eb74fe67e3576374fad524f5df33b5ad.ppt
- Количество слайдов: 47
Biliary Atresia By Eric Pang
Case JRM w CC: Hyperbilirubinemia w HPI n 12 day old M w/ elevated indirect bilirubin now w/ decreasing indirect bili but rising direct bili and elevated GGT
H&P cont…. w Allergies: none w Meds: none w Birth Hx: n n n 1 wk premature 8 lbs 15 oz Feeding well w Surgical Hx: none w Family Hx: none w PE: n n 59 th percentile weight 17 th percentile height Markedly icteric sclera Yellow stools
H&P cont…. w Labs: n n WBC: 13. 2 Alk Phos: 203 ALT and AST: 1137 Total Bilirubin: 16. 3 w Imaging: n U/S is normal except for horseshoe kidney w At this time examination was suspicious for biliary atresia but decision was made to f/u w/ hepatology in 1 wk
1 week later… w Condition was unchanged w Labs were similar: n n n Conjugated bilirubin 4 Unconjugated bilirubin 10. 5 Repeat U/S: l “no clear evidence of gallbladder or extrahepatic bile ducts” w Plan: HIDA and liver biopsy 1 wk later
1 week later w Liver Biopsy Report: n Microscopic. Description H&E-stained sections show liver with well-sampled portal tracts. The tracts are expanded, with central fibrous areas containing portal veins and hepatic arteries and looser connective tissue around the periphery containing prominent ductular proliferation. There is mild pericholangitis as well as admixed inflammation with lymphocytes and occasional eosinophils. There is bile duct plugging as well as intracanalicular and intrahepatic cholestasis
Patient HIDA scan
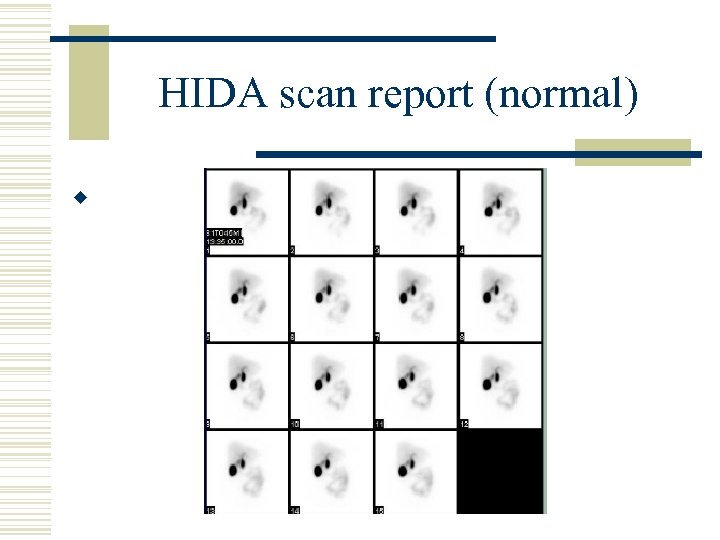
HIDA scan report (normal) w
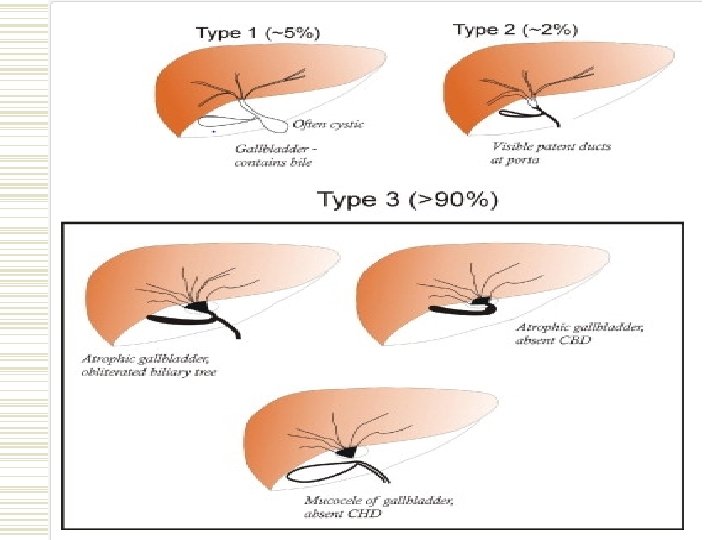
Biliary Atresia w An occlusive panductular cholangiopathy affecting both intra and extrahepatic bile ducts w Commonly classified into 3 types n n Types 1 and 2 w/ some preservation of structures Type 3 is the most common w/ grossly abnormal bile ducts
Biliary Atresia Splenic Malformation Syndrome w Known association of polysplenia w/ biliary atresia n n Found to have etiologic relationship w/ maternal diabetes Often w/ other anomalies (ie – absent IVC, situs inversus) w Theoretically due to a common embryologic insult vs. a genetic defect
BA Diagnosis w Key Features n n Conjugated jaundice persisting beyond 14 days of age Initially appear healthy but will eventually develop failure to thrive 2/2 to malabsorption of fat (and subsequently vit A, D, E, and K) U/S is useful to r/o other possible diagnosis Liver biopsy/ERCP/laparoscopy have utility as well
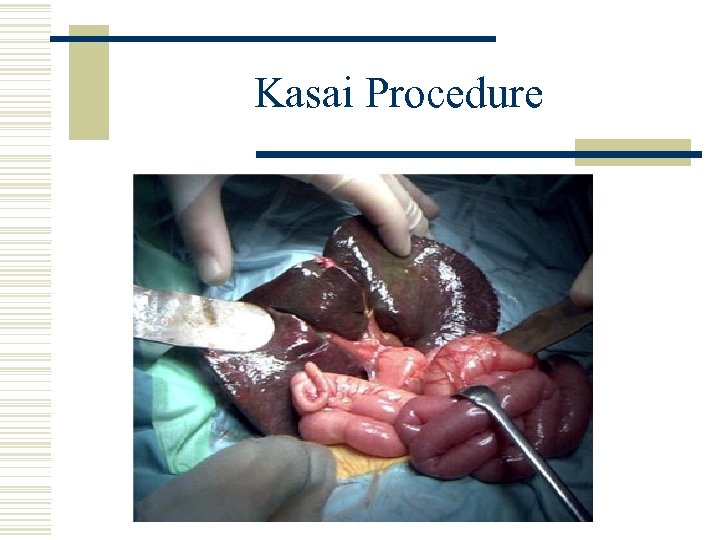
Kasai Procedure
Kasai Portoenerostomy w Briefly: n n Involves resection of gallbladder and extrahepatic biliary tree exposing the porta hepatitis Construction of a large portoenterostomy encompassing the margins of the resection
Pt taken to the OR for Kasai w/ Dr. Healey w FINDINGS: Liver felt rubbery and dense, but not fibrotic. It was mildly cholestatic. There was a streak gallbladder which, when transected, had an obliterated lumen. We were unable to do a cholangiogram due to the lack of lumen. There was atresia of the entire extrahepatic biliary tree with no recognizable biliary structures in the area of the common bile duct or extrahepatic ducts. At the portal plate, however, there was some bile seen in the area of the right biliary remnant.
Adjuvant therapy postoperatively w There isn’t a strong body of evidence supporting benefits from adjuvant drug therapies but 2 classes of drugs are widely used nonetheless n Steroids and ursodeoxycholic acid
Clinical Question w In patients with biliary atresia who have undergone Kasai procedures, does the adjuvant administration of steroids or ursodeoxycholic acid vs. placebo have benefits in time to liver transplant or clearance of jaundice?
Steroids w In theory, steroids are beneficial in multiple ways n n Anti-inflammatory effect of steroids Increase bile salt independent fraction of bile flow w Have been several studies examining benefit but only one RCT trial…
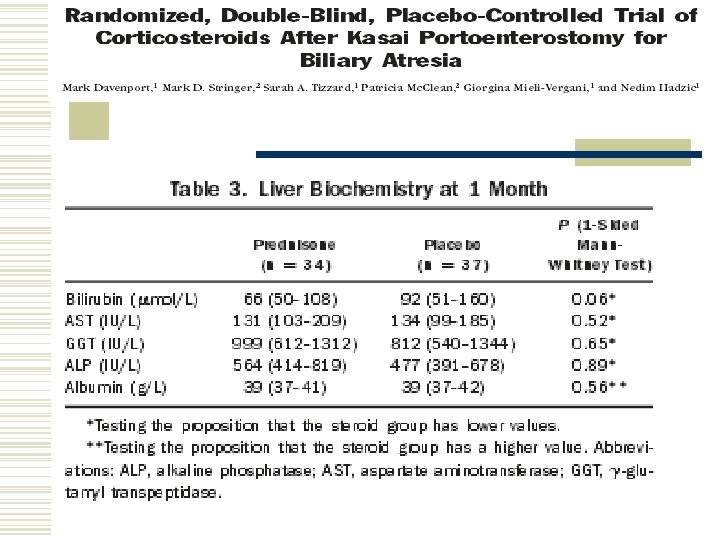
w Prospective 2 center, double blind, randomized, placebo-controlled trial w Published in 2007 in Hepatology out of King’s College London SOM and St. James’ University Hospital w Meant to examine effect of post-Kasai portoenterostomy corticosteroids w/ primary endpoints being clearance of jaundice (tbili < 20 umol/L) and the proportion of infants retaining their native livers at 6 and 12 mo
w Infants w/ type 3 isolated biliary atresia were included in the study w exclusion criteria included those w/ splenic malformation, severe cardiac anomalies, close contact w/ or evidence of infection, cirrhosis, or type 1/2 biliary atresia w operative procedures were performed by 1 of 2 surgeons in a standardized fashion, post operative nutritional schedules, abx administration, and medication administration were scripted as well. w Administered prednisilone 2 mg/kg/day POD 7 -21 and 1 mg/kg/day POD 21 -28. w 73 infants were enrolled (36 to steroids and 37 to placebo group)
w Findings: n n No significant difference for clearance of jaundice at 1, 6, or 12 mo No significant difference for transplantation at 6 or 12 mo
w Subgroup analysis for infants <70 days old at time of surgery showed significantly more clearance of jaundice in pt operated on <70 days of age (64 v 116, P<0. 01) but effect was not sustained at later sampling and there was no significant different in need for subsequent transplantation
w Conclusions: n n Steroids w/out significant benefit as far as achieving normal bilirubin or reducing the need for liver transplant Does reduce bilirubin for younger patients (<70 day old at age of surgery) but only at 1 mo w/out longer term effects
w Areas for improvement: n n n Small N could have underpowered the study Short course of steroids Low dose
w Systematic review and metanalysis published in 2012 in the Canadian Journal of Gastroenterology w Looked at studies between Jan 1969 and June 2010 using Medline, Pub. Med, EMBASE and Cochrane databases
w Out of 16 observational studies only 4 met criteria for inclusion: - - compared 2 groups of infants who underwent Kasai Sufficient data to calculate OR and RR Outcomes included normalization serum bili at 6 mo post op and early liver transplant
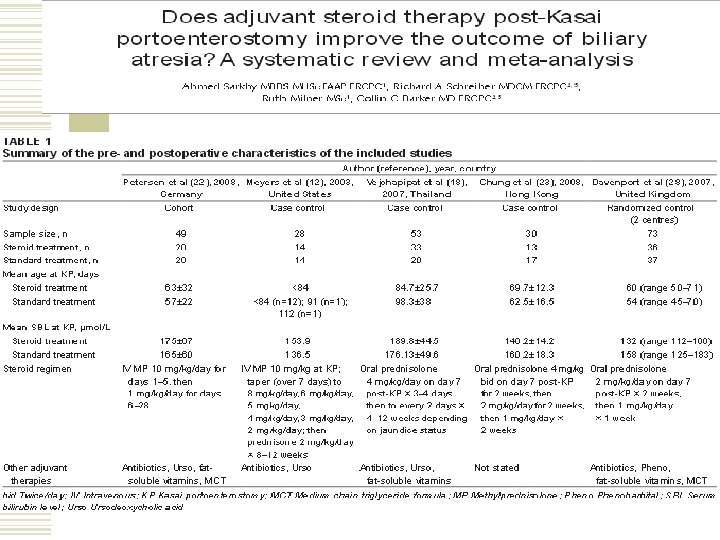
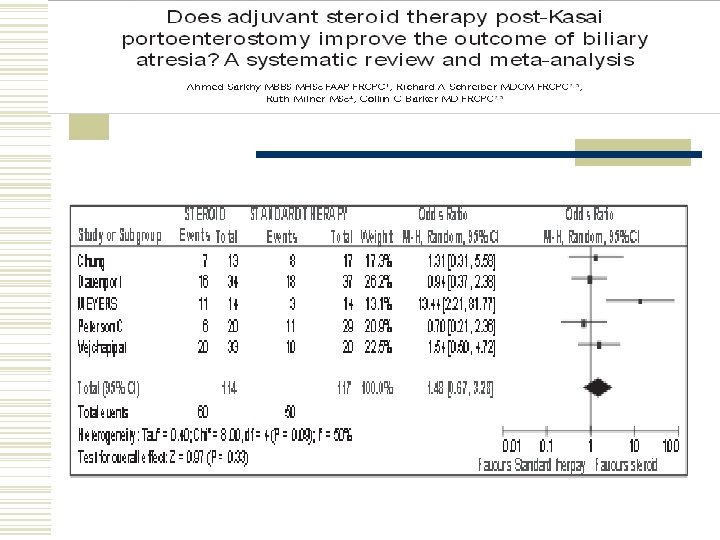
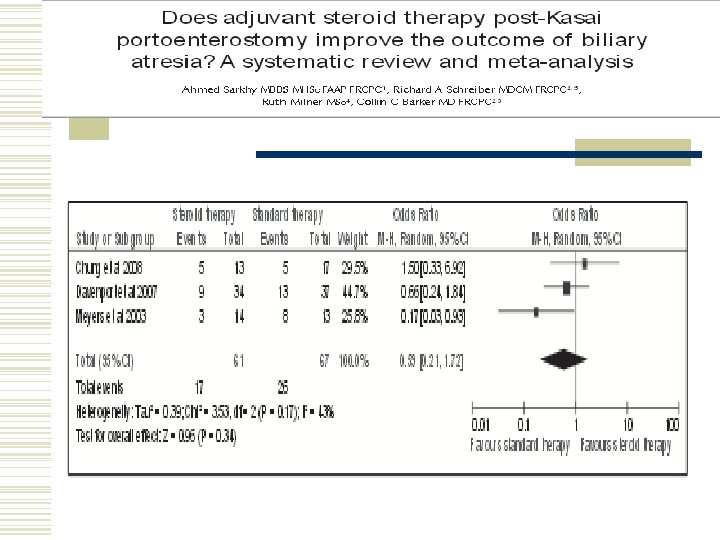
w Results: n n n 160 subjects in observational studies and 73 patients in the single RCT No significant difference for normalization of serum bilirubin at 6 mo Showed some effect in delaying transplant but not statistically significant
w Retrospective study published in 2010 in the American Journal of Surgery out of Seattle Children’s Hospital w Utilized the Pediatric Health Information System which include data from 43 children hospitals n Searched using ICD-9 coding for the Kasai procedure and the diagnosis of biliary atresia w Aimed to look at relationship of postop steroids w/ length of hospital stay
w Identified 516 patients n Of which 46% received perioperative steroids (defined as being w/in 4 days of surgery) w lengths of stay was 14. 5 ± 19. 7 for those who did not receive steroids vs. 11. 3 ± 16. 3 days for those who did receive steroids. w Postoperative steroid use was significantly associated with a 3. 5 -day decrease in postoperative length of stay
w Limitations of study include: n Use of database rely on accurate documentation, no information in database concerning dosages or schedules, labs and subsequent liver transplantation data were not available, could be skewed population w Does suggest that postoperative steroids may be beneficial in terms of time to discharge
Steroids or No Steroids? w Pros n n n Possible benefit in pt w/ Kasai procedures done early Observational studies in the past have suggested benefit in both time to transplant and clearance of jaundice Possible decrease is post operative hospital stay length
Steroids or No Steroids - Cons - Possible side effects No RCT proving benefit
The bottom line for steroids w A large prospective study examining high dose steroid use for postoperative management of biliary atresia patients is necessary w Currently there is a RCT being done sponsored by the National Institute of Diabetes and Digestive and Kidney Diseases which may help elucidate this topic further n n n Treatment dose is 4 mg/kg starting 1 -3 days post op Estimated 140 pts to be enrolled Target date of completion was 1/2013….
Ursodeoxycholic Acid
Ursodeoxycholic Acid w Hydrophilic bile acid w Has shown biochemical, histologic, and clinical benefits in pts w/ primary biliary cirrhosis and sclerosing cholangitis in reducing need for transplant w Theory is that UDCA: n n Decreases concentrations of endogenous toxic bile acids Has an immunomosuppressive property w Has been suggested that UDCA can be beneficial in biliary atresia
w Prospective study published in 2008 in Pediatrics out of Lille University Children’s Hospital in France w Study looked at patients who had undergone successful Kasai procedures and were treated w/ ursodeoxycholic acid for atleast 18 mo n n Successful surgery was defined as the clearance jaundice 6 mo post operatively Note: no pt’s received steroids
w Study prospectively followed 16 pt who had completed at least 1 yrs of UDCA treatment n n Pt’s had UDCA dc’d when clinically deemed ready by physician and were observed for changes in clinical condition and labs. Median treatment time at time of initial d/c was 2. 6 years w Labs were drawn at time of d/c and then again at time of reexamination at 6 mo n If labs had worsened (>2 x the upper limit of normal) then they were restarted on UDCA
w Of the 16 patients: n n Only 1 pt developed jaundice 3 mo post d/c w/ an elevation of his bili from 10 to 57 umol/L 13 of the pt’s had elevated LFT’s (AST/ALT/GGT) and were restarted on UDCA l 6 mo after restarted LFT’s were redrawn and showed statistically significant improvement at that time
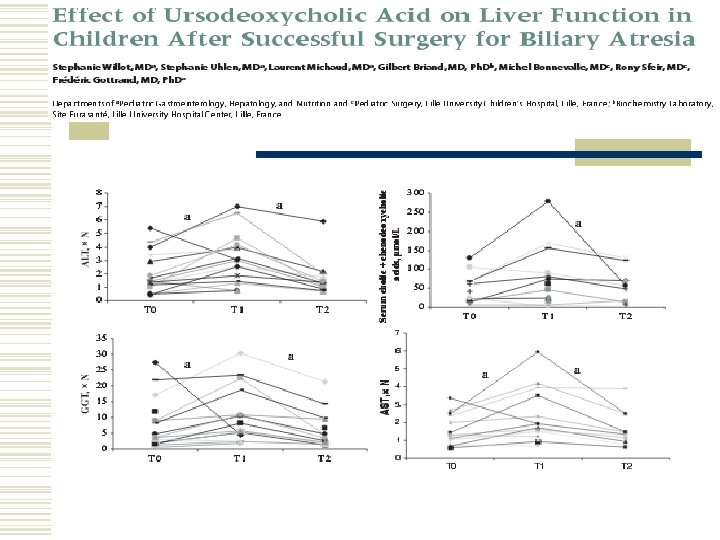
w Weaknesses: n n n No control group Only 1 pt w/ clinical change 2/2 to therapy Did not assess histology of liver w Findings suggest UDCA therapy can have long term benefits
UDCA vs No UDCA? w Pros n n Evidence supporting utility in diminishing jaundice Few side effects and generally tolerated well l H/a, weight gain, constipation, diarrhea w Cons n Cost l n For 100 capsules ($270 -$770) Clinical vs. Lab value benefits? w Again, more studies required for more definitive proof going forward.
Case JRM w Operation was completed without complication w Currently continuing to recover from operation n LFT’s normalizing On Bactrim/Ursodiol/Vitamin supplementation Advancing PO + NG feeds until goal is reached w Hopefully going home soon…
Works Cited w w w Davenport, Mark. "Biliary Atresia: Clinical Aspects. " Seminars in Pediatric Surgery 21 (2012): 175 -84. Elsevier. Web. 05 July 2013. http: //www. sciencedirect. com. offcampus. lib. washington. edu/science/article/pii/S 1055858612000352. Davenport, Mark D. Stringer, Sarah A. Tizzard, Patricia Mc. Clean, Giorgina Mieli-Vergani, and Nedim Hadzie. "Randomized, Double-Blind, Placebo-Controlled Trial of Corticosteroids After Kasai Portoenterostomy for Biliary Atresia. " Hepatology 46. 6 (2007): 1821 -827. Wiley Inter. Science. Web. 5 July 2013. http: //onlinelibrary. wiley. com/doi/10. 1002/hep. 21873/abstract; jsessionid=58145 B 6 DD 9132 BD 462894 F C 468 A 025 EA. d 03 t 03. Lao, Oliver B. , Cindy Larison, Michele Garrisson, Patrick J. Healey, and Adam B. Goldin. "Steroid Use after the Kasai Procedure for Biliary Atresia. " The American Journal of Surgery 199. 5 (2010): 680 -84. Elsevier. Web. 5 July 2013. Sarkhy, Ahmed, Richard A. Schreiber, Ruth Milner, and Collin C. Barker. "Does Adjuvant Steroid Therapy Post-Kasai Portoenterostomy Improve the Outcome of Biliary Atresia? A Systematic Review and Meta-analysis. " Canadian Journal of Gastroenterology 25. 8 (2011): 440 -44. Pulsus Group Inc. Web. 5 July 2013. <http: //www. ncbi. nlm. nih. gov/pmc/articles/PMC 3186729/> Willot, Stephanie Uhlen, Laurent Michaud, Gilbert Briand, Michel Bonnevalle, Rony Sfeir, and Frederic Gottrand. "Effect of Ursodeoxycholic Acid on Liver Function in Children After Successful Surgery for Biliary Atresia. " Pediatrics 122. 6 (2008). Pediatrics. Web. 05 July 2013. http: //pediatrics. aappublications. org/content/122/6/e 1236. long
eb74fe67e3576374fad524f5df33b5ad.ppt