80d8071558fc82e03c9dff743ab75051.ppt
- Количество слайдов: 40
BLOOD TRANSFUSION REACTION IN PEDIATRIC AGE GROUP- A TERTIARY CARE CENTRE BASED STUDY Suhailur Rehman Arif SH, Mehdi G, Afzal K, Siddiqui S Department of Pathology & Pediatrics, JN Medical College, AMU, Aligarh
Types of transfusion reactions Transfusion reactions may be acute or delayed: Acute transfusion reaction (within 24 hours). Delayed transfusion reaction (> 24 hr upto months and years) Acute transfusion reactions are further subdivided into immunologic and non-immunologic reactions.
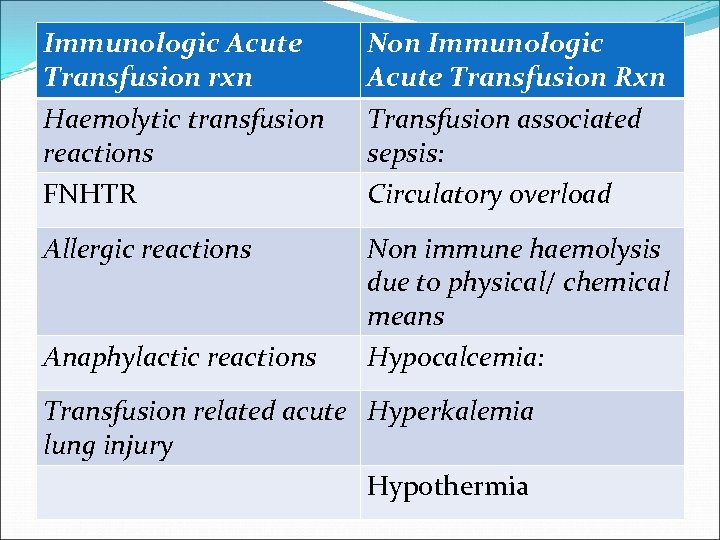
Immunologic Acute Transfusion rxn Non Immunologic Acute Transfusion Rxn Haemolytic transfusion reactions FNHTR Transfusion associated sepsis: Circulatory overload Allergic reactions Non immune haemolysis due to physical/ chemical means Hypocalcemia: Anaphylactic reactions Transfusion related acute Hyperkalemia lung injury Hypothermia
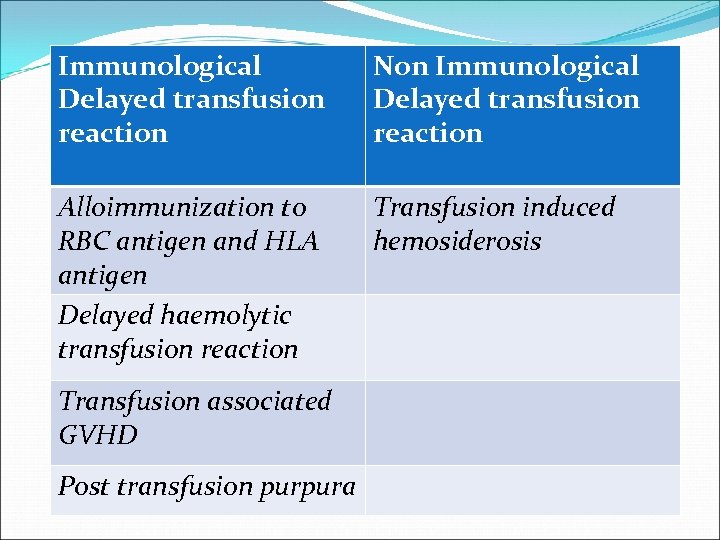
Immunological Delayed transfusion reaction Non Immunological Delayed transfusion reaction Alloimmunization to RBC antigen and HLA antigen Delayed haemolytic transfusion reaction Transfusion induced hemosiderosis Transfusion associated GVHD Post transfusion purpura
Introduction Pediatric transfusion concerns are usually divided into two periods: § Neonates from birth through 4 months § Older infants (>4 months) and children
Reason for considering neonates and infants separately: § Small blood volume § Decreased production of endogenous Erythropoietin in the premature infant. § Physiological anemia of infancy. They have immature immune and metabolic processes Transfusion reaction in neonates and infants deferred from adults for the similar reasons.
Objective of the study It was seen in my pediatric posting during internship that , a large number transfusion reactions in neonates and infants occurred as compared to adults. When I searched the literature, we found very few studies in pediatric age group to the best of my effort. So, I decided to perform this study during my post graduate study and I found a very alarming results.
Aim of the study: To analyse the type of transfusion reaction seen in pediatric age group due to different components. To analyse most common type of transfusion reaction. To find the probable reason associated with them.
Materials and methods The study was conducted on 500 patients admitted to pediatric ward of JN Medical College, AMU, Aligarh, India Pt. who were given transfusion of any of the component were evaluated for transfusion reactions accordingly.
Transfusion reactions that occurred in the course of study were evaluated under following heads: Clinical profile of the patients was assessed before and after transfusion. Blood grouping and cross matching was done by standard techniques (Gel Technology, Diamed Gmb. H Cressier FR Switzerland).
Component transfused. Volume transfused. Time taken for transfusion. Signs and symptoms that developed after reaction if any. To find the reason for the reaction to develop.
If there is any reaction it will be examined according to the same protocol as that of adult – History of patient. Pre & post transfusion clinical profile. Volume of the component transfused. Any previous transfusion. Sample required for investigations are 1. Pre & post transfusion blood sample 2. Urine samples
Condition of the blood bag and its contents like colour of plasma, any supernatant etc. Re-cross match (using gel technique) and Agglutination test (direct and indirect) was done in every case of transfusion reaction. Urine was examined for its color or any hemoglobinuria.
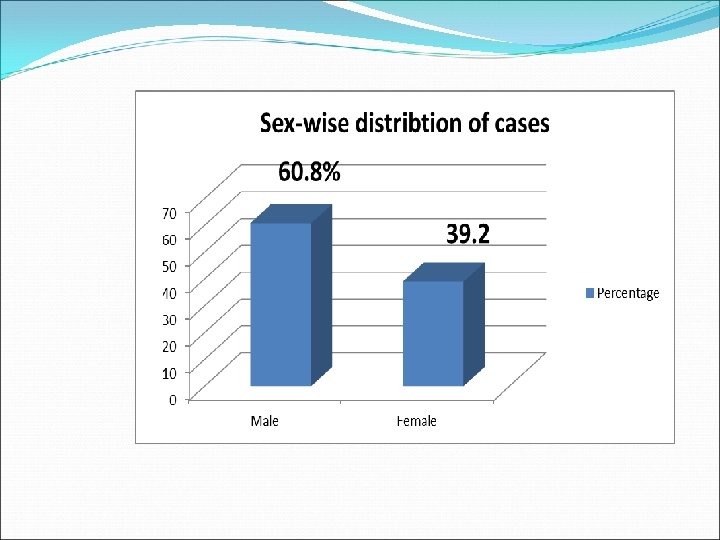
Observation and results Males were more common than females, who required blood transfusion. M: F ratio of 1. 55: 1 was found.
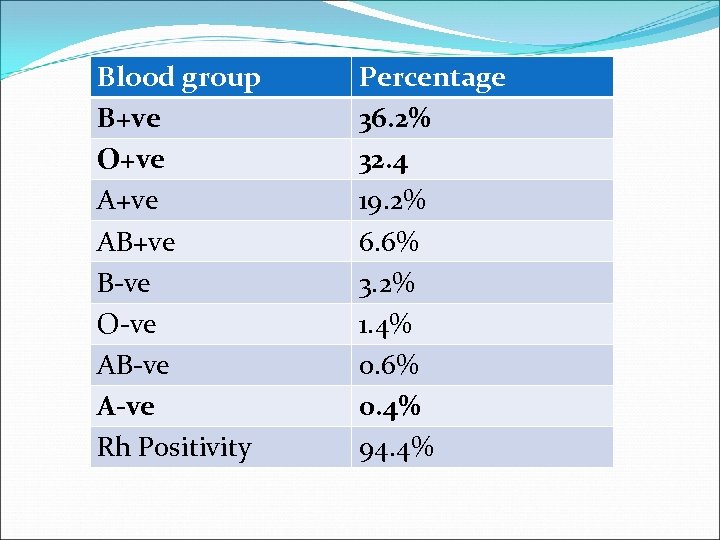
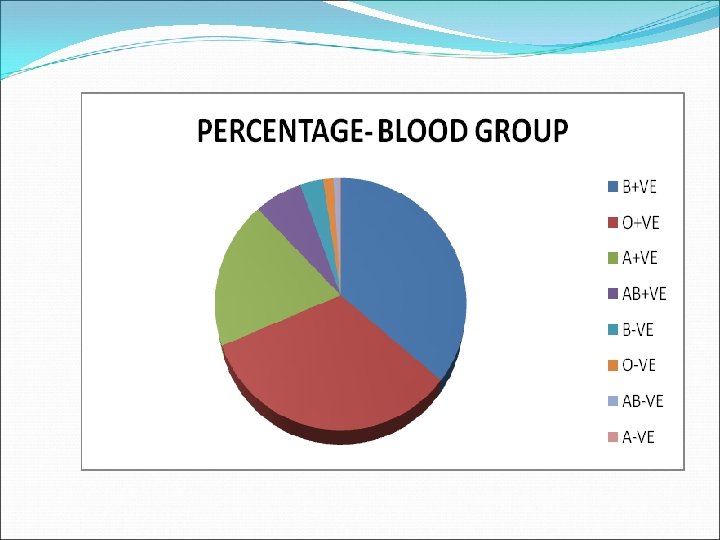
Blood group B+ve O+ve AB+ve B-ve O-ve AB-ve A-ve Rh Positivity Percentage 36. 2% 32. 4 19. 2% 6. 6% 3. 2% 1. 4% 0. 6% 0. 4% 94. 4%
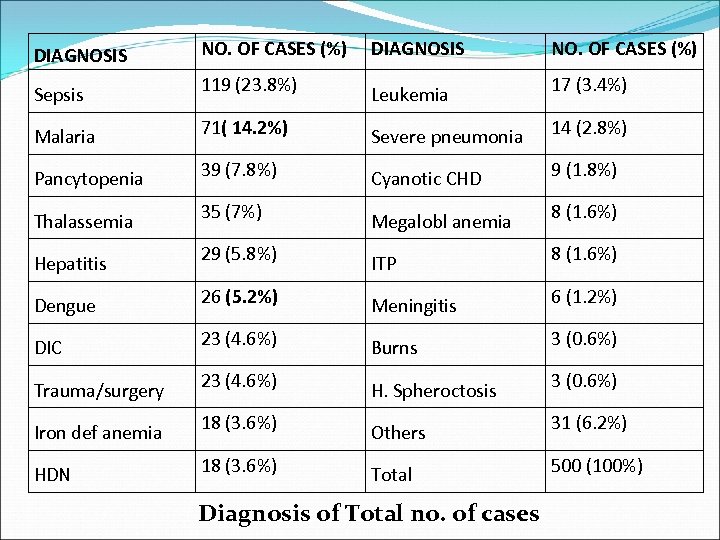
DIAGNOSIS NO. OF CASES (%) Sepsis 119 (23. 8%) Leukemia 17 (3. 4%) Malaria 71( 14. 2%) Severe pneumonia 14 (2. 8%) Pancytopenia 39 (7. 8%) Cyanotic CHD 9 (1. 8%) Thalassemia 35 (7%) Megalobl anemia 8 (1. 6%) Hepatitis 29 (5. 8%) ITP 8 (1. 6%) Dengue 26 (5. 2%) Meningitis 6 (1. 2%) DIC 23 (4. 6%) Burns 3 (0. 6%) Trauma/surgery 23 (4. 6%) H. Spheroctosis 3 (0. 6%) Iron def anemia 18 (3. 6%) Others 31 (6. 2%) HDN 18 (3. 6%) Total 500 (100%) Diagnosis of Total no. of cases
Sepsis/Infection was one of the common disease for which the transfusion was given, especially FFP. However, it was not an approved indication for transfusion. Malaria with features of hemolysis and thrombocytopenia was the 2 nd most common encountered disease, due to endemecity in an around Aligarh.
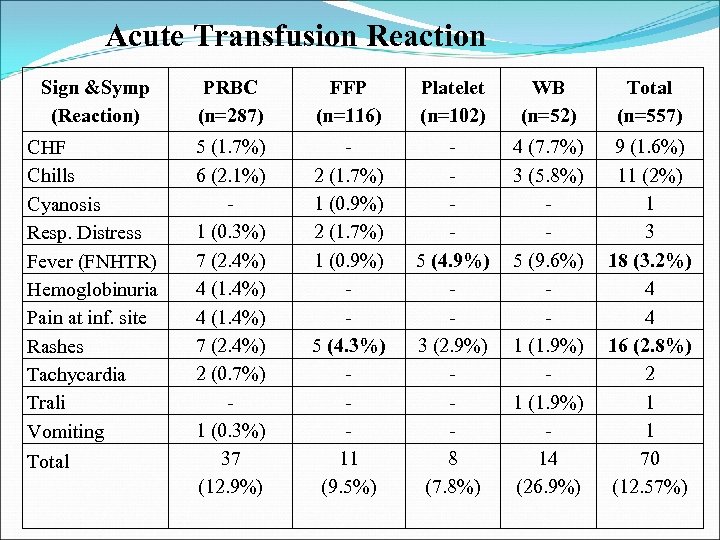
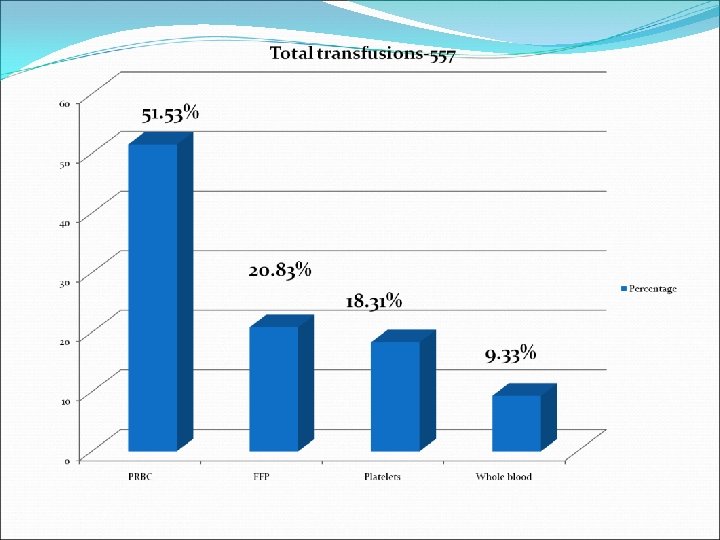
Acute Transfusion Reaction Sign &Symp (Reaction) PRBC (n=287) FFP (n=116) Platelet (n=102) WB (n=52) Total (n=557) CHF Chills Cyanosis Resp. Distress Fever (FNHTR) Hemoglobinuria Pain at inf. site Rashes Tachycardia Trali Vomiting 5 (1. 7%) 6 (2. 1%) 1 (0. 3%) 7 (2. 4%) 4 (1. 4%) 7 (2. 4%) 2 (0. 7%) 1 (0. 3%) 37 (12. 9%) 2 (1. 7%) 1 (0. 9%) 5 (4. 3%) 11 (9. 5%) 5 (4. 9%) 3 (2. 9%) 8 (7. 8%) 4 (7. 7%) 3 (5. 8%) 5 (9. 6%) 1 (1. 9%) 14 (26. 9%) 9 (1. 6%) 11 (2%) 1 3 18 (3. 2%) 4 4 16 (2. 8%) 2 1 1 70 (12. 57%) Total
Acute transfusion reaction was seen in 12. 57% of the cases. PRBC (12. 9%)was the most common component associated with reaction followed by FFP (9. 5%). FNHTR (3. 2%)was the most common transfusion reaction encountered in pediatric age group. FNHTR was most commonly seen in WB (9. 6%)followed by platelet transfusion (4. 9%).
2 nd most common transfusion reaction seen was allergic rashes (2. 8%). Most common component responsible was FFP (4. 3%) 3 rd most common reaction seen was Chills (2%). Most commonly seen in WB and PRBC. However, in most of the cases chills was associated with fever.
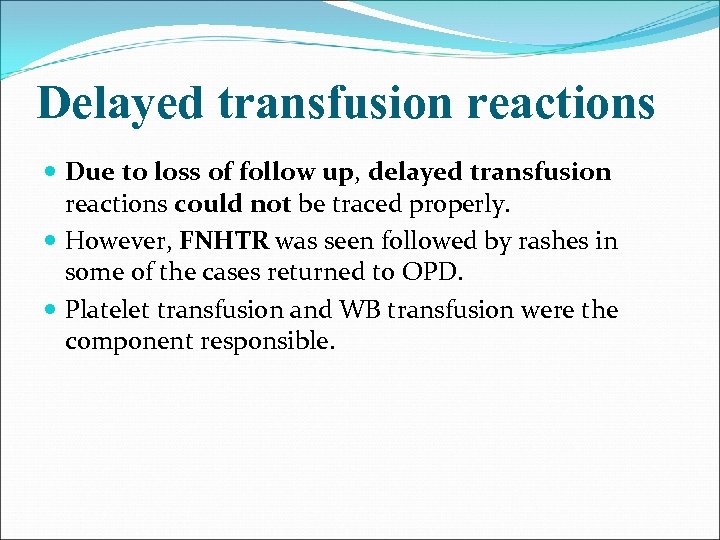
Delayed transfusion reactions Due to loss of follow up, delayed transfusion reactions could not be traced properly. However, FNHTR was seen followed by rashes in some of the cases returned to OPD. Platelet transfusion and WB transfusion were the component responsible.
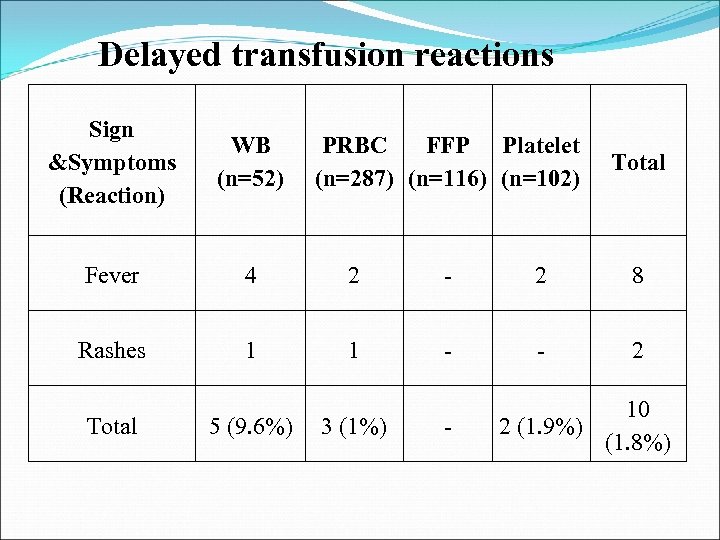
Delayed transfusion reactions Sign &Symptoms (Reaction) WB (n=52) Fever 4 2 - 2 8 Rashes 1 1 - - 2 Total 5 (9. 6%) PRBC FFP Platelet (n=287) (n=116) (n=102) 3 (1%) - Total 10 2 (1. 9%) (1. 8%)
Discussion Acute transfusion reaction was seen in 12. 57% cases. PRBC (12. 9%)was the most common component associated with reaction followed by FFP (9. 5%) and platelets (7. 8%). In a study done by Pedrosaa et al [2013], a prevalence of reactions of 3. 8% was seen in paediatric age group. None of the children who had a reaction were neonates. Regarding the total number of transfusions, adverse events occurred involving 1. 1% of packed red blood cells, 2. 4% of platelet concentrate and 0. 8% of plasma. [Pedrosaa et al , 2013]
![Oakley et al [2015] found an incidence of 6. 2 reactions per 1000 Oakley et al [2015] found an incidence of 6. 2 reactions per 1000](https://present5.com/presentation/80d8071558fc82e03c9dff743ab75051/image-27.jpg)
Oakley et al [2015] found an incidence of 6. 2 reactions per 1000 transfusions within the paediatric (age < 21) population and an incidence of 2. 4 reactions per 1000 transfusions within the adult population. Transfusion reactions were most commonly associated with PLT, followed by RBC, and then plasma transfusions. [Oakley et al. 2015]
This was an alarming result seen during this study as compared to other studies. The reasons could be: pediatric and neonatal age group who are prone and susceptible to their low blood volume and less erythropoietin production, lower immunity status etc. Transfusion reactions like fever, rashes, chills and pain at infusion sites which can be controlled easily by medications, may be under reported in other studies.
FNHTR was most commonly seen in platelets (4. 9%)and whole blood (9. 6%), the reason of which are contaminating WBCs or by cytokines in the plasma produced by the WBCs during storage. Yazer et al (2004) reported 0. 33% of nonhemolytic immunological transfusion reaction in red cell transfusions and 0. 45% in platelet transfusions. Allergic reactions were due to FFP (4. 3%) , the reason of which were A/b to donor plasma proteins.
The probable reason for higher transfusion reactions found in this study were: ØFast transfusion of the blood bags. ØMultiple transfusions in chronic programmes like thallassemia. ØProlonged transfusion due to highly viscous PRBC transfused through small bore needles in pediatric age group. ØWrong indication.
ØImproper temperature maintenance of the bag at the time of transfusion Ø The disease itself acting as an aggravating factor. A detailed eye seeking observation done by my side starting from the component preparation till the end of the transfusion and upto 24 hrs more, making detection of transfusion reaction easy, hence increasing their frequency.
Precautions which should to be taken Use of standard protocol for transfusion led by the transfusion committee should be followed strictly. Rate and volume of the blood product transfused should be according to the weight and age of the patient as they are more vulnerable to volume overload, rapid change in temperature and have immature and inexperienced cellular and humoral immune system. Every transfusion must be carefully watched; pre transfusion vitals must be checked and recorded before starting transfusion and every 15 -30 minutes after starting of transfusion.
Warming the blood bag to the body temperature If any symptoms related to transfusion reaction are seen, transfusion must be stopped immediately and attempt for starting the transfusion after a while can be taken. Slowing the rate of transfusion, if some initial symptoms develops. Changing the IV catheter, if required. But, if reactions did occur again, then the blood bag with all its content and urine should be send to the blood bank of the hospital for evaluation according to the protocol.
Some of the transfusion reactions can be controlled by medications. Leukoreduced platelets/FFP/Whole blood. Irradiation should be done wherever required. Use of single donor platelets should be encouraged in place of random donor platelets.
Specific education of staff, residents in paediatric transfusion practice is very important. The wearing and checking of patient identification e. g. Wristbands is essential in the paediatric age group.
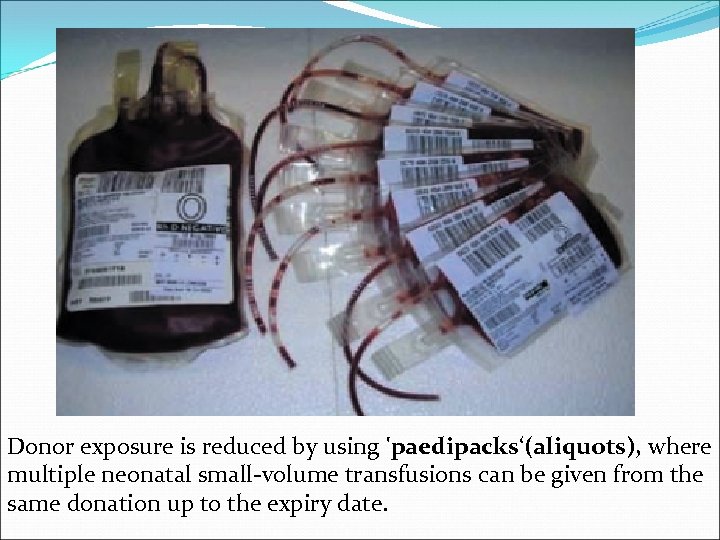
Donor exposure is reduced by using 'paedipacks‘(aliquots), where multiple neonatal small-volume transfusions can be given from the same donation up to the expiry date.
References Pedrosaa. I AKKV, Pinto FJM, Lins LDB, Deus GM. Blood transfusion reactions in children: associated factors. J. Pediatr. (Rio J. ) vol. 89 no. 4 Porto Alegre July/Aug. 2013 http: //dx. doi. org/10. 1016/j. jped. 2012. 009. Oakley FD , Woods M, Arnold S, Young PP. Transfusion reactions in pediatric compared with adult patients: a look at rate, reaction type, and associated products. Transfusion. 2015 Mar; 55(3): 56370. doi: 10. 1111/trf. 12827. Epub 2014 Aug 22. Roseff SD. Pediatric blood collection and transfusion technology. In: Herman JK, Manno CS, eds. Pediatric transfusion therapy. Bethesda, MD: AABB Press, 2002: 21747
Brecher ME, Leger RM, Linden JV, Roseff SD, editors. Technical manual. 15 th ed. Bethesda, Maryland: American association of blood banks; 2005. Corwin HL, Gettinger A. Pearl R. The CRIT study: anemia and blood transfusion in the critically ill--current clinical practice in the United States. Crit Cure Med. 2004; 32: 39 -52. Rudmann SV. Textbook of Blood Banking and Transfusion Medicine. 2 nd ed. Philadelphia, Pennsylvania: Elsevier Saunders; 2005. Hillyer CD; Shaz BH; Zimring JC; Abshire TC. Transfusion Medicine and Hemostasis: Clinical and Laboratory Aspects. New york : Elsevier; 2009.
Kleigman RM, Jenson HB, Behrman RE and Stanton BF. Nelson textbook of pediatrics. 18 th ed. Philadelphia : Elsevier; 2008. Davies P, Robertson S, Hedge S, et al. Calculating the required transfusion volume in children. Transfusion. 2007; 47: 212– 6. Roback JD , Grossman BJ , Harris T , Hillyer CD , editors. Technical manual. 17 th ed. Bethesda (MD): American Association of Blood Banks; 2011. Hillyer CD, Silberstein LE, Ness PM, Anderson KC, Roush KS. Blood Banking and Transfusion Medicine basic principles and practice. Philadelphia, Pennsylvania: Churchill Livingstone an Imprint of Elsevier Science; 2003.

80d8071558fc82e03c9dff743ab75051.ppt