39e412fb4fc22fbb1e1704da30a107d1.ppt
- Количество слайдов: 25
Blurring the Distinction Between Research and Quality Studies: The Utility of Electronic Health Records James M. Gill, MD, MPH Associate Professor of Family Medicine Senior Scientist in Health Policy Jefferson Medical College, Philadelphia, PA President, Delaware Valley Outcomes Research STFM 40 th Annual Spring Conference

Quality of Care • Measuring quality of care increasingly important for family physicians • Identify gaps in care, areas to improve • Demonstrate quality for third parties • Managed Care • Pay for Performance
Quality Measurement and Research • Good quality of care studies require same conditions as good research • Identify population • Who is an active patient (seen in past yr? ) • Which patients belong to which providers? • Outcomes – based on guidelines • Pap test every year vs. 3 three yrs • Documented receipt vs. recommended test • Confounding variables • Case mix • Seen by endocrinologist or GYN
Quality of Care Studies • Have been frequently done in family medicine • Most outpatient quality studies done on a small scale • Often done in single offices • “This study was conducted in a single family medicine teaching practice” • Often primary research done by residents and faculty
Large-Scale Quality Studies • Small scale studies difficult to generalize, difficult to publish • Large scale studies difficult because care is spread over many different locations • The problem is getting access to data on outpatient care across multiple locations • Data difficult to extract from medical records
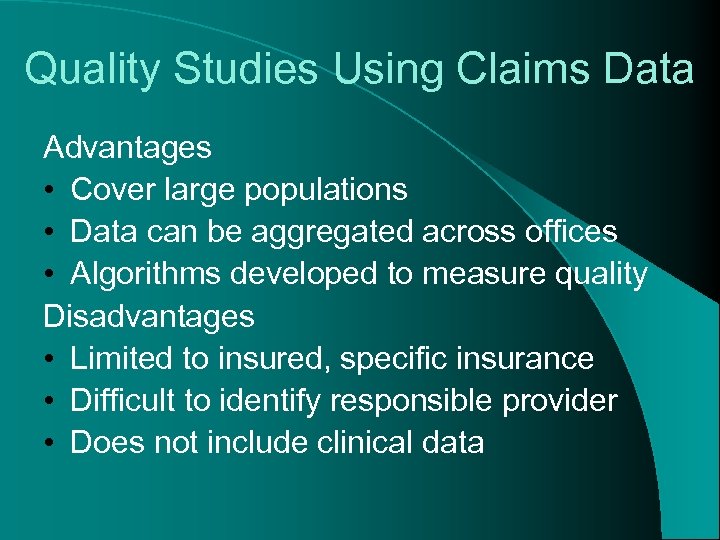
Quality Studies Using Claims Data Advantages • Cover large populations • Data can be aggregated across offices • Algorithms developed to measure quality Disadvantages • Limited to insured, specific insurance • Difficult to identify responsible provider • Does not include clinical data
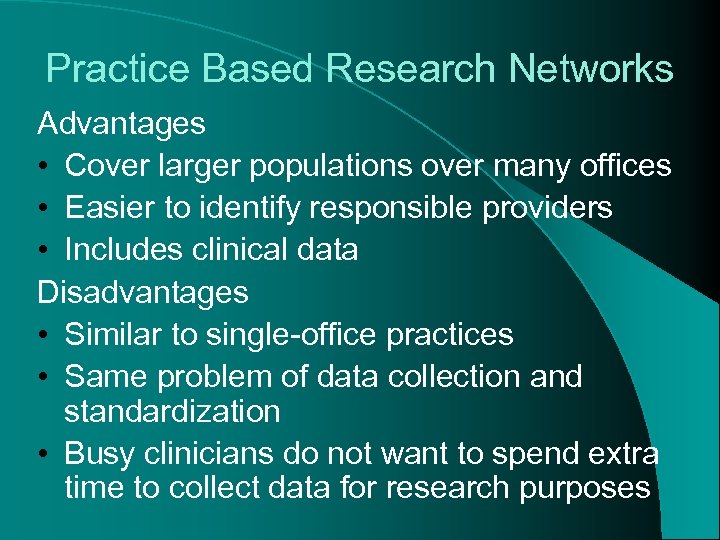
Practice Based Research Networks Advantages • Cover larger populations over many offices • Easier to identify responsible providers • Includes clinical data Disadvantages • Similar to single-office practices • Same problem of data collection and standardization • Busy clinicians do not want to spend extra time to collect data for research purposes
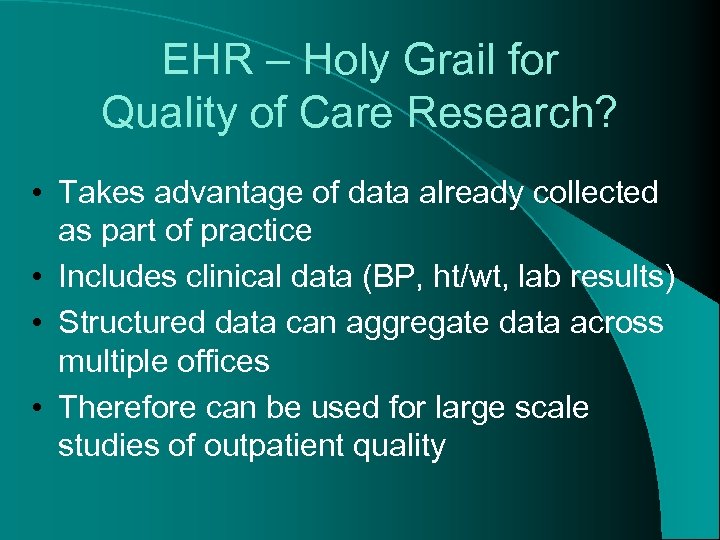
EHR – Holy Grail for Quality of Care Research? • Takes advantage of data already collected as part of practice • Includes clinical data (BP, ht/wt, lab results) • Structured data can aggregate data across multiple offices • Therefore can be used for large scale studies of outpatient quality
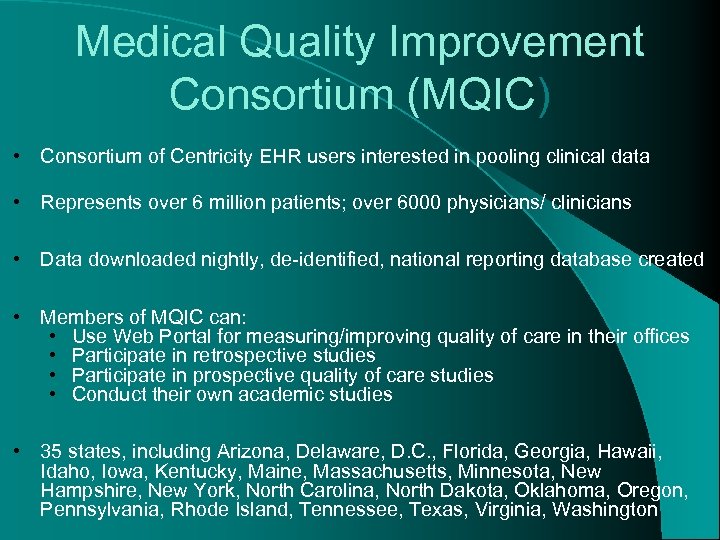
Medical Quality Improvement Consortium (MQIC) • Consortium of Centricity EHR users interested in pooling clinical data • Represents over 6 million patients; over 6000 physicians/ clinicians • Data downloaded nightly, de-identified, national reporting database created • Members of MQIC can: • Use Web Portal for measuring/improving quality of care in their offices • Participate in retrospective studies • Participate in prospective quality of care studies • Conduct their own academic studies • 35 states, including Arizona, Delaware, D. C. , Florida, Georgia, Hawaii, Idaho, Iowa, Kentucky, Maine, Massachusetts, Minnesota, New Hampshire, New York, North Carolina, North Dakota, Oklahoma, Oregon, Pennsylvania, Rhode Island, Tennessee, Texas, Virginia, Washington
Quality of Lipid Management in Outpatient Care: A National Study Using Electronic Health Records James M. Gill, MD, MPH Associate Professor of Family Medicine Senior Scientist in Health Policy Jefferson Medical College, Philadelphia, PA President, Delaware Valley Outcomes Research Ying Chen, MS Delaware Valley Outcomes Research
Methods • Study Design: • Descriptive cohort, using national EHR network • Population: • • Ages 20 -79 years Office visit during three-year study period 7/1/02 – 6/30/05 N = 1. 4 million • High Risk: 161, 468 • Moderate Risk: 186, 514 • Low Risk: 1, 037, 260
Outcome Variables • LDL at Goal • High Risk: LDL < 100 mg/dl • Moderate Risk: LDL < 130 mg/dl • Low Risk: LDL < 160 mg/dl • Lipid Test • Lipid panel every five years if 20 years or older • Annually if high risk • Appropriate Use of Lipid Lowering Medications • On medication if High Risk and LDL > 130 mg/dl
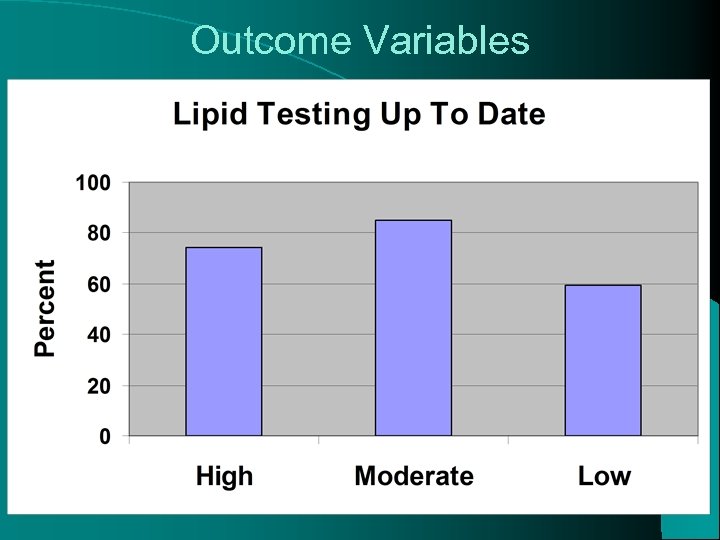
Outcome Variables
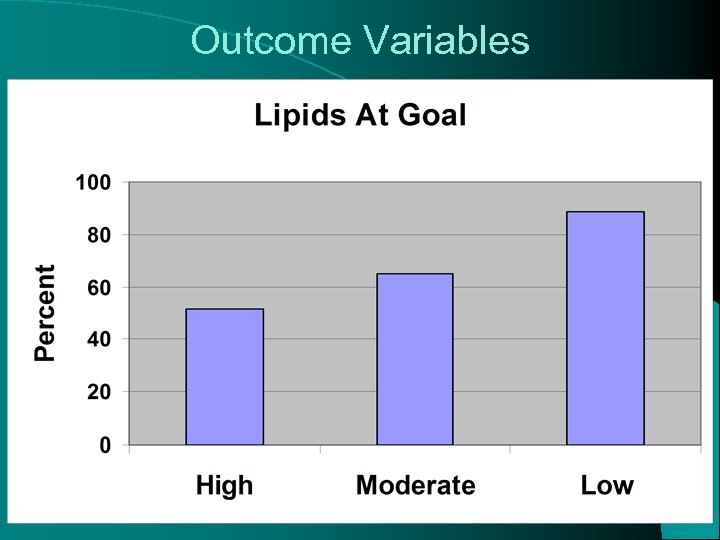
Outcome Variables
Other Retrospective MQIC Studies Diabetes Gill JM, Foy AJ, Ling L. Quality of Outpatient Care for Diabetes Mellitus in a National Electronic Health Record Network. American Journal of Medical Quality. 2006; 21(1): 13 -17. Hypertension Gill JM, Player MS, Yang W, “Patterns of antihypertensive medication use in a U. S. national practice network” North American Primary Care Research Group Orlando, FL October, 2004 Player MS, Gill JM, Bittner-Fagan H, Mainous AG. Antihypertensive prescribing practices: Impact of the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial. The Journal of Clinical Hypertension. 2006; 8(12): 860 -864 Depression Gill JM, “Treatment of Depression in Ambulatory Care: A Study From a National Electronic Health Record (EHR) Network” North American Primary Care Research Group, Tucson, AZ October, 2006 Antibiotics Gill JM, Fleischut P, Haas S, Pellini B, Crawford A, Nash DB. Use of antibiotics for adult upper respiratory infections in outpatient settings: a national ambulatory network study. Family Medicine. 2006; 38(5): 349 -54.
Using Electronic Health Record (EHR)-Based Disease Management Tools to Improve Lipid Management in Primary Care James M. Gill, MD, MPH President, Delaware Valley Outcomes Research Associate Professor of Family Medicine and Sr. Scholar in Health Policy Jefferson Medical College, Philadelphia, PA Ying Xia Chen, MS Michael Lieberman, MD, MS Joseph Glutting, Ph. D James J. Diamond, Ph. D
Design § Randomized, Controlled Trial Participant Population Primary care physicians in Medical Quality Improvement Consortium (MQIC) Experienced EHR users, see patients 8+ hrs/wk • 26 offices randomized in nine states: 13 intervention, 13 usual care • 2 family medicine residency programs, 24 community practices • Community practices range from solo to 12 physicians • 1 office dropped out • Final: 105 physicians in 25 offices All qualifying patients of those physicians included N = 64, 150
Interventions EHR-Based Disease Management Form for Lipid Management • Embedded guidelines for lipid management • Automated reminders for overdue tests or lipids not at goal • Easy access to entering data, ordering tests, prescribing meds • Easy access to printed patient education handouts • Access to web sites for lipid guidelines and education Reports • Tools to identify patients overdue for tests or lipids not at goal • Report run at beginning of study and 6 months
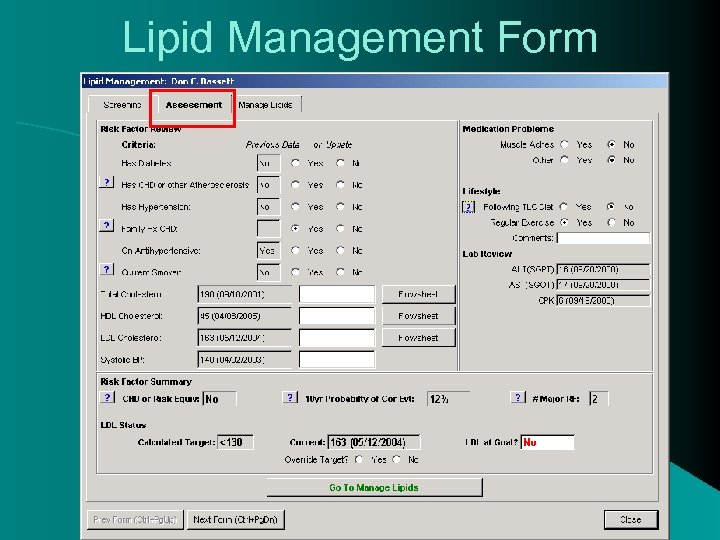
Lipid Management Form
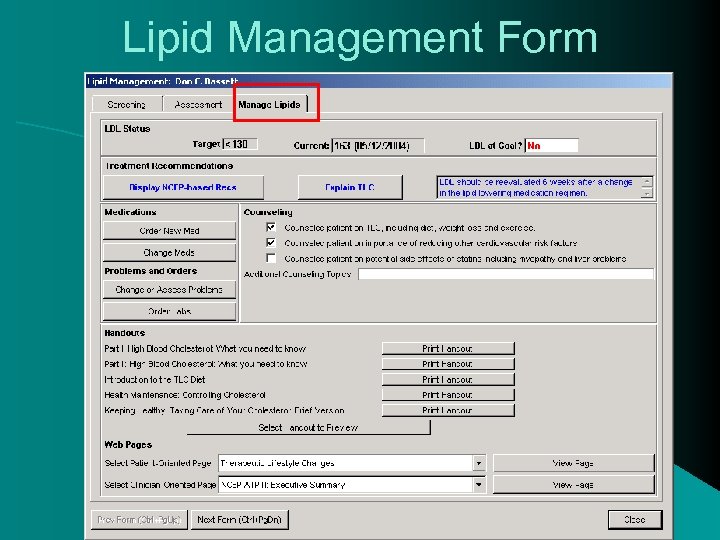
Lipid Management Form
Outcome Variables • LDL at Goal • High Risk: LDL < 100 mg/dl • Moderate Risk: LDL < 130 mg/dl • Low Risk: LDL < 160 mg/dl • Lipid Test • Lipid panel every five years if 20 years or older • Annually if high risk • Appropriate Use of Lipid Lowering Meds • On medication if: • High Risk: LDL > 130 mg/dl
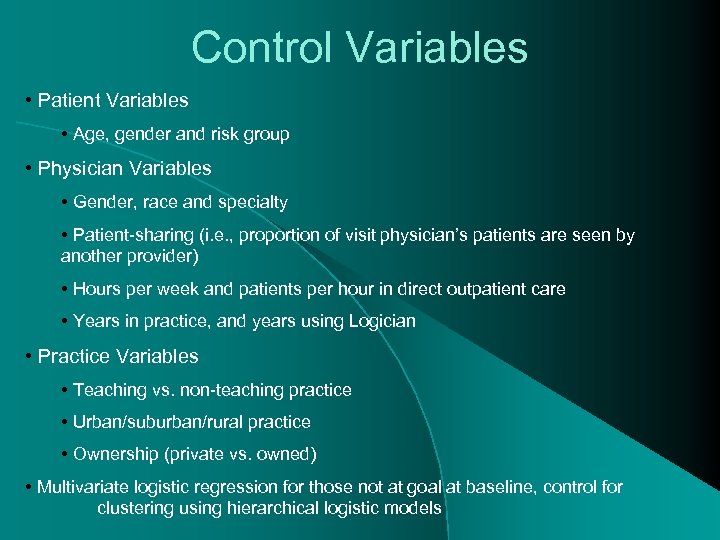
Control Variables • Patient Variables • Age, gender and risk group • Physician Variables • Gender, race and specialty • Patient-sharing (i. e. , proportion of visit physician’s patients are seen by another provider) • Hours per week and patients per hour in direct outpatient care • Years in practice, and years using Logician • Practice Variables • Teaching vs. non-teaching practice • Urban/suburban/rural practice • Ownership (private vs. owned) • Multivariate logistic regression for those not at goal at baseline, control for clustering using hierarchical logistic models
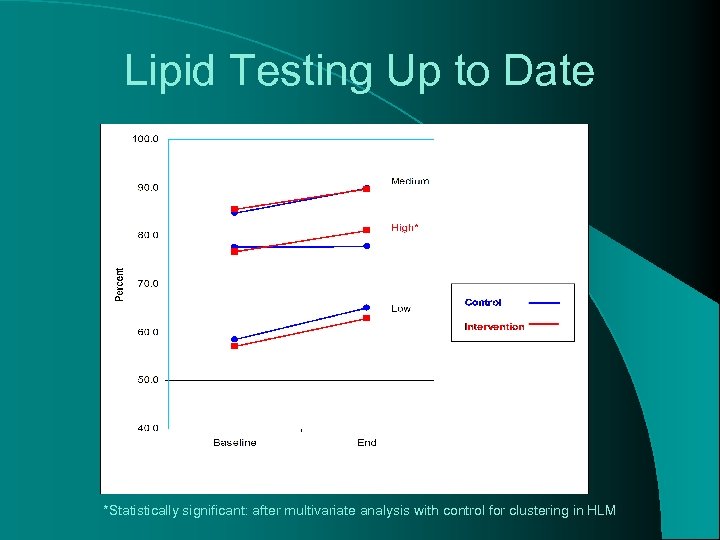
Lipid Testing Up to Date *Statistically significant: after multivariate analysis with control for clustering in HLM
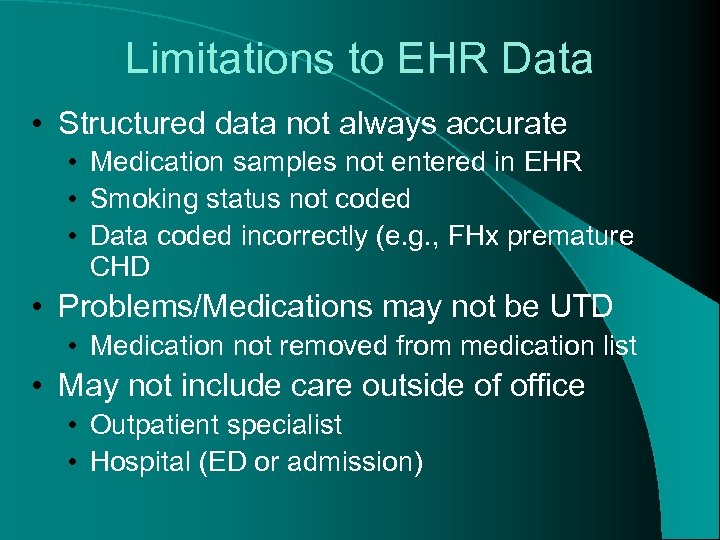
Limitations to EHR Data • Structured data not always accurate • Medication samples not entered in EHR • Smoking status not coded • Data coded incorrectly (e. g. , FHx premature CHD • Problems/Medications may not be UTD • Medication not removed from medication list • May not include care outside of office • Outpatient specialist • Hospital (ED or admission)
EHR for Quality of Care Research • Promising method for measuring outpatient quality of care on large scale • EHR allows for easy access to data • EHR network allows for data to be pooled across large number of offices • For studies requiring clinical data (e. g. , BP, BMI, lab results), EHR data more accurate than other sources • Claims data • Survey data • Ideal framework for PBRNs
39e412fb4fc22fbb1e1704da30a107d1.ppt