e93a6b480e99bdccb5eed106fbbd37eb.ppt
- Количество слайдов: 48
Birth control and breastfeeding What does the evidence say? Eve Espey, MD MPH
Mark Twain Get your facts straight, Then you can distort ‘em any way you want
Objectives Understand the current evidence related to the impact of hormonal contraception on breastfeeding Describe current expert opinion about the appropriate choice of hormonal contraceptives for breastfeeding women Be aware of future directions for research in this area
Case 18 y/o G 1 P 1 s/p NSVD yesterday is ready for discharge. You note on the chart that she is breastfeeding. You have counseled her about birth control pills. What should you prescribe?
Answer An IUD
Birth control and breastfeeding Public health issue of global importance 100 million postpartum women/yr decide: – What method – When to start it
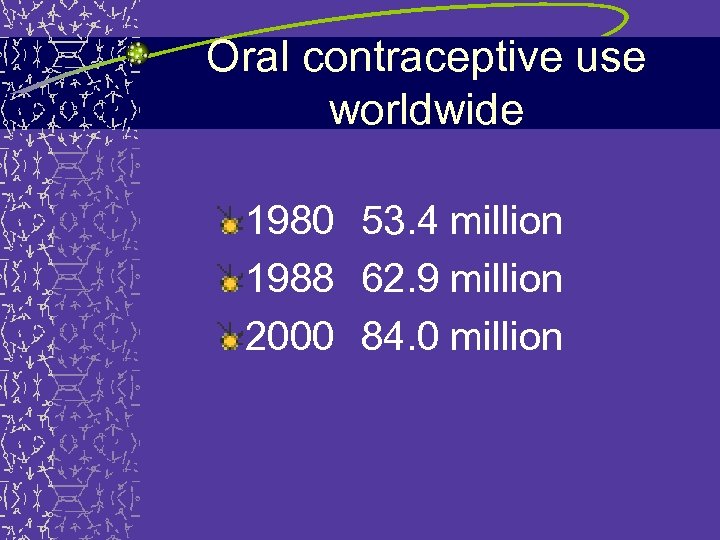
Oral contraceptive use worldwide 1980 53. 4 million 1988 62. 9 million 2000 84. 0 million

2 Good Things Postpartum contraception – Birth interval < 24 months rarely desired – Maternal/infant mortality Breastfeeding – Complete nutrition – Safe food source – Immunological defense – Saves money – Reduces risk of breast and ovarian cancer
Global strategy on infant and young child nutrition Revitalization of the global commitment to appropriate infant and young child nutrition, and in particular to breastfeeding WHO, 4/02

US commitment to breastfeeding American Academy of Pediatrics – Breastfeeding is the ideal method of feeding and nurturing infants Healthy People 2010 – Increase rates of breastfeeding initiation and continuation
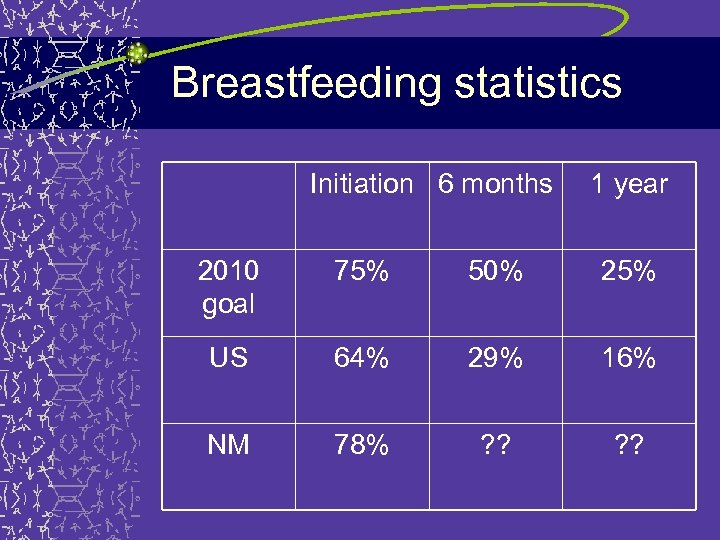
Breastfeeding statistics Initiation 6 months 1 year 2010 goal 75% 50% 25% US 64% 29% 16% NM 78% ? ?
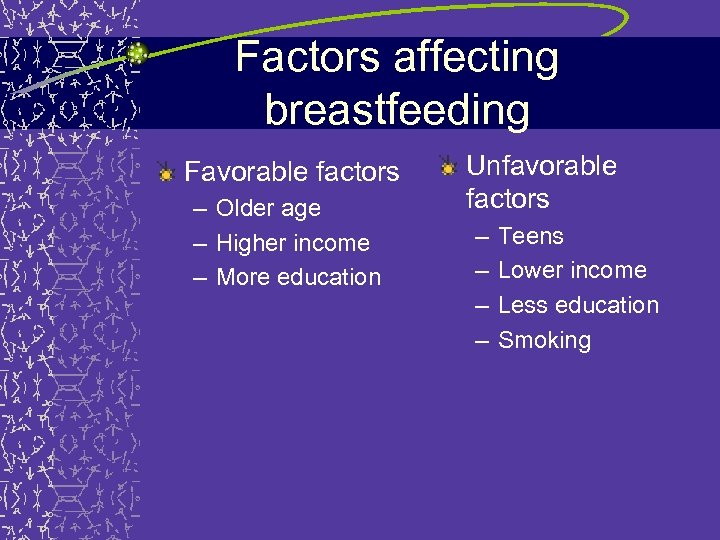
Factors affecting breastfeeding Favorable factors – Older age – Higher income – More education Unfavorable factors – – Teens Lower income Less education Smoking
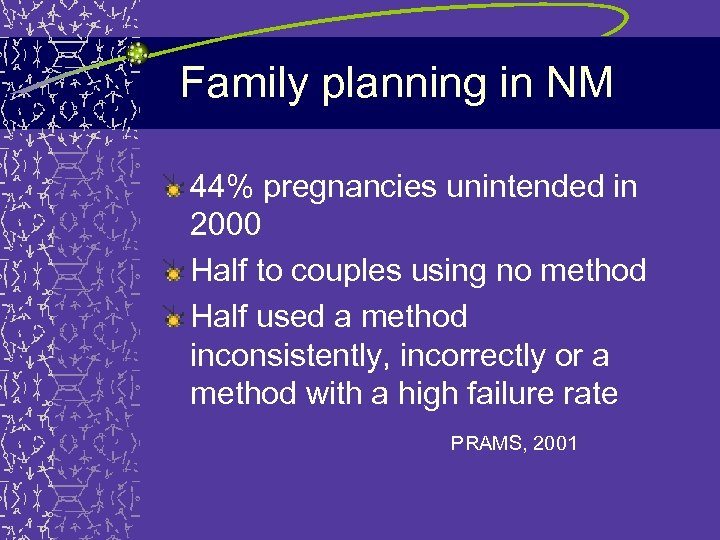
Family planning in NM 44% pregnancies unintended in 2000 Half to couples using no method Half used a method inconsistently, incorrectly or a method with a high failure rate PRAMS, 2001
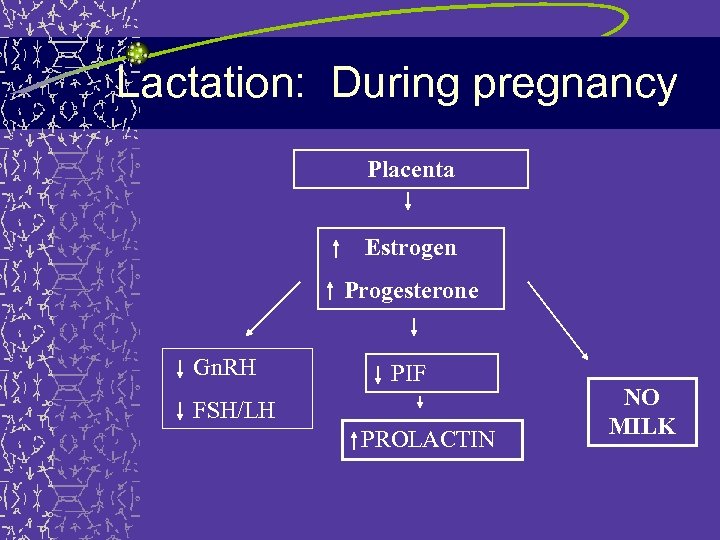
Lactation: During pregnancy Placenta Estrogen Progesterone Gn. RH PIF FSH/LH PROLACTIN NO MILK
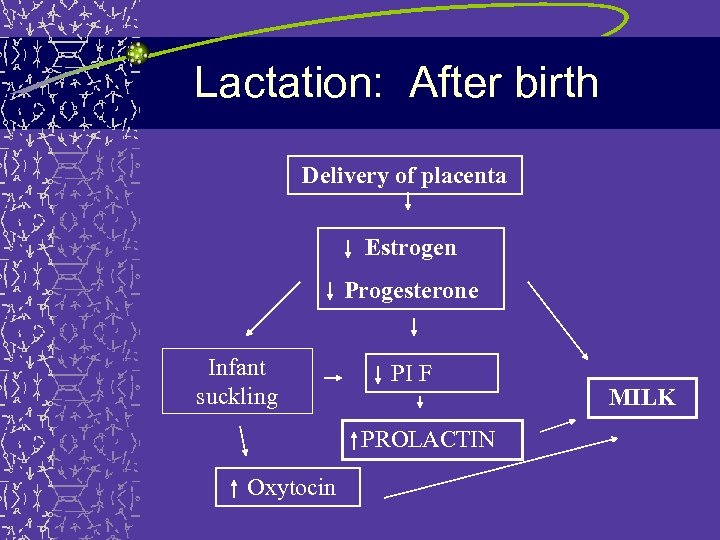
Lactation: After birth Delivery of placenta Estrogen Progesterone Infant suckling PI F PROLACTIN Oxytocin MILK

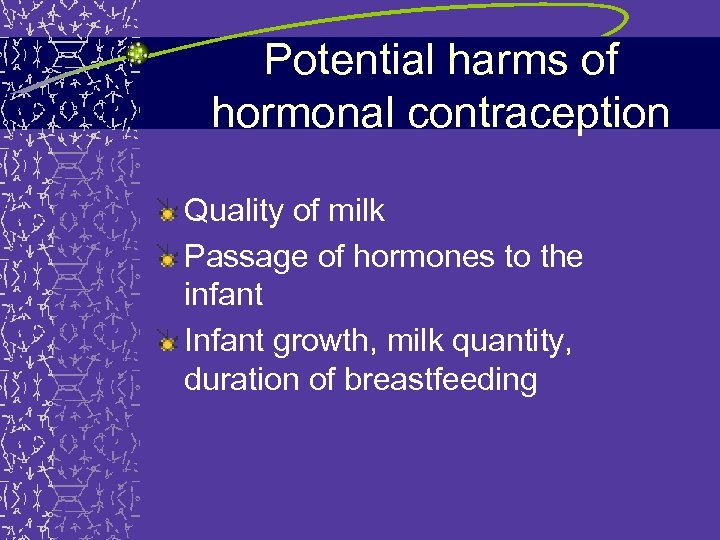
Potential harms of hormonal contraception Quality of milk Passage of hormones to the infant Infant growth, milk quantity, duration of breastfeeding
Potential harms of hormonal contraception Quality of milk Passage of hormones to the infant Infant growth, milk quantity
Quality of milk WHO, 1988 “ 10 cc aliquots expressed, freezedried and transported to London by air” Some differences in micronutrients and fat content – Conflicting interpretation of significance – Infant growth a better, but elusive
Potential harms of hormonal contraception Quality of milk Passage of hormones to the infant Infant growth, milk quantity, duration of breastfeeding
Passage of hormones to infant Case reports Measuring steroid content of breast milk Estradiol in breast milk AND in maternal serum after ingestion of pill (50 mic) 600 cc breastmilk/day from mother taking a 50 mic COC: – 10 ng of estradiol compared with – 3 -6 ng during anovulatory cycles – 6 -12 ng during ovulatory cycles
Long term effects: Nilsson, 1986 48 children exposed to COCs in breastmilk 48 controls 8 year follow-up No differences in – Growth – Disease – Intellectual development – Psychological behavior
Potential harms of hormonal contraception Quality of milk Passage of hormones to the infant Infant growth, milk quantity, duration of breastfeeding
Combined pills: 3 RCTs 2: COC vs. placebo 1: COC vs. progestin-only
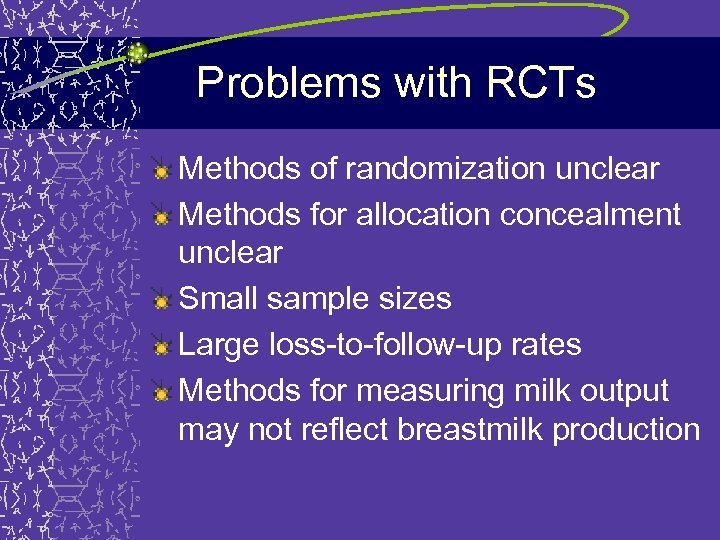
Problems with RCTs Methods of randomization unclear Methods for allocation concealment unclear Small sample sizes Large loss-to-follow-up rates Methods for measuring milk output may not reflect breastmilk production
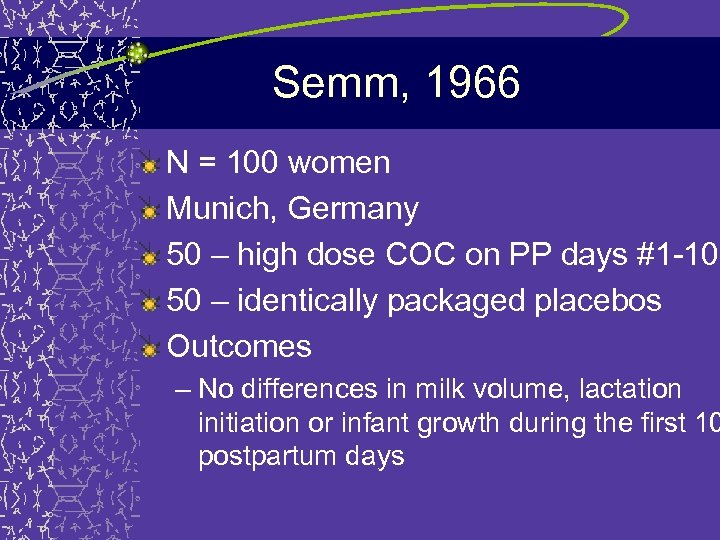
Semm, 1966 N = 100 women Munich, Germany 50 – high dose COC on PP days #1 -10 50 – identically packaged placebos Outcomes – No differences in milk volume, lactation initiation or infant growth during the first 10 postpartum days
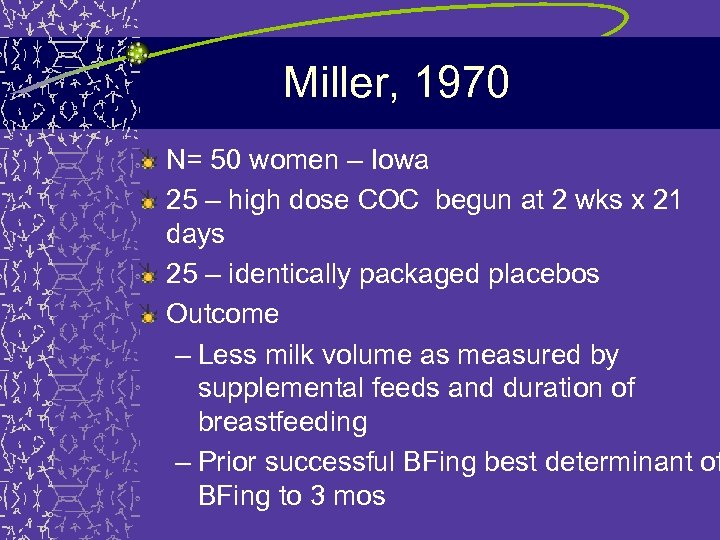
Miller, 1970 N= 50 women – Iowa 25 – high dose COC begun at 2 wks x 21 days 25 – identically packaged placebos Outcome – Less milk volume as measured by supplemental feeds and duration of breastfeeding – Prior successful BFing best determinant of BFing to 3 mos
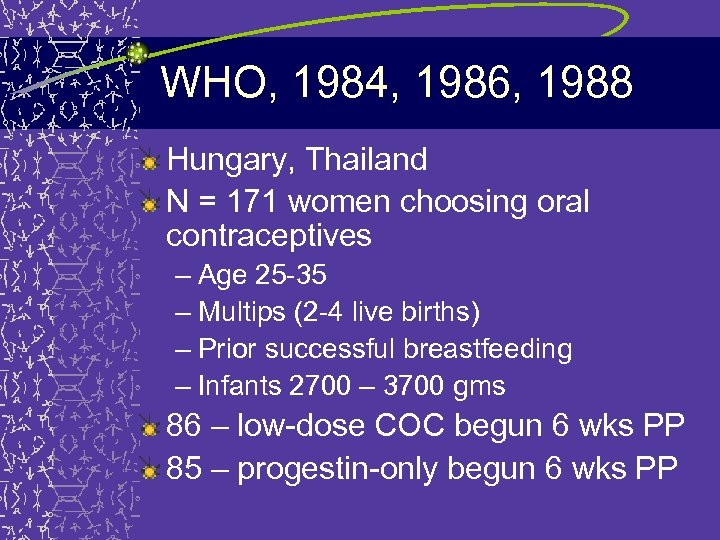
WHO, 1984, 1986, 1988 Hungary, Thailand N = 171 women choosing oral contraceptives – Age 25 -35 – Multips (2 -4 live births) – Prior successful breastfeeding – Infants 2700 – 3700 gms 86 – low-dose COC begun 6 wks PP 85 – progestin-only begun 6 wks PP
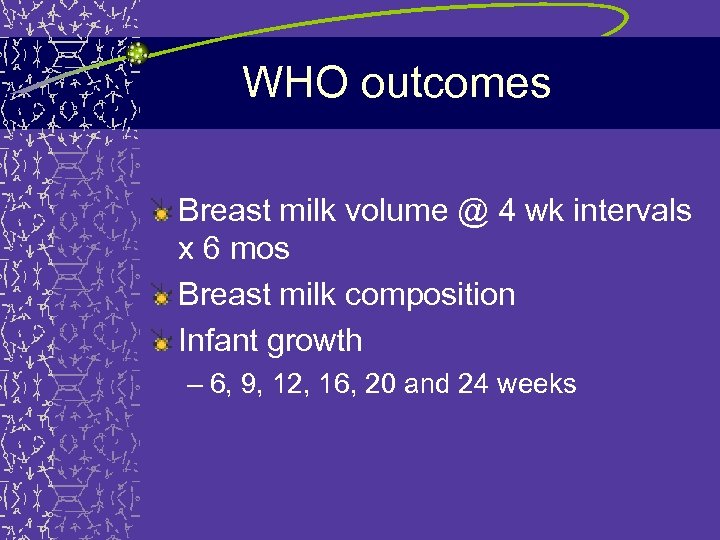
WHO outcomes Breast milk volume @ 4 wk intervals x 6 mos Breast milk composition Infant growth – 6, 9, 12, 16, 20 and 24 weeks
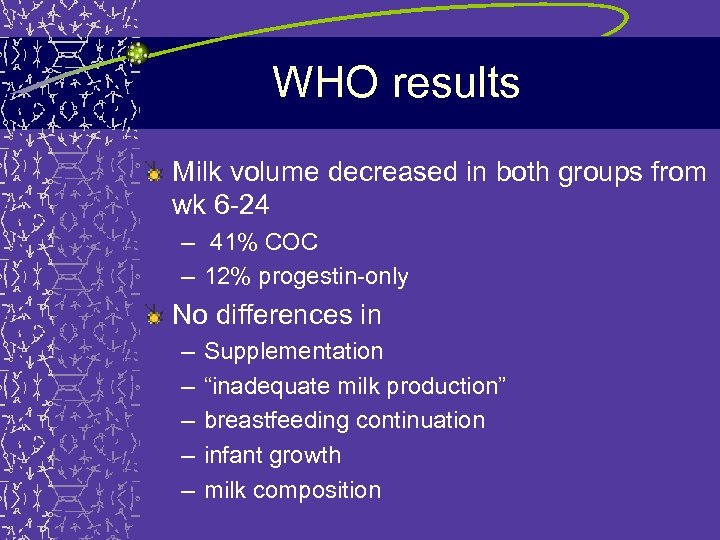
WHO results Milk volume decreased in both groups from wk 6 -24 – 41% COC – 12% progestin-only No differences in – – – Supplementation “inadequate milk production” breastfeeding continuation infant growth milk composition
WHO disclaimer “… our method of measuring milk output… may have little relationship to the amount actually ingested by the baby during that or any other 24 -hour period. ”
WHO conclusions “Combined oral contraceptives cannot be recommended for use during early lactation. The age at which it seems safe to recommend them will be a subject for debate and controversy. ”
2 RCTs: Progestin-only pills 1: Progestin-only vs. placebo 1: Progestin-only vs. progestinonly, timing of start
Velasquez, 1976 N = 20 women Mexico 12 – NET (progestin only) on PP days #1 -14 8 – identically packaged placebos Outcomes – No differences in milk volume, infant growth or milk composition during 14 days of the study
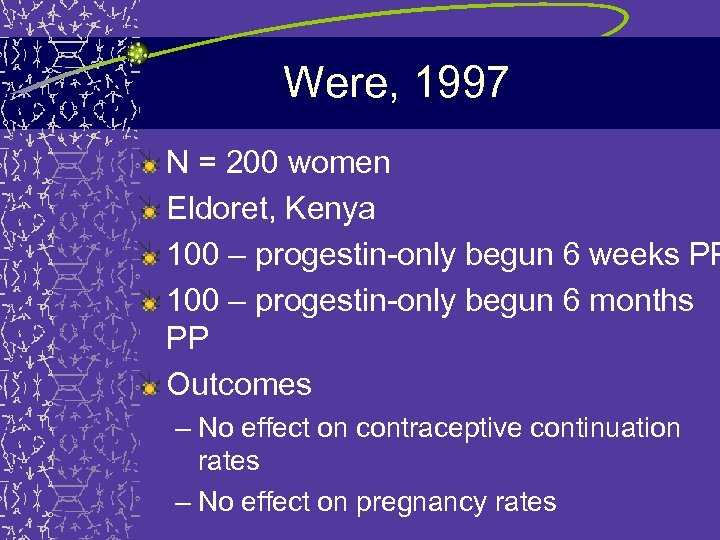
Were, 1997 N = 200 women Eldoret, Kenya 100 – progestin-only begun 6 weeks PP 100 – progestin-only begun 6 months PP Outcomes – No effect on contraceptive continuation rates – No effect on pregnancy rates
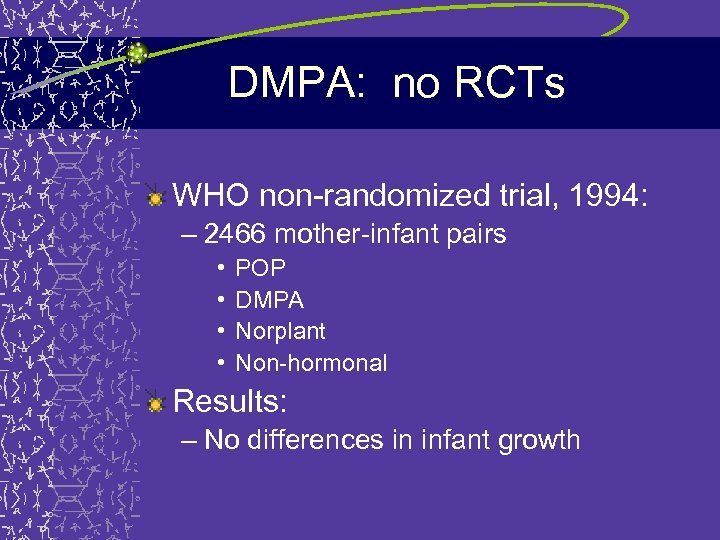
DMPA: no RCTs WHO non-randomized trial, 1994: – 2466 mother-infant pairs • • POP DMPA Norplant Non-hormonal Results: – No differences in infant growth
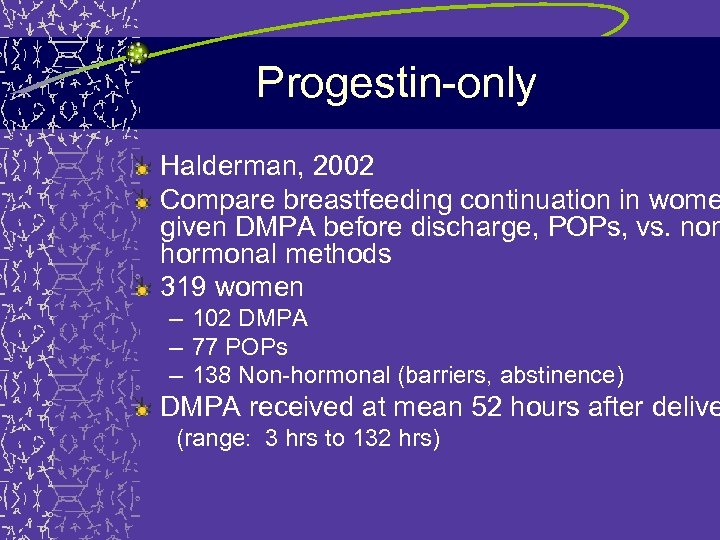
Progestin-only Halderman, 2002 Compare breastfeeding continuation in wome given DMPA before discharge, POPs, vs. non hormonal methods 319 women – 102 DMPA – 77 POPs – 138 Non-hormonal (barriers, abstinence) DMPA received at mean 52 hours after delive (range: 3 hrs to 132 hrs)
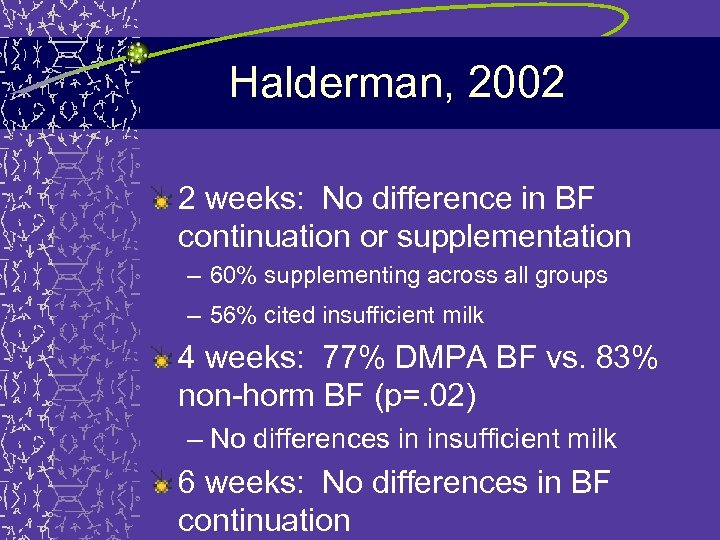
Halderman, 2002 2 weeks: No difference in BF continuation or supplementation – 60% supplementing across all groups – 56% cited insufficient milk 4 weeks: 77% DMPA BF vs. 83% non-horm BF (p=. 02) – No differences in insufficient milk 6 weeks: No differences in BF continuation
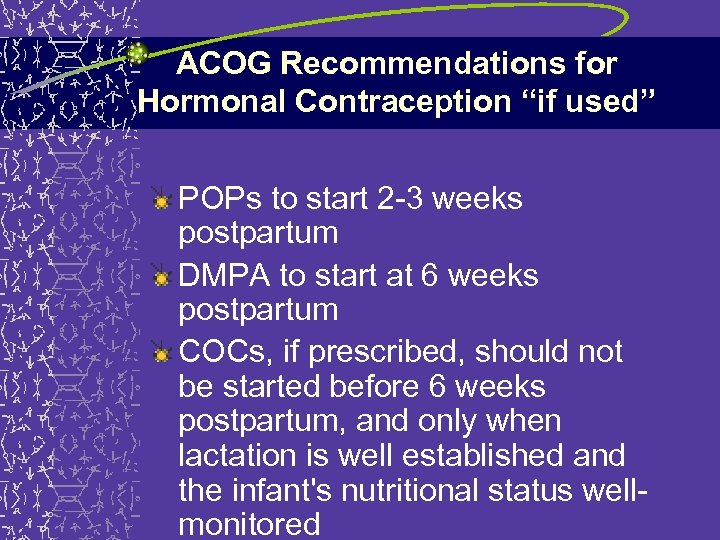
ACOG Recommendations for Hormonal Contraception “if used” POPs to start 2 -3 weeks postpartum DMPA to start at 6 weeks postpartum COCs, if prescribed, should not be started before 6 weeks postpartum, and only when lactation is well established and the infant's nutritional status wellmonitored
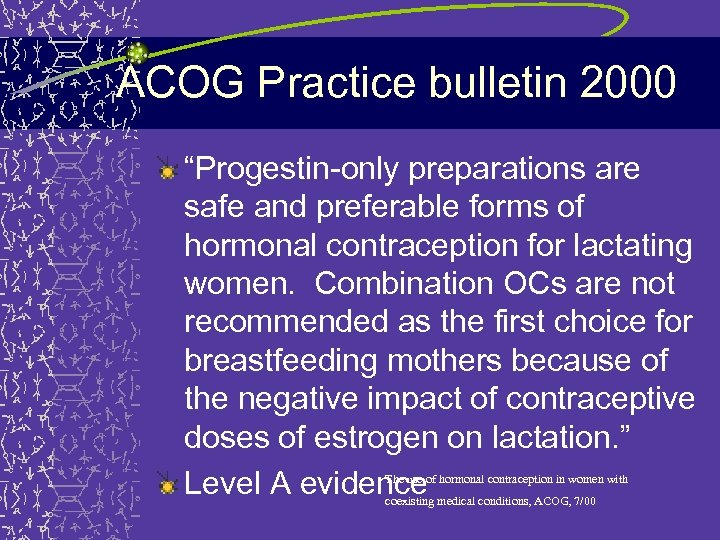
ACOG Practice bulletin 2000 “Progestin-only preparations are safe and preferable forms of hormonal contraception for lactating women. Combination OCs are not recommended as the first choice for breastfeeding mothers because of the negative impact of contraceptive doses of estrogen on lactation. ” Level A evidence The use of hormonal contraception in women with coexisting medical conditions, ACOG, 7/00
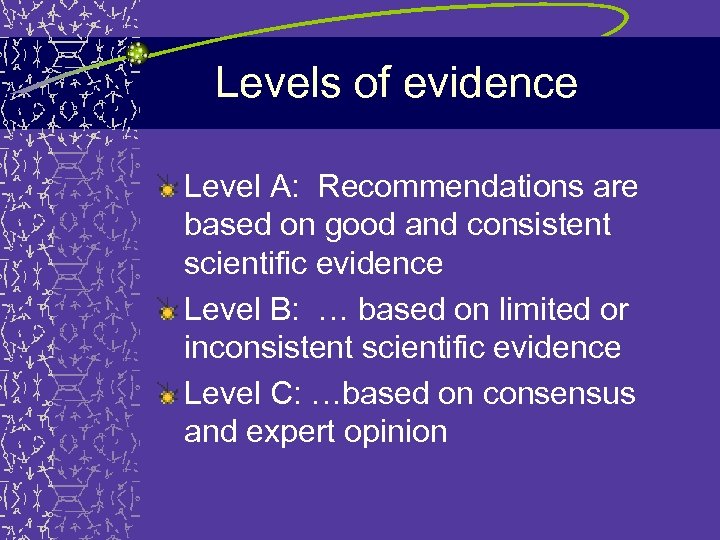
Levels of evidence Level A: Recommendations are based on good and consistent scientific evidence Level B: … based on limited or inconsistent scientific evidence Level C: …based on consensus and expert opinion
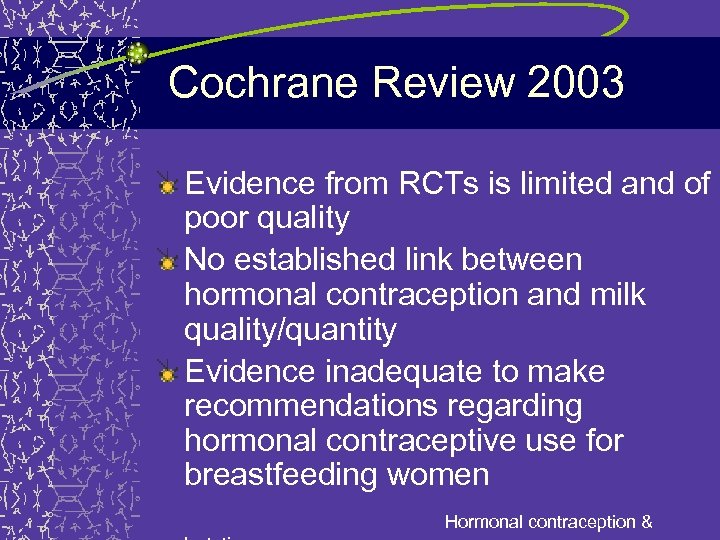
Cochrane Review 2003 Evidence from RCTs is limited and of poor quality No established link between hormonal contraception and milk quality/quantity Evidence inadequate to make recommendations regarding hormonal contraceptive use for breastfeeding women Hormonal contraception &
What do providers prescribe? Single study – Rochat 1981 – Survey: 3697 doctors in 72 countries – 831 responses - 22% response rate – 45% ever prescribed COCs for BF women – Woman’s preference – Previous BF history – International Planned Parenthood guidelines
Survey of New Mexico OB-GYNs and CNMs Questions – Prescribing practices – Attitudes about OCs for BFing women – Knowledge questions
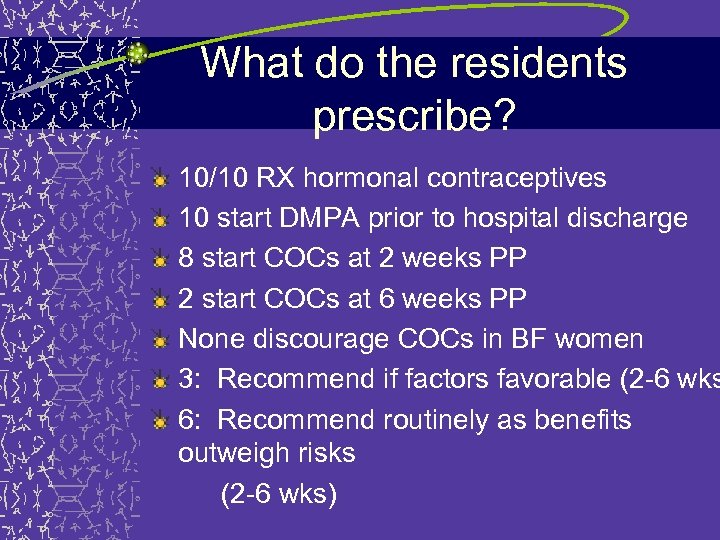
What do the residents prescribe? 10/10 RX hormonal contraceptives 10 start DMPA prior to hospital discharge 8 start COCs at 2 weeks PP 2 start COCs at 6 weeks PP None discourage COCs in BF women 3: Recommend if factors favorable (2 -6 wks 6: Recommend routinely as benefits outweigh risks (2 -6 wks)
RCT: Choice of OC for BF postpartum women Women to be randomized to POPs vs. COCs Double-blind RCT (pills packaged identically) Begin at 2 weeks PP – Outcome measures: • Breastfeeding continuation at 2 months PP • Infant weight • Method continuation
Successful breastfeeding
e93a6b480e99bdccb5eed106fbbd37eb.ppt