52e8f3a228deac21d1ff13c023cf99c8.ppt
- Количество слайдов: 59
BIRTH CRISIS: NEONATAL DEATH Amy Ellwood, MSW, LCSW Professor of Family Medicine & Psychiatry University of Nevada School of Medicine Las Vegas, Nevada aellwood@medicine. nevada. edu
Goals and Objectives Learn the immediate and long term responses to neonatal death n Learn responses in patient, family, physician and hospital staff n Become familiar with current research on managing birth crisis n Learn about psychosocial resources n
Death is a process, not an event Dying forces us to face our own mortality Death is a process beyond technology Death can be a time of growth, a time to resolve old issues
Research Psych Lit n Pub Med n Cochrane Data Base n National Center for Health Statistics n
Pregnancy & Childbirth A biological event with profound psychological and social outcomes n Occurs in the context of a relationship and culture n It reflects social values and rules n Culture provides “ experts” who preside over the birth be it shaman, midwife or physician n
Birthing History Women presided at births until the 1486 publishing of Malleus Malifaricum n Colonial New England 1620 n – Many midwives were accused of witchcraft (Karlsen, 1987) n Male physicians entered the birthing chamber in the 1500’s (Mitford, 1992)
Birthing History Prior to Louis XIV, birthing occurred in a chair or stool and still does in many “primitive” cultures n “ Only Northern Europeans lie like beetles on their backs and push the infant uphill” (Mitford, 1992) n
BIRTHING STOOL Birthing Stool
Cross Cultural Birthing Practices n Each culture has its beliefs and uniform rituals – Showers, Baptism, Naming Rituals n Each may believe their way is the best way or the only way – (Lorzoff, 1988)
Cross Cultural Practices n There are no males in present day primitive societies who correspond to obstetricians of Western Society
FYI n Scandinavia – Established system of midwives – Home visits pre and post birth – 18 months maternity AND paternity leave – Full salary – Job guarantee
NCHS Definitions Fetal Death: a death that occurs at 20 or more weeks gestation n After 28 weeks is a late fetal death ( National Center for Health Statistics, 2002) n
Neonatal Loss Includes miscarriage n Stillbirth n Sudden Infant Death (SIDS) n
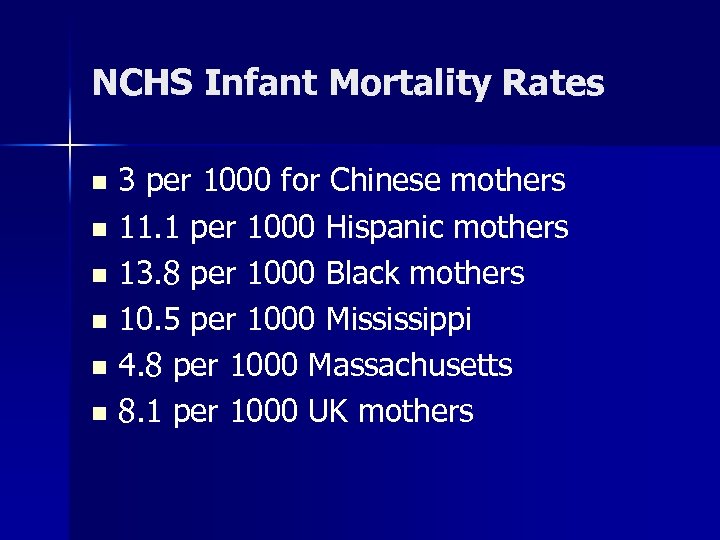
NCHS Infant Mortality Rates 3 per 1000 for Chinese mothers n 11. 1 per 1000 Hispanic mothers n 13. 8 per 1000 Black mothers n 10. 5 per 1000 Mississippi n 4. 8 per 1000 Massachusetts n 8. 1 per 1000 UK mothers n
The Planned Pregnancy Great anticipation for the arrival with “baby shower” rituals n Fantasies/expectations (conscious or unconscious) n Example: John Kennedy III, “ he will fulfill his father’s destiny” n Change in social role/identity n
Neonatal Death n Rituals to honor this event?
Why? What Parents Want to Know Theological explanation: Why did God do this to me? God’s will? n Medical causes? n Punished for past behavior: abortion, affair, drug use? n
Parental Feelings Guilt is common and often irrational n Anger, shock, excruciating sadness n Parents need to retell the story many times to integrate the experience n Listen with gentle understanding n Do not say, “ You can have another child” n Answer their questions n
Grieving Parents n n n n Wonder if they are going crazy Active intervention is essential Suicidal thoughts are common May want to move away to escape the pain May leave the relationship or divorce Increased use of alcohol and drugs May attempt a “ replacement child” too soon
Double Burden n Trauma – An event with actual or threatened death – Response involves intense fear, helplessness and horror n Bereavement/grieving
Multiples What happens if one dies and one lives? n Cannot grieve and attach at same time n Insecure attachment n
Maternal Responses The postpartum body reminds her of the pregnancy loss (sore breasts, abdomen) n Empty crib and shower gifts are reminders of a fantasy shattered n Grief, crying, anger, guilt, shock n PTSD, Major Depression, Panic
Maternal Responses Decreased or increased sexual desire n May want to replace the deceased infant too soon n Vulnerable to PTSD/MDD in subsequent pregnancy (Turton, 2001) n May not attend to other children n Relationship conflict/divorce n
Paternal Responses Societal pressure “ to be strong” and support partners (Badenhorst, 2006) n May delay grieving (O’Leary, 06) n Damage to self-esteem n May increase use of Et. OH/drugs n Decreased work performance/absence n
Paternal Responses Guilt in domestic violence or affairs n Project anger onto physician/staff or partner for “having failed” n Depression, anxiety and PTSD (Turton, 06, ) n Relationship conflict and dissatisfaction n
Sibling Responses – No systematic studies of effect of stillbirth on siblings – Initial confusion – May feel responsible “ I want the baby to die” n Magical thinking – May fear abandonment if parents are preoccupied with their own grief
Grandparents May be highly distraught during this period n Their “baby” is hurting n May feel powerless, left out, overwhelmed n
Physician Reactions Guilt, anxiety n Identification; trigger own issues n Responsibility for outcome n Fear of litigation n
Physician Reactions n Anger – Patient, nurses, system, – Project onto own family n n n Become numb, jaded Increase alcohol use Medicate self with drugs or food Affairs Become controlling
At The Time of Death Address physical and emotional needs n Limit sedation n To see or not to see the baby, that is the question n
The ALSO Method “ It is essential for parents to see and preferable to touch their baby” n Maybe not…. more later n n (ALSO Course Syllabus, 2005)
Communication Best done in patient’s first language n Patient education materials at a 4 -6 th grade level (Williams, 2002) n Use medical interpreter if necessary n
Communication Use direct eye contact unless culturally prohibited (Native Americans) n Sit down and slow down n Do not offer clichés, false hope n Ask if they have questions n
Communication Be candid/honest n Use understandable language, limit “doctor-speak” n Speak directly about death or disability n Avoid “passed on”, “unable to revive” “ is now with the ages” n
Communication “ Accept our condolences, your baby has died, we were unsuccessful in our efforts” n “ You baby has no heart beat, he is not breathing, he has died, I am sorry” n May have to repeat many times n Parents/families need time to integrate information n
Communicating With Parents n Respect privacy – Quiet room/symbol on door – Move to another floor – No throngs of residents or medical students n No one wants an audience! Call in clergy if indicated/wanted
After the Death Respect spiritual/cultural rituals n Bathing/dressing deceased infant important to some n Smell of baby shampoo creates positive olfactory memories n Pictures/mementos important to some but not all n n( Workman, 2001)
Clinical Implications Respect the parent’s wishes to see or not to see n Do not tell them they will adjust to the death better if they do see the baby. n Grief can last up to two years n Monitor for major depression n – Edinburgh Postnatal Depression Scale n Provide resources
Clinical Implications n n Follow-up Share final autopsy results Monitor siblings Discuss future pregnancy & birth control – Delay next pregnancy one year (Turton, 2001) n n Discuss anniversary reactions Respect gender differences in grieving
Take Care of Yourself n n n n Establish a “cuddle group” Process with friend, colleague Balint Group Commune with Mother Nature Reach out to those who love you Prayer, meditation, exercise Respect the healing power of pets
The Nurses Don’t forget them n They are hurting too n They need your affirmation/support n
Medical Students What about them? n What if this is their first rotation? n Help them process this event n
What the Research Says n n n Recent research doubts therapeutic value of encouraging contact with the deceased infant ( Hughes and Riches, 2003 ) Many parents are glad they did see the infant’s body but… Researchers found those who did not see had better outcomes (Hughes, 02, Turton, 06) Those who saw deceased infant had high rates of depression & PTSD in third trimester of next pregnancy (Hughes, 06)
Cochrane 2006 n “No information is available from randomised trials to indicate if there is or is not a benefit from providing specific psychological support after perinatal death” ( retrieved 3 -1 -06)
ALSO 2006 Recommendation n SORT B – “ Although lack of emotional support and grief acknowledgement for mothers suffering from perinatal loss places subsequent pregnancies at risk for poor attachment, no specific psychological support or counseling can be recommended based on current evidence’ – (ALSO Course Syllabus Update 2006)
Replacement Children n The next-born child may be treated with overprotectiveness, anxiety “ vulnerable child syndrome”(Armstrong, 04) Correlations of anxiety disorder in adolescents and maternal experience of stillbirth ( Allen, Lewinsohn, Seeley, ’ 98) Delayed development (Hughes, Turton, Hopper, Mc. Gualey, 2001)
Next Born Infants n n n Next born infants of women who had seen deceased infants had disorganized attachment behavior (Hughes, Turton, Hopper, Mc. Gauley, 2001) Infants showed delayed development (Hughes, Turton, Hopper, Mc. Gauley, 2001)
Remember Emotional pain cannot be quantified The meaning of loss is different for each person Fathers may suffer intense grief and need intervention Know your patient Take care of yourself More good quality research is needed
Perinatal Hospice Offers ways to cope with loss n Helps families who choose to carry an infant with fatal abnormalities n USA now has at least 40 perinatal hospice programs n
Marce Society Formed in 1980 n Louis Victor Marce, French psychiatrist who wrote first treatise devoted to puerperal mental illness n Promotes and facilitates research into mental health of women, infants, children around the time of childbirth n

Resources Society of Compassionate Friends: www. griefsupportdeathofchild. org/ n Marce Society: www. marcesociety. com n Hospital Chaplain n
Resources n Perinatal Hospice – www. perinatalhospice. org/ n Alexandras House – www. alexandrashouse. com
REFERENCES n n Allen, N, Lewinsohn, P, Seeley, R. (1998) Prenatal and perinatal influences on risk for psychopathology in childhood and adolescence. Dev Psychopathology, 10: 513 -529 Armstrong, D. (2004) Impact of prior perinatal loss on subsequent pregnancies, JOGNN, Nov-Dec. 33: 765 -773 Badenhorst W, Riches S, Turton P, Hughes P (2006) The psychological effects of stillbirth and neonatal death on fathers. L systematic review. J. Psychosomatic Obst & Gyn, December: 27(4): 245256 Boyle F, Vance, J, Najman, M, Thearle M. (1996) Mental health impact of stillbirth neonatal death or SIDS: prevalence and patterns of distress among mothers, Soc. Sci. Med. 43: 8: 1273 -1282
References n n n Chambers HM, Chan FY (2000) Support for women/families after perinatal death. Cochrane Database Syst Rev 2000(2): CD 000452. Review Downie A, Letendre A. (2002) Parents’ expectations of midwife-managed care following the loss of a baby in previous pregnancy. J. Adv. Nurs, July: 39: 2: 127 -36 Karlsen CF (1987) The Devil in the Shape of a Woman, New York: Vantage Books
REFERENCES n n Lozoff, B, Jordan B, Malone, S. (1988) Childbirth in Cross-Cultural Perspective, in Transitions to Parenthood, NY: Haworth Press. Mitford, J. (1992) The American Way of Birth, NY: Penguin Books National Center for Health Statistics. (2002) National vital statistics system, fetal deaths. Retrieved from www. cdc. gov/nchs/nvss. htm on 3 -106 O’Leary J, Thorwick C. (2006)Fathers’ perspectives during pregnancy, postperinatal loss. J. Obstet Gynecol Neonatal Nurs. Jan; 35: 1: 78 -86
REFERENCES n n n Hoeldtke, N, Calhoun B. (2001) Perinatal Hospice. AJOG, Sept. 185: 3: 525 -529 Hughes P. , Riches S. (2003) Psychological aspects of perinatal loss, Current Opinion in Obstetrics & Gynecology, 15: 107 -111 Hughes P, Turton P, Hopper E, Evans C. (2002) Assessment of guidelines for good practice in psychosocial care of mothers after stillbirth: a cohort study, Lancet, 360: 114 -118
REFERENCES n n Hughes P, Turton P. Hopper E, Mc. Gauley G. (2001) Disorganised attachment behaviour among infants born subsequent to stillbirth. J. Child Psychology & Psychiatry, 42: 6; 791801 Toedter L, Lasker J, Janssen H. (2001) International comparison of studies using the perinatal grief scale: a decade of research on pregnancy loss. Death Studies April-May; 25: 3: 205 -28.
REFERENCES n n Turton P, Badenhorst W, Hughes P, Ward J, Riches S, White S. (2006) Psychological impact of stillbirth on fathers in the subsequent pregnancy and puerperium. BJP 188: 165 -172 Turton P, Hughes P, Evans C, Faniman D. (2001) Incidence, correlates and predictors of PTSD in pregnancy after stillbirth, BJP, 178: 556 -560
REFERENCES Workman, E. (2001) Guiding parents through the death of their infant. JOGNN, Nov/Dec, 30: 6: 569 -573 n Newman L, Williams J. (1989) The family physician’s role following a neonatal death, J. Family Practice, 29: 5: 521 -525 n
52e8f3a228deac21d1ff13c023cf99c8.ppt