63fc211c63ff569e280cf1ee8896cf82.ppt
- Количество слайдов: 73
Becoming a worlds expert in 30 minutes • (or at least - do just as well as any world expert in 30 minutes) • No fellowship • No Big Book • The pathway has been defined and it is well paved and brightly lit.
Behold, as I guide our conversation to my narrow area of expertise
Becoming a worlds expert in 30 minutes • Bone Density Measurement So - Why bother? BORING ! !
Disclaimer • Your presenter this morning really doesn’t care about the study. Boring. Rote. Not conceptually interesting. • Beyond that - after tax reimbursement will buy you a Venti at Starbucks
Disclaimer • But - • Your presenter really cares about not looking stupid

ME stupid unreliable not worth the $ intelligent reliable worth the $
Calm Down, It’s just a bee
A WORD (OR MORE) ABOUT TREATMENT. WHY TREAT AT ALL? ? ? • Osteoporotic fractures are very common in older patients, with serious sequelae • Treatment is easy, cheap and effective • OSTEOPOROTIC FRACTURES KILL PEOPLE
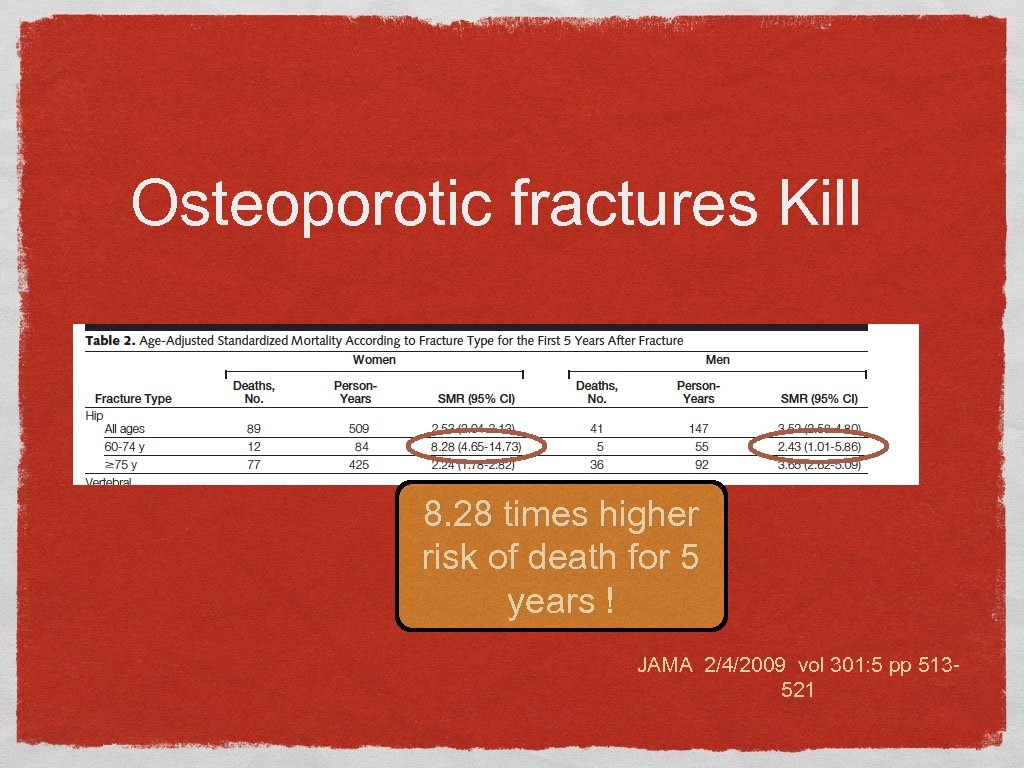
Osteoporotic fractures Kill 8. 28 times higher risk of death for 5 years ! JAMA 2/4/2009 vol 301: 5 pp 513521
Treatment Basic: Adequate Calcium intake (1200 mg/day)_ Often dietary intake adequate Vitamin D This is for Exercise everyone, Smoking Cessation regardless of Fall prevention density Moderation in ETOH

MOre aggressive Treatment Bone resorbtion decreased by 85% within Antiresorbtive therapy 3 days!! Bisphonates Monoclonal Antibody denosumab inhibits osteoclast activity and thereby reduce bone resorbtion
Treatment Bisphonates: aledronate (Binosto, Fosamax) once per week (PO) Generic: $10/month zoledronic acid (Reclast, Zometa) 5 mg every two years (IV) Generic $994/dose = $41/month Monoclonal ATB (esp for Renal Failure) Denosumab: (Prolia or Xgeva) Dosage: 60 mg SQ, every 6 months Cost $1293 per dose ($215/month) Particularly useful in patients with renal impairment http: //health. costhelper. com/osteoporosis-treatments. html
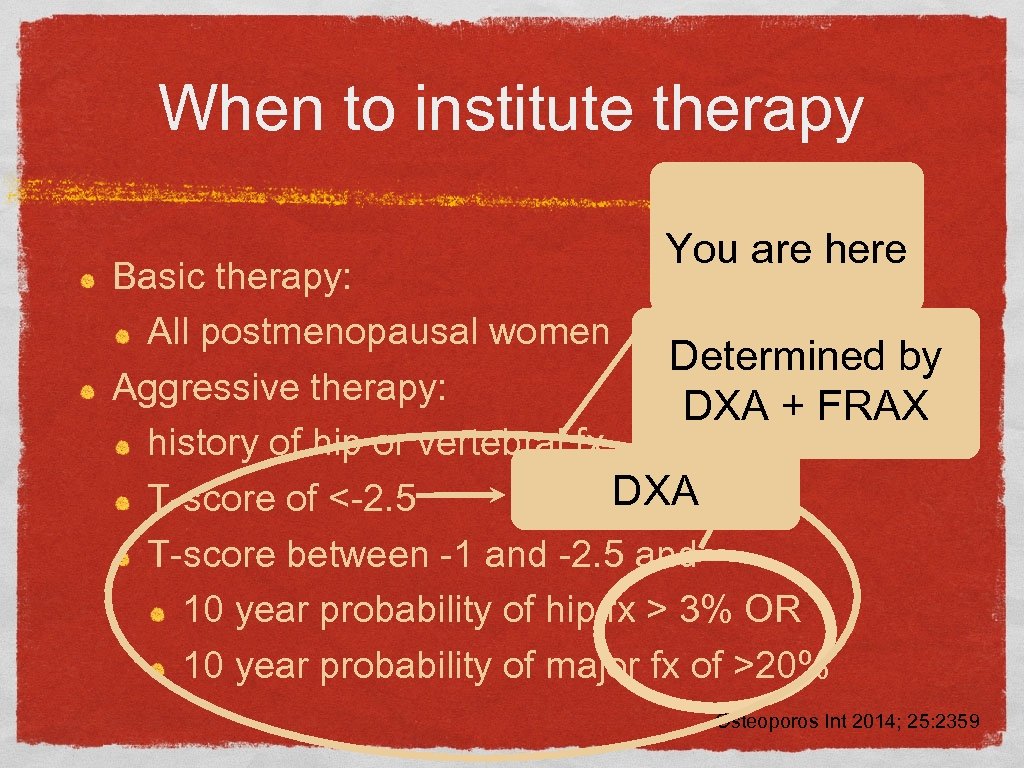
When to institute therapy You are here Basic therapy: All postmenopausal women Determined by Aggressive therapy: DXA + FRAX history of hip or vertebral fx DXA T-score of <-2. 5 T-score between -1 and -2. 5 and 10 year probability of hip fx > 3% OR 10 year probability of major fx of >20% Osteoporos Int 2014; 25: 2359
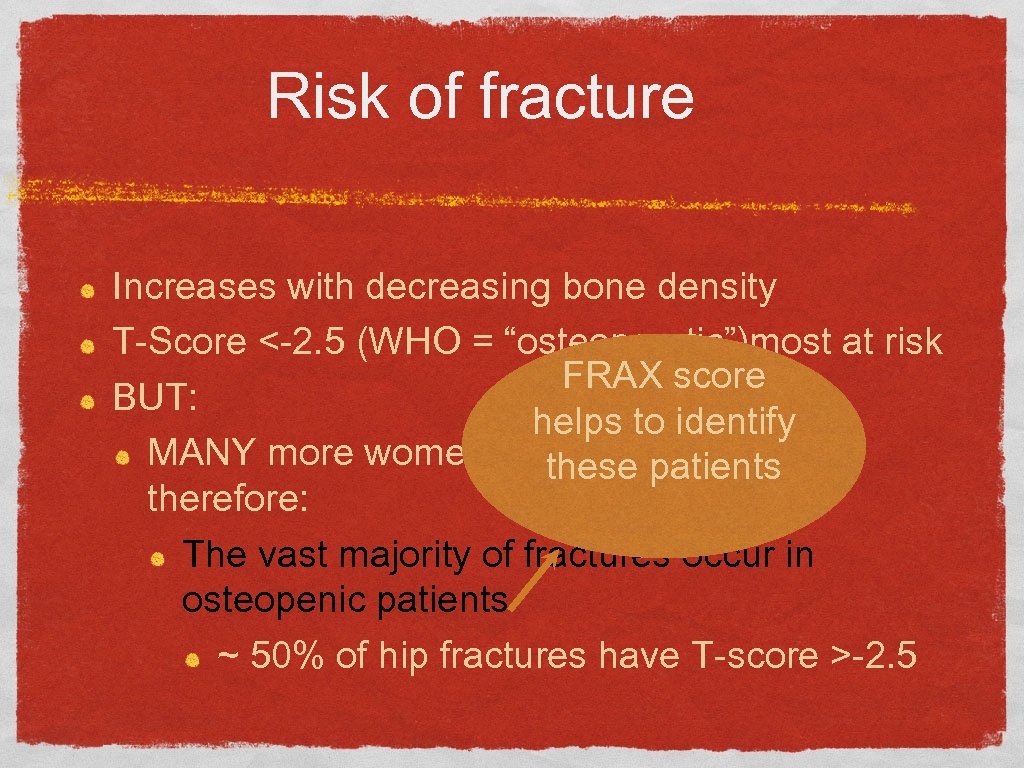
Risk of fracture Increases with decreasing bone density T-Score <-2. 5 (WHO = “osteoporotic”)most at risk FRAX score BUT: helps to identify MANY more women are “osteopenic”, these patients therefore: The vast majority of fractures occur in osteopenic patients ~ 50% of hip fractures have T-score >-2. 5
Is aggressive therapy effective? YES
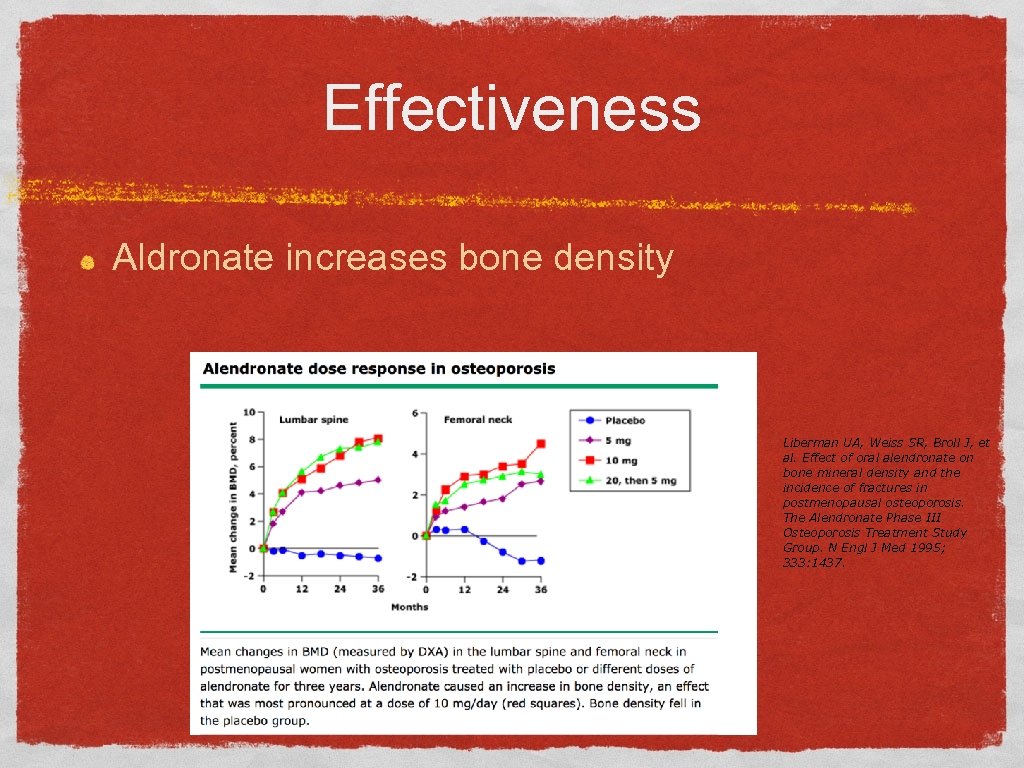
Effectiveness Aldronate increases bone density Liberman UA, Weiss SR, Broll J, et al. Effect of oral alendronate on bone mineral density and the incidence of fractures in postmenopausal osteoporosis. The Alendronate Phase III Osteoporosis Treatment Study Group. N Engl J Med 1995; 333: 1437.
Reduction in fracture incidence Treatment WORKS ~40% reduction in hip fractures
Effectiveness Bisphonates - randomized trials reduce painful spine fractures by up to 8590% reduce hip fractures by 20 -25% REDUCE ALL CAUSE MORTALITY BY 28% Despite this, most who could benefit are not treated and those who are treated < 50% continue treatment
DXA reporting: What is “right”? • International Society of Clinical Densitometry - ISCD • ISCD. org • Developed the statistical basis of the interpretation • defined what and how to report
ISCD survey • 71% of readers had seen an incorrect interpretation at least once a month • 98% of clinicians felt that poor quality reports harm patient care Lewiecki EM, et al. DXA quality matters. J Clin Densitom. 2006; 9: 388– 392. [Pub. Med: 17097522]
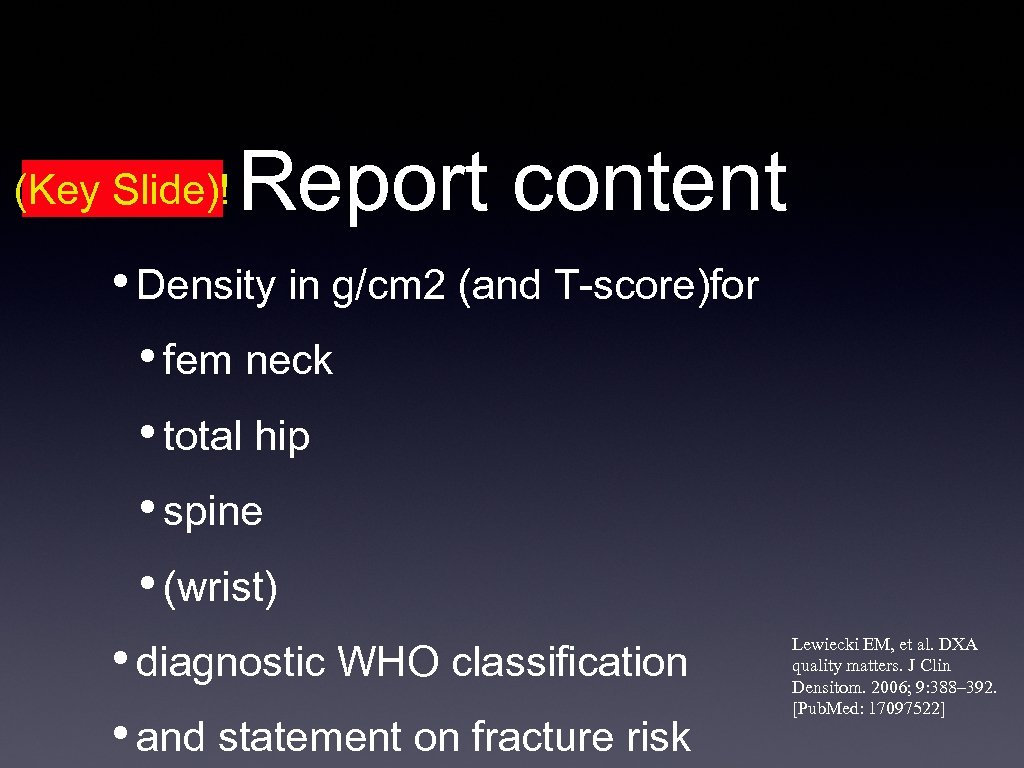
(Key Slide)! Report content • Density in g/cm 2 (and T-score)for • fem neck • total hip • spine • (wrist) • diagnostic WHO classification • and statement on fracture risk Lewiecki EM, et al. DXA quality matters. J Clin Densitom. 2006; 9: 388– 392. [Pub. Med: 17097522]
Training animals (to include radiologists) Make the right thing easy Make the wrong thing hard
Easy reporting What should be in the report Templates - with modules Module 1 - baseline or standard report Module 2 - Comparison Module 3 - FRAX report Module 4 - forearm report
![Module 1 - Standard report EXAMINATION: BONE DENSITOMETRY [<Completed Date>] COMPARISON: [None. ] HISTORY: Module 1 - Standard report EXAMINATION: BONE DENSITOMETRY [<Completed Date>] COMPARISON: [None. ] HISTORY:](https://present5.com/presentation/63fc211c63ff569e280cf1ee8896cf82/image-24.jpg)
Module 1 - Standard report EXAMINATION: BONE DENSITOMETRY [<Completed Date>] COMPARISON: [None. ] HISTORY: [<Reason For Exam>] TECHNIQUE: Bone mineral density measurements were obtained of the lumbar spine and [left hip] Risk Factors: [Postmenopausal] Instrument: Hologic serial number []
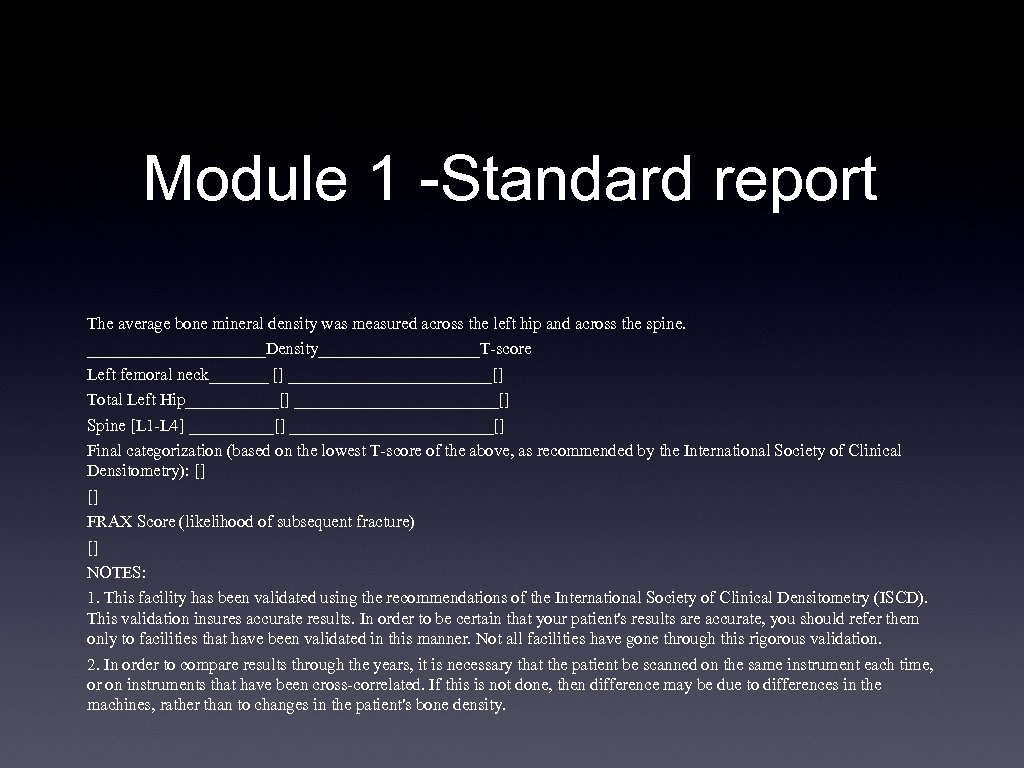
Module 1 -Standard report The average bone mineral density was measured across the left hip and across the spine. ___________Density__________T-score Left femoral neck_______ [] ____________[] Total Left Hip______[] ____________[] Spine [L 1 -L 4] _____[] ____________[] Final categorization (based on the lowest T-score of the above, as recommended by the International Society of Clinical Densitometry): [] [] FRAX Score (likelihood of subsequent fracture) [] NOTES: 1. This facility has been validated using the recommendations of the International Society of Clinical Densitometry (ISCD). This validation insures accurate results. In order to be certain that your patient's results are accurate, you should refer them only to facilities that have been validated in this manner. Not all facilities have gone through this rigorous validation. 2. In order to compare results through the years, it is necessary that the patient be scanned on the same instrument each time, or on instruments that have been cross-correlated. If this is not done, then difference may be due to differences in the machines, rather than to changes in the patient's bone density.
![Module 2 -Comparison COMPARISON WITH PRIOR EXAMINATION: Prior examination date [] Spine: Current density: Module 2 -Comparison COMPARISON WITH PRIOR EXAMINATION: Prior examination date [] Spine: Current density:](https://present5.com/presentation/63fc211c63ff569e280cf1ee8896cf82/image-26.jpg)
Module 2 -Comparison COMPARISON WITH PRIOR EXAMINATION: Prior examination date [] Spine: Current density: [] The difference between these two is greater than the experimentally determined LSC for this machine, therefore, compared to prior: Previous density: [] THERE HAS BEEN A STATISTICALLY SIGNIFICANT [] IN BONE [] Left hip: The difference between these two is less than the experimentally determined LSC for this machine, therefore, compared to prior: Current Density: [] NO STATISTICALLY SIGNIFICANT CHANGE Previous density: [] []
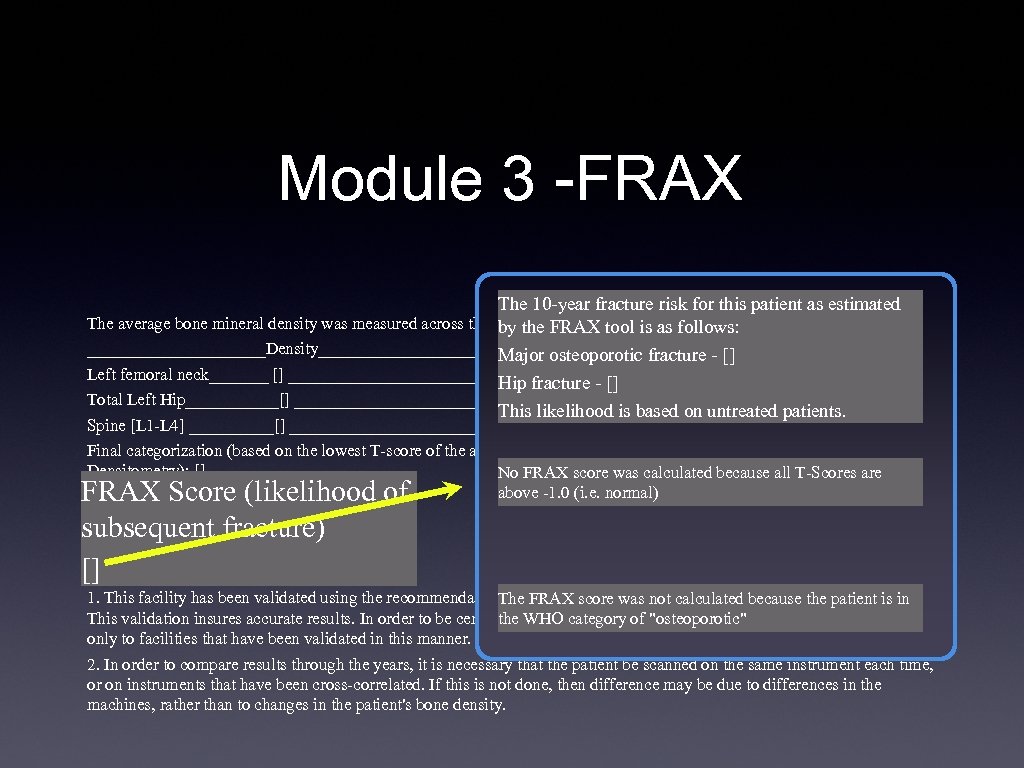
Module 3 -FRAX The 10 -year fracture risk for this patient as estimated The average bone mineral density was measured across the left hip and across theis as follows: by the FRAX tool spine. ___________Density__________T-score osteoporotic fracture - [] Major Left femoral neck_______ [] ____________[] Hip fracture - [] Total Left Hip______[] ____________[] This likelihood is based on untreated patients. Spine [L 1 -L 4] _____[] ____________[] Final categorization (based on the lowest T-score of the above, as recommended by the International Society of Clinical Densitometry): [] No FRAX score was calculated because all T-Scores are above -1. 0 (i. e. normal) [] FRAX Score (likelihood of subsequent fracture) [] NOTES: 1. This facility has been validated using the recommendations of FRAX score was Society of Clinical Densitometry (ISCD). The the International not calculated because the patient is in This validation insures accurate results. In order to be certain that your category of "osteoporotic" you should refer them the WHO patient's results are accurate, only to facilities that have been validated in this manner. Not all facilities have gone through this rigorous validation. 2. In order to compare results through the years, it is necessary that the patient be scanned on the same instrument each time, or on instruments that have been cross-correlated. If this is not done, then difference may be due to differences in the machines, rather than to changes in the patient's bone density. FRAX Score (likelihood of subsequent fracture) []
Module 4 -Radius
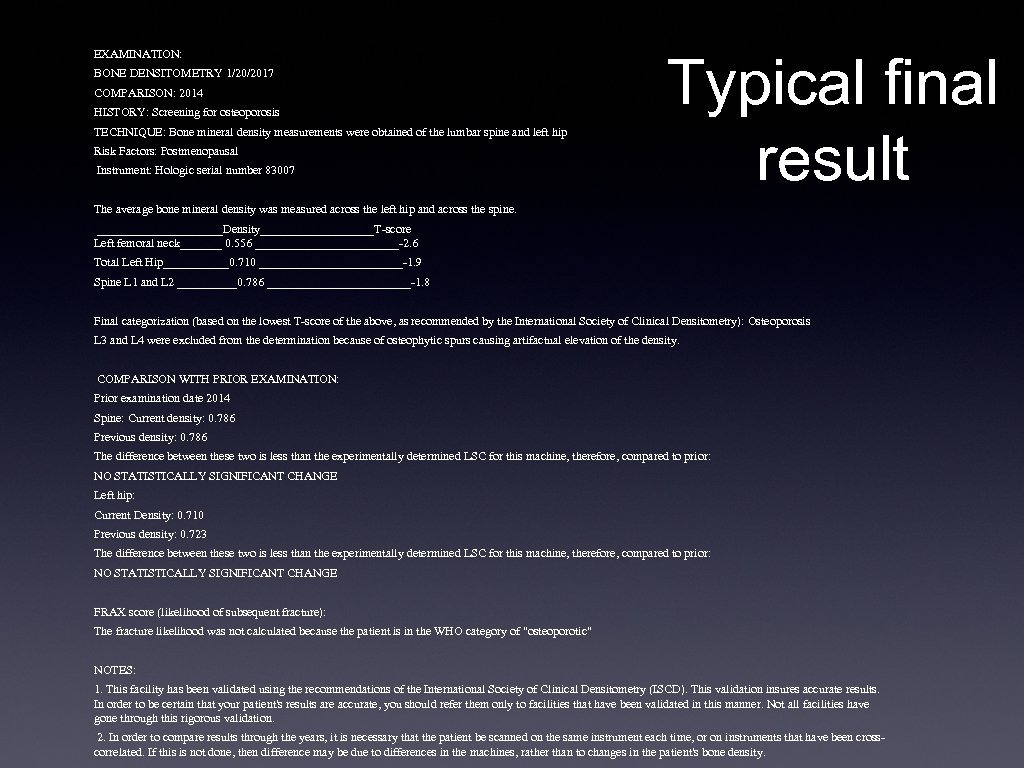
EXAMINATION: BONE DENSITOMETRY 1/20/2017 COMPARISON: 2014 HISTORY: Screening for osteoporosis TECHNIQUE: Bone mineral density measurements were obtained of the lumbar spine and left hip Risk Factors: Postmenopausal Instrument: Hologic serial number 83007 Typical final result The average bone mineral density was measured across the left hip and across the spine. ___________Density__________T-score Left femoral neck_______ 0. 556 ____________-2. 6 Total Left Hip______0. 710 ____________-1. 9 Spine L 1 and L 2 _____0. 786 ____________-1. 8 Final categorization (based on the lowest T-score of the above, as recommended by the International Society of Clinical Densitometry): Osteoporosis L 3 and L 4 were excluded from the determination because of osteophytic spurs causing artifactual elevation of the density. COMPARISON WITH PRIOR EXAMINATION: Prior examination date 2014 Spine: Current density: 0. 786 Previous density: 0. 786 The difference between these two is less than the experimentally determined LSC for this machine, therefore, compared to prior: NO STATISTICALLY SIGNIFICANT CHANGE Left hip: Current Density: 0. 710 Previous density: 0. 723 The difference between these two is less than the experimentally determined LSC for this machine, therefore, compared to prior: NO STATISTICALLY SIGNIFICANT CHANGE FRAX score (likelihood of subsequent fracture): The fracture likelihood was not calculated because the patient is in the WHO category of "osteoporotic" NOTES: 1. This facility has been validated using the recommendations of the International Society of Clinical Densitometry (ISCD). This validation insures accurate results. In order to be certain that your patient's results are accurate, you should refer them only to facilities that have been validated in this manner. Not all facilities have gone through this rigorous validation. 2. In order to compare results through the years, it is necessary that the patient be scanned on the same instrument each time, or on instruments that have been crosscorrelated. If this is not done, then difference may be due to differences in the machines, rather than to changes in the patient's bone density.
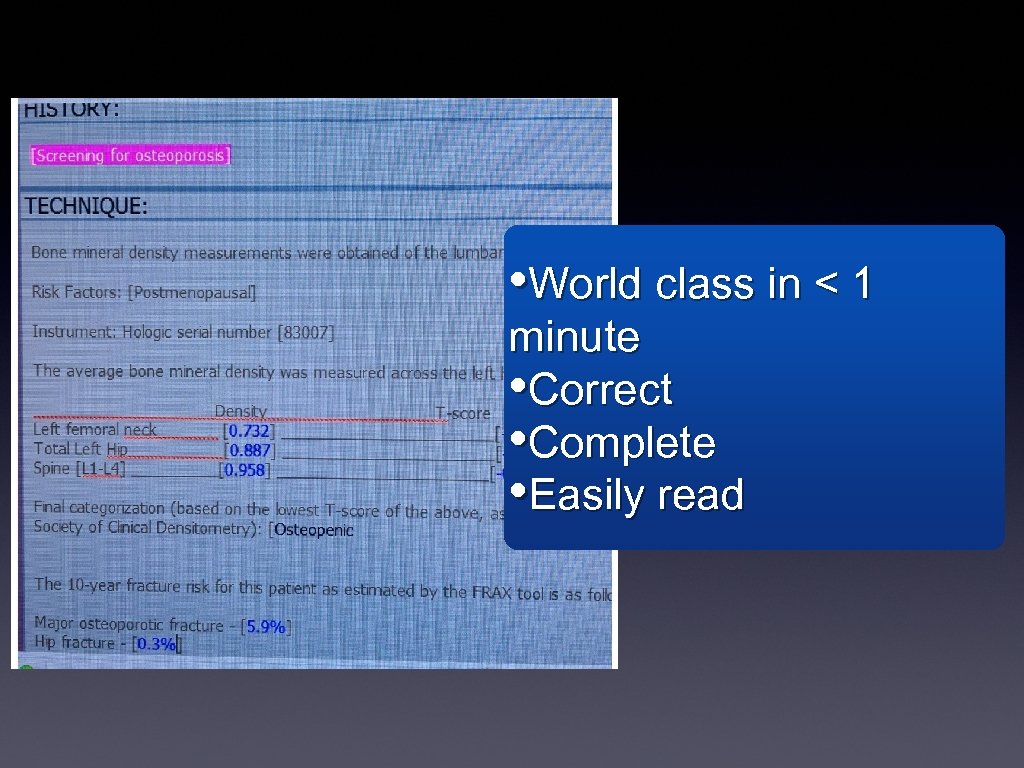
• World class in < 1 minute • Correct • Complete • Easily read
BUT WAIT THERE’S MORE You need to know: what should be reported and what should not be reported
What SHOULD be reported SPINE: • Report L 1 -L 4 - EXCEPT • any vertebrae affected by “structural change”: OR have > 1. 0 T - value difference from adjacent • Still - this is somewhat subjective • Must have at least 2 levels - cannot report single level • Totally fair to say the spine cannot be evaluated
What SHOULD be reported • Hip • Either will do • Only Total and neck, NOT Ward’s Triangle.
What SHOULD be reported Forearm: ONLY 1/3 radius value - no other is valid
What SHOULD be reported This is MOST important: Note the statistical significance of any possible change. % Change means nothing Saying “There is a statistically significant change from before” IS meaningful, and directs therapy appropriately
What Should NOT be reported • A WHO category for each level - • Only one category per patient • lowest category of • Fem Neck, Total Hip, spine.
Following the ISCD recommendations Difficulties 1) Fracture risk statement - (FRAX) Has the patient had a non-traumatic fracture ? ? ? ? Critically important, and generally, we don’t know 2) Recommendations for follow-up - best left to the clinician, I think
LSC • What is it? • “Least significant change” • The change in density that must be present to be 95% sure there is a “real” change. • It is a density (gm/cm 2) such as 0. 034. • It is not %, it is not T-score.
LSC • Can’t we use the LSC put in the machine by the company? • No • Why do they put those numbers in the report • I don’t know
LSC determination AKA: precision assessment • How do you measure it? • Each tech does 15 patients three times (three spines & three hips) • Plug results into ISCD spreadsheet. • Magically - the LSC pops out
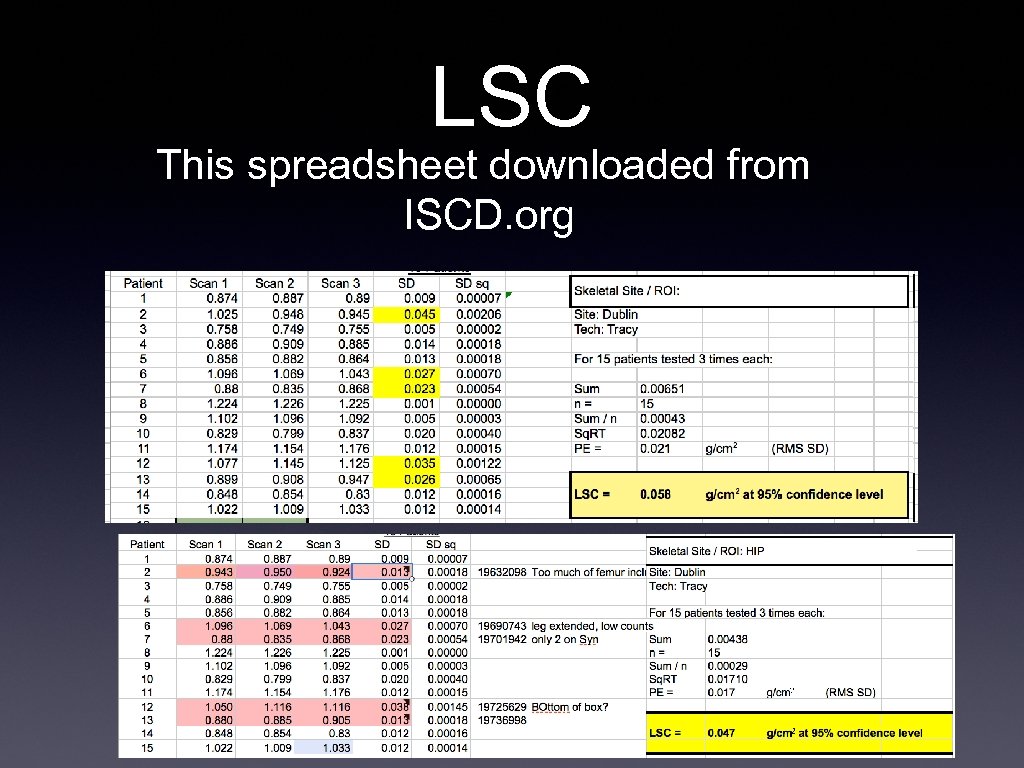
LSC This spreadsheet downloaded from ISCD. org
BUT WAIT! THREE EXAMS ON EACH PATIENT!!? ? !!! OH - THE RADIATION!!!!
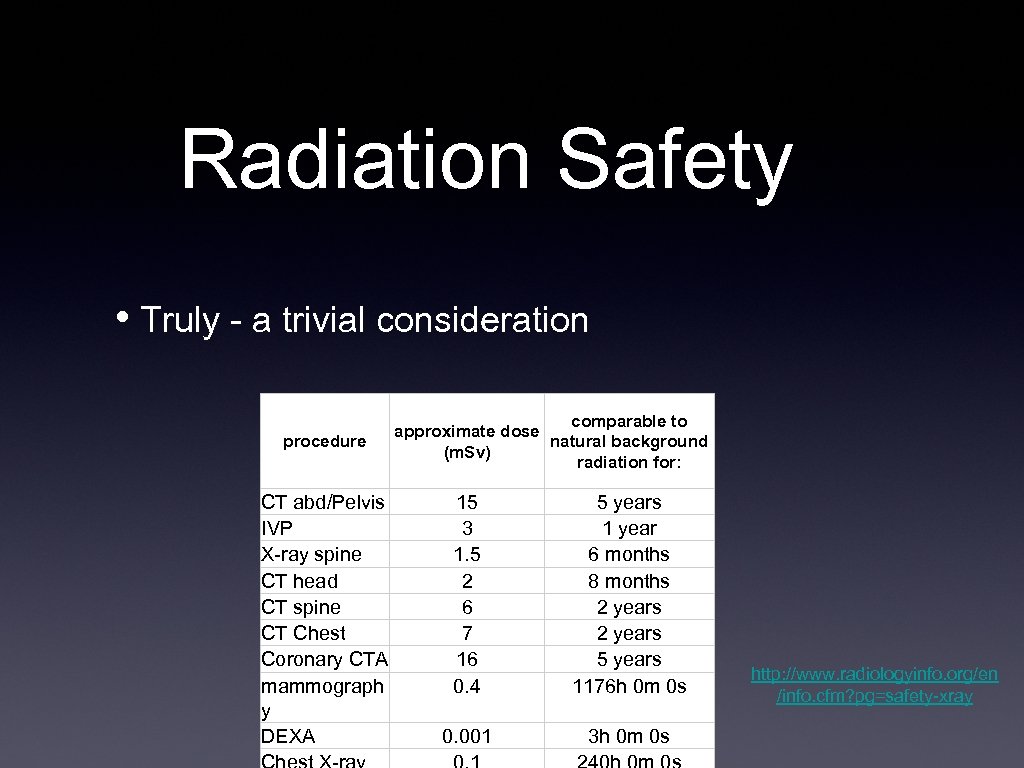
Radiation Safety • Truly - a trivial consideration procedure CT abd/Pelvis IVP X-ray spine CT head CT spine CT Chest Coronary CTA mammograph y DEXA comparable to approximate dose natural background (m. Sv) radiation for: 15 3 1. 5 2 6 7 16 0. 4 5 years 1 year 6 months 8 months 2 years 5 years 1176 h 0 m 0 s 0. 001 3 h 0 m 0 s http: //www. radiologyinfo. org/en /info. cfm? pg=safety-xray
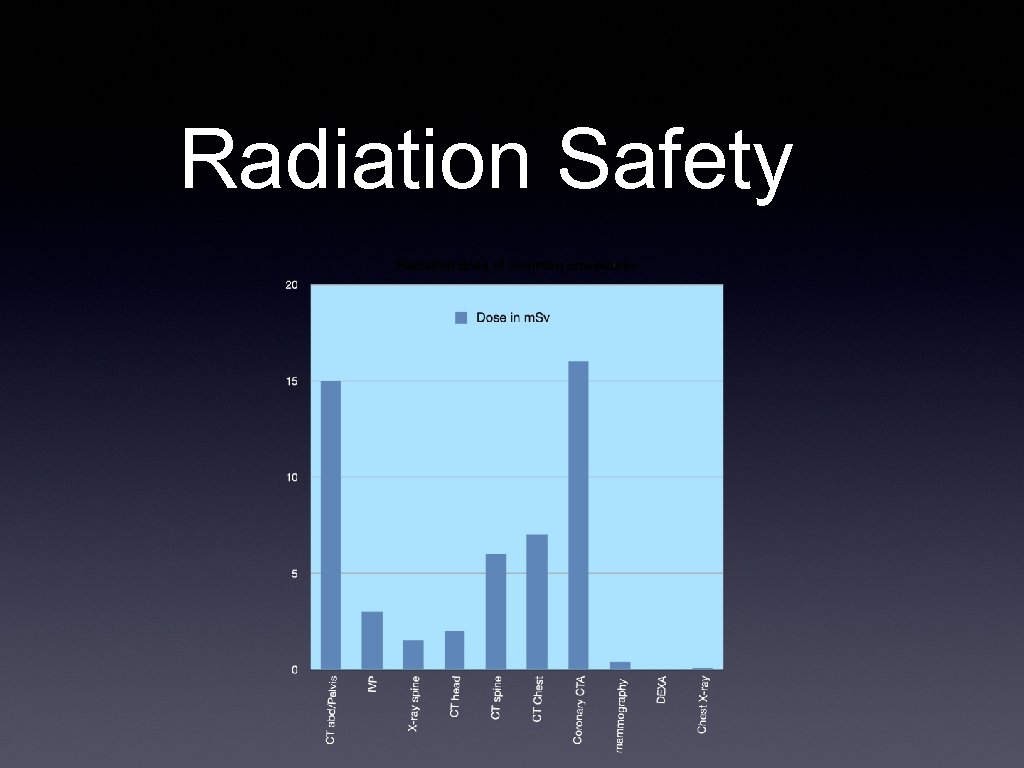
Radiation Safety
Radiation Safety one BED = 0. 036 m. Sv Therefore - a patient needs to have 36 DEXA’s to = one banana http: //en. wikipedia. org/wiki/Banana_e quivalent_dose)
LSC determination (AKA precision assessment) Precision assessment should be standard clinical practice. Precision assessment is not research and may potentially benefit patients. It should not require approval of an institutional review board. Adherence to local radiologic safety regulations is necessary. Performance of a precision assessment requires the consent of participating patients.
LSC determination (AKA precision assessment ISCD verbiage for patient consent: To find out if there has been a change in your bone density, a recent bone density test is compared with a previous test. For an accurate comparison, we must know when the change is greater than the normal day-to-day fluctuation in the measurement itself. This is done by doing mathematical calculations on repeat bone density measurements of the same person made on the same day. This is called a “precision assessment. ” You have been asked to participate in a precision assessment. You will have your bone density measured again at the [spine and hip] [spine, hip, and forearm]. After the first scan you will need to get off the table and then back on for the additional scan(s). The X-ray exposure involved in this is exceedingly small – typically less than the normal radiation all of us are exposed to on a daily basis. Nevertheless, you should not participate if you think you might be pregnant. Participation is up to you. If you do not wish to participate, it will have no effect on your future treatment or benefits at [clinic name].
FRAX • Fracture risk assessment tool. • EXTENSIVELY validated. • Available in most systems (for an additional charge) • Available online for free • Uses historical risk factors and neck density • Calculates % chance of fracture of spine, hip for 10 years. • Utility: Combines significant risk factors AND bone density into a single estimate which is used to determine when to treat • USING T-scores ALONE TO DECIDE TO TREAT IS ARCHAIC
FRAX • Useful for untreated patients with “low bone mass” (osteopenic) • Not valid in: • normals • Osteoporosis (T < -2. 5) • “treated” patients - i. e bisphonates or Denusomab • Doesn’t mean Calcium
Bugaboos i. e. things you run across daily that are not well defined. 1) Unusual variations of density in the spine which may or may not be explained by the images
Bugaboos i. e. things you run across daily that are not well defined. Spine and hips are different - One area “osteopenic”, one “osteoporotic” Not much of a problem - report the lesser
Bugaboos i. e. things you run across daily that are not well defined. Discrepant changes - Significant change in one area, not in another Or - worse Significant changes in opposite directions

Bugaboos i. e. things you run across daily that are not well defined. Comparing fewer than 4 spinal levels - LSC determined based on 4 - using fewer means: less statistical power - You SHOULD have a different LSC for 2, 3, and 4 levels, but that is not done - simply use the one LSC
Bugaboos i. e. things you run across daily that are not well defined. Using the radius: ISCD does not recommend calculating LSC for radius, and it is not done generally SO - how do you judge change?
Common Errors • Reports aren’t ISCD compliant • Rules for exclusion/inclusion of vertebral levels not followed • Statistical significance of change ignored • Inattention to the images (numbers only reported - on autopilot) • poor region definition (especially: Hip)
Sample cases
CASE 1

CASE 2 Do You: Exclude L 1/L 2? Exclude L 3?
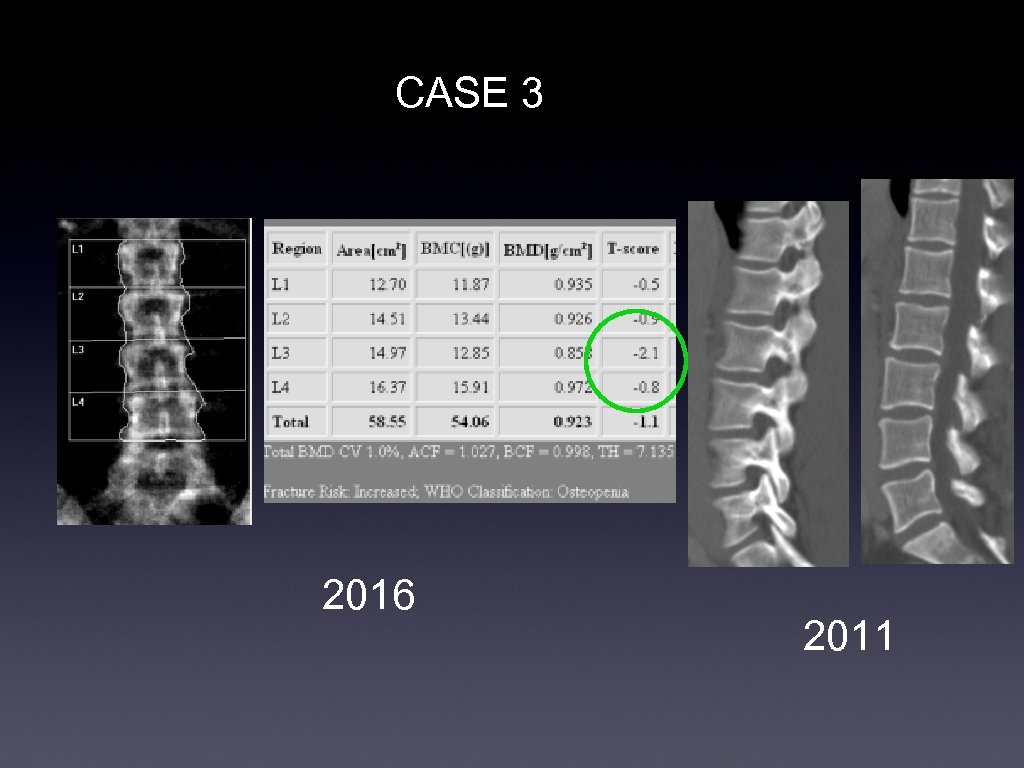
CASE 3 2016 2011
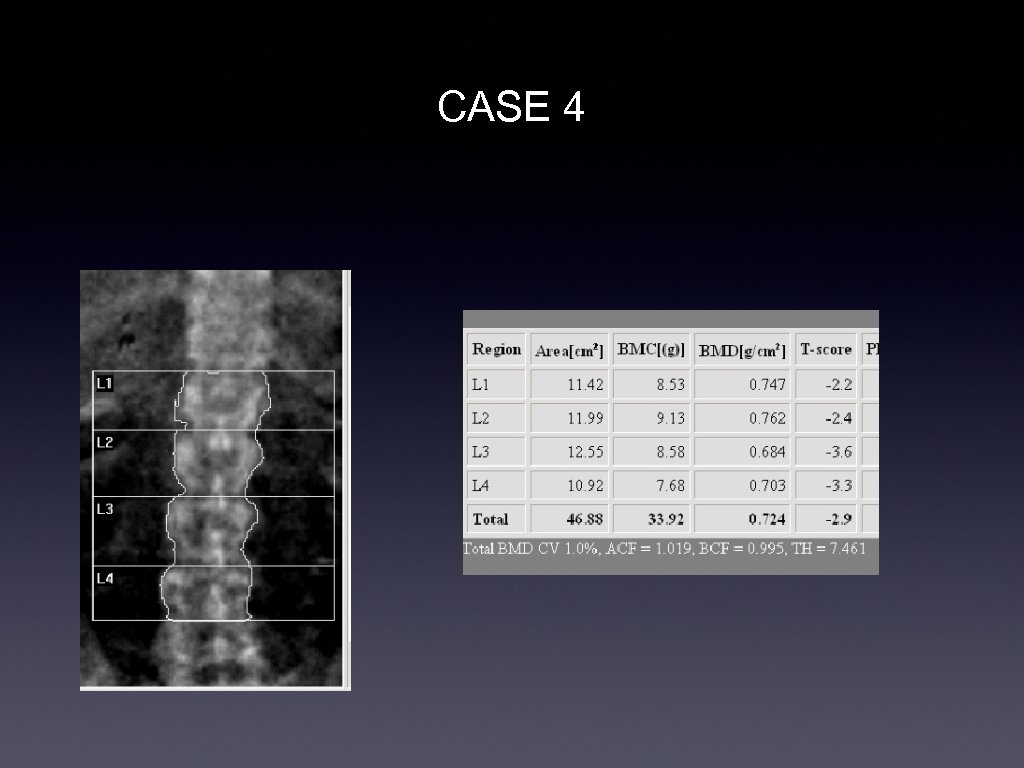
CASE 4
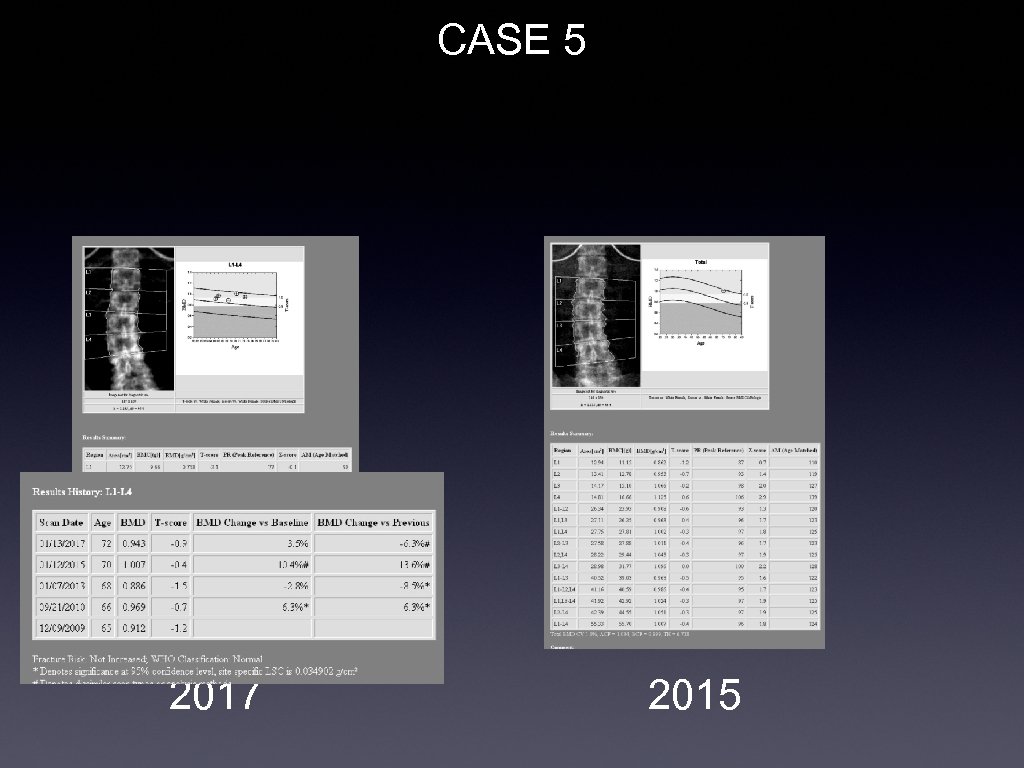
CASE 5 2017 2015
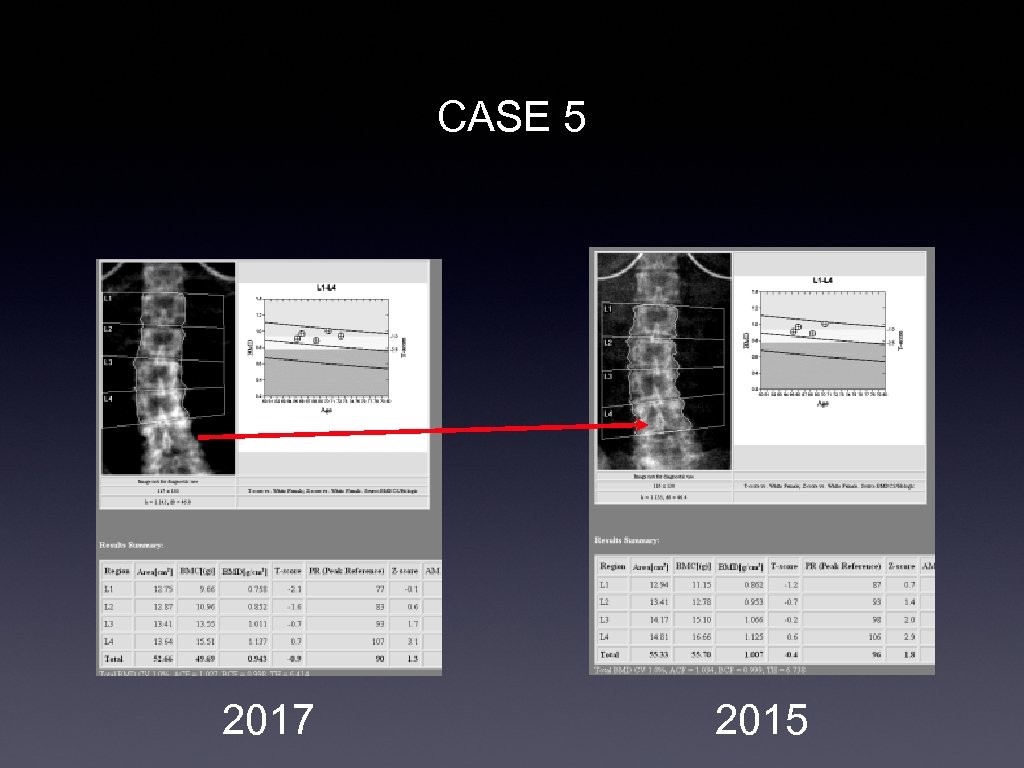
CASE 5 2017 2015

CASE 7
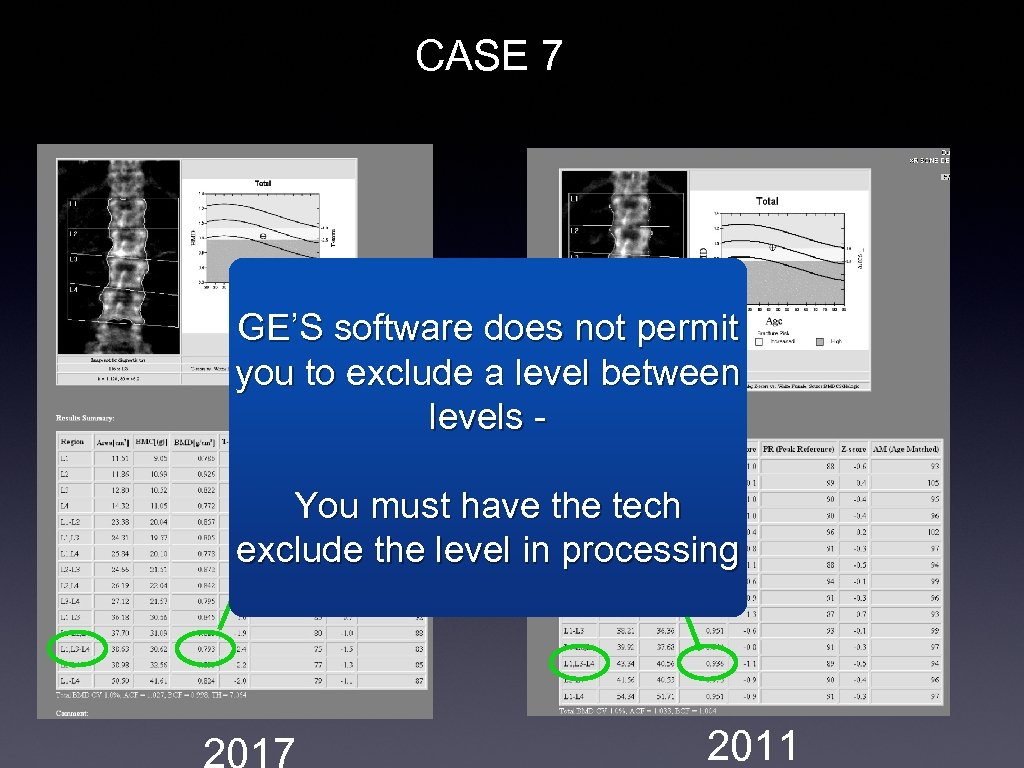
CASE 7 GE’S software does not permit 2017 - 0. 793 you to exclude a level between 2011 - 0. 936 levels - Diff: 0. 143 You must have the tech LSC = 0. 0349 exclude the level in processing 2011
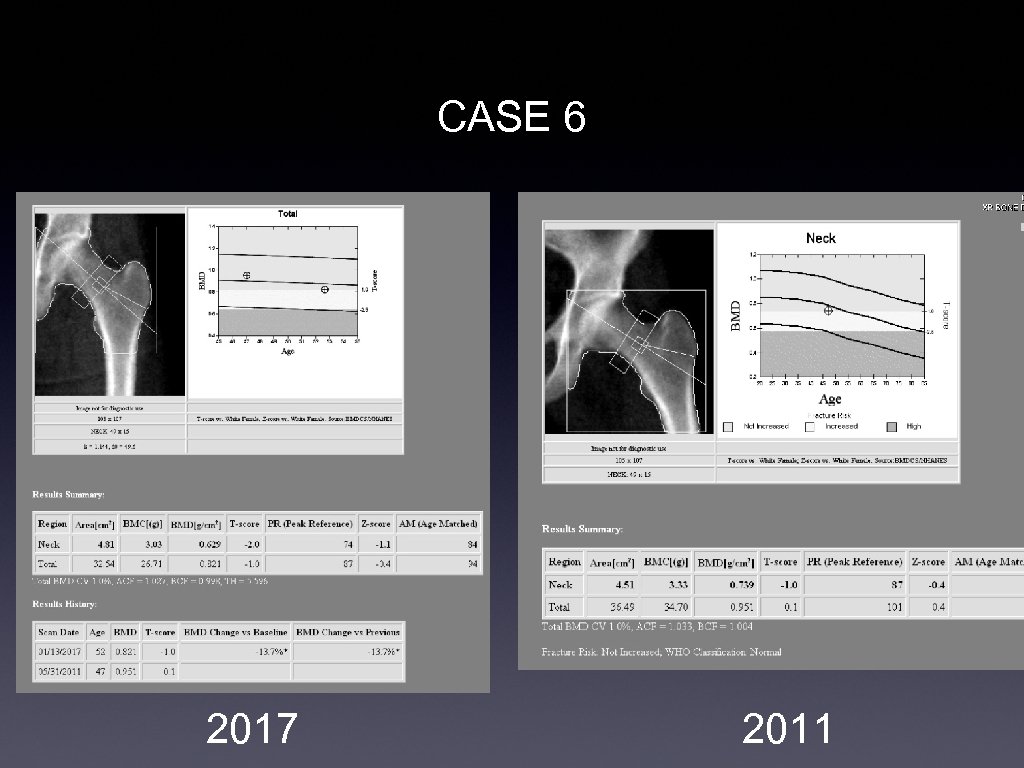
CASE 6 2017 2011
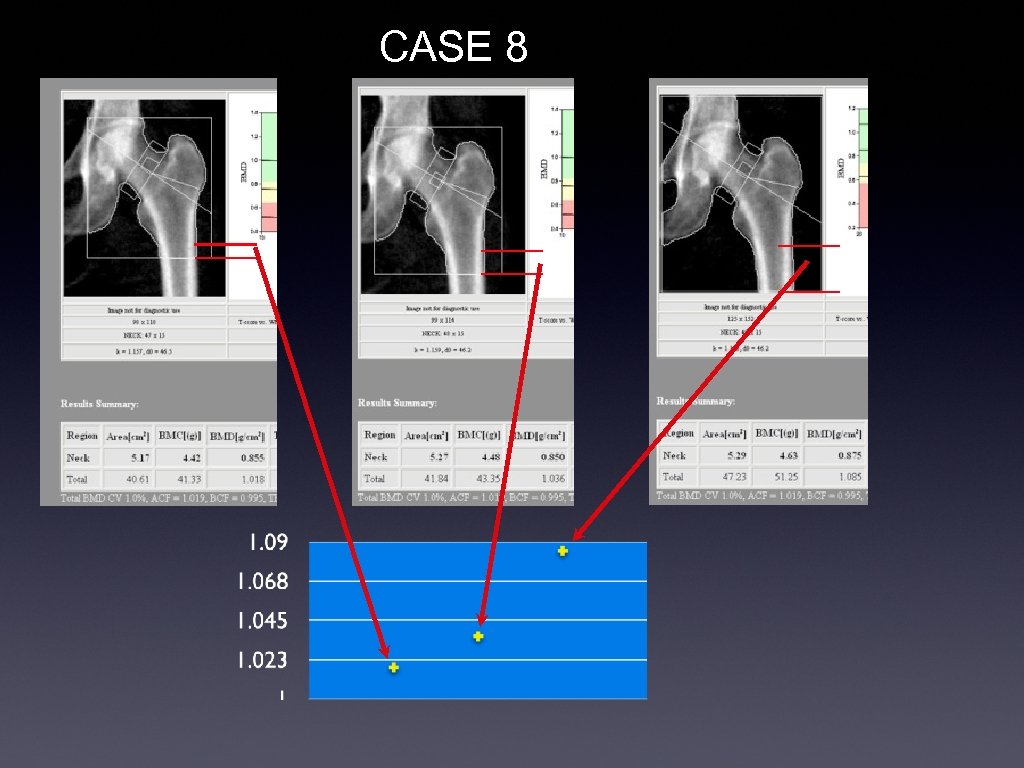
CASE 8
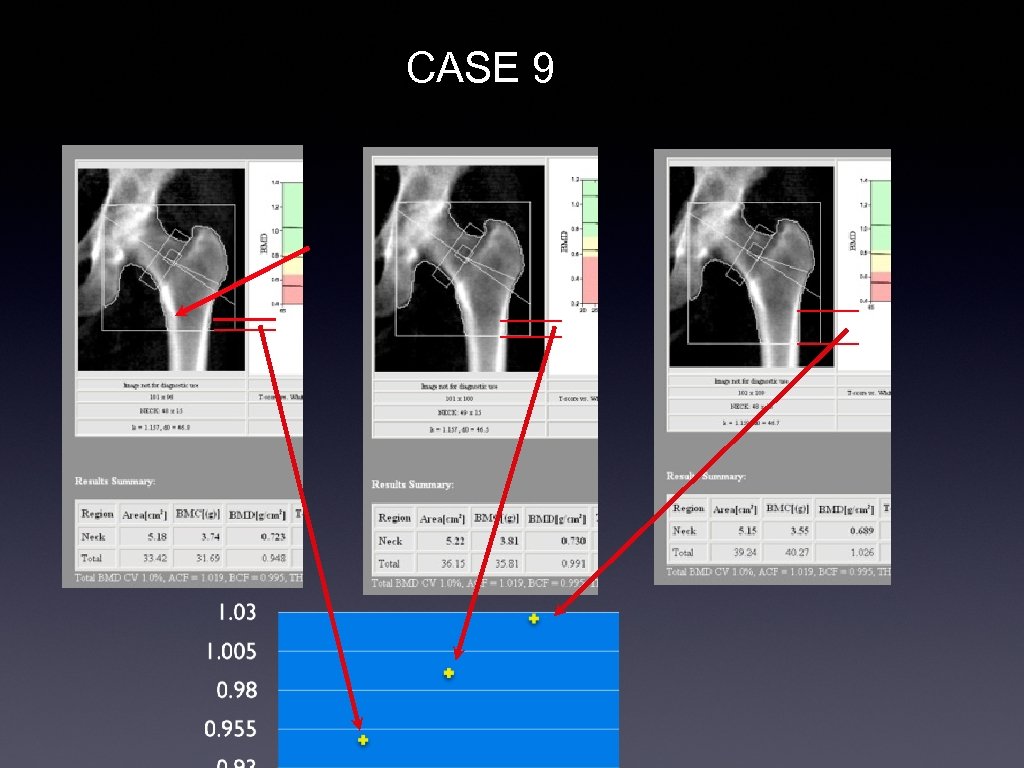
CASE 9
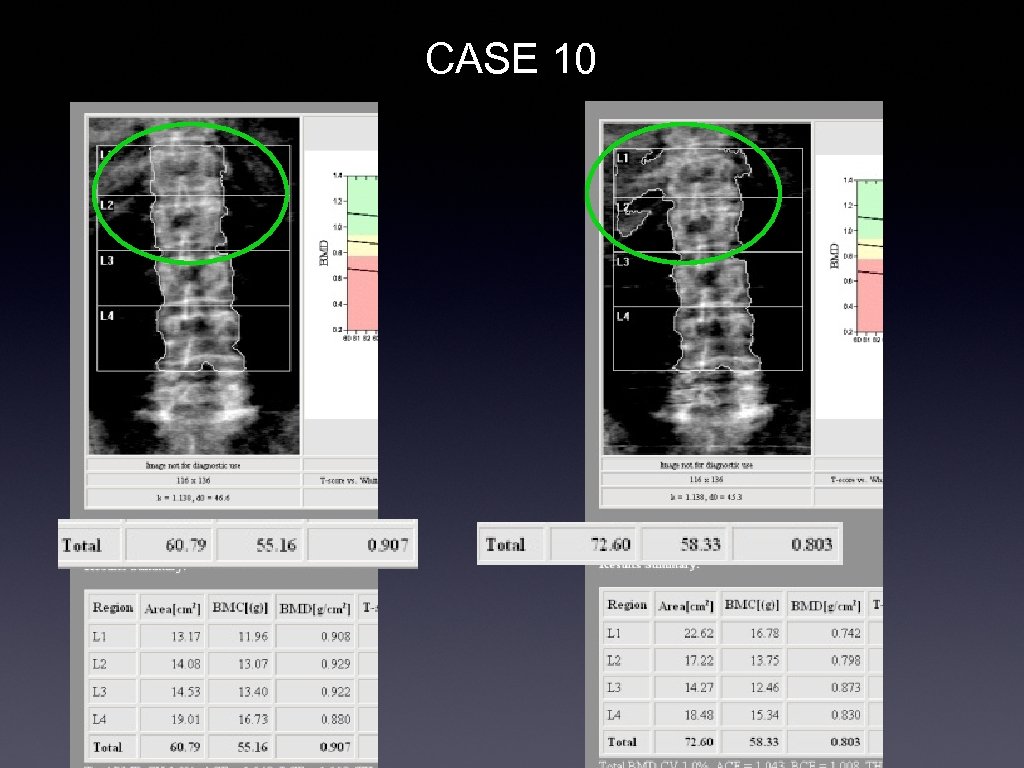
CASE 10
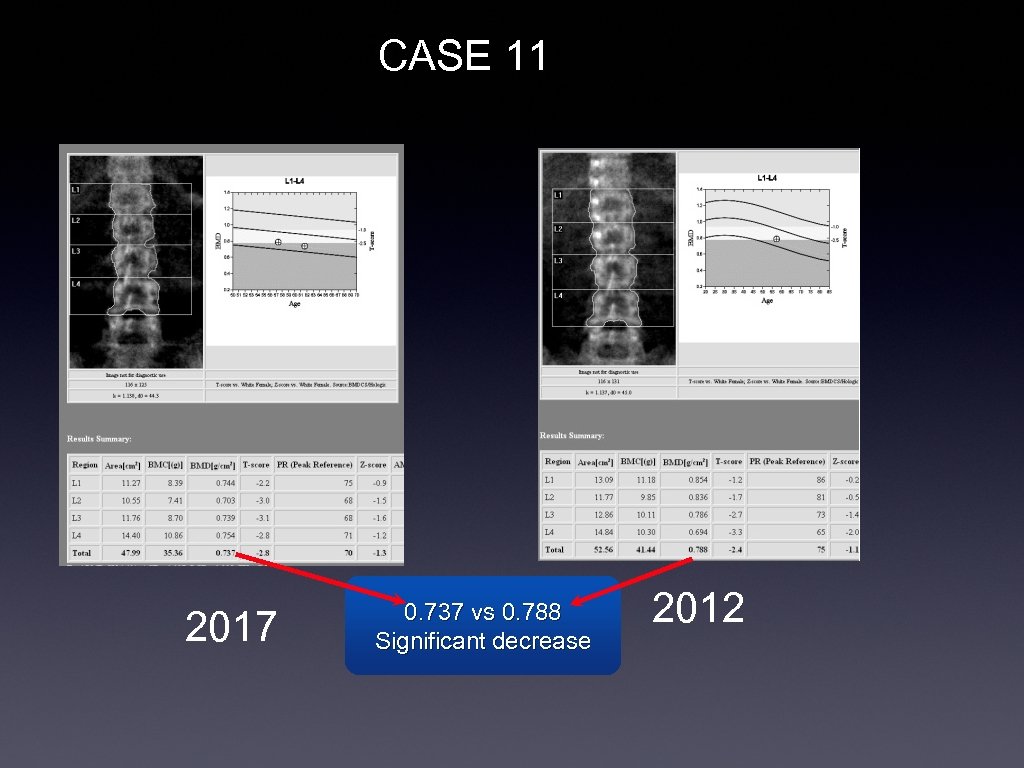
CASE 11 2017 0. 737 vs 0. 788 Significant decrease 2012
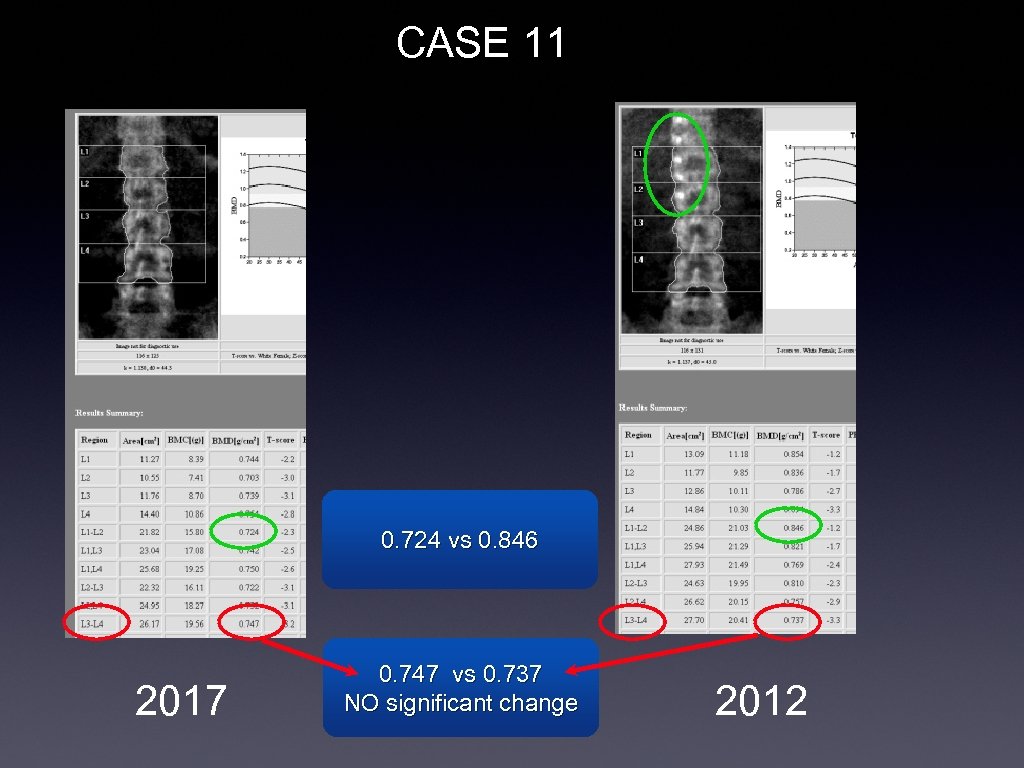
CASE 11 0. 724 vs 0. 846 2017 0. 747 vs 0. 737 NO significant change 2012
Summary • Osteoporosis treatment is: • cheap, effective, and lifesaving • DXA determines • who should be treated • the effectiveness of treatment
Summary (2) • DXA reporting is : • A hazard to your professional image (if not done properly) • Easy to learn • only four or five things to learn to do it perfectly • Easy to do perfectly with templates
References • ISCD guidelines: • http: //www. iscd. org/official-positions/6 th -iscd-position-development-conferenceadult/ • Outlines the rules for reporting in one pamphlet. • FRAX calculation: • http: //www. shef. ac. uk/FRAX/
63fc211c63ff569e280cf1ee8896cf82.ppt