bda4f6d6f5029716bfde70dae5c52381.ppt
- Количество слайдов: 88
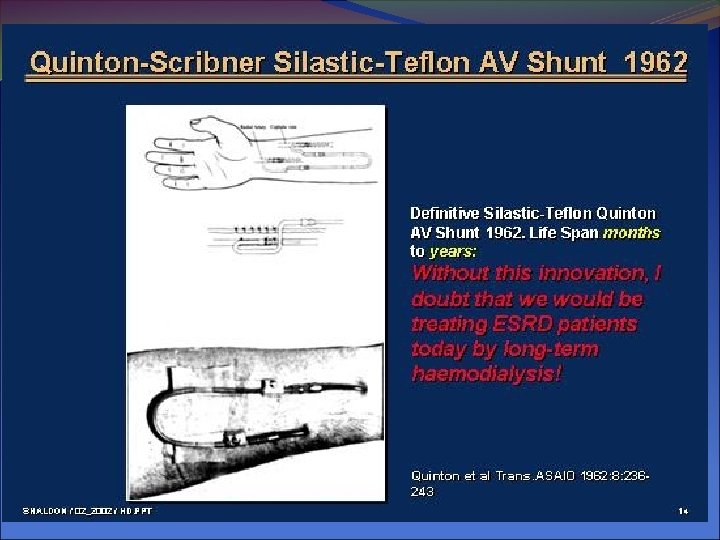
Basics Concepts Of Dialysis Naveed Aslam, MD Consultant & clinical tutor Department of Nephrology PSMMC
Outline Introduction Indications Modalities Access Apparatus Complications of dialysis access Acute complications of dialysis
Functions of Kidneys Excretory Homeostatic Endocrine Metabolic
Functions of Kidneys Fluid Balance Electrolyte Balance---Na—K---H Acid base Balance Excretion of waste products of Metabolism and Drugs Hormonal Secretion Epo—Renin—Active Vit D---D 3
Indications to initiate dialysis Diabetics: Creatinine clearance is < 15 m. L/min • Non-diabetics: creatinine clearance < 10 ml/min •
Additional Indications Symptoms • • • Pericarditis Uncontrollable fluid overload Pulmonary edema Uncontrollable and repeated hyperkalemia Coma Lethargy Less Severe Symptoms • • Azotemia Nausea Vomiting
Dialysis Definition Artificial process that partially replaces renal function Removes waste products from blood by diffusion (toxin clearance) Removes excess water by ultrafiltration (maintenance of fluid balance) Wastes and water pass into a special liquid – dialysis fluid or dialysate
Main Goals of Dialysis Remove Fluid Waste Products Urea Creatinine Potassium Phosphorous Sodium Maintain Fluid Electrolyte Acid-base balance
Therapeutic Modalities • Hemodialysis • In center dialysis • Home hemodialysis • In center nocturnal dialysis • Peritoneal Dialysis • Continuous ambulatory peritoneal dialysis • Continuous cycling peritoneal dialysis
Selection for HD/PD Clinical condition Lifestyle Patient competence/hygiene (PD - high risk of infection) Affordability / Availability
What we need for hemodialysis Access - Arteriovenous Fistula - Arteriovenous Graft - Central Venous Catheter Membane Dialysis Machine Dialysate
Dialysis Health Care Team • • • Patient Dialysis Nurse Dialysis Technician Nephrologist Nephrology Social Worker Renal Dietitian
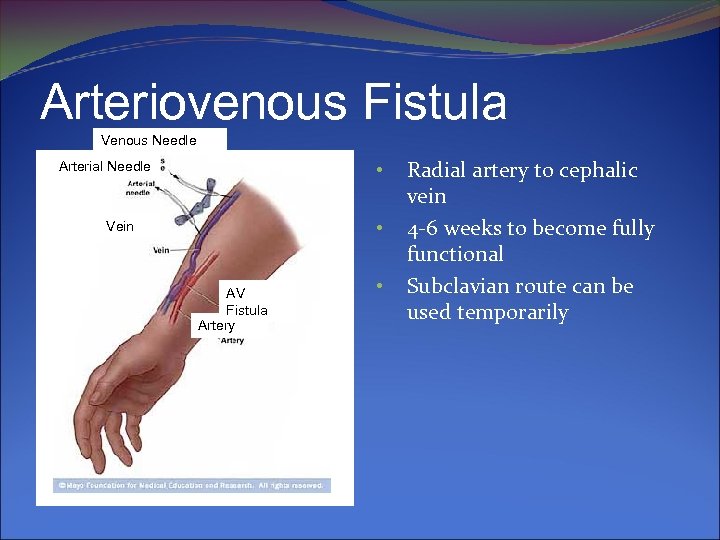
Arteriovenous Fistula Venous Needle • Arterial Needle • Vein AV Fistula Artery • Radial artery to cephalic vein 4 -6 weeks to become fully functional Subclavian route can be used temporarily

AV Fistula
Internal Arteriovenous Graft (AVG) Primary used in CRF & elderly Synthetic graft which provides a bridge between the artery and vein Needs 3 -6 weeks to heal prior to use Advantages: Decreased risk of bleeding Can be used indefinitely No dressing Allows freedom of movement
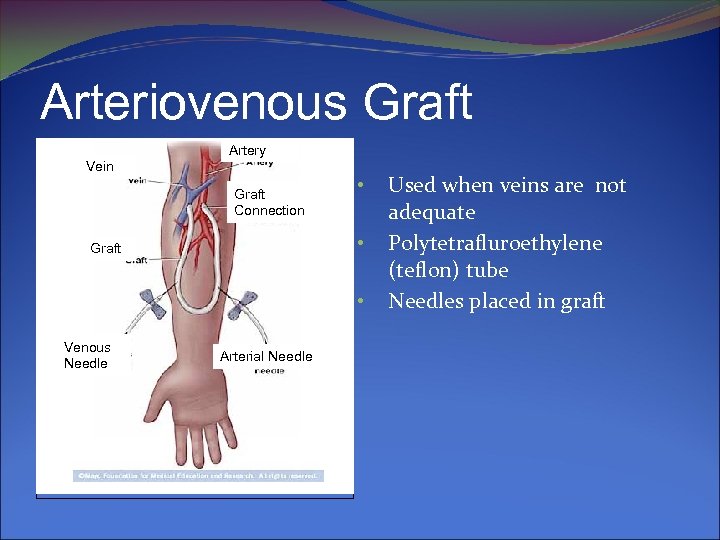
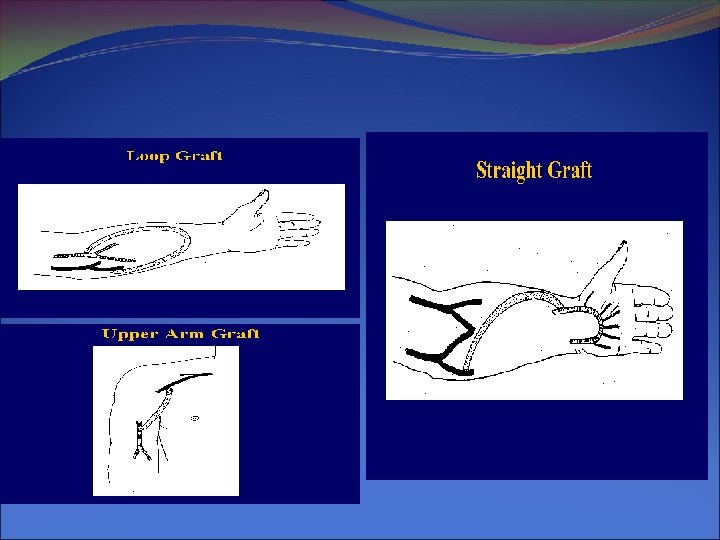
Arteriovenous Graft Artery Vein Graft Connection • • Graft • Venous Needle Arterial Needle Used when veins are not adequate Polytetrafluroethylene (teflon) tube Needles placed in graft

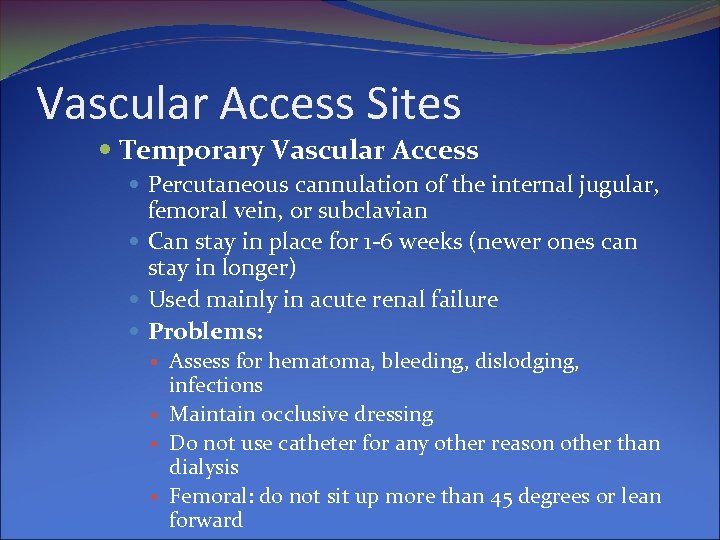
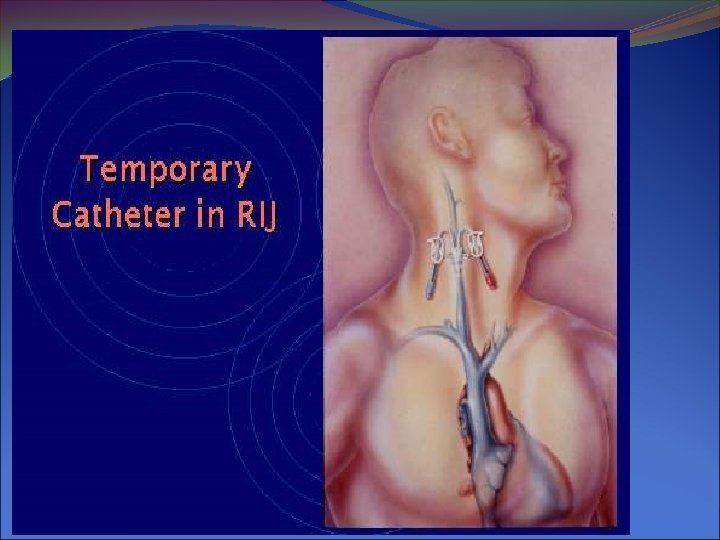
Vascular Access Sites Temporary Vascular Access Percutaneous cannulation of the internal jugular, femoral vein, or subclavian Can stay in place for 1 -6 weeks (newer ones can stay in longer) Used mainly in acute renal failure Problems: Assess for hematoma, bleeding, dislodging, infections Maintain occlusive dressing Do not use catheter for any other reason other than dialysis Femoral: do not sit up more than 45 degrees or lean forward
Vascular Access Double lumen catheter • Catheter able to provide sufficient blood flow • 11 French and greater • Avoid kinking • Secure connections, make them visible • Right size at the right place
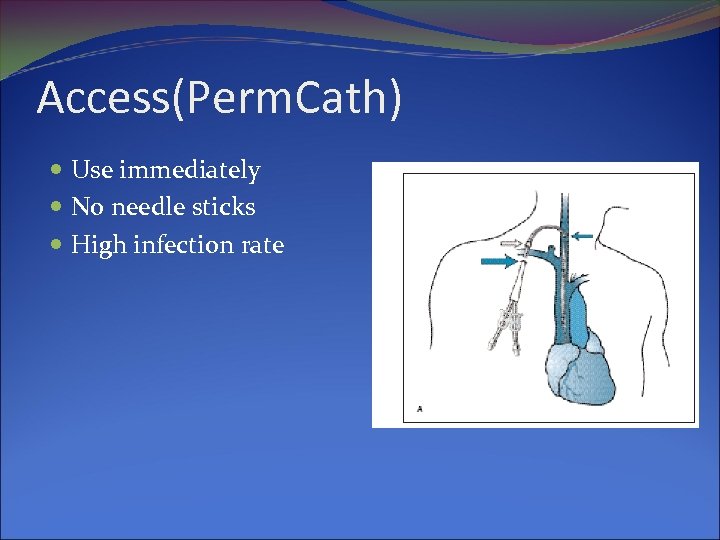
Access(Perm. Cath) Use immediately No needle sticks High infection rate
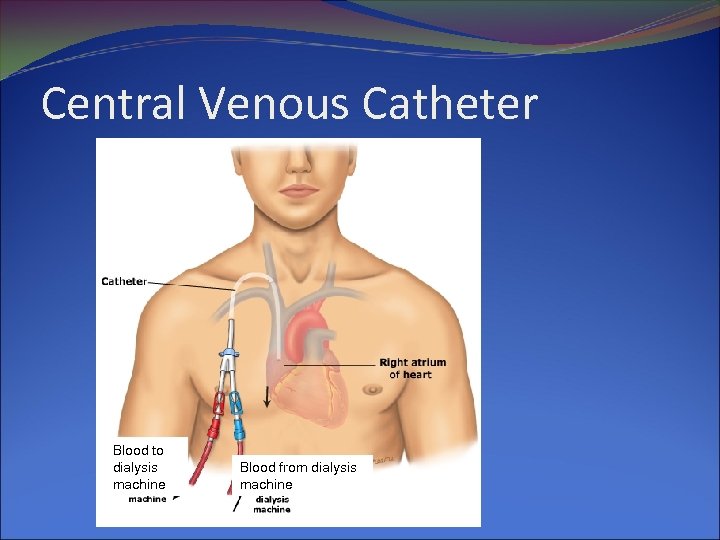
Central Venous Catheter Blood to dialysis machine Blood from dialysis machine
Recirculation Access recirculation may limit clearances IJC= 1 -2% Subclavian 4. 1% Femoral 13. 5 cm - 22. 8% Femoral 19. 5 cm - 12. 6% (@Blood flow 300 ml/min) More problematic in IHD than CRRT Kelber J et al. Am J Kidney Dis 1993; 22: 24 -29. Leblanc M et al. J Am Soc Nephrol 1995; 5: 496.
Hemodialysis Waste products filtered from blood by a semipermeable membrane and removed by the dialysis fluid, or dialysate. • In-center: 4 hours, 3 days a week • Home: may be daily • Nocturnal In-center: 6 -8 hours, 3 nights/week •
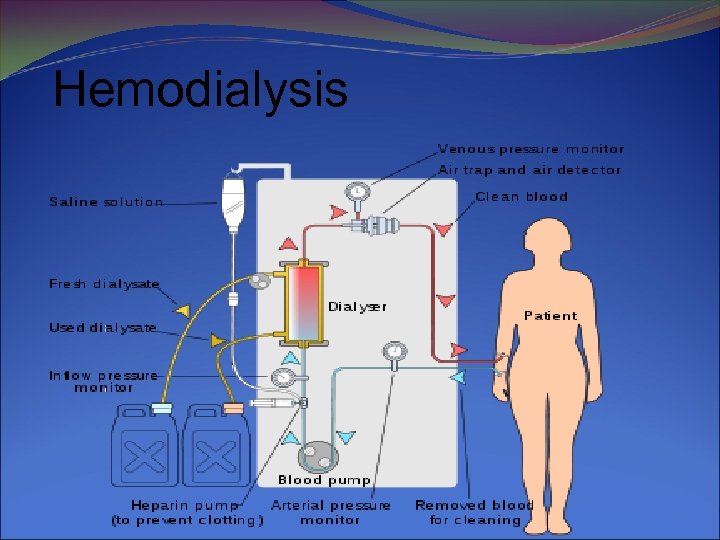
Hemodialysis
Acute Complications of Dialysis Hypotension (25 -55%) Cramps (5 -20%) Nausea and vomiting (5 -15%) Headache (5%) Chest pain (2 -5%) Back pain (2 -5%) Itching (5%) Fever and chills (<1%)
Effects of HD on Lifestyle Flexibility: Difficult to fit in with school, work esp if unit is far from home. Home HD offers more flexibility Travel: Necessity to book in advance with HD unit of places of travel Responsibility & Independence: Home HD allows the greatest degree of independence Sexual Activity: Anxiety of living with renal failure affects relationship with partner Sport & Exercise: Can exercise and participate in most sports Body Image: Esp with fistula; patient can be very self conscious about it
Problems with HD Rapid changes in BP fainting, vomiting, cramps, chest pain, irritability, fatigue, temporary loss of vision Fluid overload esp in between sessions Fluid restrictions more stringent with HD than PD Hyperkalaemia esp in between sessions Loss of independence Problems with access poor quality, blockage etc. Infection (vascular access catheters) Pain with needles Bleeding from the fistula during or after dialysis Infections during sessions; exit site infections; blood-borne viruses e. g. Hepatitis, HIV
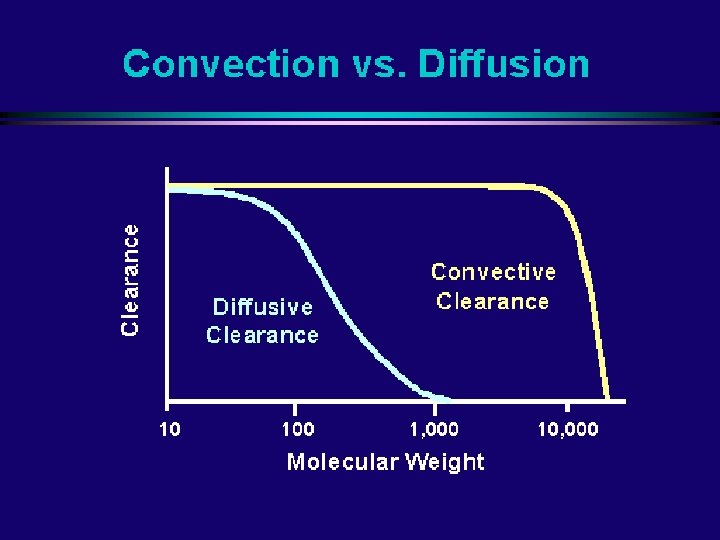
Removal of Toxins: Diffusion Depends on Concentration gradient across the membrane
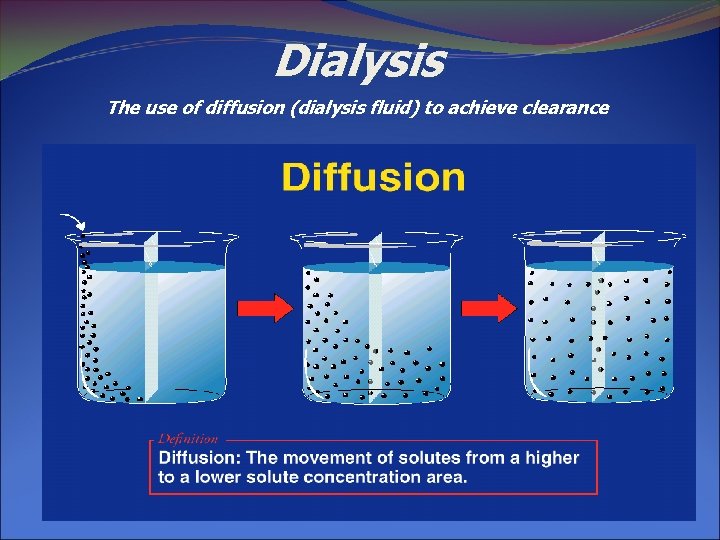
Dialysis The use of diffusion (dialysis fluid) to achieve clearance
Thomas Graham (1805 -1869)
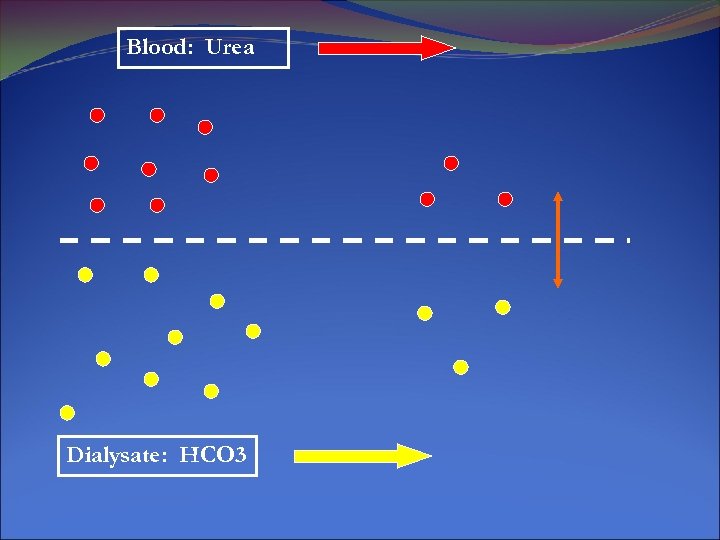
Blood: Urea Dialysate: HCO 3
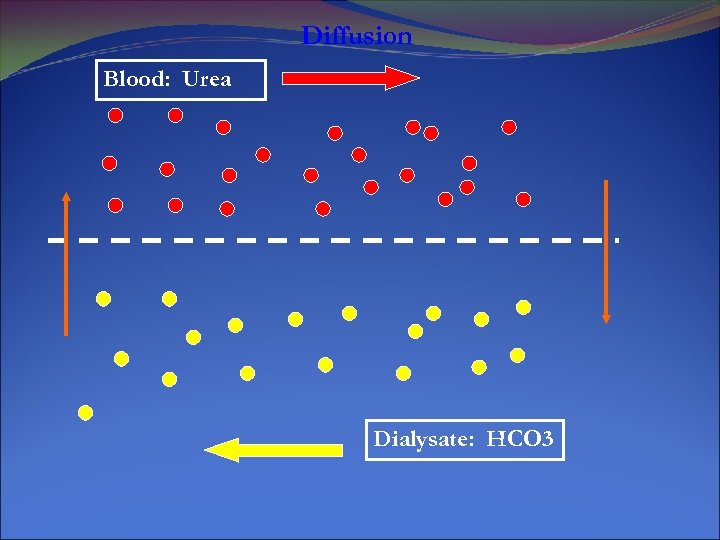
Diffusion Blood: Urea Dialysate: HCO 3
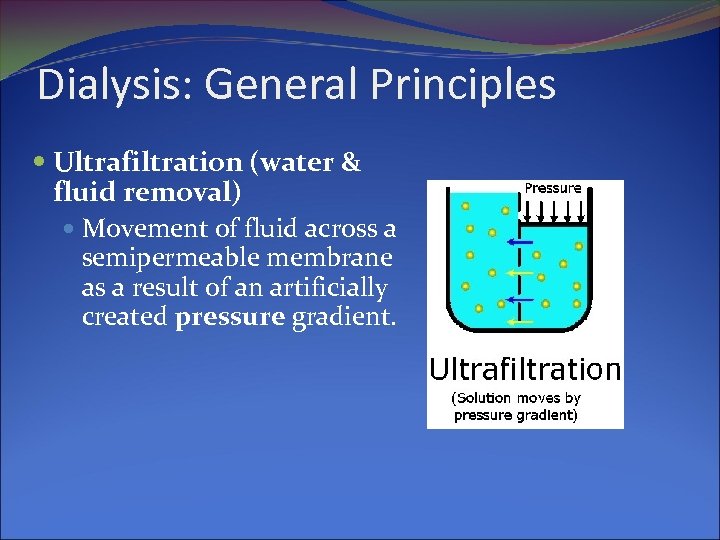
Dialysis: General Principles Ultrafiltration (water & fluid removal) Movement of fluid across a semipermeable membrane as a result of an artificially created pressure gradient.
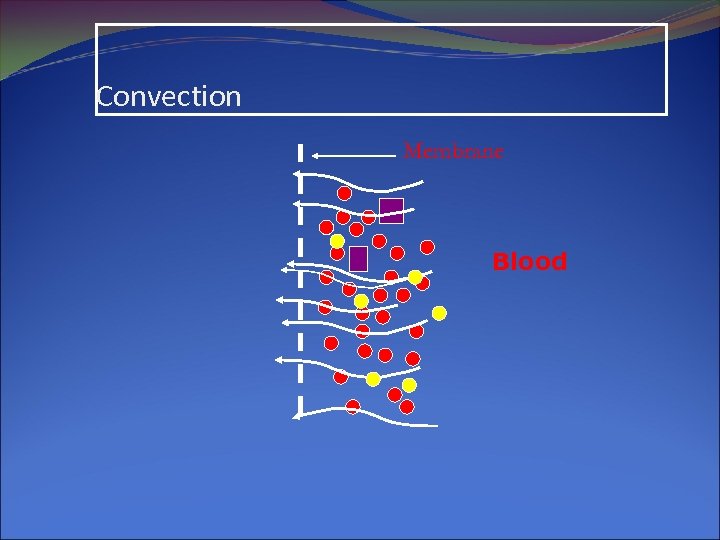
Convection Membrane Blood
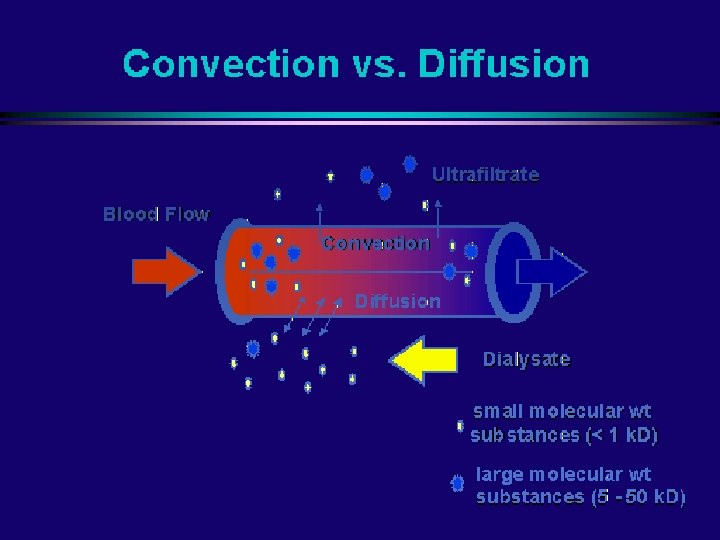
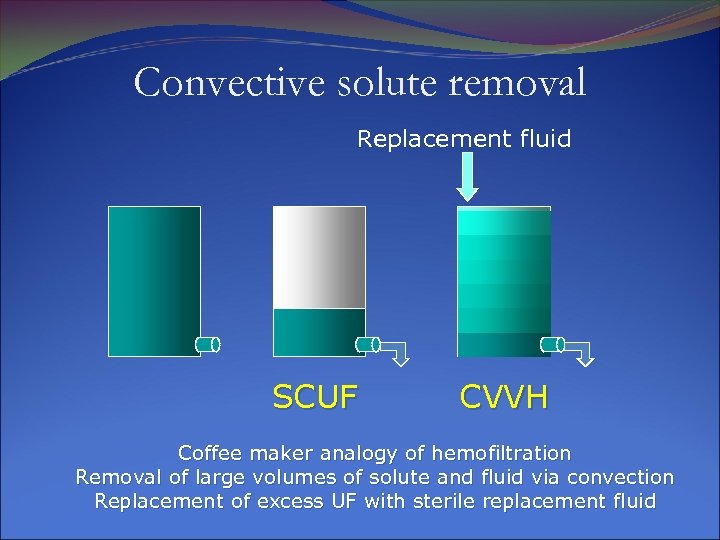
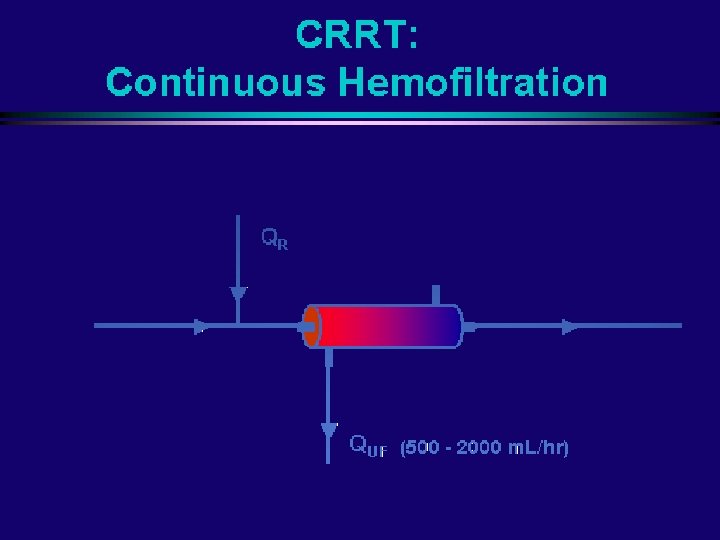
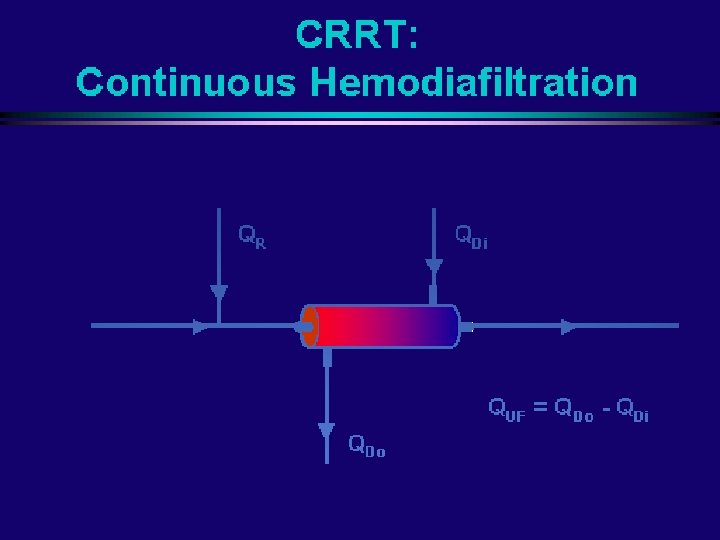
Convective solute removal Replacement fluid SCUF CVVH Coffee maker analogy of hemofiltration Removal of large volumes of solute and fluid via convection Replacement of excess UF with sterile replacement fluid
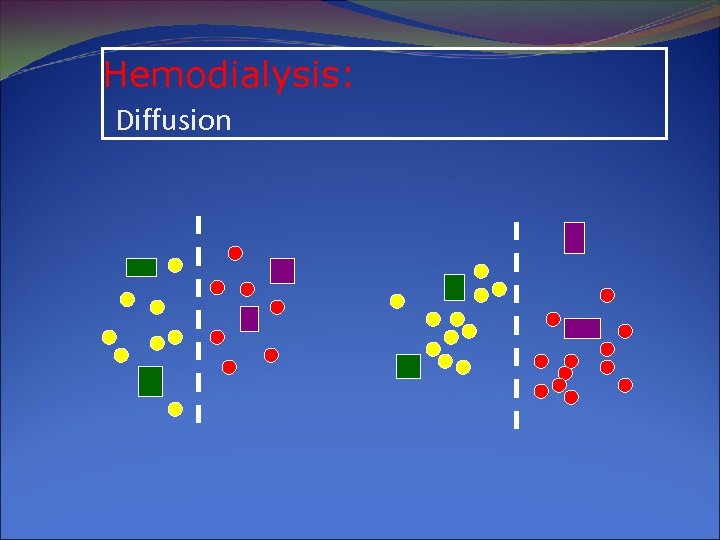
Hemodialysis: Diffusion
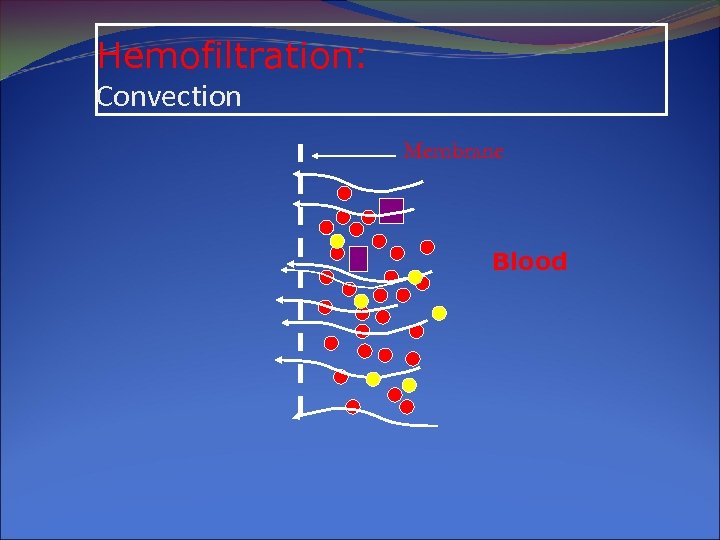
Hemofiltration: Convection Membrane Blood
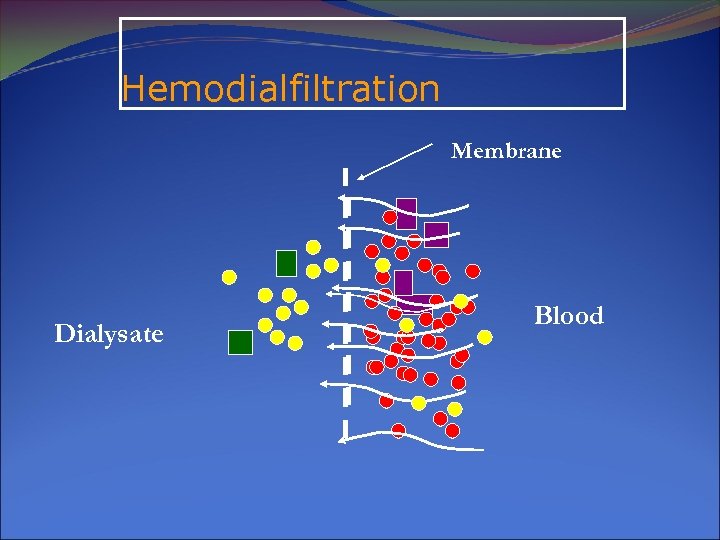
Hemodialfiltration Membrane Dialysate Blood
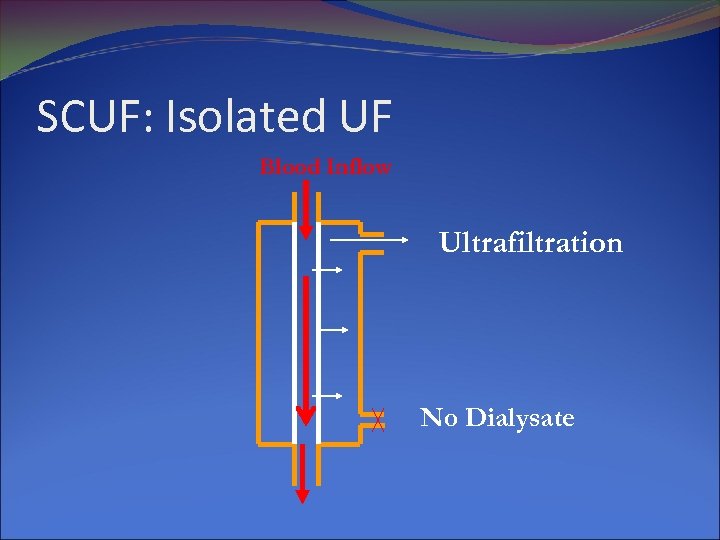
SCUF: Isolated UF Blood Inflow Ultrafiltration No Dialysate
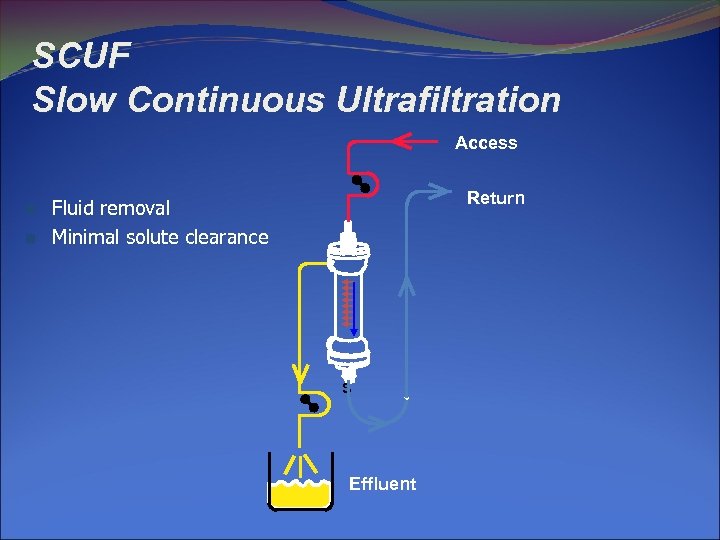
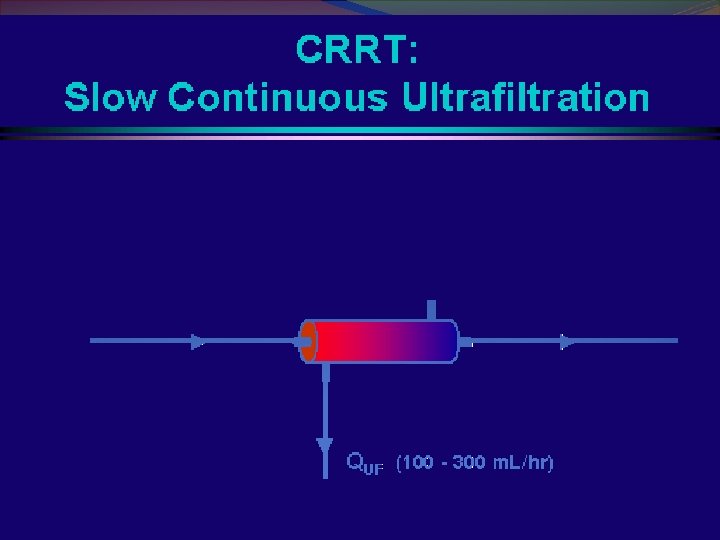
SCUF Slow Continuous Ultrafiltration Access n n Return Fluid removal Minimal solute clearance S Effluent
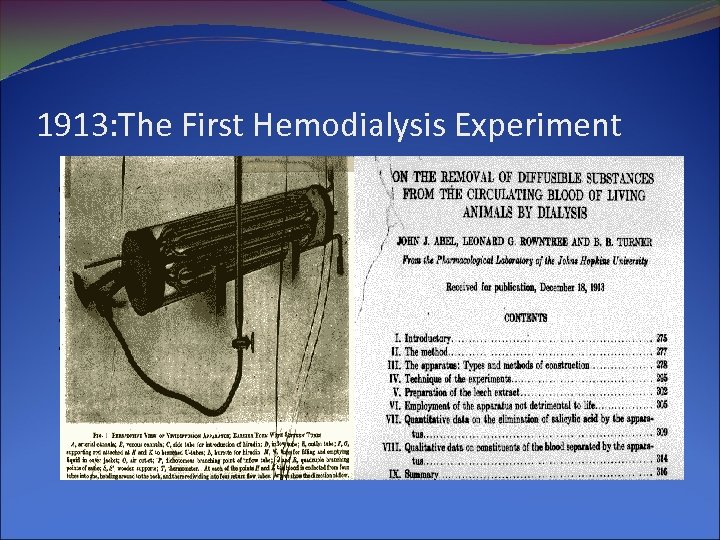
1913: The First Hemodialysis Experiment
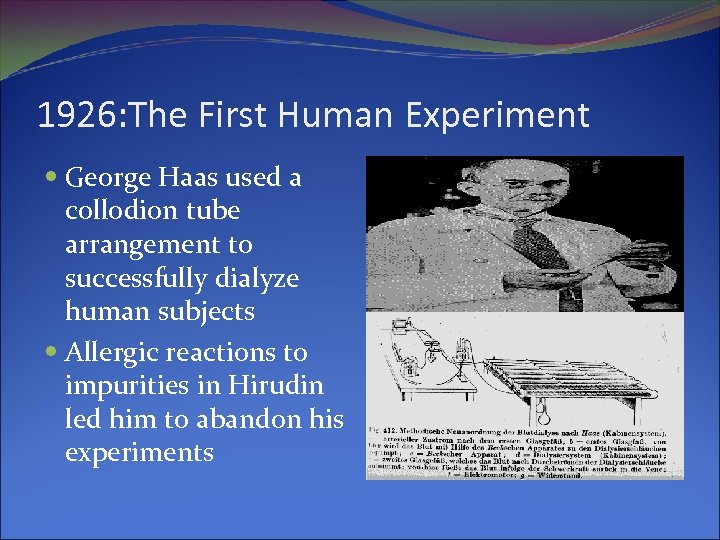
1926: The First Human Experiment George Haas used a collodion tube arrangement to successfully dialyze human subjects Allergic reactions to impurities in Hirudin led him to abandon his experiments
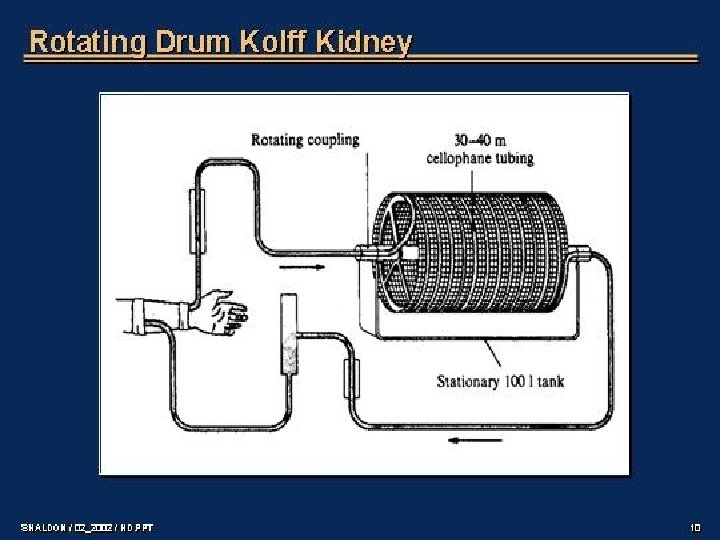
Dialyzer used by Kolf: 1943
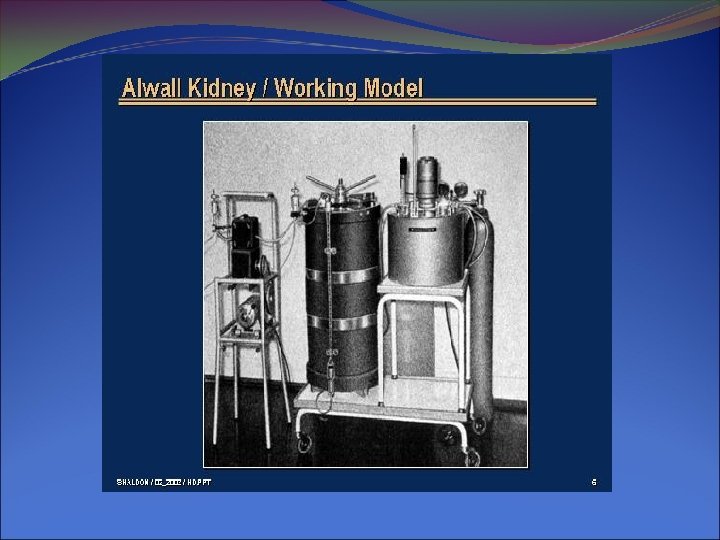
1937: Nils Alwall used the Alwall Kidney to perform the first ever hemodialysis treatment at the university of Lund, Sweden
Today's Filters
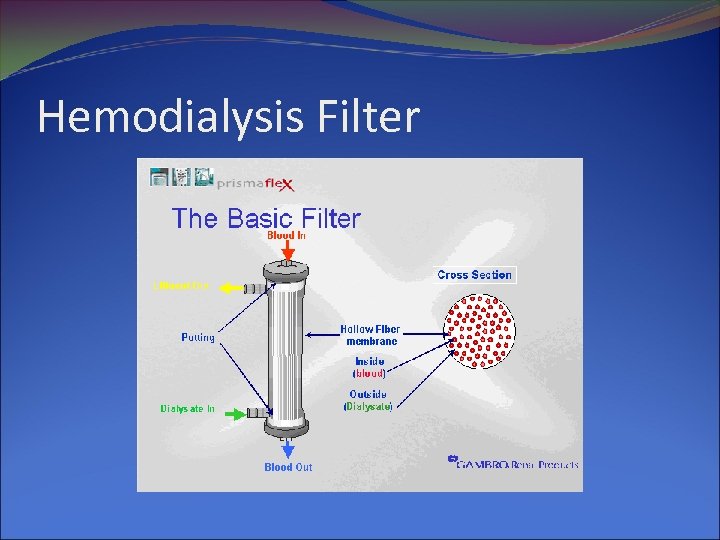
Hemodialysis Filter
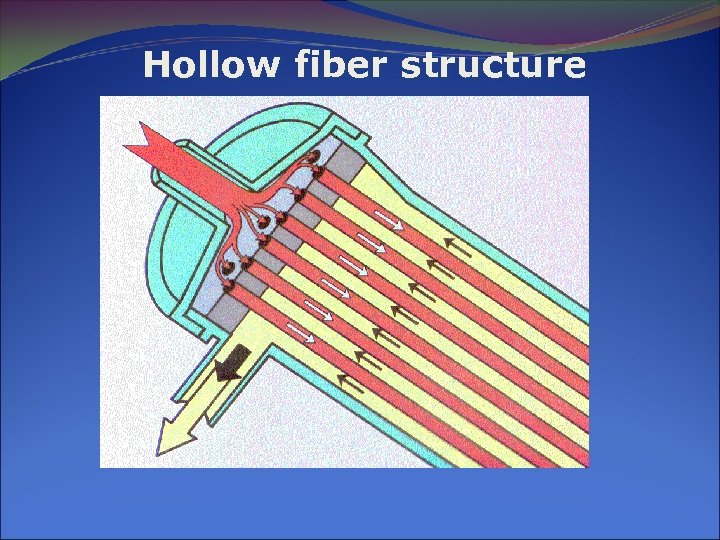
Hollow fiber structure
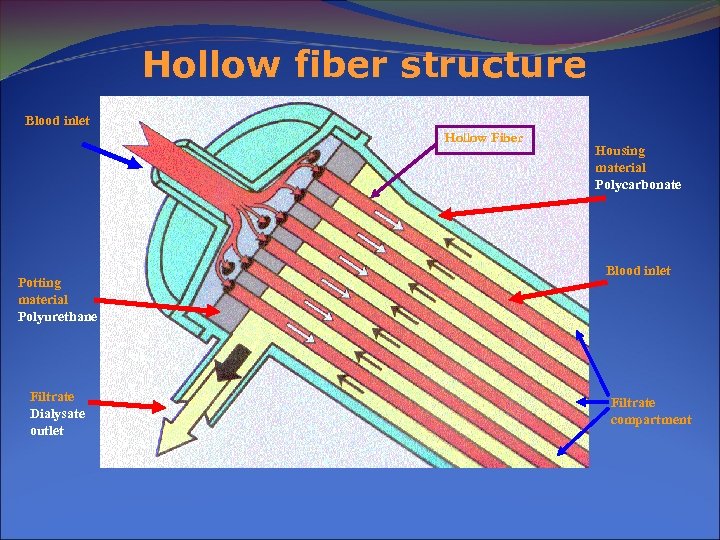
Hollow fiber structure Blood inlet Hollow Fiber Potting material Polyurethane Filtrate Dialysate outlet Housing material Polycarbonate Blood inlet Filtrate compartment
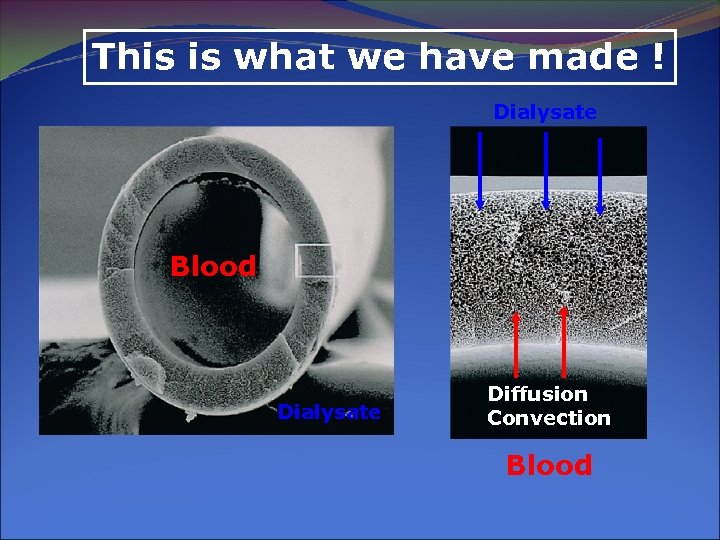
This is what we have made ! Dialysate Blood Dialysate Diffusion Convection Blood
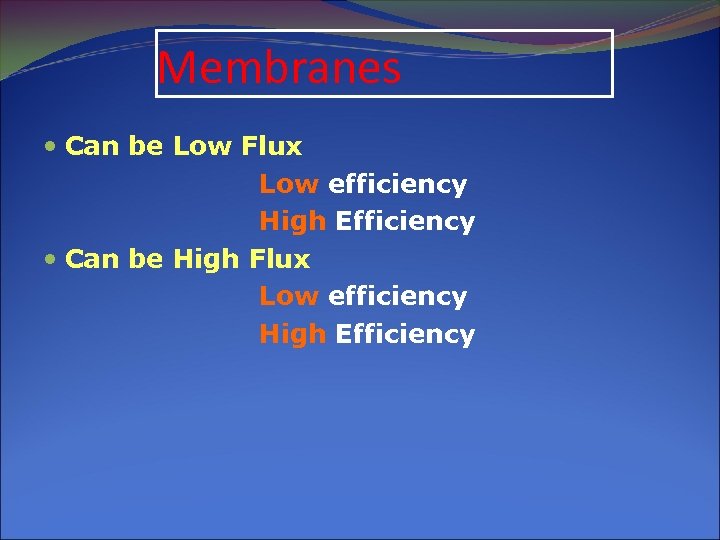
Membranes Can be Low Flux Low efficiency High Efficiency Can be High Flux Low efficiency High Efficiency
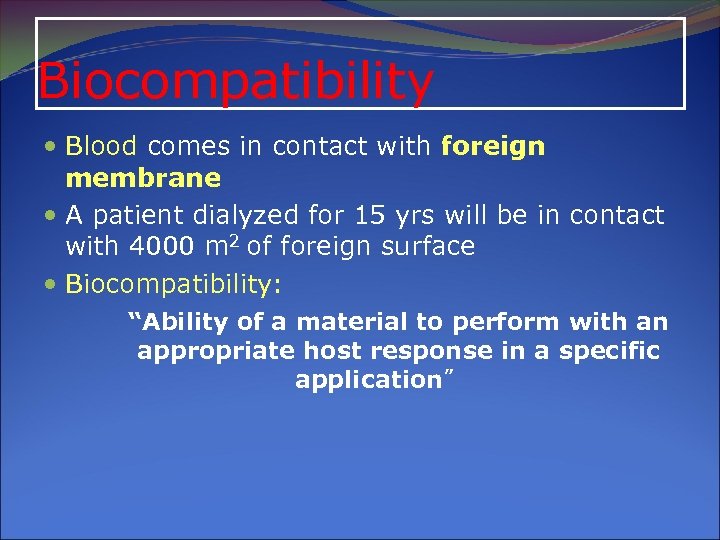
Biocompatibility Blood comes in contact with foreign membrane A patient dialyzed for 15 yrs will be in contact with 4000 m 2 of foreign surface Biocompatibility: “Ability of a material to perform with an appropriate host response in a specific application”
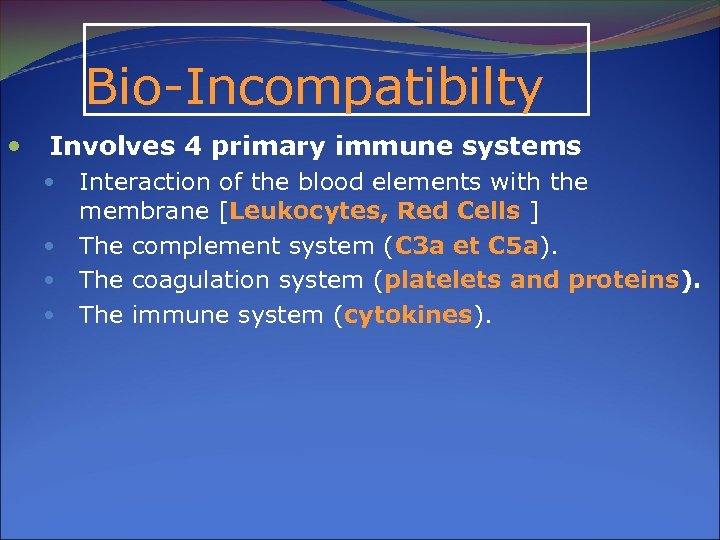
Bio-Incompatibilty Involves 4 primary immune systems Interaction of the blood elements with the membrane [Leukocytes, Red Cells ] The complement system (C 3 a et C 5 a). The coagulation system (platelets and proteins). The immune system (cytokines).
![Clinical Consequences Hypersensitivity reactions Infections Β-2 Microglobulin[ Dialysis Related Amyloidosis] Malnutrition Renal Reserve decline Clinical Consequences Hypersensitivity reactions Infections Β-2 Microglobulin[ Dialysis Related Amyloidosis] Malnutrition Renal Reserve decline](https://present5.com/presentation/bda4f6d6f5029716bfde70dae5c52381/image-64.jpg)
Clinical Consequences Hypersensitivity reactions Infections Β-2 Microglobulin[ Dialysis Related Amyloidosis] Malnutrition Renal Reserve decline
![Synthetic Polysulfone [PS] PS + Polyvinylpyrrolidine [PS] Polyarlyethersulfone [PES] Polymethylmetacrylate [PMMA] Polyacrylonitrile [PAN] Polycarbonate Synthetic Polysulfone [PS] PS + Polyvinylpyrrolidine [PS] Polyarlyethersulfone [PES] Polymethylmetacrylate [PMMA] Polyacrylonitrile [PAN] Polycarbonate](https://present5.com/presentation/bda4f6d6f5029716bfde70dae5c52381/image-65.jpg)
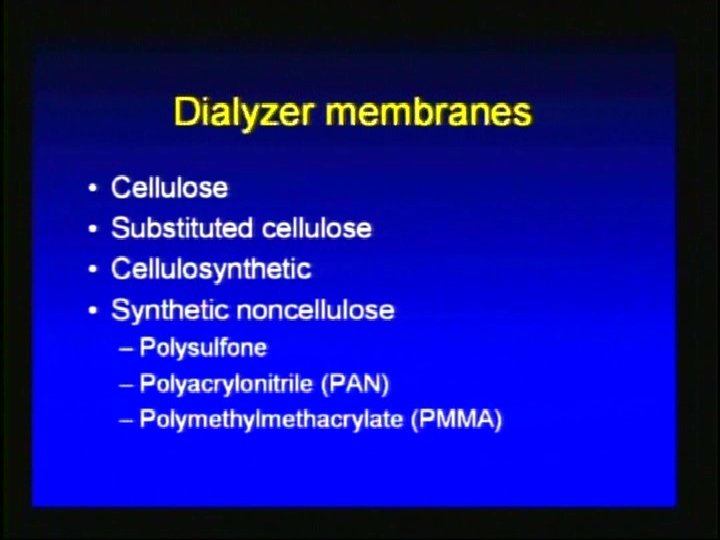
Synthetic Polysulfone [PS] PS + Polyvinylpyrrolidine [PS] Polyarlyethersulfone [PES] Polymethylmetacrylate [PMMA] Polyacrylonitrile [PAN] Polycarbonate [PC] Polycarbonate Polyether [Gambrane] Helixone –PS using nanotechnology
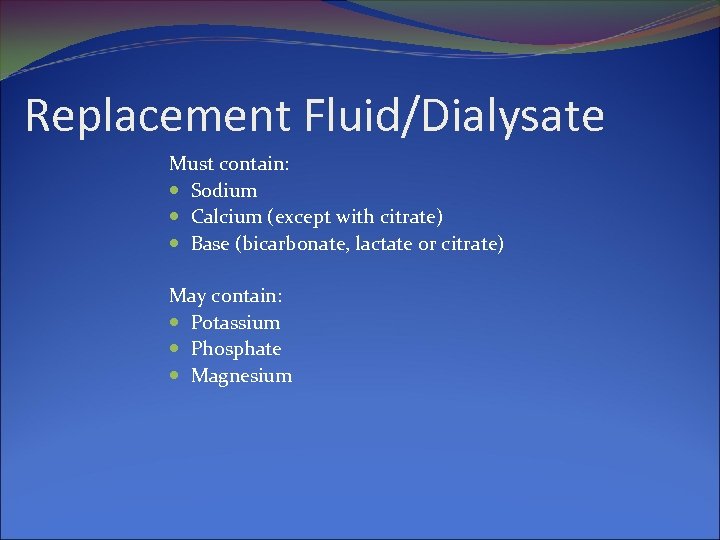
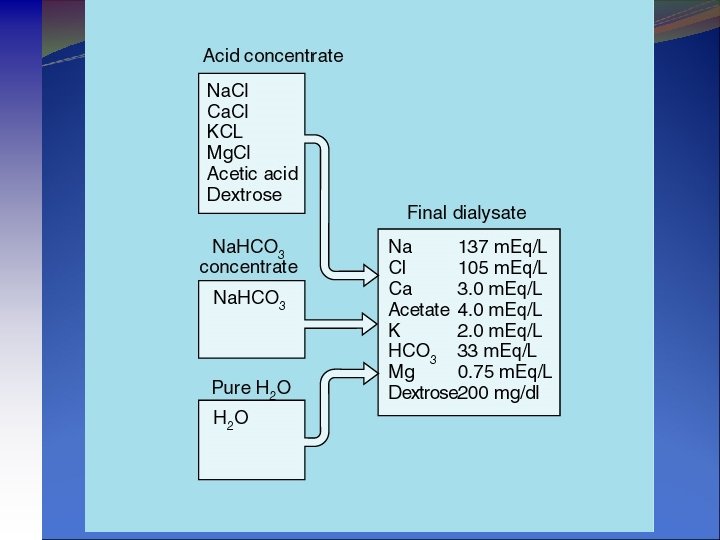
Replacement Fluid/Dialysate Must contain: Sodium Calcium (except with citrate) Base (bicarbonate, lactate or citrate) May contain: Potassium Phosphate Magnesium
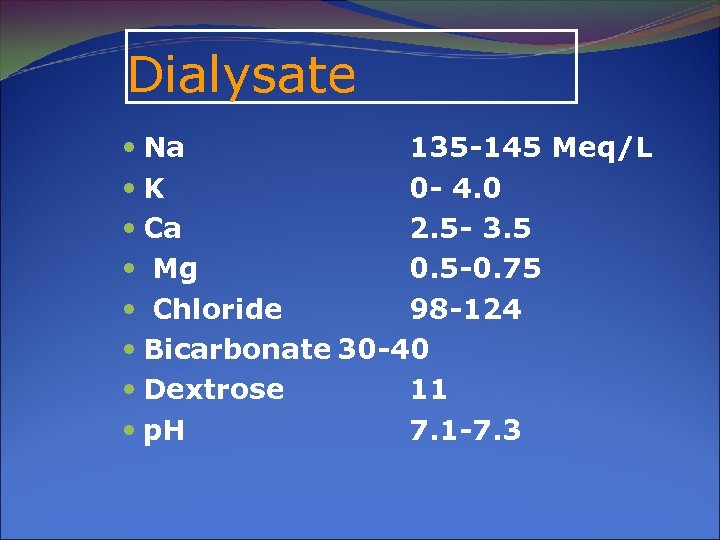
Dialysate Na 135 -145 Meq/L K 0 - 4. 0 Ca 2. 5 - 3. 5 Mg 0. 5 -0. 75 Chloride 98 -124 Bicarbonate 30 -40 Dextrose 11 p. H 7. 1 -7. 3
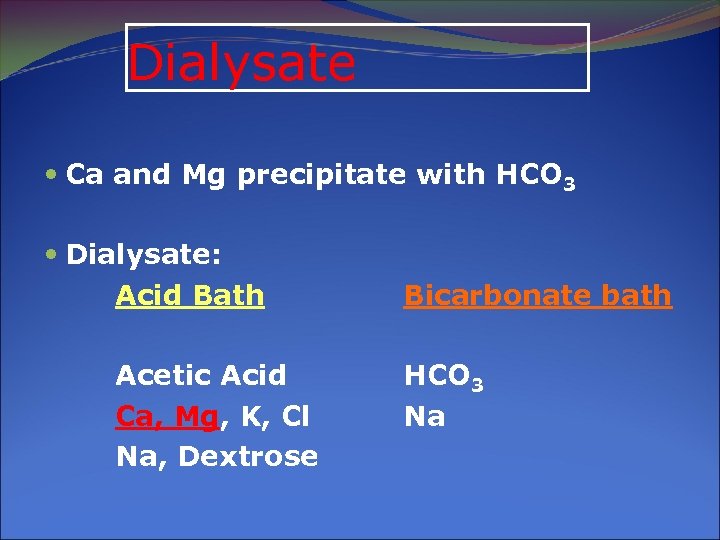
Dialysate Ca and Mg precipitate with HCO 3 Dialysate: Acid Bath Acetic Acid Ca, Mg, K, Cl Na, Dextrose Bicarbonate bath HCO 3 Na
![Dialysate Mixing by the machine at the time of dialysis [1: 34, Dialysate: Water] Dialysate Mixing by the machine at the time of dialysis [1: 34, Dialysate: Water]](https://present5.com/presentation/bda4f6d6f5029716bfde70dae5c52381/image-70.jpg)
Dialysate Mixing by the machine at the time of dialysis [1: 34, Dialysate: Water] H+ + HCO 3 H 2 CO 3 p. H 7 -7. 4 No ppt of Ca & Mg
Factors Influencing Solute Removal Molecular weight of the solute Dialyzer Access BF Dialysate Time on dialysis Machine MODALITY ACCSES RECIRCULATION
WHAT IS IN CURRENT PRACTICE DAILY DIALYSIS ON LINE HDF HOME HD TIDAL HD AFB CITRASATE
Peritoneal Dialysis Ø The process takes place inside the body. Ø A tube (Tenckhoff catheter) is inserted into the abdominal cavity. Ø Special dialysis fluid is drained into the abdomen. Ø Excess waste and water pass from the blood into the fluid and after a few hours the fluid is drained out.
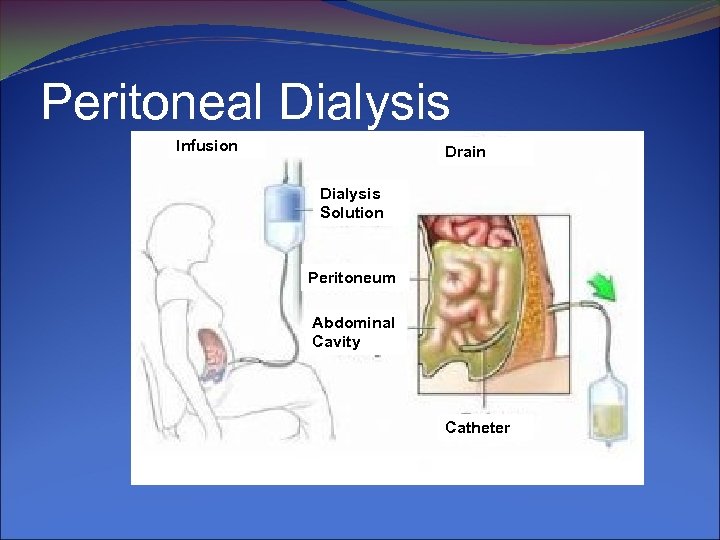
Peritoneal Dialysis Infusion Drain Dialysis Solution Peritoneum Abdominal Cavity Catheter
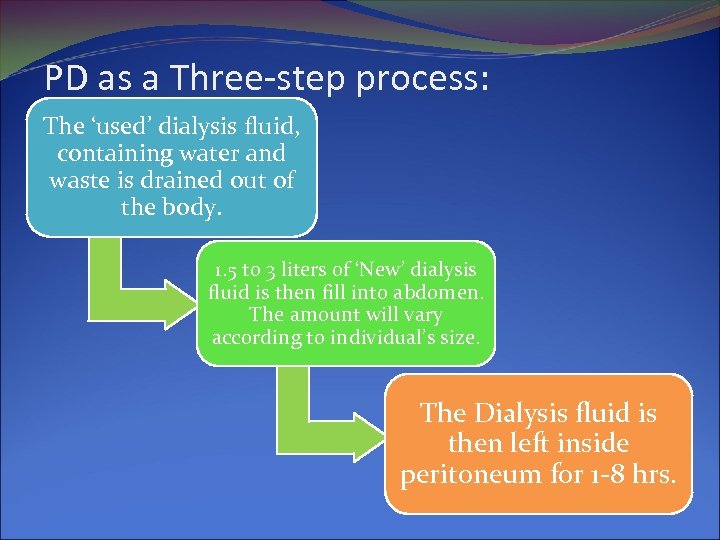
PD as a Three-step process: The ‘used’ dialysis fluid, containing water and waste is drained out of the body. 1. 5 to 3 liters of ‘New’ dialysis fluid is then fill into abdomen. The amount will vary according to individual’s size. The Dialysis fluid is then left inside peritoneum for 1 -8 hrs.
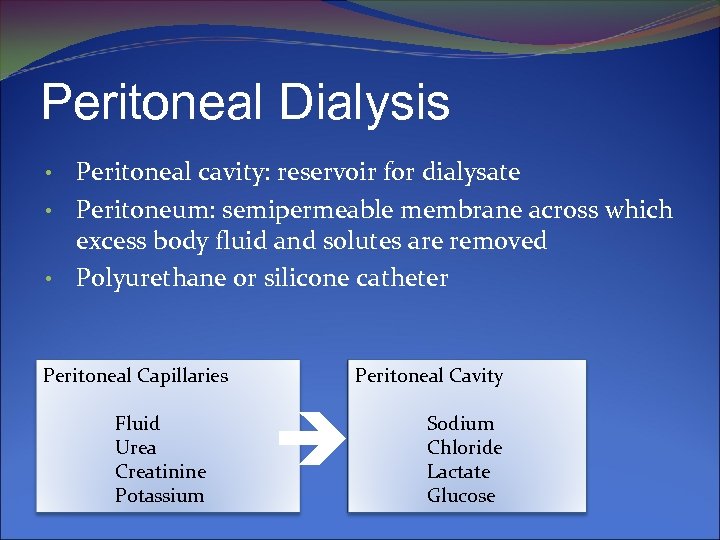
Peritoneal Dialysis Peritoneal cavity: reservoir for dialysate • Peritoneum: semipermeable membrane across which excess body fluid and solutes are removed • Polyurethane or silicone catheter • Peritoneal Capillaries Fluid Urea Creatinine Potassium Peritoneal Cavity Sodium Chloride Lactate Glucose
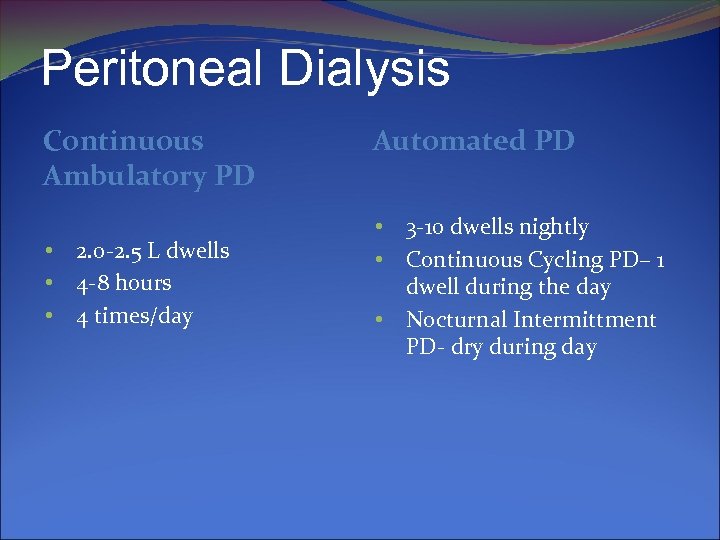
Peritoneal Dialysis Continuous Ambulatory PD • • • 2. 0 -2. 5 L dwells 4 -8 hours 4 times/day Automated PD • • • 3 -10 dwells nightly Continuous Cycling PD– 1 dwell during the day Nocturnal Intermittment PD- dry during day
CAPD Dialysis takes place 24 hrs a day, 7 days a week Patient is not attached to a machine for treatment Exchanges are usually carried out by patient after training by a CAPD nurse Most patients need 3 -5 exchanges a day i. e. 4 -6 hour intervals (Dwell time) 30 mins per exchange May use 2 -3 litres of fluid in abdomen No needles are used Less dietary and fluid restriction
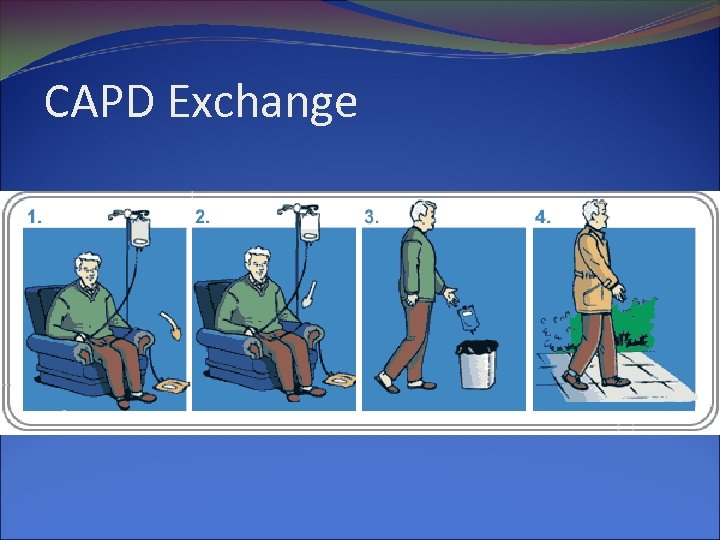
CAPD Exchange
APD Uses a home based machine to perform exchanges Overnight treatment whilst patient sleeps The APD machine controls the timing of exchanges, drains the used solution and fills the peritoneal cavity with new solution Simple procedure for the patient to perform Requires about 8 -10 hrs Machines are portable, with in-built safety features and requires electricity to operate
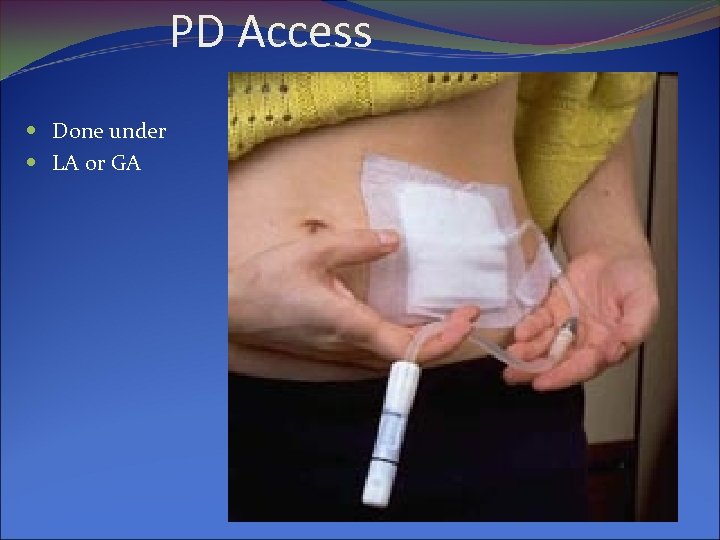
PD Access Done under LA or GA

APD
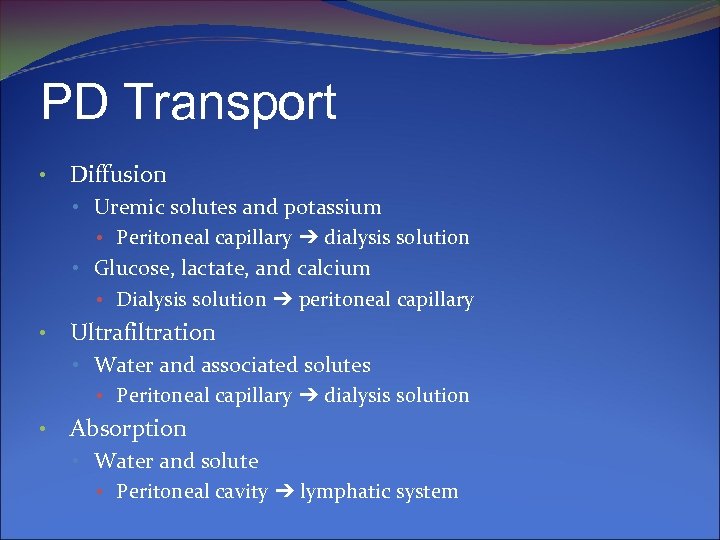
PD Transport • Diffusion • Uremic solutes and potassium • Peritoneal capillary ➔ dialysis solution • Glucose, lactate, and calcium • Dialysis solution ➔ peritoneal capillary • Ultrafiltration • Water and associated solutes • Peritoneal capillary ➔ dialysis solution • Absorption • Water and solute • Peritoneal cavity ➔ lymphatic system
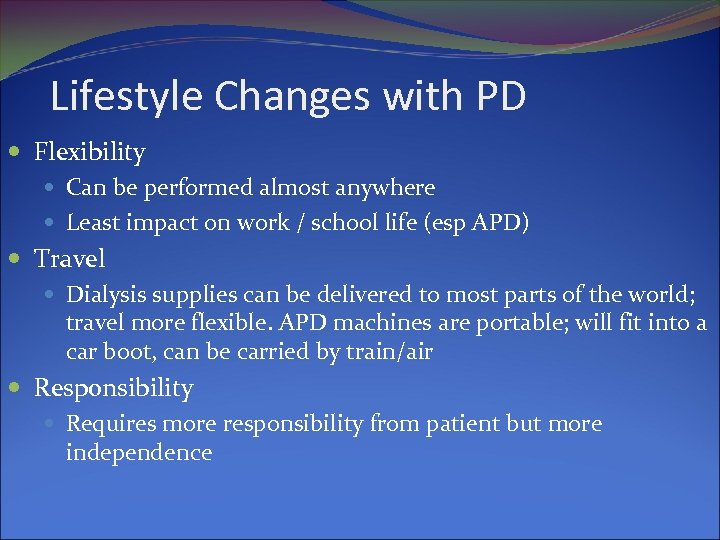
Lifestyle Changes with PD Flexibility Can be performed almost anywhere Least impact on work / school life (esp APD) Travel Dialysis supplies can be delivered to most parts of the world; travel more flexible. APD machines are portable; will fit into a car boot, can be carried by train/air Responsibility Requires more responsibility from patient but more independence
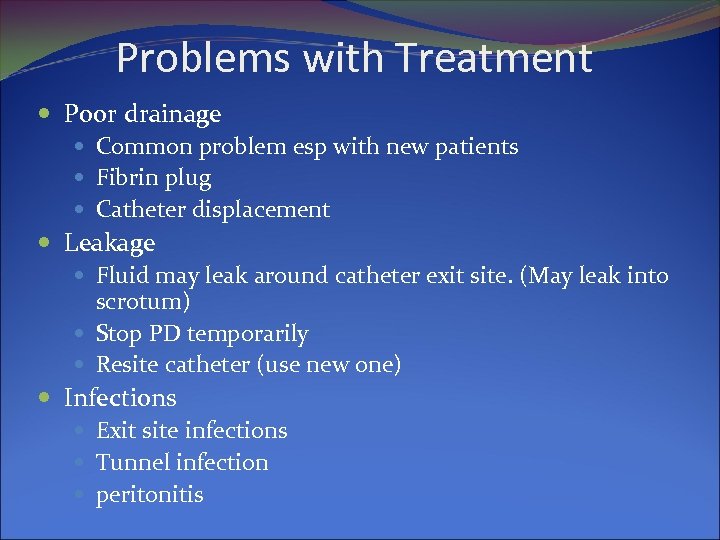
Problems with Treatment Poor drainage Common problem esp with new patients Fibrin plug Catheter displacement Leakage Fluid may leak around catheter exit site. (May leak into scrotum) Stop PD temporarily Resite catheter (use new one) Infections Exit site infections Tunnel infection peritonitis
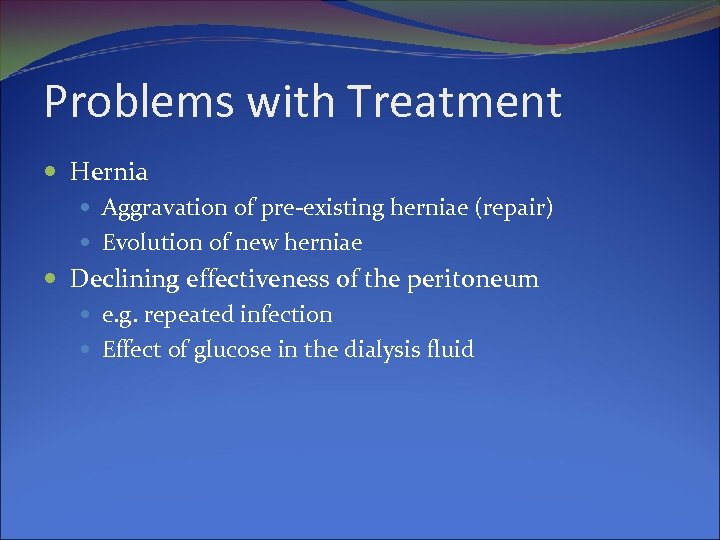
Problems with Treatment Hernia Aggravation of pre-existing herniae (repair) Evolution of new herniae Declining effectiveness of the peritoneum e. g. repeated infection Effect of glucose in the dialysis fluid
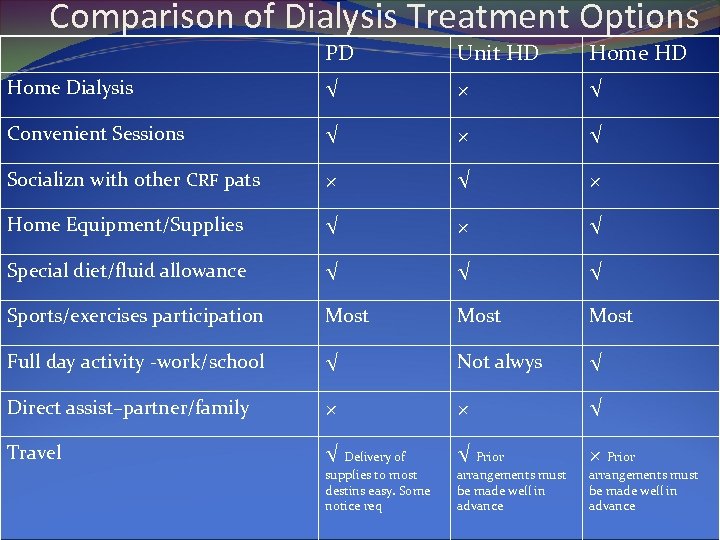
Comparison of Dialysis Treatment Options PD Unit HD Home Dialysis √ × √ Convenient Sessions √ × √ Socializn with other CRF pats × √ × Home Equipment/Supplies √ × √ Special diet/fluid allowance √ √ √ Sports/exercises participation Most Full day activity -work/school √ Not alwys √ Direct assist–partner/family × × √ Travel √ Delivery of √ Prior × Prior supplies to most destins easy. Some notice req arrangements must be made well in advance

THANKS e-mail: drnavaslam@gmail. com
bda4f6d6f5029716bfde70dae5c52381.ppt