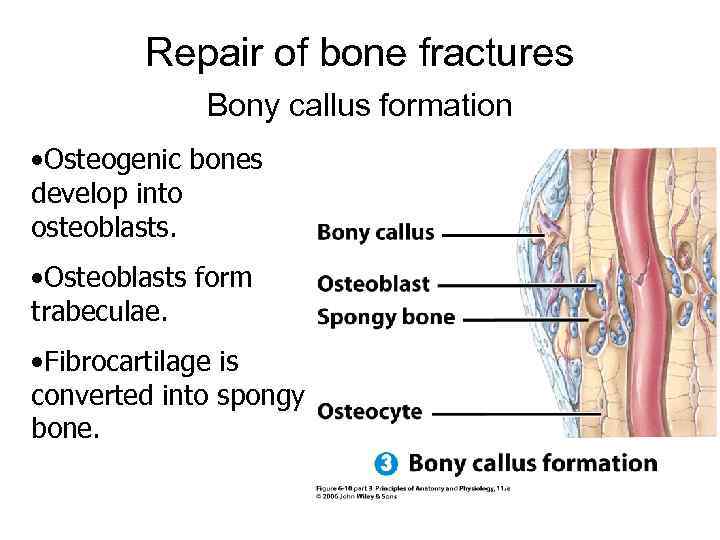
Repair of bone fractures Bony callus formation • Osteogenic bones develop into osteoblasts. • Osteoblasts form trabeculae. • Fibrocartilage is converted into spongy bone.
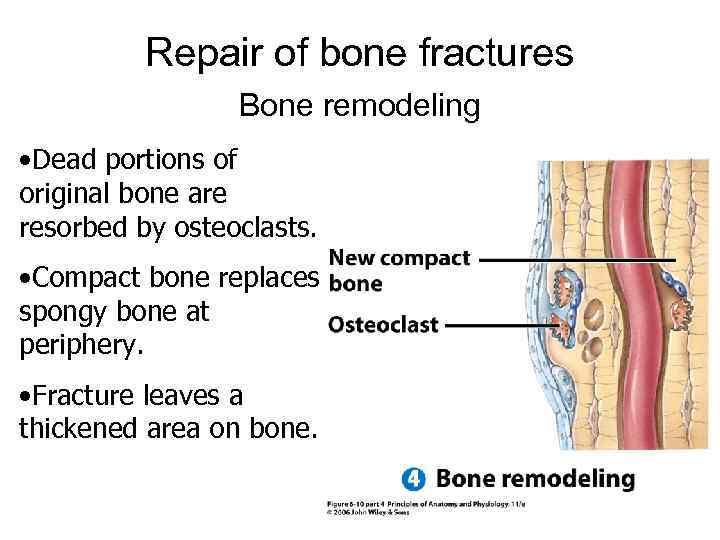
Repair of bone fractures Bone remodeling • Dead portions of original bone are resorbed by osteoclasts. • Compact bone replaces spongy bone at periphery. • Fracture leaves a thickened area on bone.
Factors Affecting Bone Growth and Bone Remodeling • Normal bone metabolism depends on several factors • Minerals – Large amounts of calcium and phosphorus and smaller amounts of magnesium, fluoride, and manganese are required for bone growth and remodeling • Vitamins – Vitamin A stimulates activity of osteoblasts – Vitamin C is needed for synthesis of collagen – Vitamin D helps build bone by increasing the absorption of calcium from foods in the gastrointestinal tract into the blood – Vitamins K and B 12 are also needed for synthesis of bone proteins Copyright 2009, John Wiley & Sons, Inc.
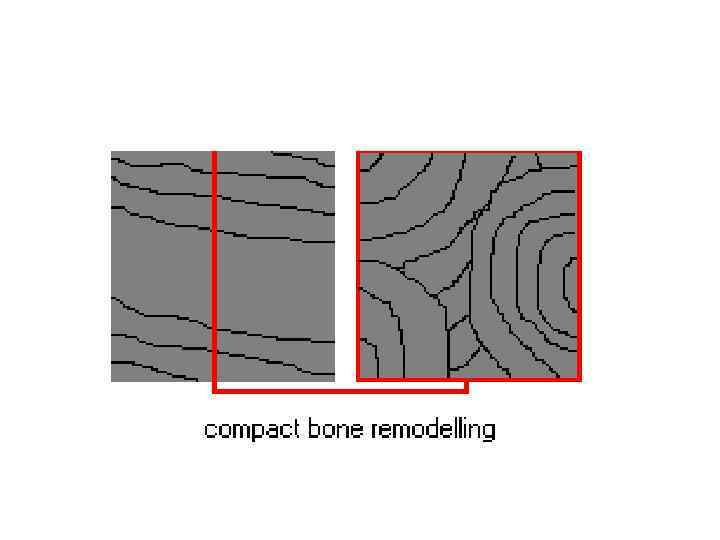
Bone is Dynamic! Bone is constantly remodeling and recycling • • Coupled process between: Bone deposition (by osteoblasts) Bone destruction/resorption (by osteoclasts) 5 -7% of bone mass recycled weekly All spongy bone replaced every 3 -4 years. All compact bone replaced every 10 years.
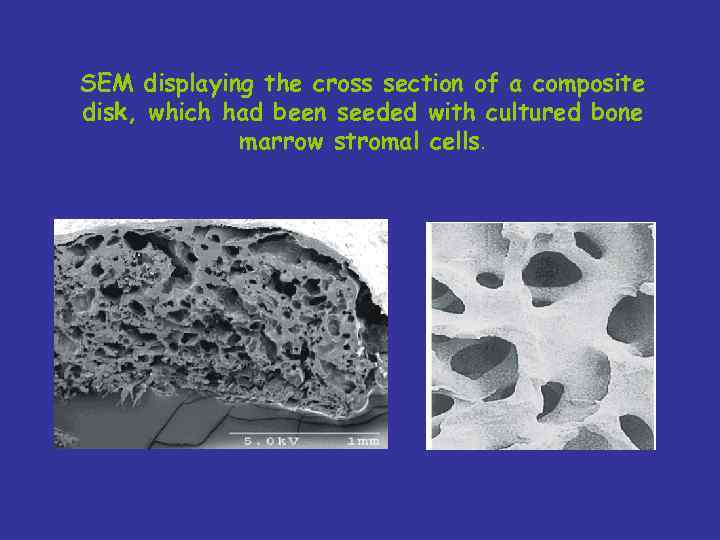
SEM displaying the cross section of a composite disk, which had been seeded with cultured bone marrow stromal cells.

• 1. Структура материала Bio-Oss • 2. Врастание сосудов и клеток, образующих кость • 3. Завершенное образование кости
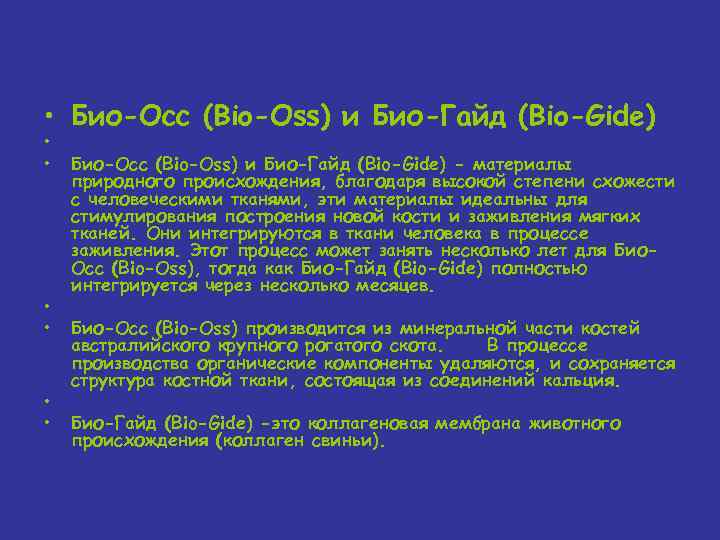
• Био-Осс (Bio-Oss) и Био-Гайд (Bio-Gide) • • • Био-Осс (Bio-Oss) и Био-Гайд (Bio-Gide) - материалы природного происхождения, благодаря высокой степени схожести с человеческими тканями, эти материалы идеальны для стимулирования построения новой кости и заживления мягких тканей. Они интегрируются в ткани человека в процессе заживления. Этот процесс может занять несколько лет для Био. Осс (Bio-Oss), тогда как Био-Гайд (Bio-Gide) полностью интегрируется через несколько месяцев. Био-Осс (Bio-Oss) производится из минеральной части костей австралийского крупного рогатого скота. В процессе производства органические компоненты удаляются, и сохраняется структура костной ткани, состоящая из соединений кальция. Био-Гайд (Bio-Gide) -это коллагеновая мембрана животного происхождения (коллаген свиньи).
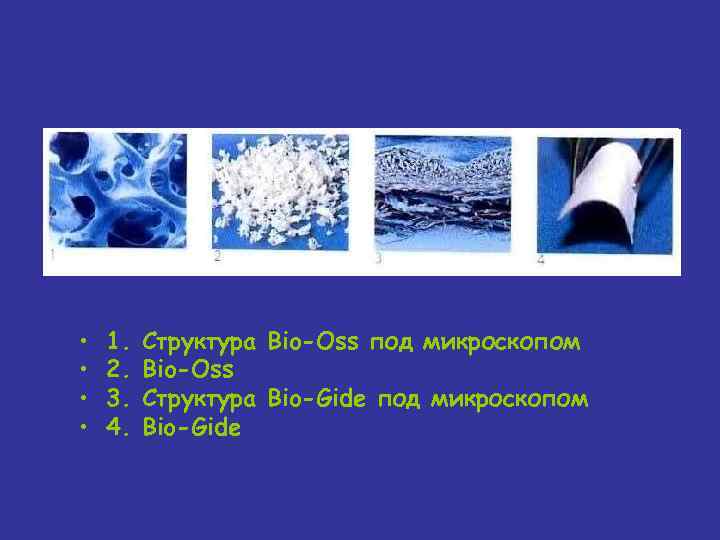
• • 1. 2. 3. 4. Структура Bio-Oss под микроскопом Bio-Oss Структура Bio-Gide под микроскопом Bio-Gide
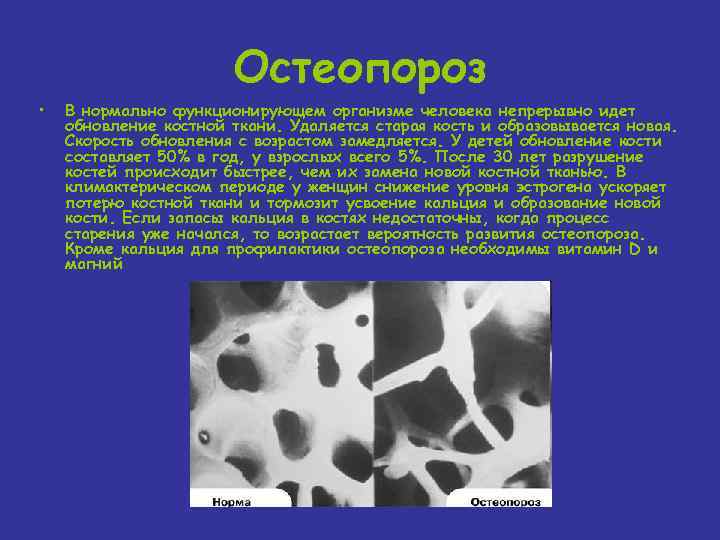
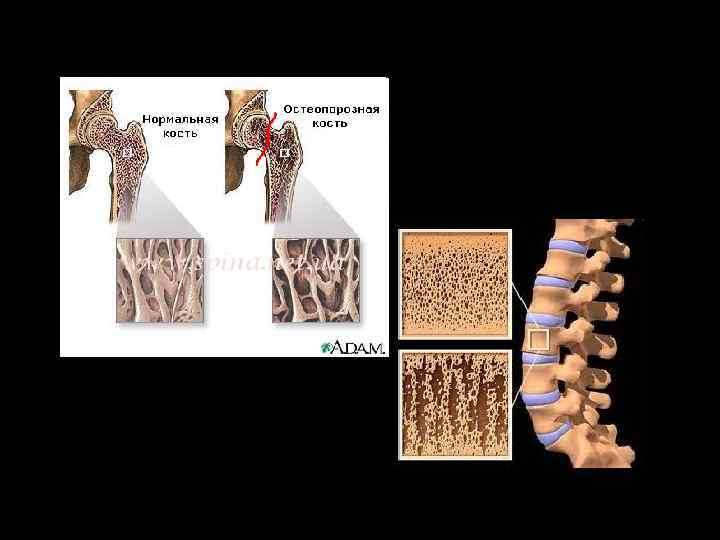
Остеопороз • В нормально функционирующем организме человека непрерывно идет обновление костной ткани. Удаляется старая кость и образовывается новая. Скорость обновления с возрастом замедляется. У детей обновление кости составляет 50% в год, у взрослых всего 5%. После 30 лет разрушение костей происходит быстрее, чем их замена новой костной тканью. В климактерическом периоде у женщин снижение уровня эстрогена ускоряет потерю костной ткани и тормозит усвоение кальция и образование новой кости. Если запасы кальция в костях недостаточны, когда процесс старения уже начался, то возрастает вероятность развития остеопороза. Кроме кальция для профилактики остеопороза необходимы витамин D и магний
• Основные факторы, повышающие риск развития остеопороза: • наследственность; курение ; хрупкое телосложение; употребление алкоголя; светлая кожа; большое потребление кофеина; ранний климакс; малоподвижный образ жизни; лекарственные препараты, такие как: кортикостероиды, левотироксин, противосудорожные средства, гепарин.
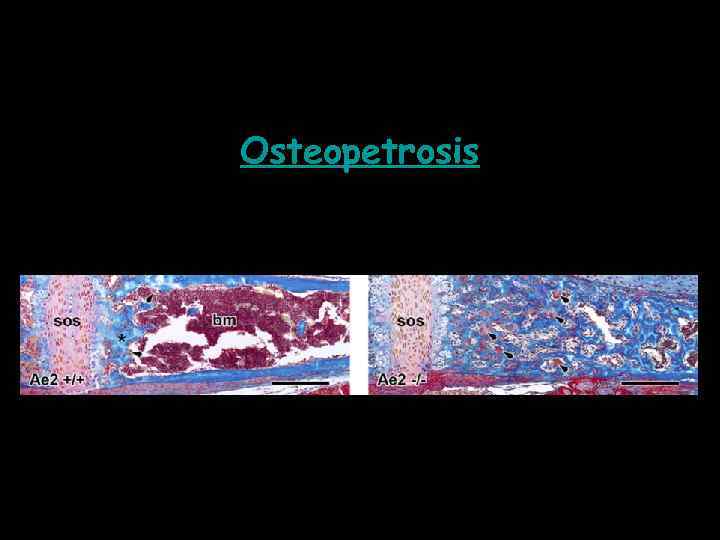
Osteopetrosis
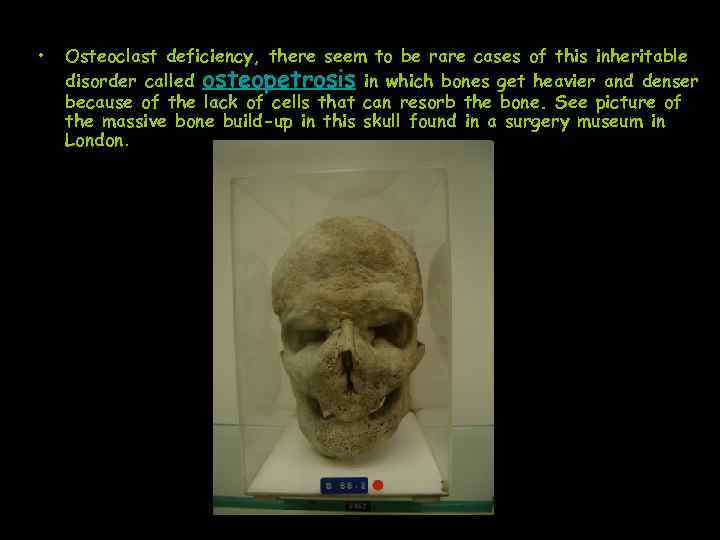
• Osteoclast deficiency, there seem to be rare cases of this inheritable disorder called osteopetrosis in which bones get heavier and denser because of the lack of cells that can resorb the bone. See picture of the massive bone build-up in this skull found in a surgery museum in London.
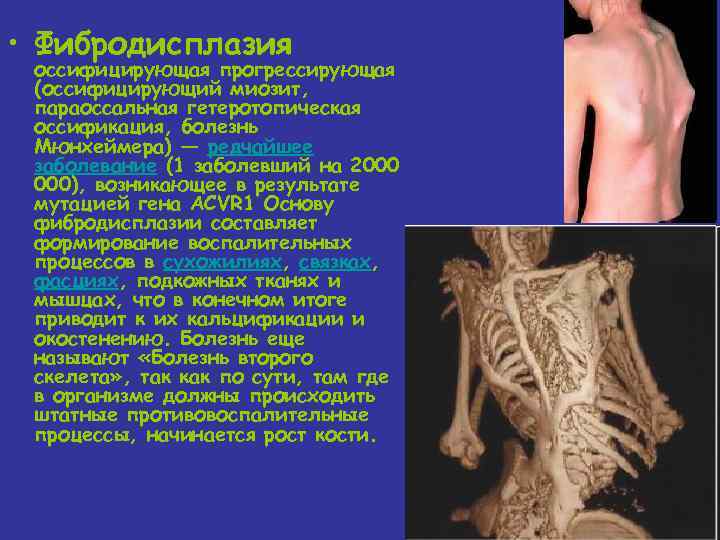
• Фибродисплазия оссифицирующая прогрессирующая (оссифицирующий миозит, параоссальная гетеротопическая оссификация, болезнь Мюнхеймера) — редчайшее заболевание (1 заболевший на 2000 000), возникающее в результате мутацией гена ACVR 1 Основу фибродисплазии составляет формирование воспалительных процессов в сухожилиях, связках, фасциях, подкожных тканях и мышцах, что в конечном итоге приводит к их кальцификации и окостенению. Болезнь еще называют «Болезнь второго скелета» , так как по сути, там где в организме должны происходить штатные противовоспалительные процессы, начинается рост кости.
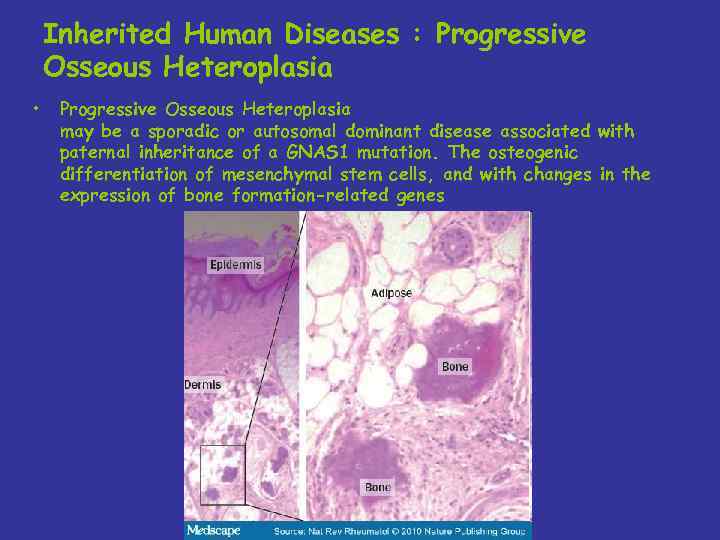
Inherited Human Diseases : Progressive Osseous Heteroplasia • Progressive Osseous Heteroplasia may be a sporadic or autosomal dominant disease associated with paternal inheritance of a GNAS 1 mutation. The osteogenic differentiation of mesenchymal stem cells, and with changes in the expression of bone formation-related genes

Inherited Human Diseases : Progressive Osseous Heteroplasia
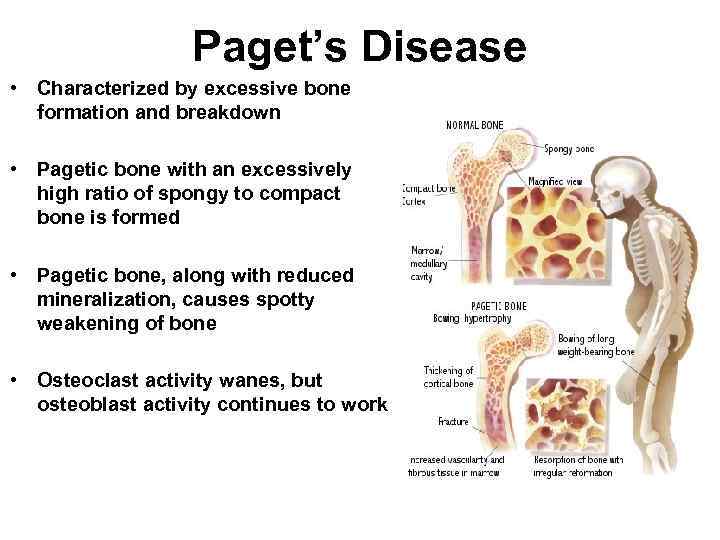
Paget’s Disease • Characterized by excessive bone formation and breakdown • Pagetic bone with an excessively high ratio of spongy to compact bone is formed • Pagetic bone, along with reduced mineralization, causes spotty weakening of bone • Osteoclast activity wanes, but osteoblast activity continues to work