e0b48125e38baa83b5ff1ce3605aa7df.ppt
- Количество слайдов: 33

BIDMC Emergency Department Check-out and Copay Collection Presented by: Ambulatory Education & Systems Team Final 4/4/05 1
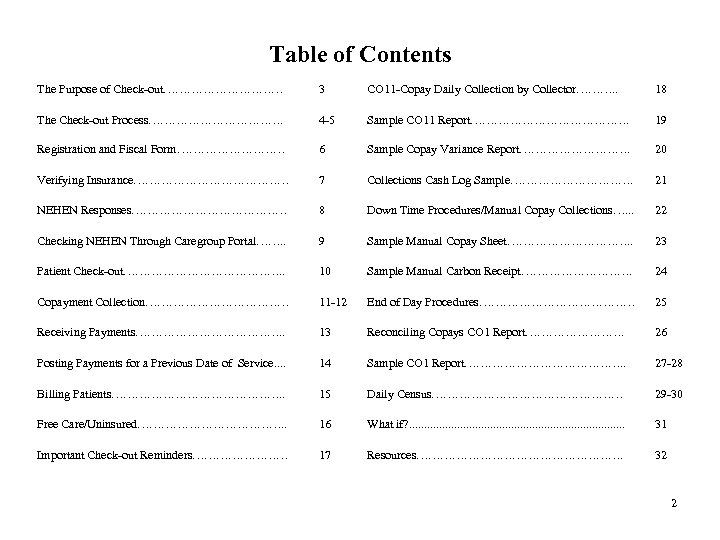
Table of Contents The Purpose of Check-out…………… 3 CO 11 -Copay Daily Collection by Collector………. . 18 The Check-out Process………………. 4 -5 Sample CO 11 Report…………………. 19 Registration and Fiscal Form…………… 6 Sample Copay Variance Report……………. 20 Verifying Insurance………………… 7 Collections Cash Log Sample……………. 21 NEHEN Responses………………… 8 Down Time Procedures/Manual Copay Collections…. . . 22 Checking NEHEN Through Caregroup Portal……. . 9 Sample Manual Copay Sheet……………. . 23 Patient Check-out…………………. . 10 Sample Manual Carbon Receipt……………. 24 Copayment Collection……………… 11 -12 End of Day Procedures………………… 25 Receiving Payments………………. . 13 Reconciling Copays CO 1 Report…………. 26 Posting Payments for a Previous Date of Service. . 14 Sample CO 1 Report…………………. . 27 -28 Billing Patients…………………. . 15 Daily Census…………………… 29 -30 Free Care/Uninsured………………. . 16 What if? . . . . 31 Important Check-out Reminders………… 17 Resources………………………. 32 2
The Purpose of Check-out is an important part of the Emergency Department discharge process. The Check-out process is in place for verifying eligibility and collecting co-payments or Self Pay payments for all patients being discharged home from the ED. All components of the Check-out process are critical to ensure that patient visits are billed accurately. A Registration Specialist will be assigned to the Check out process during the hours of 9 a-10 p (or as staffing permits) Part I Verify Demographic/Fiscal When verifying demographics and insurance, please confirm/ obtain: § Patient Name/Social Security number/Address/Phone number § Primary Care Physician § Next of Kin § Marital Status § Employment Status/Employer Part II Verify Insurance Eligibility Staff should confirm insurance eligibility for the visit to the ED § Verify insurance eligibility through the online NEHEN system (review PDS) or by calling Insurance company directly if it is a Commercial Insurance § Benefit level/Plan Type (HMO, PPO, etc. ) § Insurance Start Date/Eligibility Date § Verify Emergency Room co-pay amount Part III Collect Co-pay/Other Payment (If applicable) Staff should confirm if co-pay is applicable to that days Emergency Department Visit § Collect co-pay amount if applicable to visit 3
The Check-Out Process • While covering Check Out, you will be wearing a pager that will be connected to our ED computer system. You will be paged each time a patient is being discharged. When you are paged, the expectation is that you would either go to the room and escort the patient to the check out office or meet the patient at the check out office. *Please note: if you are in the middle of registering another patient, you have time to complete that task…and it is okay to ask your co-worker for help! Script: When paged regarding a discharged patient: • A. ) If you collect the patient from the exam room – “Hello, my name is _____. I understand that you are being discharged. Have you received your Discharge Instructions? (If not, ask the nurse/doctor for them) Please come with me and we will confirm your registration information and complete your discharge process. ” • B. ) If you meet the patient at the check out office – “Hello, my name is _____. I understand that you are being discharged. Have you received your Discharge Instructions? (If not, page the nurse/doctor for them) Please have a seat so that we can confirm your registration information and complete your discharge process. ” • You will have a key to the check out office and locked drawer. Place your cash bag in the locked drawer when not in use during your shift. The Cash Box will also be contained in the locked drawer. • Cash Box- This box will contain $100 cash and should be used to make change for patients. This money remains in the cash box and payments you collect will go into your cash bag: • At the beginning of your shift you will verify that the cash box contains a beginning balance of $100. • At the end of your shift you will verify that the cash box contains an ending balance of $100 • You will complete the “Collections Cash Log” at the beginning and end of your shift to to verify the balance in the 4 cash box ($100). Two signatures are required to verify this.
The Check-out Process • Throughout each shift, Patient Data Sheets (PDS) will be printing out at the checkout office printer. The PDS forms should be filed in the Alpha Accordion file. As patients are discharged and walked or sent to the Checkout office, the Registration Specialist should match the PDS sheet to the discharge sheet (matching the name and BIDMC# to the discharge instructions) given to patient by nurse or doctor. The patients insurance, co-pay information and NEHEN eligibility response (if applicable) will be printed on the PDS sheet. • Re-verify the patients information(via the “e”dit function in CCC). When going through the “edit” function don’t forget to go through all 3 forms…. (Reg, Fiscal and EW) • After reviewing the patients information, you will move on to the “Check Out Enter/Edit” function (“che”). Collect Copayment or Other Payments as appropriate. Stamp PDS with “OK” stamp. • At the end of your shift(the last 20 minutes), you will need to print the CO 11 report and reconcile your collections. If there any discrepancies, you will need to either correct it in CCC (via the Cke Out option (if data entry error), or complete a Variance Report. Once you have reconciled your collections put all receipts and monies (cash, check and credit card receipts) in an envelope (with your name and date) and drop it in the safe. Place your empty cash bag in the cabinet above the desk in the Check Out office. Complete Cash Box reconciliation as described on page 4. The keys to the check out office and cash box are on the same key ring. The keys and check out pager should be handed off between shifts. At the end of the day, the last Registration Specialist covering the check out office should put the pager and the keys in the cash bag marked “CHECK OUT” and return it to the Supply Pyxis in the Green/Purple supply closet. In the morning, the first person to cover the check out office (or the Practice Manager, lead or designated staff reconciling the collections) will retrieve the CHECK OUT cash bag from the Green/Purple Supply Pyxis. Please note: each Registration Specialist has their own login and password for the Green/Purple Pyxis. 5
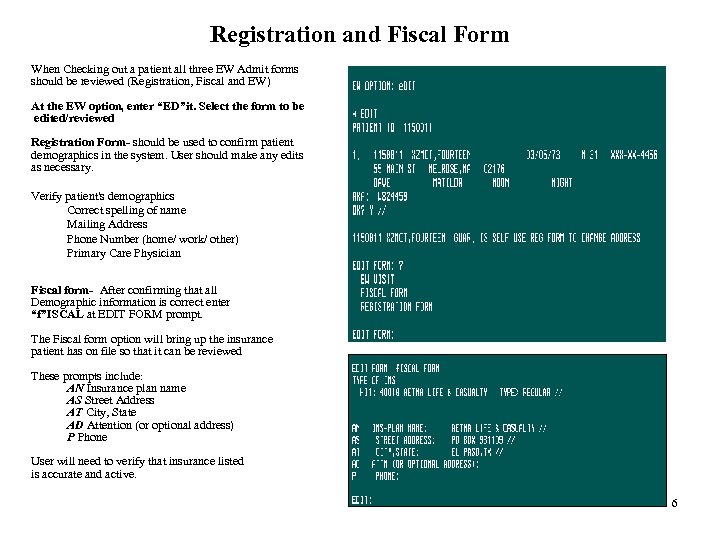
Registration and Fiscal Form When Checking out a patient all three EW Admit forms should be reviewed (Registration, Fiscal and EW) At the EW option, enter “ED”it. Select the form to be edited/reviewed Registration Form- should be used to confirm patient demographics in the system. User should make any edits as necessary. Verify patient's demographics Correct spelling of name Mailing Address Phone Number (home/ work/ other) Primary Care Physician Fiscal form- After confirming that all Demographic information is correct enter “f”ISCAL at EDIT FORM prompt. The Fiscal form option will bring up the insurance patient has on file so that it can be reviewed These prompts include: AN Insurance plan name AS Street Address AT City, State AD Attention (or optional address) P Phone User will need to verify that insurance listed is accurate and active. 6
Verifying Insurance NEHEN is an on-line insurance verification tool that is integrated with CCC and is used to verify insurance eligibility for the following payers: Tufts (including Secure Horizons) Harvard Pilgrim (including First Seniority) Blue Cross Medicare Medicaid NHP (Neighborhood Health Plan) Eligibility information should print out on the bottom of the PDS that comes through the printer in the Check-out office. § Match the information in CCC with the eligibility information provided at the bottom of the PDS. § If there any inconsistencies between CCC and NEHEN eligibility information, update CCC appropriately via the EW/Edit option. § Use NEHEN stand alone option available at the EW prompt to re-check eligibility if needed Please review the Mini Reg/Update Mini Reg Manual for instructions on reviewing and interpreting NEHEN eligibility responses. 7
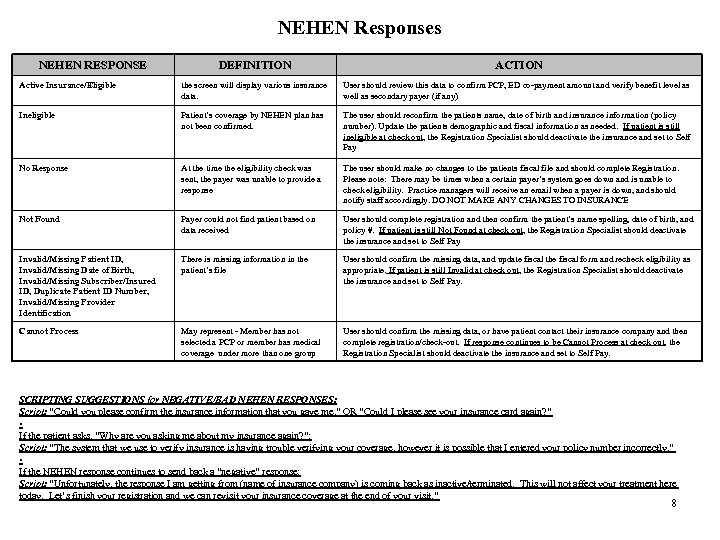
NEHEN Responses NEHEN RESPONSE DEFINITION ACTION Active Insurance/Eligible the screen will display various insurance data. User should review this data to confirm PCP, ED co-payment amount and verify benefit level as well as secondary payer (if any) Ineligible Patient’s coverage by NEHEN plan has not been confirmed. The user should reconfirm the patients name, date of birth and insurance information (policy number). Update the patients demographic and fiscal information as needed. If patient is still ineligible at check out, the Registration Specialist should deactivate the insurance and set to Self Pay No Response At the time the eligibility check was sent, the payer was unable to provide a response The user should make no changes to the patients fiscal file and should complete Registration. Please note: There may be times when a certain payer’s system goes down and is unable to check eligibility. Practice managers will receive an email when a payer is down, and should notify staff accordingly. DO NOT MAKE ANY CHANGES TO INSURANCE Not Found Payer could not find patient based on data received User should complete registration and then confirm the patient’s name spelling, date of birth, and policy #. If patient is still Not Found at check out, the Registration Specialist should deactivate the insurance and set to Self Pay Invalid/Missing Patient ID, Invalid/Missing Date of Birth, Invalid/Missing Subscriber/Insured ID, Duplicate Patient ID Number, Invalid/Missing Provider Identification There is missing information in the patient’s file User should confirm the missing data, and update fiscal the fiscal form and recheck eligibility as appropriate. If patient is still Invalid at check out, the Registration Specialist should deactivate the insurance and set to Self Pay. Cannot Process May represent - Member has not selected a PCP or member has medical coverage under more than one group User should confirm the missing data, or have patient contact their insurance company and then complete registration/check-out. If response continues to be Cannot Process at check out, the Registration Specialist should deactivate the insurance and set to Self Pay. SCRIPTING SUGGESTIONS for NEGATIVE/BAD NEHEN RESPONSES: Script: “Could you please confirm the insurance information that you gave me. ” OR “Could I please see your insurance card again? ” • If the patient asks, “Why are you asking me about my insurance again? ”: Script: “The system that we use to verify insurance is having trouble verifying your coverage, however it is possible that I entered your policy number incorrectly. ” • If the NEHEN response continues to send back a “negative” response: Script: “Unfortunately, the response I am getting from (name of insurance company) is coming back as inactive/terminated. This will not affect your treatment here today. Let’s finish your registration and we can revisit your insurance coverage at the end of your visit. ” 8
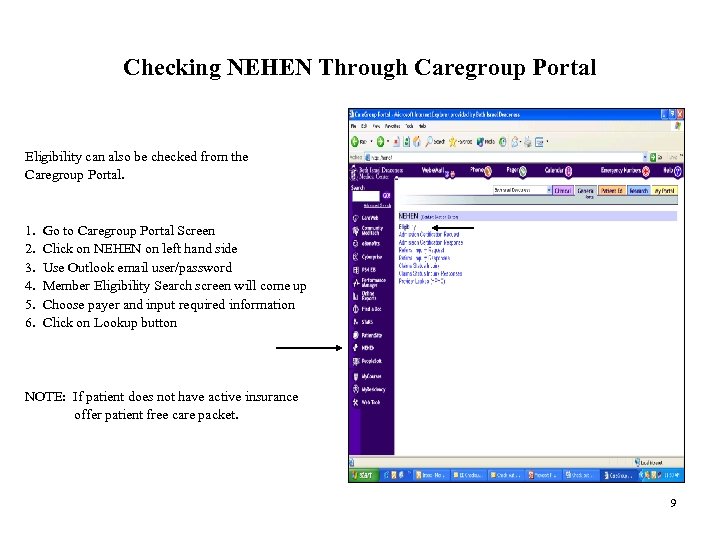
Checking NEHEN Through Caregroup Portal Eligibility can also be checked from the Caregroup Portal. 1. Go to Caregroup Portal Screen 2. Click on NEHEN on left hand side 3. Use Outlook email user/password 4. Member Eligibility Search screen will come up 5. Choose payer and input required information 6. Click on Lookup button NOTE: If patient does not have active insurance offer patient free care packet. 9
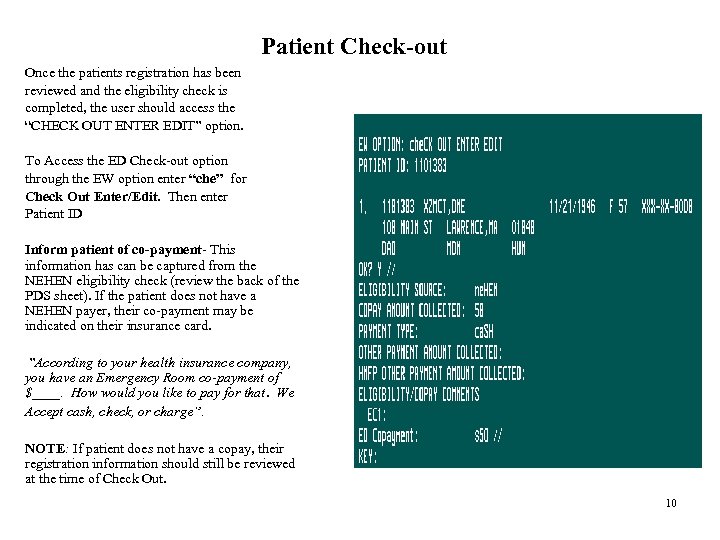
Patient Check-out Once the patients registration has been reviewed and the eligibility check is completed, the user should access the “CHECK OUT ENTER EDIT” option. To Access the ED Check-out option through the EW option enter “che” for Check Out Enter/Edit. Then enter Patient ID Inform patient of co-payment- This information has can be captured from the NEHEN eligibility check (review the back of the PDS sheet). If the patient does not have a NEHEN payer, their co-payment may be indicated on their insurance card. ”According to your health insurance company, you have an Emergency Room co-payment of $____. How would you like to pay for that. We Accept cash, check, or charge”. NOTE: If patient does not have a copay, their registration information should still be reviewed at the time of Check Out. 10
Copayment Collection Co-payments are a form of cost sharing between the managed care plan and patient, in which the managed care patient makes a small payment to the provider at the time of service. • Our goal is to collect 100% of co-payments at the time of service. • Co-payment amounts are usually located on the patient's insurance card and in the NEHEN response. Staff should request the card at each visit in order to confirm insurance and co-payment amount. • Patients with Medicaid do NOT pay a copay. • Patients are expected to pay their co-payments at the time of service. • The likelihood of collecting payments significantly decreases as time goes by. Copay Supplies: Order From Office Depot: Locking Security Bag - Item no. 538 -777 Locking Cash Box - Item no. 398 -750 POS devices are ordered directly from Blue Cross-Provider Technology Unit. • The main customer service # is 800 -451 -8123. Request From Ambulatory Administration (Lynne Brophy): BIDMC Stamp Co-pay signage Request from Patient Financial Services, Cash Processing Dept (Vicky Favis or Beth O’Toole • Pre Printed Manual Receipts 11
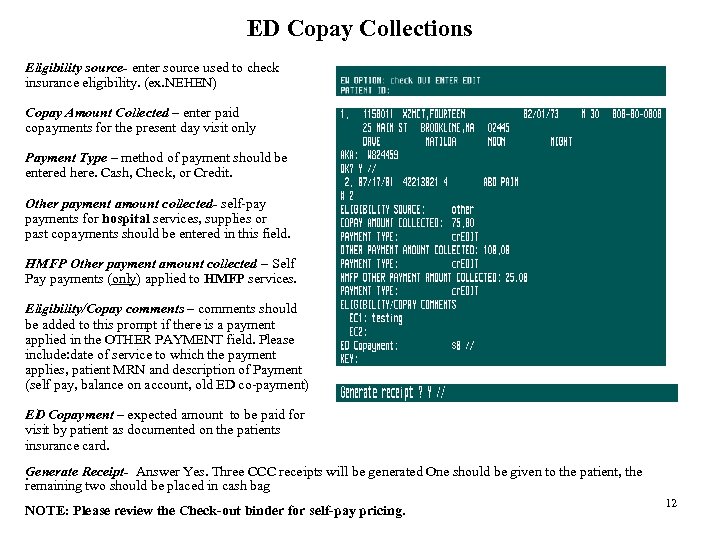
ED Copay Collections Eligibility source- enter source used to check insurance eligibility. (ex. NEHEN) Copay Amount Collected – enter paid copayments for the present day visit only Payment Type – method of payment should be entered here. Cash, Check, or Credit. Other payment amount collected- self-pay payments for hospital services, supplies or past copayments should be entered in this field. HMFP Other payment amount collected – Self Pay payments (only) applied to HMFP services. Eligibility/Copay comments – comments should be added to this prompt if there is a payment applied in the OTHER PAYMENT field. Please include: date of service to which the payment applies, patient MRN and description of Payment (self pay, balance on account, old ED co-payment) ED Copayment – expected amount to be paid for visit by patient as documented on the patients insurance card. Generate Receipt- Answer Yes. Three CCC receipts will be generated One should be given to the patient, the . remaining two should be placed in cash bag NOTE: Please review the Check-out binder for self-pay pricing. 12
Receiving Payments Processing Credit Card Payments: There are 2 machines: labeled HMFP and Hospital § Co-payments should be run through the HOSPITAL credit card machine!! § Take credit card from patient § Swipe card through machine, enter payment amount then press enter. § Take first copy of receipt from machine and give to patient to sign § Give patient second copy printed from machine and copy of BIDMC receipt generated from CCC. § Paperclip the remaining 2 system generated receipts to the signed credit card slip and place in your cash bag, § HMFP (physician) machine will also need to be used when patients is self-pay. You will be processing 2 credit card payments! (See Self Pay pricing in Check Out Binder) § HMFP Credit Card Machine ONLY: Enter patient Medical Record number when the machine prompts for Invoice # Processing Check/ Cash Payments: If payment is by check: § If the patient is paying a co-payment or hospital portion of a self payment make check out to BIDMC § HMFP money may also be collected (Self Payments ONLY). Ask patient to write a separate check made out to HMFP § Write patient’s Medical Record Number on check § Give patient copy of system generated receipt § Paperclip the remaining 2 receipts to the payment and place in your cash bag, If Payment is by cash: § Collect cash and make change if necessary from the cash box § Give patient copy of system generated receipt § Paperclip the remaining 2 receipts to the payment and place in your cash bag, 13
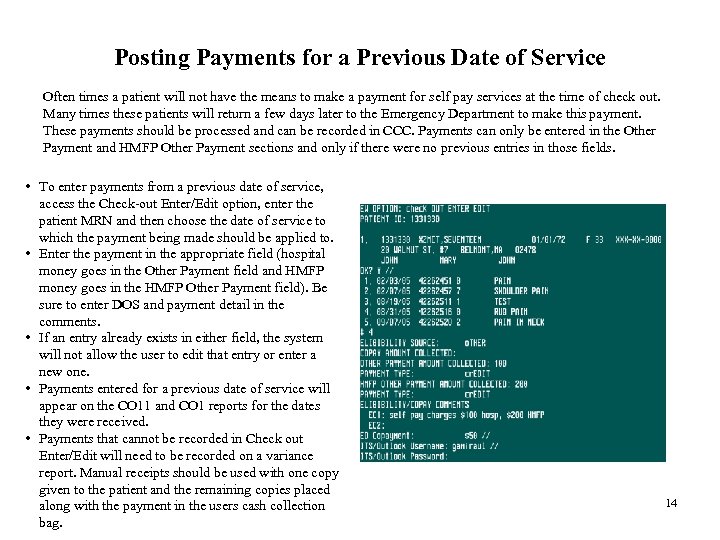
Posting Payments for a Previous Date of Service Often times a patient will not have the means to make a payment for self pay services at the time of check out. Many times these patients will return a few days later to the Emergency Department to make this payment. These payments should be processed and can be recorded in CCC. Payments can only be entered in the Other Payment and HMFP Other Payment sections and only if there were no previous entries in those fields. • To enter payments from a previous date of service, access the Check-out Enter/Edit option, enter the patient MRN and then choose the date of service to which the payment being made should be applied to. • Enter the payment in the appropriate field (hospital money goes in the Other Payment field and HMFP money goes in the HMFP Other Payment field). Be sure to enter DOS and payment detail in the comments. • If an entry already exists in either field, the system will not allow the user to edit that entry or enter a new one. • Payments entered for a previous date of service will appear on the CO 11 and CO 1 reports for the dates they were received. • Payments that cannot be recorded in Check out Enter/Edit will need to be recorded on a variance report. Manual receipts should be used with one copy given to the patient and the remaining copies placed along with the payment in the users cash collection bag. 14
Billing Patients Processing Patients who request to be billed: § § Go into CCC/ EW/ Edit In comments under the fiscal section enter: Bill patient, your initials, date 15
Free Care/Uninsured • For patients 65 and older please provide them with an application for free care and information sheet regarding 2005 changes to the Free Care application process. • For patients under 65 please provide them with the MBR (Medical Benefit Request) packet and information sheet regarding 2005 changes to the Free Care application process. (Please do not provide them with a free care application). • Important note: In both cases the patient will be referred to the Financial Counseling Office. 16
Important Check-Out Reminders • Worker’s Comp and Auto/Liability do NOT require a co-pay. If the patient does not have all the required billing information the visit specific insurance should be set to self-pay. Be sure the patient has been given a copy of the Information Worksheet • RCI (Rape Crisis Intervention)- do NOT collect co-pay for RCI patients. Guarantor and Incident Specific Guarantor should be: • Michelle Leone • P. O. Box 15675 • Boston, MA 02215 • For a follow-up ED visit (example: suture removal) do NOT collect co-pay as long as the original copayment was received. If we did not collect the original payment, then the patient should pay the co-pay amount during their follow-up visit (“other payment” prompt). • Make sure patient gets a receipt for their payment • When Check Out has been completed stamp “OK” on the PDS sheets and place in the OK folder. The “OK” stamp indicates that a Registration Specialist has ‘checked-out’ the patient. 17
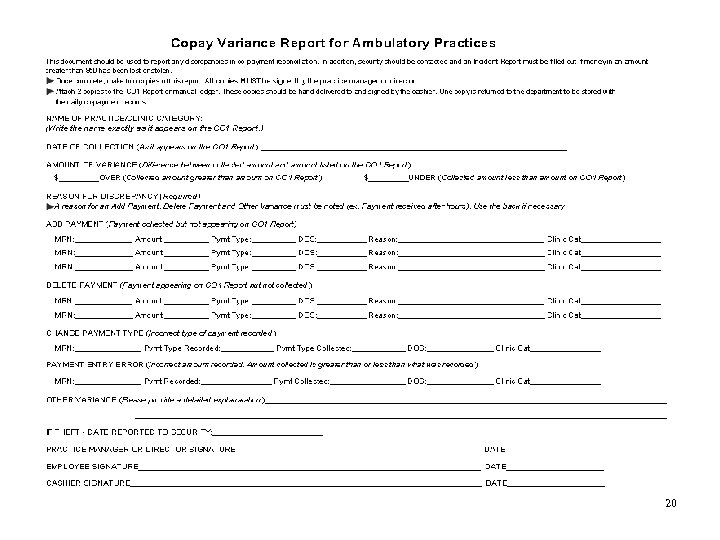
CO 11 – Co-pay Daily collection by Collector At the end of your shift, print the “CO 11” “Detail by Collector” report. This report prints a list of all payments collected by each individual staff member in the department that day. § § § Highlight the section of the report with your name on it. Count the money you have collected and make sure that the total on the report equals the total in your cash bag. If this does not match review your receipts to locate error. Edit Payment field in the Check Out Enter/Edit option as needed. If changes are made be sure to reprint the receipt and attach to old receipt. Place the money from your cash bag with the CO 11 report in an envelope, write the date and your name on the envelope and drop in the safe. . If the money collected does not match the amount indicated on the report you must complete a variance report (page 19). This variance report must accompany the CO 11 report and deposit. (note: clinic category = Emergency Unit) At the beginning and end of your shift you must verify that the cash box contains $100. Count the money with a colleague or supervisor and use the “Collections Cash Log” (page 20) to document this verification. Both you and your colleague/supervisor must sign off. First thing each morning all collections and reports will be verified by the manager or supervisor. 18
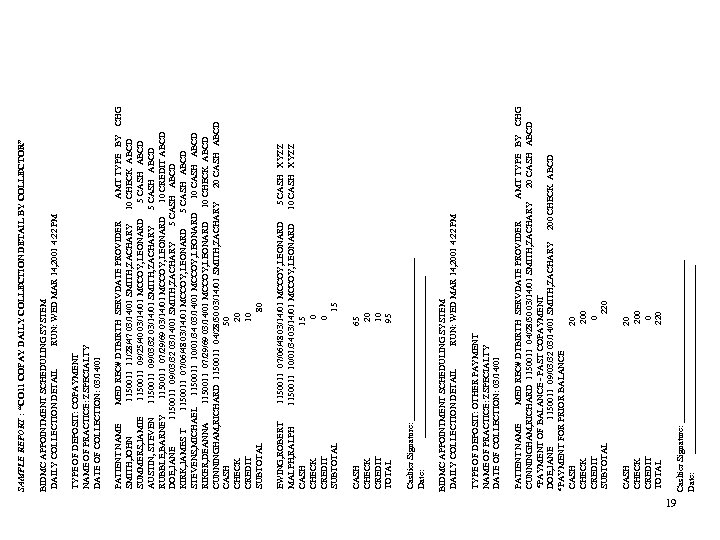
19 Cashier Signature: __________________ Date: _____________________ CASH 20 CHECK 200 CREDIT 0 TOTAL 220 PATIENT NAME MED REC# DTBIRTH SERVDATE PROVIDER AMT TYPE BY CHG CUNNINGHAM, RICHARD 1150011 04/28/50 03/14/01 SMITH, ZACHARY 20 CASH ABCD *PAYMENT OF BALANCE - PAST COPAYMENT DOE, JANE 1150011 09/03/32 03/14/01 SMITH, ZACHARY 200 CHECK ABCD *PAYMENT FOR PRIOR BALANCE CASH 20 CHECK 200 CREDIT 0 SUBTOTAL 220 TYPE OF DEPOSIT: OTHER PAYMENT NAME OF PRACTICE: ZSPECIALTY DATE OF COLLECTION: 03/14/01 BIDMC APPOINTMENT SCHEDULING SYSTEM DAILY COLLECTION DETAIL RUN: WED MAR 14, 2001 4: 22 PM Cashier Signature: __________________ Date: __________________ CASH 65 CHECK 20 CREDIT 10 TOTAL 95 EWING, ROBERT 1150011 07/06/48 03/14/01 MCCOY, LEONARD 5 CASH XYZZ MALPH, RALPH 1150011 10/01/34 03/14/01 MCCOY, LEONARD 10 CASH XYZZ CASH 15 CHECK 0 CREDIT 0 SUBTOTAL 15 PATIENT NAME MED REC# DTBIRTH SERVDATE PROVIDER AMT TYPE BY CHG SMITH, JOHN 1150011 11/28/47 03/14/01 SMITH, ZACHARY 10 CHECK ABCD SUMMERS, JAMIE 1150011 09/25/40 03/14/01 MCCOY, LEONARD 5 CASH ABCD AUSTIN, STEVEN 1150011 09/03/32 03/14/01 SMITH, ZACHARY 5 CASH ABCD RUBBLE, BARNEY 1150011 07/29/69 03/14/01 MCCOY, LEONARD 10 CREDIT ABCD DOE, JANE 1150011 09/03/32 03/14/01 SMITH, ZACHARY 5 CASH ABCD KIRK, JAMES T 1150011 07/06/48 03/14/01 MCCOY, LEONARD 5 CASH ABCD STEVENS, MICHAEL 1150011 10/01/34 03/14/01 MCCOY, LEONARD 10 CASH ABCD RIKER, DEANNA 1150011 07/29/69 03/14/01 MCCOY, LEONARD 10 CHECK ABCD CUNNINGHAM, RICHARD 1150011 04/28/50 03/14/01 SMITH, ZACHARY 20 CASH ABCD CASH 50 CHECK 20 CREDIT 10 SUBTOTAL 80 TYPE OF DEPOSIT: COPAYMENT NAME OF PRACTICE: ZSPECIALTY DATE OF COLLECTION: 03/14/01 BIDMC APPOINTMENT SCHEDULING SYSTEM DAILY COLLECTION DETAIL RUN: WED MAR 14, 2001 4: 22 PM SAMPLE REPORT : “CO 11 COPAY DAILY COLLECTION DETAIL BY COLLECTOR”
20
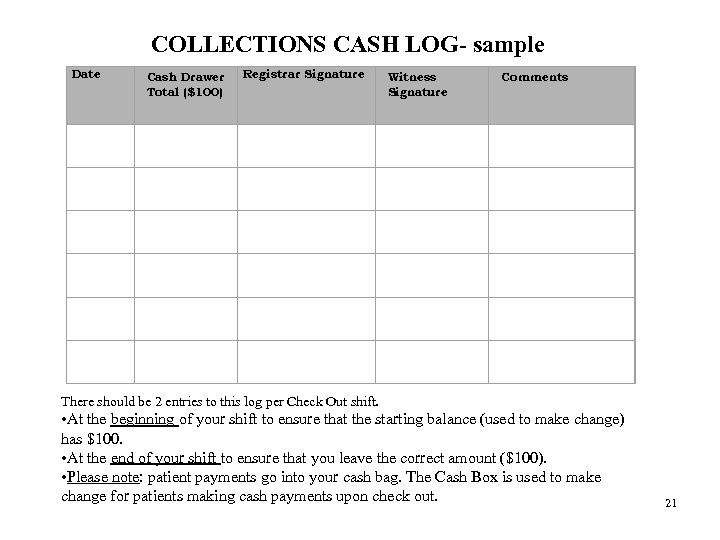
Date COLLECTIONS CASH LOG- sample Registrar Signature Cash Drawer Witness Comments Total ($100) Signature There should be 2 entries to this log per Check Out shift. • At the beginning of your shift to ensure that the starting balance (used to make change) has $100. • At the end of your shift to ensure that you leave the correct amount ($100). • Please note: patient payments go into your cash bag. The Cash Box is used to make change for patients making cash payments upon check out. 21
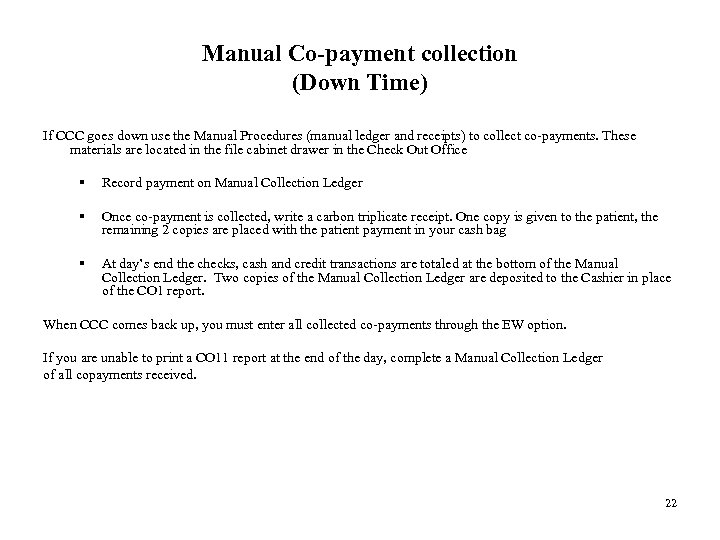
Manual Co-payment collection (Down Time) If CCC goes down use the Manual Procedures (manual ledger and receipts) to collect co-payments. These materials are located in the file cabinet drawer in the Check Out Office § Record payment on Manual Collection Ledger § Once co-payment is collected, write a carbon triplicate receipt. One copy is given to the patient, the remaining 2 copies are placed with the patient payment in your cash bag § At day’s end the checks, cash and credit transactions are totaled at the bottom of the Manual Collection Ledger. Two copies of the Manual Collection Ledger are deposited to the Cashier in place of the CO 1 report. When CCC comes back up, you must enter all collected co-payments through the EW option. If you are unable to print a CO 11 report at the end of the day, complete a Manual Collection Ledger of all copayments received. 22
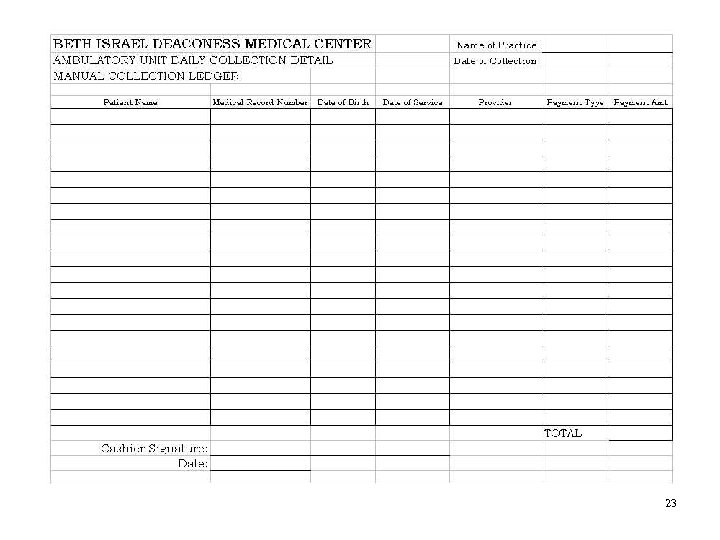
23
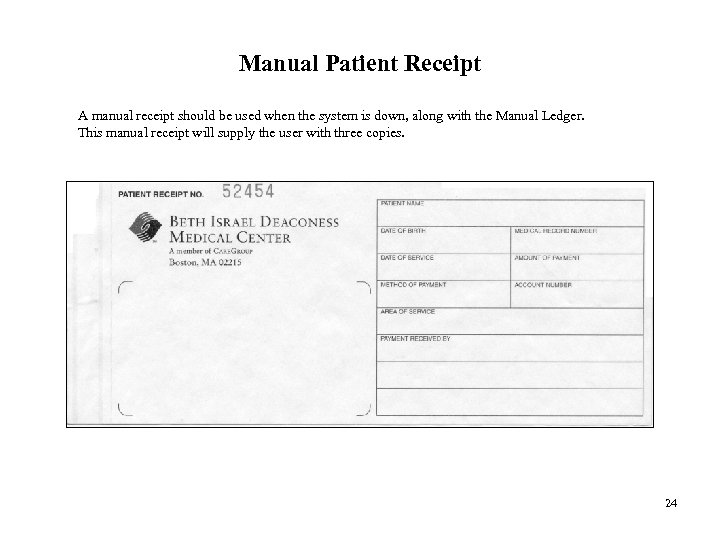
Manual Patient Receipt A manual receipt should be used when the system is down, along with the Manual Ledger. This manual receipt will supply the user with three copies. 24
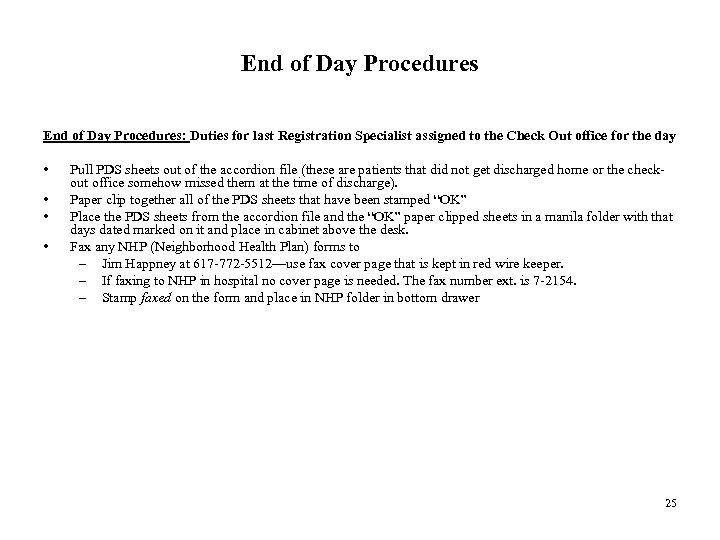
End of Day Procedures: Duties for last Registration Specialist assigned to the Check Out office for the day • • Pull PDS sheets out of the accordion file (these are patients that did not get discharged home or the checkout office somehow missed them at the time of discharge). Paper clip together all of the PDS sheets that have been stamped “OK” Place the PDS sheets from the accordion file and the “OK” paper clipped sheets in a manila folder with that days dated marked on it and place in cabinet above the desk. Fax any NHP (Neighborhood Health Plan) forms to – Jim Happney at 617 -772 -5512—use fax cover page that is kept in red wire keeper. – If faxing to NHP in hospital no cover page is needed. The fax number ext. is 7 -2154. – Stamp faxed on the form and place in NHP folder in bottom drawer 25
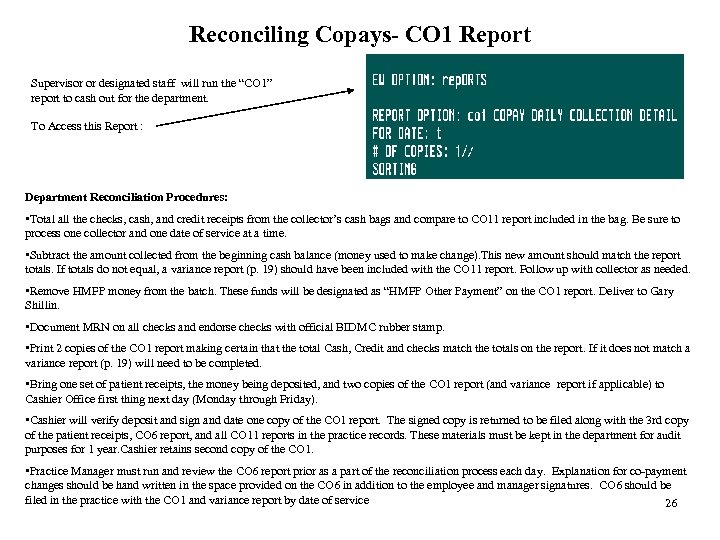
Reconciling Copays- CO 1 Report Supervisor or designated staff will run the “CO 1” report to cash out for the department. To Access this Report : Department Reconciliation Procedures: • Total all the checks, cash, and credit receipts from the collector’s cash bags and compare to CO 11 report included in the bag. Be sure to process one collector and one date of service at a time. • Subtract the amount collected from the beginning cash balance (money used to make change). This new amount should match the report totals. If totals do not equal, a variance report (p. 19) should have been included with the CO 11 report. Follow up with collector as needed. • Remove HMFP money from the batch. These funds will be designated as “HMFP Other Payment” on the CO 1 report. Deliver to Gary Shillin. • Document MRN on all checks and endorse checks with official BIDMC rubber stamp. • Print 2 copies of the CO 1 report making certain that the total Cash, Credit and checks match the totals on the report. If it does not match a variance report (p. 19) will need to be completed. • Bring one set of patient receipts, the money being deposited, and two copies of the CO 1 report (and variance report if applicable) to Cashier Office first thing next day (Monday through Friday). • Cashier will verify deposit and sign and date one copy of the CO 1 report. The signed copy is returned to be filed along with the 3 rd copy of the patient receipts, CO 6 report, and all CO 11 reports in the practice records. These materials must be kept in the department for audit purposes for 1 year. Cashier retains second copy of the CO 1. • Practice Manager must run and review the CO 6 report prior as a part of the reconciliation process each day. Explanation for co-payment changes should be hand written in the space provided on the CO 6 in addition to the employee and manager signatures. CO 6 should be filed in the practice with the CO 1 and variance report by date of service 26
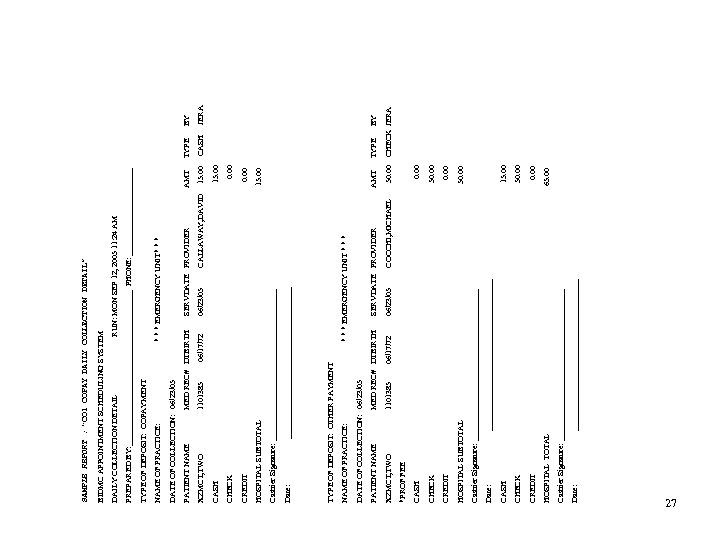
Date: ___________________ Cashier Signature: ___________________ HOSPITAL TOTAL 65. 00 CREDIT 0. 00 CHECK 50. 00 CASH 15. 00 Date: ___________________ Cashier Signature: ___________________ HOSPITAL SUBTOTAL 50. 00 CREDIT 0. 00 CHECK 50. 00 CASH 0. 00 *PROF FEE XZMCT, TWO 1101385 06/17/72 06/23/05 COCCHI, MICHAEL 50. 00 CHECK JERA PATIENT NAME MED REC# DTBIRTH SERVDATE PROVIDER AMT TYPE BY DATE OF COLLECTION: 06/23/05 NAME OF PRACTICE: * * * EMERGENCY UNIT * * * TYPE OF DEPOSIT: OTHER PAYMENT Date: ___________________ Cashier Signature: ___________________ HOSPITAL SUBTOTAL 15. 00 CREDIT 0. 00 CHECK 0. 00 CASH 15. 00 XZMCT, TWO 1101385 06/17/72 06/23/05 CALLAWAY, DAVID 15. 00 CASH JERA PATIENT NAME MED REC# DTBIRTH SERVDATE PROVIDER AMT TYPE BY DATE OF COLLECTION: 06/23/05 NAME OF PRACTICE: * * * EMERGENCY UNIT* * * TYPE OF DEPOSIT: COPAYMENT PREPARED BY: ____________________ PHONE: ___________ DAILY COLLECTION DETAIL RUN: MON SEP 12, 2005 11: 24 AM BIDMC APPOINTMENT SCHEDULING SYSTEM SAMPLE REPORT : “CO 1 COPAY DAILY COLLECTION DETAIL” 27
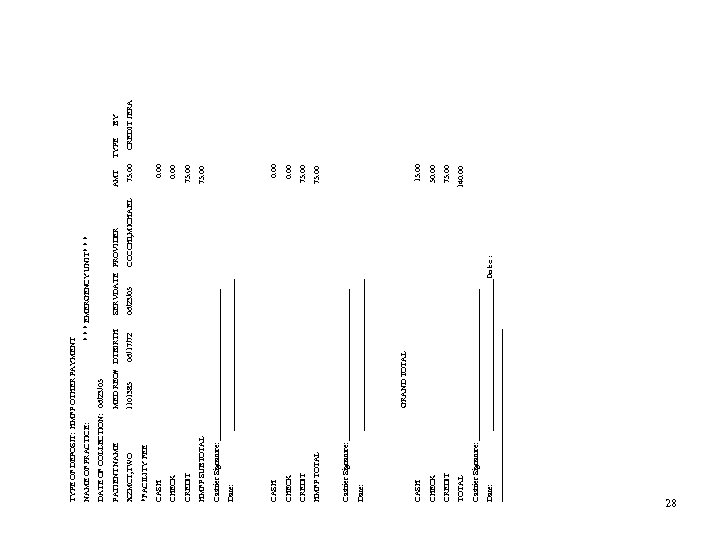
Date: ___________________Date: __________________ Cashier Signature: ___________________ TOTAL 140. 00 CREDIT 75. 00 CHECK 50. 00 CASH 15. 00 GRAND TOTAL Date: ___________________ Cashier Signature: ___________________ HMFP TOTAL 75. 00 CREDIT 75. 00 CHECK 0. 00 CASH 0. 00 Date: ___________________ Cashier Signature: ___________________ HMFP SUBTOTAL 75. 00 CREDIT 75. 00 CHECK 0. 00 CASH 0. 00 *FACILITY FEE XZMCT, TWO 1101385 06/17/72 06/23/05 COCCHI, MICHAEL 75. 00 CREDIT JERA PATIENT NAME MED REC# DTBIRTH SERVDATE PROVIDER AMT TYPE BY DATE OF COLLECTION: 06/23/05 NAME OF PRACTICE: * * * EMERGENCY UNIT* * * TYPE OF DEPOSIT: HMFP OTHER PAYMENT 28
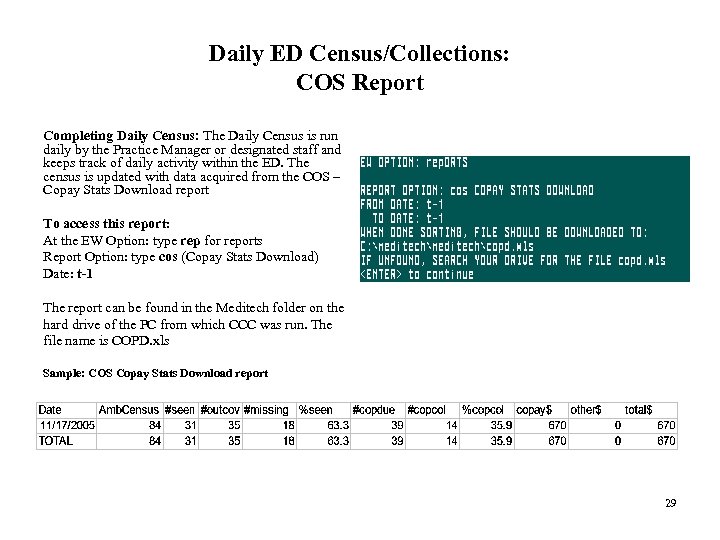
Daily ED Census/Collections: COS Report Completing Daily Census: The Daily Census is run daily by the Practice Manager or designated staff and keeps track of daily activity within the ED. The census is updated with data acquired from the COS – Copay Stats Download report To access this report: At the EW Option: type rep for reports Report Option: type cos (Copay Stats Download) Date: t-1 The report can be found in the Meditech folder on the hard drive of the PC from which CCC was run. The file name is COPD. xls Sample: COS Copay Stats Download report 29
Daily ED Census/Collections: COS Report (cont. ) • • • Date = The date that patients were discharged Amb. Census = number of patients registered and admitted to the ED #Seen = the number of patients on the Amb Census minus patients who were admitted, left without being seen and have auto/liability or worker’s comp insurance #Outcov = the number of patients who were registered outside of the Check Out office business hours. Count all patients registered before 9: 00 am and after 10: 00 pm. #missing = the number of patients that did not go through the Check Out office during Check Out office business hours %seen = the percentage of patients from the #seen and #missing columns who went through the Check Out office #copdue = the number of #seen + #missing visits that have insurance that require a copay #copcol = the number of visits where a copay was collected %copcol = the percentage of visits requiring a copay that were actually collected copay$ = the actual amount of copay money collected other$ = the actual amount of “other payments” collected. total$ = the total money collected (copay + other payments) 30
Daily ED Census/Collections Report • The information that is reported via the COS report is to be entered in the Monthly Copay Report on the shared drive (s: drive under ED Checkout/Check Out Office/Monthly Copay Report) • Locate the appropriate date—remember you are working on yesterday’s info. • Under each column, record the information that was reported from the COS report • From the File Menu, choose Save. • Print a copy of the spreadsheet • It is now safe to close the spreadsheet. • Attach the COS report to the deposit slips for the appropriate date and place in the folder for that month in the bottom drawer (same file cabinet as the cash box) 31
What if? • If a patient has a complaint, please take down information, call back number and give to either Karen Lottatore or Gary Shillin. If it is an extreme emergency, page either Karen or Gary immediately. • If a patient has questions regarding their discharge instructions, contact the nurse who was working with the patient. • What if the patient doesn’t have their discharge instructions? – Page the Primary Nurse • What if my CO 11 report doesn’t match the amount of money I have in my cash bag? – Review your receipts to see if you can locate the discrepancy. Edit the Check out option as necessary. If you are unable to locate the error complete a variance report that details the nature of the discrepancy. Submit the variance report with your CO 11, receipts and money at the end of your shift. 32
Resources Ambulatory Educations and Systems Team: Amy Goldman 617 -667 -1590 Jerry Amirault 617 -667 -1593 Policy Questions: Your Supervisor 33
e0b48125e38baa83b5ff1ce3605aa7df.ppt