94aec557ac3be3e6b3b42fdafe92529b.ppt
- Количество слайдов: 55
Blood Glucose Measuring in the Pre-Hospital Setting 1
Purpose 1. To prepare Certified First Responders (CFR) and EMTBasics (EMT-Bs) with current certification to utilize a blood glucose measuring device (glucometry) when operating under NY State – approved BLS protocols for Altered Mental Status (AMS), in accordance with: • NYS DOH Policy Statements 05 -04, 12 -01 • Revised NYS BLS Protocol for AMS (M-2) • Suffolk County EMS Medical Director / Suffolk REMAC Standard of Care 2. To provide a review of diabetic and neurologic (CVA/TIA and Seizure) emergencies. 2
Education & Training Objectives • • • Indications to perform glucose test How to obtain blood sample Instruction on glucometer operation What to do with test result Proper disposal of sharps / contaminants Proper action for blood borne pathogen exposure • Proper documentation 3
Note Information within this presentation should be tailored to the specific glucometer used by the ambulance service and should include a review of the manufacturer’s instructions. Documentation of successful completion of this training, by signing the Attestation of Completion Form and completing the hands-on skills review, is required for authorization to perform blood glucose monitoring in the field 4
Agency Responsibility • Ensure compliance with Suffolk County EMS Policy and NY State EMS BLS Protocol • Provide information to the agency’s inclusion in the CLIA Permit-Waiver** • Procure equipment • Provide training and re-training as needed • Establish an agency policy for equipment calibration and maintenance, per manufacturer’s recommendations 5
What is CLIA and why do we need a Permit-Waiver? • The use of blood glucometry equipment and the measurement of a patient’s blood sugar constitutes use of laboratory-acquired specimen data to diagnose and treat a patient • NY State DOH regulations contained in the Clinical Laboratories Evaluation Program (CLEP) require that laboratories, including ambulance services, meet State DOH standards for “laboratories” as a function of the Clinical Laboratories Improvement Amendments (CLIA). • Blood glucometry is a permit-waived test as defined as a simple laboratory examination and procedure that has an insignificant risk of an erroneous result • Suffolk County EMS holds the Multi-Site Permit-waiver for the entire EMS System with each ambulance service listed as an “off-site” laboratory 6
What is CLIA and why do we need a Permit-Waiver? • The permit-waiver application and fee is submitted bi-annually by Suffolk County EMS. • The permit expires every 2 years, current permit effective until April 19, 2015. • If you are affiliated with an ambulance service in Suffolk County operating at the ALS level, your agency already has the proper permit-waiver in place. • If you are affiliated with an ambulance service in Suffolk County operating at the BLS level, or if you are in a BLS-First Response (BLS-FR) agency, your administration has been asked to provide site specific information so we can add your BLS agency to the list of off-site laboratories. Failure to comply will result in your agency being unable to perform blood glucometry. • The CLIA Permit-waiver requires that the agency comply with manufacturer's recommendations for glucometer maintenance and calibration/control testing and documentation. 7
Changes in protocol • As approved by the NY State Commissioner of Health, and adopted by the NYS DOH Bureau of EMS, the Suffolk County EMS Medical Director, in conjunction with the Suffolk REMAC, has authorized the implementation of the revised NY State AMS protocol, which includes 2 new skills for BLS providers: – obtaining blood sugar readings to assist in the identification of hypoglycemia; and the – administration of intranasal naloxone to patients with opiate/opioid overdose. 8
Glucometry Devices • Typical glucometer used to check blood sugar levels. • Many different types and models. 9
• Per NY State DOH requirements, the use of “dextrostix” are prohibited. A glucometer must be used. 10
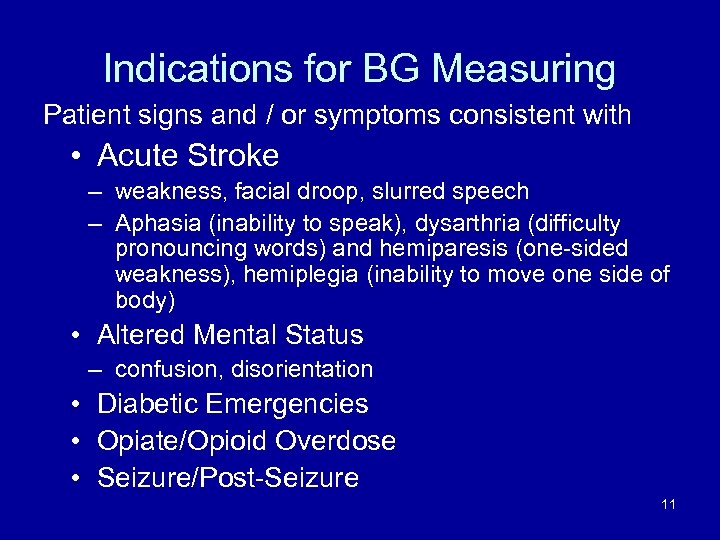
Indications for BG Measuring Patient signs and / or symptoms consistent with • Acute Stroke – weakness, facial droop, slurred speech – Aphasia (inability to speak), dysarthria (difficulty pronouncing words) and hemiparesis (one-sided weakness), hemiplegia (inability to move one side of body) • Altered Mental Status – confusion, disorientation • Diabetic Emergencies • Opiate/Opioid Overdose • Seizure/Post-Seizure 11
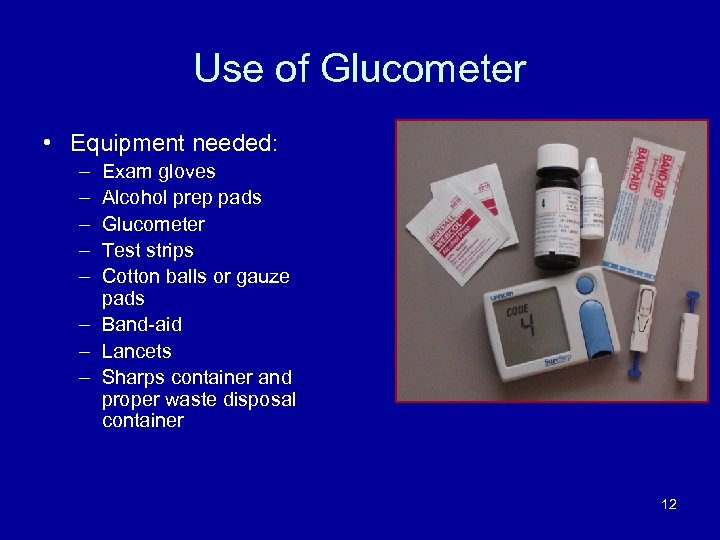
Use of Glucometer • Equipment needed: – – – Exam gloves Alcohol prep pads Glucometer Test strips Cotton balls or gauze pads – Band-aid – Lancets – Sharps container and proper waste disposal container 12
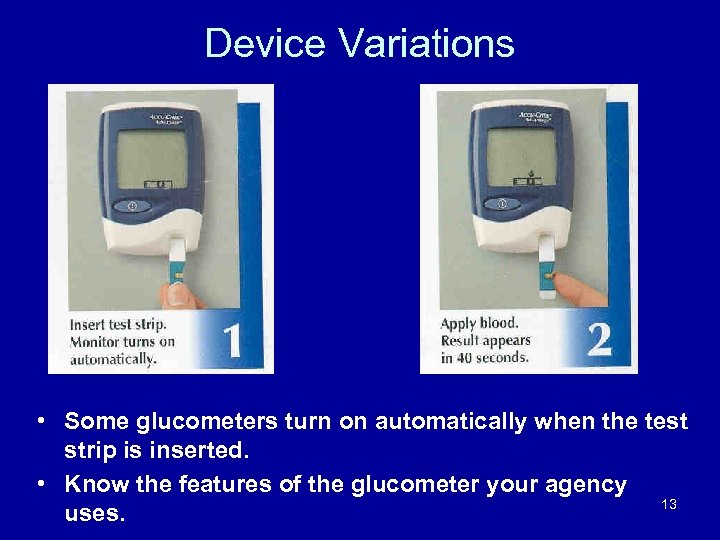
Device Variations • Some glucometers turn on automatically when the test strip is inserted. • Know the features of the glucometer your agency 13 uses.
Manufacturer-Specific Maintenance • Set up requires identification of: – Proper batch number for test strips – Routine control testing – Calibration when necessary – Documentation of control testing and calibrating – Follow manufacturer’s directions 14
Care of the Blood Glucometer • Handle with care! • Do NOT expose to excessive heat, humidity, cold, dust, or dirt • Clean as directed by manufacturer • Store the glucometer and supplies in the case provided by the manufacturer 15
Blood Glucometer Errors Can result from: • Improper calibration of glucometer • Lack of glucometer maintenance and cleaning • Battery failure • Test strip failure • Codes on strip container and glucometer don’t match * Proper care and maintenance of glucometers can help prevent these errors 16
NY State EMS BASIC LIFE SUPPORT PROTOCOL Suffolk County EMS BLOOD GLUCOMETRY POLICY • NOTE: The use of blood glucometry may be of clinical benefit in cases of known history of diabetes controlled by medication with suspected diabetic emergencies, seizure, stroke/CVA, opiate/opioid overdose and behavioral emergencies, and may provide agencies with information necessary to help determine the appropriate treatment and hospital destination for patients with s/s of stroke/CVA. • BLS providers should refer to the most current New York State BLS Altered Mental Status protocol (M-2) ; M-2 revision has been officially published and referred under NYS Policy Statement 13 -10 17
Suffolk County EMS BLS Blood Glucometry Policy • Request Advanced Life Support (ALS) but do not delay transport to the hospital waiting for ALS, or to perform blood glucometry • It is understood that the applicable New York State DOH Basic Life Support (BLS) Protocols are always to be initiated in conjunction with this policy, particularly for AMS, suspected stroke/CVA, seizure, overdose, and behavioral emergencies. • Assess the situation for potential or actual danger. If the scene/situation is not safe, retreat to a safe location, create a safe zone, and obtain additional assistance from a police agency. 18
Suffolk County EMS BLS Blood Glucometry Policy • Persons suspected of a behavioral emergency must be presumed to have an underlying medical or traumatic condition causing the AMS. All suicidal or violent threats or gestures must be taken seriously. • These patients should be in police custody if they pose a danger to themselves or to others. If the patient poses a danger to themselves or others and police are not present, summon police for assistance. • Consider the use of soft restraints per current policy to protect the patient and yourself 19
Suffolk County EMS BLS Blood Glucometry Policy • Perform patient assessment. This protocol is intended for use for any adult patient presenting with the Signs and/or Symptoms of : – stroke – seizure activity; – syncopal episode; – opiate/opioid overdose – previously diagnosed history of diabetes and whose complaints are consistent with signs and symptoms of hypoglycemia. • NOTE: Altered Mental Status denotes a change in the patient’s mentation from their usual status as defined by anyone who is familiar with the patient……OR……. . • • the EMS provider reasonably believes the patient’s GCS is usually 15 and the patient presents with a GCS less than 15. 20
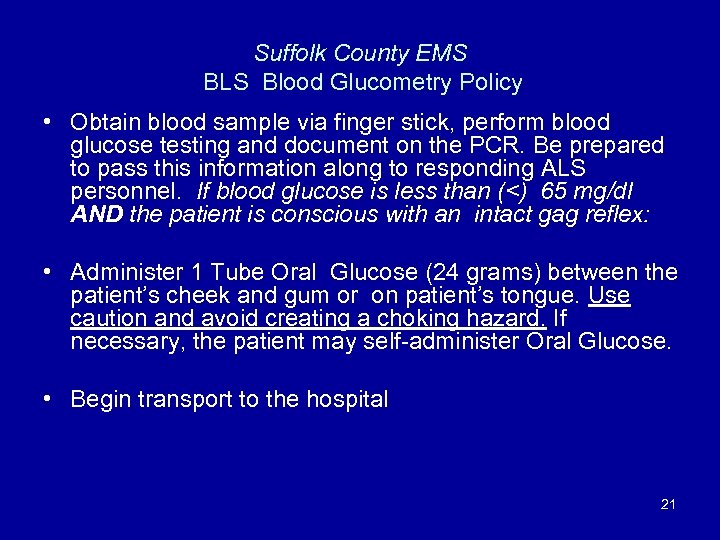
Suffolk County EMS BLS Blood Glucometry Policy • Obtain blood sample via finger stick, perform blood glucose testing and document on the PCR. Be prepared to pass this information along to responding ALS personnel. If blood glucose is less than (<) 65 mg/dl AND the patient is conscious with an intact gag reflex: • Administer 1 Tube Oral Glucose (24 grams) between the patient’s cheek and gum or on patient’s tongue. Use caution and avoid creating a choking hazard. If necessary, the patient may self-administer Oral Glucose. • Begin transport to the hospital 21
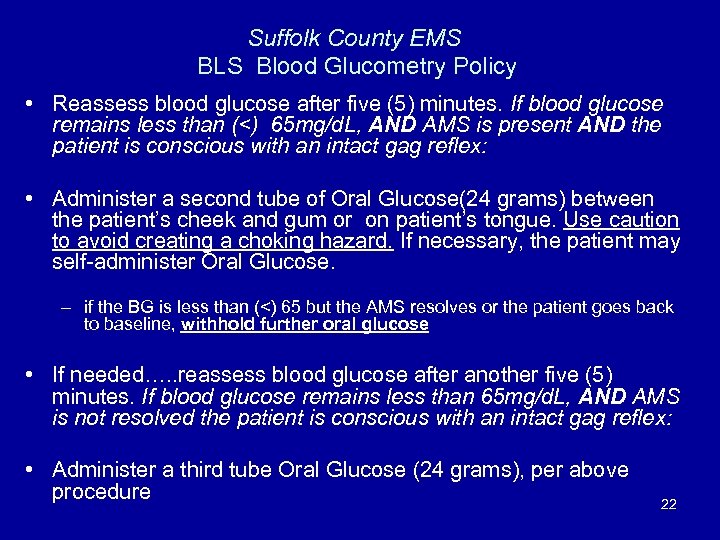
Suffolk County EMS BLS Blood Glucometry Policy • Reassess blood glucose after five (5) minutes. If blood glucose remains less than (<) 65 mg/d. L, AND AMS is present AND the patient is conscious with an intact gag reflex: • Administer a second tube of Oral Glucose(24 grams) between the patient’s cheek and gum or on patient’s tongue. Use caution to avoid creating a choking hazard. If necessary, the patient may self-administer Oral Glucose. – if the BG is less than (<) 65 but the AMS resolves or the patient goes back to baseline, withhold further oral glucose • If needed…. . reassess blood glucose after another five (5) minutes. If blood glucose remains less than 65 mg/d. L, AND AMS is not resolved the patient is conscious with an intact gag reflex: • Administer a third tube Oral Glucose (24 grams), per above procedure 22
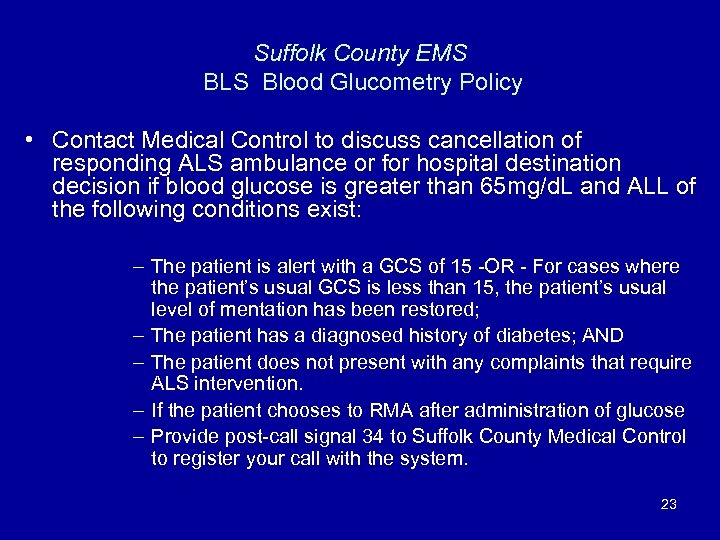
Suffolk County EMS BLS Blood Glucometry Policy • Contact Medical Control to discuss cancellation of responding ALS ambulance or for hospital destination decision if blood glucose is greater than 65 mg/d. L and ALL of the following conditions exist: – The patient is alert with a GCS of 15 -OR - For cases where the patient’s usual GCS is less than 15, the patient’s usual level of mentation has been restored; – The patient has a diagnosed history of diabetes; AND – The patient does not present with any complaints that require ALS intervention. – If the patient chooses to RMA after administration of glucose – Provide post-call signal 34 to Suffolk County Medical Control to register your call with the system. 23
N Y S T A T E B L S P R O T O C O L 24
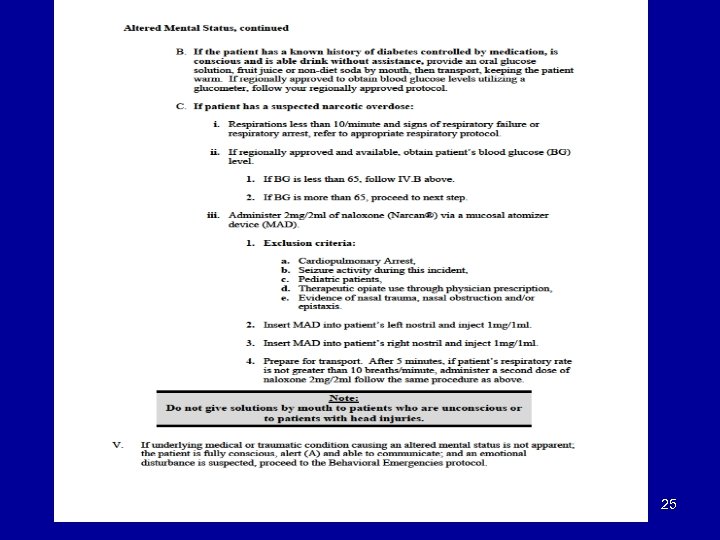
25
26
Fingerstick Procedure For Accurate Glucose Results Credit to: Duke University
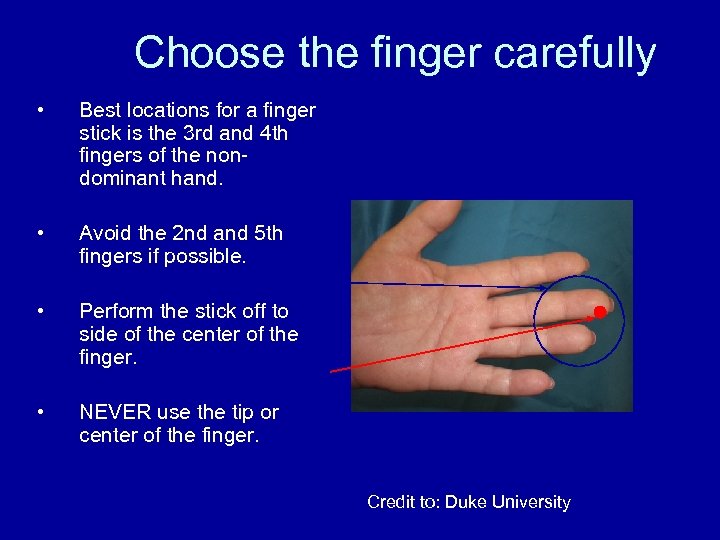
Choose the finger carefully • Best locations for a finger stick is the 3 rd and 4 th fingers of the nondominant hand. • Avoid the 2 nd and 5 th fingers if possible. • Perform the stick off to side of the center of the finger. • NEVER use the tip or center of the finger. Credit to: Duke University
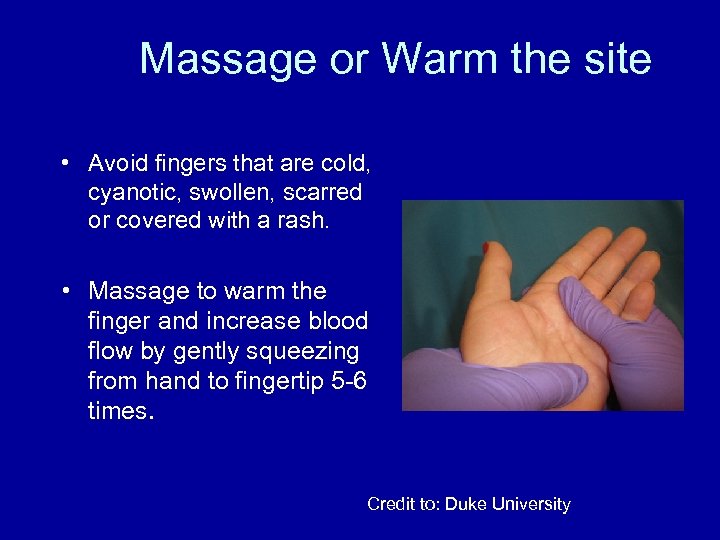
Massage or Warm the site • Avoid fingers that are cold, cyanotic, swollen, scarred or covered with a rash. • Massage to warm the finger and increase blood flow by gently squeezing from hand to fingertip 5 -6 times. Credit to: Duke University
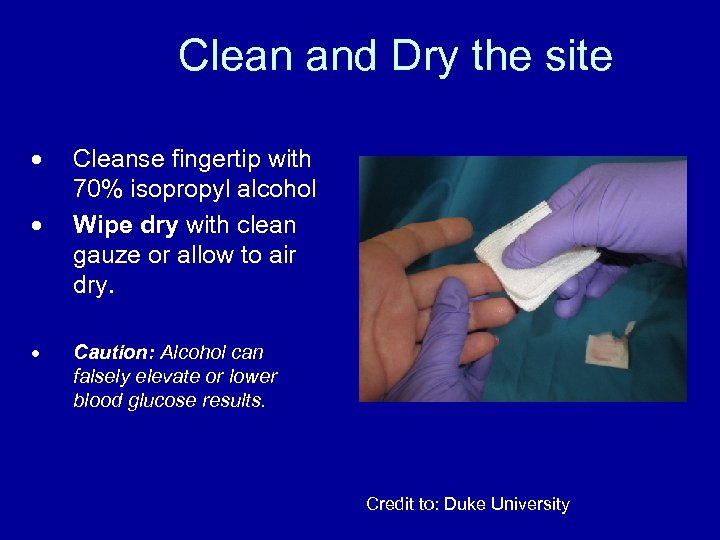
Clean and Dry the site Cleanse fingertip with 70% isopropyl alcohol Wipe dry with clean gauze or allow to air dry. Caution: Alcohol can falsely elevate or lower blood glucose results. Credit to: Duke University
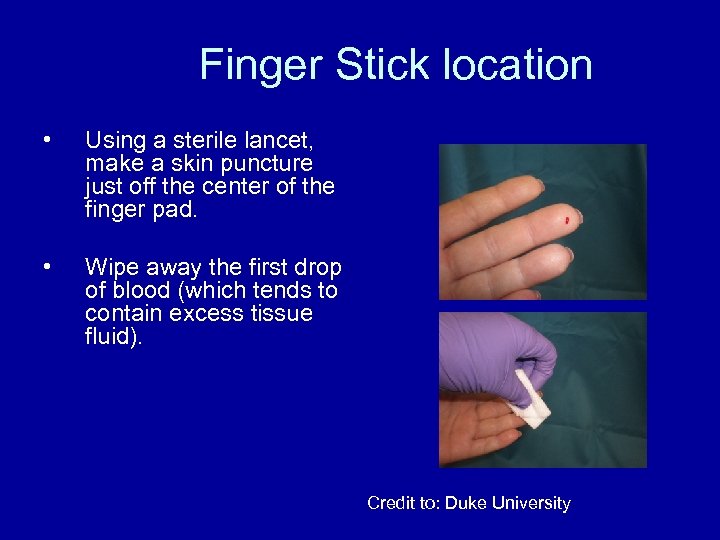
Finger Stick location • Using a sterile lancet, make a skin puncture just off the center of the finger pad. • Wipe away the first drop of blood (which tends to contain excess tissue fluid). Credit to: Duke University
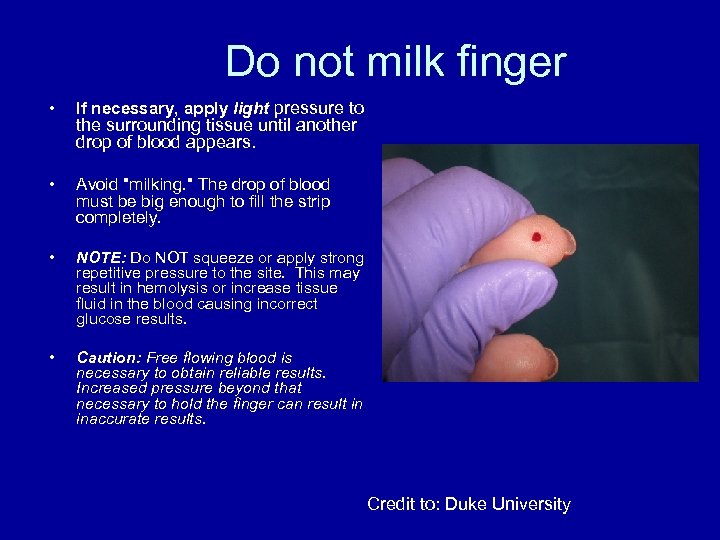
Do not milk finger • If necessary, apply light pressure to • Avoid "milking. " The drop of blood must be big enough to fill the strip completely. • NOTE: Do NOT squeeze or apply strong repetitive pressure to the site. This may result in hemolysis or increase tissue fluid in the blood causing incorrect glucose results. • Caution: Free flowing blood is necessary to obtain reliable results. Increased pressure beyond that necessary to hold the finger can result in inaccurate results. the surrounding tissue until another drop of blood appears. Credit to: Duke University
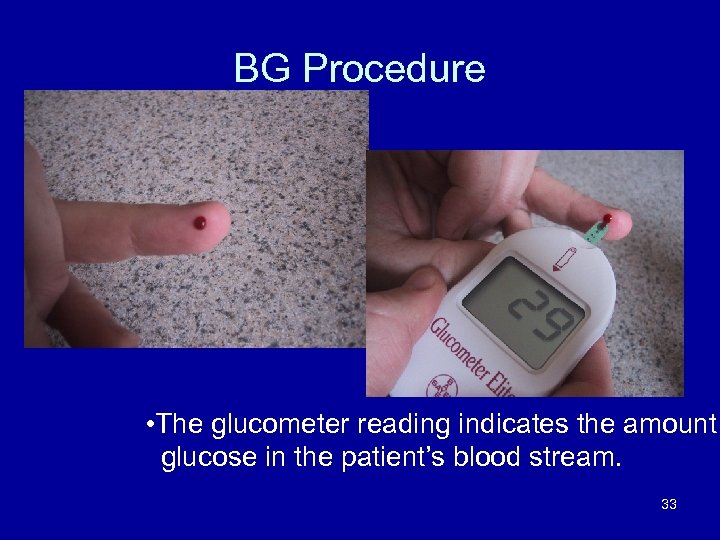
BG Procedure • The glucometer reading indicates the amount glucose in the patient’s blood stream. 33
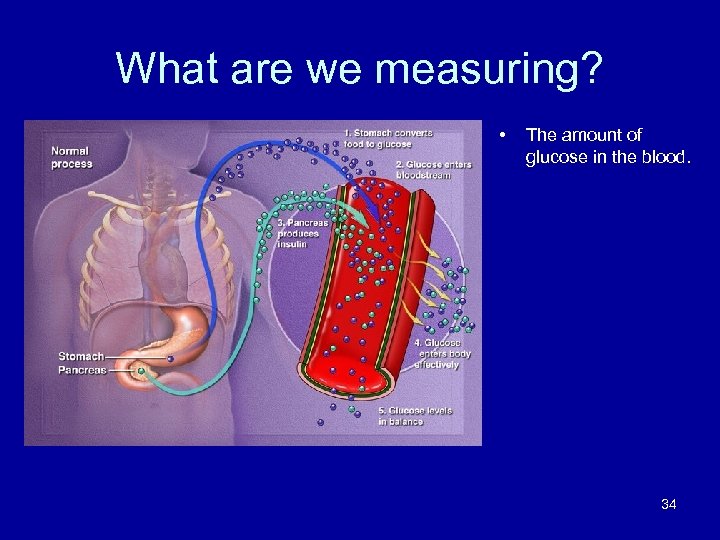
What are we measuring? • The amount of glucose in the blood. 34
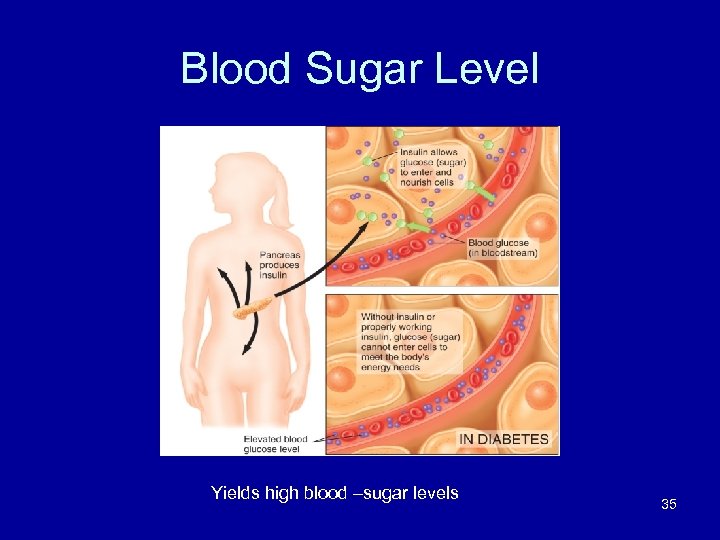
Blood Sugar Level Yields high blood –sugar levels 35
Hyperglycemia and Hypoglycemia • Both lead to diabetic emergencies. • Hyperglycemia: Blood glucose is above normal. – Result of lack of insulin – Untreated, results in DKA
Hyperglycemia and Hypoglycemia • Hypoglycemia: Blood glucose is below normal. – Untreated, results in unresponsiveness and hypoglycemic crisis • Signs and symptoms of hyperglycemia and hypoglycemia are similar.
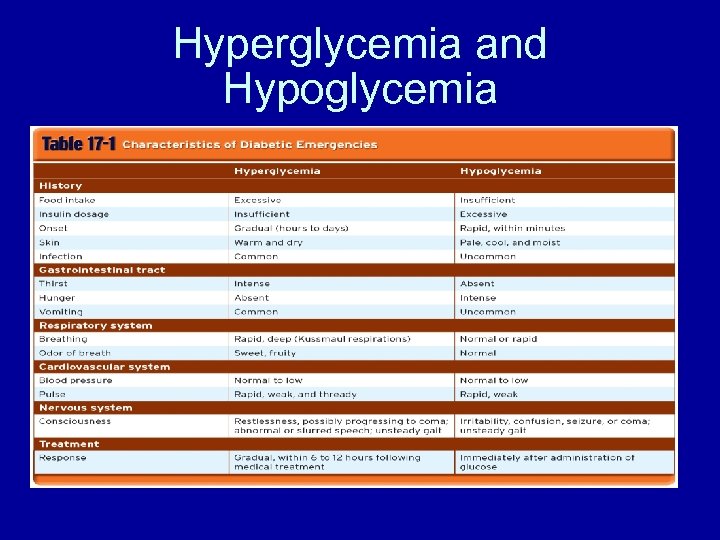
Hyperglycemia and Hypoglycemia
What Now? Properly dispose of sharp Treat the Patient Document Results 39
Administering Glucose • If the blood glucose reading is less than (<) 65 mg/dl and the patient is awake w/ intact gag reflex, let patient them squeeze oral glucose into his/her mouth 40
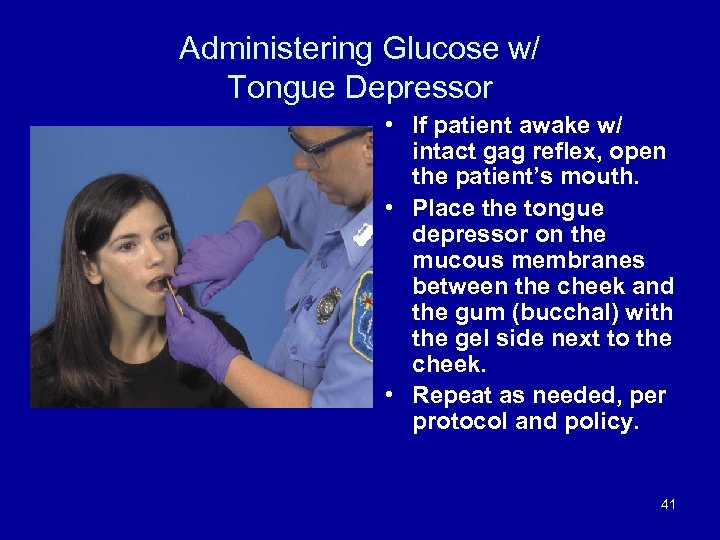
Administering Glucose w/ Tongue Depressor • If patient awake w/ intact gag reflex, open the patient’s mouth. • Place the tongue depressor on the mucous membranes between the cheek and the gum (bucchal) with the gel side next to the cheek. • Repeat as needed, per protocol and policy. 41
Differential Pre-hospital Impressions • Since many of the signs and symptoms of hypoglycemia mimic those of other illnesses / events , it has become the standard of care to use blood glucometry in assisting the provider in determining both a hospital destination and what further intervention during transport is warranted. Some common conditions that hypoglycemia might mimic: – Overdose (Especially Alcohol and Opiates/Opioids) – TIA/CVA (including aphasia, dysarthria and hemiparesis) – Postictal state • In essence, all of these can manifest in “AMS” – Therefore, the modification to the NYS AMS Protocol, to include: • Nasal Narcan administration at the BLS level • Glucometry 42
Hypoglycemia versus Opioid Overdose • If the patient’s blood glucose is greater than (>) 65 mg /dl, the patient is not “hypoglycemic” and other causes of AMS should be explored • Given the new treatment options of inhalation narcan, consider opioid overdose if the patient has AMS and respiratory depression with pinpoint pupils 43
Hypoglycemia versus Stroke/CVA • If patient’s blood glucose is greater than (>) 65 mg/dl and their respiratory rate is normal and there is no evidence of opioid overdose…. consider stroke/CVA 44
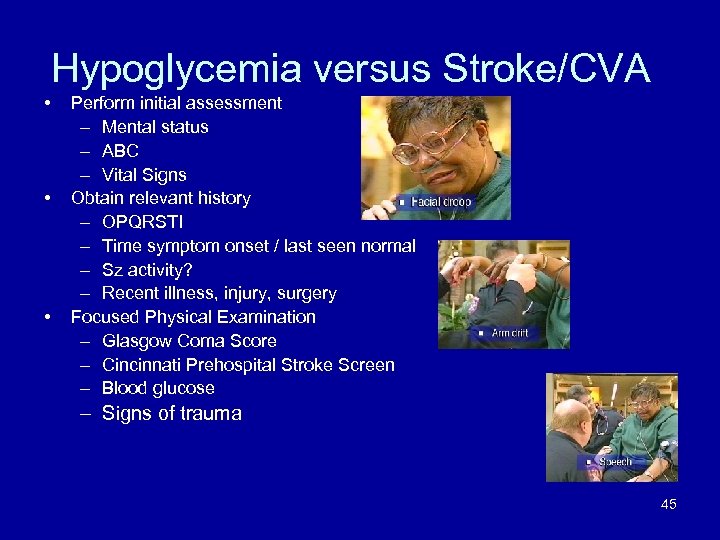
Hypoglycemia versus Stroke/CVA • • • Perform initial assessment – Mental status – ABC – Vital Signs Obtain relevant history – OPQRSTI – Time symptom onset / last seen normal – Sz activity? – Recent illness, injury, surgery Focused Physical Examination – Glasgow Coma Score – Cincinnati Prehospital Stroke Screen – Blood glucose – Signs of trauma 45
Opioid Overdose The signs and symptoms of opioid overdose and the administration of inhalation narcan are covered in the required on-line video review and skills affirmation process Congratulations, you have successfully completed the education phase of blood glucometry
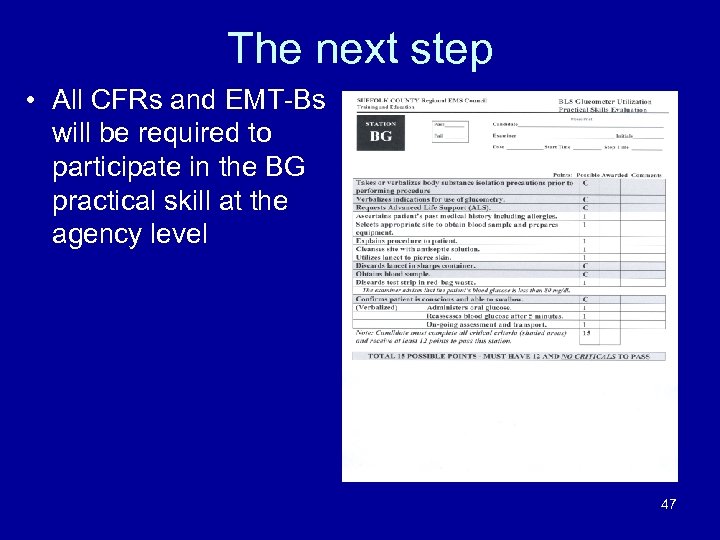
The next step • All CFRs and EMT-Bs will be required to participate in the BG practical skill at the agency level 47
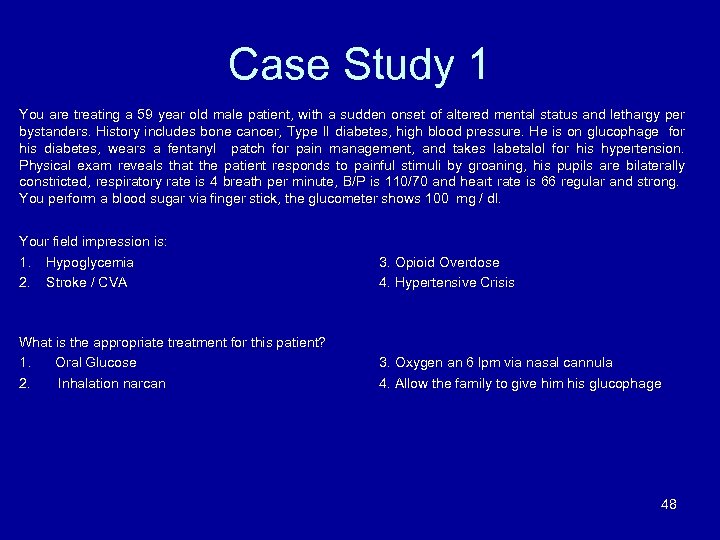
Case Study 1 You are treating a 59 year old male patient, with a sudden onset of altered mental status and lethargy per bystanders. History includes bone cancer, Type II diabetes, high blood pressure. He is on glucophage for his diabetes, wears a fentanyl patch for pain management, and takes labetalol for his hypertension. Physical exam reveals that the patient responds to painful stimuli by groaning, his pupils are bilaterally constricted, respiratory rate is 4 breath per minute, B/P is 110/70 and heart rate is 66 regular and strong. You perform a blood sugar via finger stick, the glucometer shows 100 mg / dl. Your field impression is: 1. Hypoglycemia 2. Stroke / CVA 3. Opioid Overdose 4. Hypertensive Crisis What is the appropriate treatment for this patient? 1. Oral Glucose 2. Inhalation narcan 3. Oxygen an 6 lpm via nasal cannula 4. Allow the family to give him his glucophage 48
Case Study 2 You are treating a 56 year old female patient, with a sudden onset of altered mental status, with difficulty in speaking. History includes heart disease with several TIAs. Patient’s daughter states that the patient was fine all morning, and went into the room when she “heard a sound of breaking glass. ” Daughter also states that the patient returned from an overseas airline flight several days ago. Patient takes no medications on a regular basis. Physical exam reveals that the patient’s eyes are opened spontaneously, pupils are normal in size, equal and reactive, respiratory rate is 14 breath per minute, B/P is 140/90 and heart rate is 72 regular and strong. Because of the AMS, you perform a blood sugar via finger stick, the glucometer shows 88 mg / dl. Cincinnati Prehospital Stroke Screen reveals that the patient has pronator drift with concurrent facial droop and cannot speak normally. Your field impression is: • 2. Hypoglycemia Stroke / CVA 3. Opioid Overdose 4. Acute Myocardial Infarction What is the appropriate treatment for this patient? • 2. Oral Glucose Follow NYS BLS Stroke/CVA Protocol 3. Assist the patient with her prescribed nitroglycerine 4. Inhalation Narcan 49
Case Study 3 You are treating a 26 year old male patient, with a sudden onset of altered mental status, which you are told progressed to “unconsciousness” prior to your arrival on a construction site. The supervisor states that the job needed to be finished so he ordered the crew to work through lunch. He states that he “thinks the patient has sugar problems” and “just returned to work several days ago after recovering from an onthe-job back injury. ” Physical exam reveals that the patient is A&O x 3, speaking well, pupils are normal in size, equal and reactive, respiratory rate is 18 breath per minute, B/P is 126/84 and heart rate is 80 regular and strong. Because of the AMS, you perform a blood sugar via finger stick, the glucometer shows 50 mg / dl. Your field impression is: • • Hypoglycemia Stroke / CVA 3. Opioid Overdose 4. Complications from Back Injury What is the appropriate treatment for this patient? • 2. Oral Glucose Low Dose Aspirin 3. Oxygen, and transport to the closest Trauma Center 4. Inhalation narcan 50
Post-Use Reporting Requirements • All cases of INH narcan must be reported by making a post-call signal 34 to Medical Control at 444 -3600 as soon as feasible after the call to register the call with the system. • All cases of INH narcan must be reported to Suffolk County EMS by sending the post-use data form and a copy of the PCR, within 24 hours of use, either by FAX (852 -5028) or EMAIL to marty. matuza@suffolkcountyny. gov • These cases are to be reported whether or not you perform a blood sugar, as required by NYS DOH policy. • It is the responsibility of the BLS Provider administering the 51 form to report its use.
Post-Use Reporting Requirements • There is no requirement to report obtaining a blood glucose determination in cases where you may obtain a blood sugar reading but you DO NOT administer inhalation narcan 52
The next step Now that you have completed the educational portion of blood glucometry, contact your agency training officer for the required skills review Complete the on-line video and required skills review for inhalation narcan 53
The next step • Documentation for successful completion includes your: • Attestation of Training form for blood glucometry • Skills affirmation checklist for blood glucometry • On-line certificate for inhalation narcan video • Skills affirmation checklist for inhalation narcan 54
END OF PRESENTATION Thank you for your continued support of the Suffolk County EMS System and for taking the time necessary to improve the level of care that you can provide to your patients. Don’t forget to complete the Attestation of Training and Skills Affirmation Forms. 55
94aec557ac3be3e6b3b42fdafe92529b.ppt