7c9402f75fdde2c722cb91272cb762c1.ppt
- Количество слайдов: 40
Benchmarking and IT Meet Pay For Performance Demands Donna Isgett, RN, MSN Vice President of Clinical Effectiveness Mc. Leod Health, Florence, SC Gail E. Latimer, RN, MSN Vice President and Chief Nursing Officer Siemens Medical Solutions, Malvern, PA
Learning Objectives § Identify strategies to promote Pay for Performance § Describe the process and methodologies Mc. Leod has employed to build it’s culture of quality evidence-based practice and transparency § Understand the role of physician and executive leadership in developing this culture § Identify CMS outcomes achieved to date as a result of the Medicare demonstration project Page 2

Quality - Quality Everywhere 1997 • Dana Farber Cancer Institute Event 2000 • To Err is Human, IOM Report • Healthgrades. com • Business Roundtable: Leapfrog Group • Crossing the Quality Chasm, IOM Report • JCAHO Sentinel Event Alerts 2002 • Robert Wood Johnson - Pursuing Perfection Grant • CMS 7 Scopes of Work 2004 • Premier/CMS Demonstration Project Page 3

Mc. Leod Quality Publication Features: Modern Healthcare US News and World Report USA Today Milliken Award for Quality CMS/Premier Demonstration Project “Top Performer” Page 4
Quality - Pay for Performance CMS/Premier Hospital Quality Incentive § The first national project to measure hospital performance and offer additional Medicare payment for top quality care (October, 2003) § Widely accepted quality measures(34) § 27 indicators from the National Quality Forum § Public reporting 278 participating hospitals AMI, CABG, HF, CAP, Hip and Knee Page 5
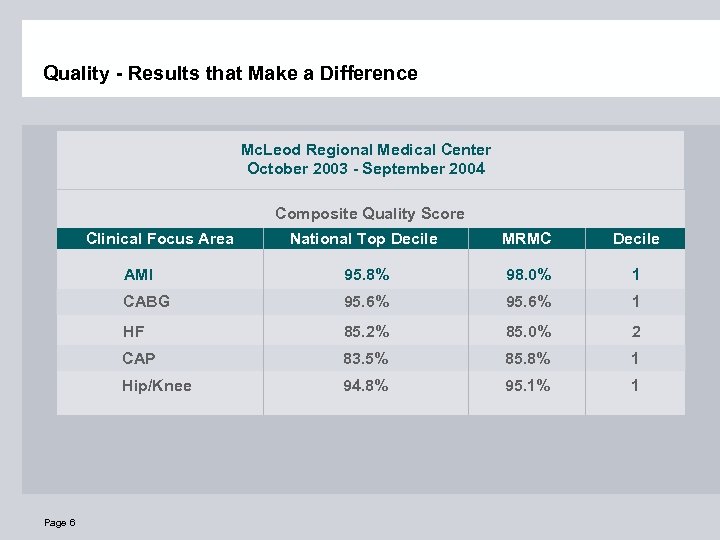
Quality - Results that Make a Difference Mc. Leod Regional Medical Center October 2003 - September 2004 Composite Quality Score Clinical Focus Area MRMC Decile AMI 95. 8% 98. 0% 1 CABG 95. 6% 1 HF 85. 2% 85. 0% 2 CAP 83. 5% 85. 8% 1 Hip/Knee Page 6 National Top Decile 94. 8% 95. 1% 1
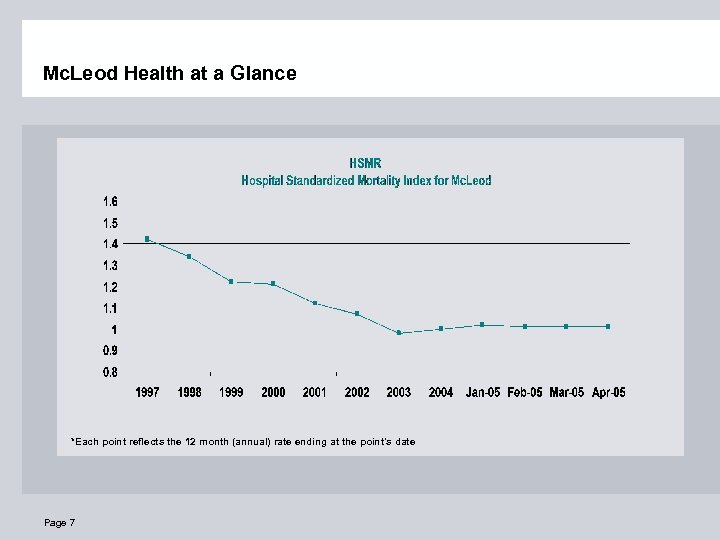
Mc. Leod Health at a Glance *Each point reflects the 12 month (annual) rate ending at the point's date Page 7
Page 8

Core Success Factors Reliability Theory Physician & Executive Engagement Change Theory Page 9 Quality Core Value Core Success Factors Prioritization Improvement Methodology
Clinical Effectiveness: Promoting Change Quality Core Value Core Success Factors Page 10
Core Values Value of Person Value of Integrity Value of Caring Value of Quality Page 11
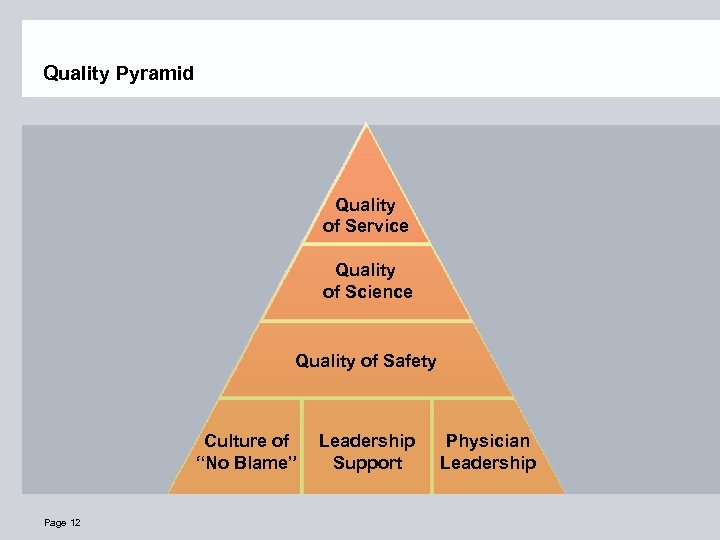
Quality Pyramid Quality of Service Quality of Science Quality of Safety Culture of “No Blame” Page 12 Leadership Support Physician Leadership
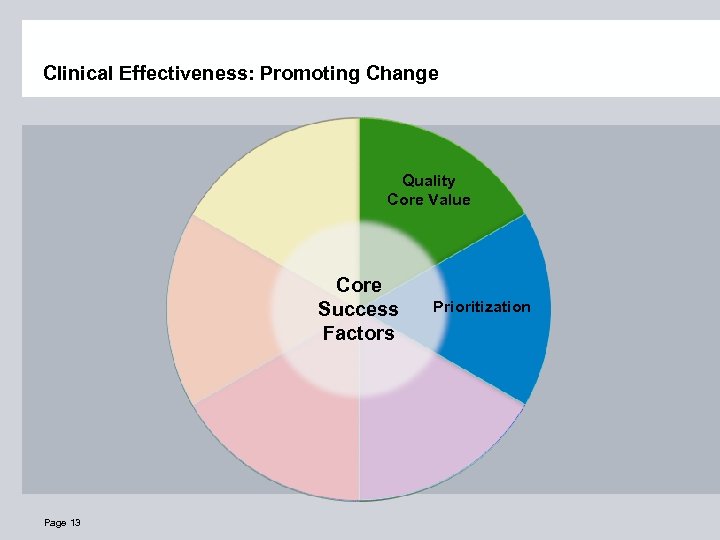
Clinical Effectiveness: Promoting Change Quality Core Value Core Success Factors Page 13 Prioritization
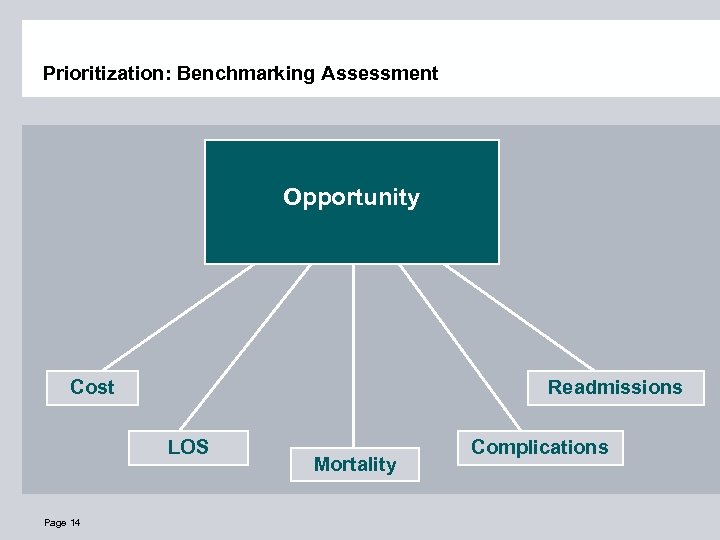
Prioritization: Benchmarking Assessment Opportunity Cost Readmissions LOS Page 14 Mortality Complications
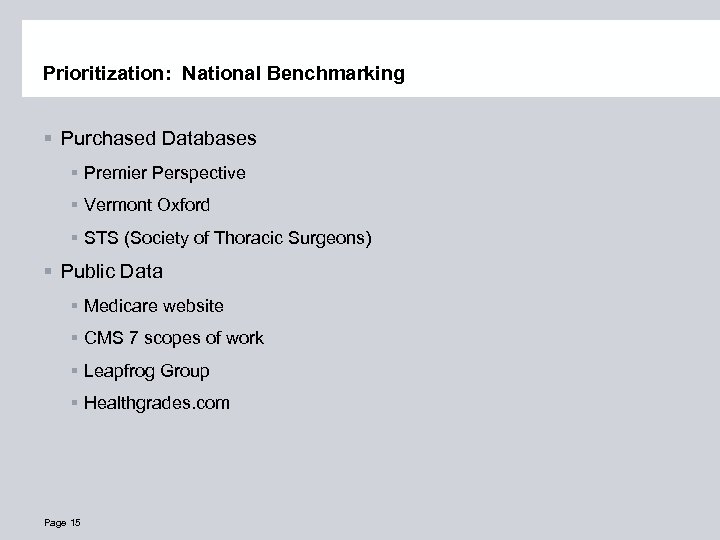
Prioritization: National Benchmarking § Purchased Databases § Premier Perspective § Vermont Oxford § STS (Society of Thoracic Surgeons) § Public Data § Medicare website § CMS 7 scopes of work § Leapfrog Group § Healthgrades. com Page 15
Clinical Effectiveness: Promoting Change Quality Core Value Core Success Factors Prioritization Improvement Methodology Page 16
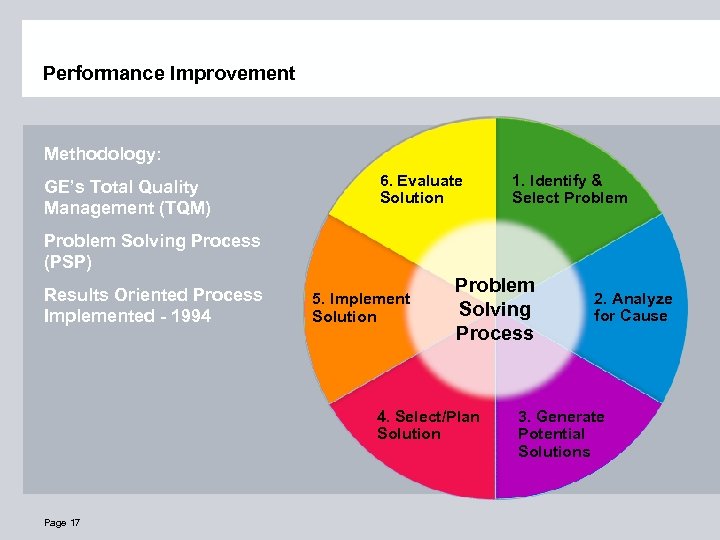
Performance Improvement Methodology: GE’s Total Quality Management (TQM) 6. Evaluate Solution 1. Identify & Select Problem Solving Process (PSP) Results Oriented Process Implemented - 1994 5. Implement Solution Problem Solving Process 4. Select/Plan Solution Page 17 2. Analyze for Cause 3. Generate Potential Solutions
Clinical Effectiveness: Promoting Change Quality Core Value Core Success Factors Change Theory Page 18 Prioritization Improvement Methodology
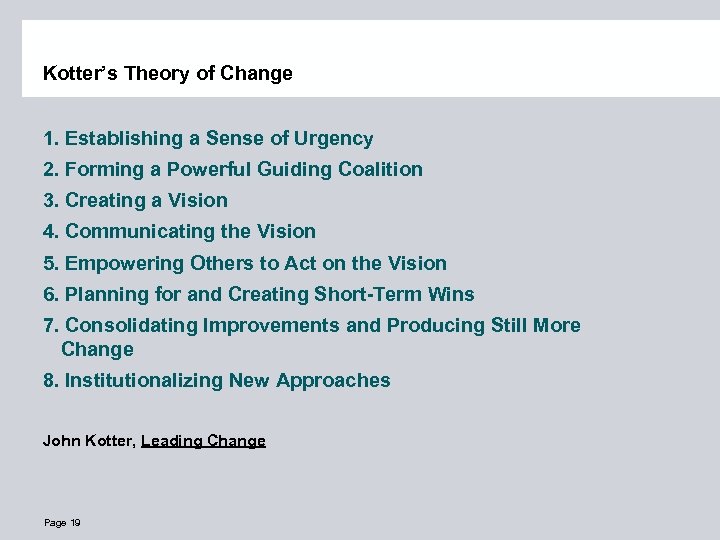
Kotter’s Theory of Change 1. Establishing a Sense of Urgency 2. Forming a Powerful Guiding Coalition 3. Creating a Vision 4. Communicating the Vision 5. Empowering Others to Act on the Vision 6. Planning for and Creating Short-Term Wins 7. Consolidating Improvements and Producing Still More Change 8. Institutionalizing New Approaches John Kotter, Leading Change Page 19
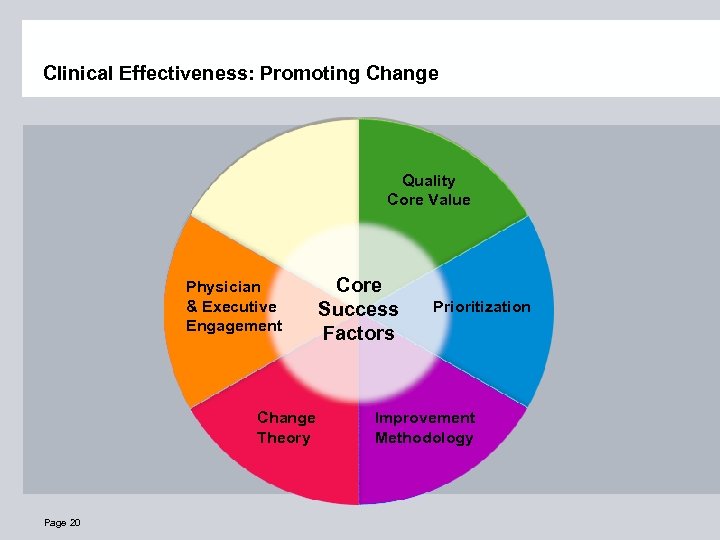
Clinical Effectiveness: Promoting Change Quality Core Value Physician & Executive Engagement Change Theory Page 20 Core Success Factors Prioritization Improvement Methodology
Clinical Effectiveness: Quality of the Science Design Principles: § Physician Leadership § Evidence Based § Data Driven Senior Leadership Key: § Priority of Work § Dedicated Staff § Implementation of Ideas Page 21

Core Success Factors Reliability Theory Physician & Executive Engagement Change Theory Page 22 Quality Core Value Core Success Factors Prioritization Improvement Methodology
Intent, Vigilance and Hard Work: 101 Performance Level 1 (Designing basic failure prevention) § Common equipment, standard orders sheets § Personal check lists § Working harder next time § Feedback of information on compliance § Awareness and training Page 23 © Institute for Healthcare Improvement
Level 1 Changes at Mc. Leod § Pre-printed order sets § Data feedback to physicians and hospital staff § Education to physicians and hospital staff § Pre-printed Rx scripts § Disease specific discharge sheets to include detailed instructions/meds Page 24 © Institute for Healthcare Improvement
Human Factors and Reliability Science: 102 Performance Level 2 § Decision aids and reminders built into the system § Desired action the default (based on evidence) § Redundancy § Scheduling § Taking advantage of habits and patterns § Standardization of process Page 25 © Institute for Healthcare Improvement
Level 2 Changes at Mc. Leod § Decision aids and reminders built into the system: § Antibiotics in Pyxis in ER and reminder on Pyxis "Blood cultures needed? Check with physician” § Decision aids and reminders built into the system: § List of all positive troponins for intervention § Desired action the default (based on evidence): § House-wide pneumonia vaccination standing order § Desired action the default (based on evidence): § Automatic printing of smoking cessation information for patients § Redundancy: § Medication check against allergies Page 26 © Institute for Healthcare Improvement
Level 2 Changes at Mc. Leod § Taking advantage of habits and patterns § All operative antibiotics given as leaving holding area § Radiologist to contact ED physician if chest XRay positive for pneumonia § Standardization of process § All patients screened for smoking at admission and counseled on discharge Page 27 © Institute for Healthcare Improvement

Core Success Factors Reliability Theory Physician & Executive Engagement Change Theory Page 28 Quality Core Value Core Success Factors Prioritization Improvement Methodology
Key Ways IT Can Support Pay for Performance § Reliability § Hand-off communication § Patients “in the know” Page 29
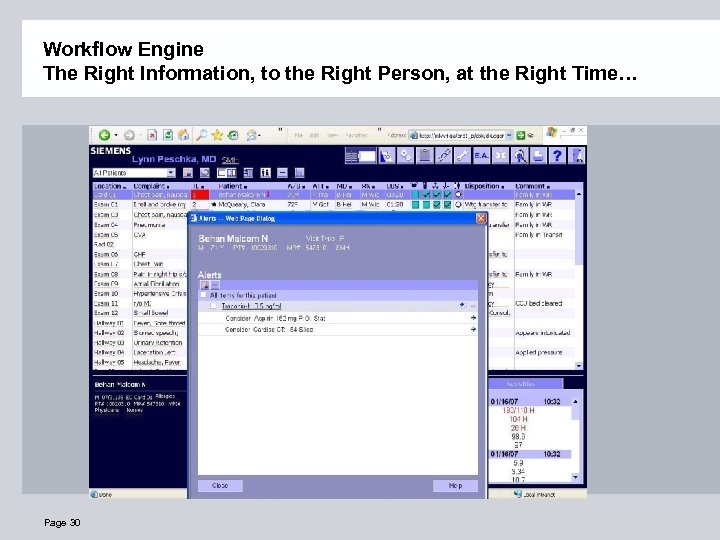
Workflow Engine The Right Information, to the Right Person, at the Right Time… Page 30
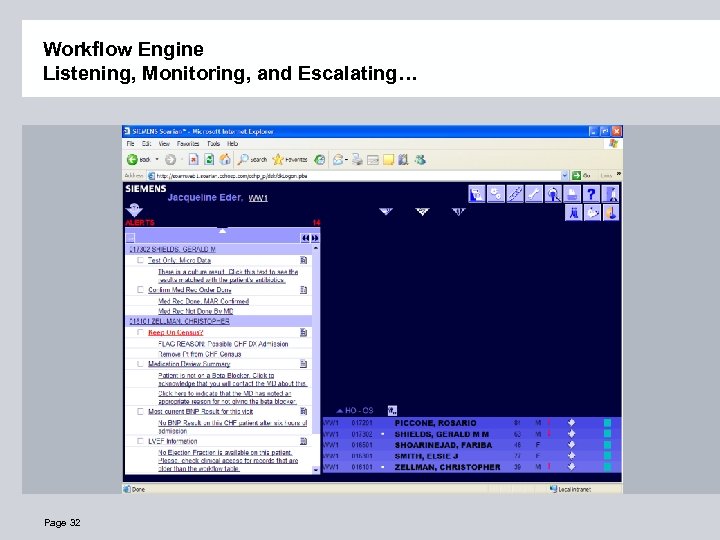
Workflow Engine Listening, Monitoring, and Escalating… Page 32
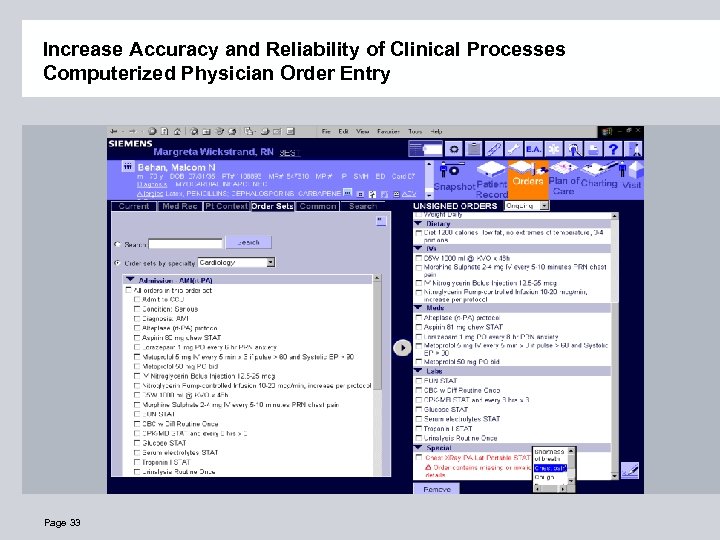
Increase Accuracy and Reliability of Clinical Processes Computerized Physician Order Entry Page 33
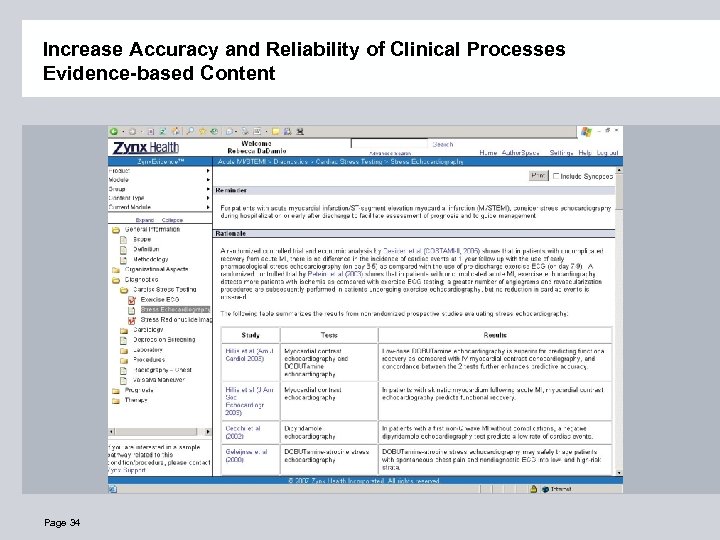
Increase Accuracy and Reliability of Clinical Processes Evidence-based Content Page 34
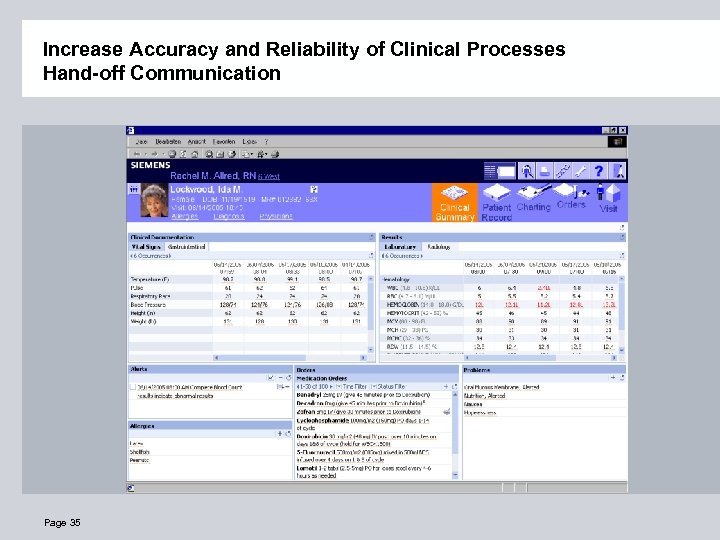
Increase Accuracy and Reliability of Clinical Processes Hand-off Communication Page 35
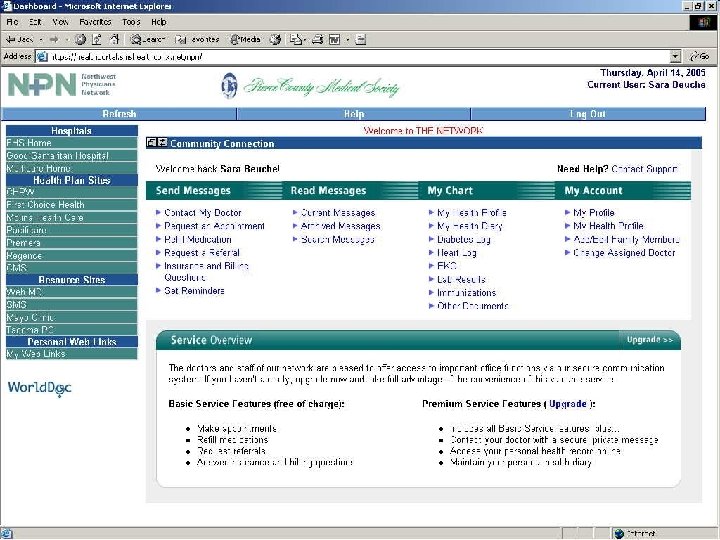
Page 36
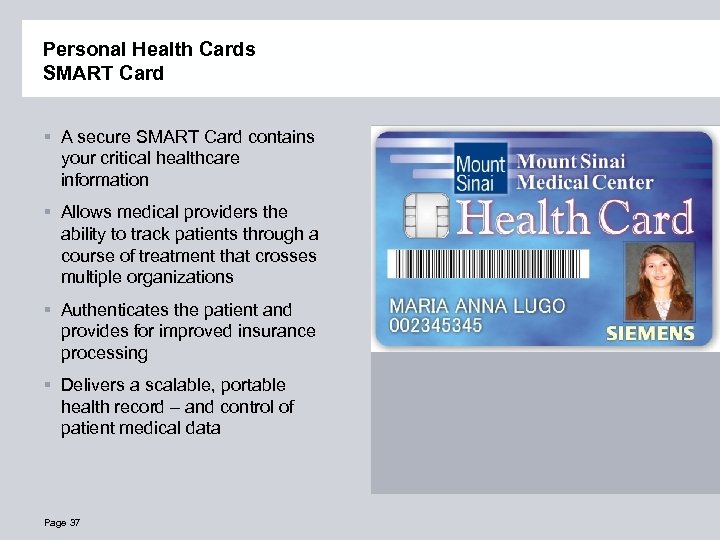
Personal Health Cards SMART Card § A secure SMART Card contains your critical healthcare information § Allows medical providers the ability to track patients through a course of treatment that crosses multiple organizations § Authenticates the patient and provides for improved insurance processing § Delivers a scalable, portable health record – and control of patient medical data Page 37
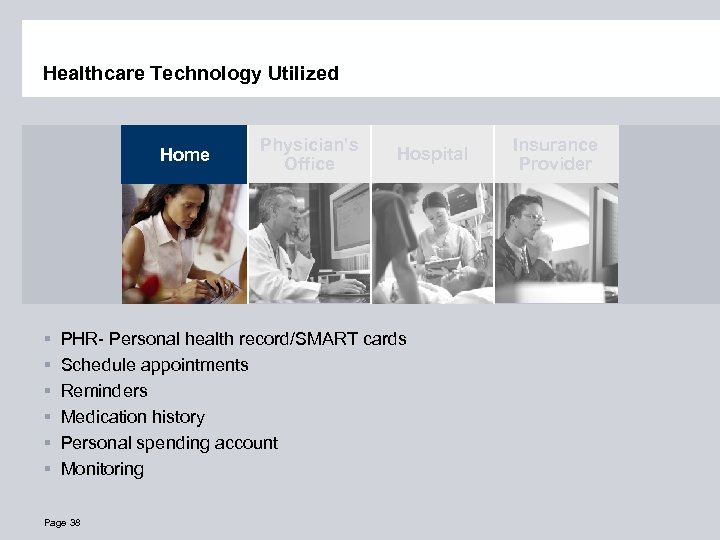
Healthcare Technology Utilized Home § § § Physician’s Office Hospital PHR- Personal health record/SMART cards Schedule appointments Reminders Medication history Personal spending account Monitoring Page 38 Insurance Provider
Healthcare Technology Utilized Home § § § Physician’s Office Interoperability Electronic patient records Referring physicians Trends/ benchmarking Billing Page 39 Hospital Insurance Provider
Healthcare Technology Utilized Home Physician’s Office Clinical Information System § § § Point of care information Evidence-based practice CPOE Workflow engine PACS/results Trends/benchmarking Page 40 Hospital Insurance Provider
Healthcare Technology Utilized Home § Clinical information § Billing codes § Payment § Trends/benchmarking Page 41 Physician’s Office Hospital Insurance Provider
7c9402f75fdde2c722cb91272cb762c1.ppt