Benign Prostatic Hypertrophy 2008 Causes of symptoms Hyperplasia

Benign Prostatic Hypertrophy 2008
Causes of symptoms Hyperplasia of epithelial and stromal components of prostate Progressive obstruction of urinary outflow Increased activity of detrusor muscle Causes Frequency, nocturia Poor flow , intermittent stream Hesitation, terminal dribbling
Prevalence Men > 50 = 41% have symptoms of LUTS Only 18% have a diagnosis Only 10% aware of drugs or surgery that will help it
Risk factors Age ? obesity

Differential diagnosis Poorly controlled diabetes Neurological disorders Urinary tract infections Abacterial prostatitis Overactive bladder Drugs – diuretics, anticholinergics, antidepressants Lifestyle factors – caffeine, alcohol, xs fluids
Abnormal symptoms The presence of the following symptoms indicates referral to urologist for futher assessment Urinary incontinence Retention Dysuria Haematuria Acute change in symptoms
Examination Palpation of abdomen for enlarged bladder enlarged kidneys constipation Rectal examination for Size and consistency of prostate gland
Investigations Blood tests Fbc esr U&e’s Fasting blood sugar ? PSA – level rises with increasing volume of prostate gland Urinalysis Infection haematuria
Investigations Additional tests as appropriate by GP Ultrasound for residual urine volume Urinary diaries
Specialist investigations Reasons for doing them Patient reassurance Patient explanation Objective assessment of symptoms Diagnostic precision Ranking of treatment options Prediction of treatment outcome
Specialist investigations Uroflowmetry max flow rate and volume of residual urine after voiding – low flow rate indicates need for TURP Bladder pressure studies pressure measurement during filling and emptying (cystometry) gives information on over/under activity of detrusor muscle and obstruction of bladder outlet. Predicts response to treatment. Use antimuscarinics for over activity and turp for bladder outlet obstruction

Specialist investigations Urinary tract imaging Ultrasound to estimate residual urine Urethroscopy Visual inspection of bladder and uerethra is used in dysuria or haematuria
Assesment A validated questionnaire using international prostate symptom scale. Completion gives total score of 35 1 – 7 mild 8 – 19 moderate 20 – 35 severe Response to the quality of life questionnaire strong predictor or whether intervention is necessary
Scoring system Ask 7 questions. Answers on scale 0 – 5 depending on severity of symptoms For first 6 questions scores are Not at all = 0 < 1 in 5 = 1 < half the time = 2 About half the time = 3 > half the time = 4 Almost always = 5 Q7 Never = 0, once = 1, 2x = 2, 3x = 3, 4x = 4, 5x = 5
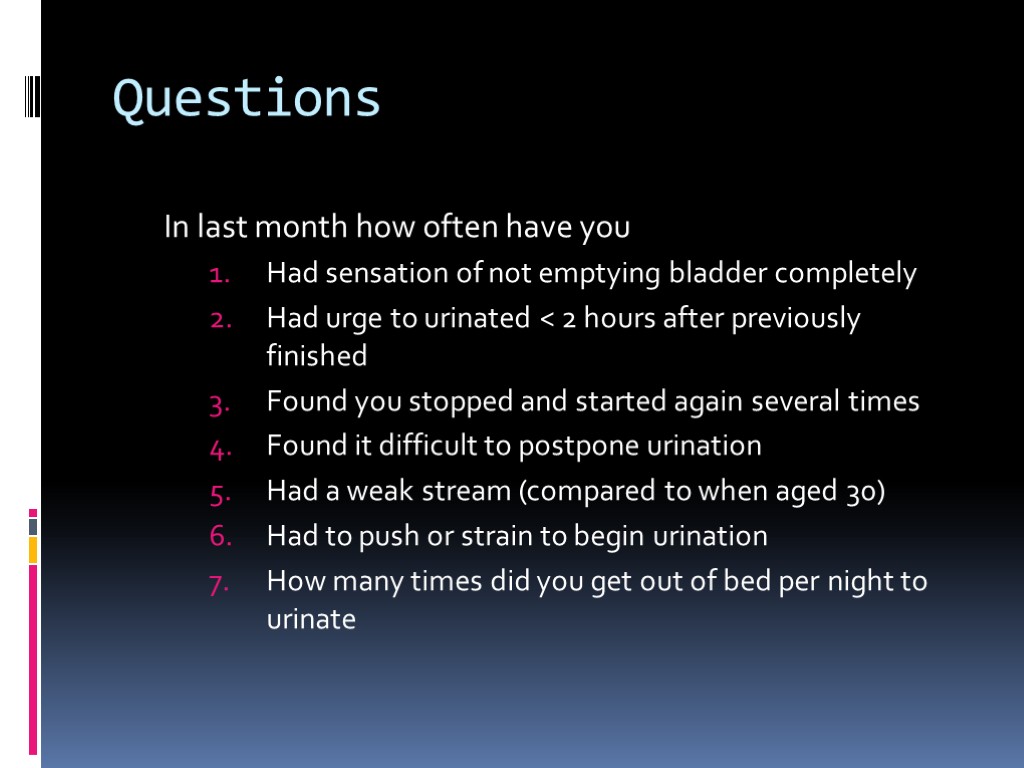
Questions In last month how often have you Had sensation of not emptying bladder completely Had urge to urinated < 2 hours after previously finished Found you stopped and started again several times Found it difficult to postpone urination Had a weak stream (compared to when aged 30) Had to push or strain to begin urination How many times did you get out of bed per night to urinate
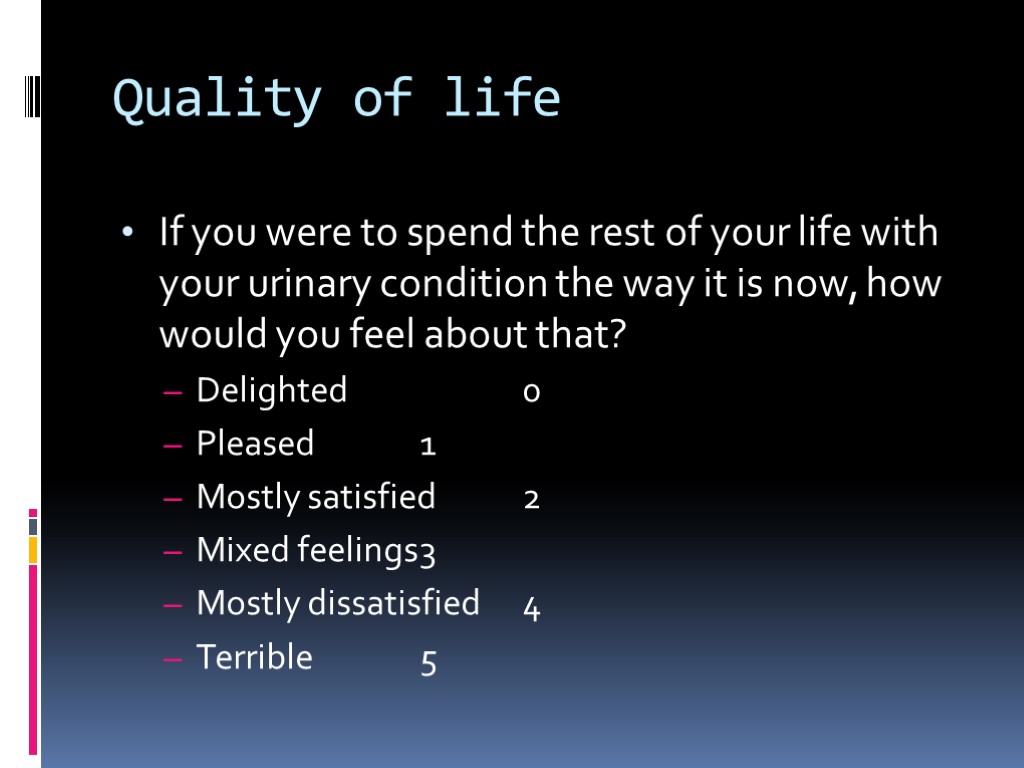
Quality of life If you were to spend the rest of your life with your urinary condition the way it is now, how would you feel about that? Delighted 0 Pleased 1 Mostly satisfied 2 Mixed feelings 3 Mostly dissatisfied 4 Terrible 5
Management Lifestyle modification Reduce fluid intake Stop diuretics if poss Avoid xs night time fluid intake/caffeine /alcohol Empty bladder before long trips/meetings
Management Treat co morbid contributing conditions Diabetes uti
Management Drug therapy Alpha blockers Improve bladder and prostate smooth muscle tone More effective than 5 alpha reductase inhibitors All work equally well Tamsulosin and alfuzosin require no dose titration
Management Surgery Adverse effects of surgery Loss of ejaculation Erectile dysfunction Retrograde ejaculation Incontinence Stricture formation Urinary retention
Management Drug therapy 5 alpha reductase inhibitors Reduce prostate volume Reduces risk of prostate cancer, increases risk of high grade disease Combined therapy Men with large prostate > 40g or PSA >4 or moderate to severe symptoms combined therapy will prevent 2 episodes of clinical progression per 100men over 4yrs. Much less effective for men with smaller prostates
Management Drug therapy Storage problems Men with symptoms of urinary urgency, frequency, small, urine volumes and nocturia in the absence of serious obstructive symptoms are categorised as over active bladder Bladder training Biofeedback Antimuscarinic drugs ( oxybutinin, tolteridine) alone or in combination with treatment for obstructive symptoms
Management Surgery TURP Greatest improvement in symptoms 5% severe haemorrhage risk Requires GA Alternative energy sources for TURP Ultrasound Laser microwave
benign_prostatic_hypertrophy.ppt
- Количество слайдов: 23

