5a0dff023cec43e23eb6bc53e917b63f.ppt
- Количество слайдов: 36
BLOOD BANKING 1 - BLOOD PRODUCTS 2 - AUTOLOGOUS TRANSFUSION M. H. Shaheen Maadi Armed Forces Hospital
BLOOD COMPONENTS I- Red Cells: For oxygen carrying capacity II- Plasma : For coagulation proteins III- Platelets: For microvascular bleeding
RED CELL COMPONENTS 1 - Whole blood (2 - Red cell concentrates (Packed RBC 3 - Washed red cells 4 - Leukocyte depleted red cells 5 - Frozen red cells
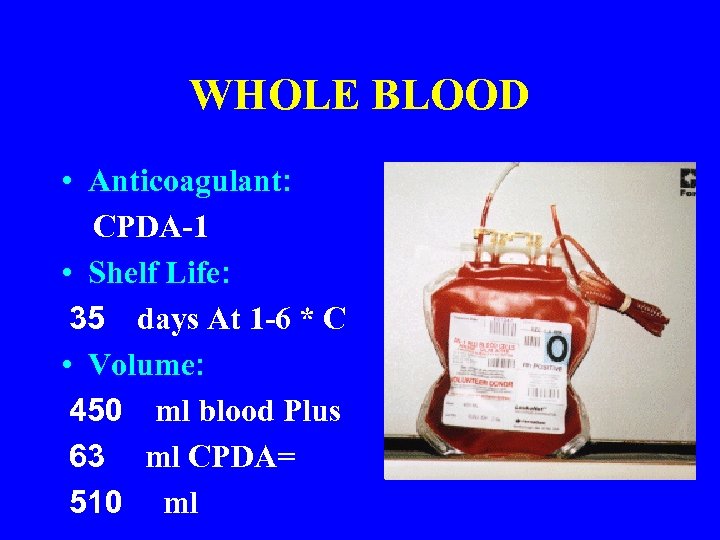
WHOLE BLOOD • Anticoagulant: CPDA-1 • Shelf Life: 35 days At 1 -6 * C • Volume: 450 ml blood Plus 63 ml CPDA= 510 ml
Cont… WHOLE BLOOD • Poor in coagulation proteins & platelets • Corrects oxygen carrying capacity and volume simultaneously • Indicated for the management of trauma and extensive blood loss • One unit of whole blood increases Hct by 3% and Hb level by ~ 1 gm

FRESH WHOLE BLOOD • Less than 5 days old • Indications: - Exchange transfusion Major surgery with massive blood loss Liver transplantation Open heart surgery in infants
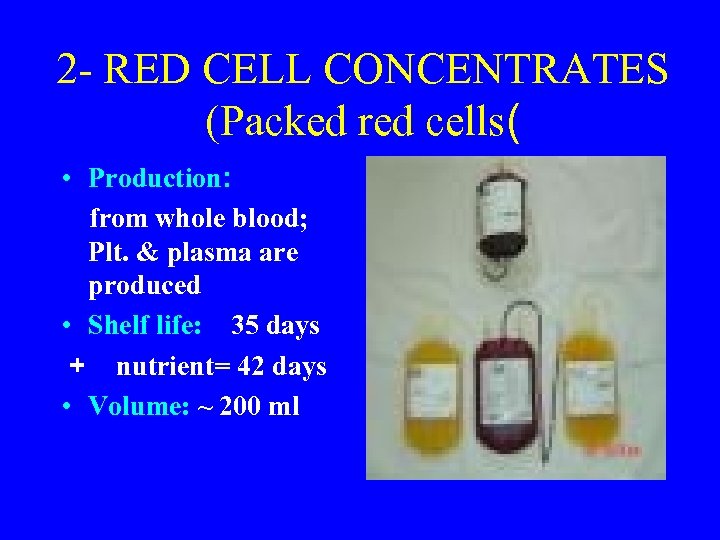
2 - RED CELL CONCENTRATES (Packed red cells( • Production: from whole blood; Plt. & plasma are produced • Shelf life: 35 days + nutrient= 42 days • Volume: ~ 200 ml
Cont…. Packed Red Cells Indications: • Correction of oxygen carrying capacity • Chronic anemia • Before major surgery • Trauma and emergency transfusion
3 - Leukocyte Depleted Red Cells • Preparation: Nylon wool filters • Indication: Non-hemolytic febrile reactions
4 - Washed Red Cells • Manual and automated washing systems • Must be transfused before 24 hours • Washing removes plasma proteins and reduce allergic transfusion reactions • indicated in recurrent an/or sever reactions
4 - Frozen Red Cells • Production: Red cells + Cryoprotective • Storage: Liquid nitrogen or Freezers • Preparation prior to transfusion: Thawing washing and addition of glucose • Transfusion: Within 24 after preparatoin • Indications: Rare blood groups Subgroup antibodies
Appropriate Transfusion Practice of Red Cell Products in various surgical settings • One unit of red cells : 3% increment in Hct increases Hb level by ~ 1 gm • Do not measure Hb &/or Hct before 2 hours • Factors adversely affecting the benefit from transfused red cells: - Continued blood loss - Hemolysis; immune mediated & mechanical - Suppression of erythropoiesis
Red Cell Transfusion in Acute Blood Loss • Blood loss of < 10% of total blood volume: No replacement therapy • Loss Up to 20% : Replace by crystalloids • Loss > 25% : Require red cell transfusion • Preoperative Hb < 10 gm: Historical gold standard for red cell transfusion • Each case must be evaluated individually
II- PLATELET PREPARATIONS 1 - Platelet Concentrates 2 - Apheresis Platelet Units
Appropriate Transfusion practice of Platelet Concentrates • Unit of Platelet Transfusion: - Conventional requirement is 6 units of pooled platelet concentrate - Apheresis platelet unites are largely dependent on donor parameters • Single donor (apheresis) platelets have low risk to recipients than do pooled platelets
Platelet Transfusion Dose • Apheresis Platelets contains 3 x 10^11 Plts • Six units of pooled platelet concentrate= 5. 5 ) 6 x 10^10) Plts • Appropriate transfusion requirement for normal size individual • Post-transfusion increment of ; 5 - 8 x 10^9 /L
Cont… Platelet Transfusion Dose • Approximately one unit of platelet concentrate for each 10 kg body weigh • Objective in the preoperative period: Platelet count > 60, 000 x 10^6 /L • Post-transfusion platelet survival: 8 - 6 days
III- PLASMA DERIVATIVES • Plasma products commonly requested: (1 - Fresh Frozen Plasma (FFP 2 - Cryoprecipitate 3 - Fibrin Glue • Plasma and its derivatives represent a valuable source in transfusion practice • Plasma production: Manually, Aphersis, Industrial fractionation
(1 - Fresh Frozen Plasma (FFP • Storage: 18 * C for up to 1 year • Transfusion: Thawed over 20 30 min • Validity: 24 hours after thawing
Indications of FFP 1 - Multiple acquired coagulation defects: • Liver disease • Massive transfusion • DIC • Rapid reversal of warfarin effect : 2 - Plasma Infusion or exchange • TTP • HUS 3 - Congenital coagulation defects
2 - Cryoprecipiate • Production: FFP thawed at 4* C • Storage: At 18 * C for 1 year • Properties: contains fibrinogen, F VIII and v. WF • Indication: Fibrinogen deficiency & hemophilia A
3 - Fibrin Glue • Topical hemostatic blood product • Production: 1 Cryoprecipitate 2 - Thrombin • Cut , tailored and pasted • Indication: Hemostatic and sealant in cardiac , vascular and other surgical procedures
AUTOLOGOUS BLOOD TRANSFUSION • HISTORY: Remote: 100 years ago Recent: HIV In 1980 th.
ADVANTAGES • Eliminates transfusion transmitted diseases (Hepatitis and HIV( • Prevention of transfusion immunologic reactions • Enhanced recovery from postoperative anemia • High cost benefit LIMITATION: • Risk of blood donation in some cardiac patients
Methods of Collection of Autologous Blood Donations 1 - Preoperative 2 - Intraoperative blood salvage 3 - Intraoperative hemodilutionn
1 - Preoperative Autologous Transfusion • Autologous donation once a week - Normal erythropoiesis - Adequate iron supply • Large volume if cryopreservation is available • Well tolerated even in by some high risk donors • Limitation: Anemia developing during the donation interval (Erythropoietin may help( • In USA , less than 2% require allogeniec blood for elective surgery
2 - Intraoperative Blood Salvage 1 - Systems without washing: - Modified suction devices - Simple and cheap : 2 - Washing systems combined suction device and continuos flow centrifugal system Processing of large blood volume Save ~ 50% of allogeneic blood requirements
3 - Intraoperative Hemodilution • Collection of autologous blood just before the start of surgery • Value in open heart surgery: - Saving of platelet number and function - Reduction of red cell loss - Improves tissue perfusion and oxygenation - Less expensive than preoperative donations








5a0dff023cec43e23eb6bc53e917b63f.ppt